UNIT II Cardiovascular System Hypertension Cardiovascular System Hypertension
- Slides: 25
UNIT II Cardiovascular System Hypertension
• Cardiovascular System: – Hypertension, – Congestive Heart Failure – Ischemic Heart Disease • • Angina Myocardial Infarction Atherosclerosis Arteriosclerosis
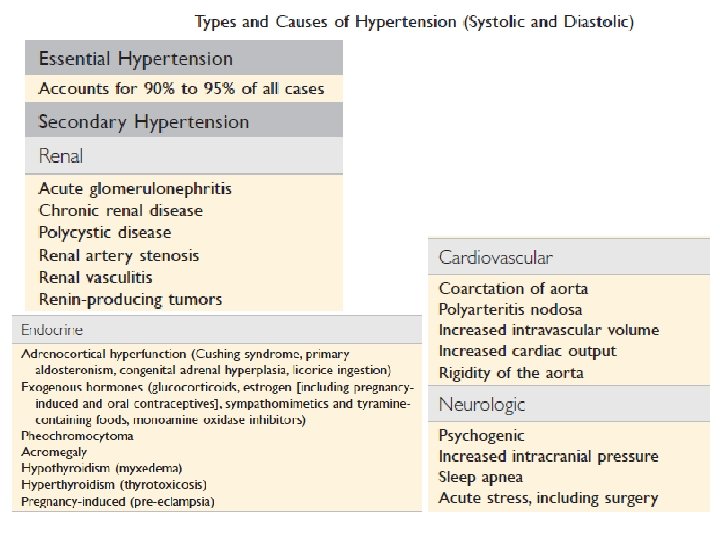
HYPERTENSION • 120/80 • top number is systolic blood pressure. – highest pressure when your heart beats and pushes the blood round your body • bottom one is diastolic blood pressure. – lowest pressure when your heart relaxes between beats • Systemic and local blood pressure: need to maintained within a narrow range to prevent adverse outcomes. • Low blood pressure (hypotension) results in inadequate organ perfusion, organ dysfunction, and sometimes tissue death. • High blood pressure (hypertension) causes vessel and endorgan damage and major risk factors for atherosclerosis.
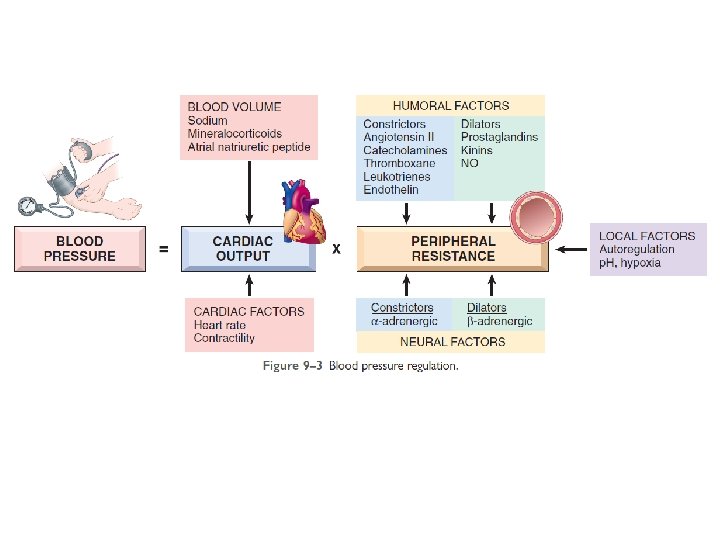
• Blood pressure is a function of cardiac output and peripheral vascular resistance, • both of which are influenced by multiple genetic and environmental factors. • heart attack, heart failure, stroke and kidney disease
• integration of various inputs ensures adequate systemic perfusion, despite regional demand differences. • Cardiac output is a function of stroke volume and heart rate. • The most important determinant of stroke volume is filling pressure, which is regulated through sodium homeostasis and its effect on blood volume. • Heart rate and myocardial contractility (a second factor affecting stroke volume) are both regulated by the α- and β-adrenergic systems (in addition to their effects on vascular tone).
• Peripheral resistance is regulated predominantly at level of the arterioles by neural and hormonal inputs. • Vascular tone reflects a balance between vasoconstrictors (including angiotensin II, catecholamines, and endothelin) and vasodilators (including kinins, prostaglandins, and NO). • Resistance vessels also exhibit autoregulation, increased blood flow induces vasoconstriction to protect tissues against hyperperfusion. • Blood pressure is fine-tuned by – tissue p. H and – hypoxia • to accommodate local metabolic demands.
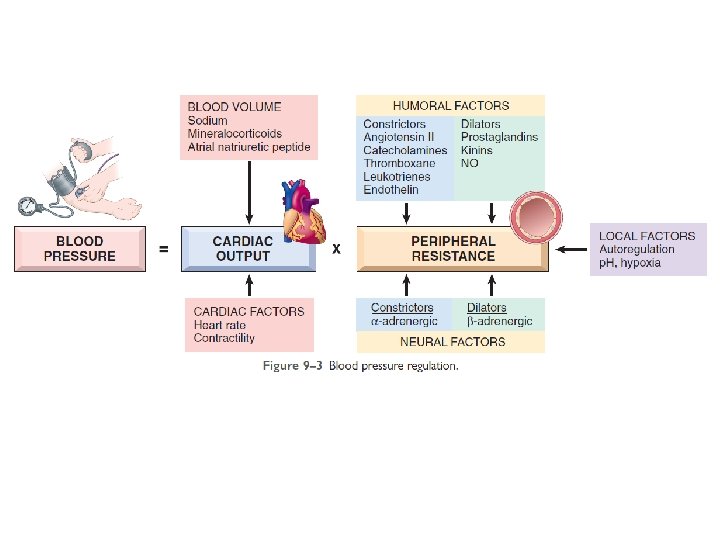
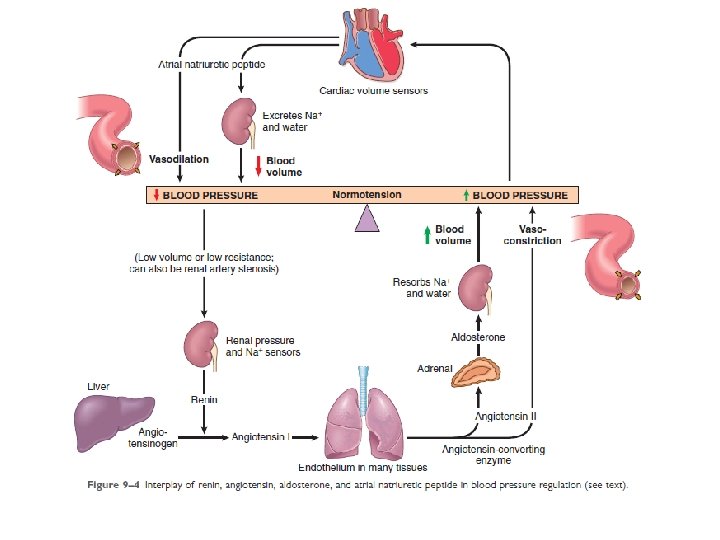
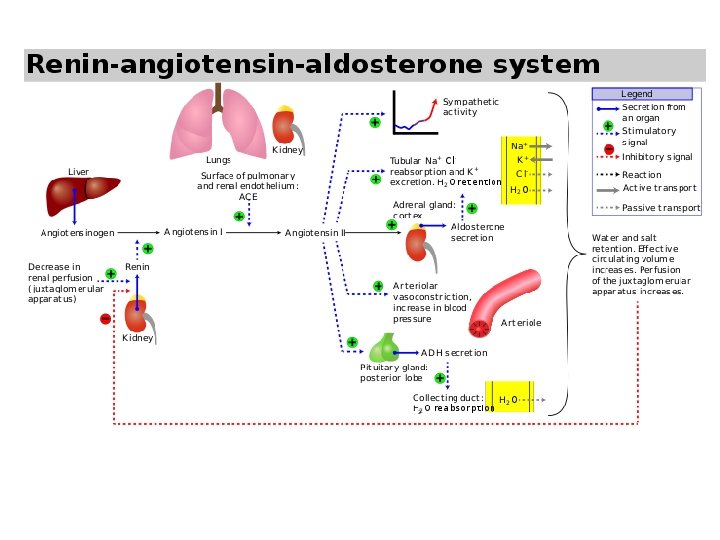
• Factors released from the kidneys, adrenals, and myocardium interact to influence vascular tone and to regulate blood volume – by adjusting sodium balance. • kidneys filters approx. 180 liters of plasma (total blood, 60 times a day) • 99. 5% of the filtered salt must be reabsorbed to maintain total body sodium levels • About 98% of the filtered sodium: reabsorbed by active transporters • Recovery of the remaining 2% of sodium occurs by way of epithelial sodium channel (ENa. C), – tightly regulated by the renin–angiotensin system – determines net sodium balance
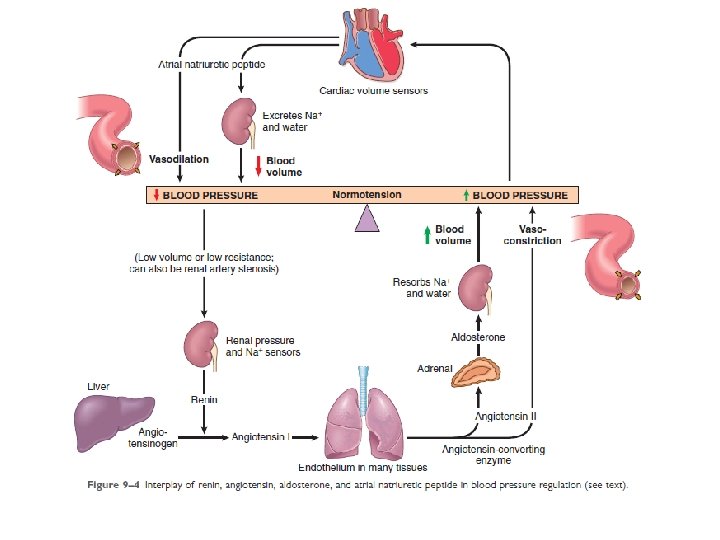
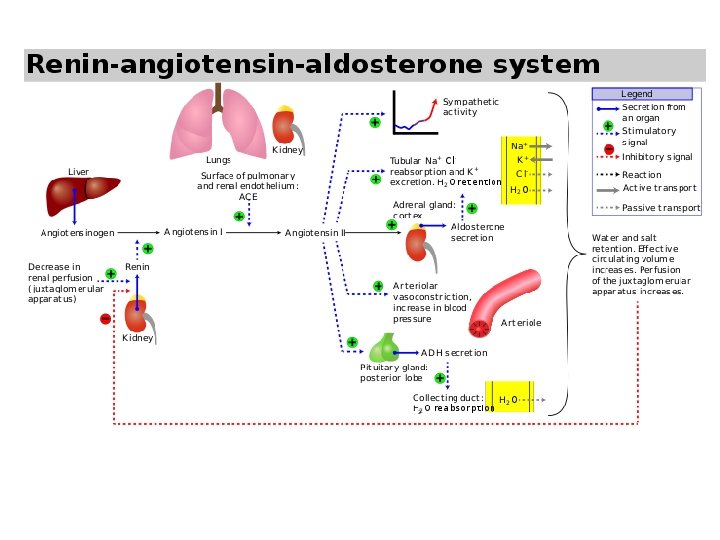
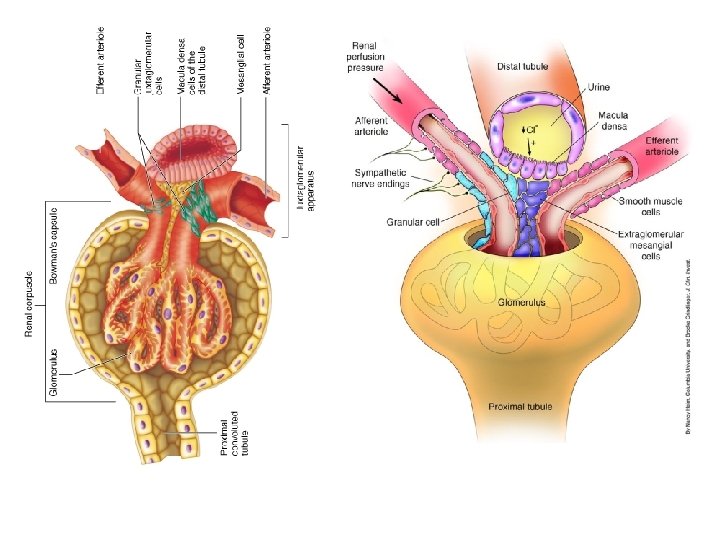
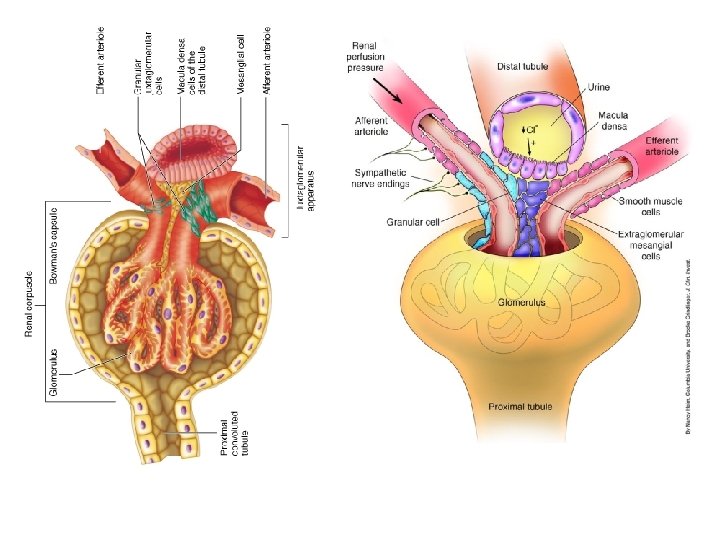
• Kidneys affect (by renin– angiotensin system) – peripheral resistance and – sodium excretion/retention • Cells that sense changes in blood pressure or blood volume present: – kidneys – heart
• These cells release several important regulators to maintain normal blood pressure, as follows: • Renin is a proteolytic enzyme produced by renal juxtaglomerular cells, myoepithelial cells that surround the glomerular afferent arterioles. • released in response to – low blood pressure in afferent arterioles – elevated levels of circulating catecholamines – low sodium levels in the distal convoluted tubules • (glomerular filtration rate falls (e. g. , when the cardiac output is low), • leading to increased sodium resorption by the proximal tubules and • leads to lower sodium levels at distil part of glomerules)
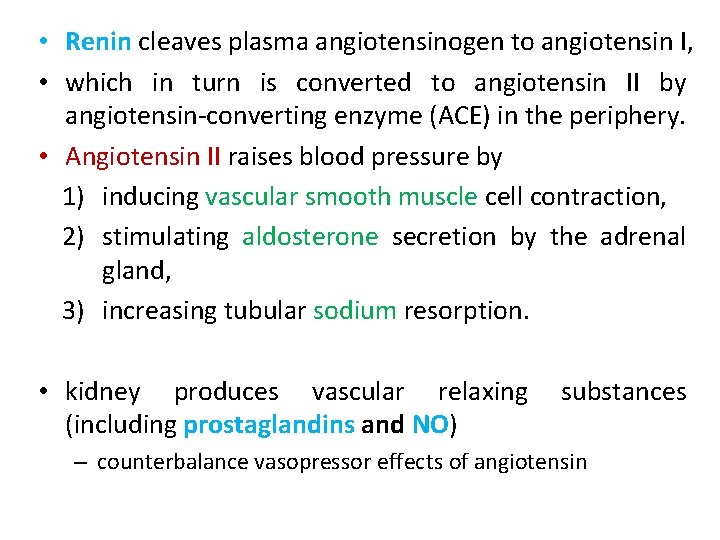
• Renin cleaves plasma angiotensinogen to angiotensin I, • which in turn is converted to angiotensin II by angiotensin-converting enzyme (ACE) in the periphery. • Angiotensin II raises blood pressure by 1) inducing vascular smooth muscle cell contraction, 2) stimulating aldosterone secretion by the adrenal gland, 3) increasing tubular sodium resorption. • kidney produces vascular relaxing (including prostaglandins and NO) substances – counterbalance vasopressor effects of angiotensin
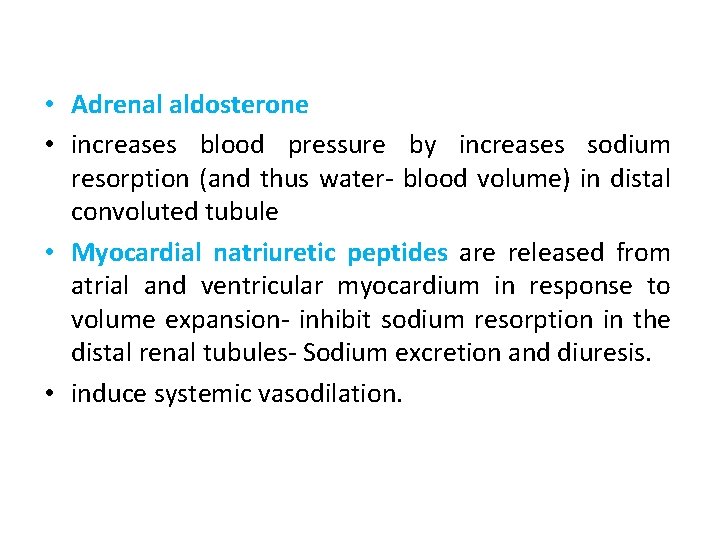
• Adrenal aldosterone • increases blood pressure by increases sodium resorption (and thus water- blood volume) in distal convoluted tubule • Myocardial natriuretic peptides are released from atrial and ventricular myocardium in response to volume expansion- inhibit sodium resorption in the distal renal tubules- Sodium excretion and diuresis. • induce systemic vasodilation.
HYPERTENSION • associated with considerable morbidity and affecting many organs, including heart, brain, and kidneys. • cardiac complications of hypertension- result from – Pressure overload – Ventricular hypertrophy • Myocyte hypertrophy- adaptive response to pressure overload (there are limits to adapt) • Persistent hypertension can results in dysfunction, cardiac dilation, CHF, and even sudden death. – Systemic hypertension- left side of heart – Pulmonary hypertension cause right-sided hypertensive changes—so-called cor pulmonale.
• criteria for diagnosis of systemic hypertensive heart disease are 1. left ventricular hypertrophy in absence of other cardiovascular pathology (e. g. , valvular stenosis) 2. history or pathologic evidence of hypertension
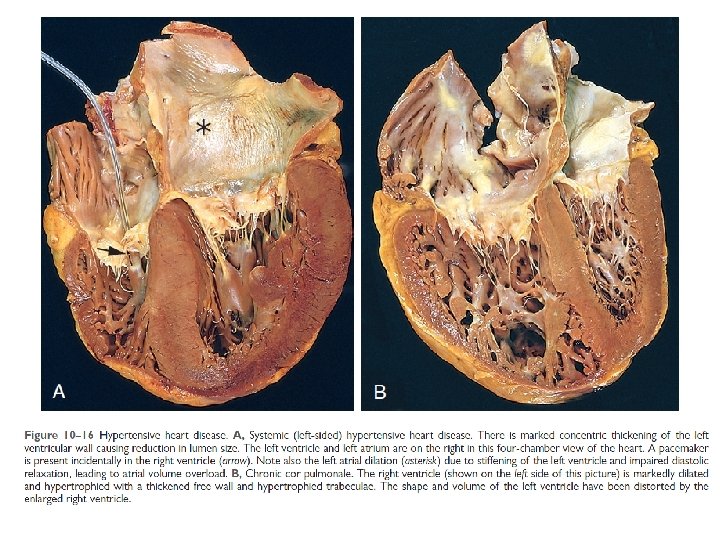
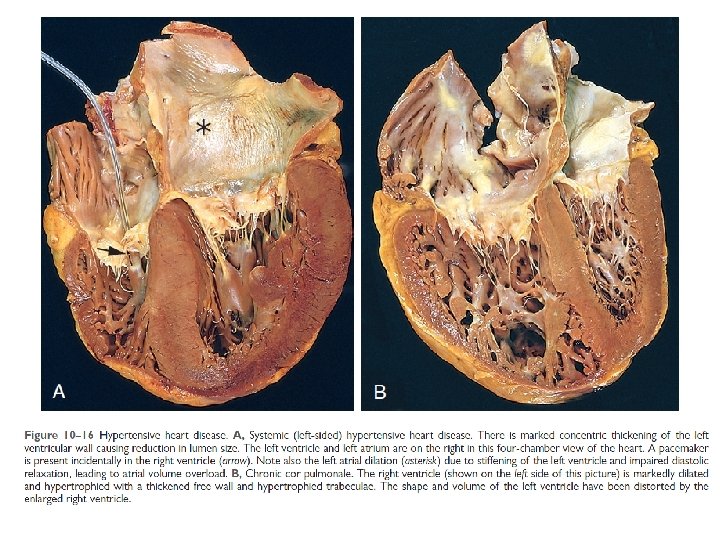
• Systemic hypertension imposes pressure overload on heart - gross and microscopic changes • Essential feature of systemic hypertensive heart disease is left ventricular hypertrophy • heart weight can exceed 500 g (normal, 320 to 360 g), • left ventricular wall thickness can exceed 2. 0 cm (normal, 1. 2 to 1. 4 cm). • With time, increased left ventricular wall thickness imparts a stiffness that impairs diastolic filling and can result in left atrial dilation.
• Depending on the severity and duration of the condition, underlying cause of hypertension, and adequacy of therapeutic control, patients can 1. Have normal life and die of unrelated causes 2. Develop progressive IHD -potentiating coronary atherosclerosis 3. Suffer progressive renal damage or cerebrovascular stroke 4. Experience progressive heart failure
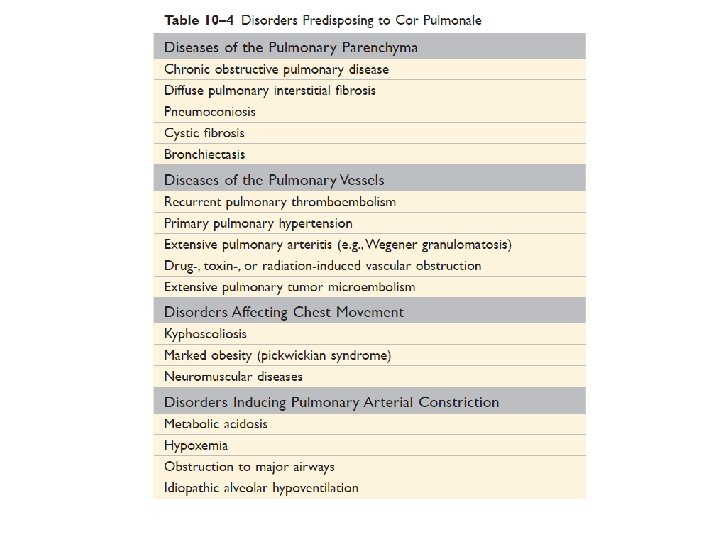
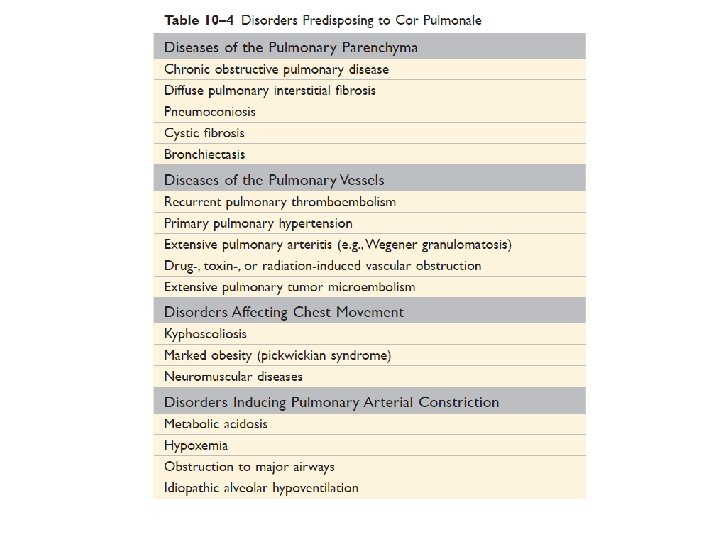
• Cor pulmonale consists of right ventricular hypertrophy and dilation—accompanied by right heart failure • caused by pulmonary hypertension attributable to primary disorders of the lung parenchyma or pulmonary vasculature • Cor pulmonale can be – acute in onset, as with pulmonary embolism, or – can have a slow and insidious onset when due to prolonged pressure overloads • in chronic lung and pulmonary vascular disease
• In acute cor pulmonale, right ventricle - only dilation • an embolism may cause sudden death, heart may even be of normal size • Chronic cor pulmonale is characterized by right ventricular (and often right atrial) hypertrophy • In extreme cases, thickness of right ventricular wall may be comparable with or even exceed left ventricle • When ventricular failure develops, right ventricle and atrium are dilated • As chronic cor pulmonale occurs due to pulmonary hypertension, pulmonary arteries often contain atheromatous plaques and other lesions, – reflecting long standing pressure elevations
• Reference: Robbins, Basic Pathology by Elsevier