Unit 8 Notes Cardiac Muscle Cardiac muscle can




- Slides: 94
Unit 8 Notes
Cardiac Muscle • Cardiac muscle can contract spontaneously and independently, even if all nervous connections are severed • Different muscle cells in different areas have different rhythms – Atrial cells: 60 beats/min – Ventricular cells: 20 -40 beats/min • Because of this, we need a controlling system to regulate & coordinate contractions!
What controls the heart beating? • 2 controlling systems – Nerves of Autonomic Nervous System • Acts like “brakes” and “accelerators” – Intrinsic Conduction System • AKA nodal system • Enforces a contraction rate to keep everything together
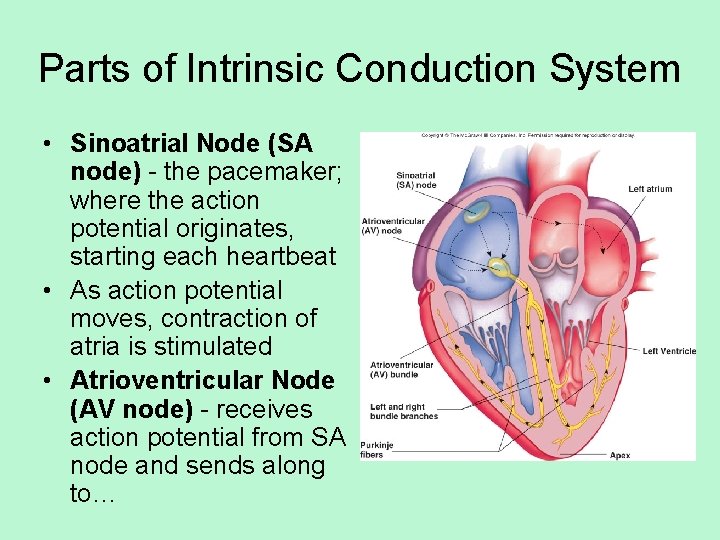
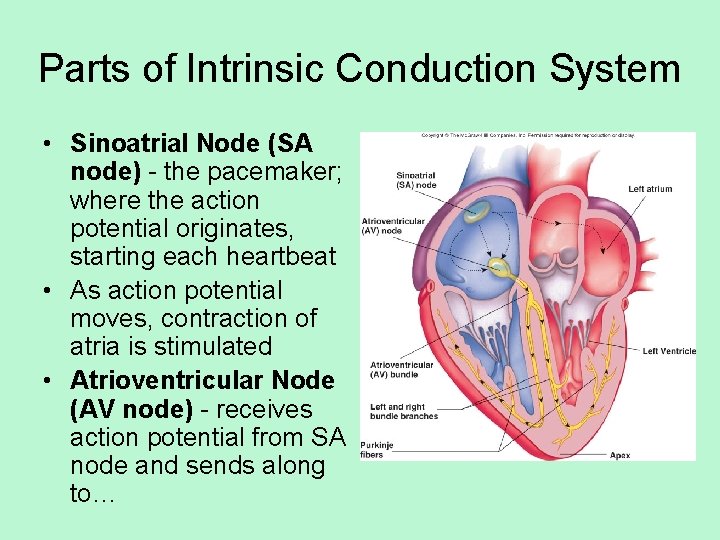
Parts of Intrinsic Conduction System • Sinoatrial Node (SA node) - the pacemaker; where the action potential originates, starting each heartbeat • As action potential moves, contraction of atria is stimulated • Atrioventricular Node (AV node) - receives action potential from SA node and sends along to…
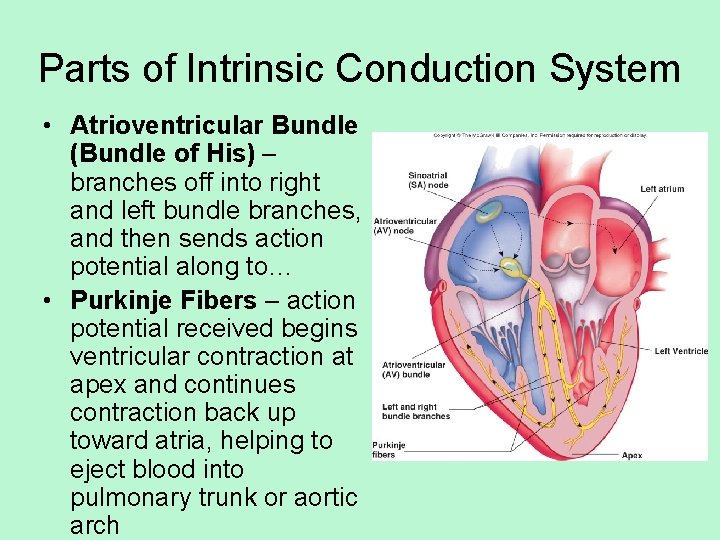
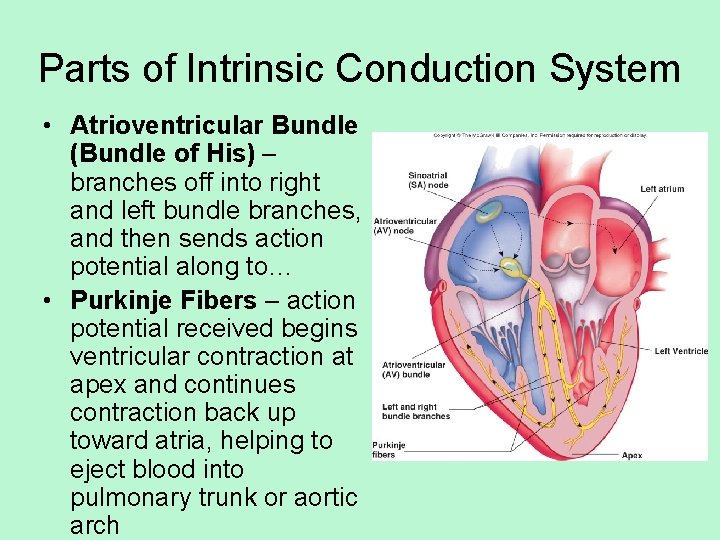
Parts of Intrinsic Conduction System • Atrioventricular Bundle (Bundle of His) – branches off into right and left bundle branches, and then sends action potential along to… • Purkinje Fibers – action potential received begins ventricular contraction at apex and continues contraction back up toward atria, helping to eject blood into pulmonary trunk or aortic arch
• http: //highered. mcgrawhill. com/sites/0072495855/student_view 0/ chapter 22/animation__conducting_system _of_the_heart. html
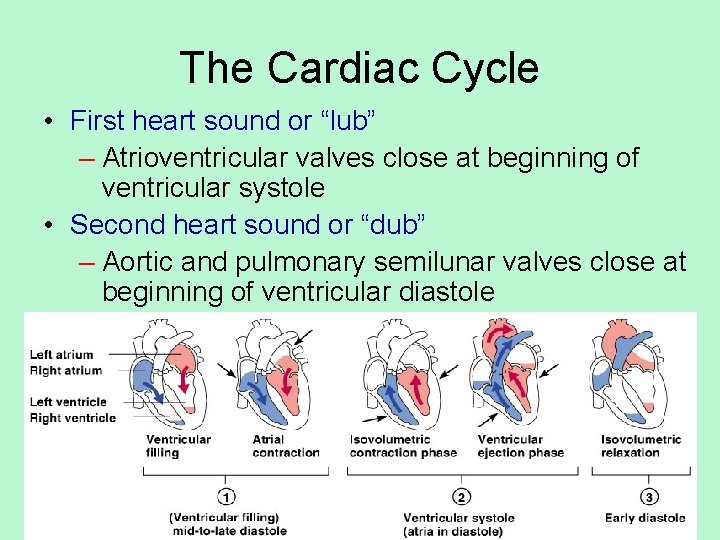
The Cardiac Cycle • • Refers to one complete heartbeat Systole – heart contraction Diastole – heart relaxation Since most of pumping done by ventricles, terms usually refer to ventricles (unless otherwise stated) • Normal length of cycle: 0. 8 seconds – Translates into 75 beats/min (average)
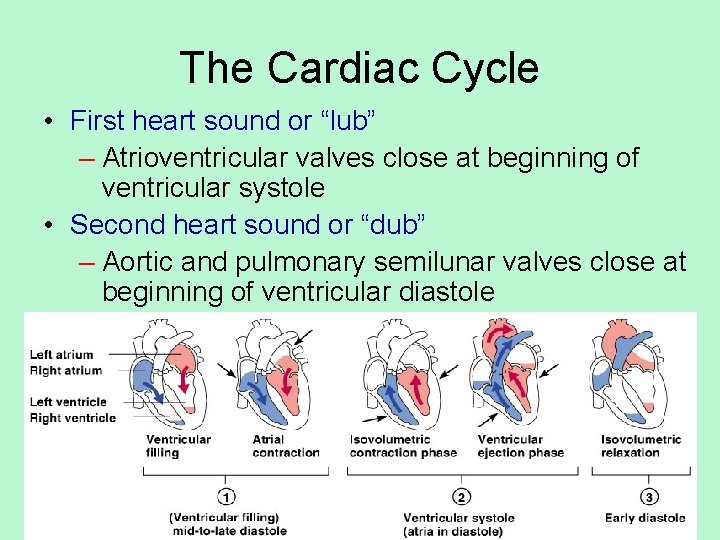
The Cardiac Cycle • First heart sound or “lub” – Atrioventricular valves close at beginning of ventricular systole • Second heart sound or “dub” – Aortic and pulmonary semilunar valves close at beginning of ventricular diastole
• http: //highered. mcgrawhill. com/sites/0072495855/student_view 0/ chapter 22/animation__the_cardiac_cycle_ _quiz_1_. html
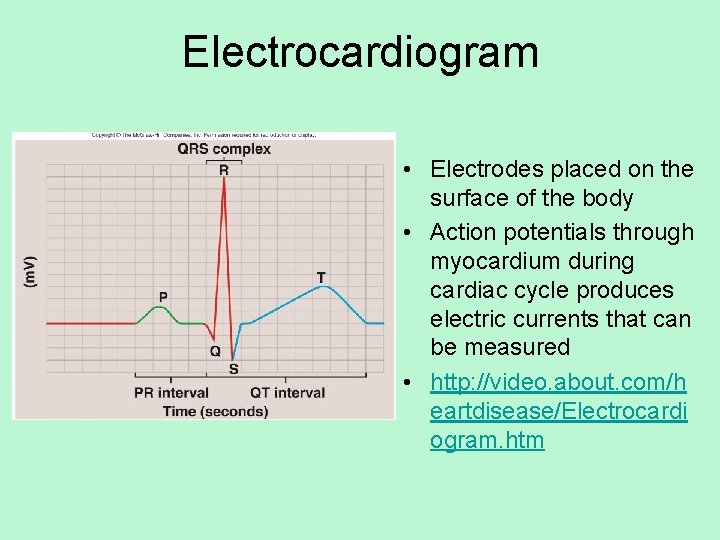
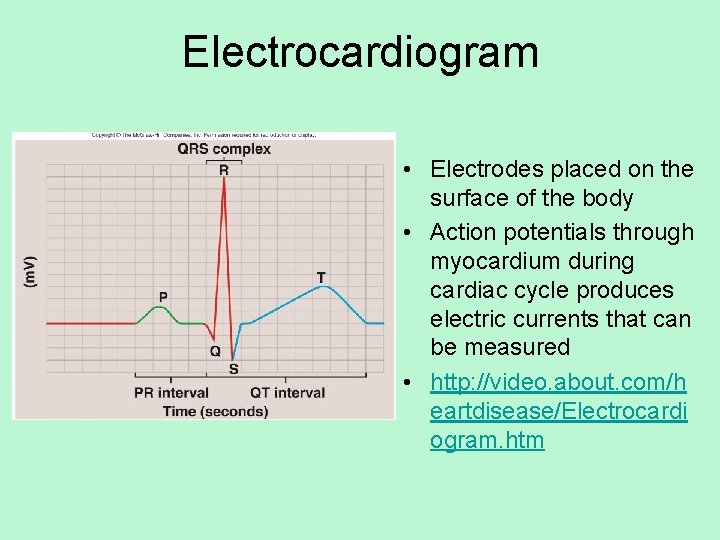
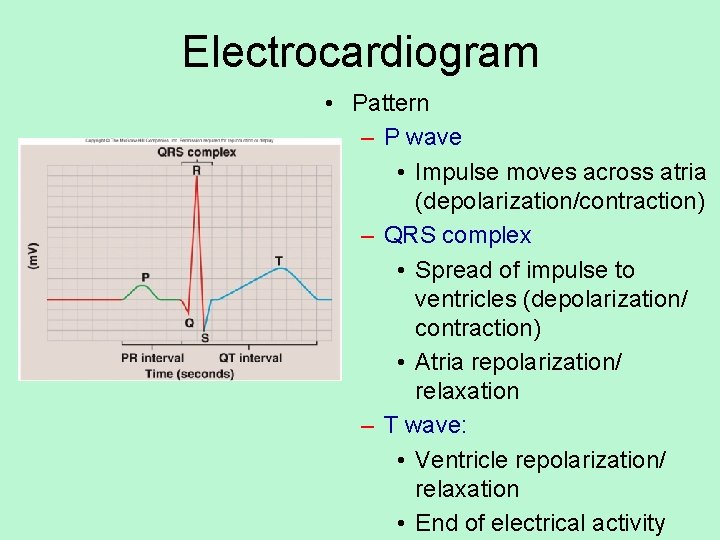
Electrocardiogram • Electrodes placed on the surface of the body • Action potentials through myocardium during cardiac cycle produces electric currents that can be measured • http: //video. about. com/h eartdisease/Electrocardi ogram. htm
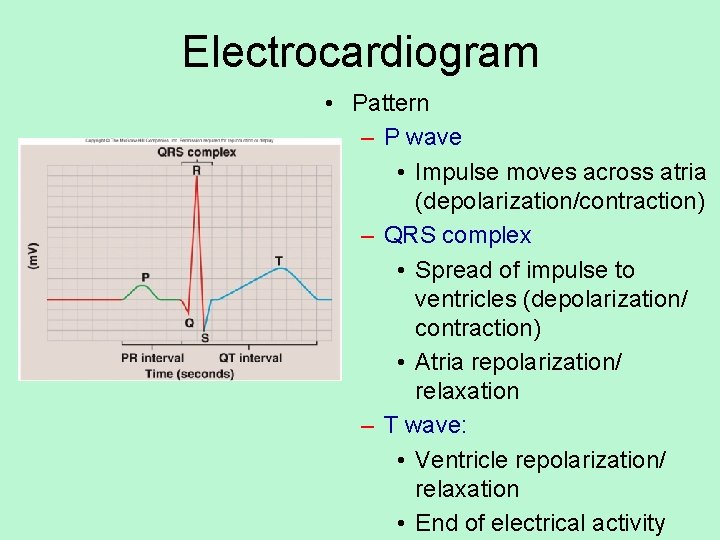
Electrocardiogram • Pattern – P wave • Impulse moves across atria (depolarization/contraction) – QRS complex • Spread of impulse to ventricles (depolarization/ contraction) • Atria repolarization/ relaxation – T wave: • Ventricle repolarization/ relaxation • End of electrical activity
Cardiac Arrhythmias • When any electrical activity of the heart is irregular
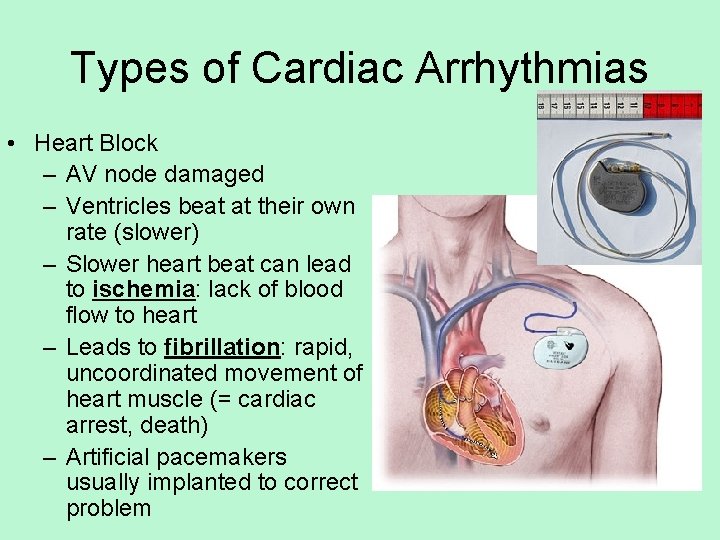
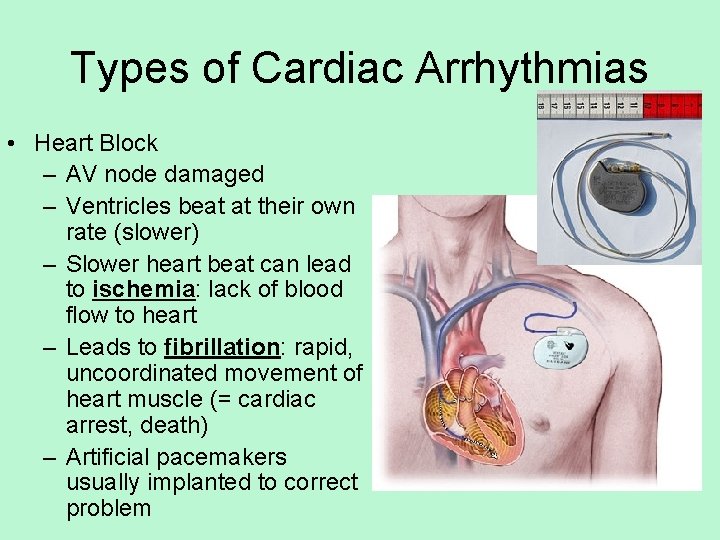
Types of Cardiac Arrhythmias • Heart Block – AV node damaged – Ventricles beat at their own rate (slower) – Slower heart beat can lead to ischemia: lack of blood flow to heart – Leads to fibrillation: rapid, uncoordinated movement of heart muscle (= cardiac arrest, death) – Artificial pacemakers usually implanted to correct problem
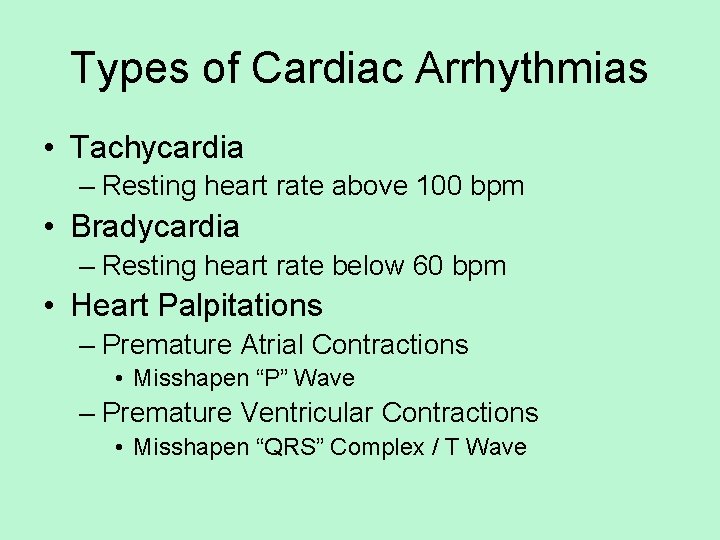
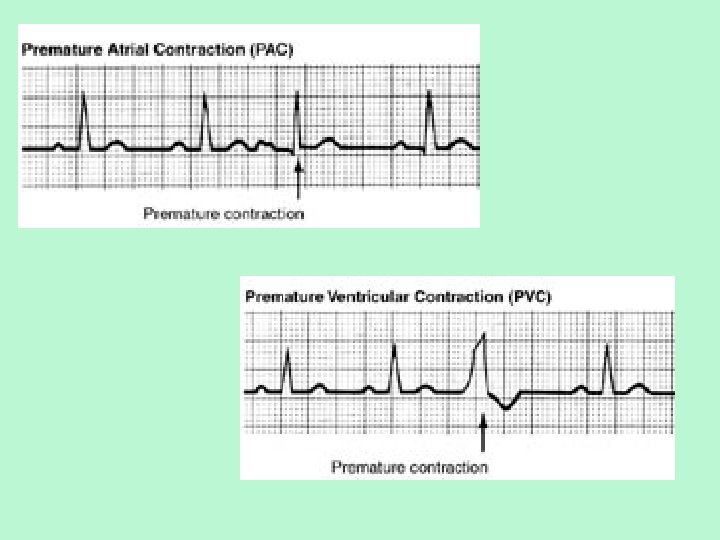
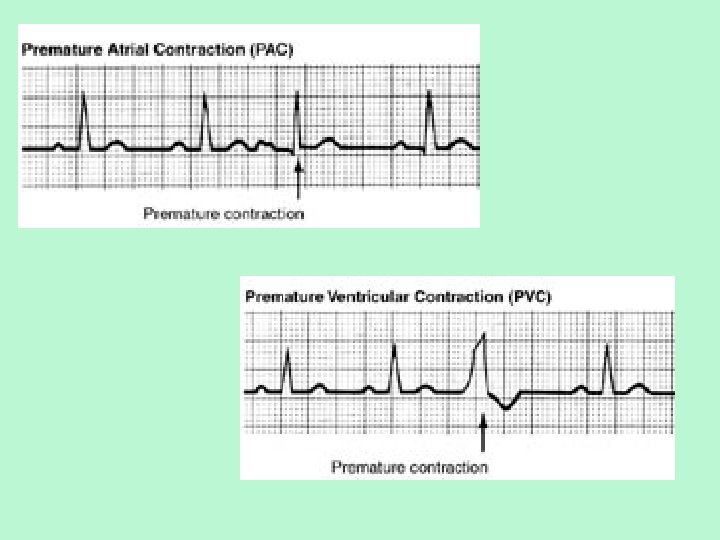
Types of Cardiac Arrhythmias • Tachycardia – Resting heart rate above 100 bpm • Bradycardia – Resting heart rate below 60 bpm • Heart Palpitations – Premature Atrial Contractions • Misshapen “P” Wave – Premature Ventricular Contractions • Misshapen “QRS” Complex / T Wave
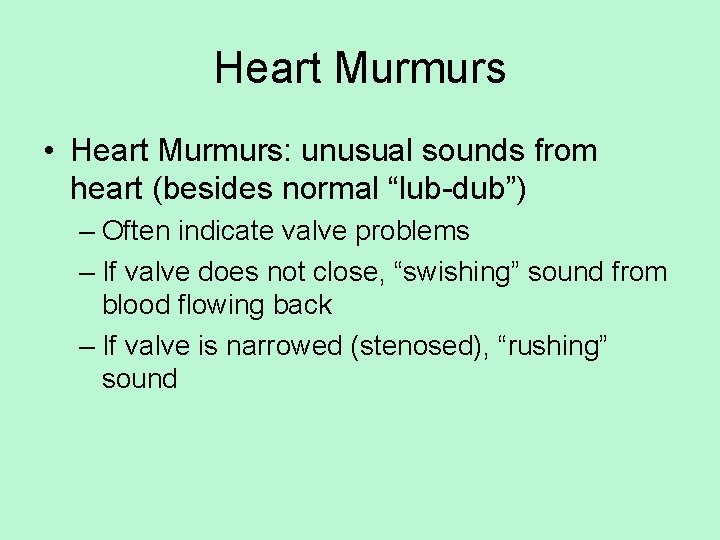
Heart Murmurs • Heart Murmurs: unusual sounds from heart (besides normal “lub-dub”) – Often indicate valve problems – If valve does not close, “swishing” sound from blood flowing back – If valve is narrowed (stenosed), “rushing” sound
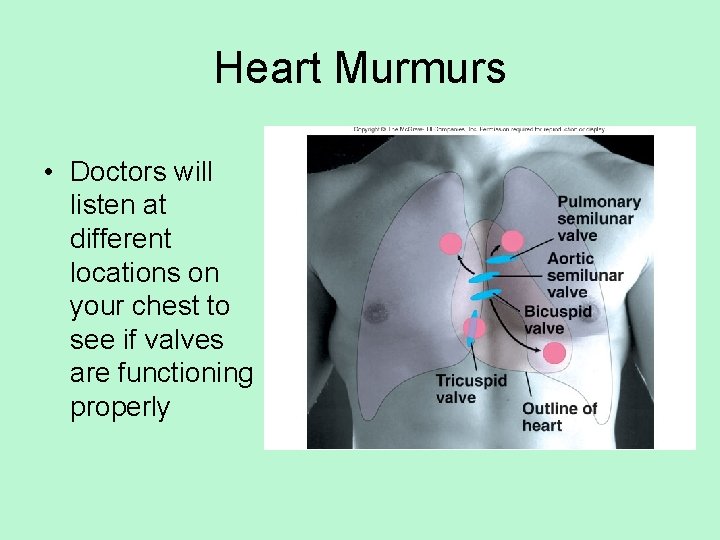
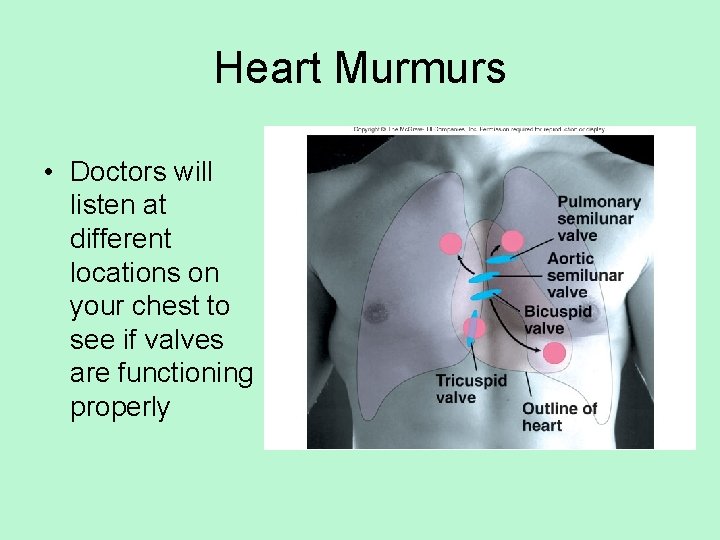
Heart Murmurs • Doctors will listen at different locations on your chest to see if valves are functioning properly

Now, let’s talk about blood flow in the rest of the body!!! The Vascular System: Taking Blood to the Body and Back
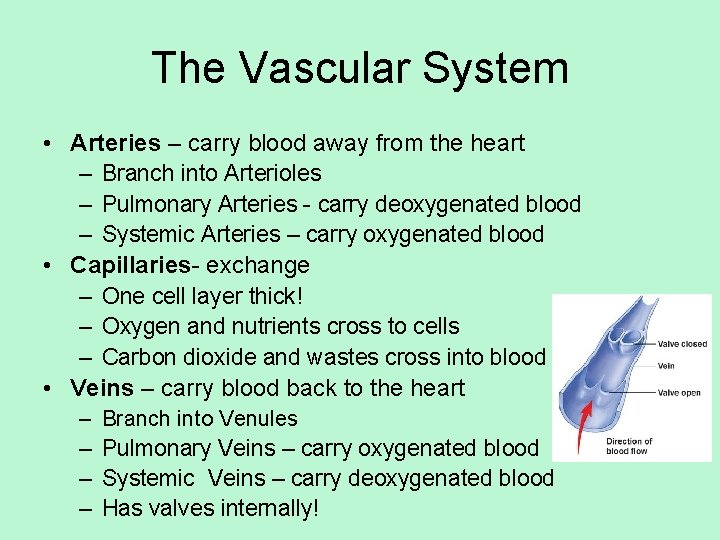
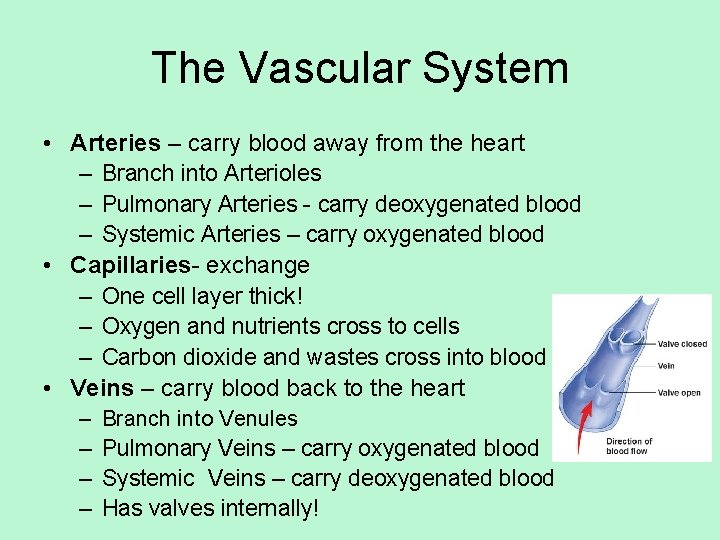
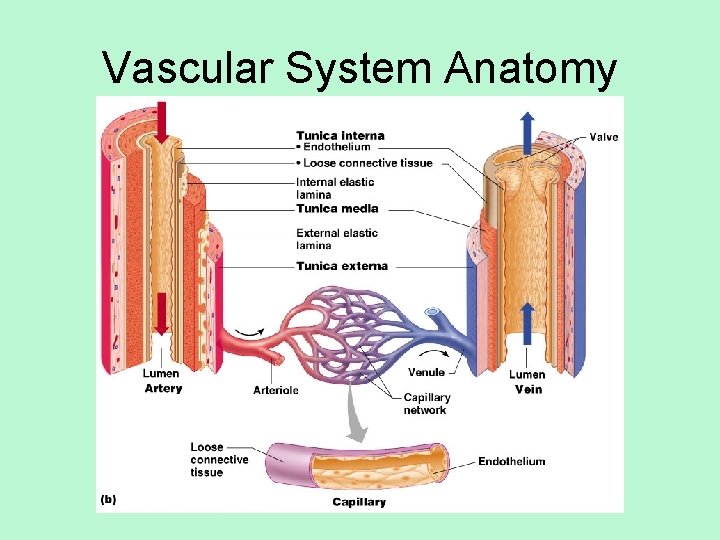
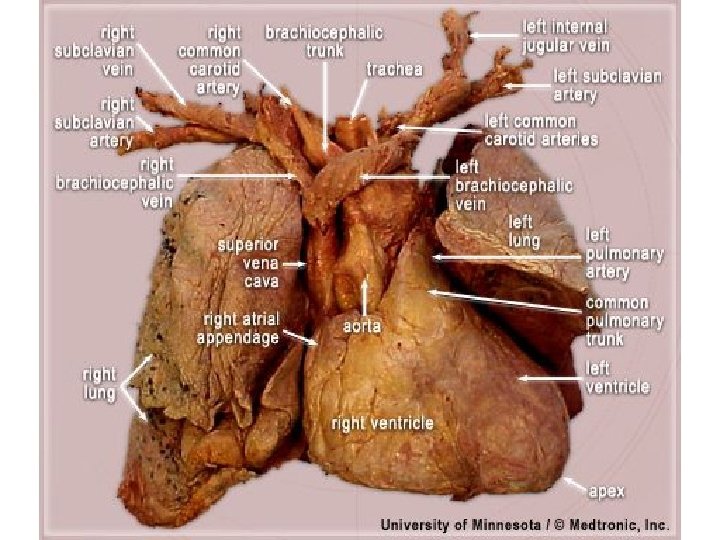
The Vascular System • Arteries – carry blood away from the heart – Branch into Arterioles – Pulmonary Arteries - carry deoxygenated blood – Systemic Arteries – carry oxygenated blood • Capillaries- exchange – One cell layer thick! – Oxygen and nutrients cross to cells – Carbon dioxide and wastes cross into blood • Veins – carry blood back to the heart – – Branch into Venules Pulmonary Veins – carry oxygenated blood Systemic Veins – carry deoxygenated blood Has valves internally!
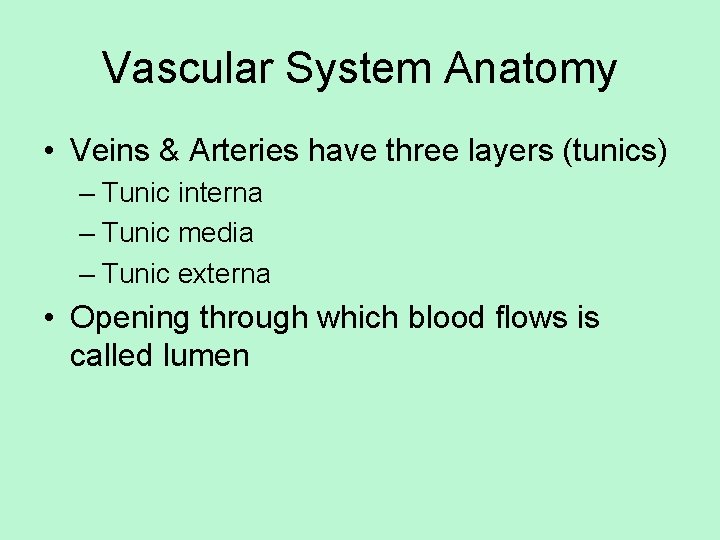
Vascular System Anatomy • Veins & Arteries have three layers (tunics) – Tunic interna – Tunic media – Tunic externa • Opening through which blood flows is called lumen
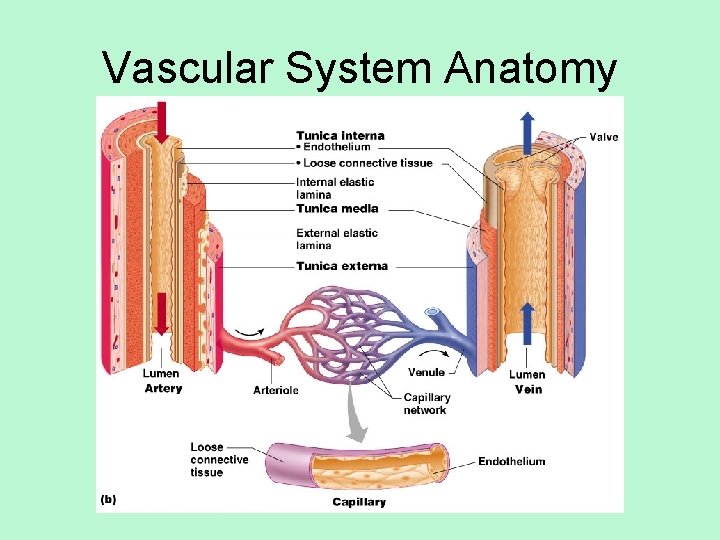
Vascular System Anatomy
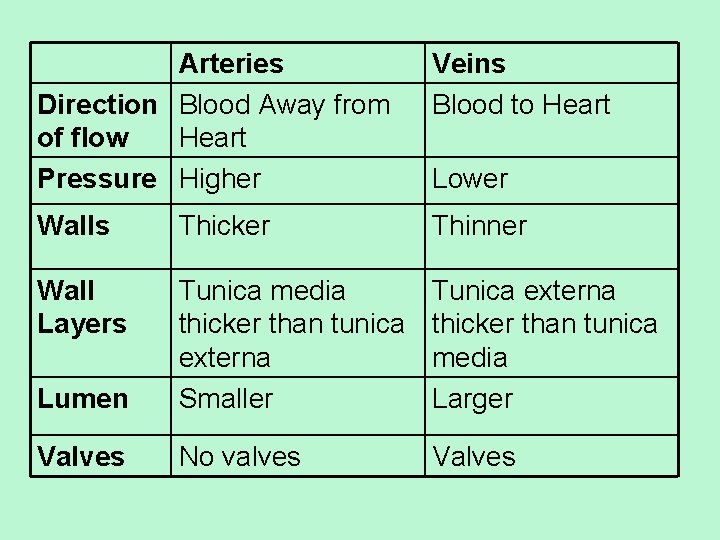
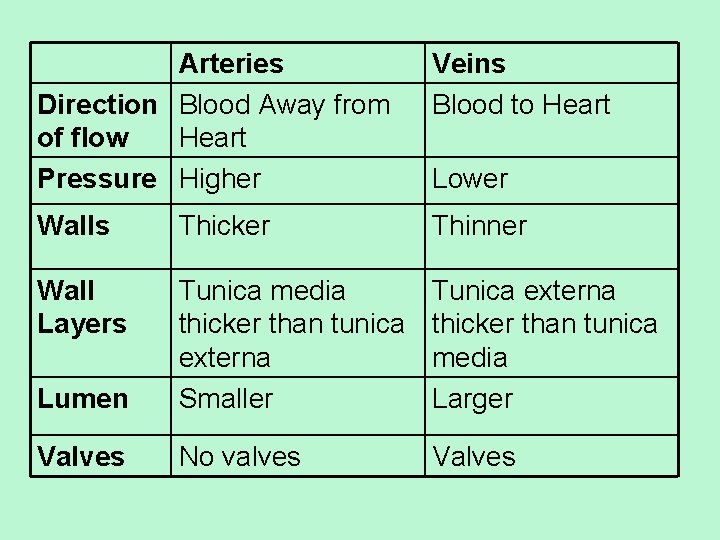
Arteries Direction Blood Away from of flow Heart Pressure Higher Veins Blood to Heart Walls Thicker Thinner Wall Layers Lumen Tunica media thicker than tunica externa Smaller Tunica externa thicker than tunica media Larger Valves No valves Valves Lower

Vital Signs
Vital Signs • • • Pulse Blood Pressure Respiratory Rate Body Temperature All indicate the efficiency of the system
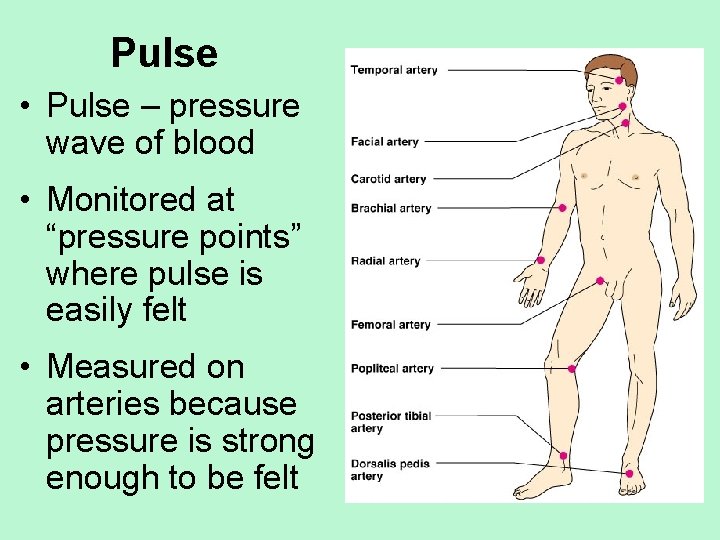
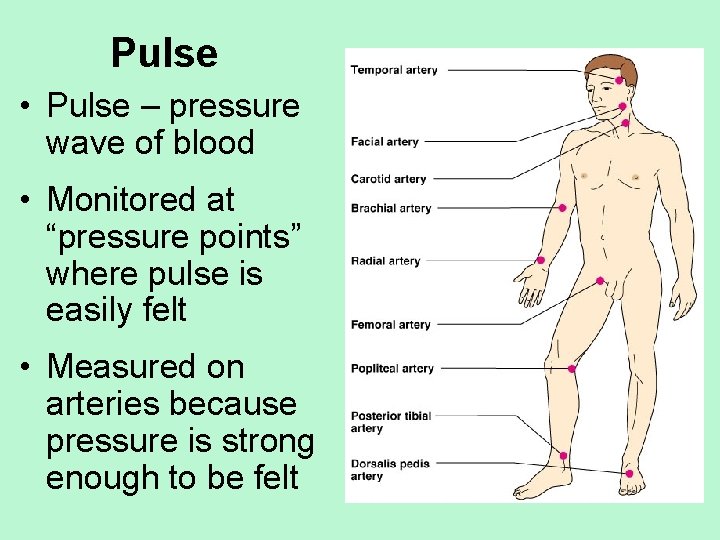
Pulse • Pulse – pressure wave of blood • Monitored at “pressure points” where pulse is easily felt • Measured on arteries because pressure is strong enough to be felt
Pulse • Radial pulse and Carotid pulse most common (helps to have the artery close to the surface & hard surface to press it on) • Average pulse is 65 -80 beats per minute • Pulse influenced by activity, postural changes, and emotions… stress… tests… homework… you know • Pressure points can also be used as compression point if trying to stop blood flow
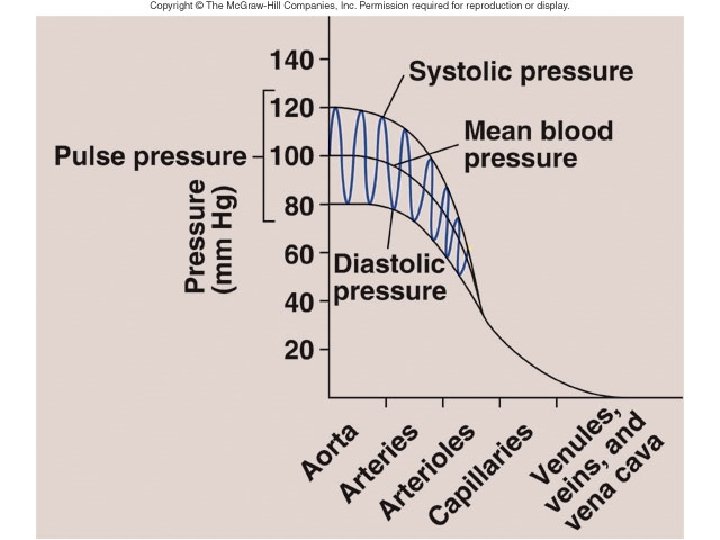
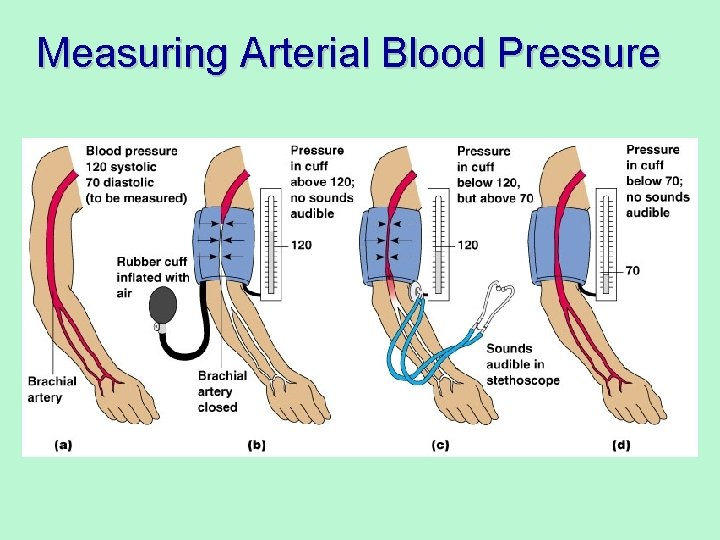
Blood Pressure • Measurements by health professionals are made on the pressure in large arteries (usually the brachial artery) • Pressure in blood vessels decreases as the distance away from the heart increases (not feeling the pressure created by the left ventricle as much!)
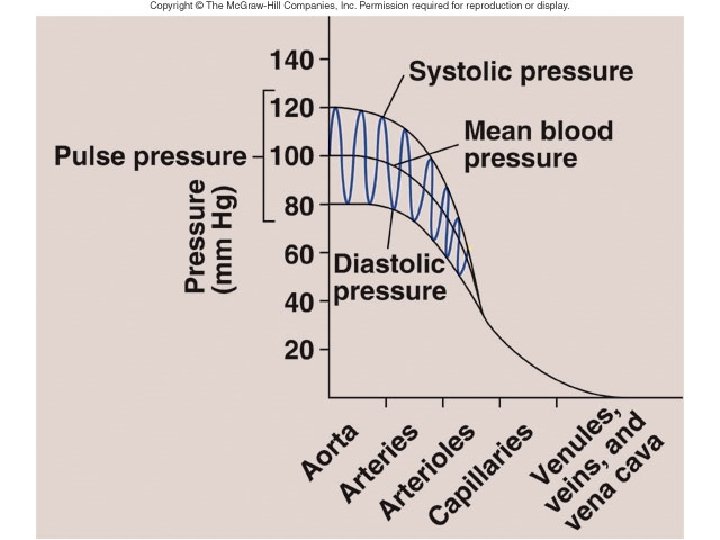
Blood Pressure • Systolic Pressure (heart ventricles contract) • Diastolic Pressure (heart ventricles relax) • Blood Pressure= systolic/diastolic • Normal= 120/80
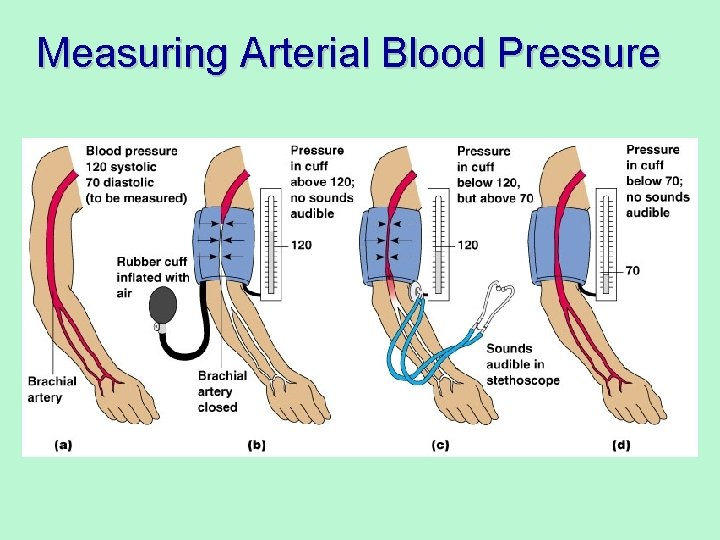
Measuring Arterial Blood Pressure
Changing Blood Pressure • Temperature – Heat has a vasodilation effect – Cold has a vasoconstricting effect • Chemicals – Various substances can cause increases or decreases • Diet
Blood
Blood Facts • Only fluid tissue in human body • Blood heavier than water and 5 times thicker • Slightly basic – p. H approximately 7. 4 • Temperature slightly higher than body temperature (100. 4°F) • Approximately 6 quarts (1. 5 gallons) in adult •
Blood Facts • Blood stays in a closed system except… – White blood cells travel in and out of the blood stream (lymphatic system) – Water and solutes (ions, nutrients, etc) travel in and out of the blood stream
Blood Functions Include… • Distribution & Transport – Respiratory Gases – Nutrients – Wastes – Bacteria, Viruses, Toxins, etc. • Regulation and Maintenance – Hormonal Regulation – p. H balance (blood is a buffer!) – Temperature
Blood Functions Include… • Protection – Clotting – Immunity
Composition of Blood • Plasma – 55% of blood – Mostly water (90%) – Plasma proteins • Albumin – p. H • Clotting Proteins • Antibodies - defense – – – Salts (electrolytes) Nutrients Waste Products Hormones Gases
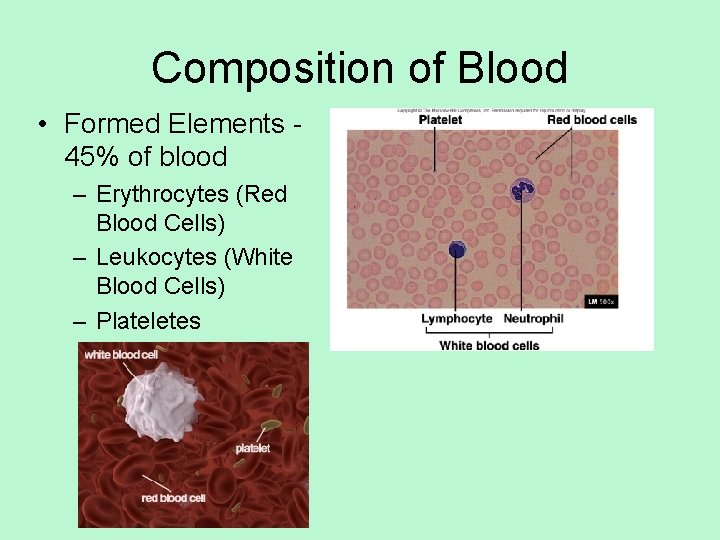
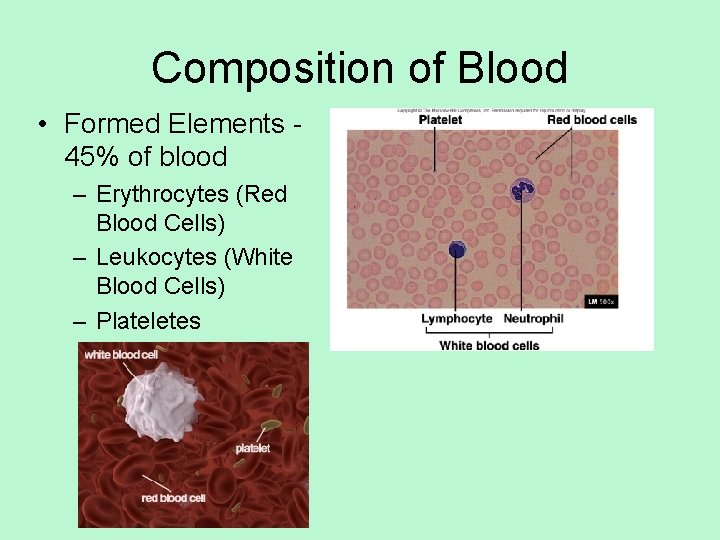
Composition of Blood • Formed Elements 45% of blood – Erythrocytes (Red Blood Cells) – Leukocytes (White Blood Cells) – Plateletes
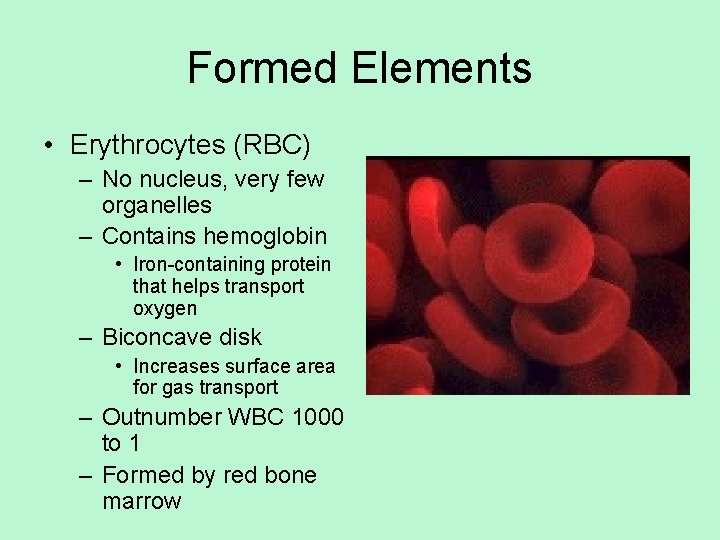
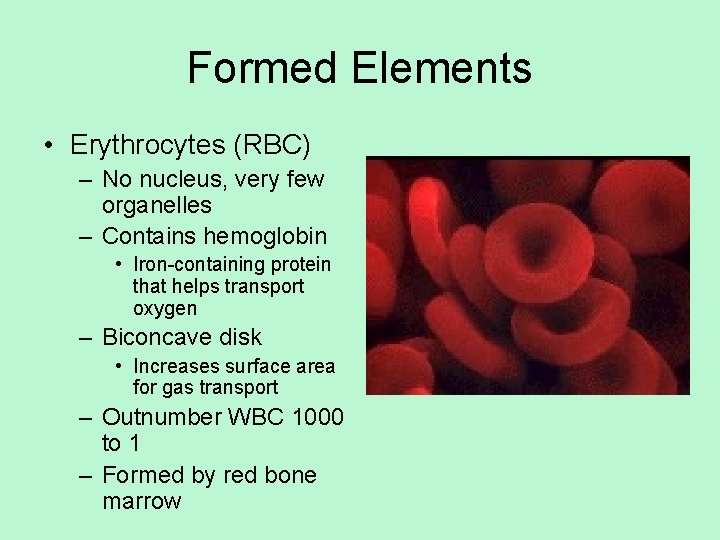
Formed Elements • Erythrocytes (RBC) – No nucleus, very few organelles – Contains hemoglobin • Iron-containing protein that helps transport oxygen – Biconcave disk • Increases surface area for gas transport – Outnumber WBC 1000 to 1 – Formed by red bone marrow
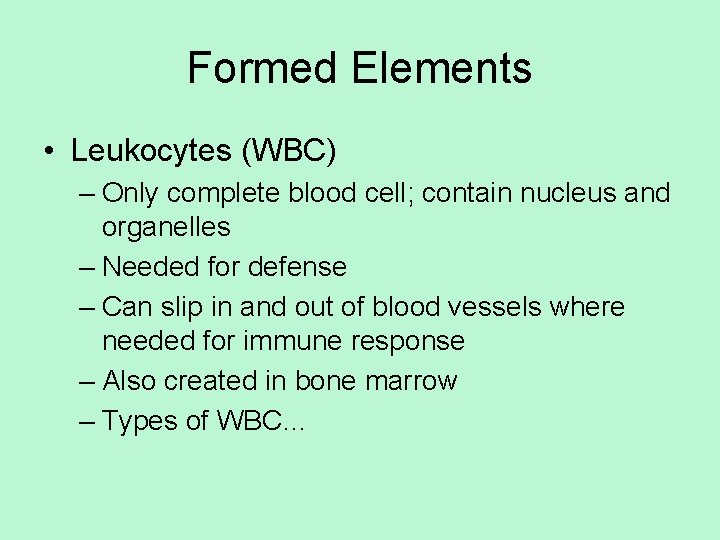
Formed Elements • Leukocytes (WBC) – Only complete blood cell; contain nucleus and organelles – Needed for defense – Can slip in and out of blood vessels where needed for immune response – Also created in bone marrow – Types of WBC…
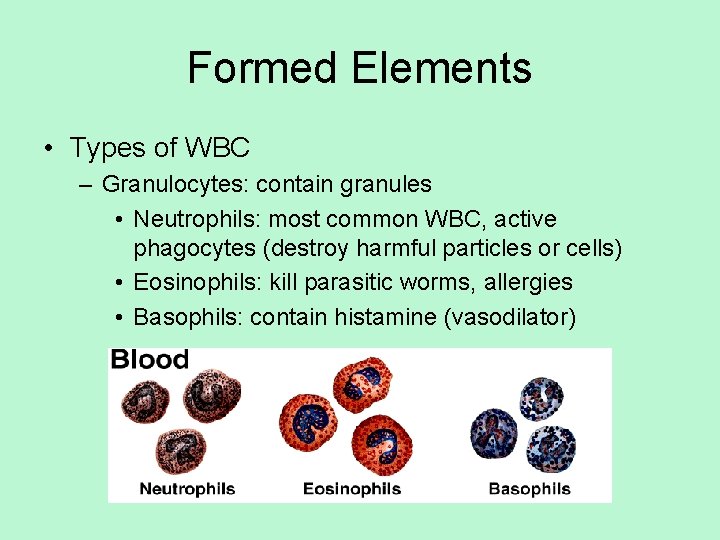
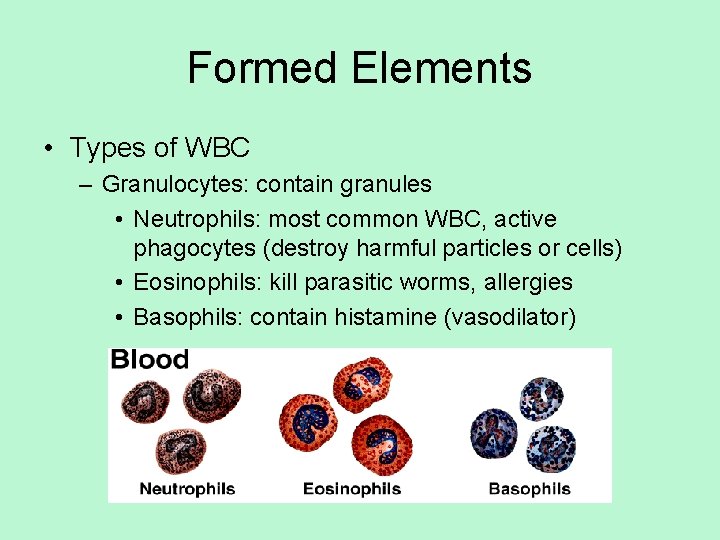
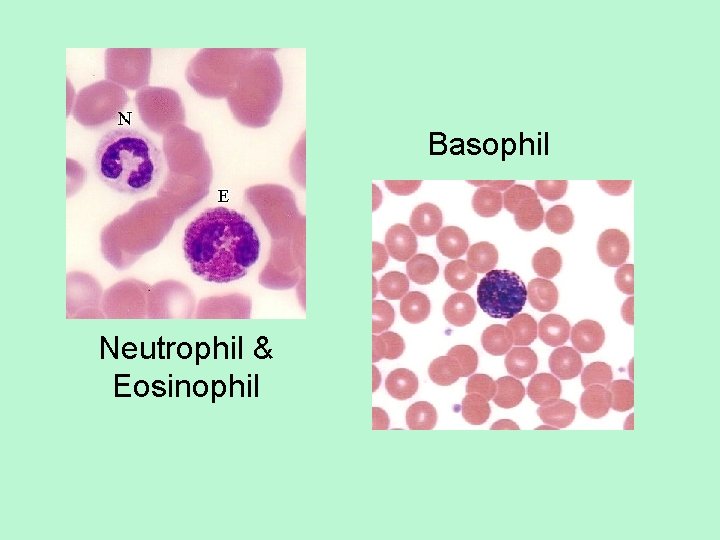
Formed Elements • Types of WBC – Granulocytes: contain granules • Neutrophils: most common WBC, active phagocytes (destroy harmful particles or cells) • Eosinophils: kill parasitic worms, allergies • Basophils: contain histamine (vasodilator)
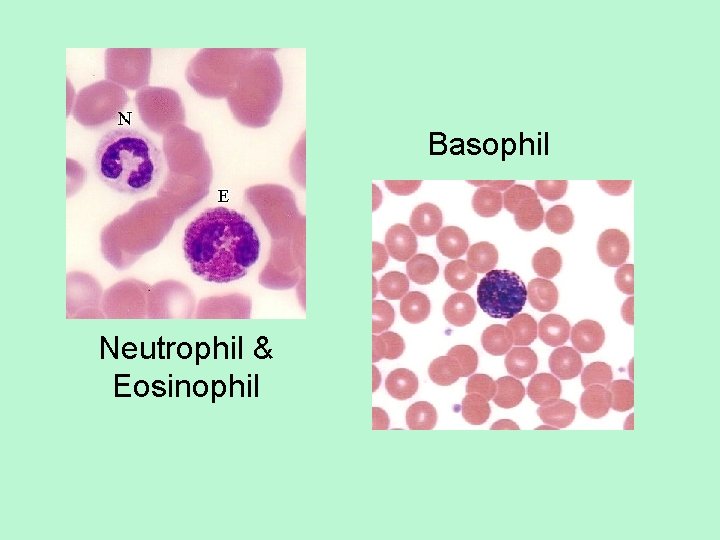
Basophil Neutrophil & Eosinophil
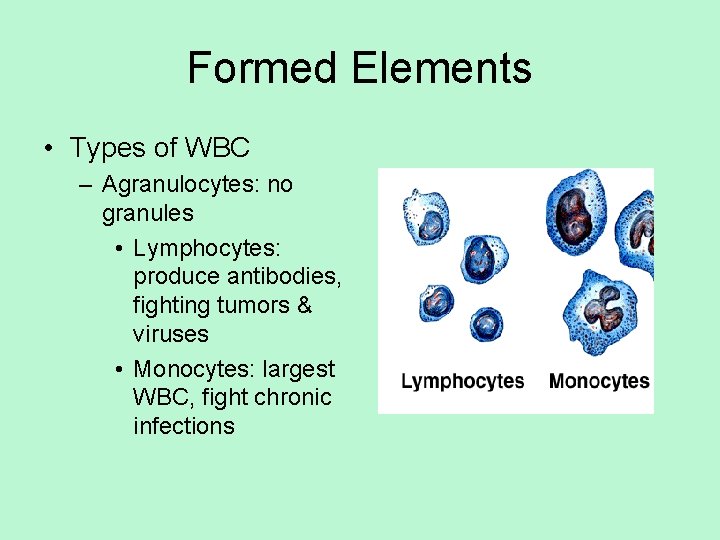
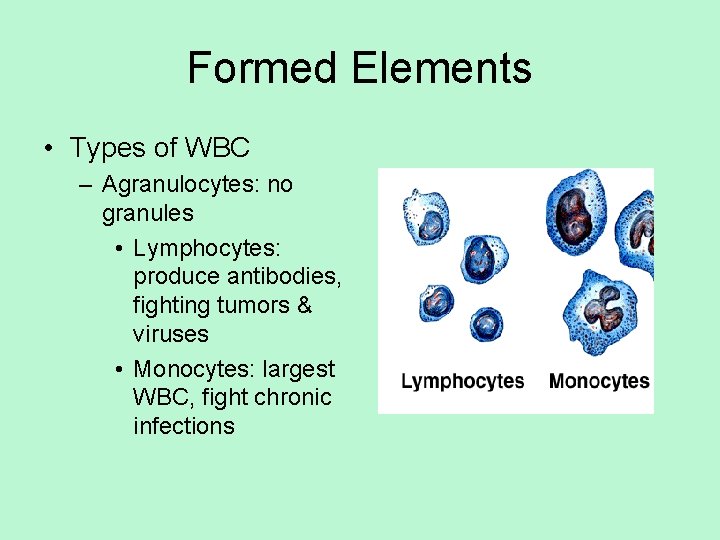
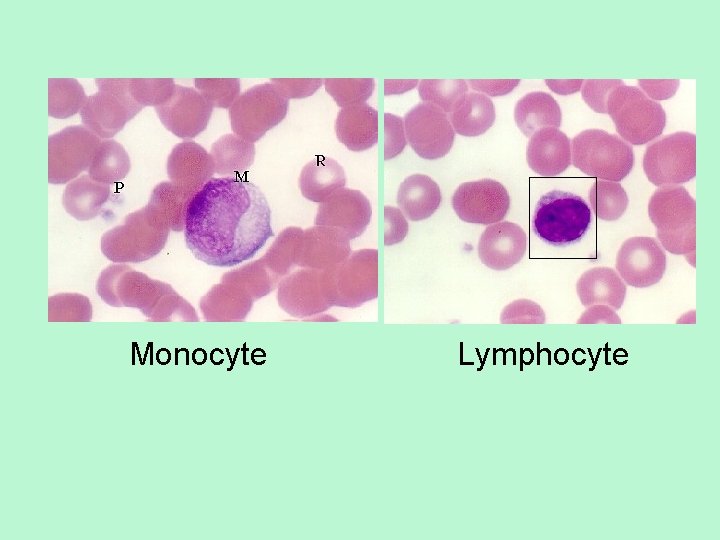
Formed Elements • Types of WBC – Agranulocytes: no granules • Lymphocytes: produce antibodies, fighting tumors & viruses • Monocytes: largest WBC, fight chronic infections
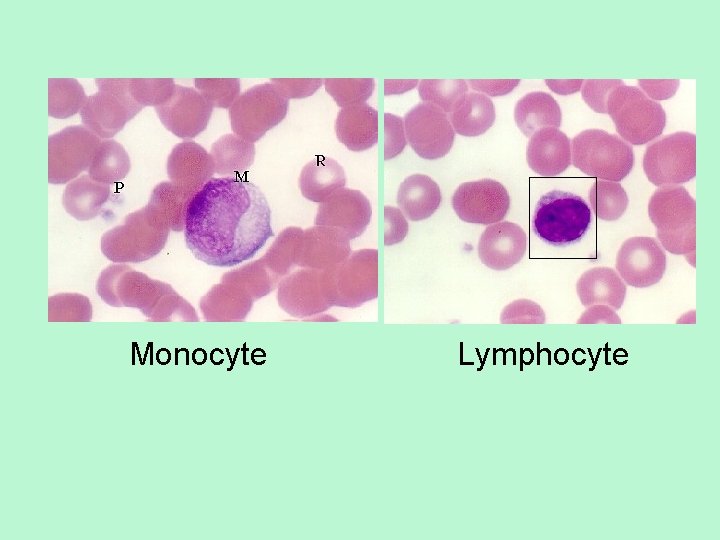
Monocyte Lymphocyte
Formed Elements • Platelets – Not cells, but rather fragments – Important in blood clotting
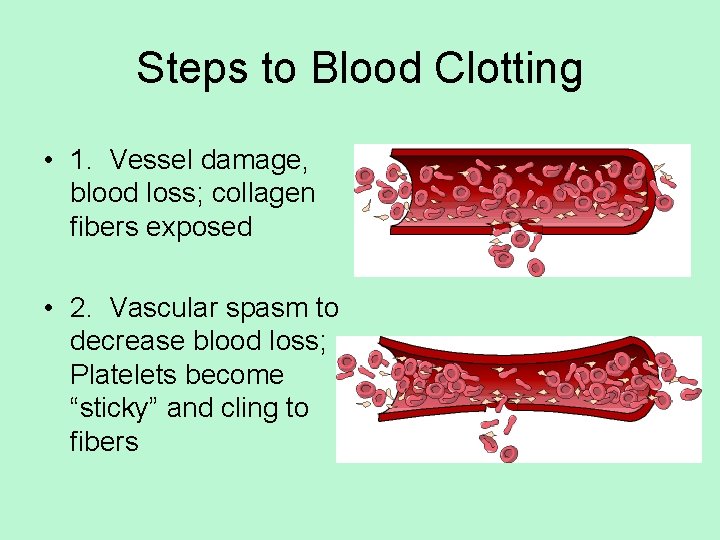
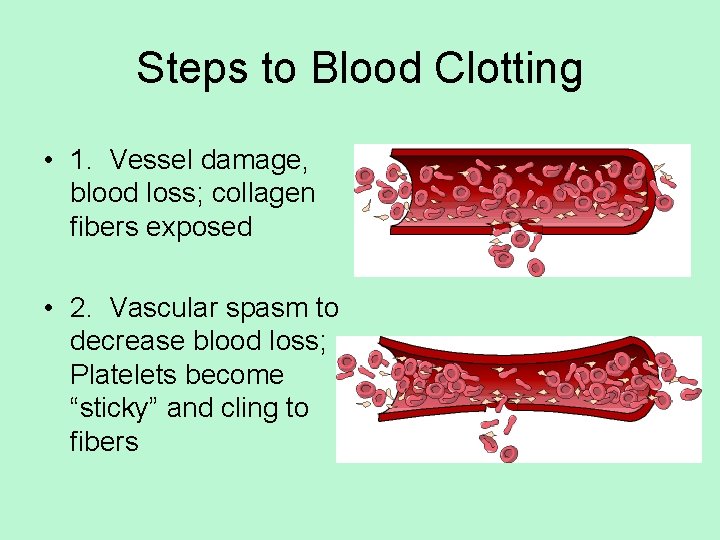
Steps to Blood Clotting • 1. Vessel damage, blood loss; collagen fibers exposed • 2. Vascular spasm to decrease blood loss; Platelets become “sticky” and cling to fibers
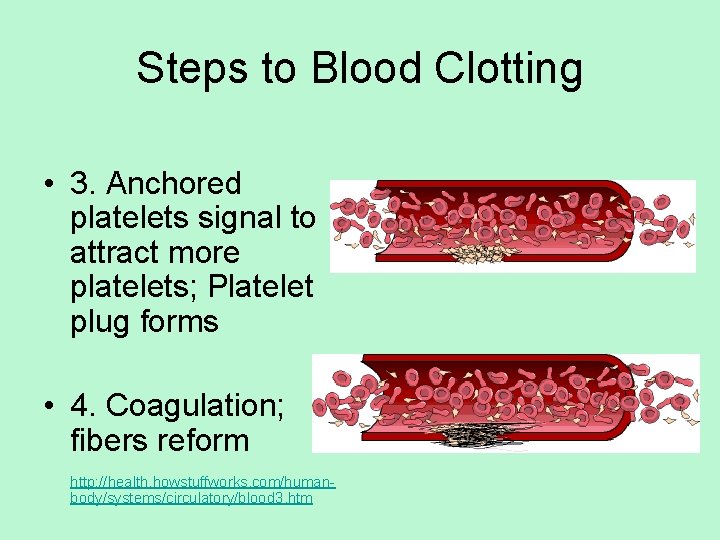
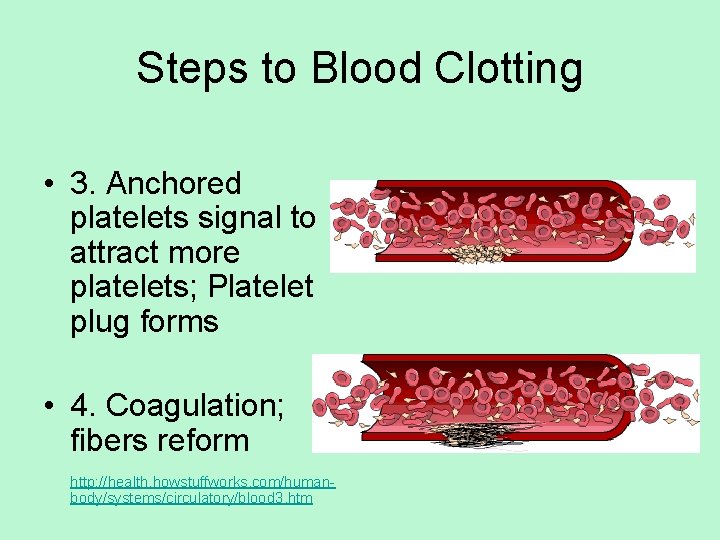
Steps to Blood Clotting • 3. Anchored platelets signal to attract more platelets; Platelet plug forms • 4. Coagulation; fibers reform http: //health. howstuffworks. com/humanbody/systems/circulatory/blood 3. htm
Blood Transfusions • Body can only compensate for a certain amount of blood loss – Loss of 15 -30% of blood: weakness – Loss of over 30%: severe shock, usually fatal • Therefore, we need to replace the blood when it is lost! – Blood treated with an anticoagulant (prevents clotting) can be refrigerated at 4°C for about 35 days
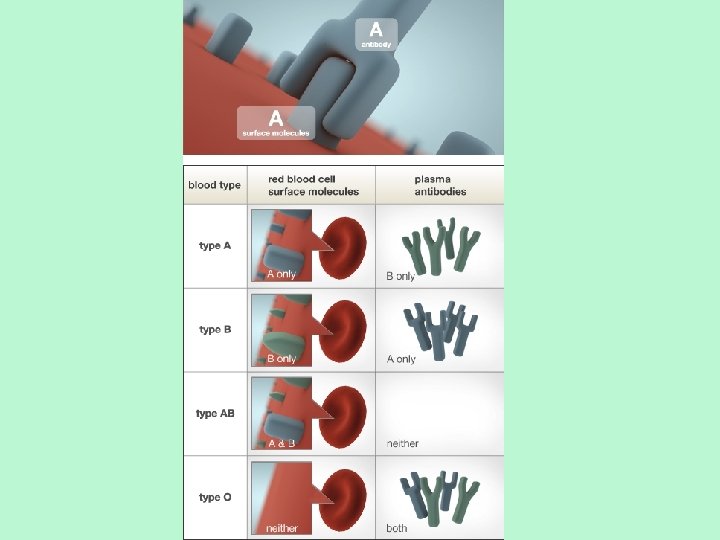
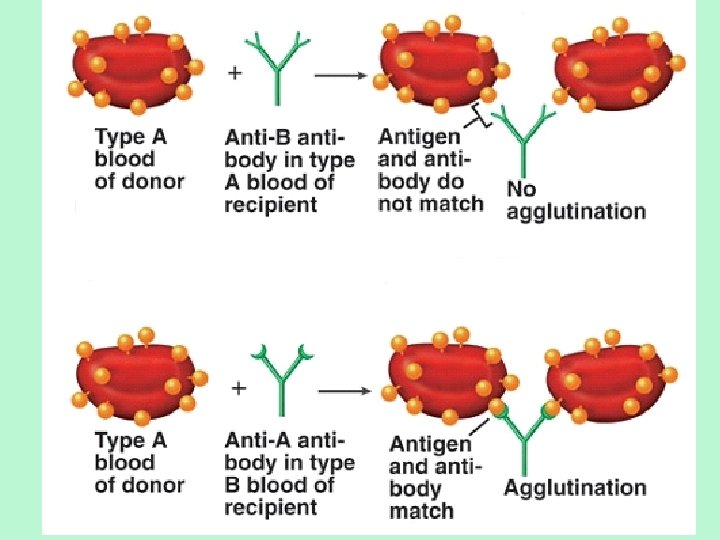
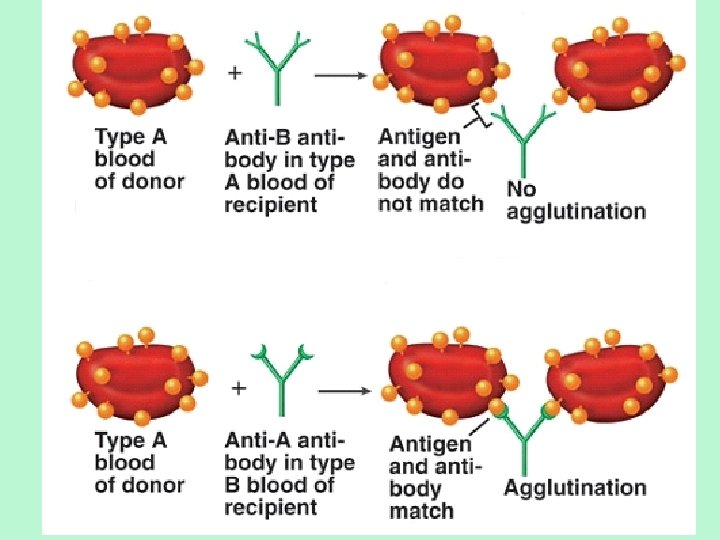
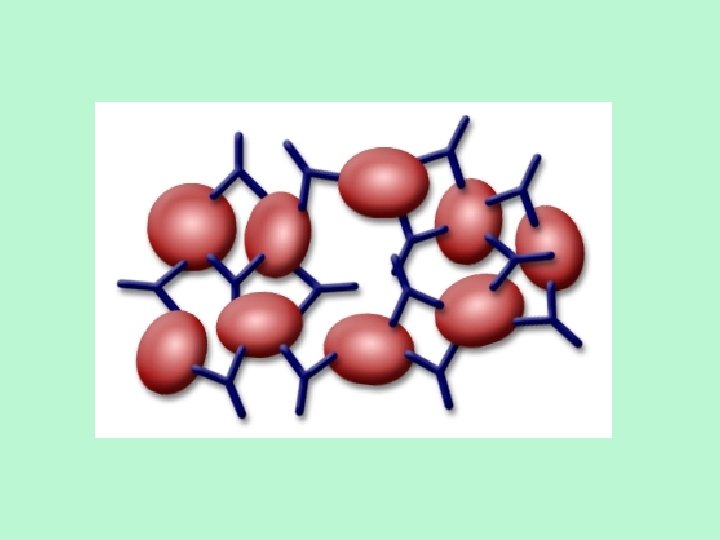
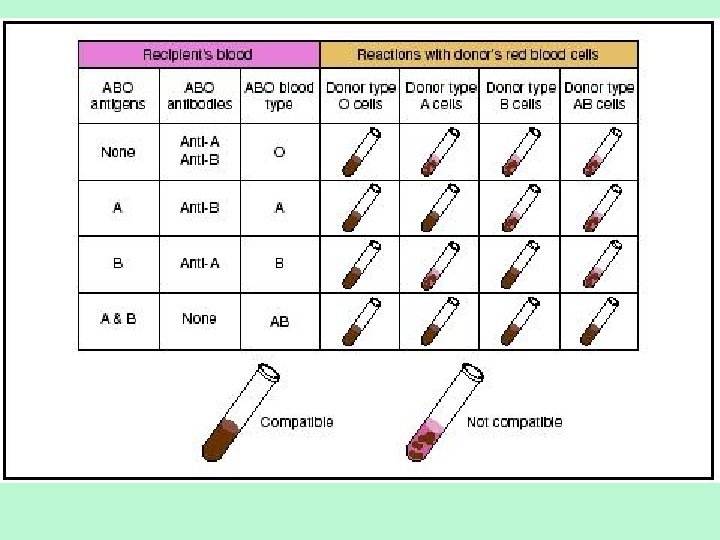
Blood Transfusions • However, blood must be compatible with your body! – All plasma membranes of RBC bear certain proteins (antigens) which are unique – We also have antibodies looking for antigens – We can tolerate our own antigens, but if we get different antigens from another person, antibodies will attack RBC! – This causes RBC’s to clump (agglutination)
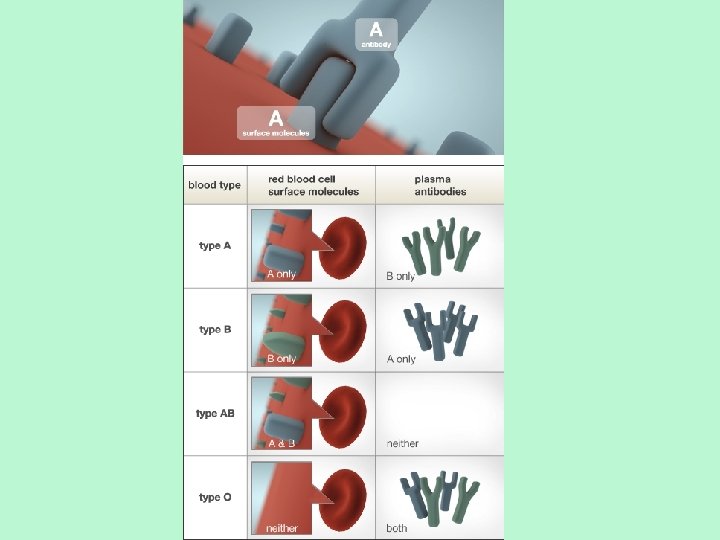
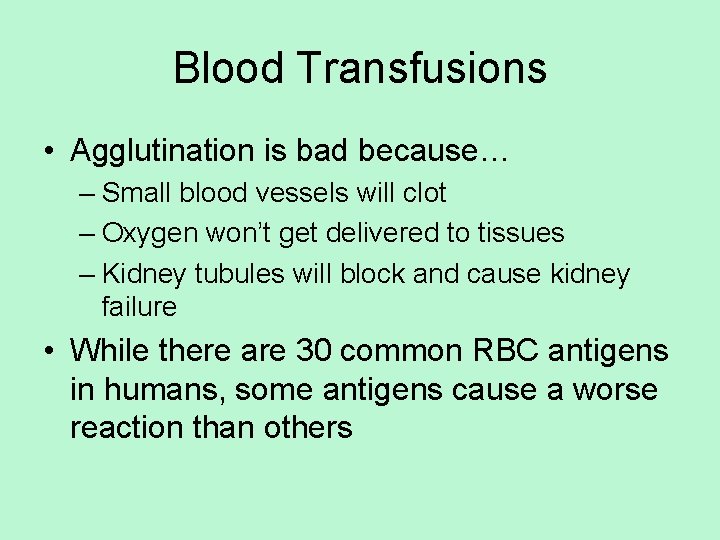
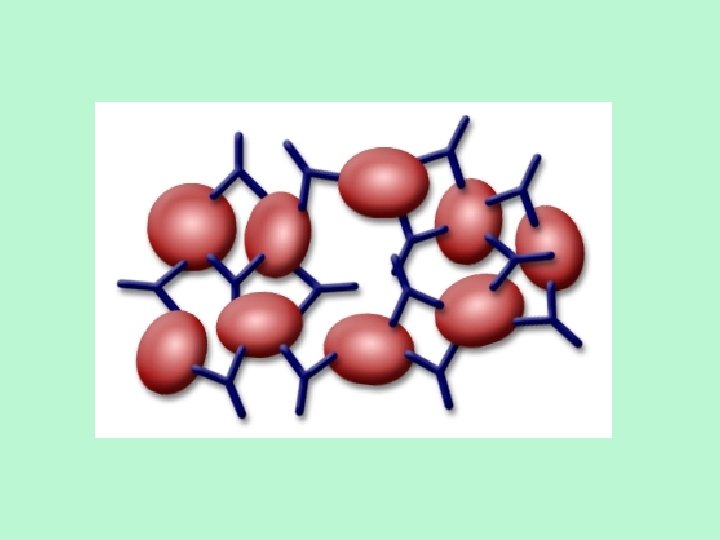
Blood Transfusions • Agglutination is bad because… – Small blood vessels will clot – Oxygen won’t get delivered to tissues – Kidney tubules will block and cause kidney failure • While there are 30 common RBC antigens in humans, some antigens cause a worse reaction than others
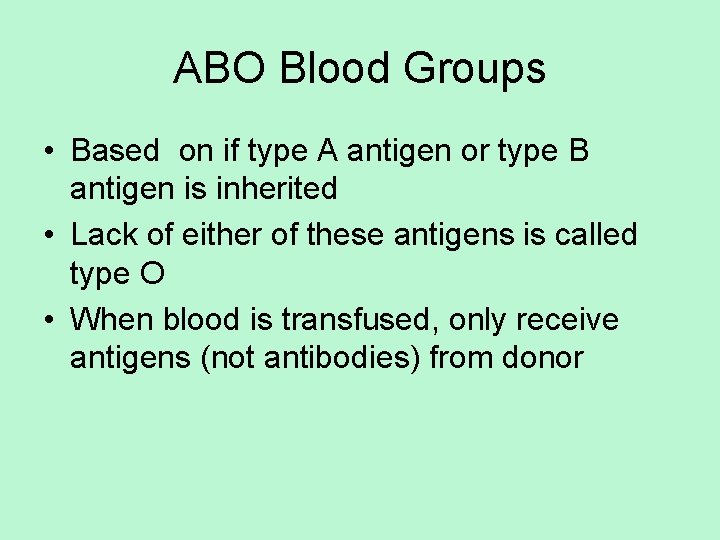
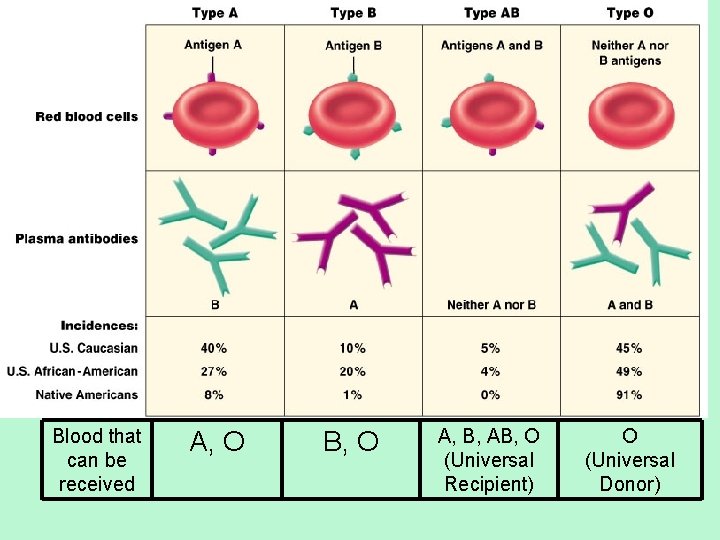
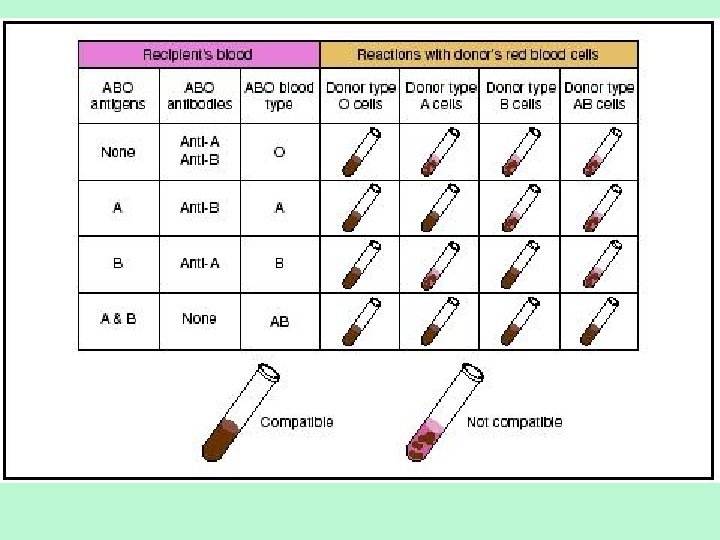
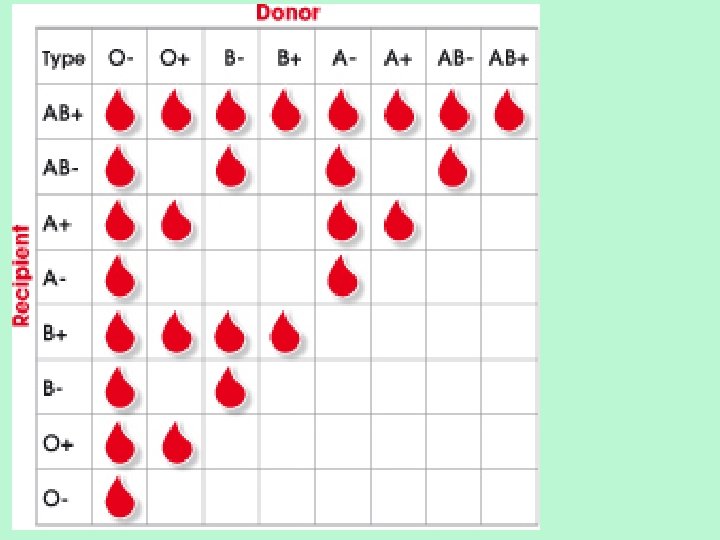
ABO Blood Groups • Based on if type A antigen or type B antigen is inherited • Lack of either of these antigens is called type O • When blood is transfused, only receive antigens (not antibodies) from donor
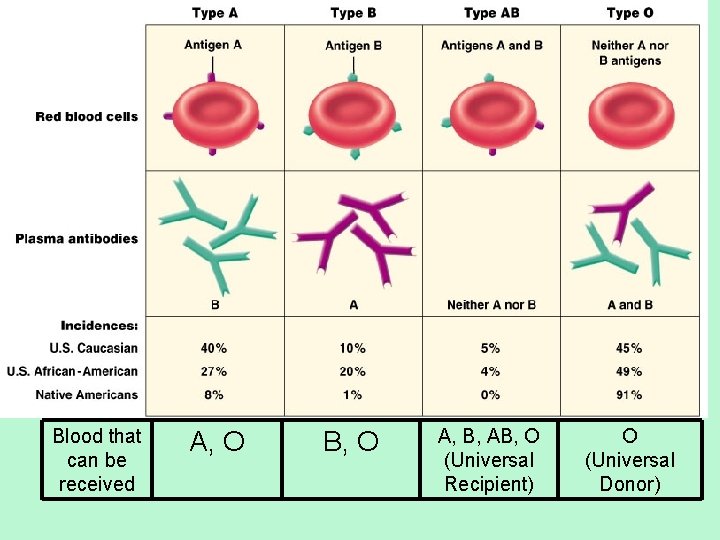
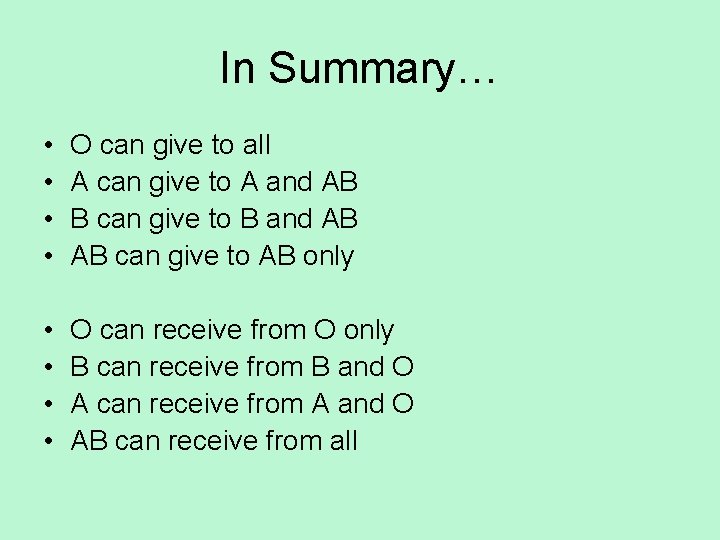
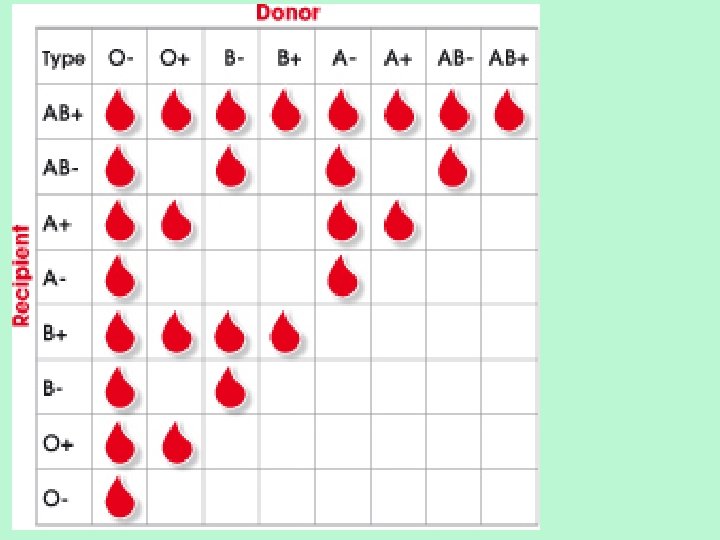
Blood that can be received A, O B, O A, B, AB, O (Universal Recipient) O (Universal Donor)
In Summary… • • O can give to all A can give to A and AB B can give to B and AB AB can give to AB only • • O can receive from O only B can receive from B and O A can receive from A and O AB can receive from all
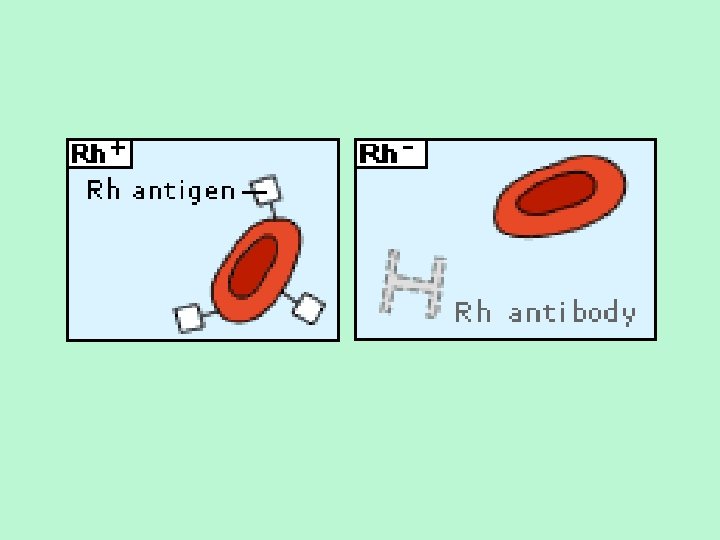
Rh Blood Typing • Named because of the presence or absence of Rh antigens (originally studied in Rhesus monkeys) – Rh+: have antigen – Rh-: don’t have antigen • Rh antibodies are not automatically formed in Rh- individuals; blood must be exposed to Rh+ blood to develop antibodies against it
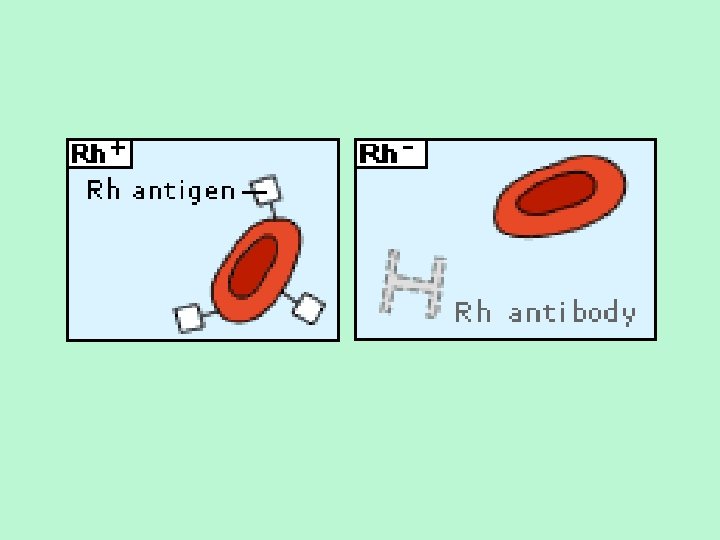
Rh Blood Typing • Rh+ person can get either + or – blood because they have no antibodies! • However, if Rh– person receives Rh+ blood, antibodies can form – Okay for first transfusion, but in 2 nd transfusion, antibodies will attack new Rh+ blood = bad. • In summary: – Rh+ can get Rh+ or Rh– blood – Rh– should only get Rh– blood
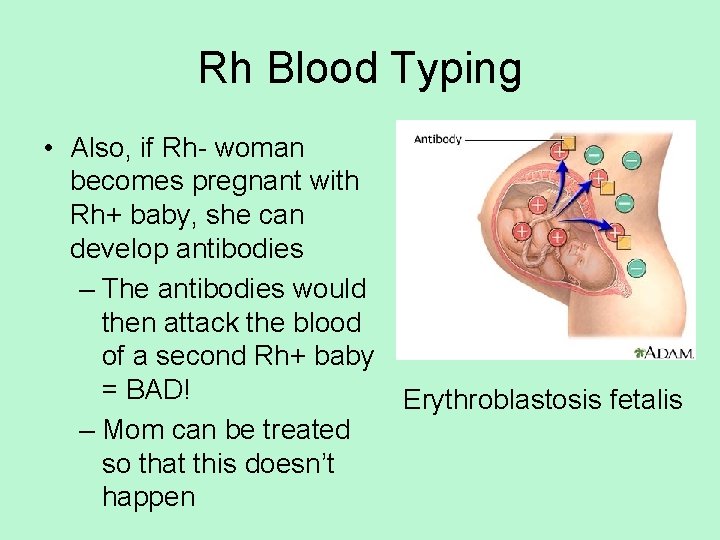
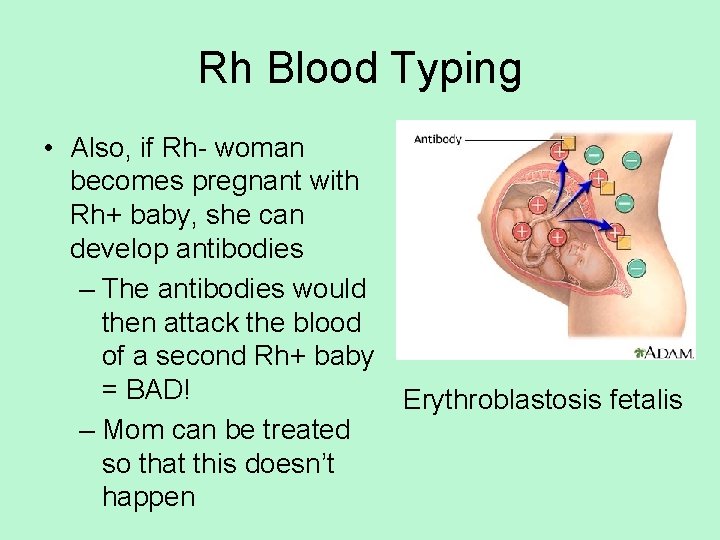
Rh Blood Typing • Also, if Rh- woman becomes pregnant with Rh+ baby, she can develop antibodies – The antibodies would then attack the blood of a second Rh+ baby = BAD! – Mom can be treated so that this doesn’t happen Erythroblastosis fetalis
Cardiovascular Conditions
Review of some terms… • Ischemia: lack of blood flow to the heart • Fibrillation: rapid, uncoordinated movement of the heart muscle due to ischemia • Cardiac Arrest: blood flow to body ceases, leads to death
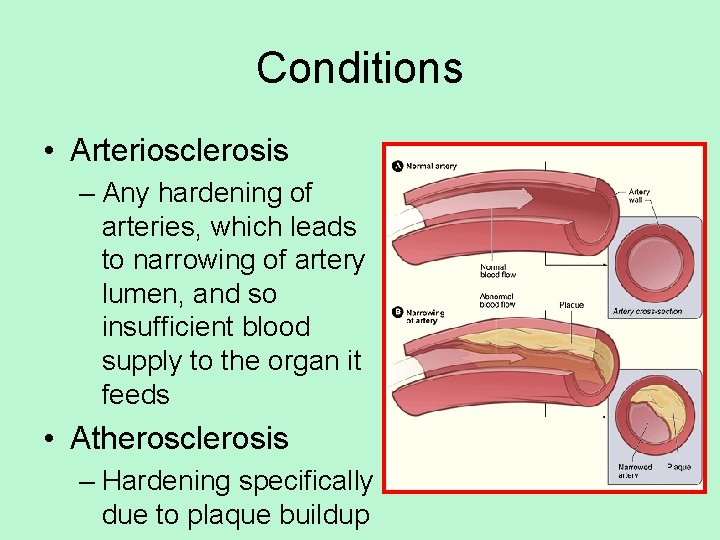
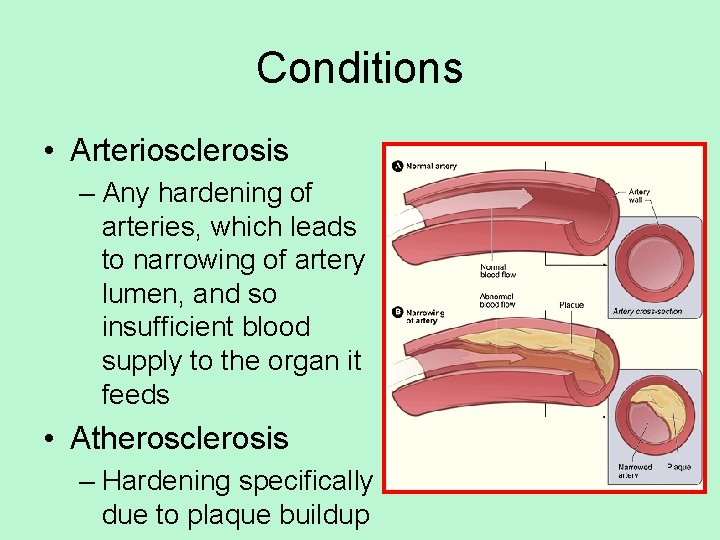
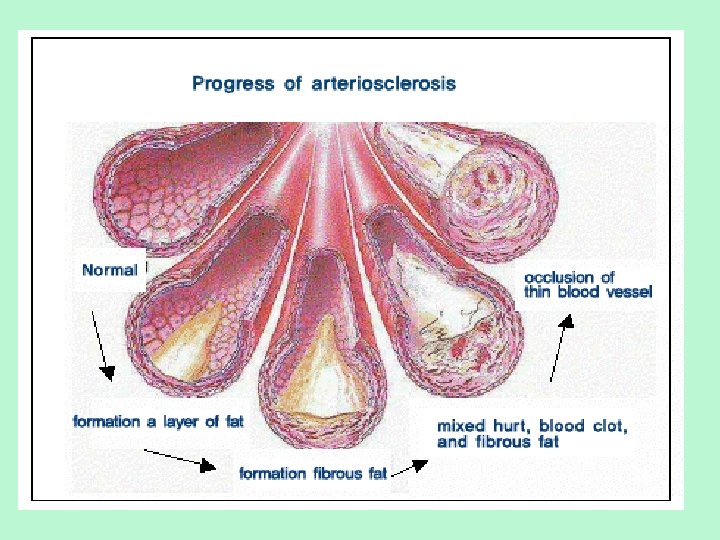
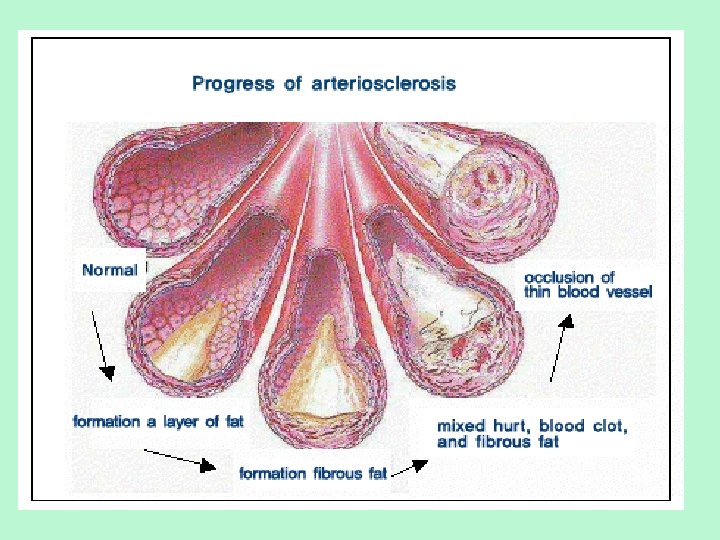
Conditions • Arteriosclerosis – Any hardening of arteries, which leads to narrowing of artery lumen, and so insufficient blood supply to the organ it feeds • Atherosclerosis – Hardening specifically due to plaque buildup

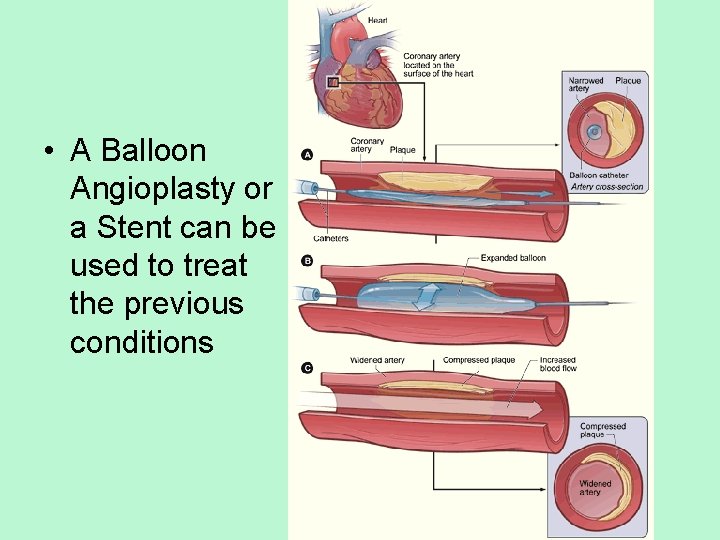
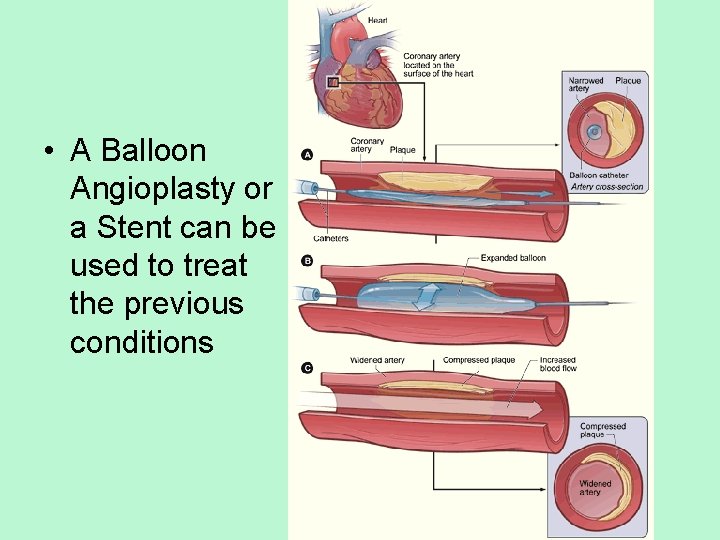
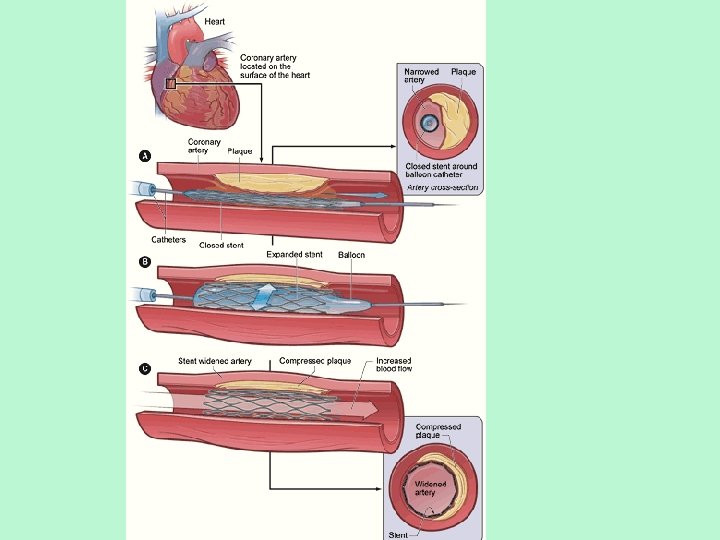
• A Balloon Angioplasty or a Stent can be used to treat the previous conditions
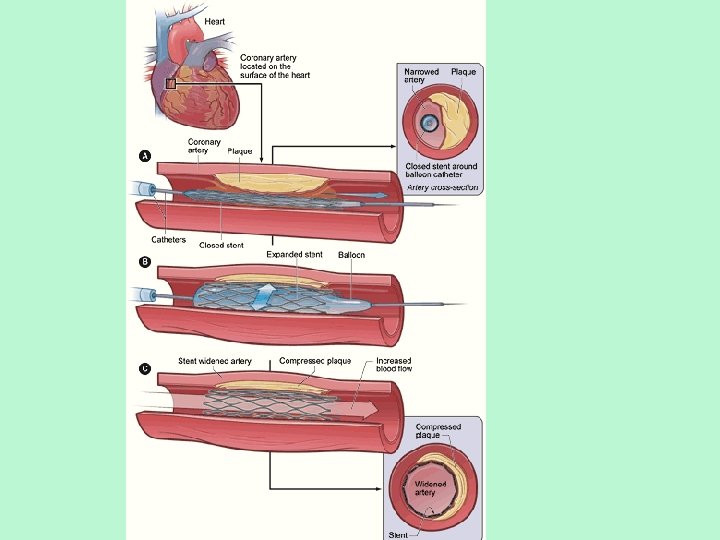
• http: //www. nhlbi. nih. gov/health/dci/Diseas es/Angioplasty_All. html
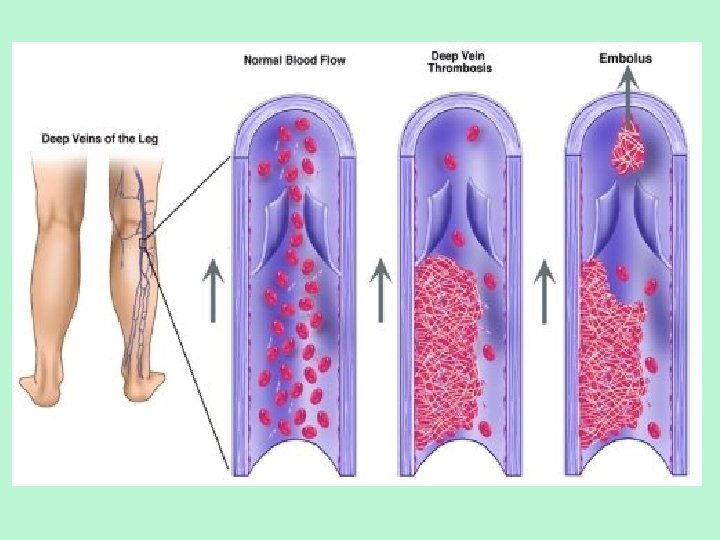
Conditions • Thrombosis: blood clot in an intact blood vessel – Can happen in arteries or veins – Most common in veins of the legs – Compression stocking and anticoagulants can help
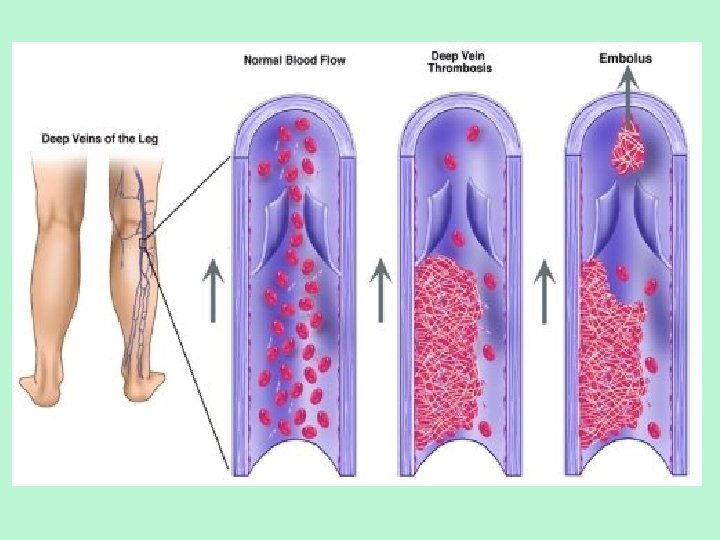
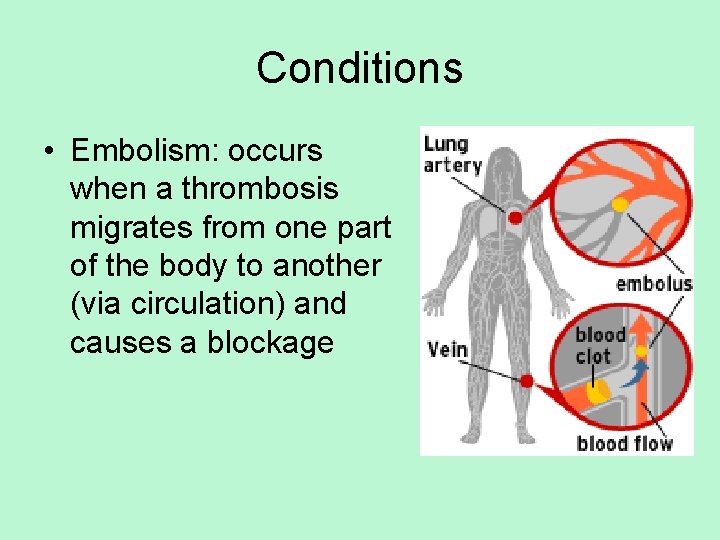
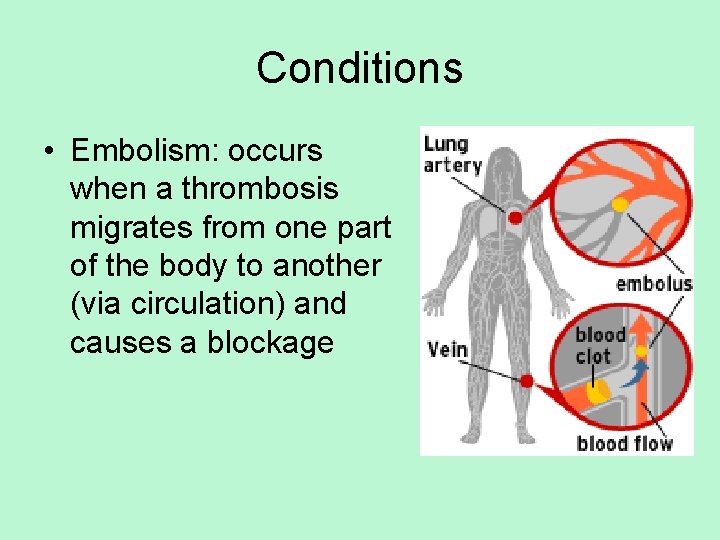
Conditions • Embolism: occurs when a thrombosis migrates from one part of the body to another (via circulation) and causes a blockage
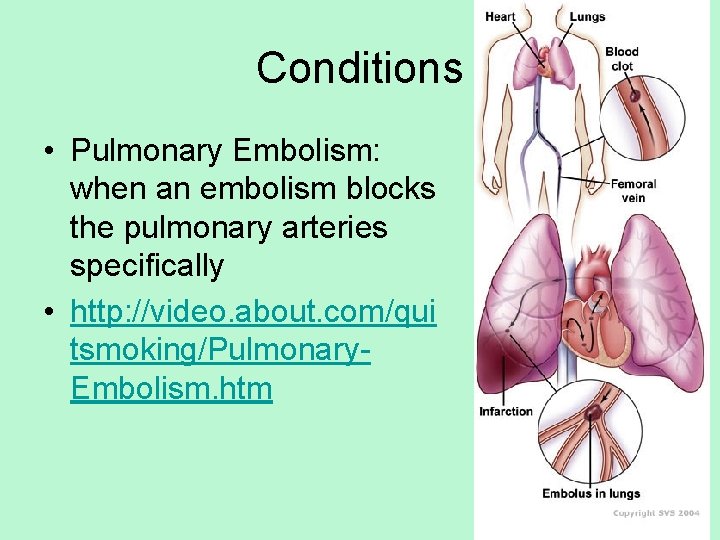
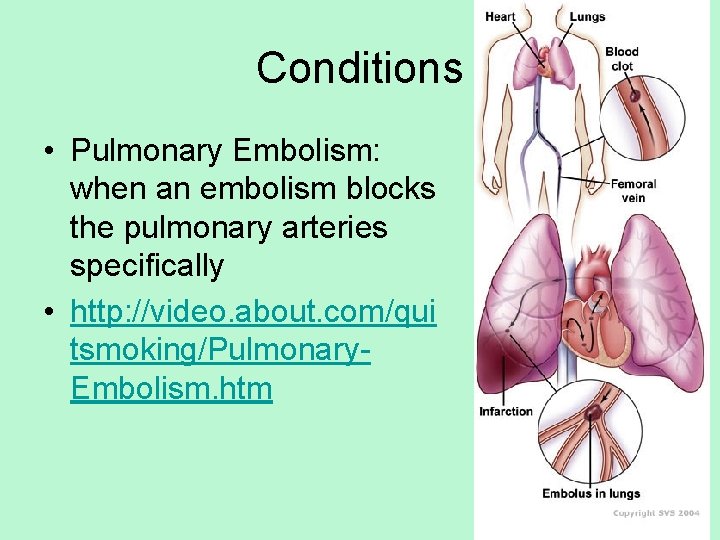
Conditions • Pulmonary Embolism: when an embolism blocks the pulmonary arteries specifically • http: //video. about. com/qui tsmoking/Pulmonary. Embolism. htm
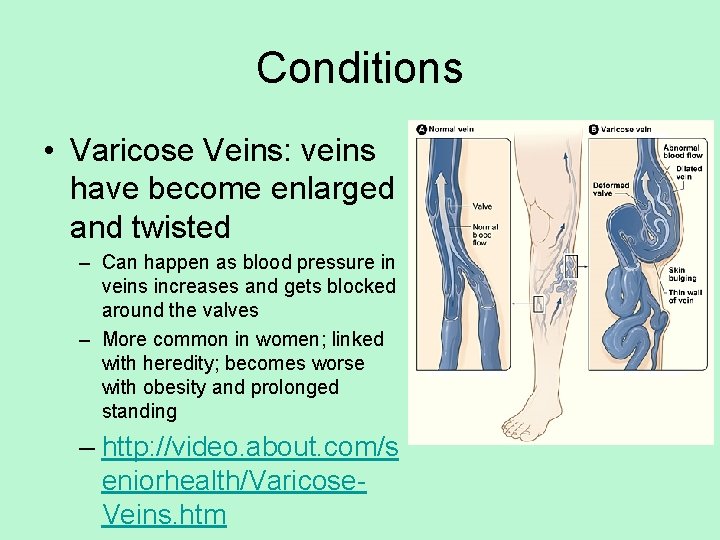
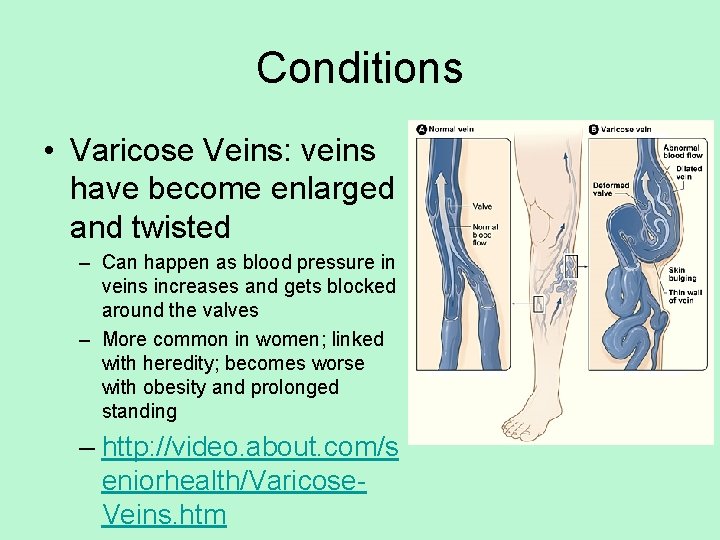
Conditions • Varicose Veins: veins have become enlarged and twisted – Can happen as blood pressure in veins increases and gets blocked around the valves – More common in women; linked with heredity; becomes worse with obesity and prolonged standing – http: //video. about. com/s eniorhealth/Varicose. Veins. htm
Conditions • Hypertension: high blood pressure – Systolic above 140 and diastolic above 90 – Can indicate other issues – http: //video. about. com/highbloodpressure/Blo od-Pressure. htm
• Your chances of developing high blood pressure also higher if you: – Are overweight – Are a man over the age of 45 / woman over 55 – Have a family history of high blood pressure • Other things that can raise blood pressure include: – Eating too much salt – Drinking too much alcohol – Not getting enough potassium in your diet – Not doing enough physical activity – Taking certain medicines – Having long-lasting stress – Smoking
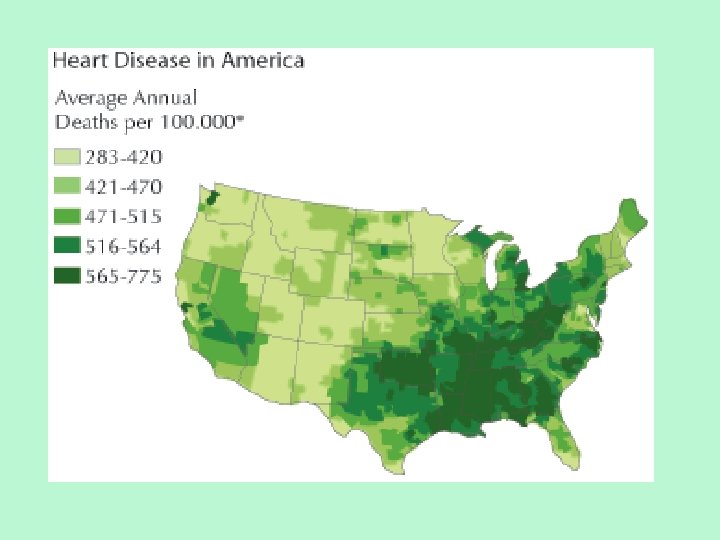
Conditions • Coronary Heart/Artery Disease (CHD) – End result of plaques within the walls of the arteries that supply the myocardium with oxygen – #1 killer in the US – Often leads to myocardial infarction – Angina (heart pains) can indicate CHD
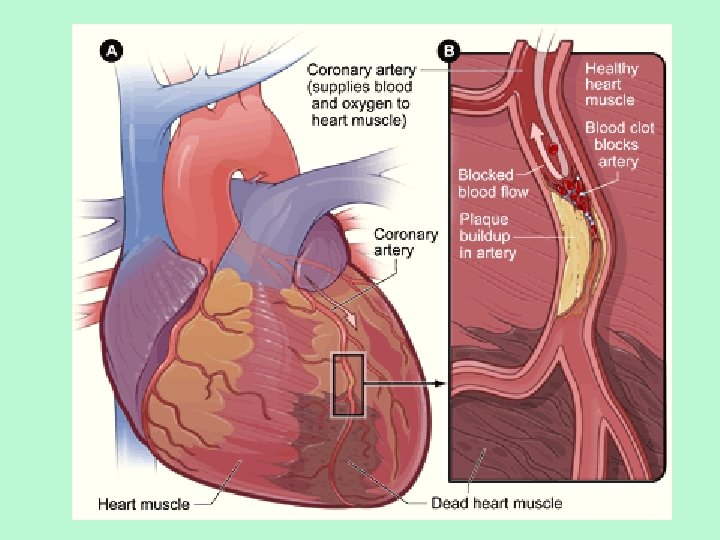
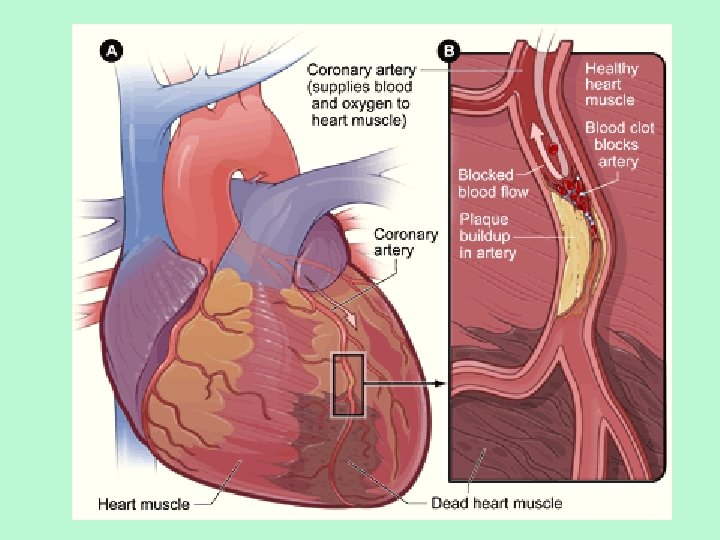
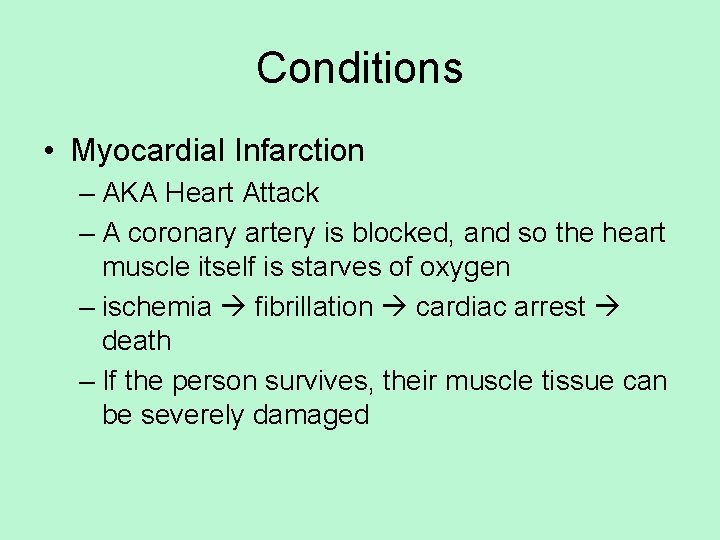
Conditions • Myocardial Infarction – AKA Heart Attack – A coronary artery is blocked, and so the heart muscle itself is starves of oxygen – ischemia fibrillation cardiac arrest death – If the person survives, their muscle tissue can be severely damaged
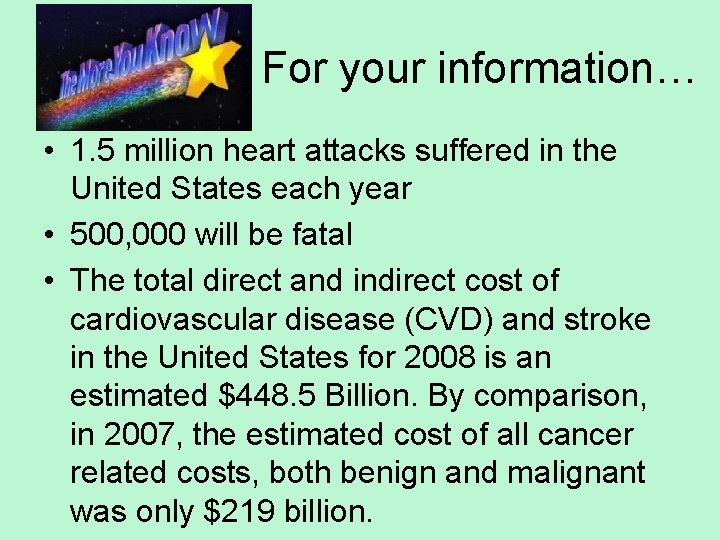
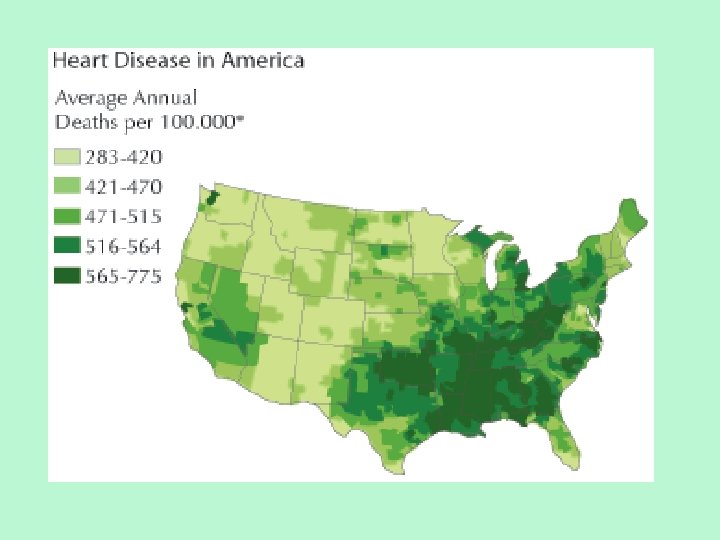
For your information… • 1. 5 million heart attacks suffered in the United States each year • 500, 000 will be fatal • The total direct and indirect cost of cardiovascular disease (CVD) and stroke in the United States for 2008 is an estimated $448. 5 Billion. By comparison, in 2007, the estimated cost of all cancer related costs, both benign and malignant was only $219 billion.
• http: //video. about. com/heartdisease/Heart. Attack. htm • http: //video. about. com/heartdisease/Heart. Bypass. htm • http: //video. about. com/heartdisease/LVAssist-Device. htm
Conditions • Congestive Heart Failure – The heart muscle is weakened (due to CHD, myocardial infarctions, hypertension, viral infections, or stresses such as childbirth & chemo/radiation) – Decline in pumping efficiency – Inadequate circulation in body – leading to cyanosis and swelling of limbs/abdomen – Because blood not being pumped to body, can get backed up in lungs, causing shortness of breath
• http: //video. about. com/heartdisease/Cong estive-Heart-Failure. htm
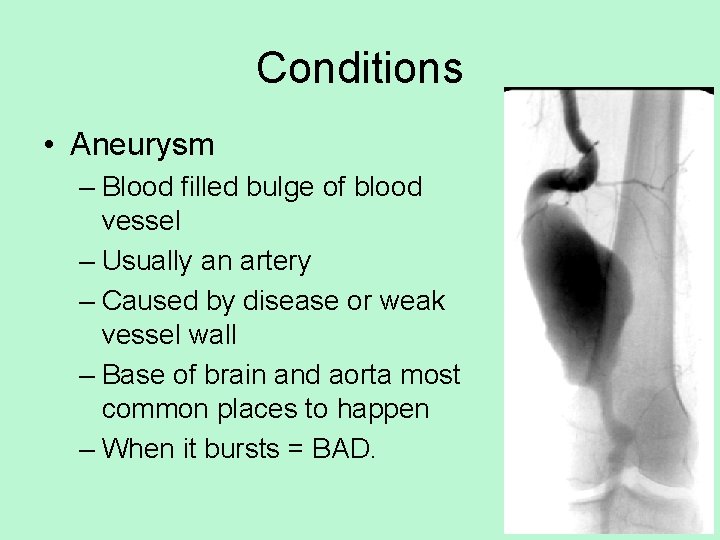
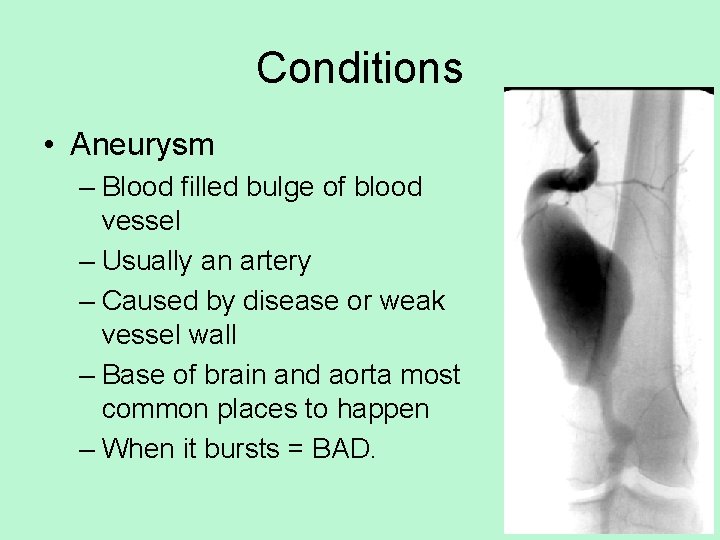
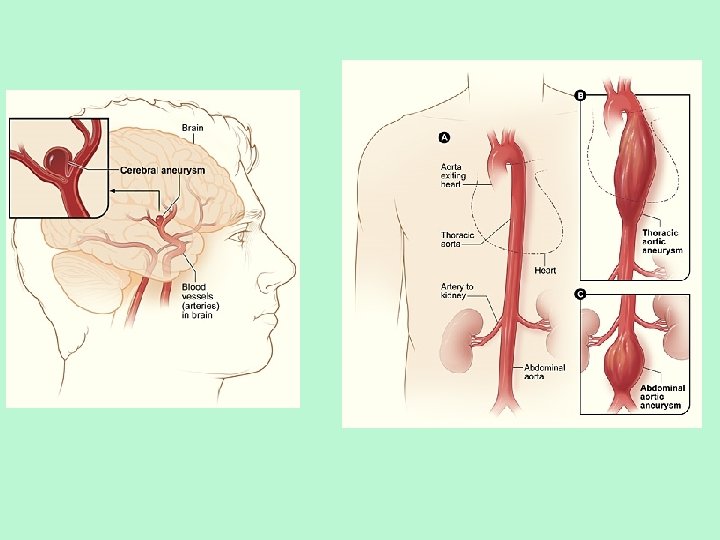
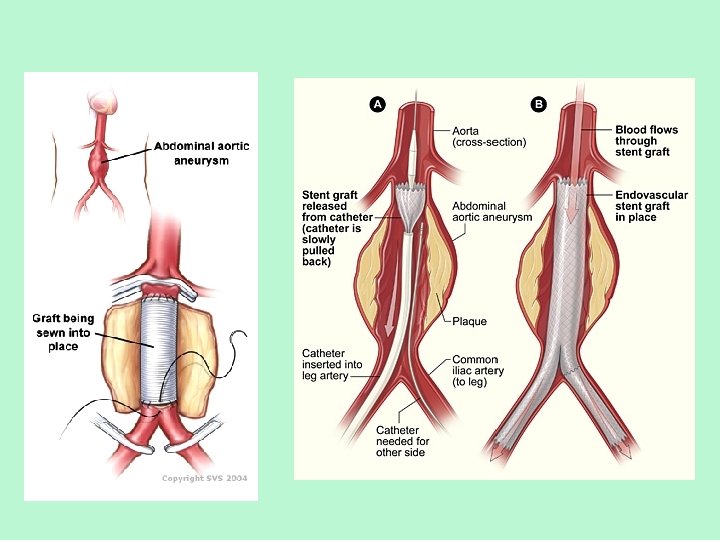
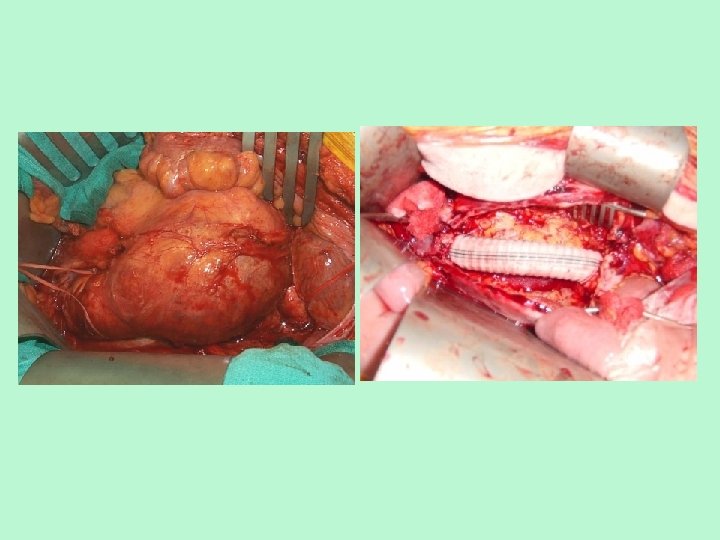
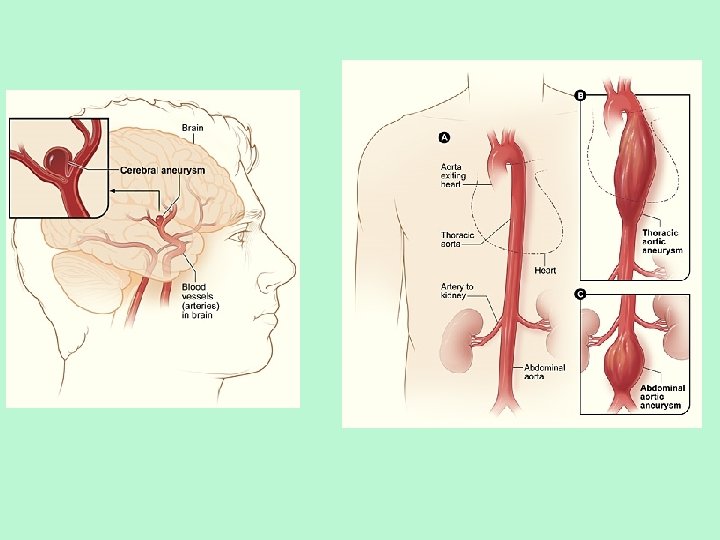
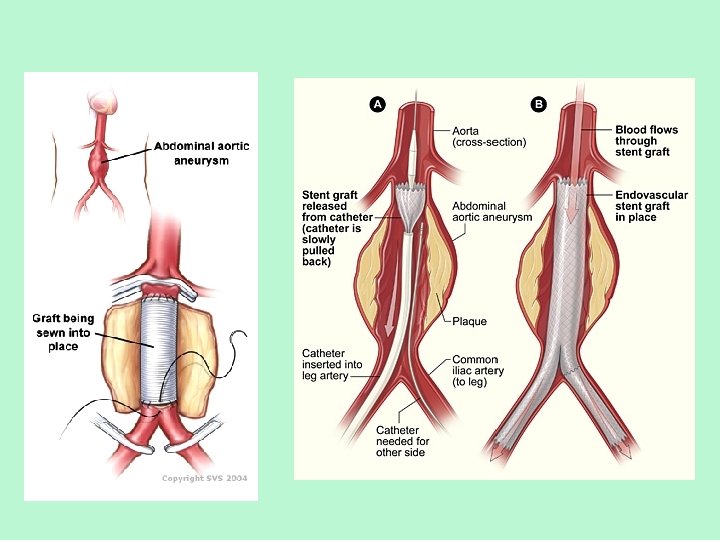
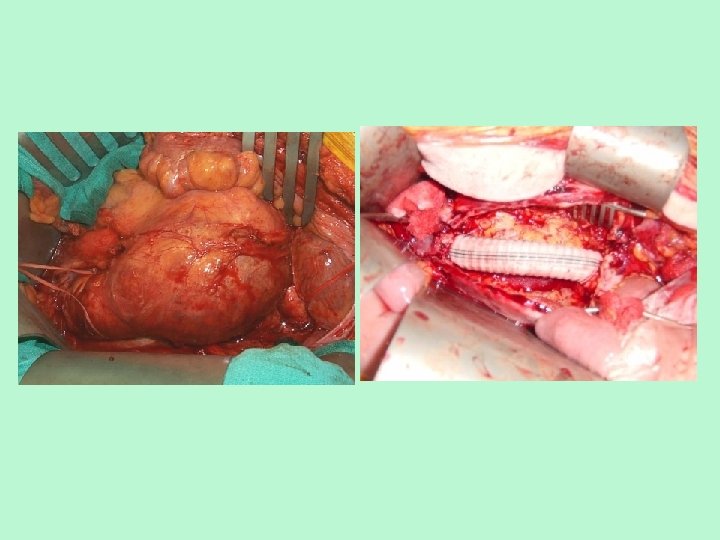
Conditions • Aneurysm – Blood filled bulge of blood vessel – Usually an artery – Caused by disease or weak vessel wall – Base of brain and aorta most common places to happen – When it bursts = BAD.
Conditions • Heart Block – AV Node is damaged, which means ventricles beat at their own rate, which is slower than normal – ischemia fibrillation cardiac arrest death – Pacemaker can be implemented
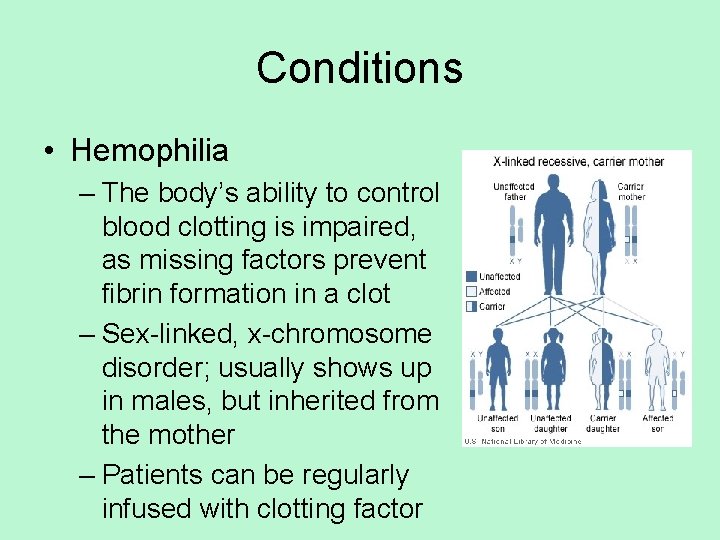
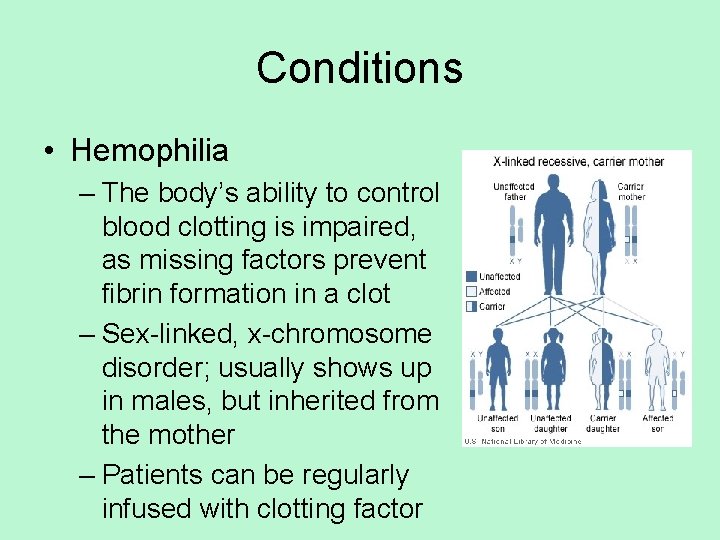
Conditions • Hemophilia – The body’s ability to control blood clotting is impaired, as missing factors prevent fibrin formation in a clot – Sex-linked, x-chromosome disorder; usually shows up in males, but inherited from the mother – Patients can be regularly infused with clotting factor

• Hemophilia in European royalty is featured prominently and thus is sometimes known as "the royal disease". Queen Victoria passed the mutation to her son Leopold and, through several of her daughters, to various royals across the continent, including the royal families of Spain, Germany, and Russia.
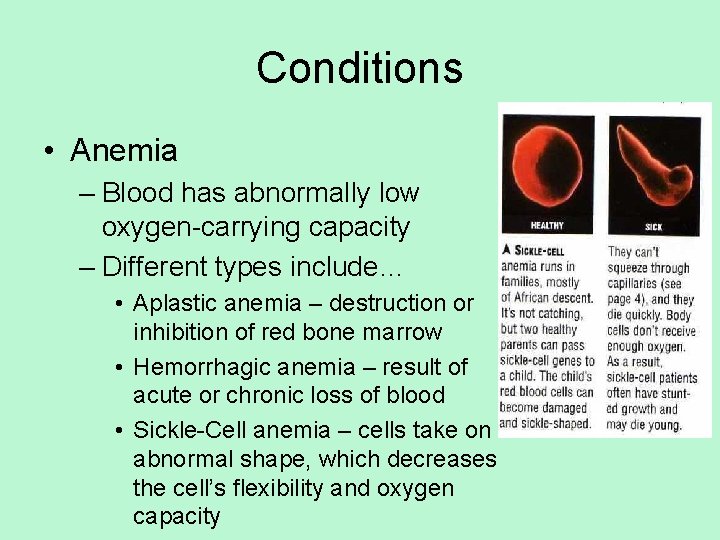
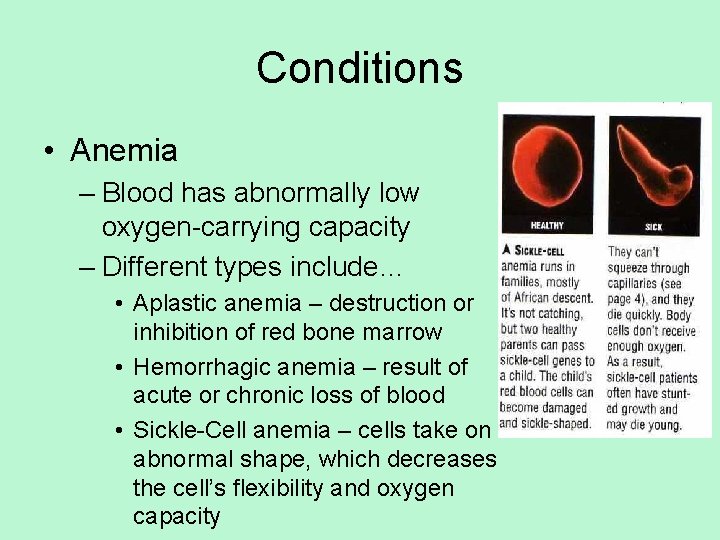
Conditions • Anemia – Blood has abnormally low oxygen-carrying capacity – Different types include… • Aplastic anemia – destruction or inhibition of red bone marrow • Hemorrhagic anemia – result of acute or chronic loss of blood • Sickle-Cell anemia – cells take on abnormal shape, which decreases the cell’s flexibility and oxygen capacity