UNIT 5 NURSING PROCESS Mrs Nidhina Paul LECTURER

- Slides: 44
UNIT : 5 NURSING PROCESS Mrs. Nidhina Paul LECTURER YNC
LEARNING OBJECTIVEES At the end of the class students will be able to: Ø Identify a client’s health status and actual or potential health problems or needs. Ø Establish plans to meet the identified needs. Ø Deliver specific nursing interventions to meet those needs. Ø Achieve scientifically- based, holistic, individualized care for the client. Ø Achieve the opportunity to work collaboratively with clients, others.
INTRODUCTION • The term NURSING PROCESS originated in 1955 by Haul. Nursing process is the foundation of nursing profession. It Serves as a guide for professional nursing practice, which Identifies and discovers health care needs of the patient/family/community. The Nursing Process enables the nurse to organize and deliver nursing care.
NURSING PROCESS DEFINITION: A systematic problem-solving approach used to identify, prevent and treat actual or potential health problems and promote wellness.
• Nursing Process is an orderly, systemic manner of determining the client’s problem, making plans to solve them, initiating the plan or assigning others to implement it and evaluating the extent to which the plan was effective in resolving the identified problem. [Yura and Walsh]
• It is synonymous with the PROBLEM SOLVING APPROACH that directs the nurse and the client to determine the need for nursing care, to plan and implement the care and evaluate the result. • It is a G O S H approach (goal-oriented, organized, systematic and humanistic care) for efficient and effective provision of nursing care.
CHARACTERISTICS OF THE NURSING PROCESS • • Cyclic dynamic in nature Flexible Client centered Focus on problem solving & Decision making Interpersonal & Collaborative style Universal applicability Use of critical thinking.
BENEFITS • Continuity of care • Prevention of duplication • Individualized care • Standards of care • Increased client participation • Collaboration of care • Economical • Facilitates documentation
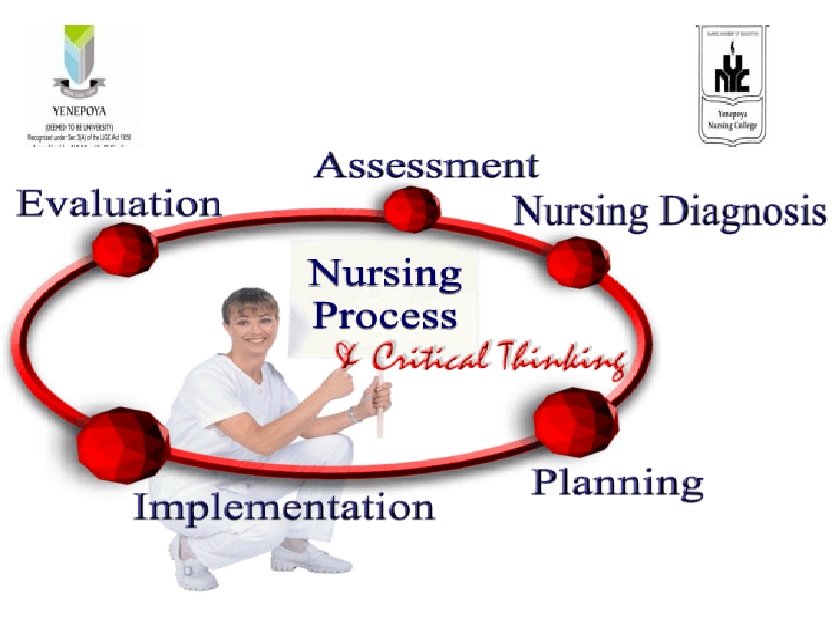
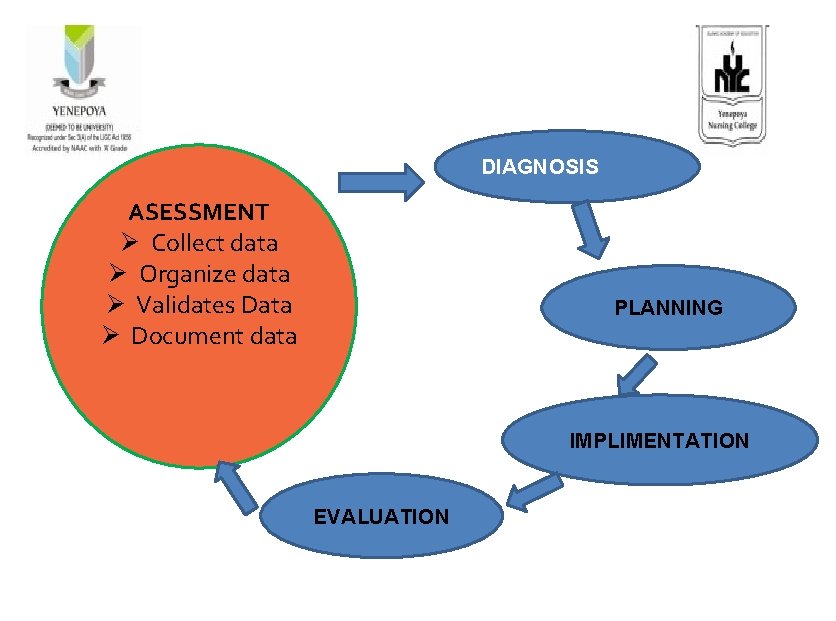
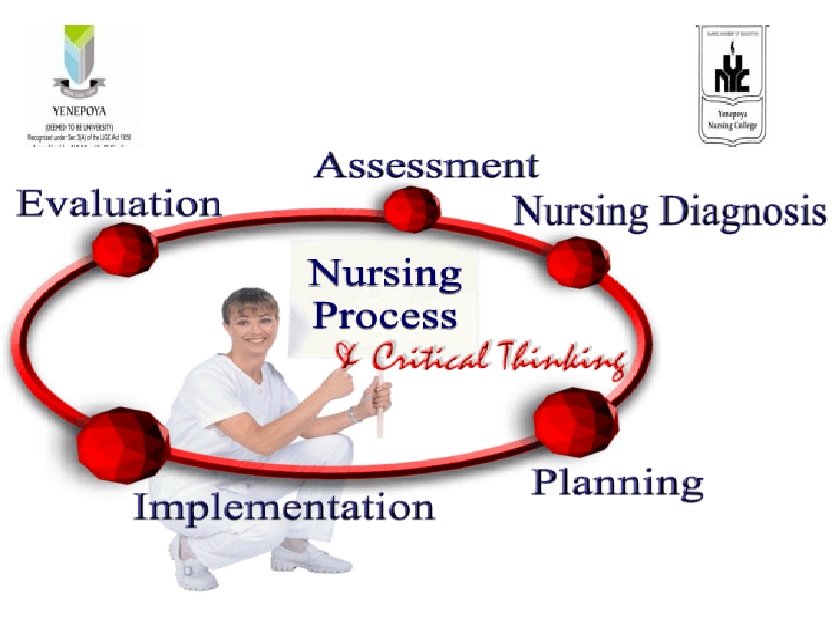
PHASES/ STEPS a. Assessment b. Diagnosis c. Planning d. Implementation e. Evaluation
ASSESSMENT DIAGNOSIS a. Collect data a. Analyze data b. Organize data b. Identify health c. Validate data problems, risk, and d. Analyze data Strengths e. Document data c. Formulate diagnostic statements
PLANNING IMPLEMENTATION a. Prioritize problems/diagnoses a. Reassess the client b. Formulate goals/desired outcome c. Select nursing interventions d. Write nursing orders b. Determine the nurse’s need for assistance c. Implement the nursing interventions d. Supervise delegated case e. Document nursing activities
ASSESSMENT • It is the systematic and continuous collection, organization, validation, and documentation of data (information) as compared to what is standard / norm. • It is continuous process carried out during all phases of the nursing process. • All phases of nursing process depend on the accurate and complete collection of data.
• It is the collection of subjective or objective data from client or others for describing the health problems. • First step of nursing process and is the first stage of problem identification. It includes the following activities
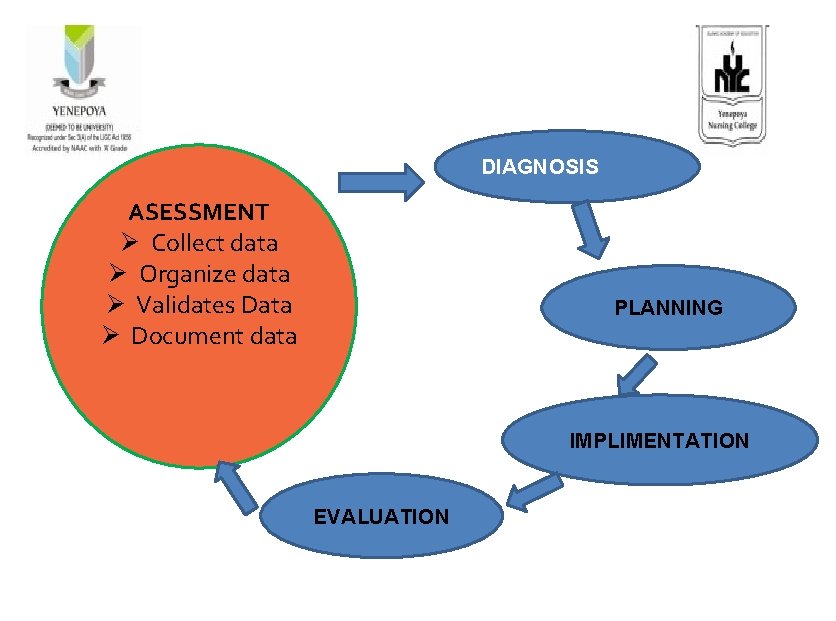
DIAGNOSIS ASESSMENT Ø Collect data Ø Organize data Ø Validates Data Ø Document data PLANNING IMPLIMENTATION EVALUATION
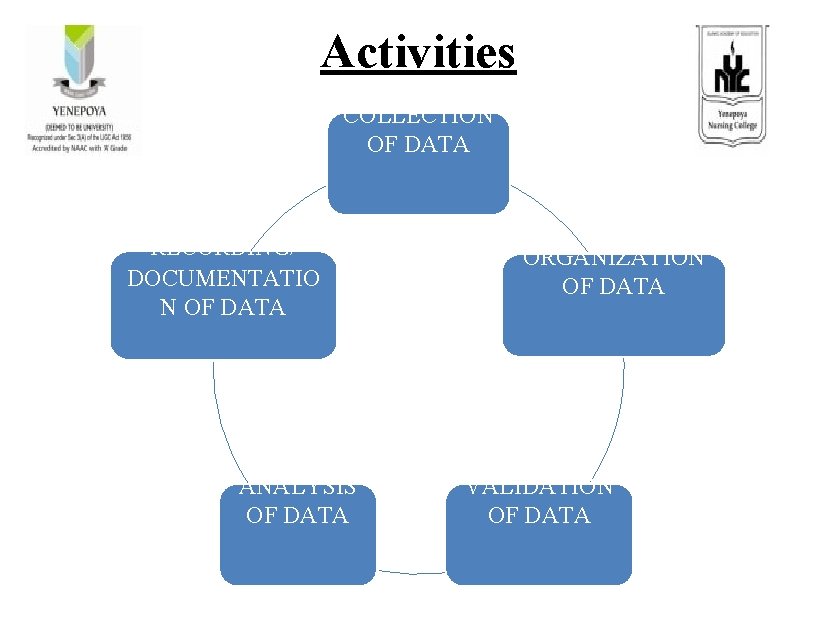
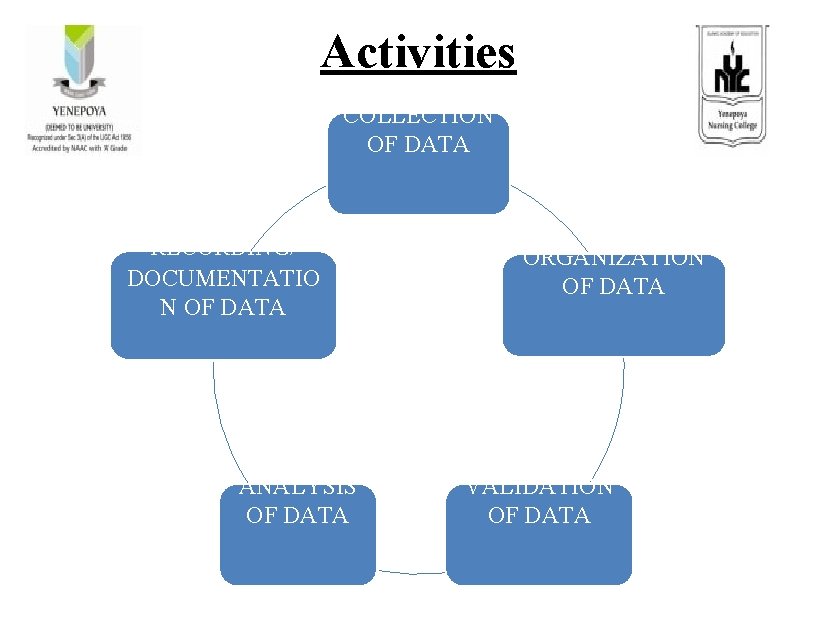
Activities COLLECTION OF DATA RECORDING/ DOCUMENTATIO N OF DATA ANALYSIS OF DATA ORGANIZATION OF DATA VALIDATION OF DATA
PURPOSE • To establish baseline information on the client. • To determine the client’s normal function. • To determine the client’s risk for diagnosis function. • To determine presence or absence of diagnosis function. • To determine client’s strengths. • To provide data for the diagnostic phase
Collecting Data • Process of gathering information about a client’s health status. • It must be both systematic & continuous Purpose • To prevent the omission of significant data • To reflect a client’s changing health status
Client data includes past history as well as current problems. • Past history • Current Problems v History of allergic v. Pain to penicillin v. Nausea v Past surgical procedures v. Sleep patterns v Chronic disease v. Religious practices
• Types Subjective Data DATA Objective data
Subjective Data/ symptoms/ covert data • Can be verified/ described by only the person who got affected. • Includes the client’s sensations, feelings, values, beliefs, attitudes and perception of personal health status and life situation. e. g. Itching, pain, feelings of worry.
Objective data /signs/ overt data • Detectable by an observer or Can be measured or tested against an accepted standard. • Can be seen, heard, felt or smelled • Obtained by observation or physical examination e. g. Discoloration of skin, BP reading.
• During Physical Examination, the nurse obtains objective data to validate subjective data. • Information supplied by family members, significant others or health professionals are considered subjective if it is not based on fact. • A complete data base of both subjective & objective data provides a base line for comparing the client’s responses to nursing & medical intervention.
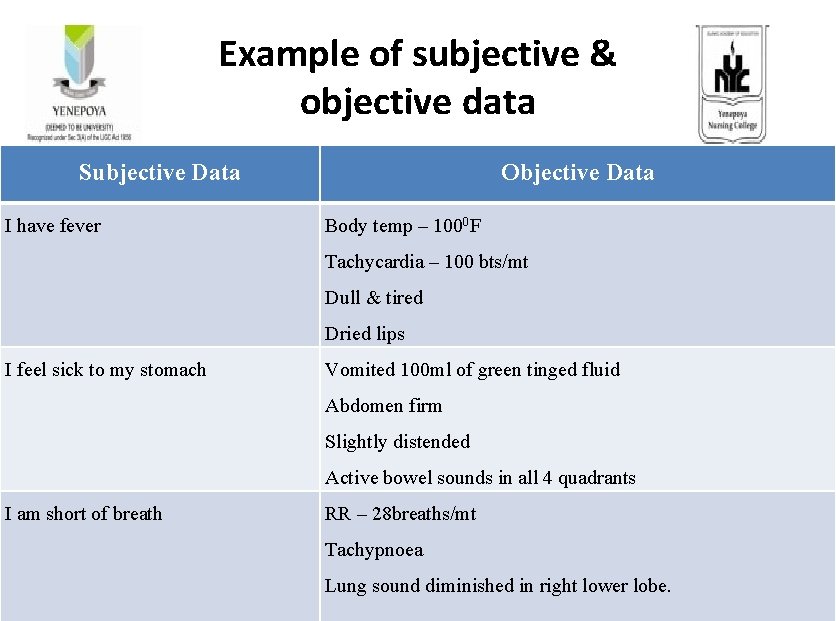
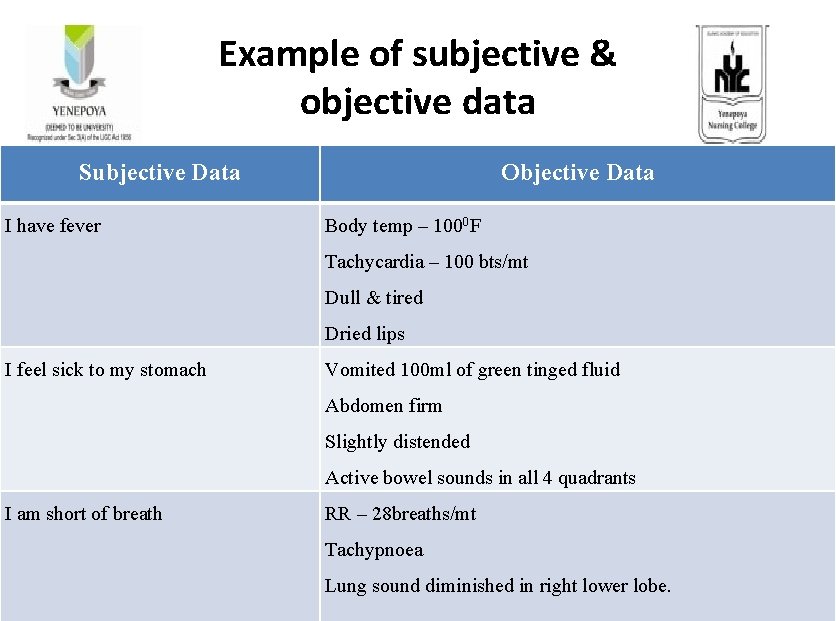
Example of subjective & objective data Subjective Data I have fever Objective Data Body temp – 1000 F Tachycardia – 100 bts/mt Dull & tired Dried lips I feel sick to my stomach Vomited 100 ml of green tinged fluid Abdomen firm Slightly distended Active bowel sounds in all 4 quadrants I am short of breath RR – 28 breaths/mt Tachypnoea Lung sound diminished in right lower lobe.
Sources Primary or secondary. • Client is the primary source of data. • Secondary or indirect sources are family members or other support persons, other health professionals, records & reports, laboratory and diagnostic analyses, and relevant literature. • All sources other than the client are considered secondary sources.
Primary Source- client best source of data Secondary support people, client records, healthcare professionals, literature *Support People- useful if pt is too young, too ill, confused *Client Records-medical records, therapy and laboratory records *Healthcare professionals- nurses, social workers, primary health providers <sharing information among professionals ensure continuity of care
Client • The best source of data • unless the client is to ill, young or confused to communicate clearly. • The client can provide subjective data that no one else can offer.
Support people • Family members, friends and care givers who know the client well, can supplement or verify information provided by the client. • They might convey information about the client’s response to illness, the stresses client was experiencing before the illness, family attitude on health and illness, the client’s home environment
• In reality, the nurse uses all three methods simultaneously when assessing the clients. e. g. During the client interview, the nurse observes, listens, asks questions, and mentally retains information, to explore in the physical examination.
Observation • Gathering data by the senses. • A conscious, deliberate skill that is developed through effort & with an organized approach.
Methods of Observation v 1. OBSERVATION v Vision: - overall appearance (body size, general weight, signs of distress or posture & grooming) discomfort, facial & body gestures, skin colour & lesions v Smell: - Body or Breath odors. v Hearing: - lung, heart sounds, bowel sounds, ability to communicate, language spoken. v Touch: - Skin temperature, moisture, muscle strength (Hand grip)
Interviewing • Planned communication • Conversation with a purpose to get information, identify problem, • Teach, provide support and therapy and counseling
Examining • Major method used in physical health assessment TECHNIQUES: (IPPA) • Inspection assessing by the use of sense of sight • Palpation examining by sense of touch using fatpads of the finger • Percussion tapping body part to produce sounds • Auscultation listening to body sounds with the use of stethoscope
WAYS OF EXAMINING Cephalocaudal- “head to toe approach” • head-neck-thorax-abdomen-extremities-toes 2. Body System- respiratory system, circulatory system, nervous system, etc. 3. Screening examination- “review of systems” • -brief review of essential functioning (nursing admission assessment form)
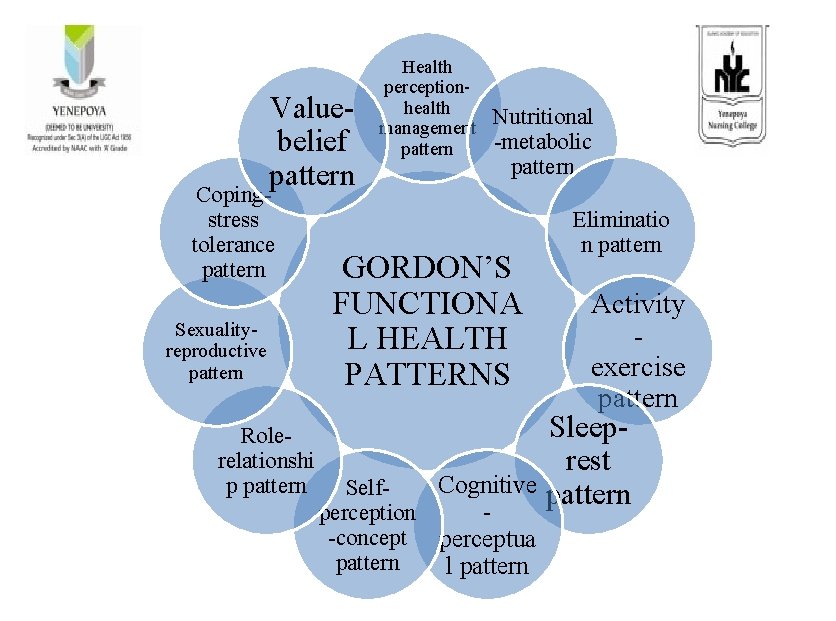
Organization of data Uses a written or computerized format that organizes assessment data systematically. • Maslow’s basic needs • Body system model • Gordon’s functional health patterns

MASLOW'S HIERARCHY OF NEEDS
BODY SYSTEMS MODEL /MEDICAL MODEL / REVIEW OF SYSTEMS • It focuses on the client’s major anatomic systems. • The framework allows nurses to collect data about past and present condition of each organ or body system and to examine thoroughly all body systems for actual and potential problems.
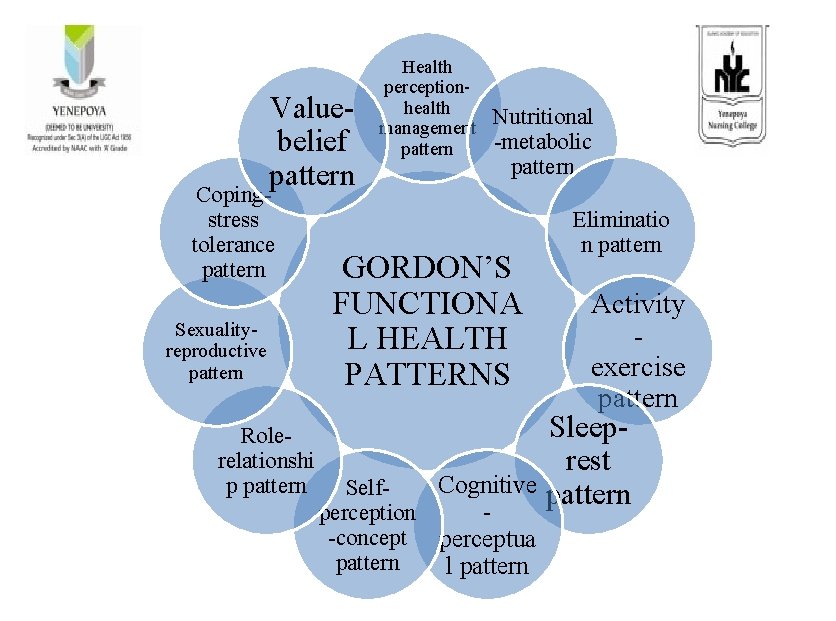
Valuebelief pattern Copingstress tolerance pattern Sexualityreproductive pattern Rolerelationshi p pattern Health perceptionhealth management pattern Nutritional -metabolic pattern GORDON’S FUNCTIONA L HEALTH PATTERNS Selfperception -concept pattern Eliminatio n pattern Activity exercise pattern Sleeprest Cognitive pattern perceptua l pattern
Validation of Data • The information gathered during assessment phase must be complete, factual, and accurate because the nursing diagnoses and interventions are based on this information. • Validation is double checking or verifying whether the data is accurate and factual. • Comparison with another source v patient or family member v record v health team member
Purposes 1. Ensure that data collection is complete 2. Ensure that objective and subjective data agree 3. Obtain additional data that may have been overlooked 4. Avoid jumping to conclusion 5. Differentiate cues and inferences
Analysis of data • Compare data against standard and identify significant cues. • Standard/norm are generally accepted measurements, model, pattern: e. g. Normal vital signs, Standard weight and height, Normal laboratory/diagnostic values, Normal growth and development pattern
Cues - subjective and objective data that can be directly observed by the nurse. (What client can say, what the nurse can see, hear, feel, smell or measure) • Inferences - Nurses interpretation or conclusions made based on the cues e. g. Red, swollen wound = infected wound,
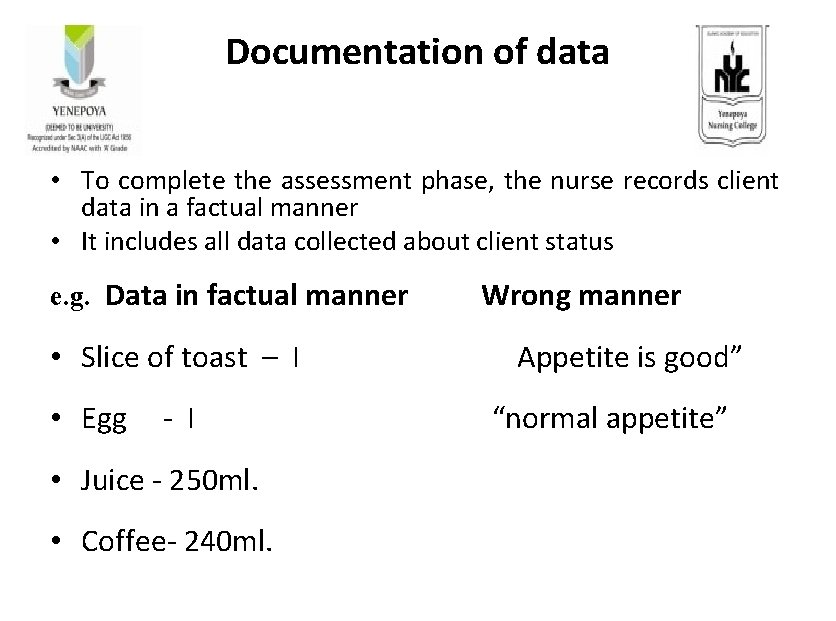
Documentation of data • To complete the assessment phase, the nurse records client data in a factual manner • It includes all data collected about client status e. g. Data in factual manner Wrong manner • Slice of toast – I Appetite is good” • Egg - I “normal appetite” • Juice - 250 ml. • Coffee- 240 ml.
• Record subjective data in client’s own words (enclose in “ ___” ). It is more accurate • Avoid generalizations – be specific • Don’t make summative statements