Unit 4 The Integumentary System Integumentary System Also




- Slides: 75
Unit 4 – The Integumentary System
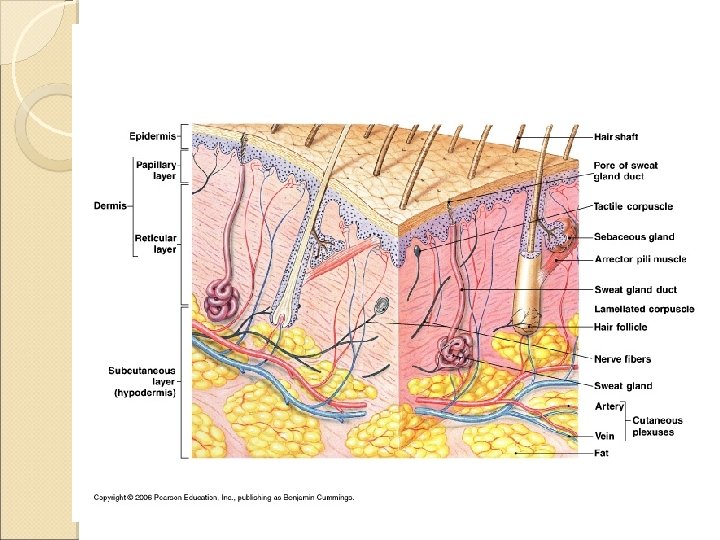
Integumentary System Also known as the Integument ◦ Accounts for 16% of your body weight ◦ First line of defense ◦ Almost 2 m 2 Consists of 2 major components ◦ Cutaneous membrane ◦ Accessory structures
Integumentary System Cutaneous membrane has two layers ◦ Epidermis ◦ Dermis Accessory structures include: ◦ Hair ◦ Nails ◦ Exocrine glands
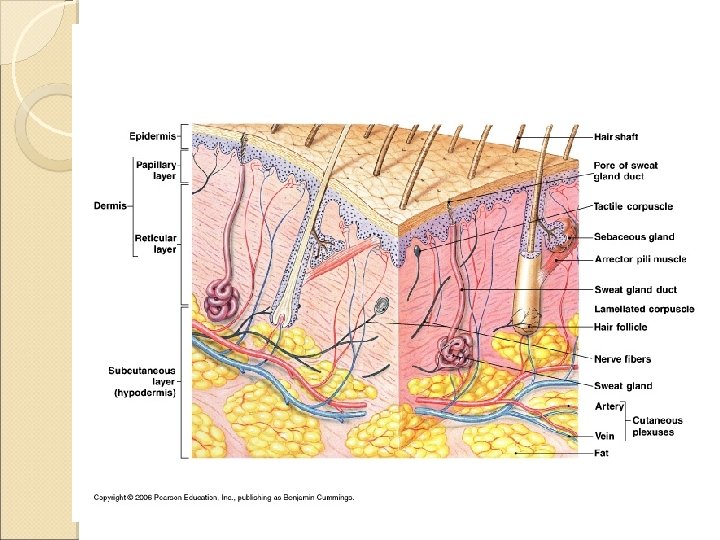
Integumentary System Blood vessels and nerves are found in the dermis Deep to the dermis, is the subcutaneous layer (hypodermis)
Integumentary System Functions of skin and subcutaneous layer: ◦ Protection ◦ Excretion ◦ Maintenance of body temperature ◦ Synthesis if vitamin D ◦ Storage of fats ◦ Detection of touch, pressure, pain, temperature
Integumentary System THE EPIDERMIS
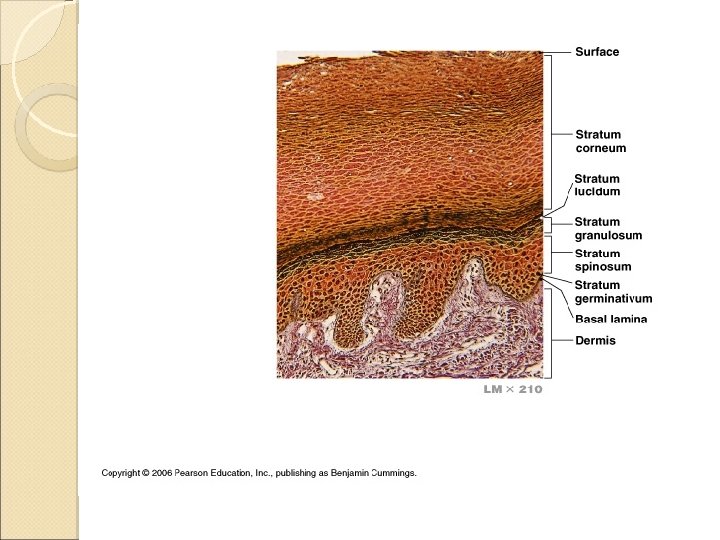
The Epidermis Stratified squamous epithelial tissue ◦ Mostly keratinocytes (contains keratin) Is comprised of several layers (deep to superficial) Stratum germinativum Stratum spinosum Stratum granulosum Stratum lucidum Stratum corneum Thin Skin – covers Thick skin – palms feet most of your body of hands, soles of
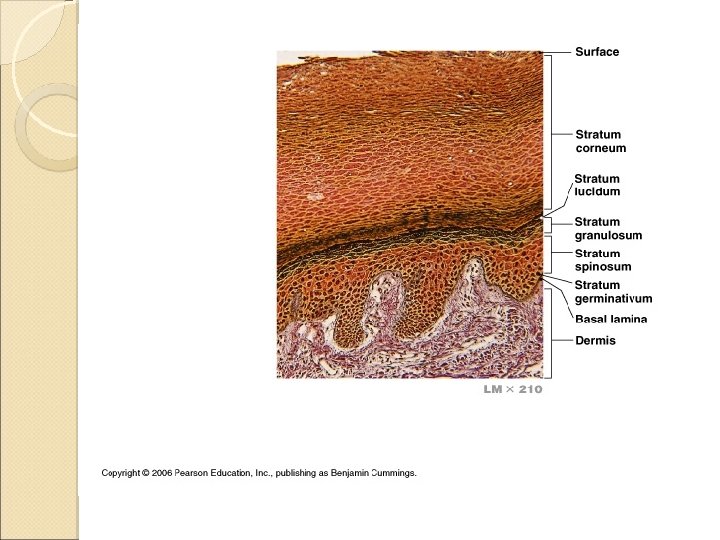
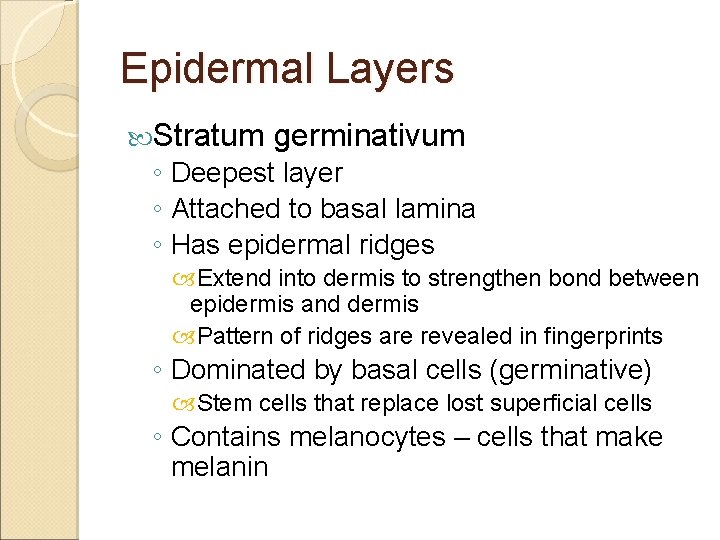
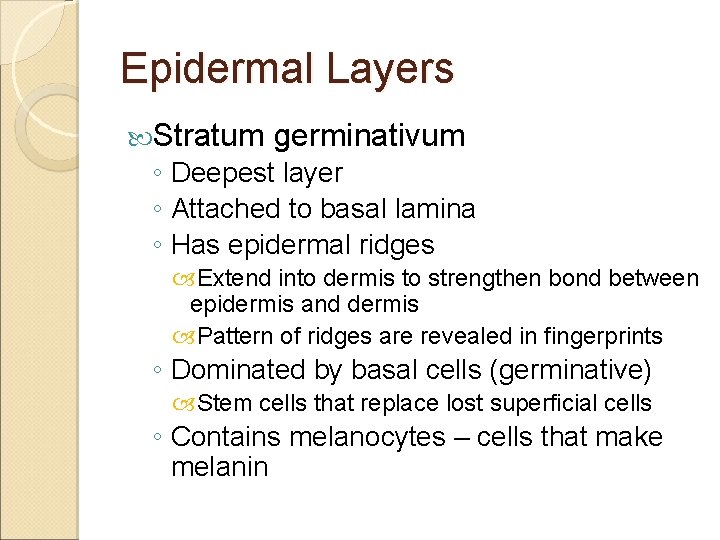
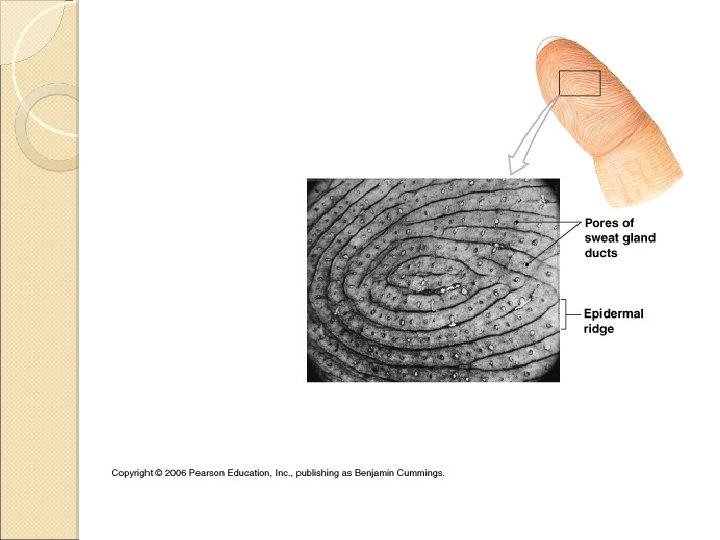
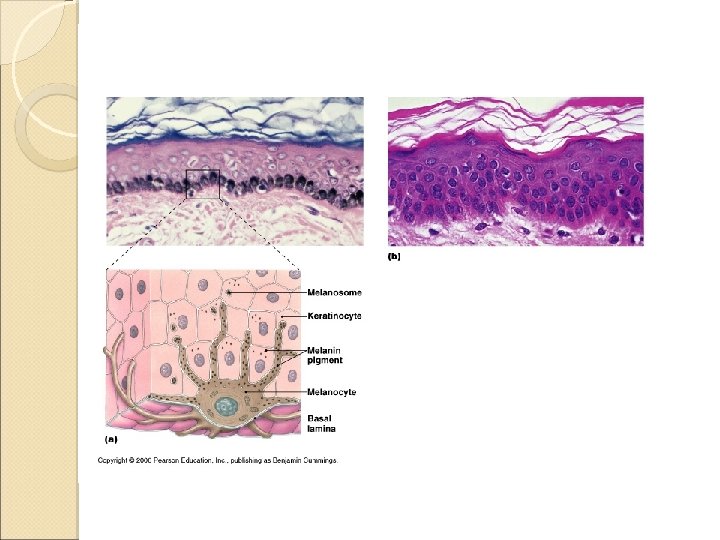
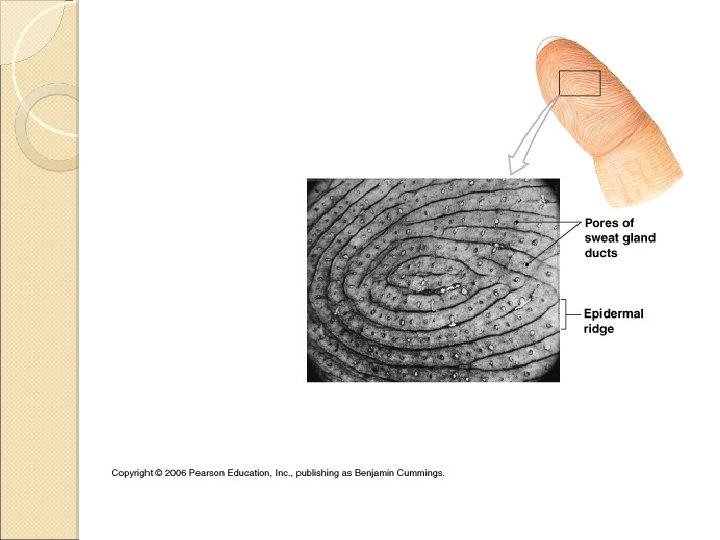
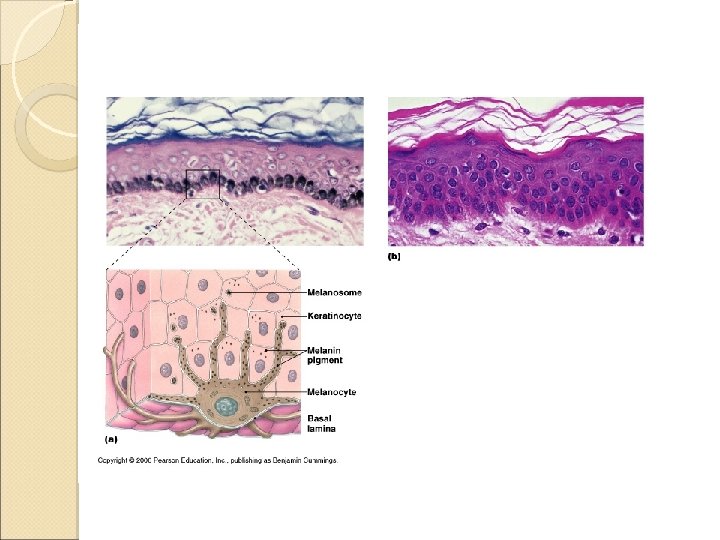
Epidermal Layers Stratum germinativum ◦ Deepest layer ◦ Attached to basal lamina ◦ Has epidermal ridges Extend into dermis to strengthen bond between epidermis and dermis Pattern of ridges are revealed in fingerprints ◦ Dominated by basal cells (germinative) Stem cells that replace lost superficial cells ◦ Contains melanocytes – cells that make melanin
Epidermal Layers Stratum spinosum ◦ 8 -10 layers of cells ◦ Made of freshly divided basal cells
Epidermal Layers Stratum granulosum ◦ “grainy layer” ◦ 3 -5 layers of cells pushed superficially from stratum spinosum ◦ Make large amounts of keratin Basis of hair and nails in humans Makes skin waterproof ◦ Cells die in this layer
Epidermal Layers Stratum lucidum ◦ Found in the palms of your hands and soles of your feet
Epidermal Layers Stratum corneum ◦ The exposed surface of the skin ◦ 15 -30 layers of keratinized cells It takes 15 -30 days for cells to move from the stratum germinativum to the stratum corneum Cells spend about 2 weeks in the stratum corneum before being shed
Epidermal Layers Stratum corneum (con’t) ◦ Is water resistant, but not waterproof Water evaporates at a rate of about 500 ml/day Called insensible perspiration Sweat glands produce sensible perspiration ◦ Blisters are formed when the connections between superficial and deeper layers are damaged. Fluid collects between layers
Integumentary System THE DERMIS
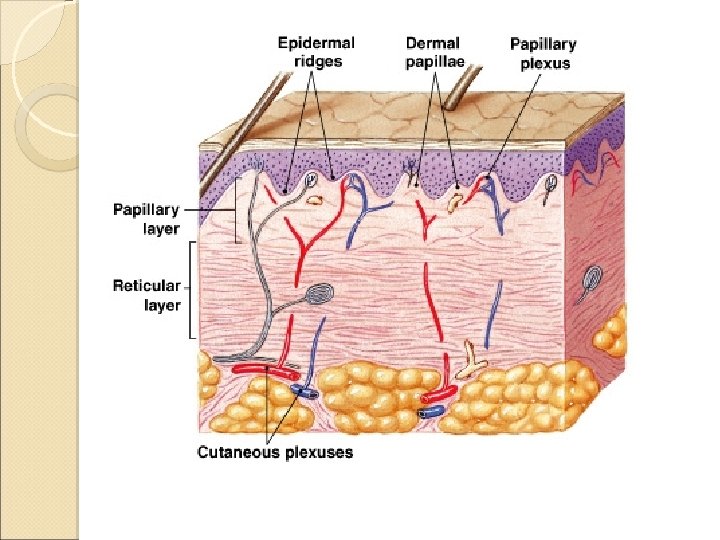
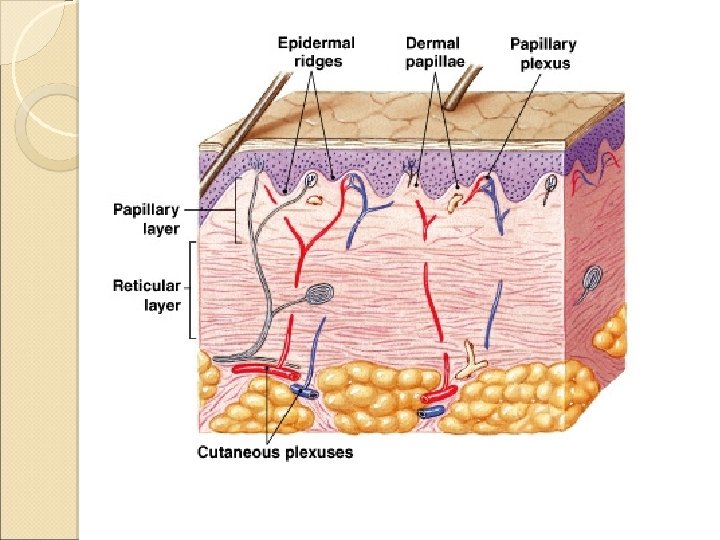
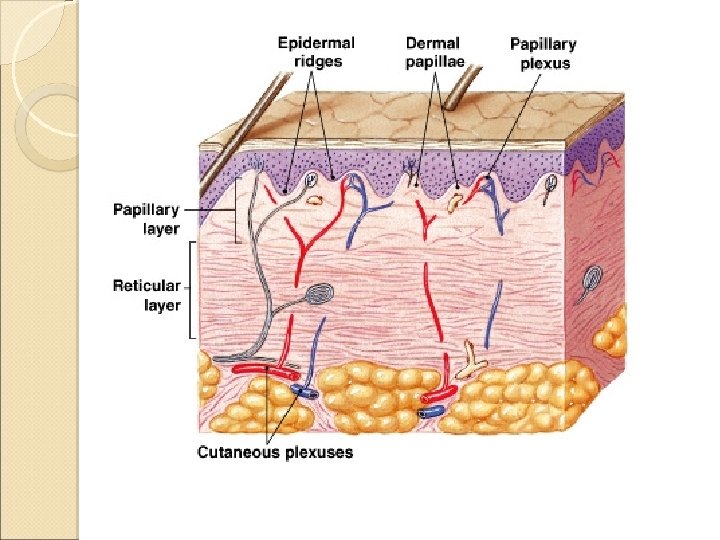
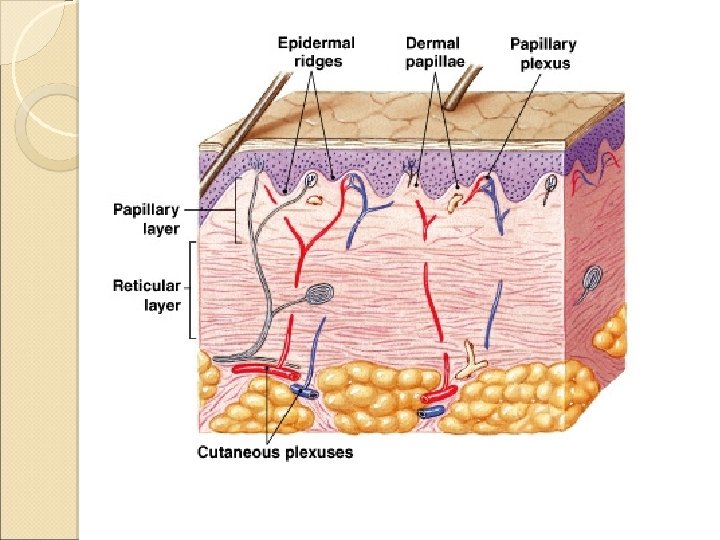
The Dermis Lies between the epidermis and the subcutaneous layer Two major components ◦ Superficial papillary layer ◦ Deeper reticular layer
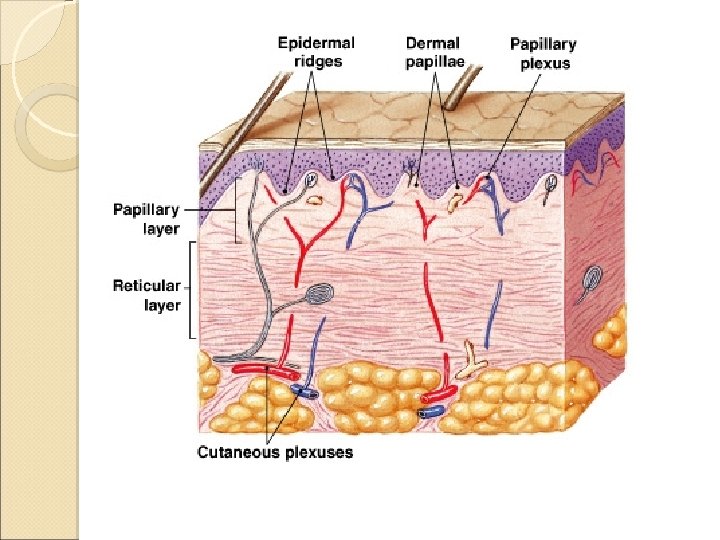
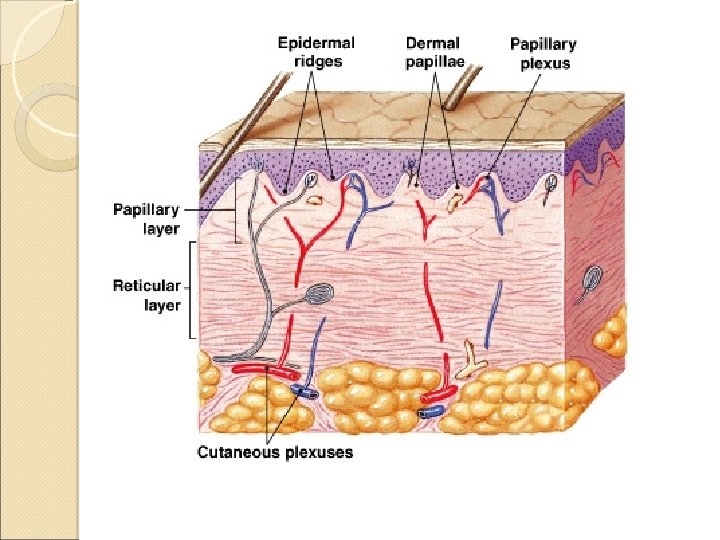
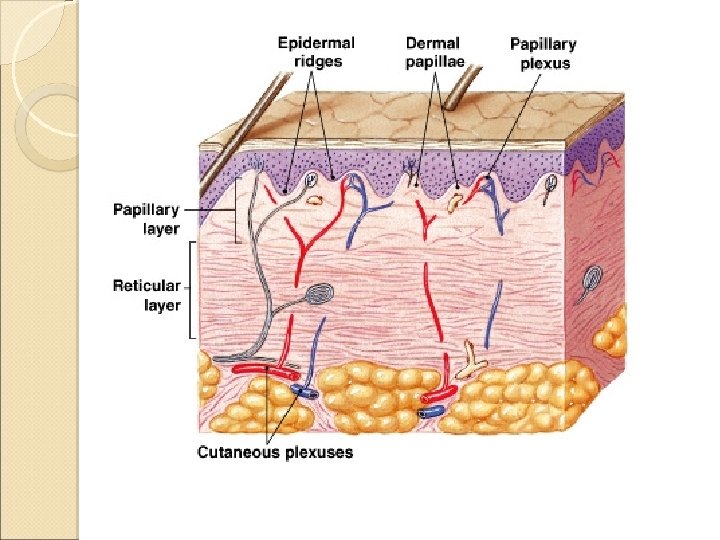
The Papillary Layer Superficial portion of dermis Areolar tissue Contains capillaries, lymphatics, and sensory neurons that supply the surface of the skin Contain dermal papillae that interlock with the epidermal ridges
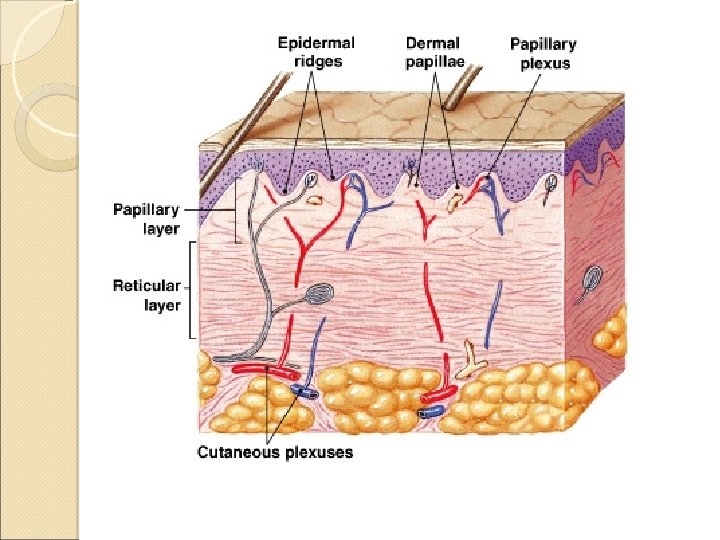
Reticular Layer Deeper portion of dermis Dense irregular connective tissue ◦ Collagen and elastic fibers Contains all cells of connective tissue proper Also contains blood vessels, lymph vessels and nerve fibers
Dermal Strength and Elasticity Dermis contains both collagen and elastic fiber ◦ Allows dermis to tolerate limited stretching Water also helps with flexibility and resilience ◦ Pinch test for dehydration Aging, hormones, UV radiation damages elastic fibers ◦ Leads to wrinkles and sagging skin
Dermal Strength and Elasticity Extensive stretching of dermis can exceed the elastic capabilities of the skin ◦ Complete recoiling of fibers is prevented ◦ Result is stretch marks Retin-A (derivitave of Vitamin A) can help repair the dermis and can lessen appearance of wrinkles and stretch marks.
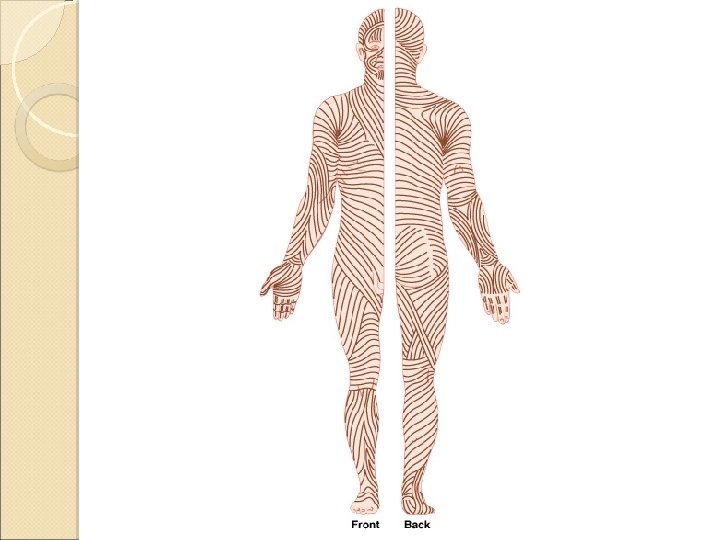
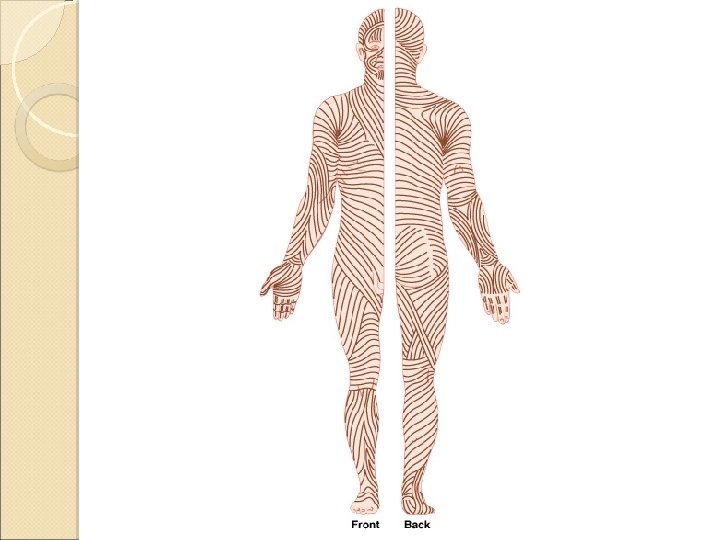
Lines of Cleavage The collagen and elastic fibers in the dermis are usually arranged in parallel bundles ◦ Arranged to resist forces during normal movement ◦ The pattern forms lines of cleavage
Lines of Cleavage Why are the lines important? ◦ Cuts parallel to the lines of cleavage will remain closed and heal with minimal scarring ◦ Cuts perpendicular to the lines will be pulled open by the recoiling elastic fibers and will result in greater scarring.
Integumentary System THE SUBCUTANEOUS LAYER
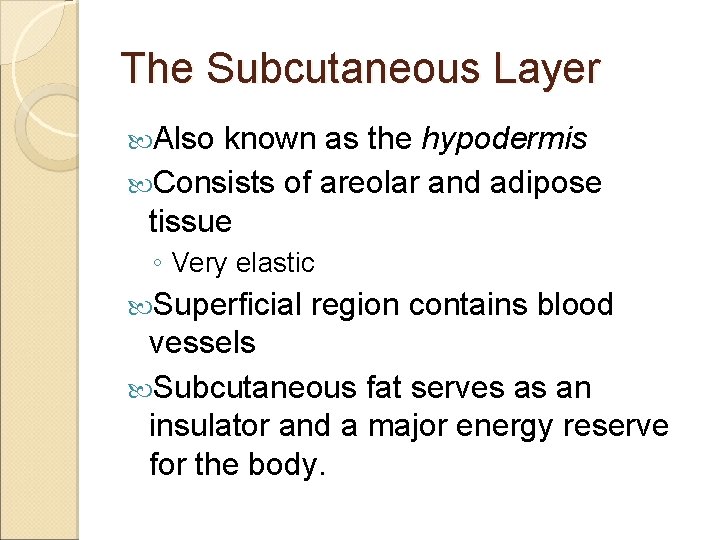
The Subcutaneous Layer Also known as the hypodermis Consists of areolar and adipose tissue ◦ Very elastic Superficial region contains blood vessels Subcutaneous fat serves as an insulator and a major energy reserve for the body.
The Subcutaneous Layer At puberty, distribution of fat starts to differ between the sexes ◦ Men tend to store fat at the neck, arms, low back, and buttocks ◦ Women tend to store fat at the breasts, buttocks, hips and thighs ◦ Both can accumulate fat in the abdominal region
Integumentary System ACCESSORY STRUCTURES
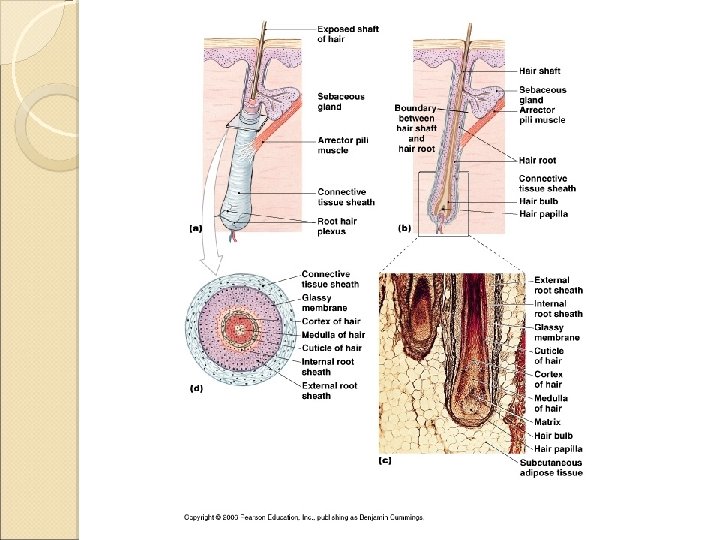
Hair – cover almost every surface of your skin ◦ Exceptions are sides and soles of feet, palms of hands, sides of toes and fingers, lips, portions of external genitalia ◦ Made of the protein keratin
Hair and Hair Follicles Function of hair on head ◦ Protect from UV radiation ◦ Cushion light blows to head ◦ Insulate skull In nostrils and ear: ◦ Prevent entry of foreign particles All hair serve as sensory receptors
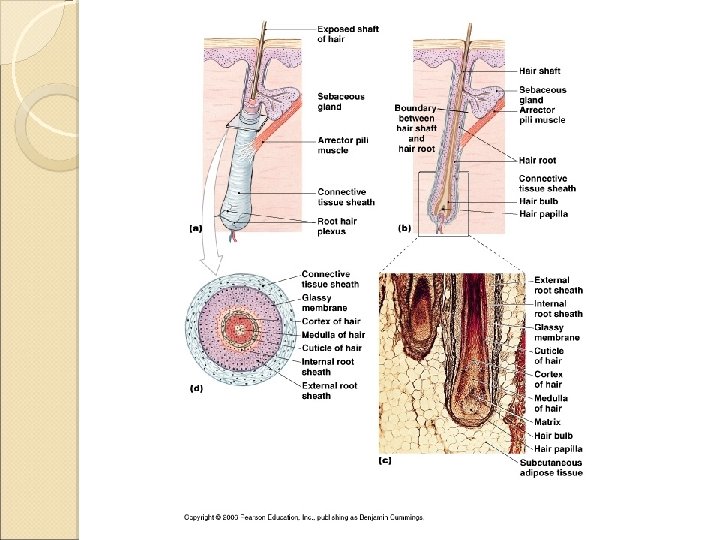
Hair and Hair Follicles Have arrector pili muscles attached to hair follicle ◦ When contracted, makes hair stand up From emotions, cold (goose bumps) In furry mammals, this will increase insulation, but doesn’t have that effect in humans
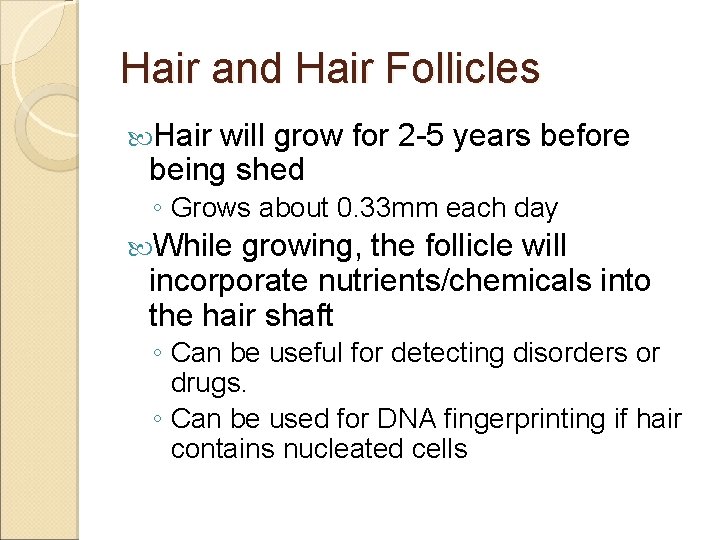
Hair and Hair Follicles Hair will grow for 2 -5 years before being shed ◦ Grows about 0. 33 mm each day While growing, the follicle will incorporate nutrients/chemicals into the hair shaft ◦ Can be useful for detecting disorders or drugs. ◦ Can be used for DNA fingerprinting if hair contains nucleated cells
Hair and Hair Follicles Hair coloration is from the melanocytes producing varying amounts of melanin in the hair follicle Different forms of melanin will give hair a dark brown, yellow-brown, or red appearance
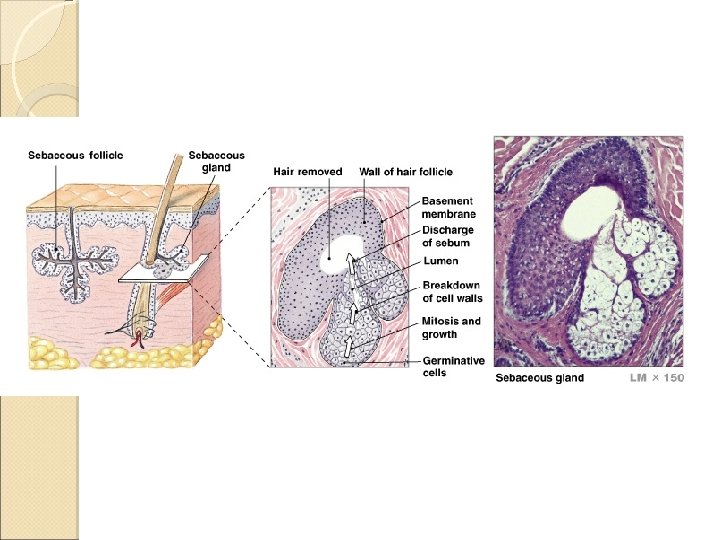
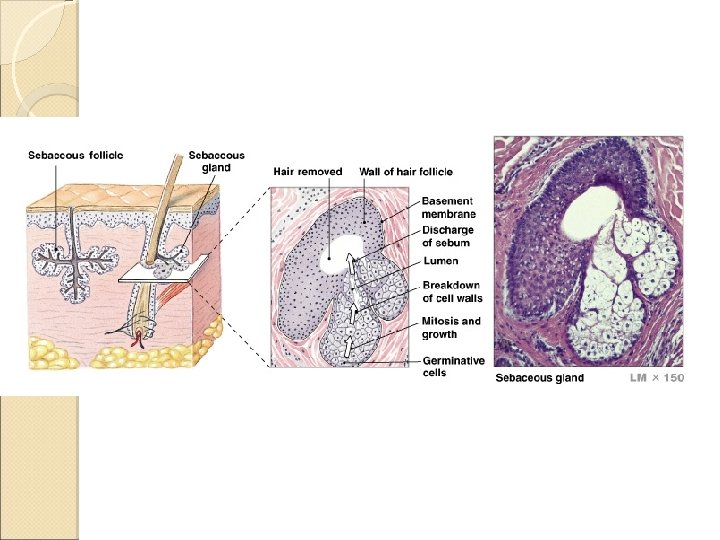
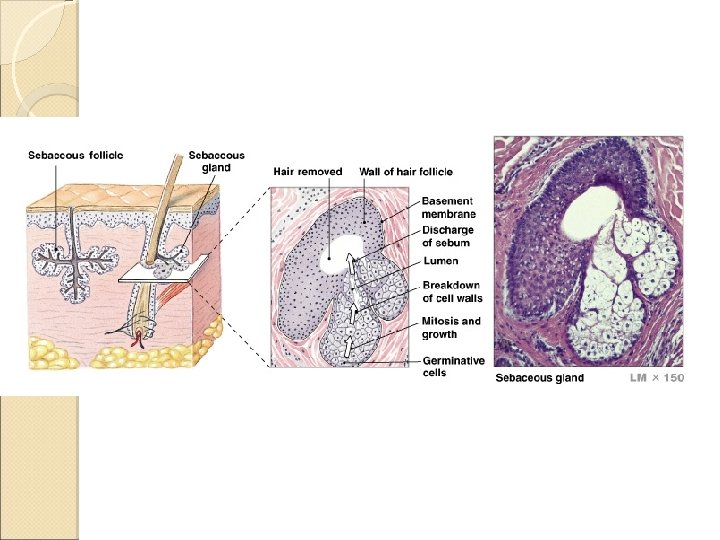
Glands In the Skin Sebaceous (Oil) Glands Can secrete oil from hair follicle or directly onto skin The secreted material is called sebum ◦ Made of fatty acids, cholesterol, proteins, and electrolytes ◦ Inhibits bacteria growth, lubricates and protects hair, and conditions surrounding skin
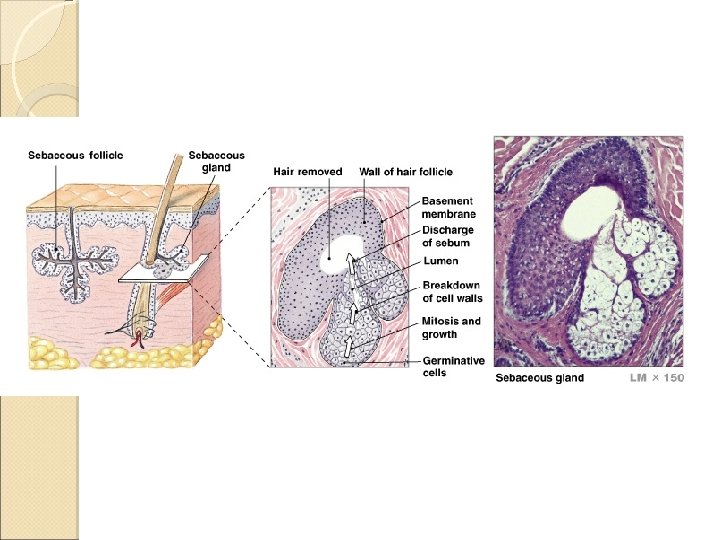
Glands In the Skin Sebaceous (Oil) Glands (Con’t) ◦ Sebaceous follicles Glands NOT associated with hair follicles Discharge sebum directly onto epidermis Located on face, back, chest, nipples, external genitalia Very active just before birth and during puberty
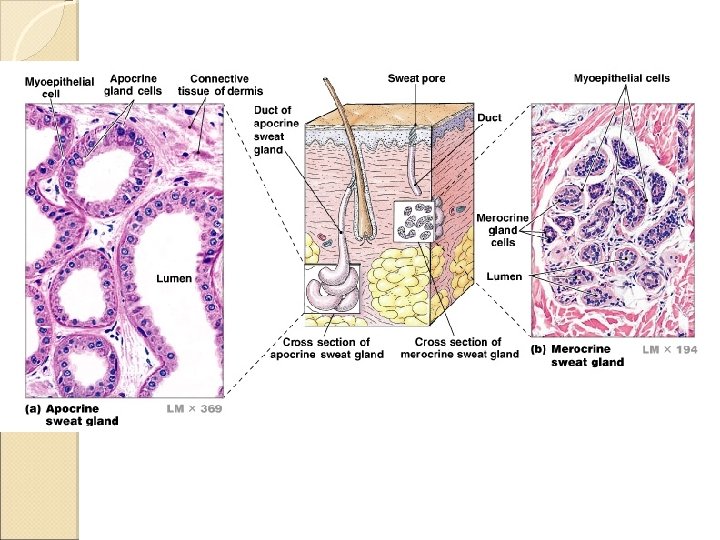
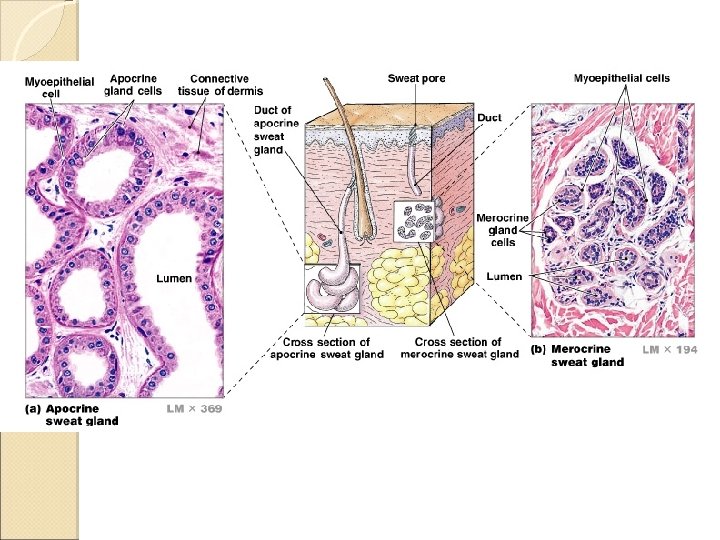
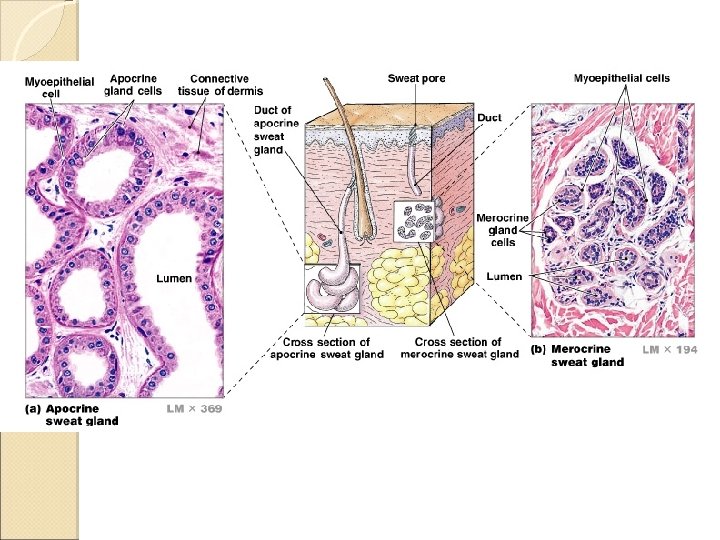
Glands In the Skin Sweat Glands ◦ Also known as sudoriferous glands ◦ Two types Apocrine sweat glands Found in armpits, around nipples, and pubic region Secrete sweat into hair follicles Sticky, cloudy, odorous secretion Begin secreting at puberty This sweat is a nutrition source for bacteria, which intensifies odor
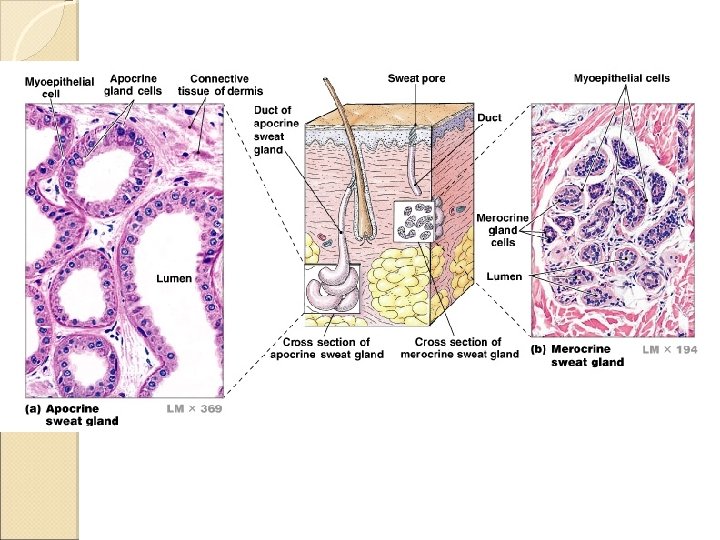
Glands In the Skin Sweat Glands (Con’t) ◦ Two types Merocrine sweat glands Discharge secretion directly onto surface of skin More numerous (2 -5 million) than apocrine glands Palms and soles have highest number 3000 per square inch Secretion is 99% water with some electrolytes (mainly sodium chloride)
Glands In the Skin �Sweat Glands (Con’t) ◦ Two types �Merocrine sweat glands �Functions: �Cool surface of skin (maintain homeostasis) �Excrete water and electrolytes �Provide protection �Dilute harmful chemicals �Discourages growth of mmicroorganisms
Nails Protect exposed dorsal surfaces of the tips of the fingers and toes Made of the protein Keratin
Integumentary System INJURY RESPONSE
Injury Response Excellent regeneration capabilities and response to stresses. Calluses form when repeated stresses from manual labor are placed on the skin ◦ The stem cells of stratum germinativum divide more rapidly, thickening the skin in that area

Injury Response
Injury Response The process of injury repair can be slow Infection repair and fluid loss can complicate The type of injury also determines rate of repair ◦ Thin, straight cut (incision) will generally heal more quickly than a scrape (abrasion) because of the relative surfaces involved

Injury Response Bleeding occurs only when the damage extends into the dermis. Why? ◦ No vessels in epidermis
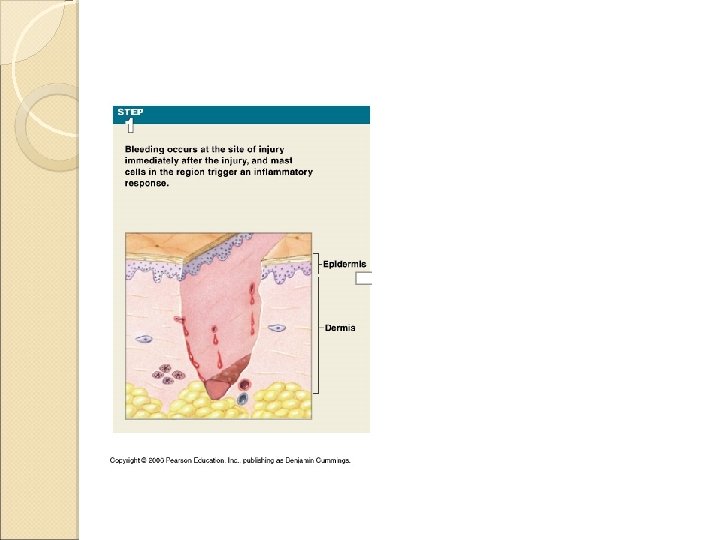
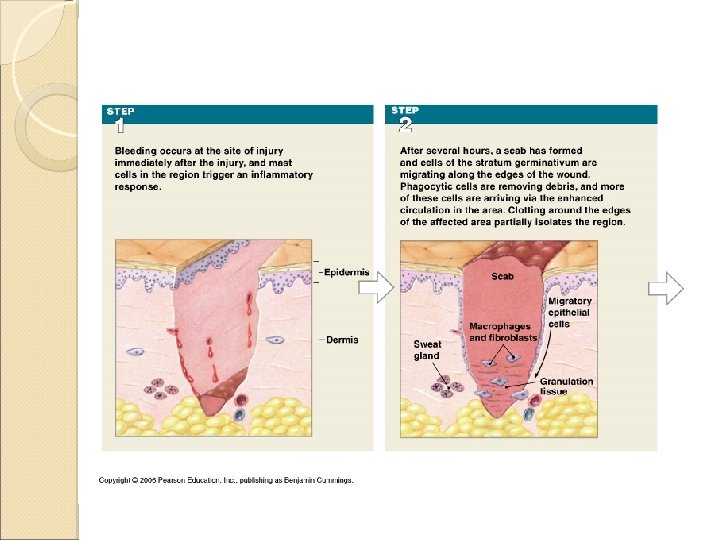
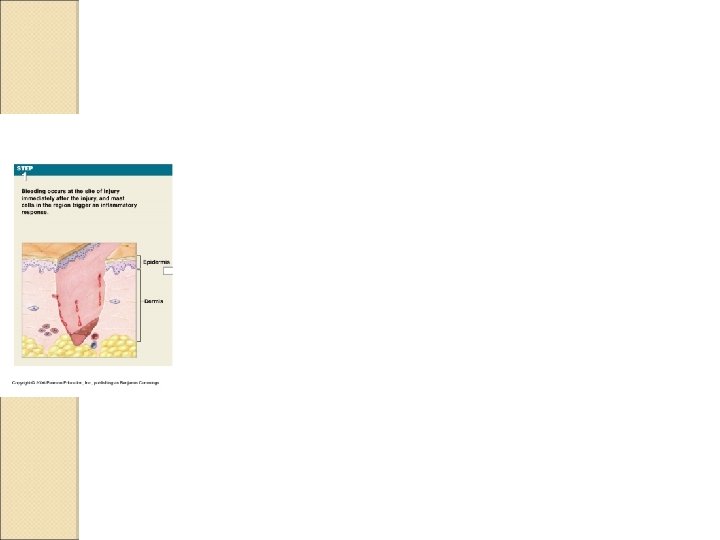
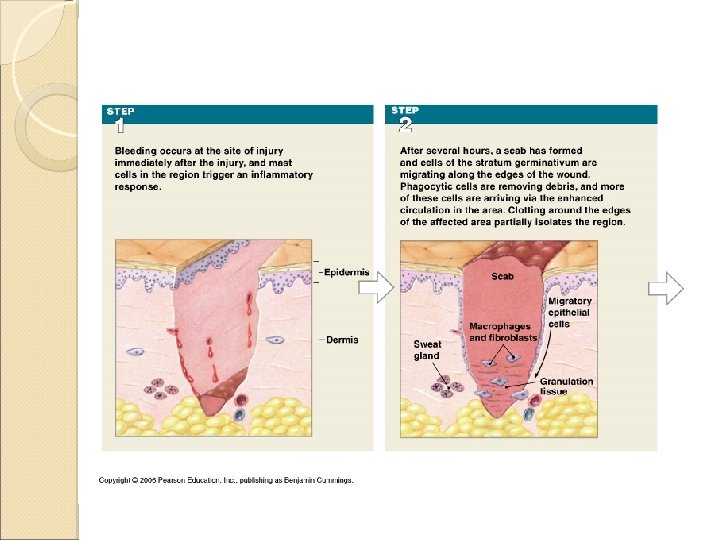
Injury Response Steps to injury response Step 1 Bleeding occurs and mast cells trigger the inflammatory response
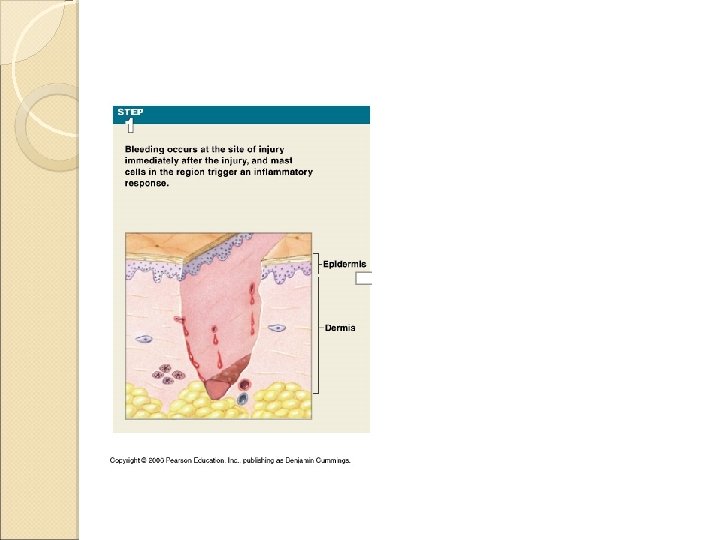
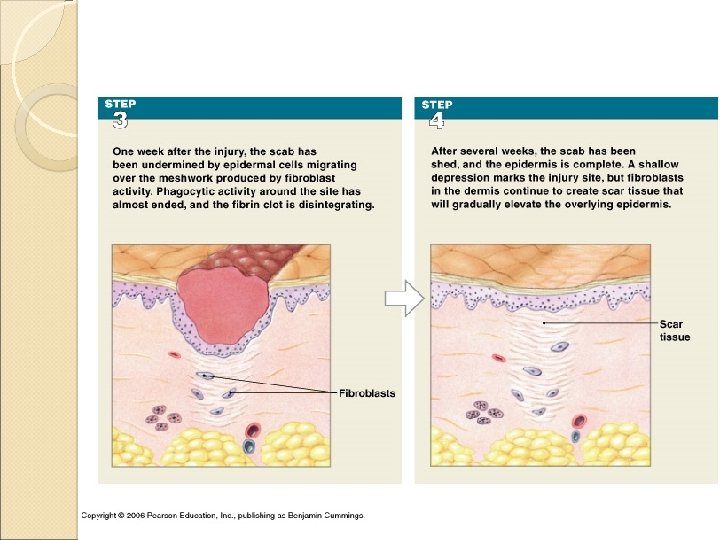
Injury Response Step 2 Blood clot (scab) forms Restores integrity of epidermis Restricts microorganisms from entering area Stratum germinativum cells migrate along edges of wound Divide rapidly to replace epidermal cells Macrophages patrol area collecting debris and pathogens
Injury Response Step 2 (con’t) Increased capillary formation enhances blood flow Combination of blood clot, fibroblasts, and new capillary network is called granulation tissue
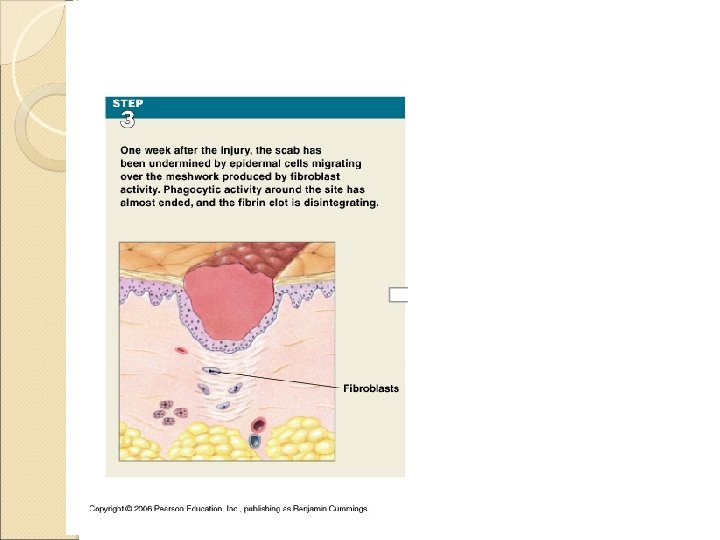
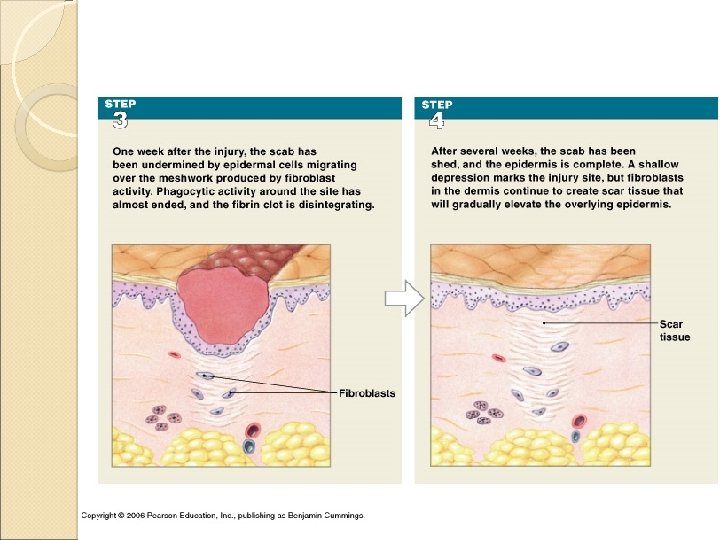
Injury Response Step 3 Over time, deeper portion of clot dissolves Number of capillaries decline Fibroblast activity leads to increase in collagen fibers and ground substance Epidermal cells have migrated over the network of collagen fibers
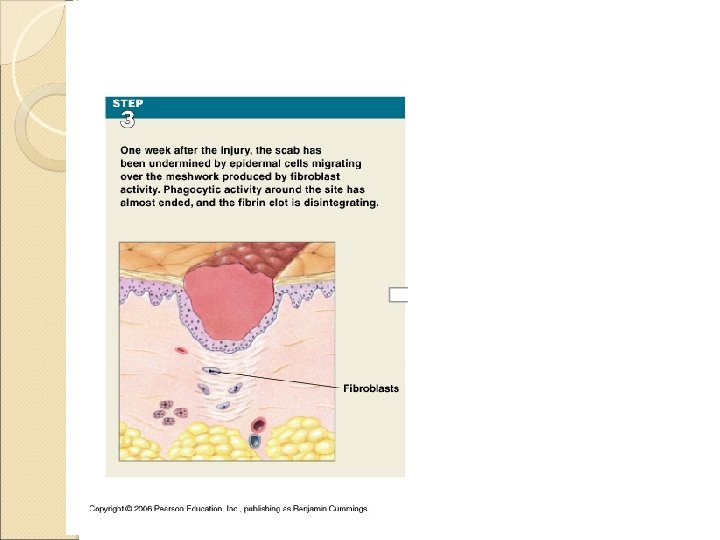
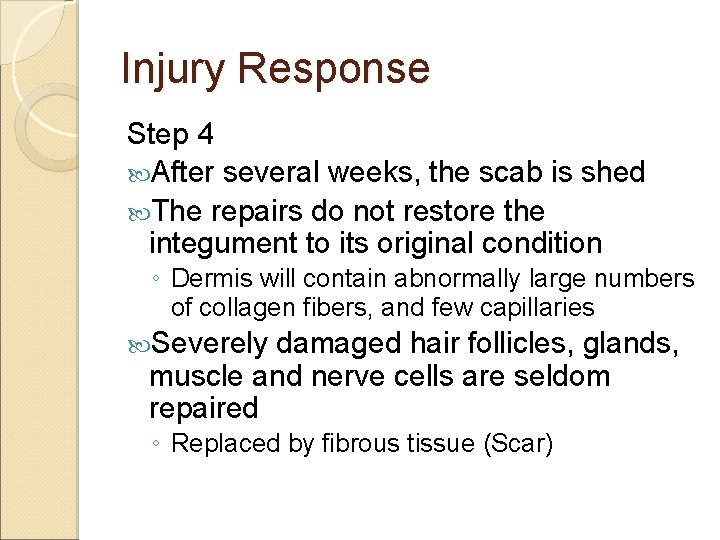
Injury Response Step 4 After several weeks, the scab is shed The repairs do not restore the integument to its original condition ◦ Dermis will contain abnormally large numbers of collagen fibers, and few capillaries Severely damaged hair follicles, glands, muscle and nerve cells are seldom repaired ◦ Replaced by fibrous tissue (Scar)
Integumentary System AGING

Aging and the Integument Effects of aging on the integument ◦ Thinning epidermis
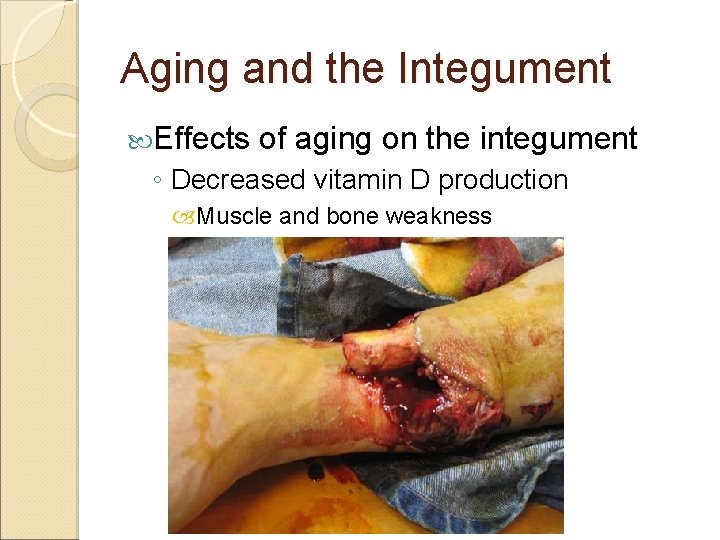
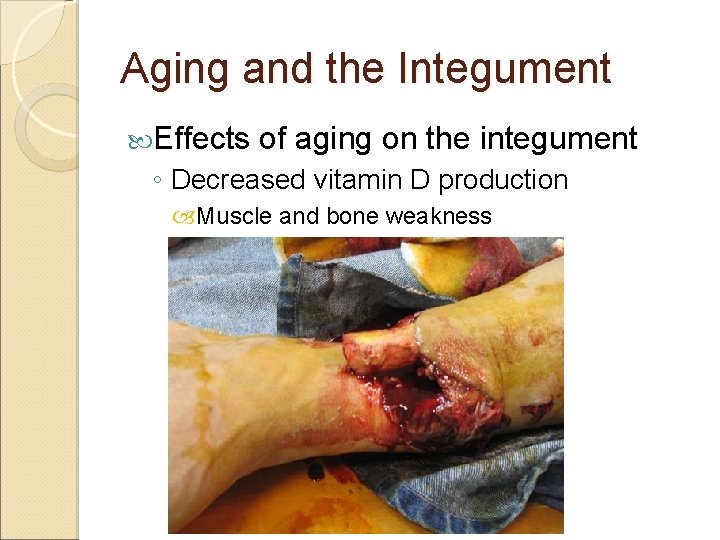
Aging and the Integument Effects of aging on the integument ◦ Decreased vitamin D production Muscle and bone weakness
Aging and the Integument Effects of aging on the integument ◦ Decreased melanocyte activity More sensitive to sun
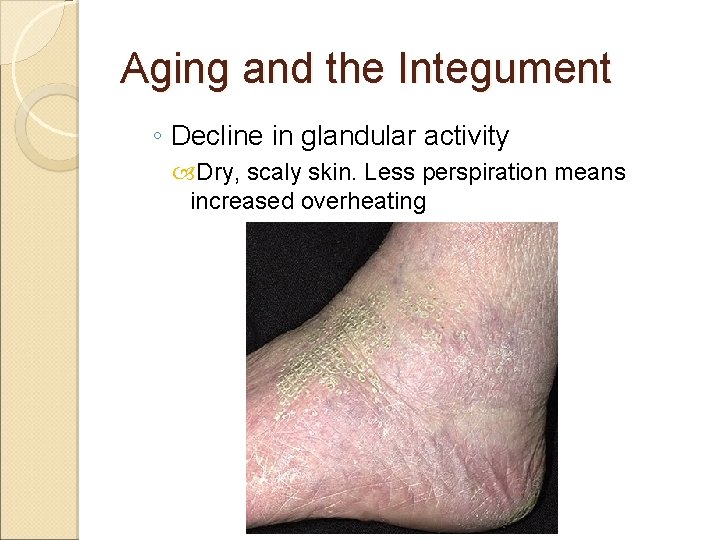
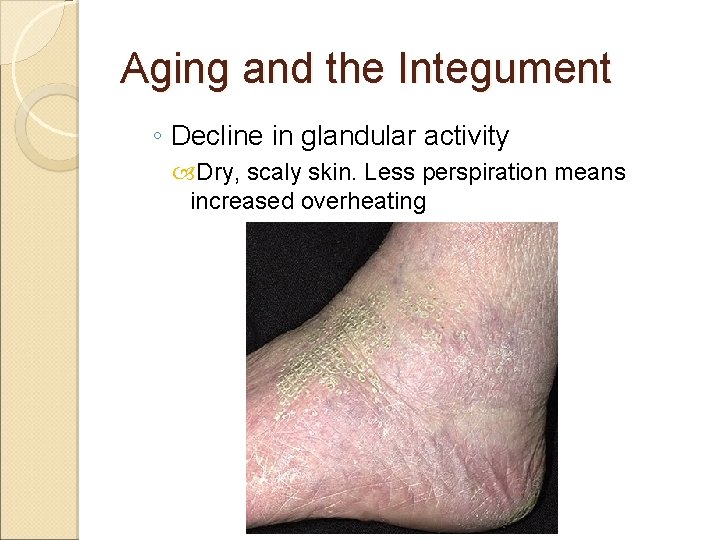
Aging and the Integument ◦ Decline in glandular activity Dry, scaly skin. Less perspiration means increased overheating
Aging and the Integument Effects of aging on the integument ◦ Reduced blood supply to dermis ◦ Hair follicles stop functioning Thinner, finer hair
Aging and the Integument Effects of aging on the integument ◦ Dermis thins Sagging and wrinkling occur
Aging and the Integument Effects of aging on the integument ◦ Decrease in sex hormones Hair characteristics and fat distribution change People of both sexes age 90 -100 tend to look alike

Aging and the Integument Effects of aging on the integument ◦ Skin repairs more slowly Repairs can take twice as long as a young adult Recurring infections may result