Understanding Test Results Cytology Codes management Colposcopy Management
- Slides: 32
Understanding Test Results
Cytology Codes & management Colposcopy- Management of cervical lesions
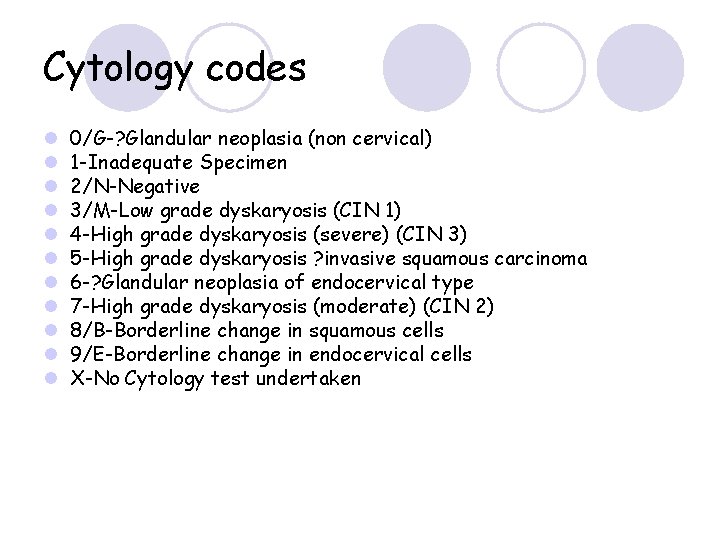
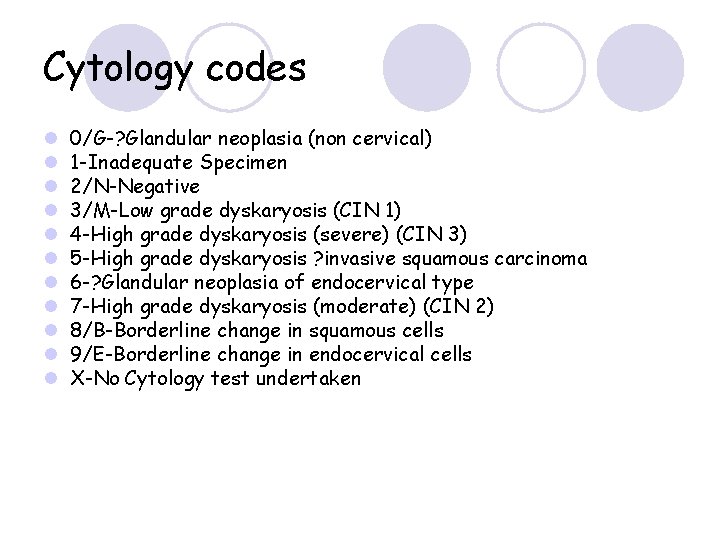
Cytology codes l l l 0/G-? Glandular neoplasia (non cervical) 1 -Inadequate Specimen 2/N-Negative 3/M-Low grade dyskaryosis (CIN 1) 4 -High grade dyskaryosis (severe) (CIN 3) 5 -High grade dyskaryosis ? invasive squamous carcinoma 6 -? Glandular neoplasia of endocervical type 7 -High grade dyskaryosis (moderate) (CIN 2) 8/B-Borderline change in squamous cells 9/E-Borderline change in endocervical cells X-No Cytology test undertaken
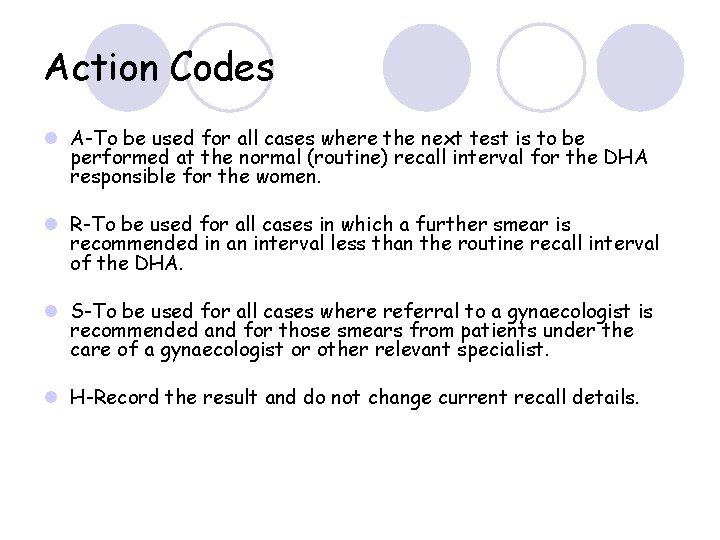
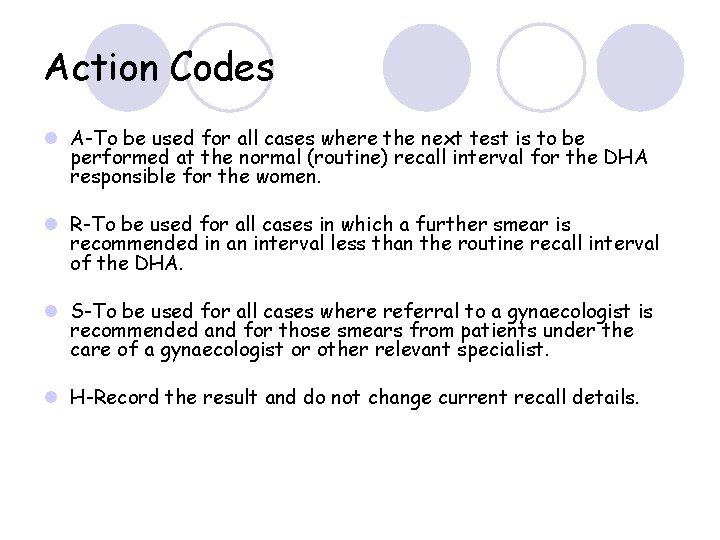
Action Codes l A-To be used for all cases where the next test is to be performed at the normal (routine) recall interval for the DHA responsible for the women. l R-To be used for all cases in which a further smear is recommended in an interval less than the routine recall interval of the DHA. l S-To be used for all cases where referral to a gynaecologist is recommended and for those smears from patients under the care of a gynaecologist or other relevant specialist. l H-Record the result and do not change current recall details.
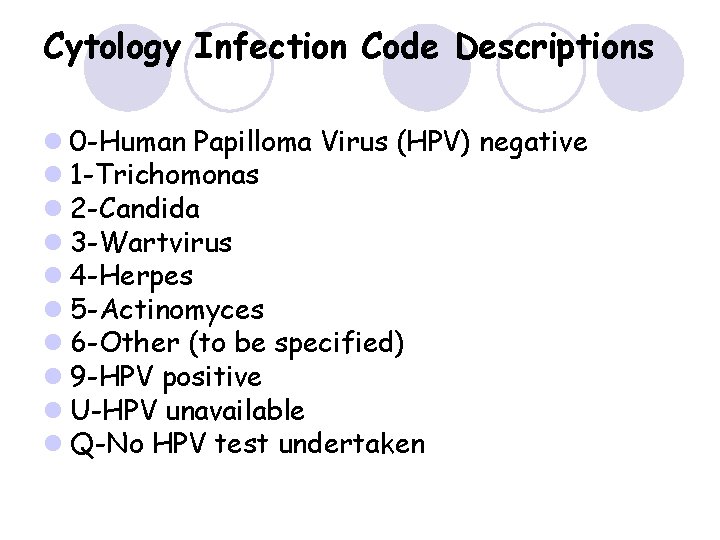
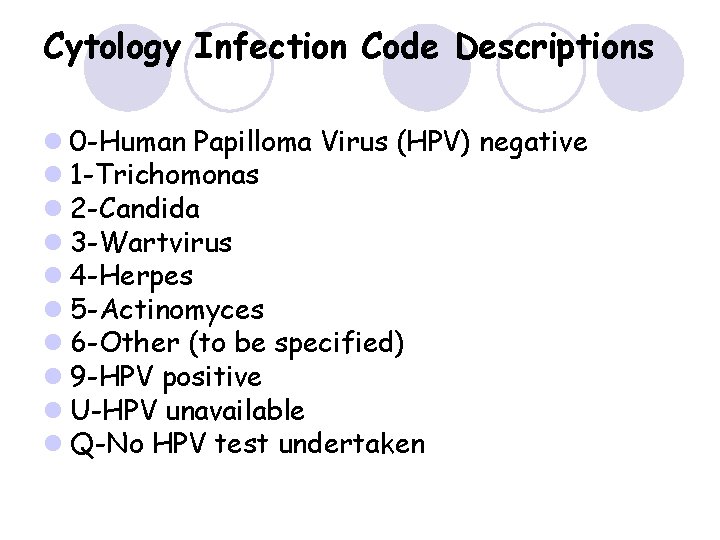
Cytology Infection Code Descriptions l 0 -Human Papilloma Virus (HPV) negative l 1 -Trichomonas l 2 -Candida l 3 -Wartvirus l 4 -Herpes l 5 -Actinomyces l 6 -Other (to be specified) l 9 -HPV positive l U-HPV unavailable l Q-No HPV test undertaken
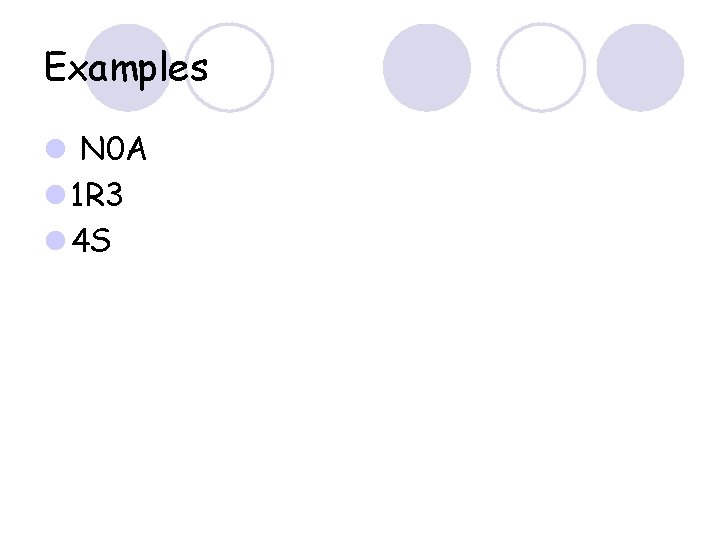
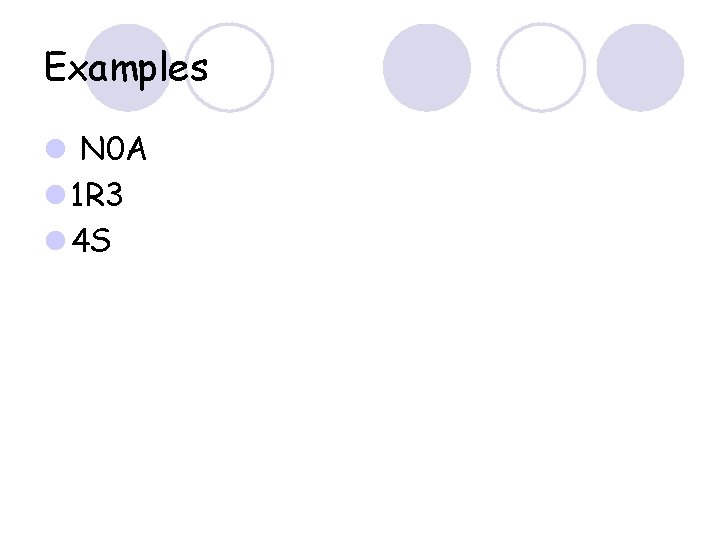
Examples l N 0 A l 1 R 3 l 4 S
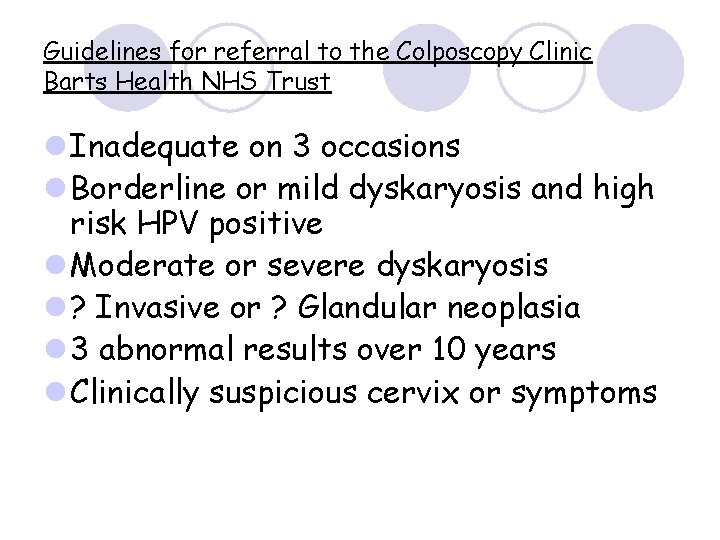
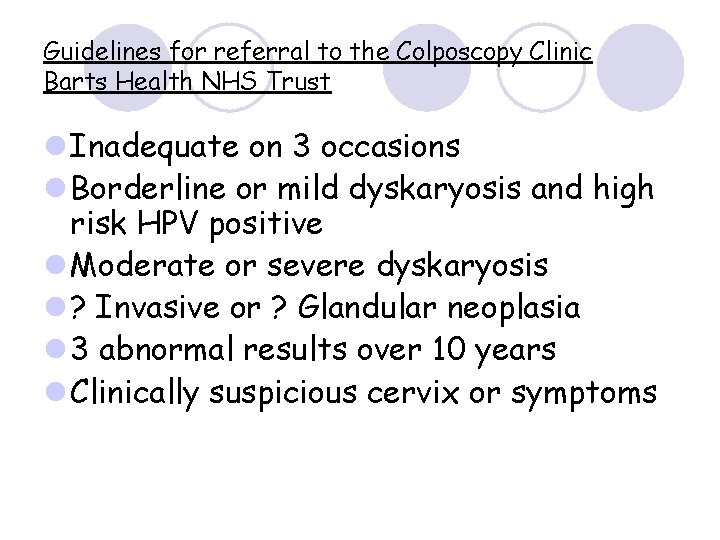
Guidelines for referral to the Colposcopy Clinic Barts Health NHS Trust l Inadequate on 3 occasions l Borderline or mild dyskaryosis and high risk HPV positive l Moderate or severe dyskaryosis l ? Invasive or ? Glandular neoplasia l 3 abnormal results over 10 years l Clinically suspicious cervix or symptoms
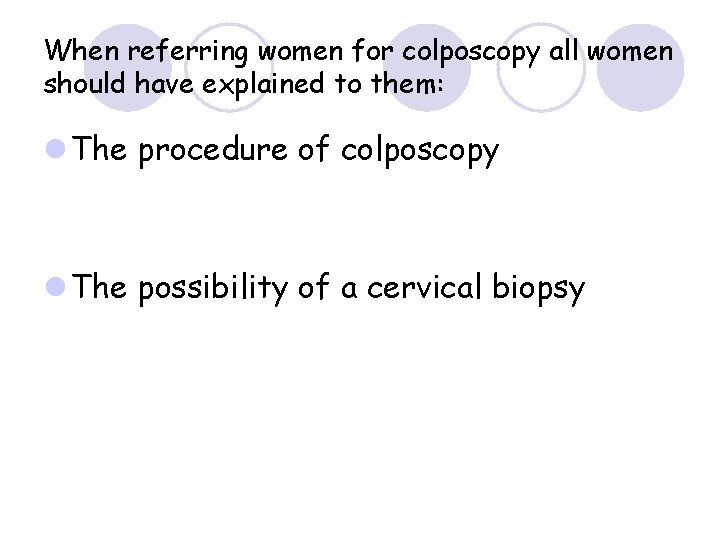
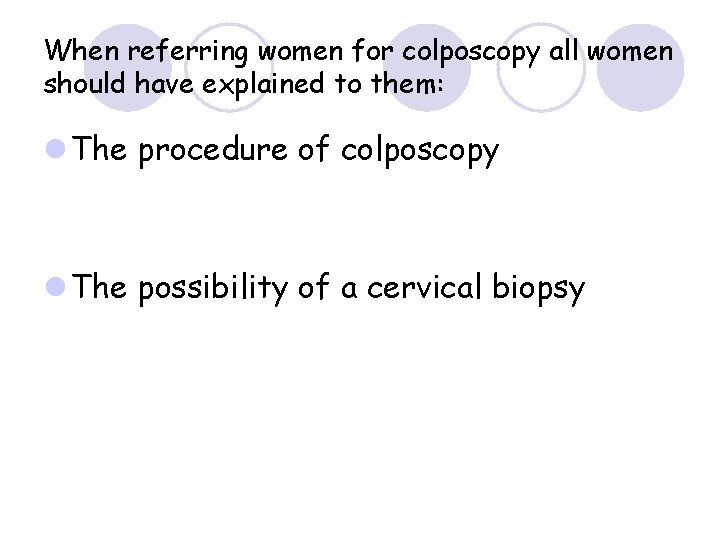
When referring women for colposcopy all women should have explained to them: l The procedure of colposcopy l The possibility of a cervical biopsy
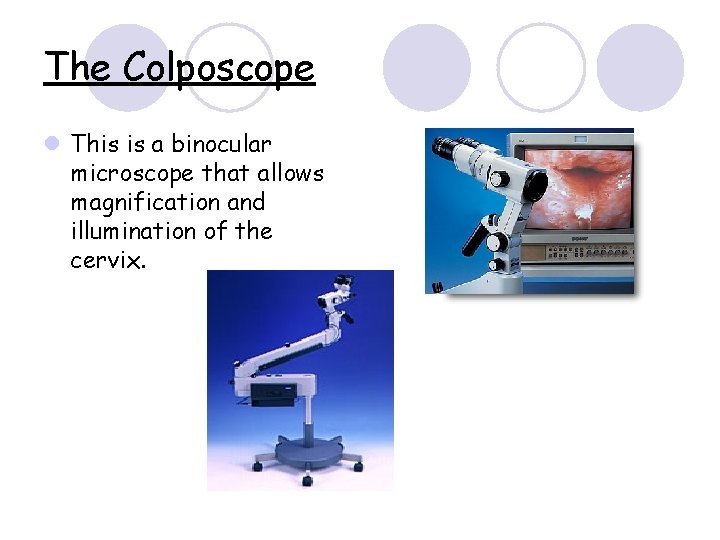
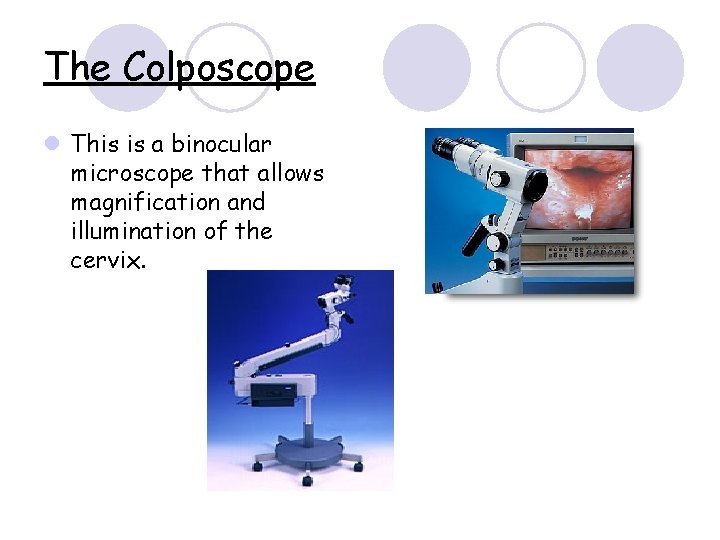
The Colposcope l This is a binocular microscope that allows magnification and illumination of the cervix.
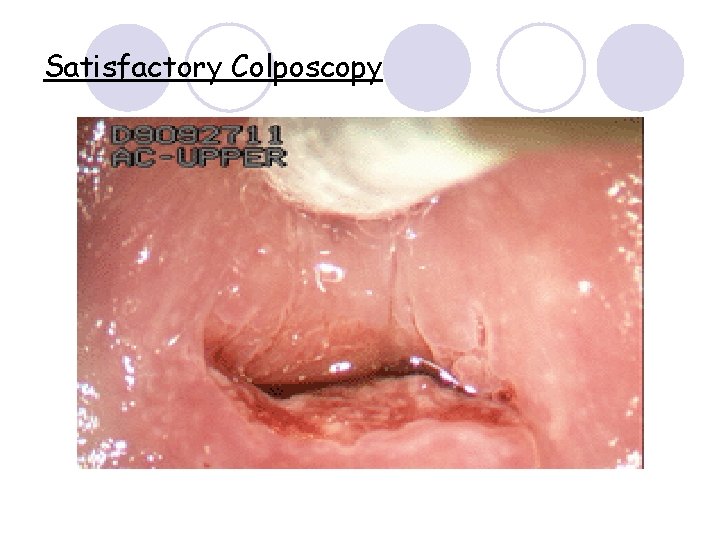
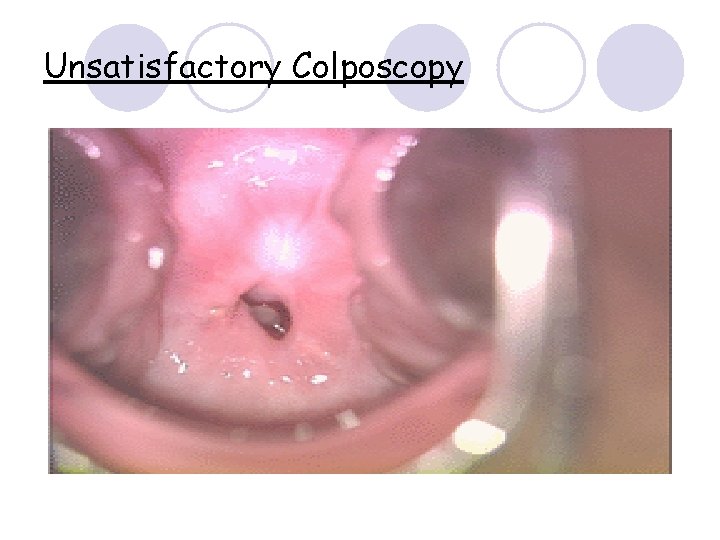
The Colposcopy Examination l Acetic acid 5% is applied. l The abnormality is identified (aceto-white change). l The colposcopic examination is considered satisfactory when the entire transformation zone has been identified, and a colposcopic impression is made. A photograph may be taken for accurate follow up. l One or more biopsies are then taken of the abnormal areas.
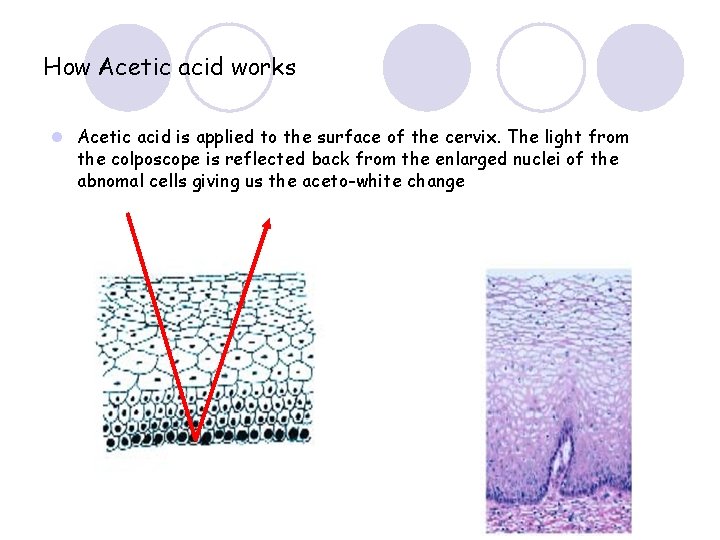
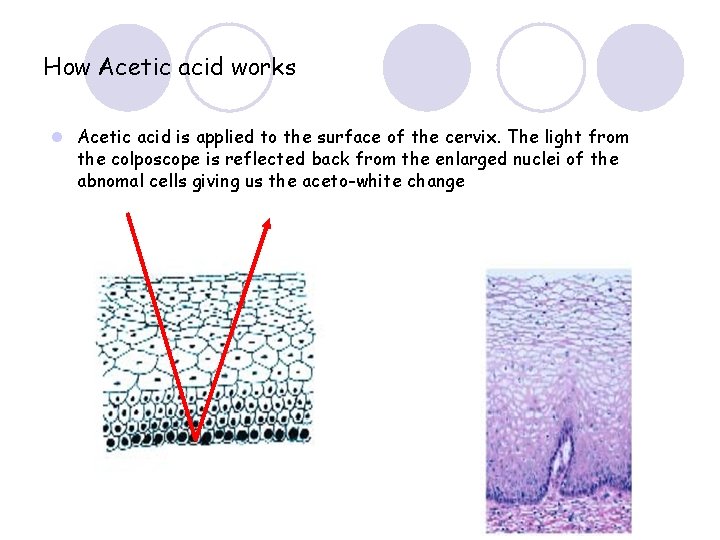
How Acetic acid works l Acetic acid is applied to the surface of the cervix. The light from the colposcope is reflected back from the enlarged nuclei of the abnomal cells giving us the aceto-white change
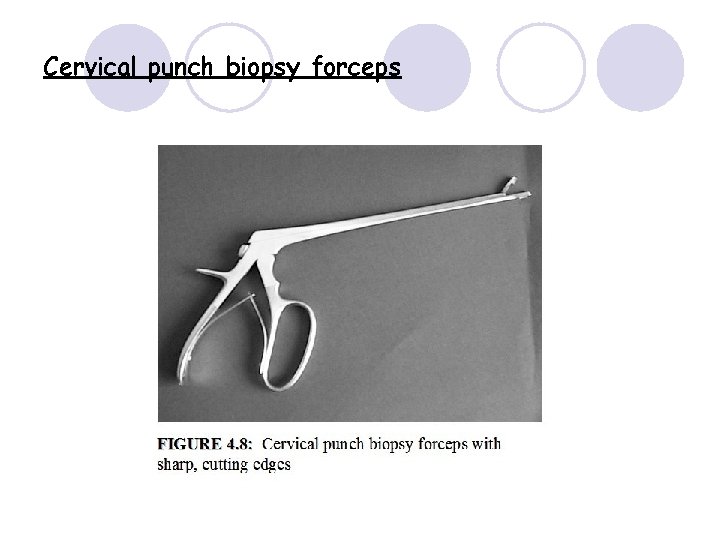
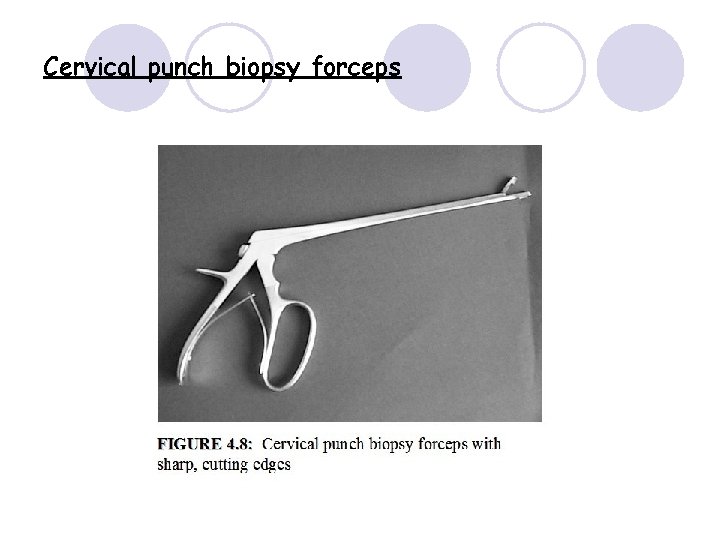
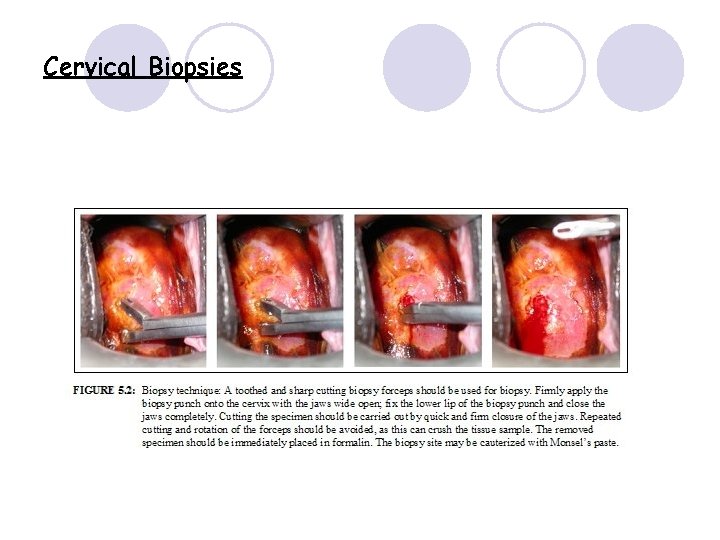
Cervical punch biopsy forceps
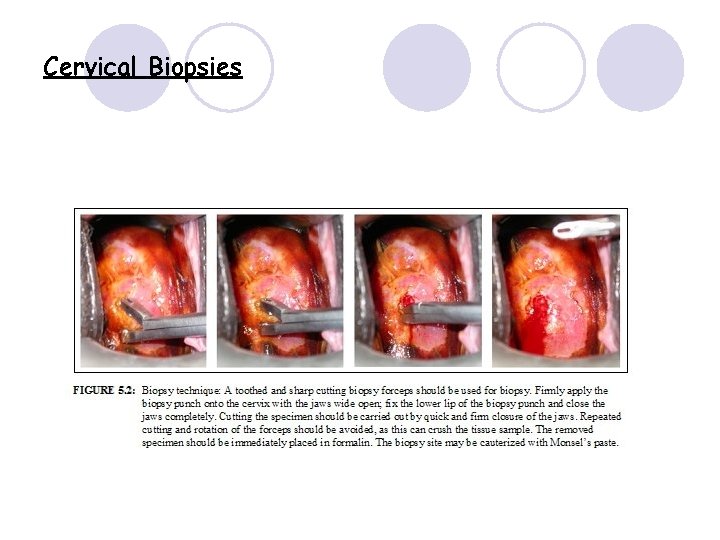
Cervical Biopsies
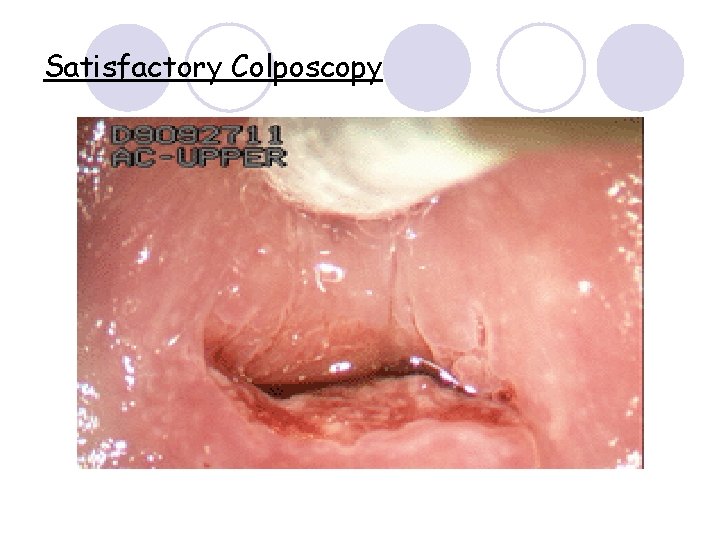
Satisfactory Colposcopy
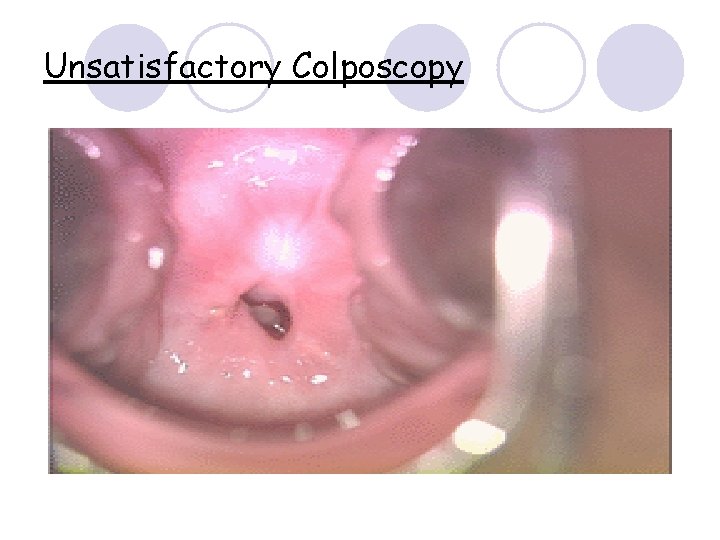
Unsatisfactory Colposcopy
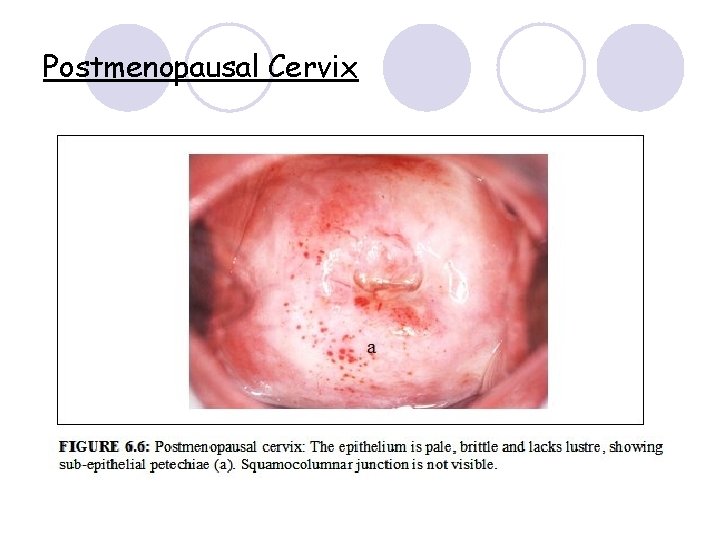
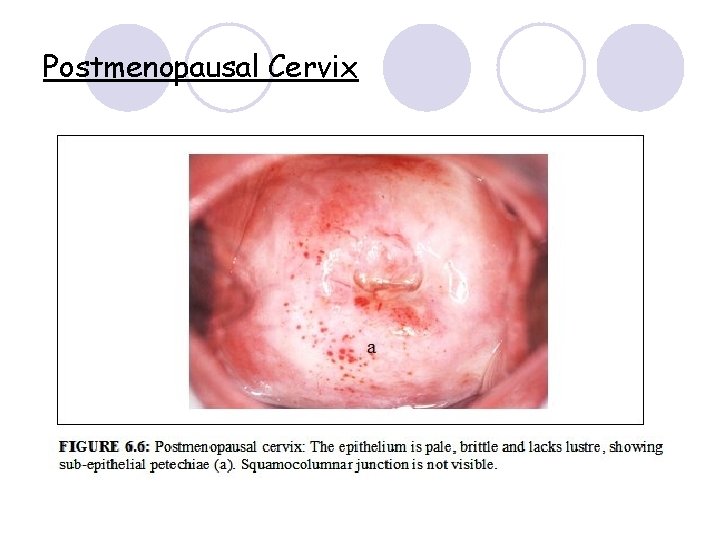
Postmenopausal Cervix
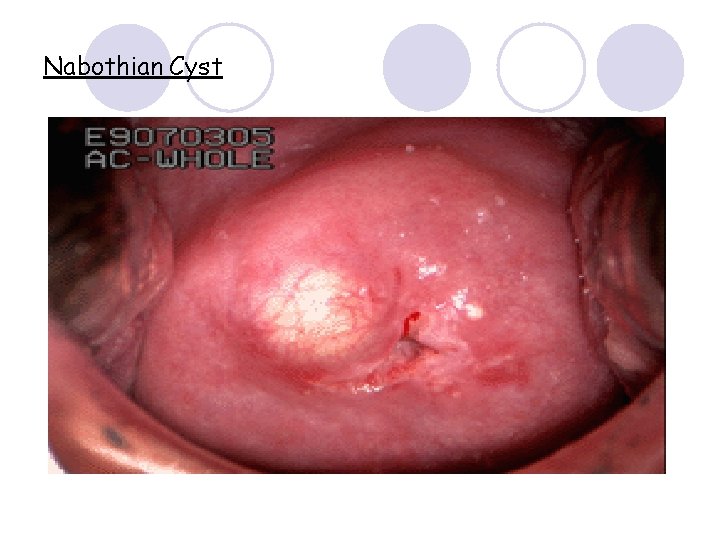
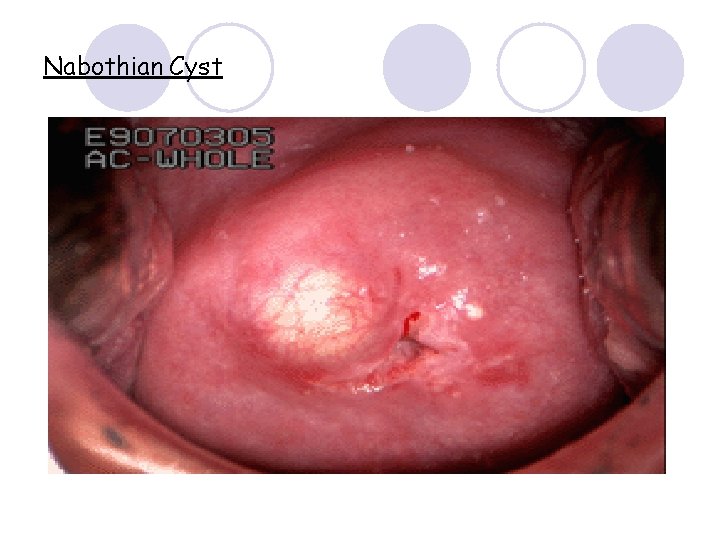
Nabothian Cyst
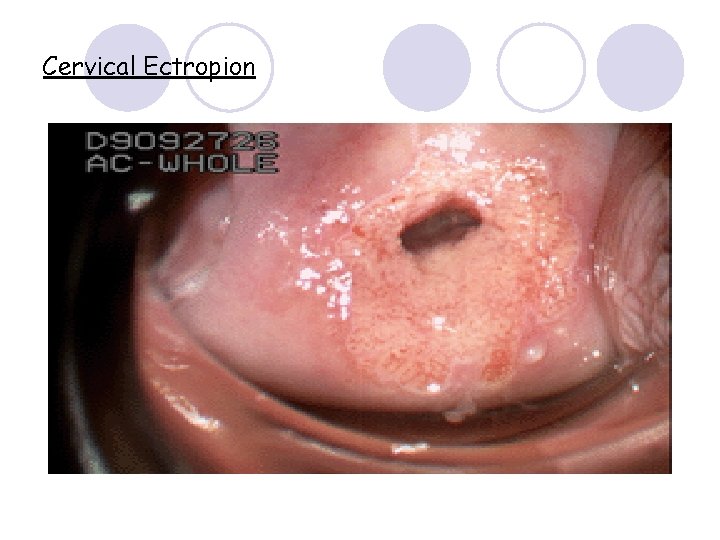
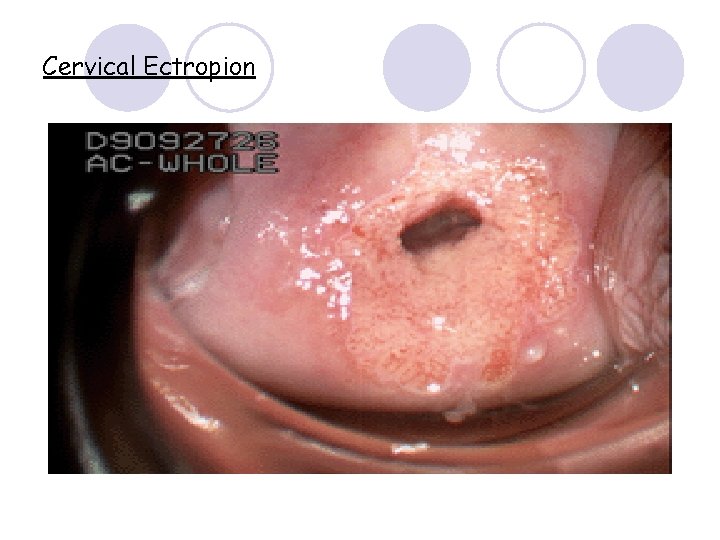
Cervical Ectropion
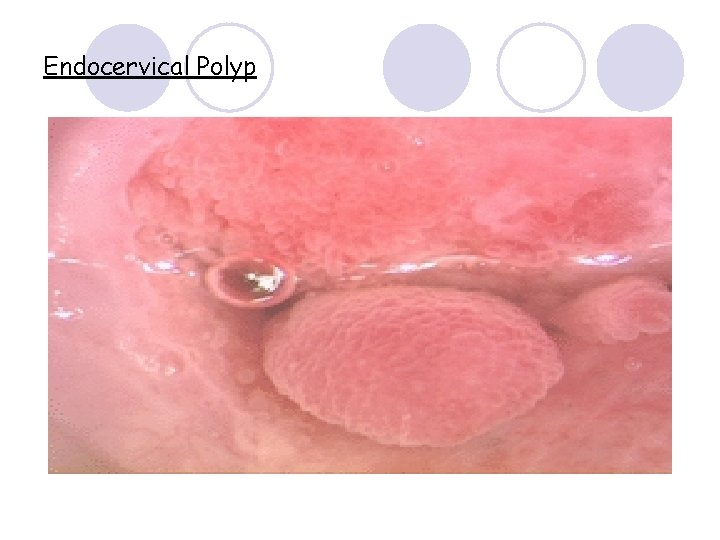
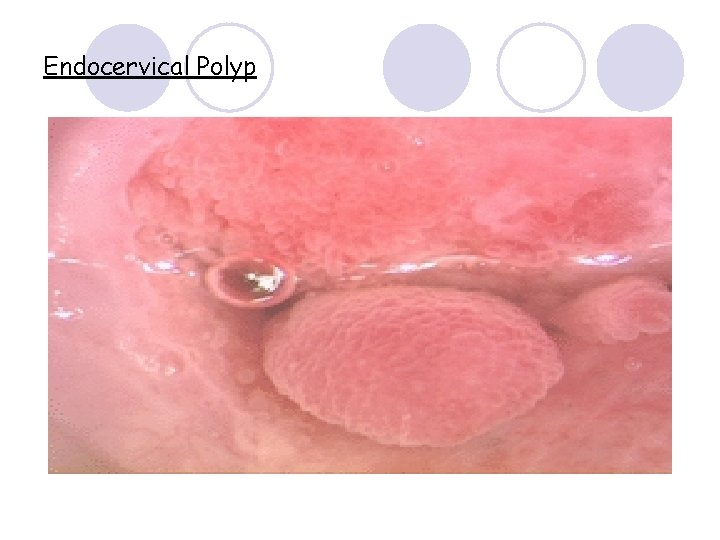
Endocervical Polyp
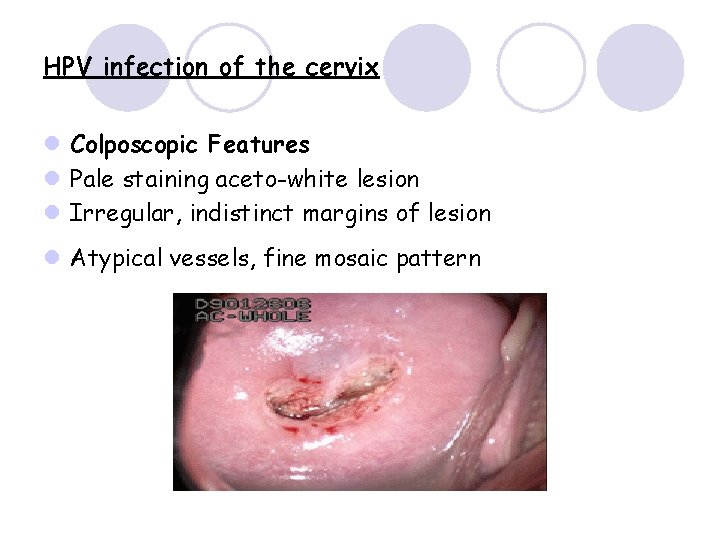
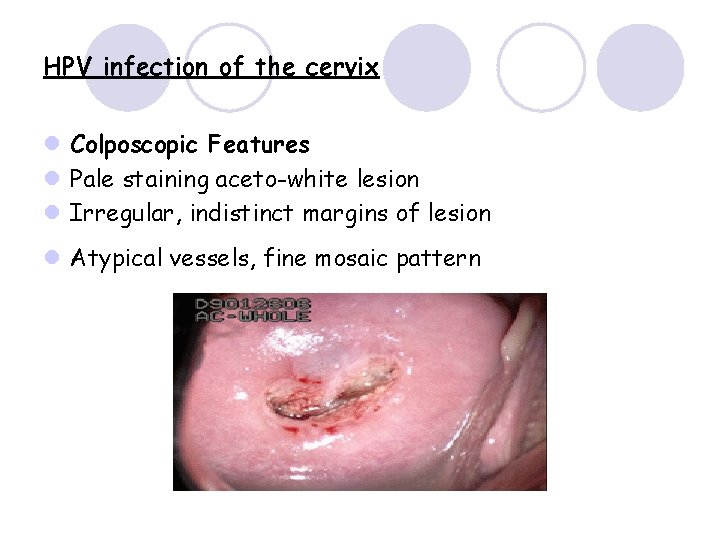
HPV infection of the cervix l Colposcopic Features l Pale staining aceto-white lesion l Irregular, indistinct margins of lesion l Atypical vessels, fine mosaic pattern
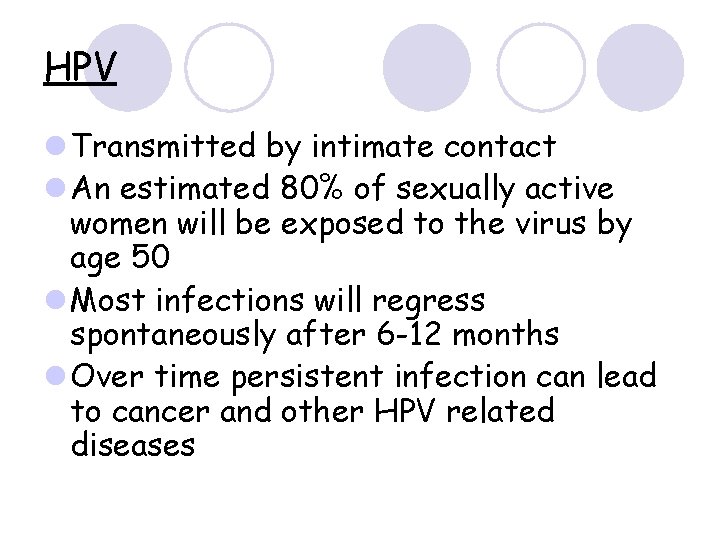
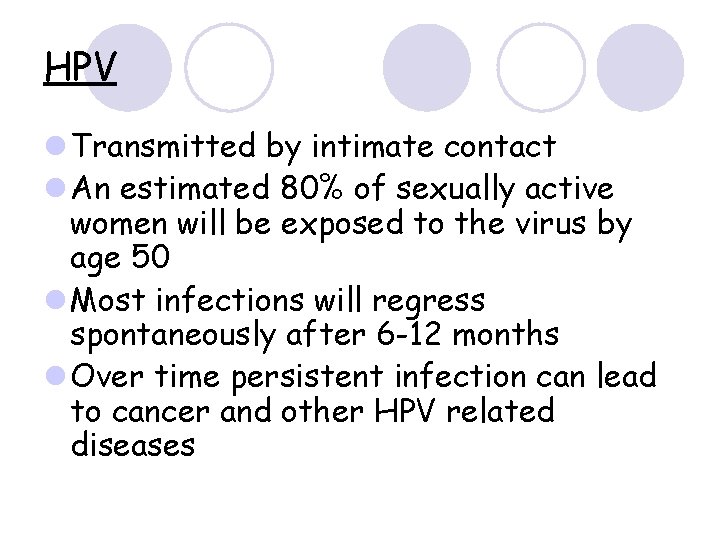
HPV l Transmitted by intimate contact l An estimated 80% of sexually active women will be exposed to the virus by age 50 l Most infections will regress spontaneously after 6 -12 months l Over time persistent infection can lead to cancer and other HPV related diseases
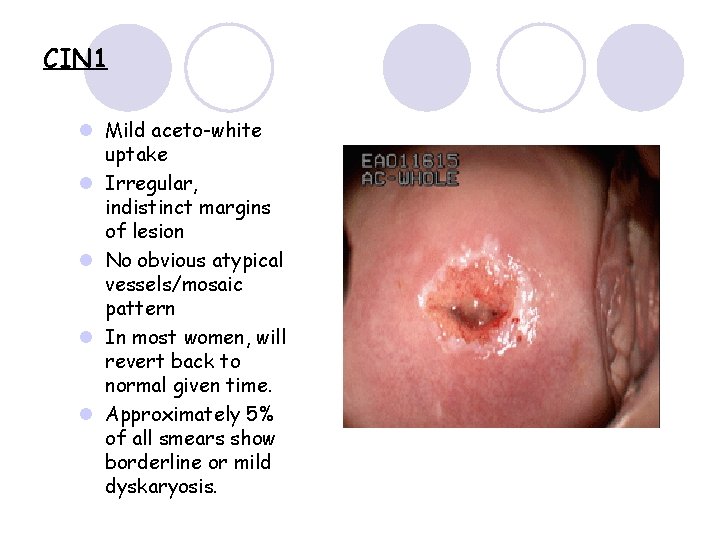
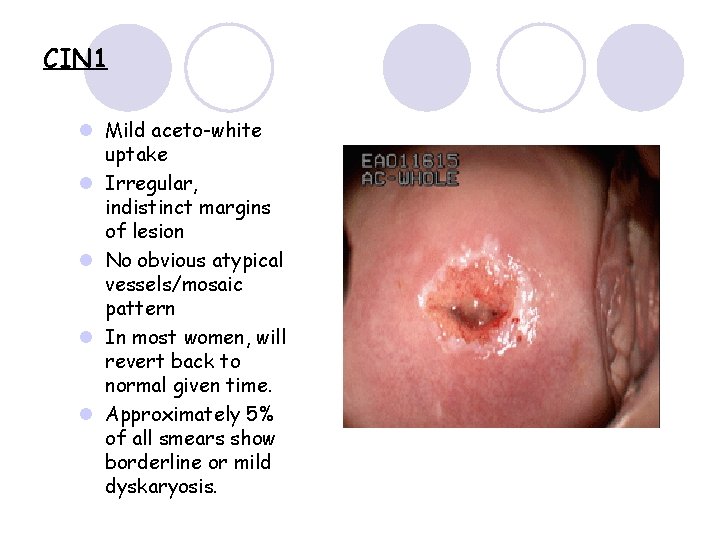
CIN 1 l Mild aceto-white uptake l Irregular, indistinct margins of lesion l No obvious atypical vessels/mosaic pattern l In most women, will revert back to normal given time. l Approximately 5% of all smears show borderline or mild dyskaryosis.
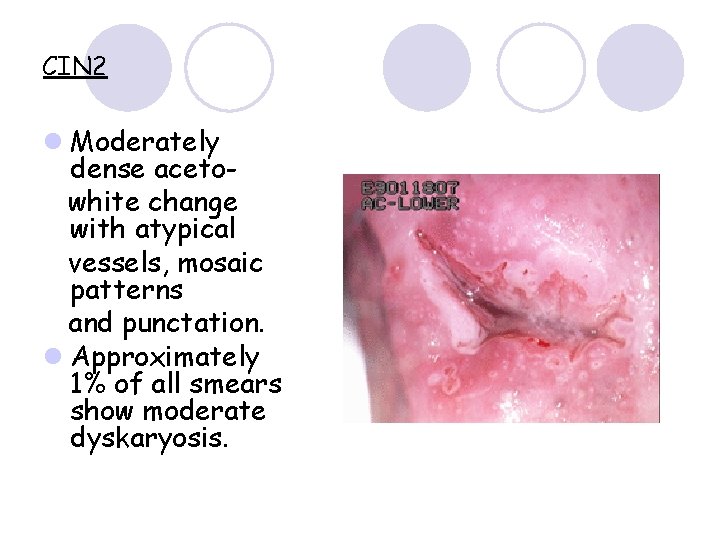
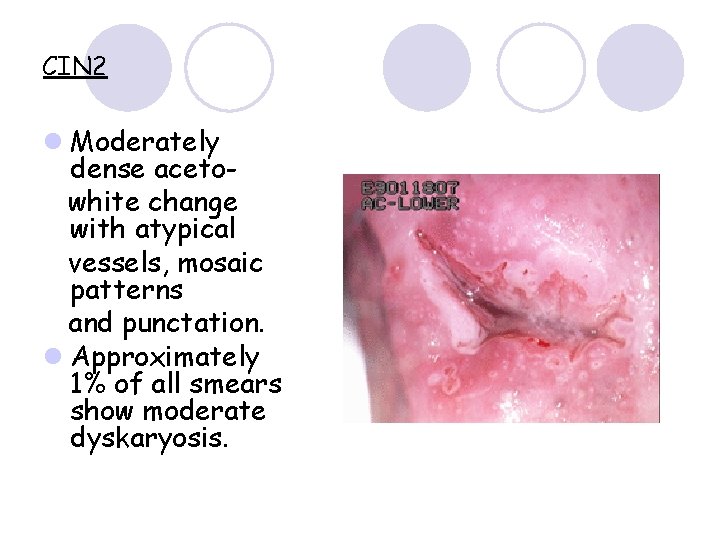
CIN 2 l Moderately dense acetowhite change with atypical vessels, mosaic patterns and punctation. l Approximately 1% of all smears show moderate dyskaryosis.
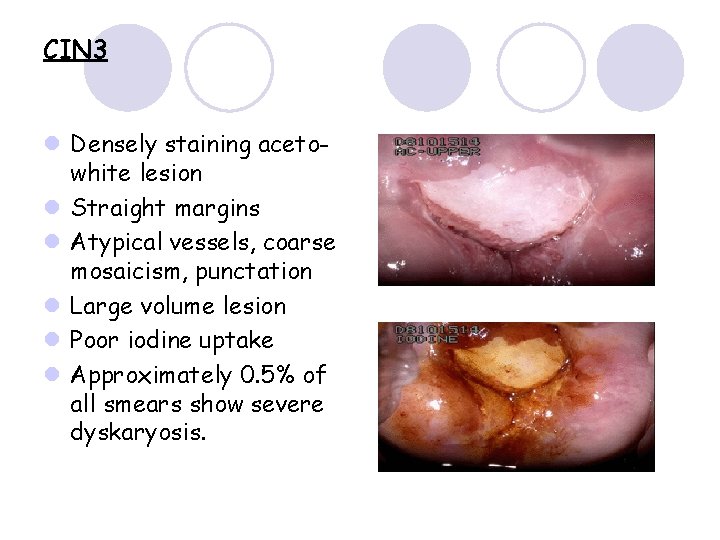
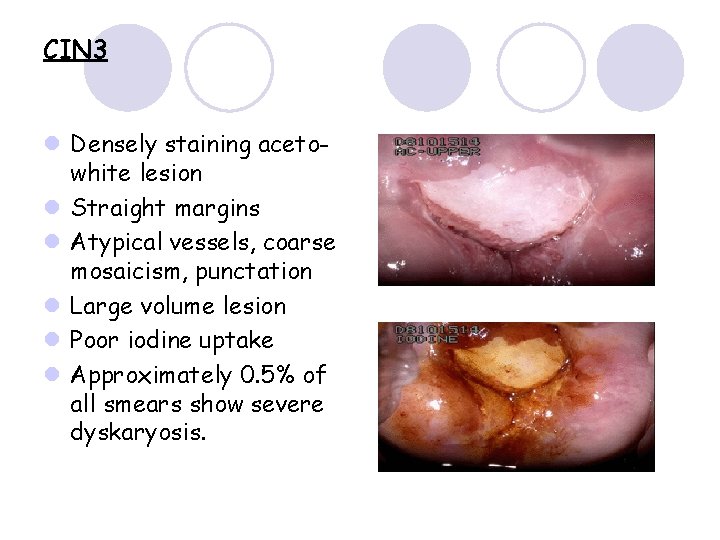
CIN 3 l Densely staining acetowhite lesion l Straight margins l Atypical vessels, coarse mosaicism, punctation l Large volume lesion l Poor iodine uptake l Approximately 0. 5% of all smears show severe dyskaryosis.
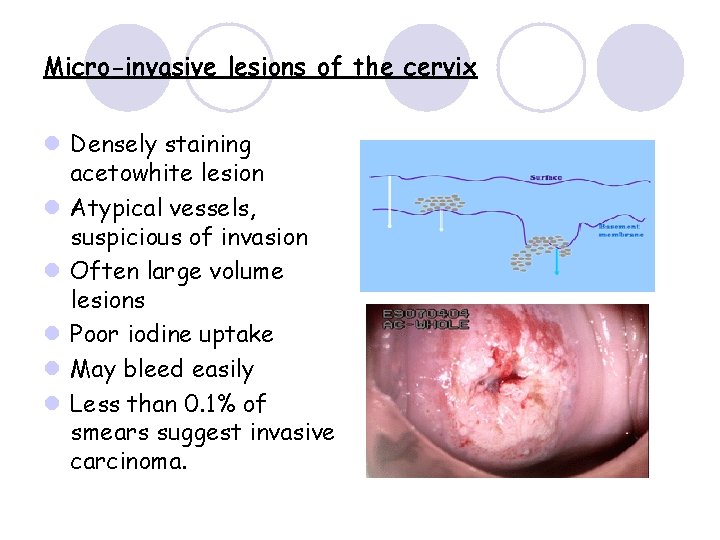
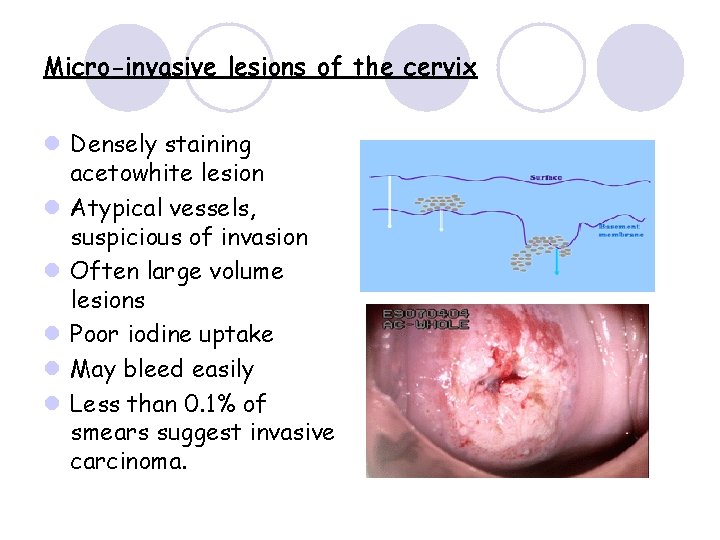
Micro-invasive lesions of the cervix l Densely staining acetowhite lesion l Atypical vessels, suspicious of invasion l Often large volume lesions l Poor iodine uptake l May bleed easily l Less than 0. 1% of smears suggest invasive carcinoma.
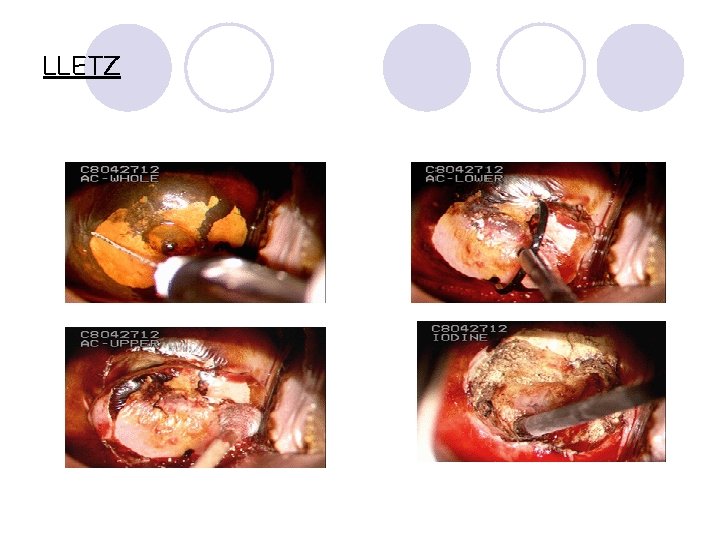
Treatment – LLETZ (Large Loop Excision of the Transformation Zone) l A diathermy pad is placed on the woman’s leg. l Local anaesthesia is injected into the four quadrants of the cervix. An appropriately sized loop is chosen and the abnormal area removed in one piece under colposcopic guidance. Ball diathermy is used to achieve haemostasis. l Facilities are available in the clinic in the event of an emergency situation. l Follow up information is reinforced before the woman leaves the clinic.
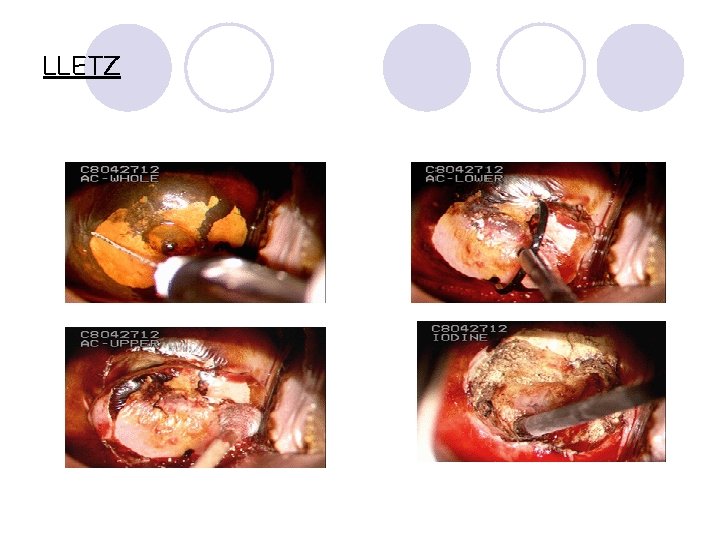
LLETZ
What are the complications? 1. 2. 3. 4. Treatment for CIN is generally very safe. Very few complications exist but some important problems can occur. Bleeding. Infection. Cervical stenosis’ and ‘cervical incompetence’ Premature rupture of membranes during pregnancy leading to early delivery Women are advised not to insert ANYTHING into the vagina for at least 4 weeks.
What is the success rate? l Ninety five percent of women have a negative smear 6 months following their first treatment.
Follow-up l A follow-up check after treatment for precancerous changes is absolutely essential. l We perform Liquid Based Cytology and HPV testing six months after treatment. l If residual precancerous cells are left behind, further Colposcopy and biopsy is performed, and a repeat LLETZ procedure, will be arranged if necessary.
Changes to practice l HPV testing - TRIAGE Given that cervical cancer will not develop without HPV, women with borderline changes or mild dyskaryosis who have a negative high risk HPV test are not likely to need treatment and should be able to safely return to routine screening. - TEST OF CURE It has now been clearly established that the successful removal of abnormal cervical cells usually also leads to the disappearance of the HPV within 12 months or so.
Further Information l www. bsccp. org. uk l www. jotrust. co. uk l www. patient. co. uk l www. cancerscreening. nhs. uk l www. londonqarc. nhs. uk