Understanding Pain and Early Management Strategies MSK Physiotherapy

- Slides: 40
Understanding Pain and Early Management Strategies MSK Physiotherapy Support Worker Development Group Emma Tocher May 2018 Review date May 2020
Aims of Session • • What is pain Types of pain: Acute vs Chronic How might patients describe their pain How and when to record pain What factors influence pain Medications Pain Management Strategies
What is pain? Pain is an unpleasant sensory or emotional experience associated with actual or potential tissue damage, or described in terms of such damage (IASP 1994).
What is pain? Pain is an unpleasant sensory or emotional experience associated with actual or potential tissue damage, or described in terms of such damage (IASP 1994).
Types of pain? • Nociceptive – Peripherally activated as a result of peripheral tissue damage or dysfunction (Klein 2005). • Neuropathic – pain arising as a direct consequence of a lesion or disease affecting the somatosensory system (Jensen et al 2011).
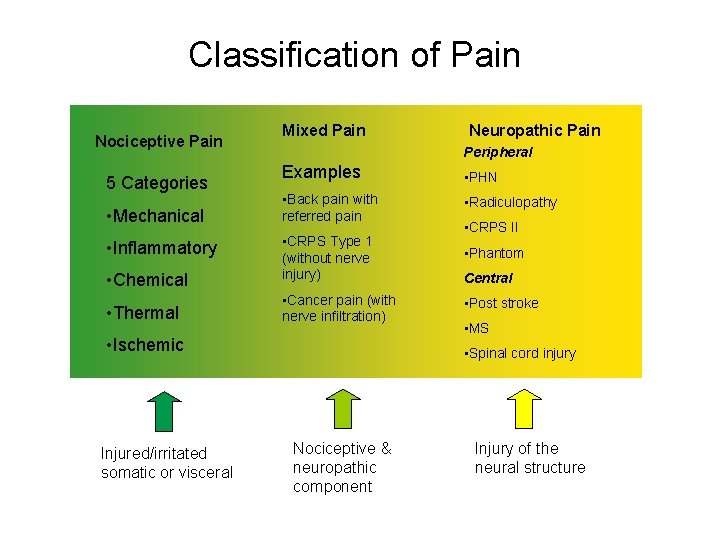
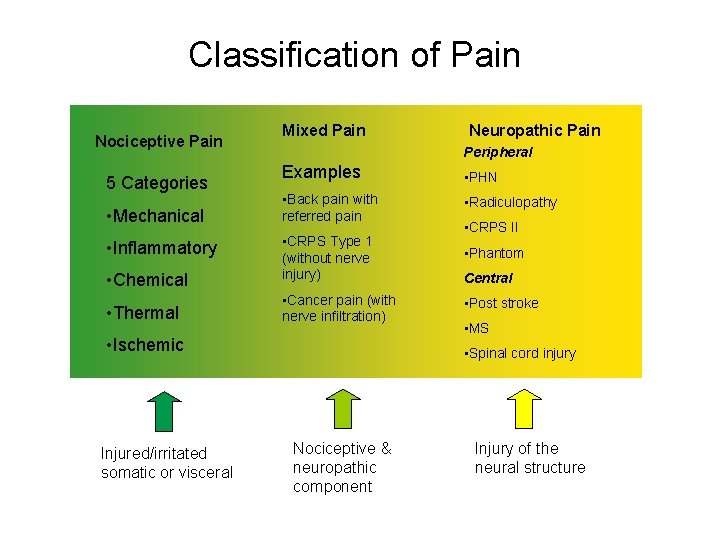
Classification of Pain Nociceptive Pain 5 Categories • Mechanical • Inflammatory • Chemical • Thermal Mixed Pain Peripheral Examples • PHN • Back pain with referred pain • Radiculopathy • CRPS Type 1 (without nerve injury) • Phantom • Cancer pain (with nerve infiltration) • Ischemic Injured/irritated somatic or visceral Neuropathic Pain • CRPS II Central • Post stroke • MS • Spinal cord injury Nociceptive & neuropathic component Injury of the neural structure
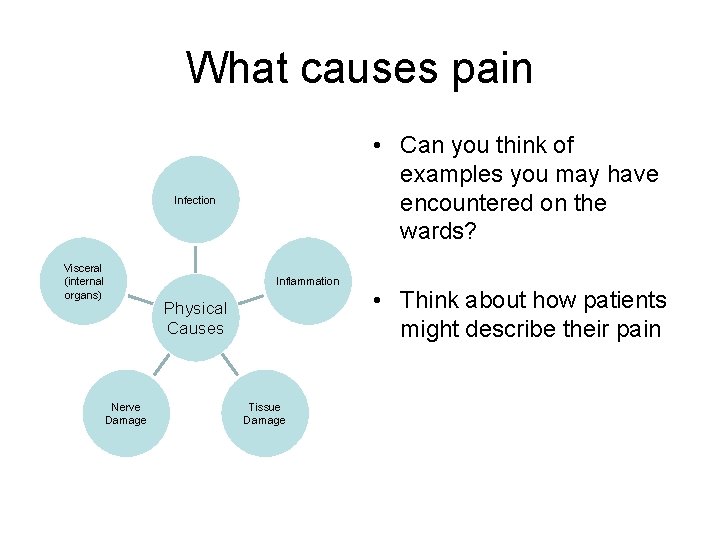
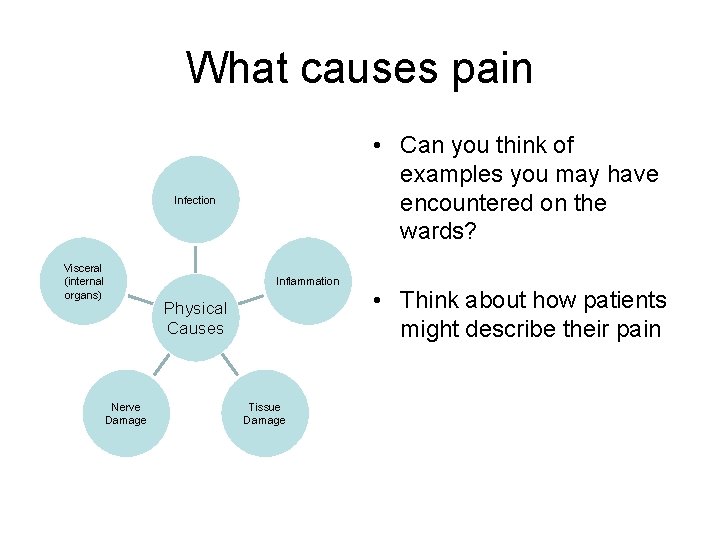
What causes pain • Can you think of examples you may have encountered on the wards? Infection Visceral (internal organs) Inflammation Physical Causes Nerve Damage Tissue Damage • Think about how patients might describe their pain
How do patients describe pain • • Aching Throbbing Burning Numbness Shooting Pins and needles Other examples?
“ Pain is whatever the experiencing person says it is, existing when he says it does” (Mc. Caffery, 1968)
Does everyone have the same perception of pain? Think… • Day 1 post-op TKJR in orthopaedics • Day 1 post-op Cholecystectomy in surgical • DME ward – OA changes in lumbar spine • ACL repair in Day Surgery • Day Hospital- Osteporosis- repeated falls • Amputee patient- phantom limb pain • Stroke patient- shoulder pain …Everyone is different
Acute Pain • Recent • Tissue damage occurring or likely to occur • Protection • Inflammation- chemicals in the area to promote healing sensitise nerve endings
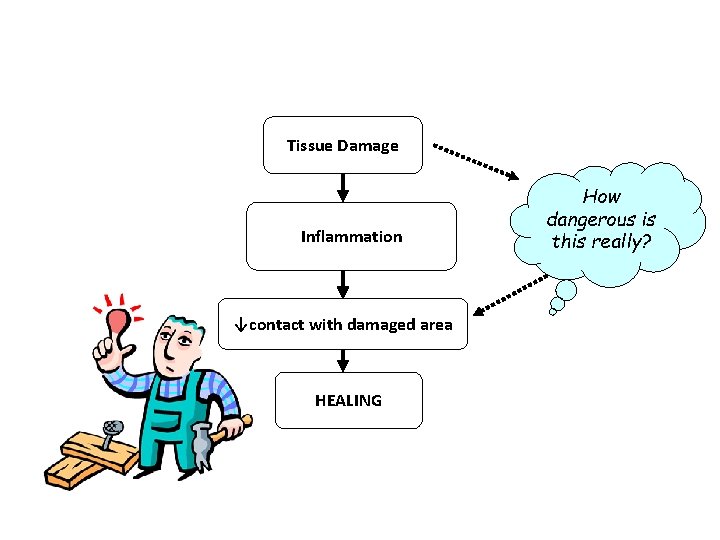
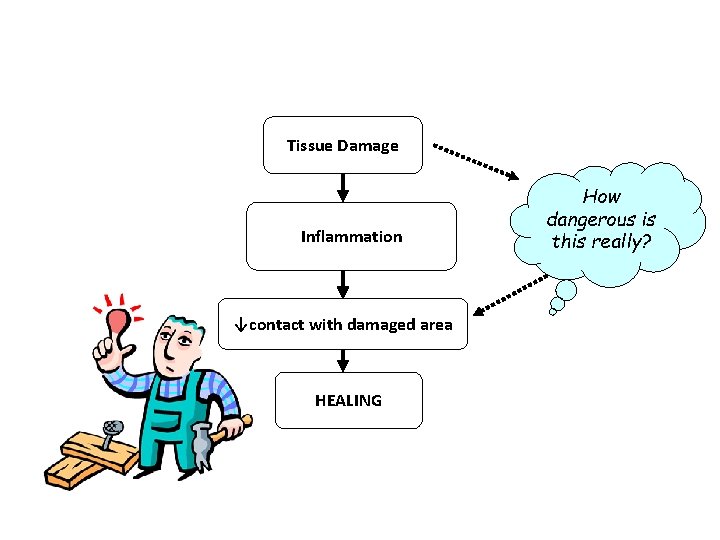
Tissue Damage Inflammation ↓contact with damaged area HEALING How dangerous is this really?
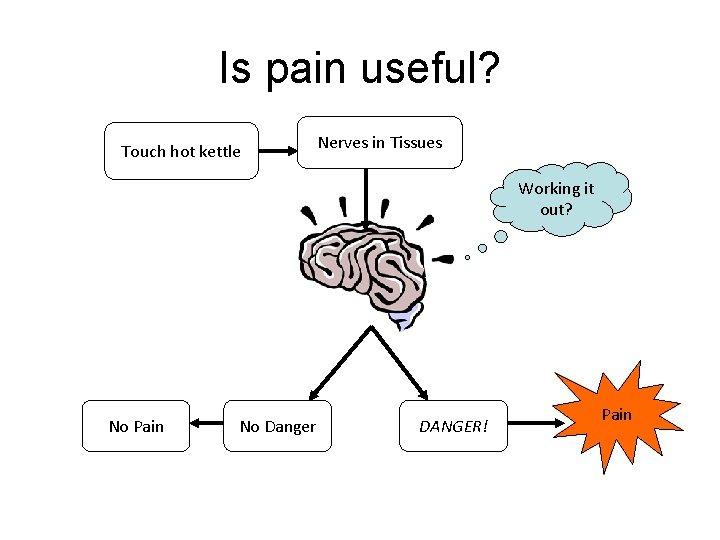
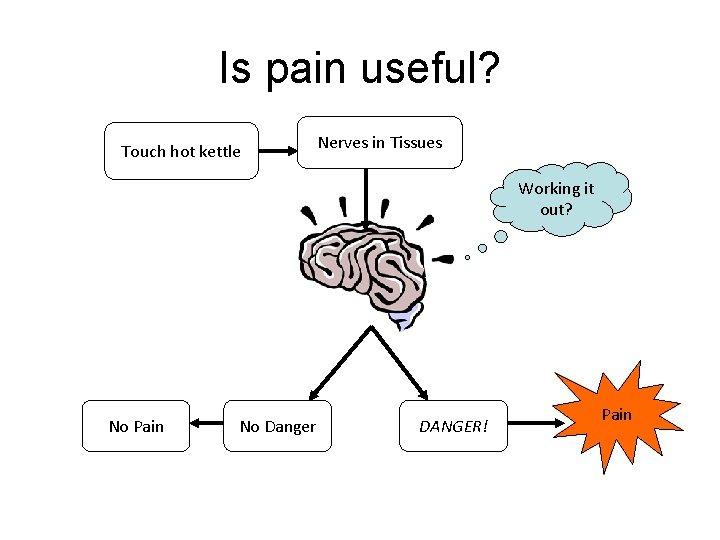
Is pain useful? Touch hot kettle Nerves in Tissues Working it out? No Pain No Danger DANGER! Pain
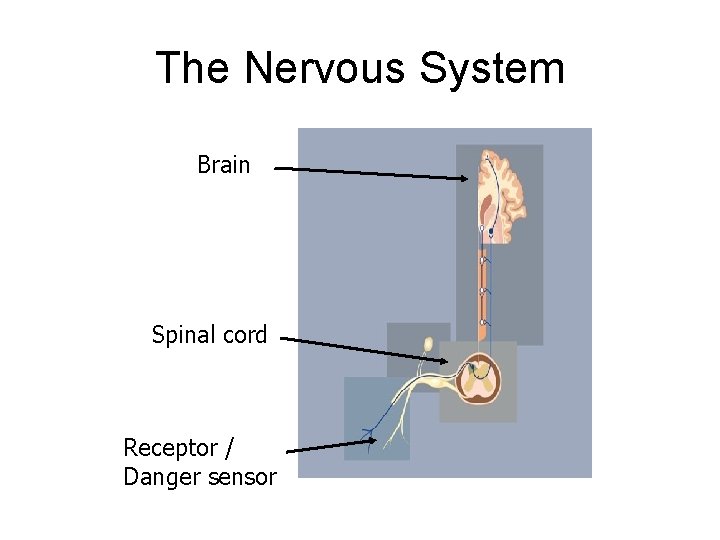
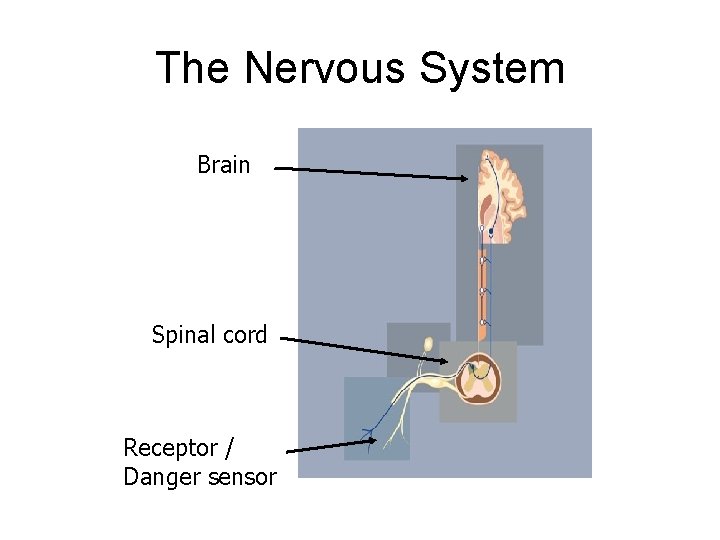
The Nervous System Brain Spinal cord Receptor / Danger sensor
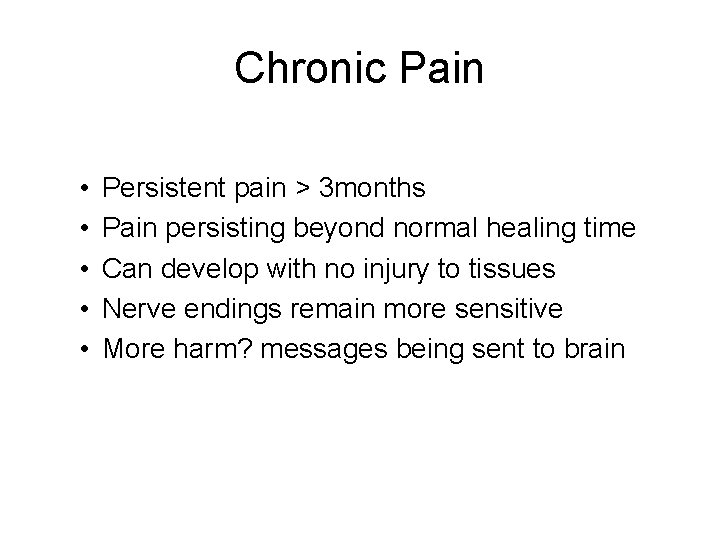
Chronic Pain • • • Persistent pain > 3 months Pain persisting beyond normal healing time Can develop with no injury to tissues Nerve endings remain more sensitive More harm? messages being sent to brain
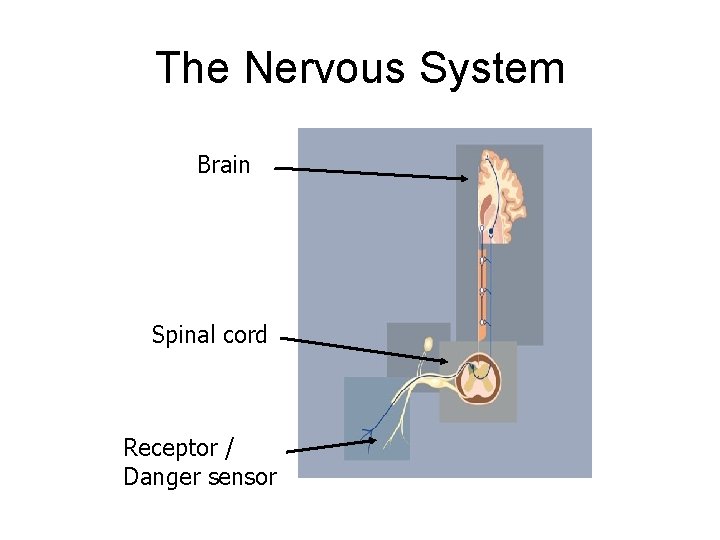
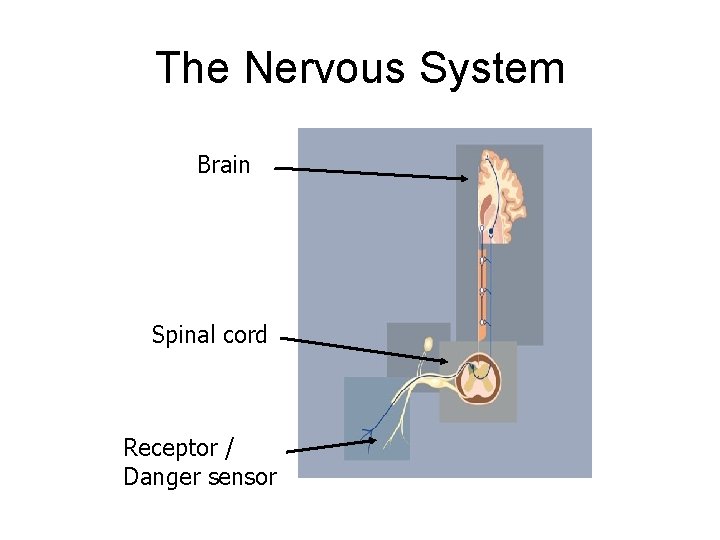
The Nervous System Brain Spinal cord Receptor / Danger sensor

Alarm on high alert!
Allodynia • Pain resulting from stimulation that is normally innocuous, for example light touch or mild temperature changes
Hyperalgesia • An increased response to a stimulus that is normally painful.
Thinking about the questions you ask… • Does your pain feel like strange, unpleasant sensations in your skin? • Does your pain make the affected skin abnormally sensitive to touch? • Does your pain come on suddenly and in bursts for no apparent reason when you’re still? The Lanss Pain Scale
Understanding Pain • https: //www. youtube. com/watch? v=RWMK ucuej. Is
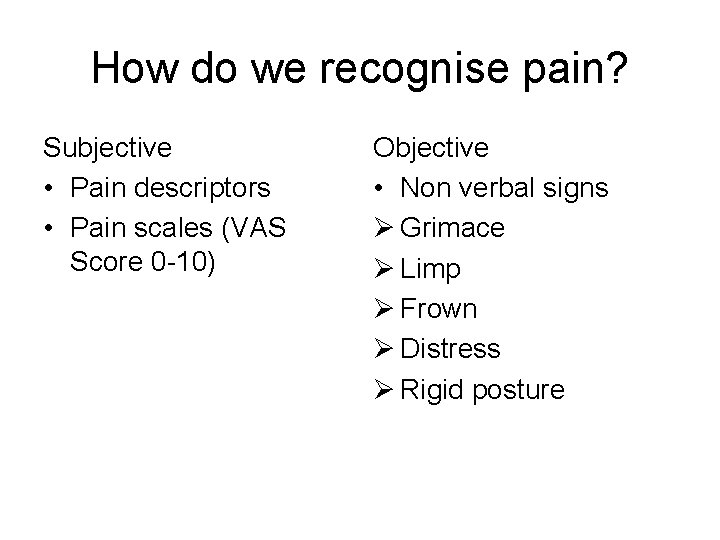
How do we recognise pain? Subjective • Pain descriptors • Pain scales (VAS Score 0 -10) Objective • Non verbal signs Ø Grimace Ø Limp Ø Frown Ø Distress Ø Rigid posture
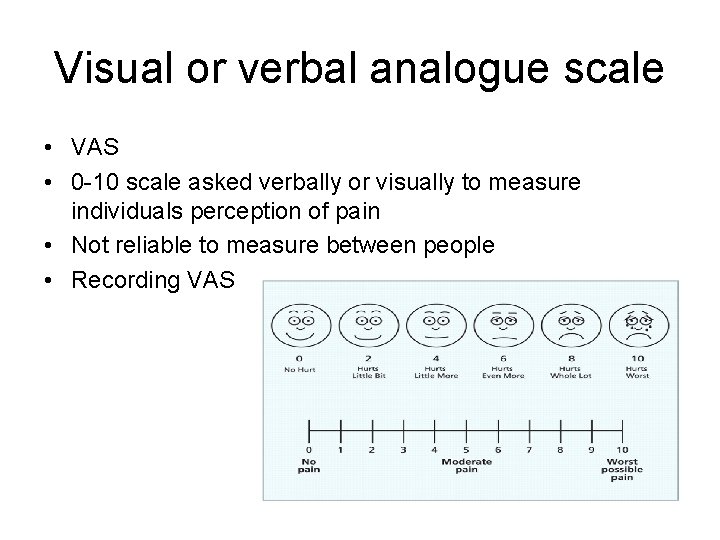
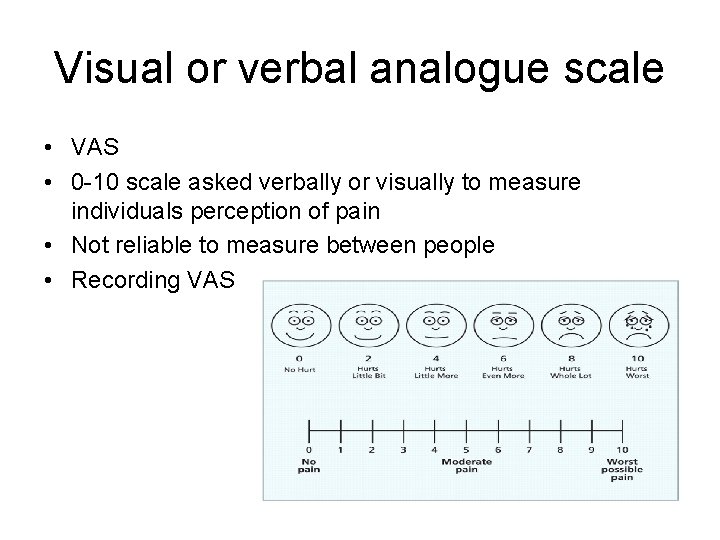
Visual or verbal analogue scale • VAS • 0 -10 scale asked verbally or visually to measure individuals perception of pain • Not reliable to measure between people • Recording VAS
Factors that can affect pain Sensations from the body Experiences of pain Work Emotions Interests Stress Family Activity levels Understanding of your pain Conflicting information from health professionals
Questions to consider • What are your clinical concerns? • What could be contributing factors to the patients pain? • What action/plan would you take? • How would you measure and document the patients pain?
Scenarios A 65 yr old gentleman was referred following a TKJR and you are asked to work on strength and ROM 3/52 post op. He is mobile with his walking sticks. Today he declines to mobilise as he feels he is “too sore” and reports he doesn’t feel people are taking his pain seriously.
Scenarios A 84 yr old gentleman is in your gym rehab class following a fall at home causing a vertebral crush fracture due to osteoporosis. He has widespread OA changes in his lumbar spine and reports he has had “pain in his back for years”.
The humble chickpea…. . What did the sick chickpea say to the doctor? I Falafel
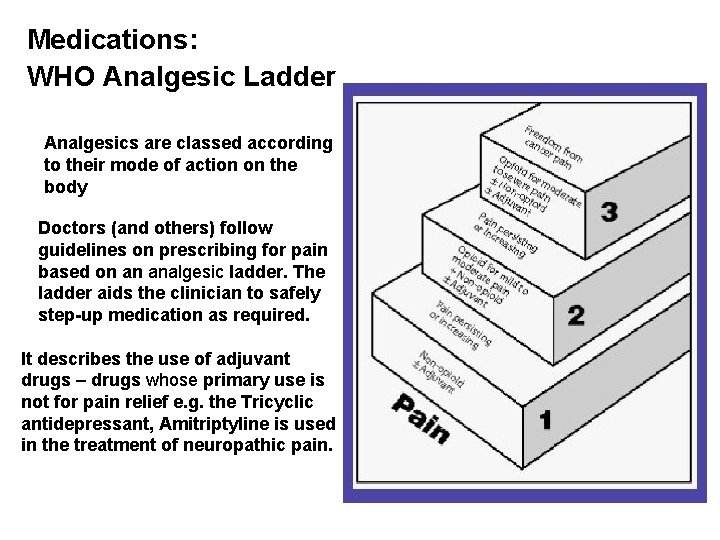
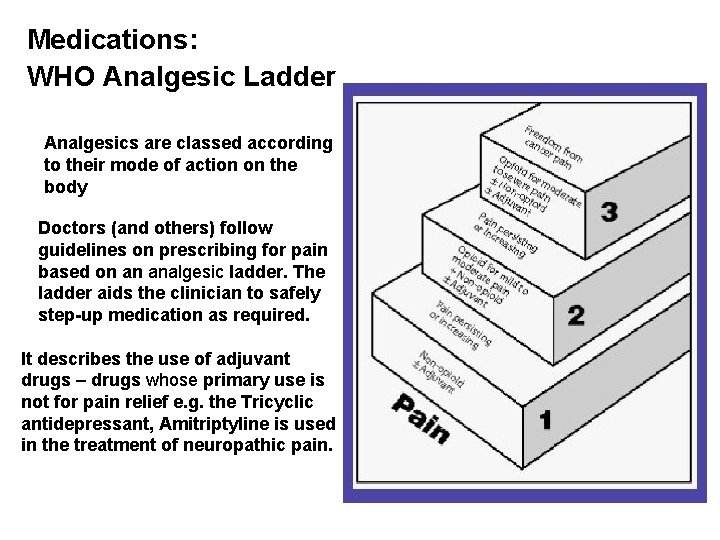
Medications: WHO Analgesic Ladder Analgesics are classed according to their mode of action on the body Doctors (and others) follow guidelines on prescribing for pain based on an analgesic ladder. The. ladder aids the clinician to safely step-up medication as required. It describes the use of adjuvant drugs – drugs whose primary use is not for pain relief e. g. the Tricyclic antidepressant, Amitriptyline is used in the treatment of neuropathic pain.
Types of Pain Medication: • • • Non-steroidal anti-inflammatory drugs (NSAIDS) Steroids Paracetamol Compound Analgesic Preparations Opioids Tricyclic Antidepressants Anticonvulsants Capsaicin Cream Antiarrhythmics/Local Anaesthetics Neuronal Blocks
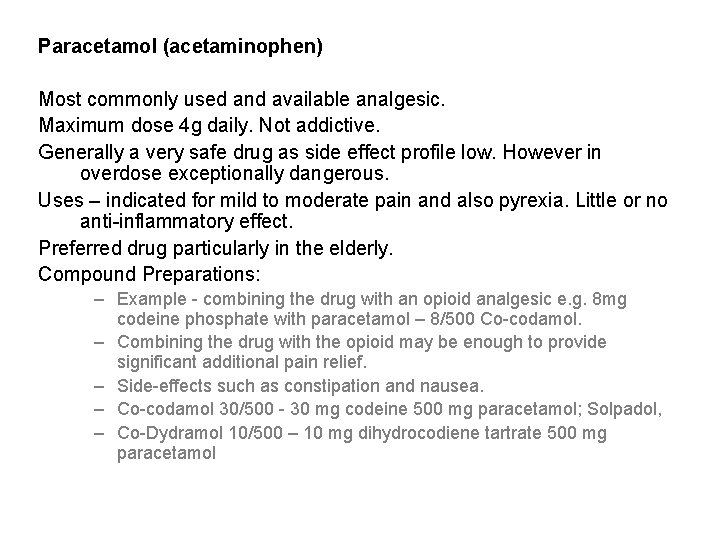
Paracetamol (acetaminophen) Most commonly used and available analgesic. Maximum dose 4 g daily. Not addictive. Generally a very safe drug as side effect profile low. However in overdose exceptionally dangerous. Uses – indicated for mild to moderate pain and also pyrexia. Little or no anti-inflammatory effect. Preferred drug particularly in the elderly. Compound Preparations: – Example - combining the drug with an opioid analgesic e. g. 8 mg codeine phosphate with paracetamol – 8/500 Co-codamol. – Combining the drug with the opioid may be enough to provide significant additional pain relief. – Side-effects such as constipation and nausea. – Co-codamol 30/500 - 30 mg codeine 500 mg paracetamol; Solpadol, – Co-Dydramol 10/500 – 10 mg dihydrocodiene tartrate 500 mg paracetamol
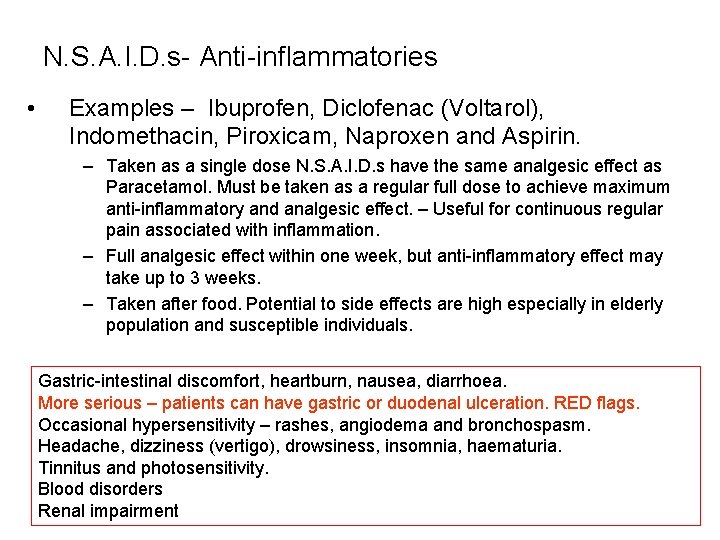
N. S. A. I. D. s- Anti-inflammatories • Examples – Ibuprofen, Diclofenac (Voltarol), Indomethacin, Piroxicam, Naproxen and Aspirin. – Taken as a single dose N. S. A. I. D. s have the same analgesic effect as Paracetamol. Must be taken as a regular full dose to achieve maximum anti-inflammatory and analgesic effect. – Useful for continuous regular pain associated with inflammation. – Full analgesic effect within one week, but anti-inflammatory effect may take up to 3 weeks. – Taken after food. Potential to side effects are high especially in elderly population and susceptible individuals. Gastric-intestinal discomfort, heartburn, nausea, diarrhoea. More serious – patients can have gastric or duodenal ulceration. RED flags. Occasional hypersensitivity – rashes, angiodema and bronchospasm. Headache, dizziness (vertigo), drowsiness, insomnia, haematuria. Tinnitus and photosensitivity. Blood disorders Renal impairment
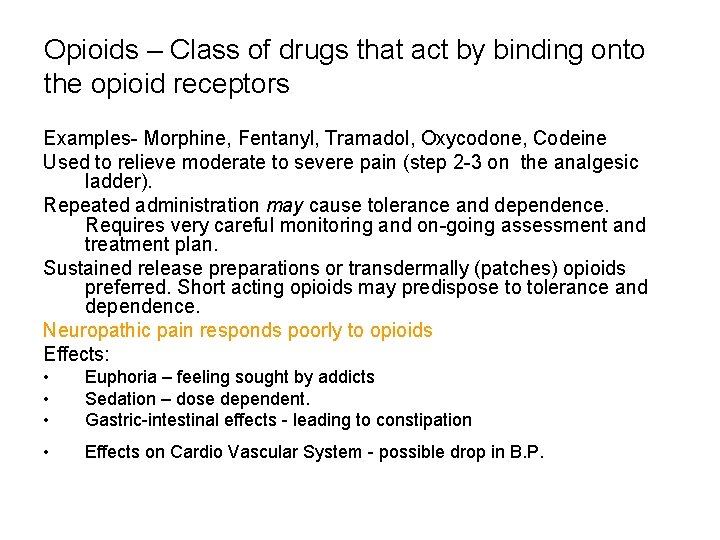
Opioids – Class of drugs that act by binding onto the opioid receptors Examples- Morphine, Fentanyl, Tramadol, Oxycodone, Codeine Used to relieve moderate to severe pain (step 2 -3 on the analgesic ladder). Repeated administration may cause tolerance and dependence. Requires very careful monitoring and on-going assessment and treatment plan. Sustained release preparations or transdermally (patches) opioids preferred. Short acting opioids may predispose to tolerance and dependence. Neuropathic pain responds poorly to opioids Effects: • • • Euphoria – feeling sought by addicts Sedation – dose dependent. Gastric-intestinal effects - leading to constipation • Effects on Cardio Vascular System - possible drop in B. P.
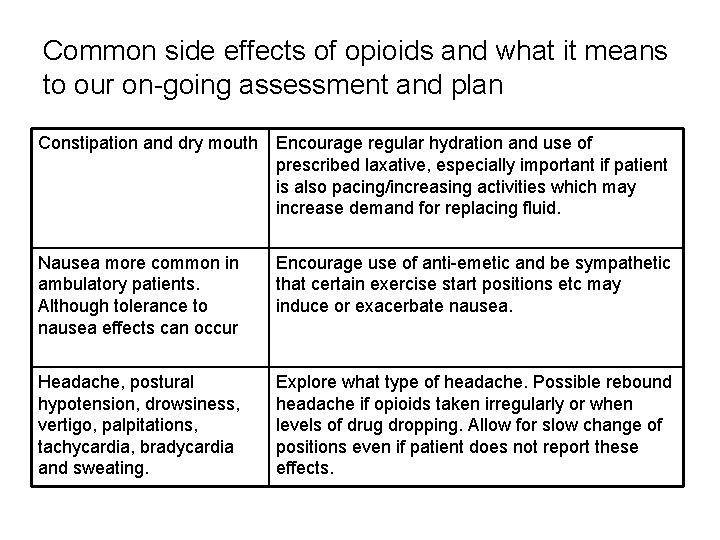
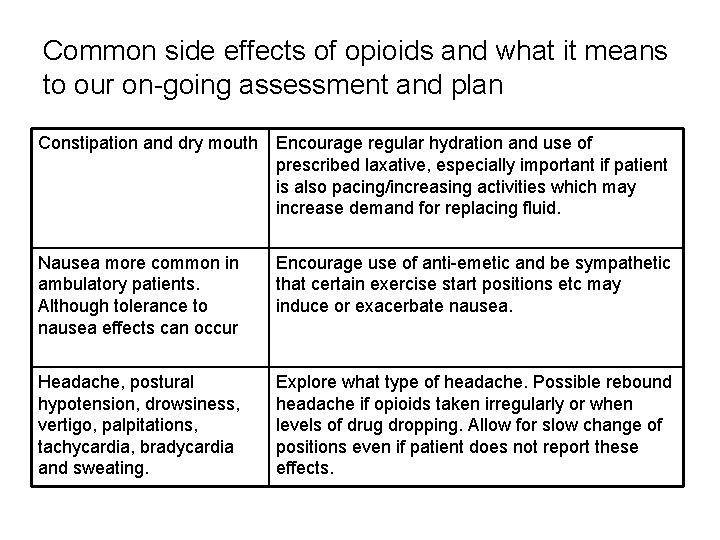
Common side effects of opioids and what it means to our on-going assessment and plan Constipation and dry mouth Encourage regular hydration and use of prescribed laxative, especially important if patient is also pacing/increasing activities which may increase demand for replacing fluid. Nausea more common in ambulatory patients. Although tolerance to nausea effects can occur Encourage use of anti-emetic and be sympathetic that certain exercise start positions etc may induce or exacerbate nausea. Headache, postural hypotension, drowsiness, vertigo, palpitations, tachycardia, bradycardia and sweating. Explore what type of headache. Possible rebound headache if opioids taken irregularly or when levels of drug dropping. Allow for slow change of positions even if patient does not report these effects.
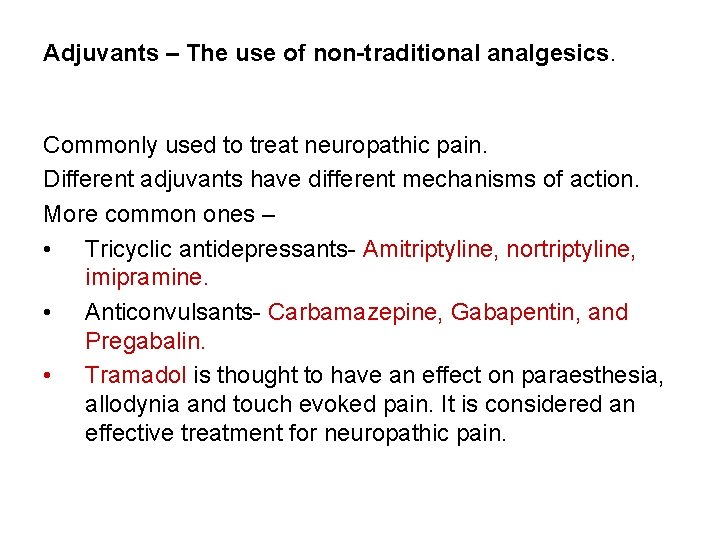
Adjuvants – The use of non-traditional analgesics. Commonly used to treat neuropathic pain. Different adjuvants have different mechanisms of action. More common ones – • Tricyclic antidepressants- Amitriptyline, nortriptyline, imipramine. • Anticonvulsants- Carbamazepine, Gabapentin, and Pregabalin. • Tramadol is thought to have an effect on paraesthesia, allodynia and touch evoked pain. It is considered an effective treatment for neuropathic pain.
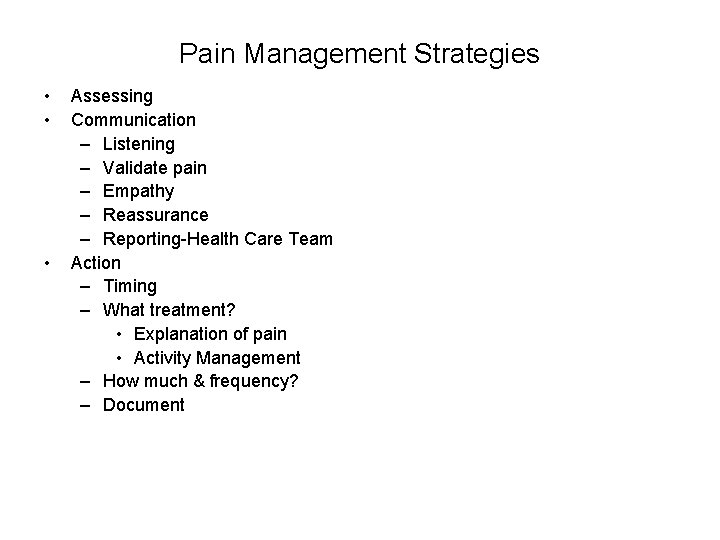
Pain Management Strategies • • • Assessing Communication – Listening – Validate pain – Empathy – Reassurance – Reporting-Health Care Team Action – Timing – What treatment? • Explanation of pain • Activity Management – How much & frequency? – Document
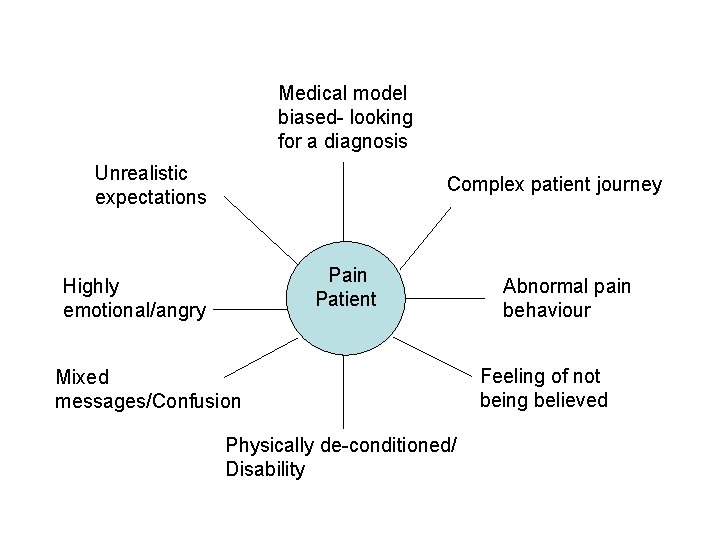
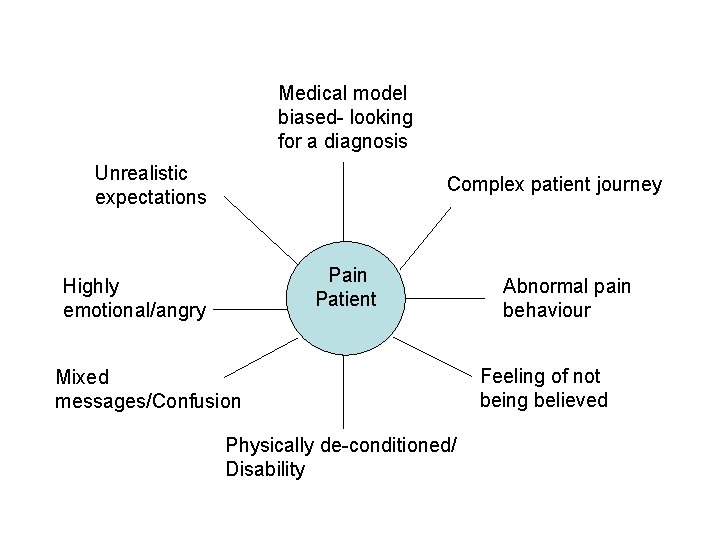
Medical model biased- looking for a diagnosis Unrealistic expectations Complex patient journey Pain Patient Highly emotional/angry Mixed messages/Confusion Physically de-conditioned/ Disability Abnormal pain behaviour Feeling of not being believed
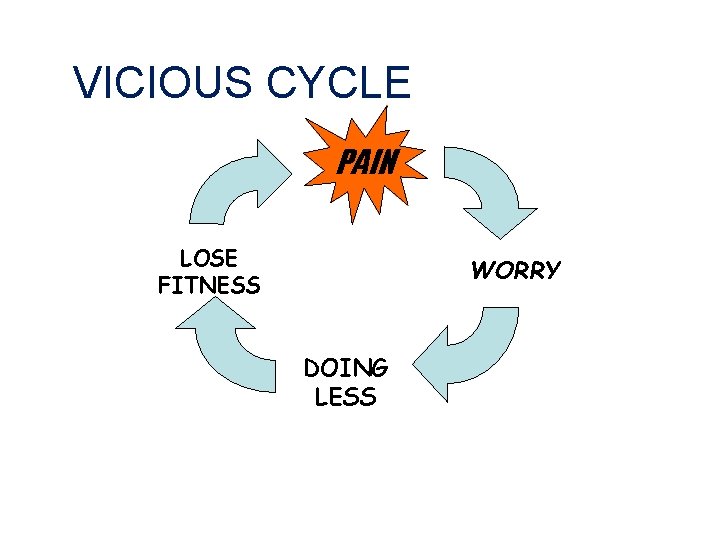
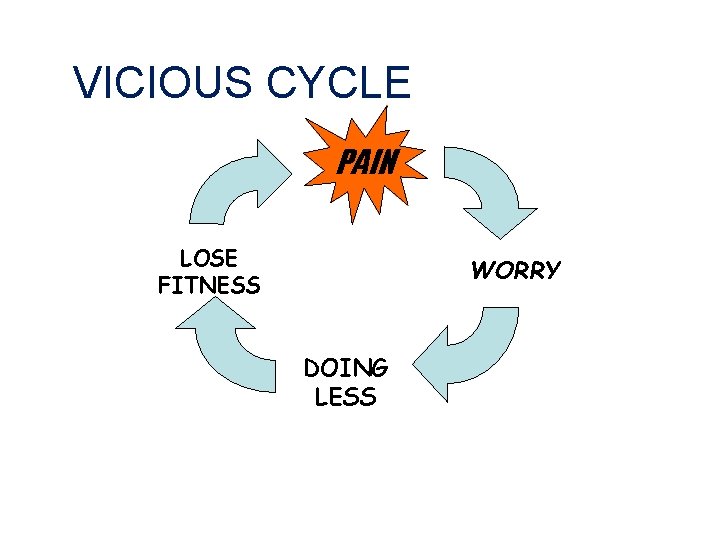
VICIOUS CYCLE PAIN LOSE FITNESS WORRY DOING LESS
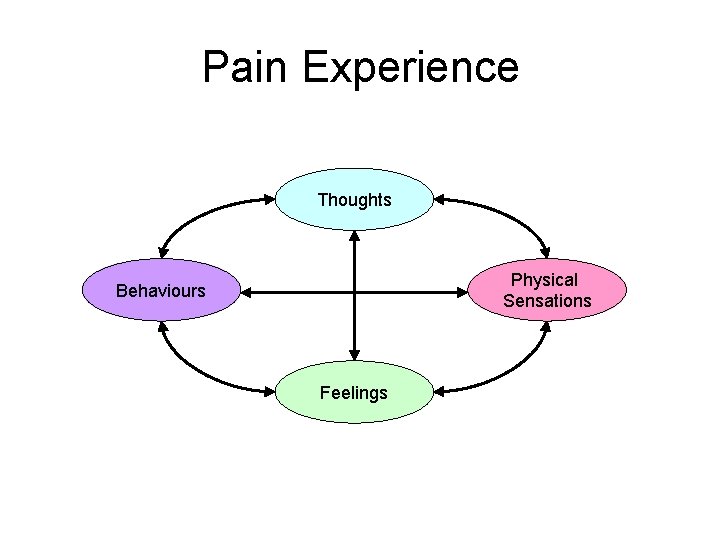
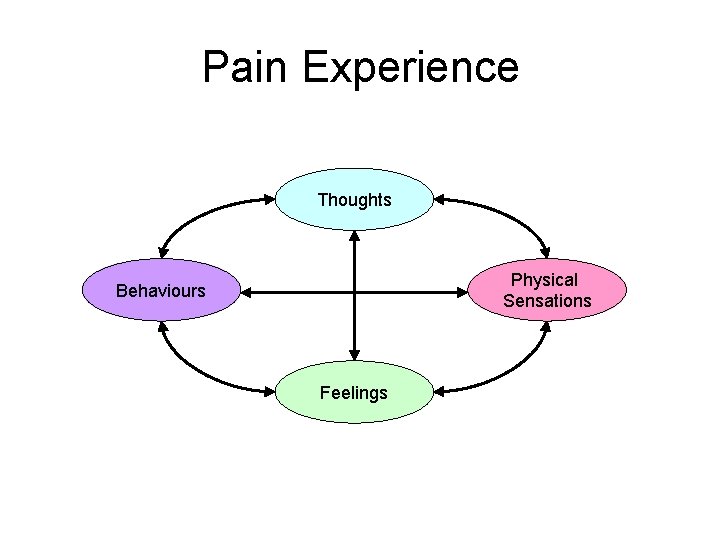
Pain Experience Thoughts Physical Sensations Behaviours Feelings
Problem Solving Treatment Approaches – What treatments would you use with your patients to help with pain?