Understanding how to improve the Care Programme Approach
- Slides: 9
Understanding how to improve the Care Programme Approach (CPA) Colbert Ncube, Programme Manager, Adult Mental Health 28 June 2018
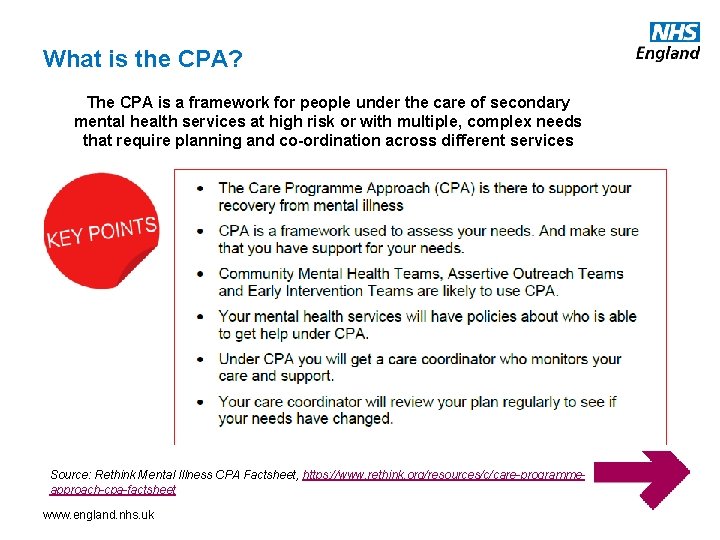
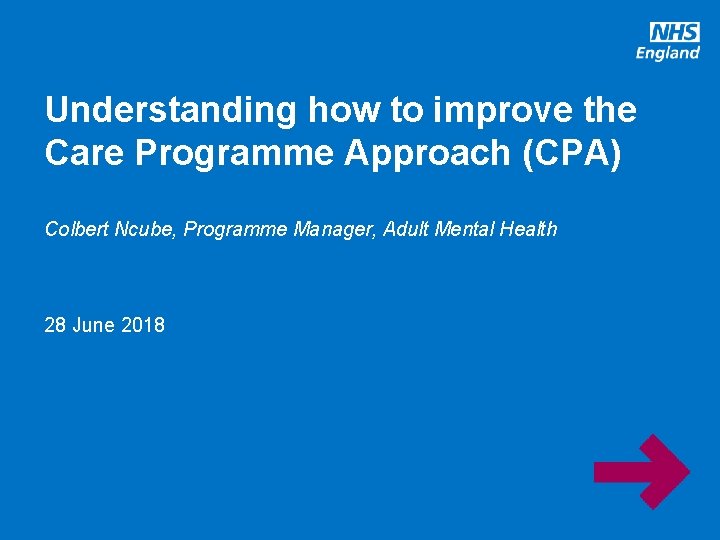
What is the CPA? The CPA is a framework for people under the care of secondary mental health services at high risk or with multiple, complex needs that require planning and co-ordination across different services Source: Rethink Mental Illness CPA Factsheet, https: //www. rethink. org/resources/c/care-programmeapproach-cpa-factsheet www. england. nhs. uk
Origins of this project • Numerous reports that the CPA framework is not conducive to driving the required improvements in community mental health services due to e. g. : o Significant time-consuming, administrative burden for staff, diminishing use of their clinical skills for therapeutic benefits to patients (paper heavy) and inefficient workforce deployment o Inadequate care planning o Lack of compliance with Care Act 2014 duties and minimal integration with non-NHS agencies (social care, housing, voluntary sector) They should, in my opinion, be trying to make you feel like you’re a partner in compiling the care plan not somebody who’s like an onlooker, as having something imposed on them • Some service users I’ve spoken to, they don’t want. Source: Service users’ experiences of recovery under to go to CPA meetings and some of them even the 2008 Care Programme Approach: A research study – said to me: ‘It’s not for us, it’s for the health Dorothy Gould 2012; Mental professionals, because they’re going to do what Health Foundation, NSUN, https: //www. mentalhealth. org. uk they want to anyway’ /sites/default/files/CPA_researc h_study. pdf CQC: ‘…enormous variation in the proportion of people on the CPA between trusts… this ranged across trusts from a low of 3% respondents on the CPA to a high of 73%’ (2016 Community Mental Health Survey Statistical release, http: //www. cqc. org. uk/sites/default/files/20161115_cmh 16_statistical_release. pdf) …’‘there is a large variation in the proportion of people on the CPA between trusts, which suggests that there are systematic differences in how trusts individually interpret and apply the CPA policy’ (2017 Community Mental Health Survey Statistical release, http: //www. cqc. org. uk/sites/default/files/20180515_cmh 17_statisticalrelease. pdf) Therefore the CPA as currently configured and interpreted appears to be a risk to the major piece of work on community MH services that we have begun. We decided to conduct some informal interviews with professionals and experts by experience to test the above hypotheses, understand emerging consensus, track down any good practice, and understand the sorts of things that people feel need to change or stay the same… 3
Findings • • • Time – Large caseloads and an overburdened workforce result in there not being enough time allocated to the development of a co-produced care plan. Ends up as a clinician led process. Medical model – CPA process is a very medically model focused Information sharing – there are variable levels of information sharing Training – there is no national level training offer. This results in a variable offer of care co-ordinationally as well as locally. Bureaucracy – CPA process is cumbersome and time intensive Guidance – the current guidance is too subjective. There are varying interpretations nationally and the document doesn’t reflect how things have moved on since 2008. Levels of CPA – there is confusion around the different levels of CPA Integration – CPA is seen as a health framework and this determines the level of engagement and ownership from social care and other agencies. Care co-ordination – there is a lack of clarity around the role of a care coordinator and what competencies are needed for the role Digital – there is a lack of integration between social care and health systems and this causes a fragmented care plan. www. england. nhs. uk 4
Suggestions for a way forward for ‘CPA alternative’ within NCCMH CMHS framework • • Clearer guidance on target service user groups and how service users ‘qualify’ for the ‘replacement’ community support offer which supports recovery and sets out clear responsibilities for all agencies such as health, social care and voluntary sector. Offer needs to focus on social determinants of recovery such as housing, social inclusion and employment and enable an individual having a sense of purpose and identity in the community with the support of a genuine and meaningful community network. Integrated care and support planning – there needs to be a rationalisation of all care planning and risk assessments in order to reduce the administrative burden on the health and social care workforce. There needs to be a clear disassociation between risk and the ability of a person to function. Care plans need to be service user directed, strengths rather than deficit based and have clear goals to support the service user’s recovery. There should be alignment with the Care Act 2014 where it applies, and Mental Health Act section 117 (MHA s 117) aftercare planning (in its current and likely revised form following the MHA Review) to avoid a situation where service users have multiple, disjointed and confusing care plans. Care plans need to be redesigned with service user input to focus on service users’ goals as they are currently very clinically-orientated. The term “care plan” doesn’t adequately encompass supporting people. There may need to be a rethink around terminology used as part of the CPA process if it remains as is. 5
Suggestions for a way forward cont. . • Training – clear core training competencies for care co-ordination with a focus on co-production of care plans and positive risk taking with an emphasis on utilising community assets rather than a focus on predominantly health and social care interventions. • Leadership – recovery-focussed services need to be part of organisational culture with board level oversight and scrutiny • Digital – more use of digital technology to enable new ways of working effectively such as integrated IT systems, use of Skype for meetings, service user focused electronic care plans. • Care co-ordination – clear guidance on what meaningful care co-ordination entails, and which roles can be used to fulfil the function of care co-ordination. There needs to be thinking around potential new roles. • Integrated teams – health and social care teams need to be working in a joined up way with shared systems which enable shared ownership from both parties which improves patient experience of the system • Recovery – the framework/process needs to focus on future planning as CPA currently doesn’t define “recovery”. There needs to be a step-down and step-up process which acknowledges the service user’s need for less and more support respectively, as appropriate. 6
Implications of a replacement to the CPA • National reporting – NHSE review of CPA-related targets set out in the Standard Contract and amend them in line with the revised framework. NHSE to work jointly with NHS Improvement (NHSI) and NHS Digital (NHSD) to review and revise any provider-level targets on the CPA. • Workforce training – NHSE/I will need to work with Health Education England (HEE) to develop a national education and training offer for care planning and care co-ordination to support delivery of the new framework. • Data Requirements – NCCMH will need to set out data requirements for a new care co-ordination/care planning framework to enable monitoring of the delivery of the framework. This will generate resource implications for provider IT systems and how they will need to change in response. Review and revision of data requirements is an existing deliverable for the NCCMH project. • Other areas of mental health and learning disability care – the CPA is used across a range of mental health and learning disability services, and not just for people under the care of non-acute, generic CMHS. Consideration needs to be given about how plans to amend or replace the CPA in the context of CMHS would affect the CPA and how it is used in other settings, such as learning disabilities and secure care settings. 7
Interim work to improve current practice • Development of a short ‘myth-busting’ guide for providers on the CPA…? • Guide could set out current minimum national data requirements and provide vital context by briefly outlining emerging thinking about the future of the CPA in the context of CMHS, and point to other relevant developments such as the MHA Review s 117 aftercare work and Care Act 2014. • This could reduce variation and enable good practice and act as a refresher following a decade of no update to CPA Guidance 8
Discussion points • Do these findings mirror local experience? • What do you think the positive aspects of care coordination are that need to be incorporated into a new framework? • Not everyone will get a care co-ordinator. How do we decide how care co-ordinators get allocated? • What are the potential unintended consequences of replacing the CPA? 9