Understanding Heart Failure By Damon Cottrell RN ACNSBC
Understanding Heart Failure By Damon Cottrell, RN, ACNS-BC, CCNS, CCRN, CEN, MS; Cynthia Bither, RN, ANP, ACNP, MSN; Renee Garnes-Spence, RN, PCCN, MSN; and Michelle Jones, RN, ANP, ACNP, MSN LPN 2009, March/April 2009 2. 3 ANCC contact hours Online: www. lpnjournal. com © 2009 by Lippincott Williams & Wilkins. All world rights reserved.
What is heart failure? n Progressive disease n Affects heart’s ability to pump effectively n Can’t supply sufficient blood and oxygen to the body’s tissues
Heart failure n Usually caused by injury to myocardium n Injury results in dilation or hypertrophy of one or both ventricles, called “remodeling” n Cardiac output and blood pressure drop
Causes of heart failure n n n Aortic regurgitation Aortic stenosis Cardiomyopathy Coronary artery disease Myocardial infarction Renal artery stenosis n n n Volume overload Dysrhythmias (atrial fibrillation) HIV Hypertension Hyperthyroidism Medications
Causes of heart failure n May be acute or chronic n Patients usually exhibit signs of shortness of breath, tiredness, swelling of feet, ankles, abdomen n May see jugular venous distention and hear a third heart sound

Signs and symptoms n n n n n Dyspnea Orthopnea Paroxysmal nocturnal dyspnea Weakness/fatigue Confusion Headache Insomnia Tachycardia Third heart sound n n n n Rales Edema Jaundice Alternating weak and strong pulse Cool, cold, or pale extremities Jugular venous distention Cyanosis
Diagnosing heart failure n History and physical: provide clues about patient’s physical status n ECG looks for dysrhythmias n Echocardiography provides information about function and heart size n Lab tests: electrolytes, thyroid studies, BUN, BNP

Classes and stages n Heart failure is divided into classifications based on specific pathophysiology n Helps guide best treatments n Heart failure is also broken down into stages n Treatment of stages is aimed at stabilizing patient’s condition and delaying progression

New York Heart Association Classification of Heart Failure Classification I n Ordinary physical activity doesn’t cause undue fatigue, dyspnea, palpitations, or chest pain n No pulmonary congestion or peripheral hypotension n Patient is considered asymptomatic n Usually no limitations of ADLs n Prognosis: Good
New York Heart Association Classification of Heart Failure Classification II n Slight limitation on ADLs n Patient reports no symptoms at rest but increased physical activity will cause symptoms n Basilar crackles and S 3 murmur may be detected n Prognosis: Good

New York Heart Association Classification of Heart Failure Classification II n Marked limitations on ADLs n Patient feels comfortable at rest but less than ordinary activity will cause symptoms n Prognosis: Fair Classification IV n Symptoms of cardiac insufficiency at rest n Prognosis: Poor
The four stages of heart failure n n Stage A: Patient at high risk of developing left ventricular dysfunction Stage B: Patients with left ventricular dysfunction who haven’t developed symptoms Stage C: Patients with left ventricular dysfunction with current or prior symptoms Stage D: Patients with refractory end-stage heart failure
Treating heart failure n Primary treatment: lifestyle modifications - restrict dietary sodium - smoking cessation - weight reduction (if indicated) - regular exercise
Treating heart failure n Medications - given to block hormones that circulate in excess when heart becomes weak - reverse changes in heart’s muscle that occur over time - first-line drugs given include angiotensinconverting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers

Medications n Most often recommended beta-blockers are bisoprolol (Concor) and carvedilol (Coreg) n Best chance of cardiac recovery with higher doses to reduce heart workload and lower BP n Evidence of lower mortality and fewer adverse reactions
Diuretics n Used mainly for symptom relief n Bumetanide (Bumex) and furosemide in low doses are preferred n Spironolactone (Aldactone) for advanced patients n African-Americans and patients with renal failure may be given Bi. Dil

Diuretics used to treat heart failure Thiazide diuretics n n n Bendroflumethiazide (Naturetin) Benzthiazide (Exna) Chlorothiazide (Diuril) Chlorthalidone (Hygroton) Hydrochlorothiazide (Hydro. DIURIL, Esidrix, Oretic) n n n Hydroflumethiazide (Diucardin, Saluron) Methyclothiazide (Enduron) Metolazone (Zaroxolyn, Mykrox) Polythiazide (Renese) Quinethazone (Hydromox) Trichlormethiazide (Metahydrin, Naqua)
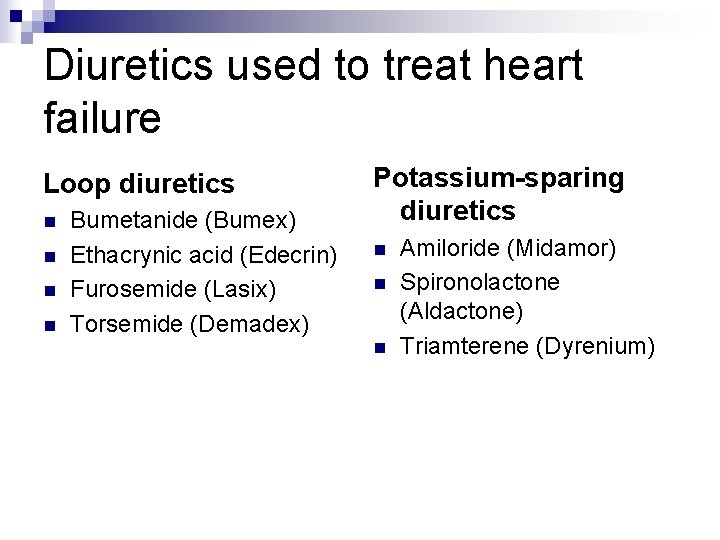
Diuretics used to treat heart failure Loop diuretics n n Bumetanide (Bumex) Ethacrynic acid (Edecrin) Furosemide (Lasix) Torsemide (Demadex) Potassium-sparing diuretics n n n Amiloride (Midamor) Spironolactone (Aldactone) Triamterene (Dyrenium)
Pacing n Many patients have delayed time interval between contraction of right and left ventricles n Synchronized biventricular pacing uses a third lead to pace ventricles simultaneously n Improves cardiac output n Nursing care: monitoring patient post procedure, elevation of head of bed, pain medication
Ventricular assist device n Supports right, left, or both ventricles n Used for patients awaiting transplant (“bridge to transplant”) n Used as treatment (“destination therapy”) n “Bridge to recovery” allows heart time to recover from remodeling; device is then removed
Nursing care of patients with a ventricular assist device n Assessment and prevention of infection at “driveline site” (patient’s abdomen) n Assess nutritional and functional status n Assess pump function and troubleshoot alarms
Monitoring patient n n Vital signs Lab results Renal function Nutritional status n n n Presence of infection or bleeding Effectiveness of anticoagulation Monitor pump parameters
Cardiac transplantation n Treatment option for end-stage heart failure n Approx. 2, 500 procedures in U. S. each year n 1 - and 3 -year survival rates 85. 6% and 79. 5% n Rigorous screening of candidates n Patient put on united organ sharing list
Cardiac transplantation n Major postoperative difference in these patients is need for chronotropic (heart rate) support n Immunosuppressive drug therapy to prevent rejection n Consists of three types of drugs: calcineurin inhibitors, corticosteroids, antimetabolites
Nursing care of transplant patients n Education on signs and symptoms of infection n Education on signs and symptoms of rejection n Nutrition counseling (well-balanced, low-fat diet) n Review follow-up visits

Nursing management/interventions for patients with heart failure n Administering medications and assessing patient response n Assessing fluid balance, intake, and output with goal of optimizing balance n Daily weights
Nursing management/interventions for patients with heart failure n Assessing jugular venous distention n Auscultating lung and heart sounds n Identifying dependent edema n Monitoring pulse, BP
Nursing management/interventions for patients with heart failure n Checking for postural hypotension n Examining skin turgor for signs of dehydration n Assessing for symptoms of fluid overload
Potential complications of HF therapy n Hypokalemia: low potassium; signs include dysrhythmias, weak muscles; can cause heart muscle weakness n Hyperkalemia: abnormally high serum potassium, especially when taking ACEs, ARBs, or spironolactone
Potential complications of HF therapy n Hyponatremia: deficiency of serum sodium n Hyperuricemia: excessive uric acid in blood
Patient teaching n Teach patients rationale for medications (doses, times, adverse reactions) n Teach patient to limit fluid to 2 liters per day n Teach patient to follow a low-sodium diet
Patient teaching n Teach patient to weight himself daily and to notify healthcare provider of an increase in weight of 3 lbs or more n Address patient’s psychological needs
- Slides: 32