UNDERSTANDING ASSESSMENTS DETERMINATIONS AND DIAGNOSES AND CHALLENGING DOCTORS
- Slides: 28
UNDERSTANDING ASSESSMENTS, DETERMINATIONS, AND DIAGNOSES - AND CHALLENGING DOCTORS WHEN NEEDED Carilyn Ellis, M. A. Clinical Psychology (Psy. D. Clinical Psychology May, 2014) Webinar for the Society for Certified Senior Advisors (CSA) January, 2014
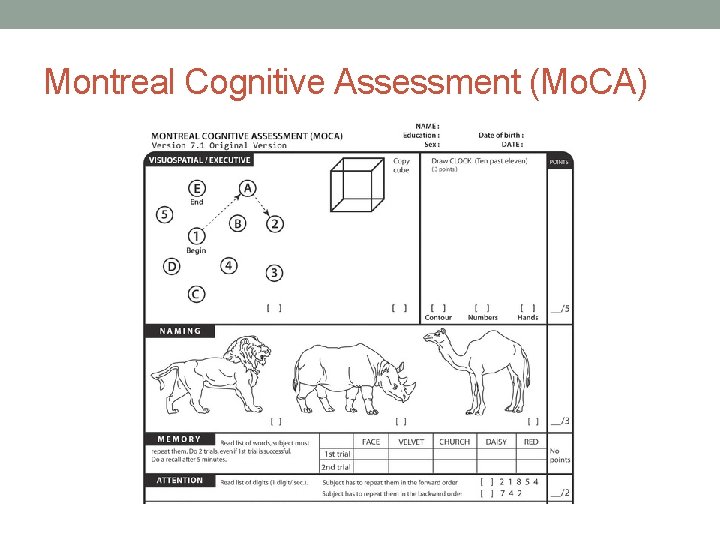
Goals: • To understand age-related (expected) vs. non-age-related decline (suggestive of dementia or other pathology) • To understand some of the basic assessments used in clinical settings (e. g. Montreal Cognitive Assessment (Mo. CA), Mini Mental Status Exam (MMSE), Mental Status Test of Older Adults (Mini. Cog), Short Blessed Test, Patient Health Questionnaire (PHQ-9) etc. • To understand the cognitive domains of these tests (what are they testing? ) • To understand what they are (screeners) and what they are not (diagnostic truth) and how to help families and older adults advocate in the medical setting.
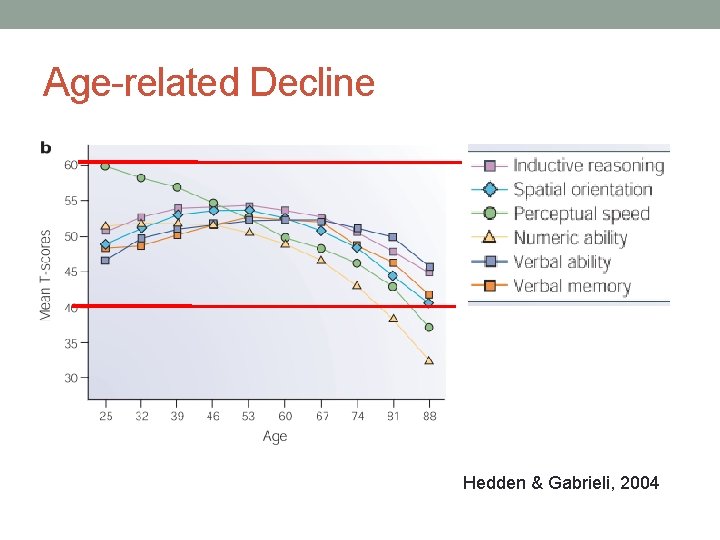
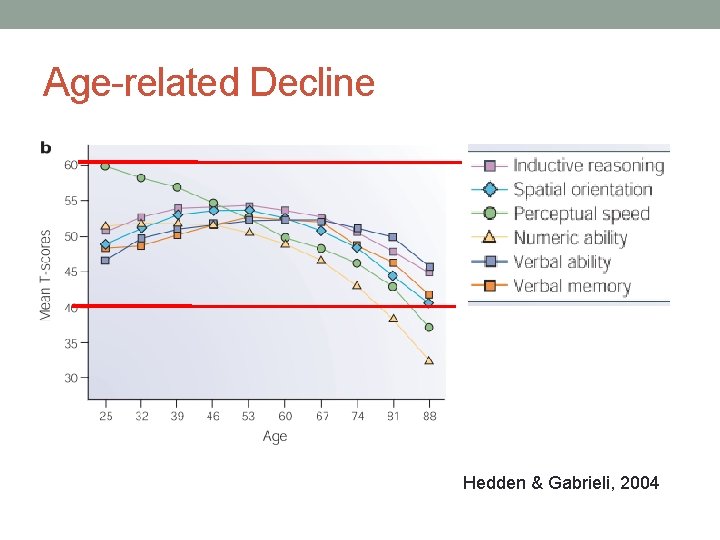
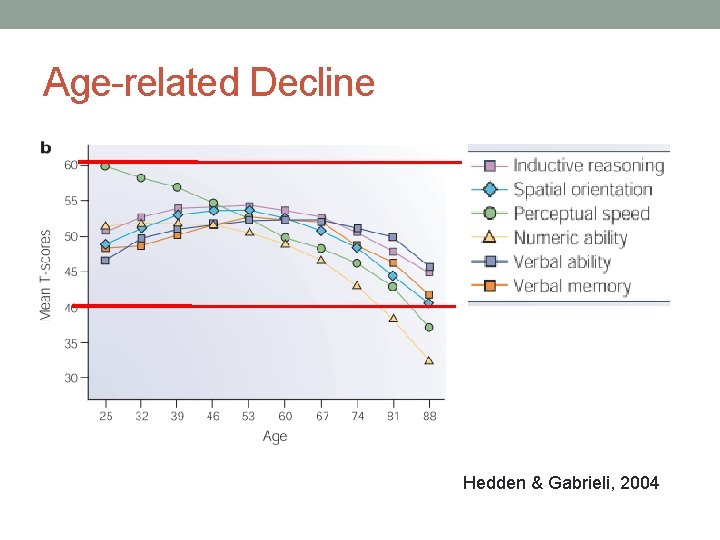
Age-related Decline Hedden & Gabrieli, 2004
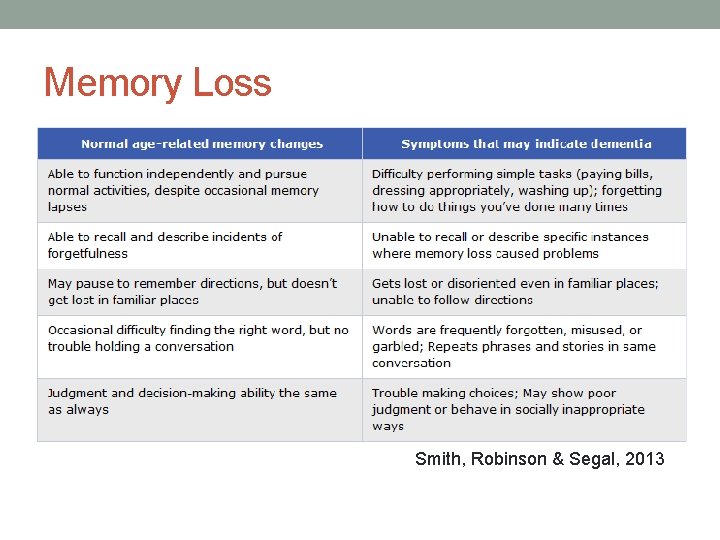
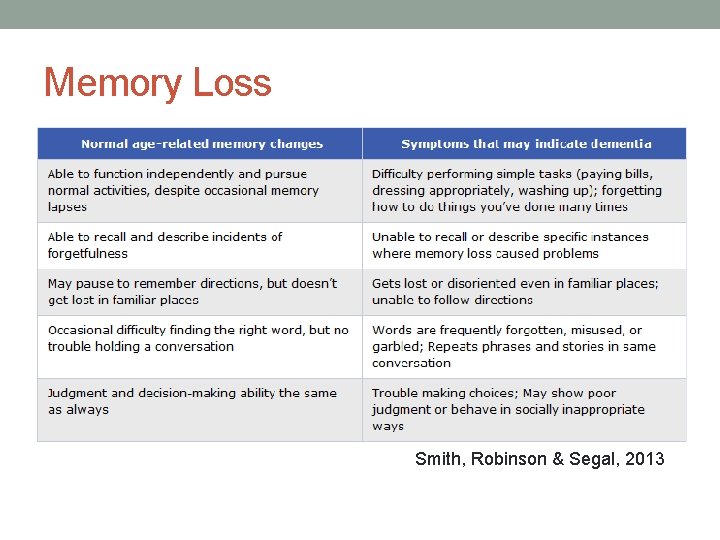
Memory Loss Smith, Robinson & Segal, 2013
When do we start to wonder…? • Look for impairment in activities of daily living. Are the person’s complaints or problems getting in the way of life? • Mark has noticed that as he gets older, he has greater difficulty finding his glasses, so he has made it a habit to place them on the table by the front door whenever he takes them off. • John has had increasing difficulty navigating his way around. He has been bumping into tables and having difficulty dressing himself. The eye doctor said his eyesight is fine.
The D’s (that aren’t Dementia!) • Delirium • Depression • Damaged Brain • Developmental Delay • Deficient Education
Domains of Cognitive Functioning • Visual/spatial (often called “visuospatial”) • Executive functioning • Memory (Immediate, working, long term, recognition) • Attention • Abstraction • Orientation • Language (verbal fluency, confrontation naming) • Math/numeric ability
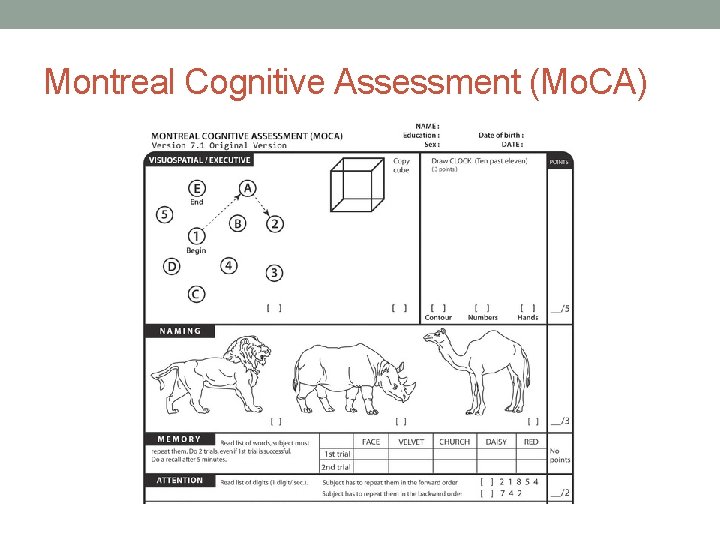
Montreal Cognitive Assessment (Mo. CA)
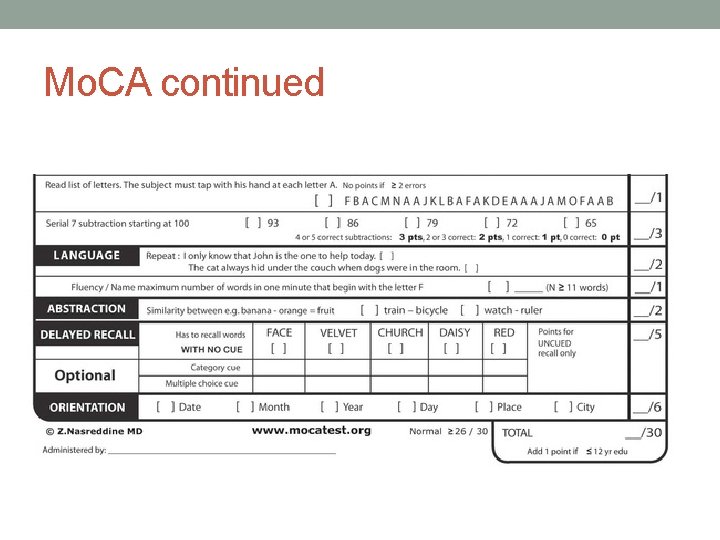
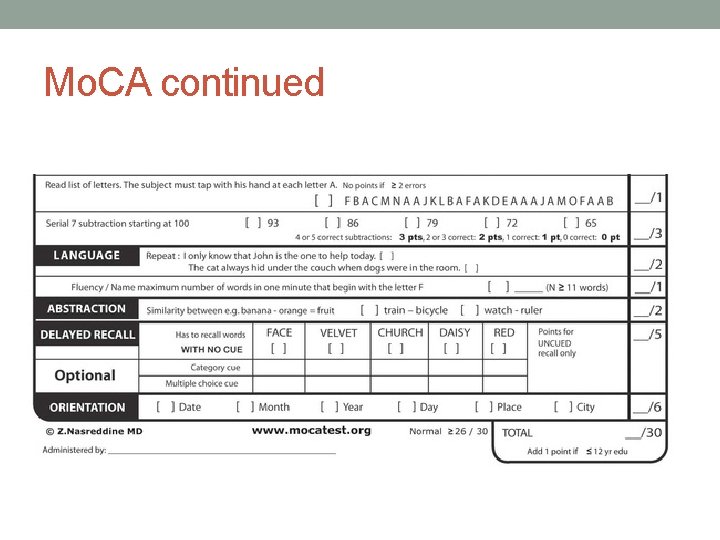
Mo. CA continued
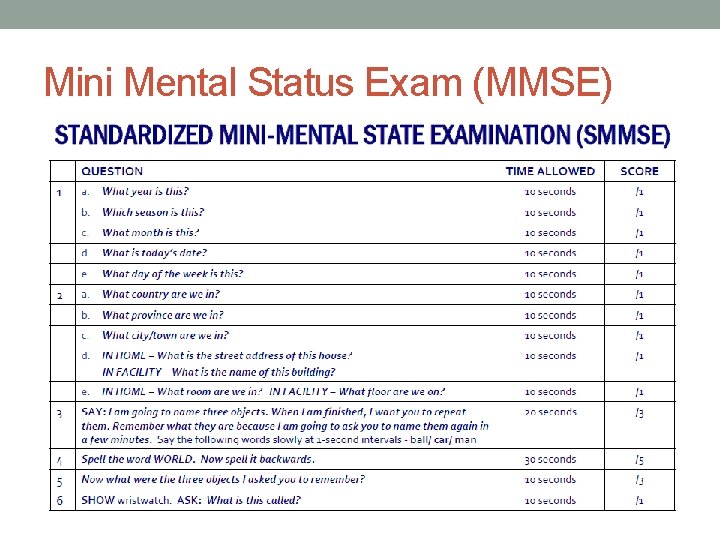
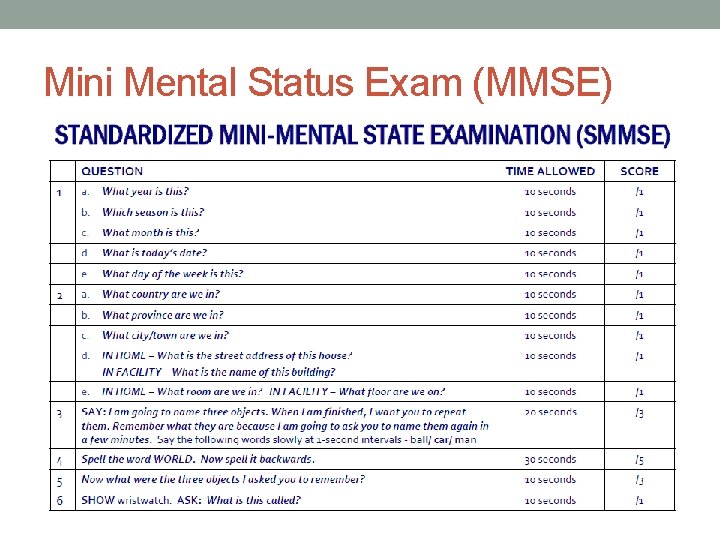
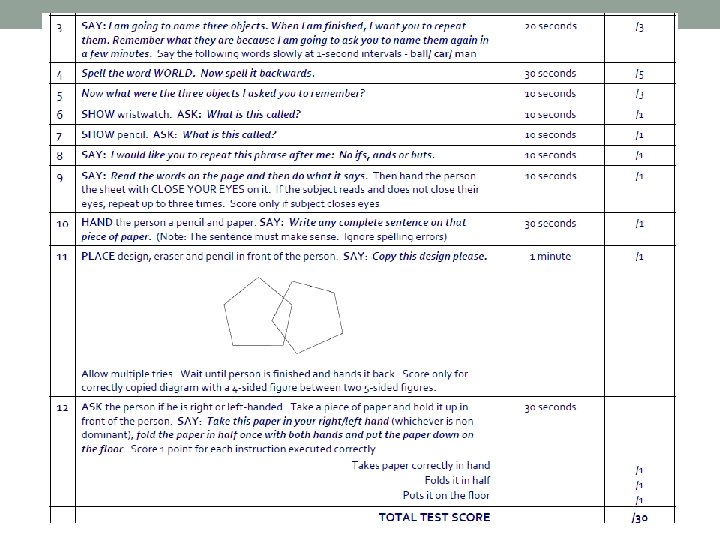
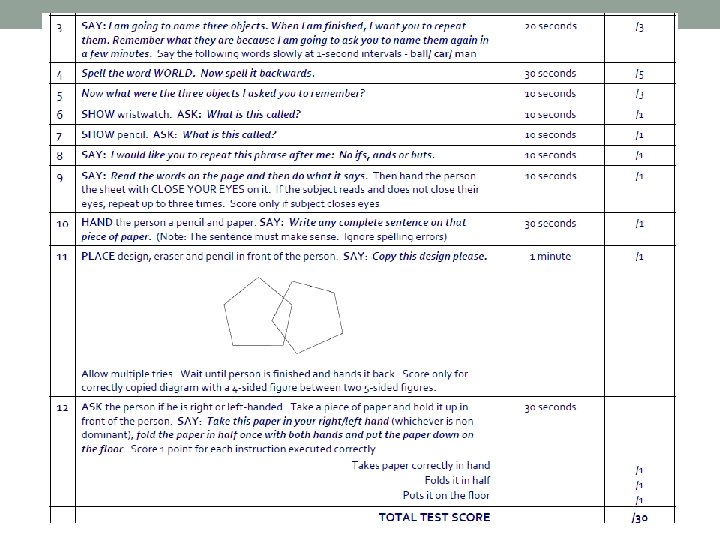
Mini Mental Status Exam (MMSE)
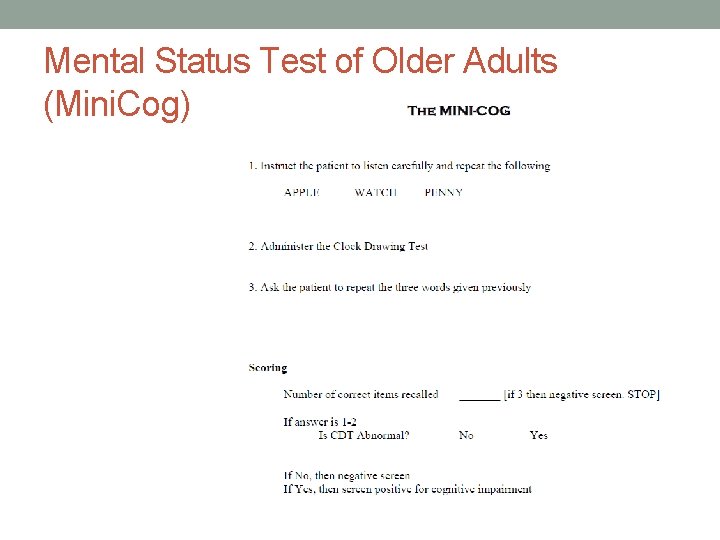
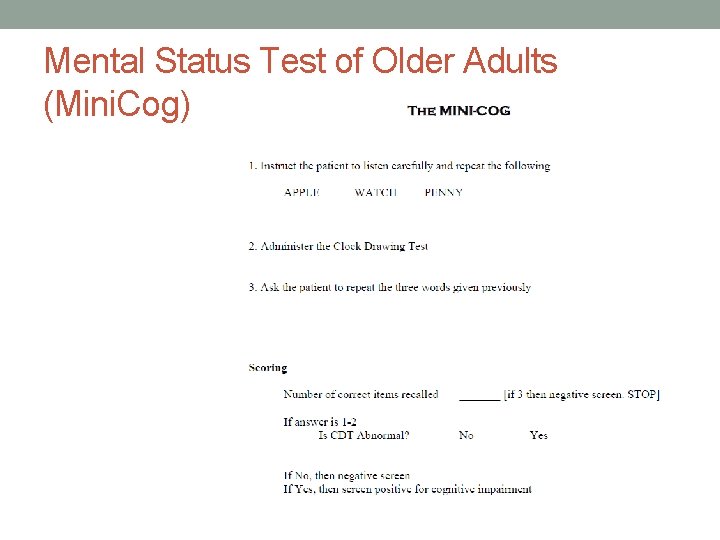
Mental Status Test of Older Adults (Mini. Cog)
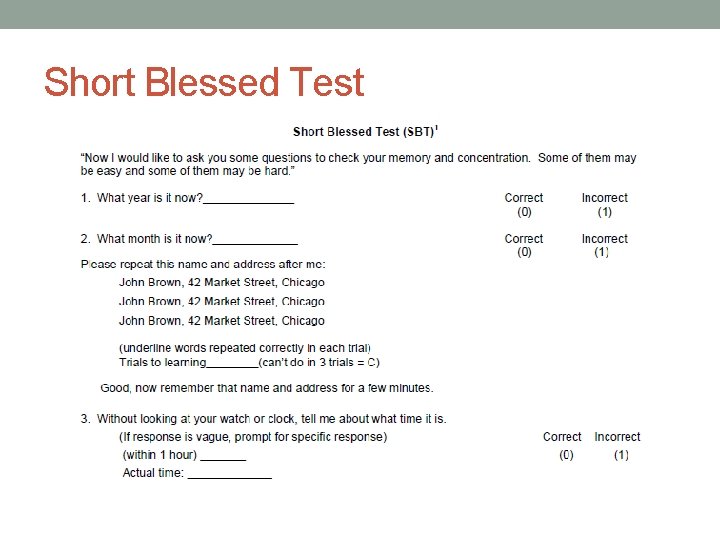
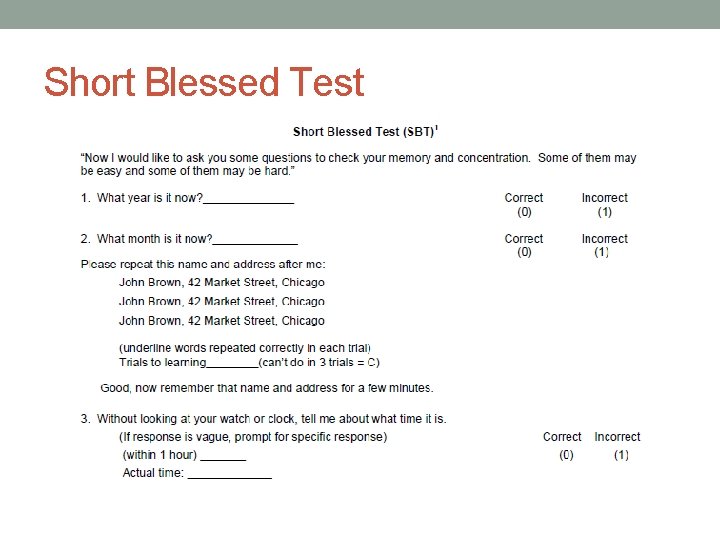
Short Blessed Test
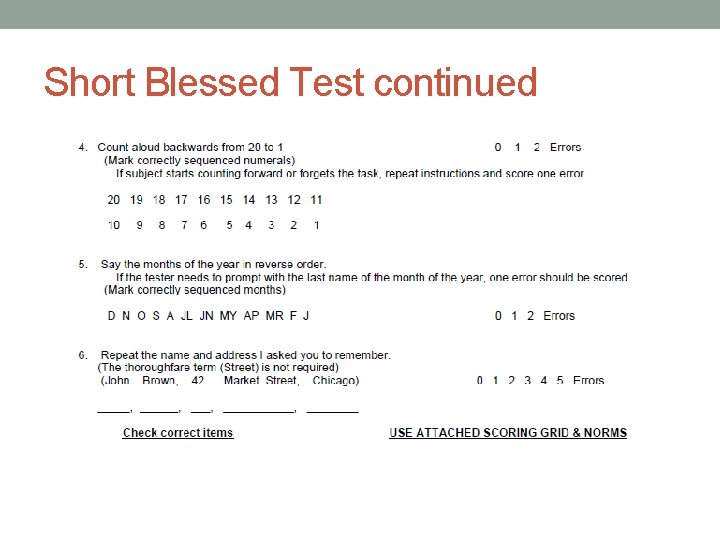
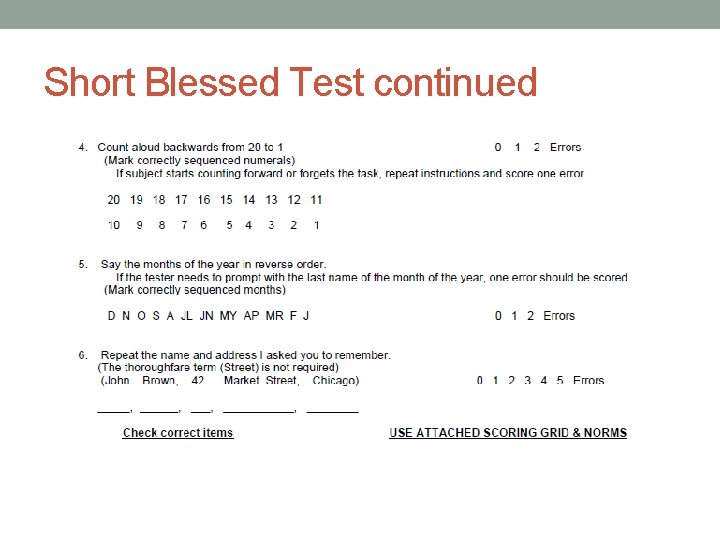
Short Blessed Test continued
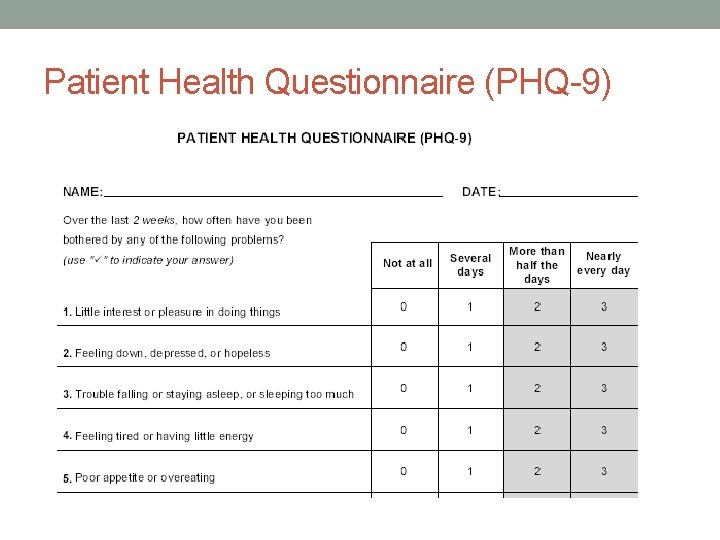
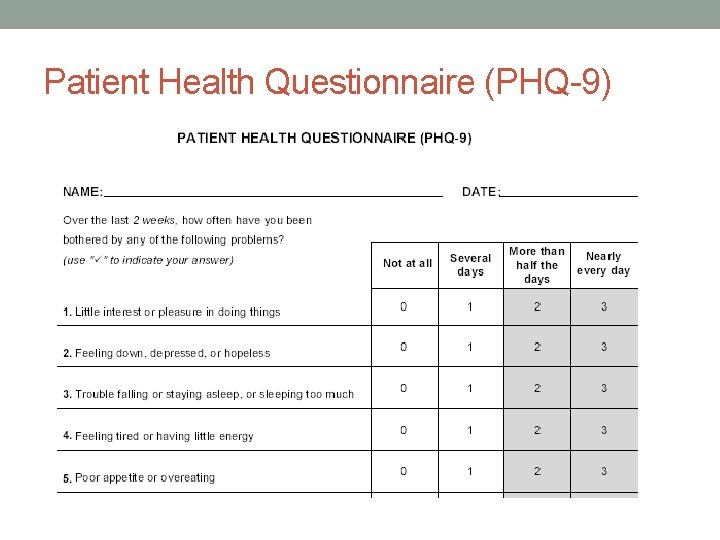
Patient Health Questionnaire (PHQ-9)
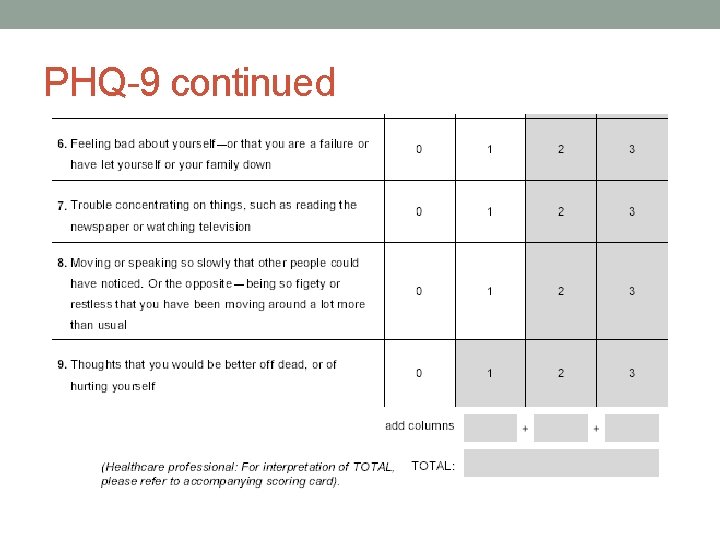
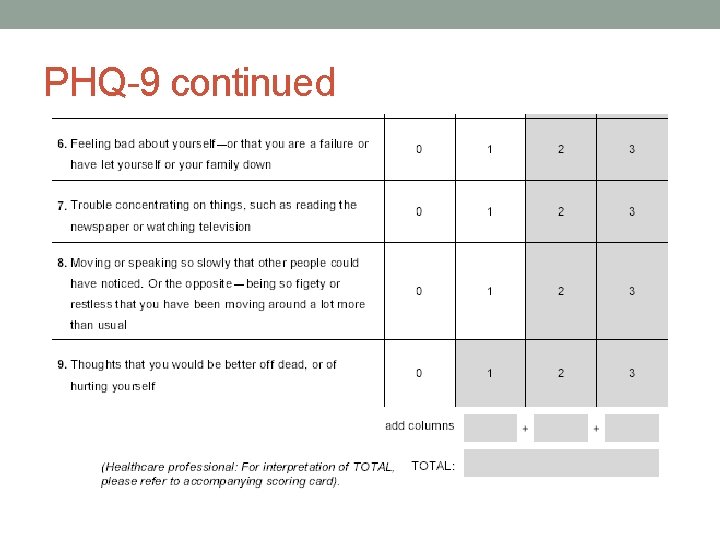
PHQ-9 continued
Why do we use these? • They’re short • They’re easy • They’re repeatable • They do have validity as screeners (they tap into domains that are affected by cognitive decline)
The Danger • Visual/Hearing Impairments • Improper administration • Diagnostic Rule Outs (The 6 D’s – alternatives to dementia) • Medication prescriptions and overuse
A note on medication • Currently in the United States, those 65 years of age and older make up 13 percent of the total population, but account for 30 percent of all prescriptions written. (Wegmann, 2013) • Nearly 3 in 10 people between ages 57 to 85 use at least five prescriptions, according to the Substance Abuse and Mental Health Services Administration (SAMHSA).
• Between 1997 and 2008, the rate of hospital admissions for conditions related to prescription medications and illicit drug use rose by 96 percent among people ages 65 and 84; for people 85 and older, admissions grew 87 percent. • SAMHSA notes medication misuse and abuse can cause a range of harmful side effects, including drug-induced delirium. (Join Together Staff, Partnership for a Drug Free America, 2011)
Assumptions and Determinations • Number 1: Dementia • Number 2: Questionable decision-making capacity • Fundamentals of Decision-Making capacity • It is NOT global • Most hospitals are concerned only with medical decision making capacity. • Cognitive impairment and decline do not automatically mean impairment in medical decision-making capacity • Decision-making capacity has multiple parts
Medical Decision Making Capacity 1) Does patient know his/her medical diagnoses? • Does patient know his/her medications, their purpose and how/when to take them? • Does patient understand: - Current treatment options - Risk/benefits of current treatment? - Risk/benefit of no treatment? - Risk/benefit of alternative treatment? • Is patient able to state/communicate a decision concerning his/her medical care? (Is it consistent? ) • Based upon the above response, is the patient able to make an informed decision concerning his/her medical care at this time? 2) The ability to designate a durable power of attorney for medical decisions.
Advocacy Knowledge is power
What you can do as a CSA: Before • Onset, Frequency, Intensity, Duration (OFID) • Prescription, over the counter and holistic med review. • Ask the doctors questions
What you can do as a CSA: After • Find out what screeners and/or diagnostic tools have been used. • Get a copy of screener/diagnostic results. Know your domains! • Check for tool/appendage impairment
What you can do continued • Request records and read the notes • Make them explain any abbreviations or medical jargon in the notes • Example: 87 y. M with CAD, afib, MCI/AD, HTN, UI w/h/o MDD. • Get a second opinion
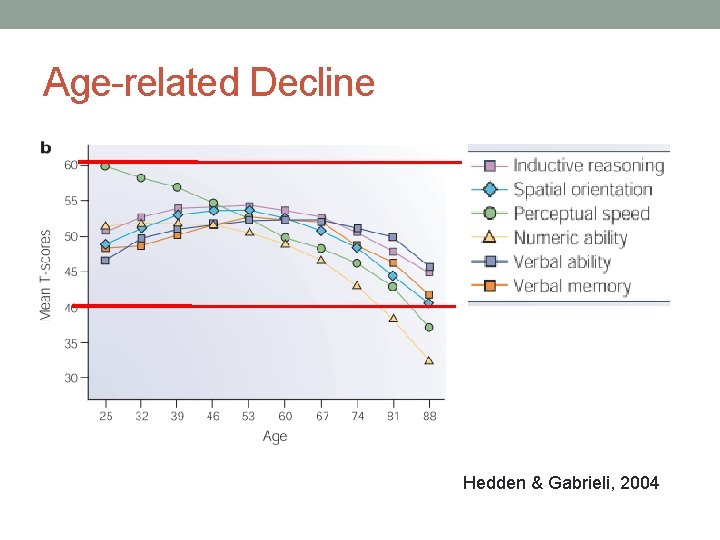
Age-related Decline Hedden & Gabrieli, 2004
Moral of the Story… • Words like dementia, Parkinson’s, Impairment…all of these induce shock. Don’t accept anything until you have definitive proof. • Knowledge is power. All patients have rights to ALL of their records. Encourage your clients to get copies. • Educate your clients on the basics and teach them the skill of questioning medical authority (in a respectful, collaborative way) • It is never wrong to ask questions of the doctors and make them prove to you what they believe. (Half the time it makes them go back and re-assess). • Ask, “Is there anything else it could be? ”