Understanding and Responding to Students who SelfMutilate Rich



- Slides: 48
Understanding and Responding to Students who Self-Mutilate Rich Lieberman Los Angeles Unified School District Suicide Prevention Unit (818) 705 -7326 rlieberm@lmu. edu
CUTTERS: Challenges to School Site Crisis Teams w Overwhelming numbers of referrals w Low risk suicide assessment w Behaviors appear contagious
MYTHS w The w All cutter is attempting suicide. cutters have been physically or sexually abused.
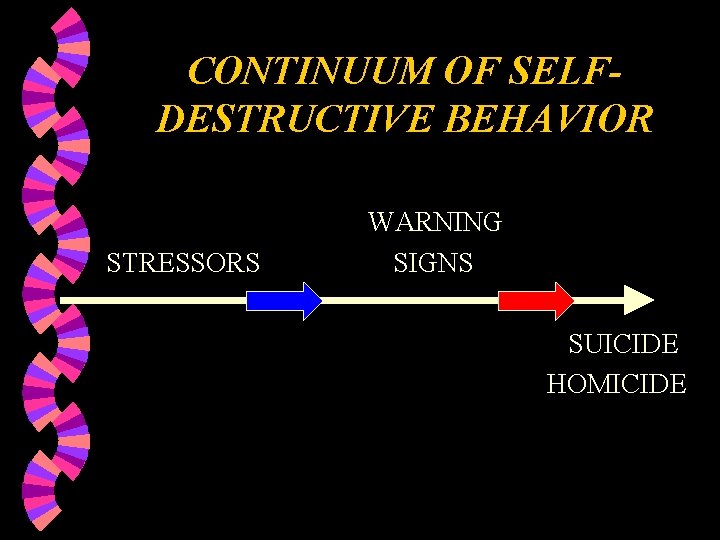
CONTINUUM OF SELFDESTRUCTIVE BEHAVIOR STRESSORS WARNING SIGNS SUICIDE HOMICIDE

DEFINITIONS w Inclusion of other Self-Injurious Behaviors (SIB) w Distinguish from ritual tattooing, branding and piercing w Not related to cognitive impairment
DEFINITIONS (2) “The definition of self-mutilation is that it is a direct, socially unacceptable, repetitive behavior that causes minor to moderate physical injury. ” Suyemoto&Kountz (2000) Self-Mutilation The Prevention Researcher Nov. , Vol. 7 No 4
CLASSIFICATIONS OF PATHOLOGICAL SELFMUTILATION w Major Self-mutilation w Stereotypic Self-mutilation w Moderate/Superficial Selfmutilation
CLASSIFICATIONS: Major Self-mutilation Infrequent act that occurs suddenly, with a great deal of tissue damage and bleeding. w Most commonly associated with psychosis and acute intoxication. w Religious or sexual themes may be present. w
CLASSIFICATIONS: Stereotypic Self-mutilation “Driven by a biological imperative to harm themselves shamelessly and without guile” Favazza Most common form: head banging w Most common population: Institutionalized/psychotic w Self-injurious behaviors (SIB) w
CLASSIFICATIONS: Stereotypic Self-mutilation • Autism (head banging, lip/wrist biting) • Retts disorder (hand washing) • Tourettes (multiple simple and complex tics, variety SIB) • Use of medication is common though behavior therapy is primary modality.
CLASSIFICATIONS: Moderate/Superficial Self-mutilation w Most common: skin cutting, burning • Compulsive: Hair pulling, scratching. • Episodic: Rapid respite from distressing thoughts/emotions/tension; regain sense of self control. • Repetitive: Addiction to self harm.
DIAGNOSIS Repetitive Self-mutilation Syndrome (RSM) RSM is recurrent failure to resist impulses to harm one’s body physically without conscious suicidal intent. Bodies Under Siege Self-mutilation and Body, Modification in Culture and Psychiatry Armando R. Favazza, M. D. Hopkins University Press Baltimore/London
DIAGNOSIS (2) RSM can be associated with many disorders. w Borderline personality disorder w Depression: mood & anxiety disorders w Impulse disorders: Episodic/gratifying w • • w Alcohol & substance abuse Suicide attempts Eating disorders Repetitive self-mutilation Post traumatic stress disorder
Repetitive Self-mutilation Syndrome PREVALENCE & ONSET w w w Onset: late childhood-early adolescence Rates higher in adolescence: approximately 1400 per 100, 000 Rates higher in females Rates higher in psychiatric pop. Behaviors may become chronic and persist for 5 -10 yrs. or longer if left untreated.
Repetitive Self-mutilation Syndrome PREDISPOSING FACTORS w w w Onset linked to “stressful” situations Physical/sexual abuse in childhood Early history of hospitalization/surgery Parental alcoholism/depression Perfectionist tendencies/dissatisfaction with body Inability to tolerate and express emotions
WHY DO PEOPLE ENGAGE IN SELF -INFLICTED VIOLENCE? w Meets a multitude of needs w Relief from overwhelming feelings w Communication w Stop inducing or preventing dissociation Alderman, T. (1997) The Scarred Soul: Understanding and Ending Self-Inflicted Violence (New Harbinger Press, Oakland, CA. )
WHY DO PEOPLE ENGAGE IN SELF -INFLICTED VIOLENCE? w Self-punishment: scars/blood concrete reminders w Physical expression of pain w Re-enacting previous abuse
WHY DO PEOPLE ENGAGE IN SELF -INFLICTED VIOLENCE? Bottom Lines Euphoric feelings w Establishing control w “Self-mutilation is an active, direct, concrete representation of intense anguish. ”
PHENOMENOLOGY “Although self-mutilators sometimes report feeling guilty or disgusted after an incident, most adolescents report feeling relief, release, calm or satisfaction…ending the anger, tension or dissociation. ” Suyemoto K. (1998) The functions of self-mutilation. Clinical Psychology Review, 18(5), 531 -554
PHENOMENOLOGY (2) Precipitating event: usually the perception of an interpersonal loss or abandonment w Poor coping skills w Reacting to overwhelming emotions by dissociating w Isolation w
FAMILY AND DEVELOPMENTAL FACTORS Families characterized by divorce, neglect or deprivation of parental care w Parental loss = emotional distancing and inconsistent parental warmth w Often a history of childhood physical/sexual abuse w

TREATMENTS w Biological w Psychological and Social w Cognitive/Behavioral Therapy “There is no single, correct therapeutic approach. Prevention is key. ” Favazza
TREATMENTS: Biological w Serotonin (SSRIs) w Preferred treatment for depression and anxiety disorders. w Primarily affect on impulsivity/compulsivity
TREATMENTS: Psychological and Social w Making and maintaining a relationship w Breaking the habit w Maintaining change Tantam & Whitaker (1992)
TREATMENTS: Psychological and Social w Analyze precipitating events • Identify thoughts and emotions • Where/how wounds • Goal: Reduce tensions w Gain control over cutting Hawton (1990)
TREATMENTS: Cognitive/Behavioral Therapy w Connection between thoughts and behaviors w Facilitated by directing attention away from environment and towards thoughts w Replace negative perceptions with focus on positive qualities.
SCHOOL INTERVENTIONS: General strategies for Educators w Consider outside referral w Strategies related to increasing abilities to verbalize and express emotions w Teach coping skills: loss w Connectedness with caring adults
SCHOOL INTERVENTIONS: General strategies for Educators Talk about self-inflicted violence w Be available and supportive (keep your negative reactions to yourself!) w Set reasonable behavioral limits w Do not discourage self-injury w
SCHOOL INTERVENTIONS: General strategies for Educators w Substitute behaviors w Stress management techniques w Alternative therapies include art therapy and EMDR w Recognize the severity
SCHOOL INTERVENTIONS: General strategies for Educators Substitute behaviors w Help seeking behaviors w Journals/drawing w Get active: exercise w Advocacy: reaching out to others w Cognitive-behavioral approaches
SCHOOL INTERVENTIONS: General strategies for Educators Substitute behaviors w Rubber bands w Holding books out at arms length w Standing on tip toes w Substitute ice or magic marker for sharp implement
SCHOOL INTERVENTIONS: General strategies to limit contagion Divide w Assess for suicide risk w Get parents involved and supported w Utilize school/district/community extracurricular resources w Do not have assemblies, presentations or show videos w
WARNING SIGNS OF YOUTH SUICIDE Suicide notes w Threats w Plan/method/access w Depression (helplessness/hopelessness) w • Masked depression (risk taking behaviors, gun play, alcohol/substance abuse) w Giving away prized possessions

WARNING SIGNS OF YOUTH SUICIDE w Efforts to hurt self • Running into traffic • Jumping from heights • Scratching/cutting/marking the body Death & suicidal themes w Sudden changes in personality, friends, behaviors w
SCHOOL SITE CRISIS TEAM w Members: • Designated reporter • Administrator • Support personnel Assess and Advise w Collaborate with law enforcement and local mental health resources w
SUICIDE INTERVENTION Procedures w Assessment of risk w Duty to warn w Duty to refer w Caveats: • Collaboration • Documentation
RISK ASSESSMENT w LOW: Ideation? w MODERATE: Previous suicidal behaviors? w HIGH: Current plan method/access?
SUICIDE INTERVENTION: Risk Assessment w LOW: Ideation? “Have you ever thought about suicide (harming yourself)? ” • Current thoughts • Past thoughts (<6 months) • Non-verbal warning signs (writing/drawing)
SUICIDE INTERVENTION: Risk Assessment w MODERATE: behaviors? Previous suicidal “Have you ever tried it before? ” • Previous attempts/gestures/RARD • Previous hospitalizations • Previous trauma (abuse, victimization) • Medications
SUICIDE INTERVENTION: Risk Assessment w HIGH RISK: Current plan? “Do you have a plan to kill yourself now? How would you do it? ” • Method? Assess access • Firearms mentioned? • Refusal to sign no-harm agreement
SUICIDE INTERVENTION: Risk Assessment: Exacerbating factors w Precipitating events w High stressors (family, school, loss) w Poor access to resources
SUICIDE INTERVENTION: Intervention strategies w LOW RISK: w Reassure and supervise student w Warn parent w Assist in connecting with school and community resources w Suicide-proof environments w Mobilize a support system w No-Harm agreements w Transportation issues
SUICIDE INTERVENTION: Intervention strategies w No-Harm agreements emphasize: w Connectedness with adults w Help–seeking behaviors w Communication skills w Grief resolution w Linkages with community and district resources
SUICIDE INTERVENTION: Intervention strategies w MODERATE /HIGH RISK: w Supervise (restrooms, bus) w Release to: w Parent (may not be appropriate if child is high risk) w Law enforcement w Psychiatric mobile responder w Release adult to: 3 rd party; IUSD Employee? Call District Office.
SUICIDE INTERVENTION: Duty to Warn w. Would calling the parent place the child in greater danger? If so, call Children’s Protective Services. w. Warning parents w. Available/Cooperative? w. Assessment w. Mental information Health insurance w. Release w. Educate of information parents on depression; suicidal/self injurious behaviors; “She is doing this for attention!”
SUICIDE INTERVENTION: Duty to Refer w. Emergency response teams w. Collaborating w. Local with law enforcement district resource guides w. Cultural/developmental/sexuality w. District resources (Special Ed) factors
Understanding and Responding to Students who Self-Mutilate Very complex behavior that fulfills a multitude of needs w Dispel myths w Contagion: often runs in peer groups w Respond individually w Assess for suicide risk w
Understanding and Responding to Students who Self-Mutilate Warn and involve parents w Utilize school/community resources w Do not discourage self harm w Do teach substitute behaviors that focus on help-seeking/communication skills, reduction of tension and isolation w