Uncommon Arteriopathies Vasculitis Temporal arteritis Periarteritis Nodosa SLE
- Slides: 20
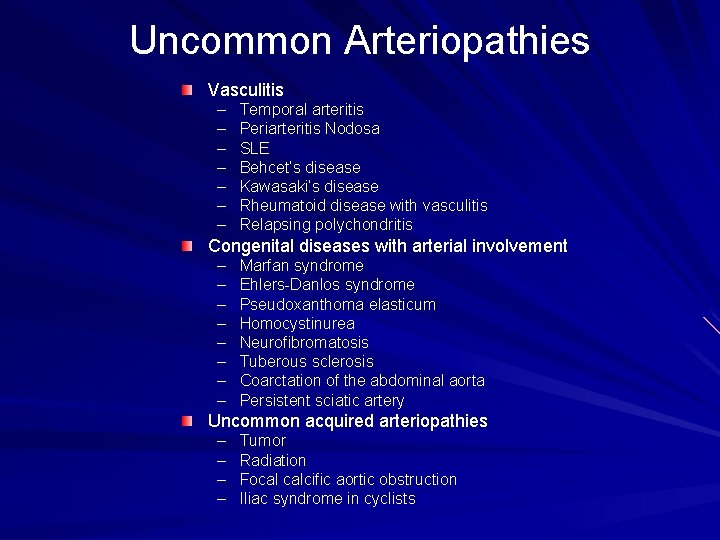
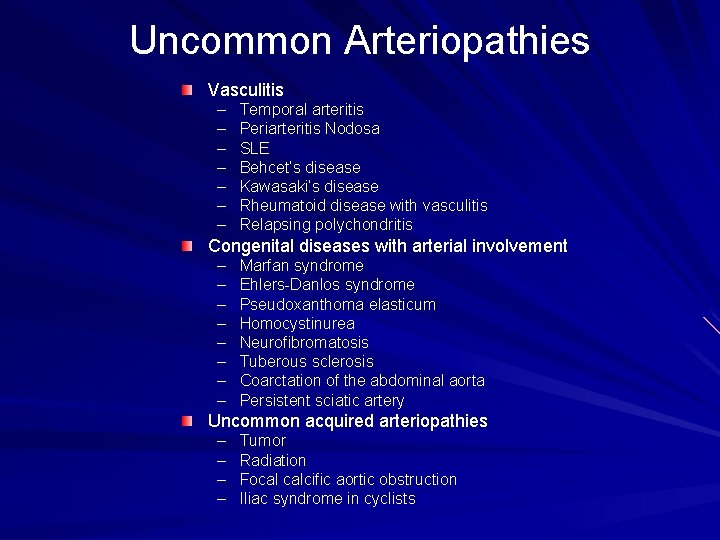
Uncommon Arteriopathies Vasculitis – – – – Temporal arteritis Periarteritis Nodosa SLE Behcet’s disease Kawasaki’s disease Rheumatoid disease with vasculitis Relapsing polychondritis Congenital diseases with arterial involvement – – – – Marfan syndrome Ehlers-Danlos syndrome Pseudoxanthoma elasticum Homocystinurea Neurofibromatosis Tuberous sclerosis Coarctation of the abdominal aorta Persistent sciatic artery Uncommon acquired arteriopathies – – Tumor Radiation Focal calcific aortic obstruction Iliac syndrome in cyclists
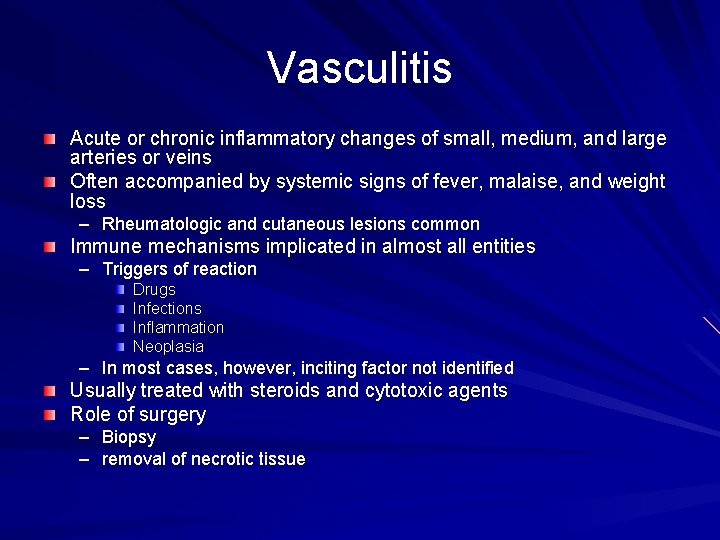
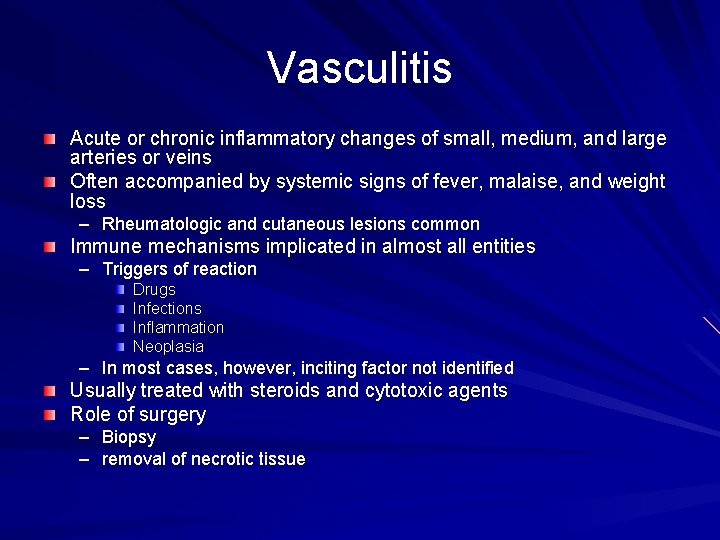
Vasculitis Acute or chronic inflammatory changes of small, medium, and large arteries or veins Often accompanied by systemic signs of fever, malaise, and weight loss – Rheumatologic and cutaneous lesions common Immune mechanisms implicated in almost all entities – Triggers of reaction Drugs Infections Inflammation Neoplasia – In most cases, however, inciting factor not identified Usually treated with steroids and cytotoxic agents Role of surgery – Biopsy – removal of necrotic tissue
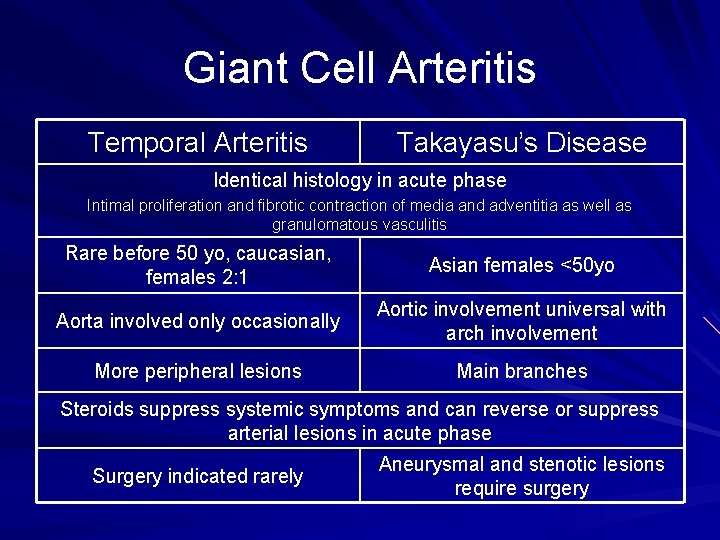
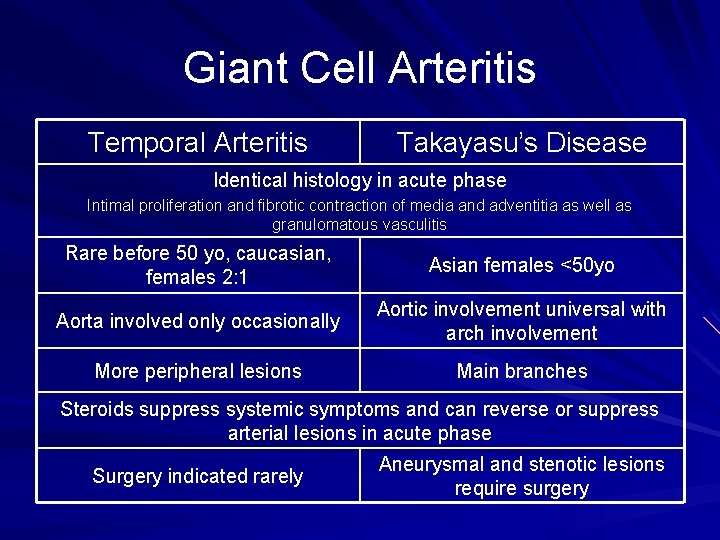
Giant Cell Arteritis Temporal Arteritis Takayasu’s Disease Identical histology in acute phase Intimal proliferation and fibrotic contraction of media and adventitia as well as granulomatous vasculitis Rare before 50 yo, caucasian, females 2: 1 Asian females <50 yo Aorta involved only occasionally Aortic involvement universal with arch involvement More peripheral lesions Main branches Steroids suppress systemic symptoms and can reverse or suppress arterial lesions in acute phase Surgery indicated rarely Aneurysmal and stenotic lesions require surgery
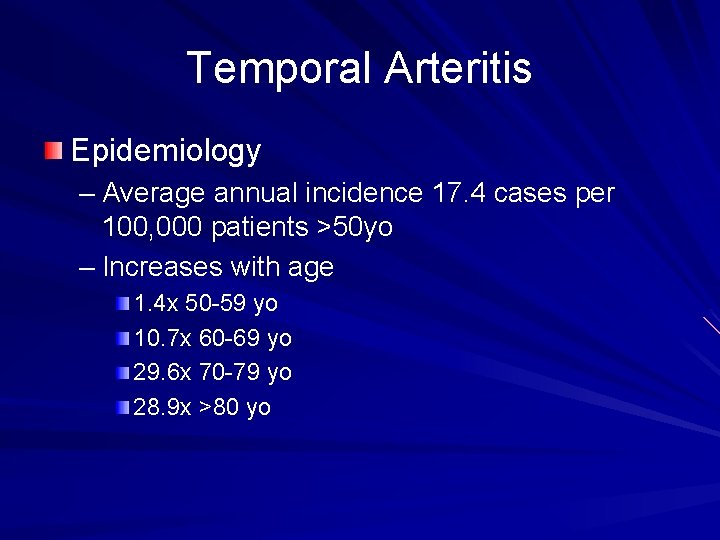
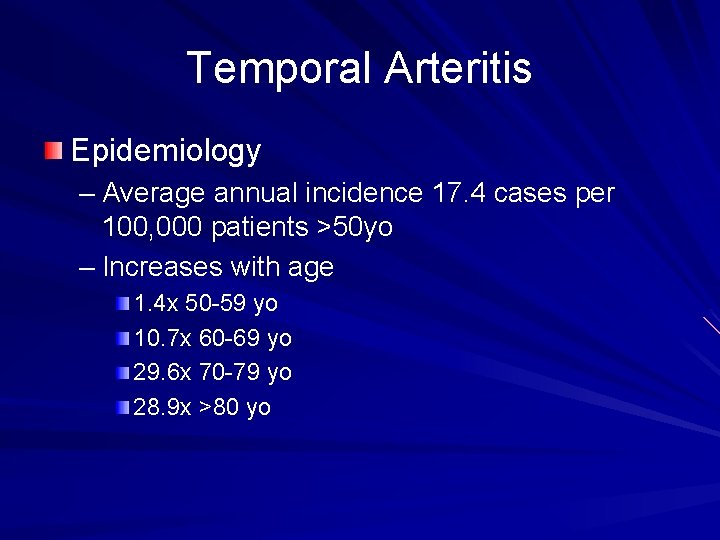
Temporal Arteritis Epidemiology – Average annual incidence 17. 4 cases per 100, 000 patients >50 yo – Increases with age 1. 4 x 50 -59 yo 10. 7 x 60 -69 yo 29. 6 x 70 -79 yo 28. 9 x >80 yo
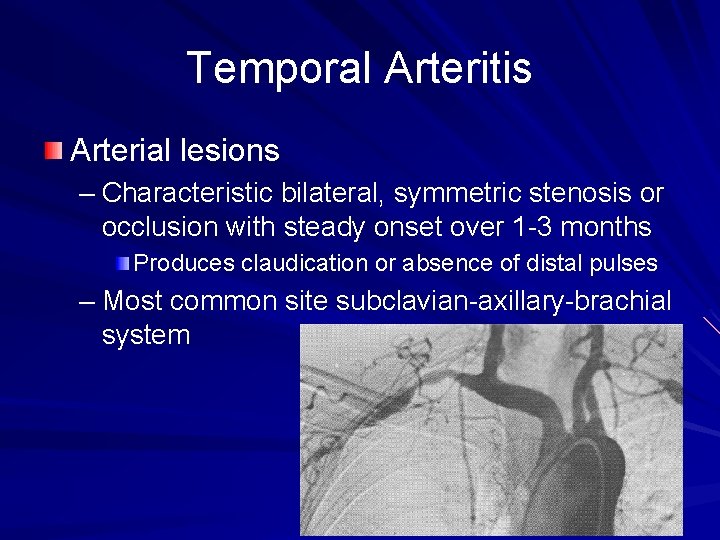
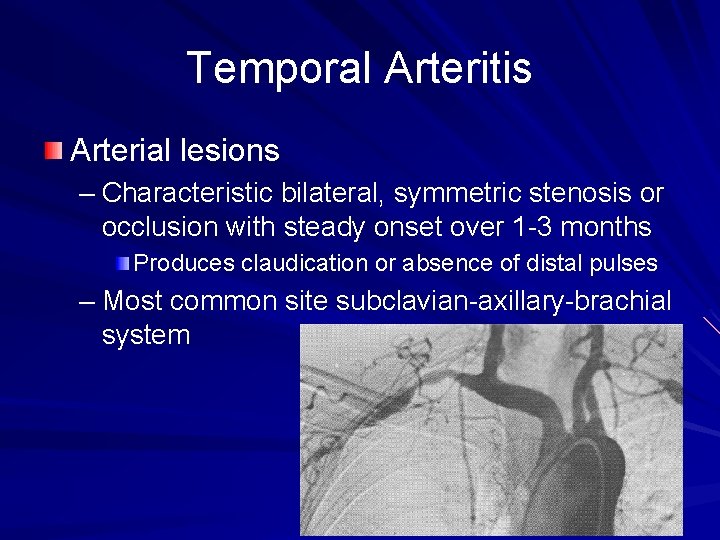
Temporal Arteritis Arterial lesions – Characteristic bilateral, symmetric stenosis or occlusion with steady onset over 1 -3 months Produces claudication or absence of distal pulses – Most common site subclavian-axillary-brachial system
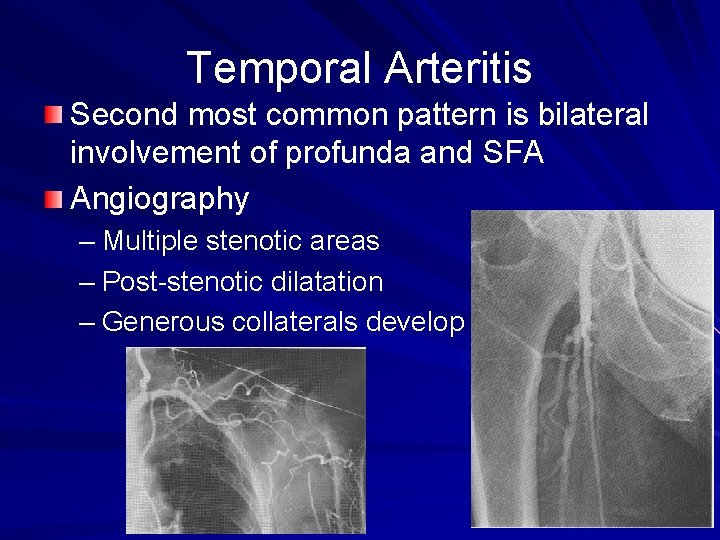
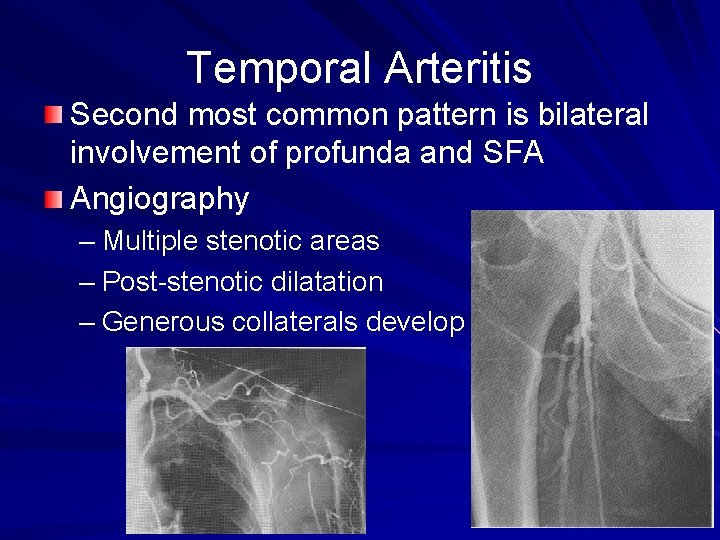
Temporal Arteritis Second most common pattern is bilateral involvement of profunda and SFA Angiography – Multiple stenotic areas – Post-stenotic dilatation – Generous collaterals develop
Temporal Arteritis Clinical picture – Typically begins with flu-like illness Malaise Fever Weight loss Scalp tenderness or headache – Symptoms intensify over 1 -3 weeks Tender, red, or elevated temporal/occipital arteries occurs in 45 -60% of patients Jaw claudication 2/3 of patients – Eye symptoms occur at about 3 months Blindness, amarosis, extraocular muscle dysfunction – Opthalmic, posterior ciliary, retinal vessels “prime medical emergency in opthamology” (Niederkohr et al, Opthamology 112: 744, 2005) – Large arteries involved 9 -14% Death caused by dissection, aneurysm rupture, MI, or stroke
Temporal Arteritis Laboratory Findings – Elevated ESR (40 -140) in active disease – Mild normocytic anemia – Mild leukocytosis and thrombocytosis Temporal Artery Biopsy – Outpatient procedure under local anesthesia 2 cm of vessel <0. 5% complication rate – 90 -99% sensitivity Ultrasound less reliable (Karassa et al, Ann Int Med 142: 359, 2005) – 60 -70% sensitivity – Dark halo around temporal artery lumen Therapy – Should not be delayed while awaiting biopsy If biopsy negative then withdraw steroids 60 mg/day prednisone, then tapered over subsequent weeks
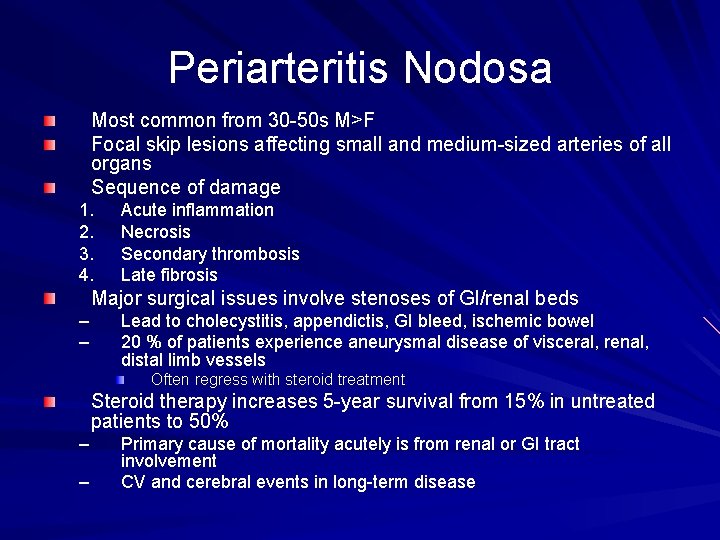
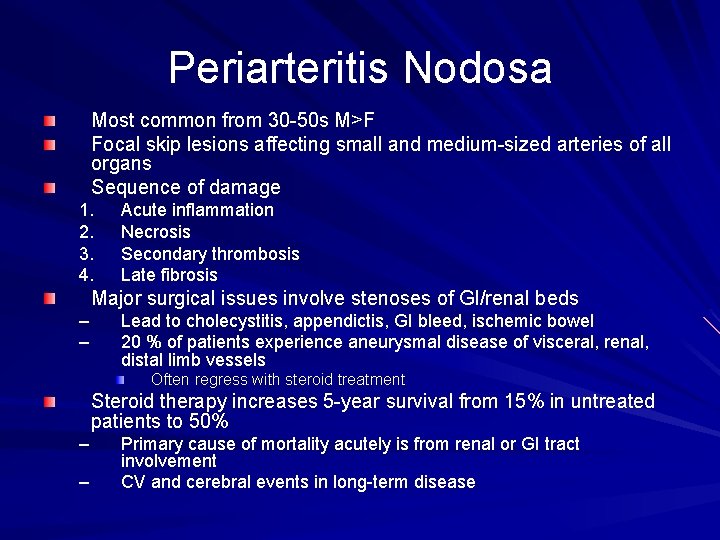
Periarteritis Nodosa Most common from 30 -50 s M>F Focal skip lesions affecting small and medium-sized arteries of all organs Sequence of damage 1. 2. 3. 4. Acute inflammation Necrosis Secondary thrombosis Late fibrosis Major surgical issues involve stenoses of GI/renal beds – – Lead to cholecystitis, appendictis, GI bleed, ischemic bowel 20 % of patients experience aneurysmal disease of visceral, renal, distal limb vessels Often regress with steroid treatment Steroid therapy increases 5 -year survival from 15% in untreated patients to 50% – – Primary cause of mortality acutely is from renal or GI tract involvement CV and cerebral events in long-term disease
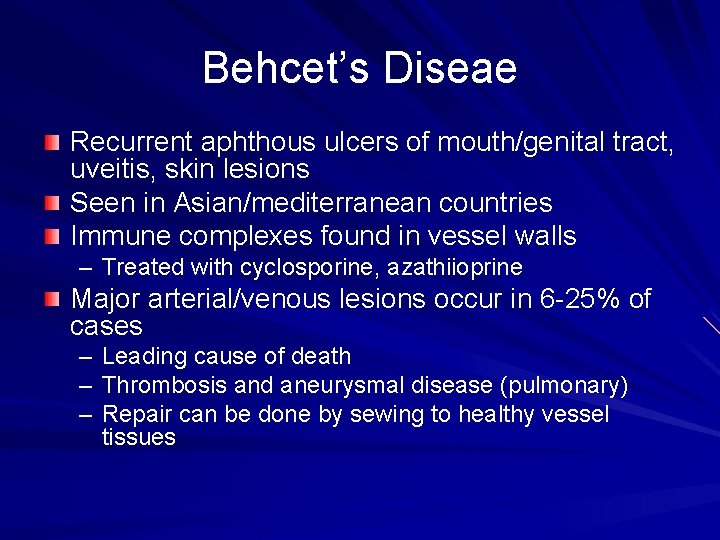
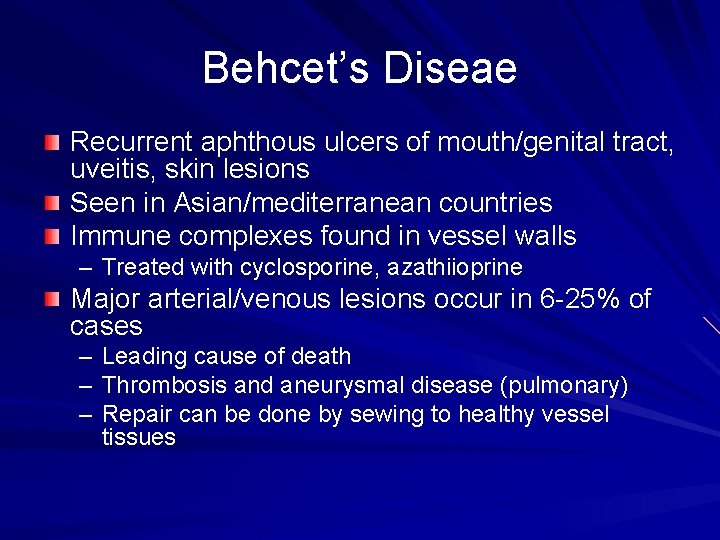
Behcet’s Diseae Recurrent aphthous ulcers of mouth/genital tract, uveitis, skin lesions Seen in Asian/mediterranean countries Immune complexes found in vessel walls – Treated with cyclosporine, azathiioprine Major arterial/venous lesions occur in 6 -25% of cases – Leading cause of death – Thrombosis and aneurysmal disease (pulmonary) – Repair can be done by sewing to healthy vessel tissues
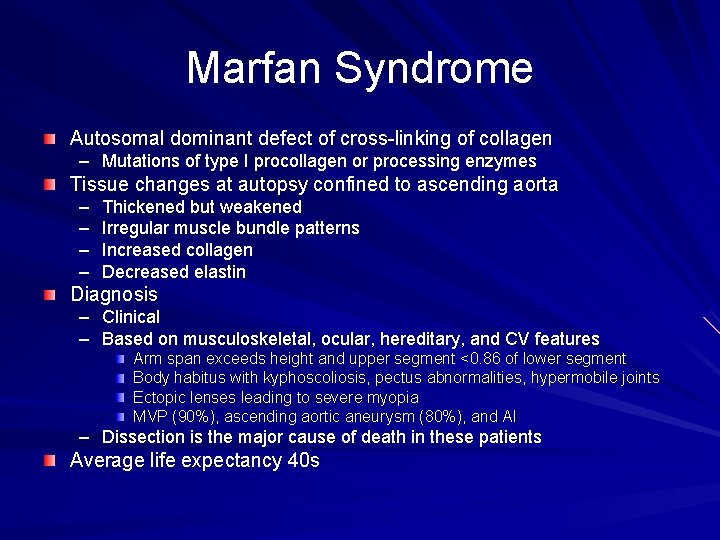
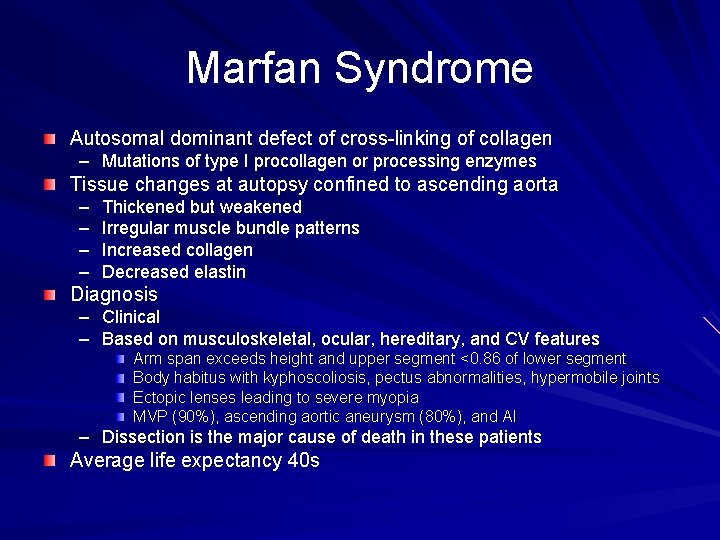
Marfan Syndrome Autosomal dominant defect of cross-linking of collagen – Mutations of type I procollagen or processing enzymes Tissue changes at autopsy confined to ascending aorta – – Thickened but weakened Irregular muscle bundle patterns Increased collagen Decreased elastin Diagnosis – Clinical – Based on musculoskeletal, ocular, hereditary, and CV features Arm span exceeds height and upper segment <0. 86 of lower segment Body habitus with kyphoscoliosis, pectus abnormalities, hypermobile joints Ectopic lenses leading to severe myopia MVP (90%), ascending aortic aneurysm (80%), and AI – Dissection is the major cause of death in these patients Average life expectancy 40 s
Marfan’s Syndrome Surgical Therapy – Ascending aortic issues Treated with resection and graft repair – Descending aorta involvement rare Medical therapy may be equal if end organ ischemia not present – Chronic disease (aneurysmal dilatation) Elective replacement at >6 cm Beta blocker therapy
Ehlers-Danlos Syndrome First described in 1682 Incidence 1: 150, 000 people, M=F Clinical characteristics – – Joint hypermobility Increased skin elasticity Easy bruising Abnormal scarring Wide splitting and gross ecchymoses “cigarette paper scars” 12 different types based on clinical presentation, genetics, and biochemical defects Autosomal dominant with incomplete penetrance – only 50% of cases have family history – Genetic defects lead to abnormal structure, synthesis, or secretion of type III collagen Leads to weakness of vessel walls with ruptures, dissections, or aneurysm formation
Type IV EDS Arterial defects rare and occur primarily in Type IV (4% of patients) Do not present with classic symptoms Clinical – – – Spontaneous colon perforations, splenic ruptures, uterine ruptures, PTX CVAs common Most patients unaware of disease until affected by catastrophic event Ruptured artery, dissection, aneurysm formation in patient in late 20 s – Can occur spontaneously or with minor trauma Cikrit et al JVS 5: 248, 1987 – – – Femoral-popliteal 27% Aortoiliac 25% Carotid, vertebral, subclavian, axillary 23% Visceral 17% Brachial/radial 6% Invasive diagnostic tests or monitoring should not be used – – – Large retroperitoneal hematomas simply from femoral venous catheters Arteriography has 67% complication rate including death Should use duplex, CT-A, MRA
Management of EDS Expectant until vascular event occurs – If bleeding is not active and limb is viable then conservative treatment with bedrest – Operative intervention should be avoided unless clearly necessary Simple exposure of vessels can be problematic Massive hemorrhage can occur due to friability Simple ligation with umbilical tape may be best option Bypasses can be reinforced with teflon pledgets – Fibrin glue High mortality with 44% of patients dying before intervention and 20% after – No cure – 90% of patients die before middle age from catastrophic vascular event
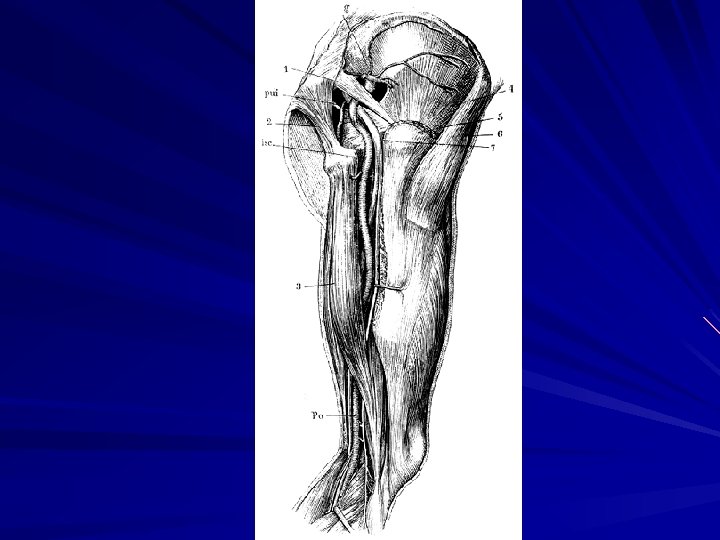
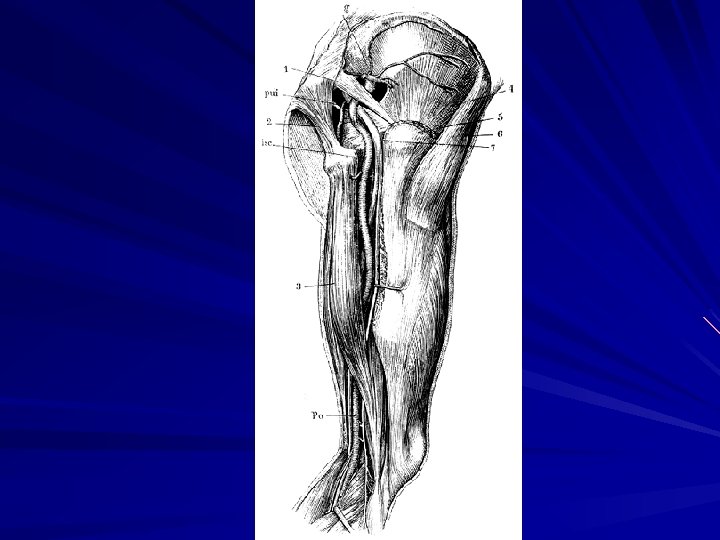
Persistent Sciatic Artery Fewer than 100 reported cases – Prevalence of 0. 25 per 1000 patients studied by angiography Embryology – Femoral plexus Supplied ventrally by hypogastric to evolve later into fem-pop system Supplied dorsally by axial artery to later regress to gluteal artery – Complete form of syndrome the sciatic vessel communicates directly with popliteal artery Creates paradox where femoral pulse is absent but distal pulses full “Cowie’s sign”
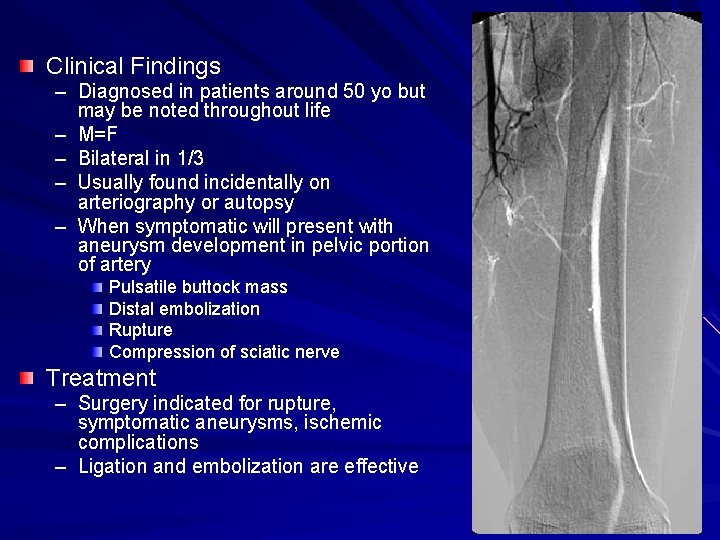
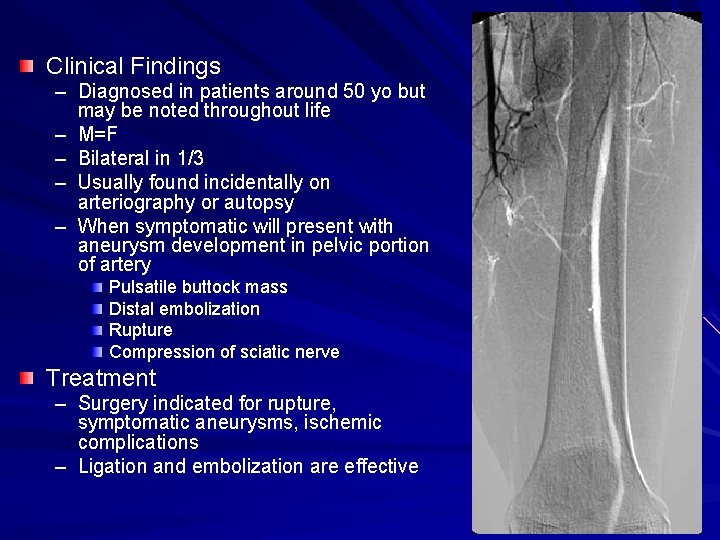
Clinical Findings – Diagnosed in patients around 50 yo but may be noted throughout life – M=F – Bilateral in 1/3 – Usually found incidentally on arteriography or autopsy – When symptomatic will present with aneurysm development in pelvic portion of artery Pulsatile buttock mass Distal embolization Rupture Compression of sciatic nerve Treatment – Surgery indicated for rupture, symptomatic aneurysms, ischemic complications – Ligation and embolization are effective
Uncommon Arteriopathies Vasculitis – – – – Temporal arteritis Periarteritis Nodosa SLE Behcet’s disease Kawasaki’s disease Rheumatoid disease with vasculitis Relapsing polychondritis Congenital diseases with arterial involvement – – – – Marfan syndrome Ehlers-Danlos syndrome Pseudoxanthoma elasticum Homocystinurea Neurofibromatosis Tuberous sclerosis Coarctation of the abdominal aorta Persistent sciatic artery Uncommon acquired arteriopathies – – Tumor Radiation Focal calcific aortic obstruction Iliac syndrome in cyclists