UMR Plan Advisor and Care Management Services Why





- Slides: 24
UMR - Plan Advisor and Care Management Services

Why are we here today? • As of 1/1/17, all member medical support is through UMR • UMR Plan Advisors are taking the place of Quantum Care Coordinators Same services are provided, just a new company and new phone number to contact on your new ID card • Enhancement to plan effective 1/1/17 No referrals required for Specialist visit or Physical Therapy session – but consult with your Primary Care Physician as you may need pre-authorization

UMR TOOLS, SERVICES AND PROGRAMS 3 © 2013 United Health. Care Services, Inc.
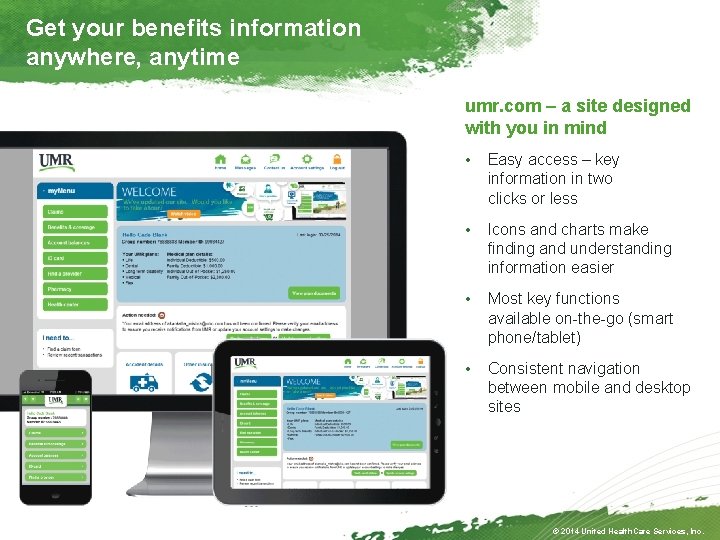
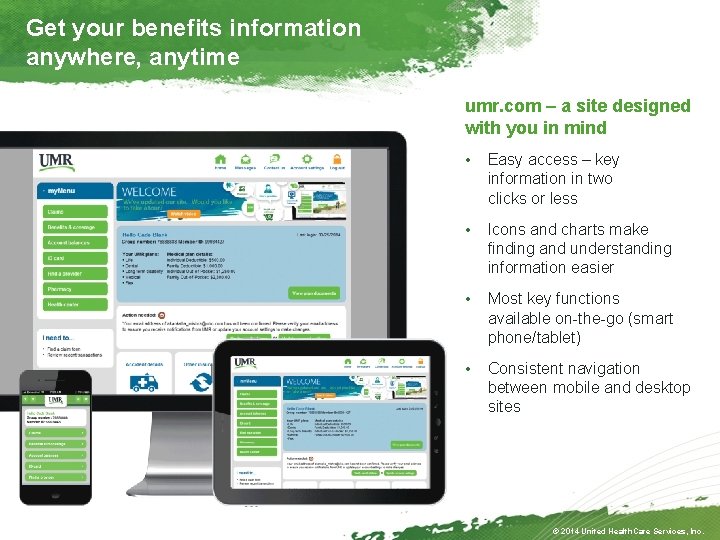
Get your benefits information anywhere, anytime umr. com – a site designed with you in mind • Easy access – key information in two clicks or less • Icons and charts make finding and understanding information easier • Most key functions available on-the-go (smart phone/tablet) • Consistent navigation between mobile and desktop sites © 2014 United Health. Care Services, Inc.
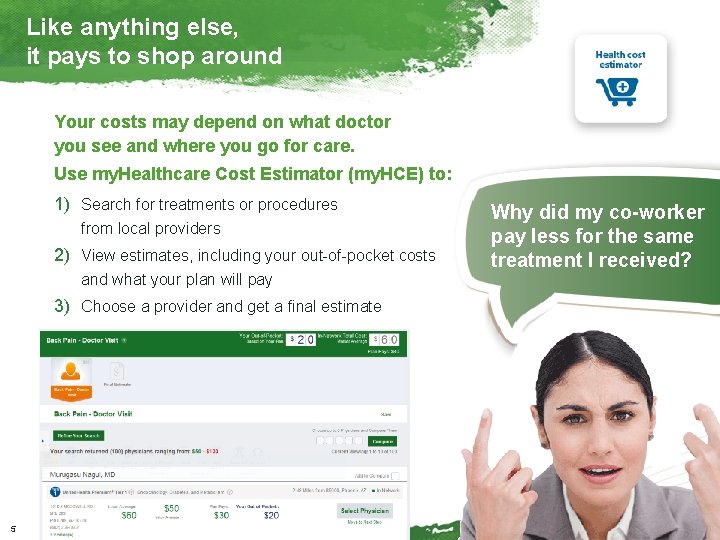
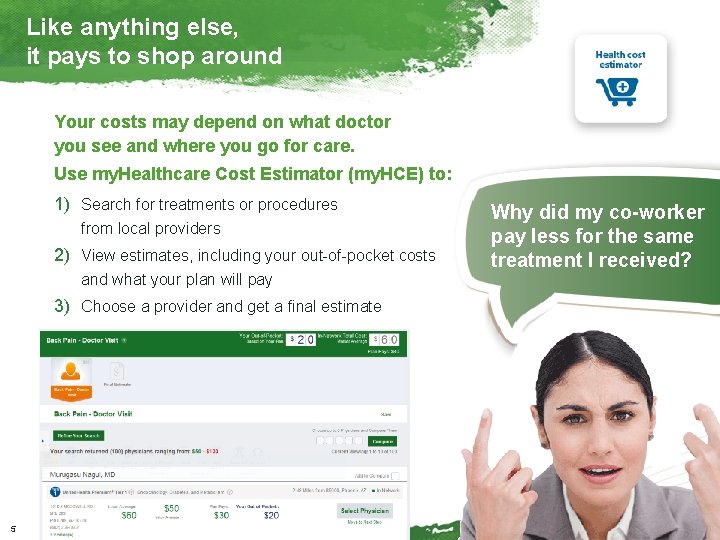
Like anything else, it pays to shop around Your costs may depend on what doctor you see and where you go for care. Use my. Healthcare Cost Estimator (my. HCE) to: 1) Search for treatments or procedures from local providers 2) View estimates, including your out-of-pocket costs and what your plan will pay Why did my co-worker pay less for the same treatment I received? 3) Choose a provider and get a final estimate 5 © 2013 United Health. Care Services, Inc.
UMR Plan Advisor 6 © 2011 United Health. Care Services, Inc.
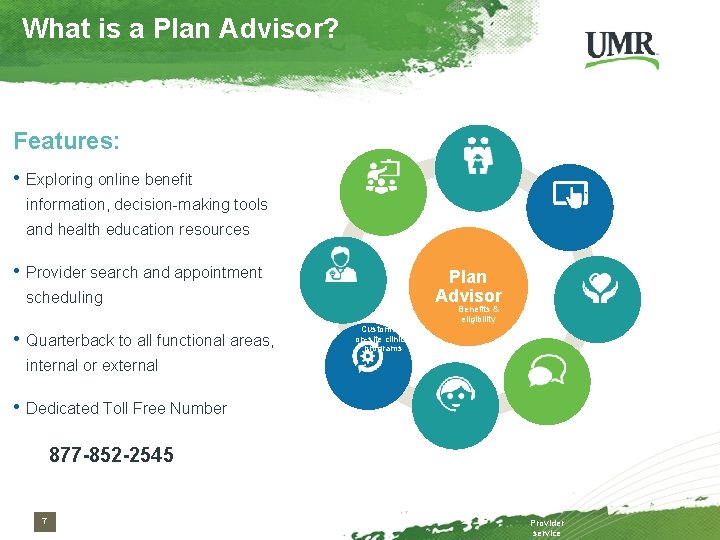
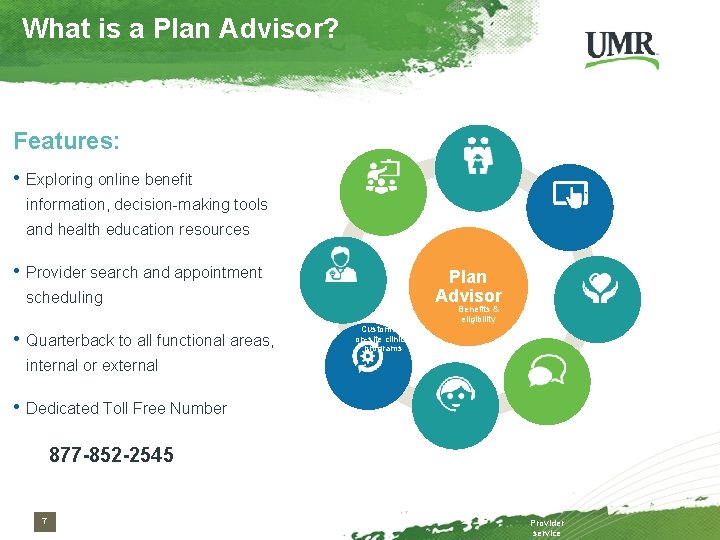
What is a Plan Advisor? Features: • Exploring online benefit information, decision-making tools and health education resources • Provider search and appointment Plan Advisor scheduling • Quarterback to all functional areas, Customer’s on-site clinical programs internal or external • Dedicated Toll Free Number Benefits & eligibility Web tools & education Primary Care referrals Care management 877 -852 -2545 7 Network Guidance Provider service

Enhanced customer service The advisor team is focused on member customer service. To that end, we expect calls to take longer. Core claim processing and provider calls are handled by other resources. 8
Case Management 9 © 2011 United Health. Care Services, Inc.
What is Case Management? UMR assigns a dedicated nurse case manager to situations including: • Catastrophic Events: Transplants, major trauma, premature infants, lengthy inpatient stays, complex/multiple levels of care • Events requiring intervention: Home infusion therapy, post-trauma rehab For the purpose of: • Negotiate out of network services • Propose alternative treatment plans/levels of care, as requested • Coordinate with local resources and EAPs • Educate employees and family members Case Management outreach and related services are always voluntary, but participation is highly beneficial.
Disease Management and Healthe. Notes

We can help you control your symptoms… UMR’s disease management program helps members with: • Asthma (adults and children) • Diabetes (adults and children) • Hypertension (high blood pressure) • Chronic obstructive pulmonary disease What if I have a chronic medical condition? (COPD) • Coronary artery disease • Heart failure • Depression (when occurring with one of the other listed conditions) Educational materials on this program were sent to home addresses in early January 12 © 2013 United Health. Care Services, Inc.
Member Experience • Enrollment specialist will contact the member via telephone to schedule the initial appointment with a Nurse health coach or member can self-enroll • Member agrees to enroll and schedules initial session • Members will schedule regular telephonic appointments to discuss their progress over a period of time • Members also receive educational materials, web tools and a quarterly newsletter © 2011 United Health. Care Services, Inc.

Rewards for participation Sign up and earn a $100 reward card: To qualify, you must: • Have one of the chronic conditions • Enroll in the program • Agree to complete an initial To enroll, self- refer on UMR. com or call your plan advisor: 877 -852 -2545 assessment • Participate in at least two followup calls with your personal RN coach 14 © 2013 United Health. Care Services, Inc.
Healthe. Notes • Personalized, targeted communications designed to improve health, encourage compliance, and highlight savings opportunities – Identify care opportunities – Provide patients with valuable info – Improve the overall health of the member population by providing actionable opportunities 15 © 2011 United Health. Care Services, Inc.
Maternity Management 16 © 2011 United Health. Care Services, Inc.
Member Experience • Member either self enrolls via the internet or phone – Enrollment must be in either the first or second trimester to qualify for the incentive • Welcome packet sent to member – Member can choose from five pregnancy books • Member & nurse schedule regular calls – minimum of 1 call per trimester • Post-partum call after the delivery • Member receives satisfaction survey • $25 gift card mailed to member © 2011 United Health. Care Services, Inc.
Member Experience Book Selections NEW : Additional supportive programming: Pre-pregnancy and Loss of Pregnancy © 2011 United Health. Care Services, Inc.
Nurse. Line / Nurse. Chat 19 © 2011 United Health. Care Services, Inc.
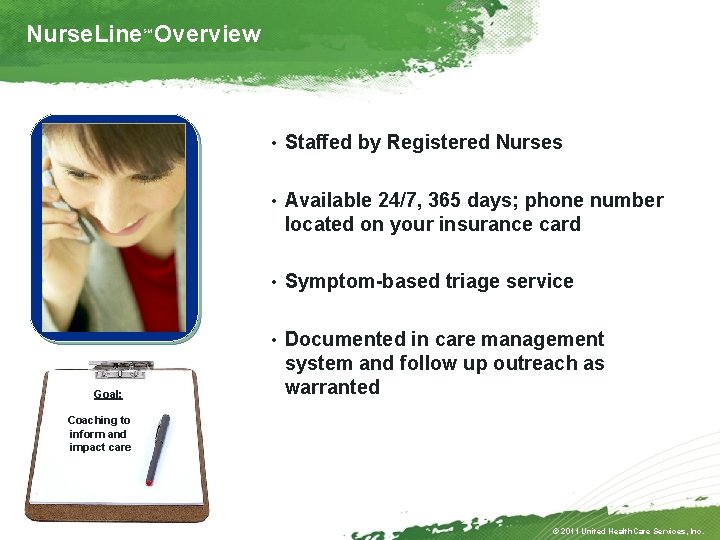
Nurse. Line Overview SM • Staffed by Registered Nurses • Available 24/7, 365 days; phone number located on your insurance card • Symptom-based triage service • Documented in care management Goal: system and follow up outreach as warranted Coaching to inform and impact care © 2011 United Health. Care Services, Inc.
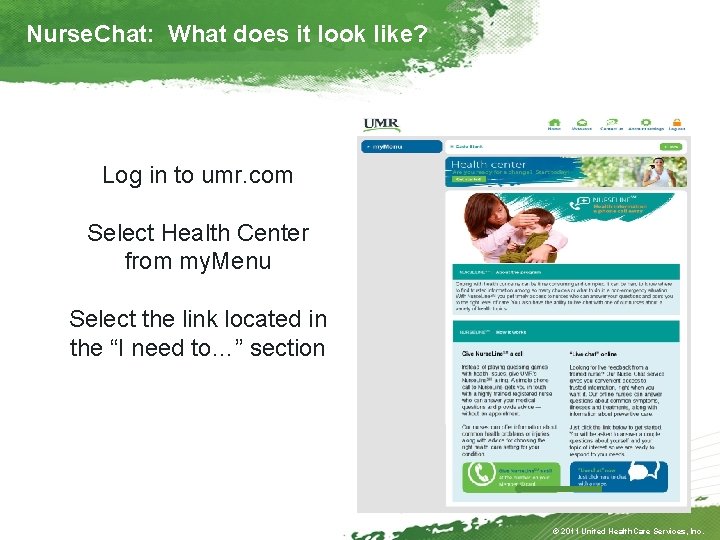
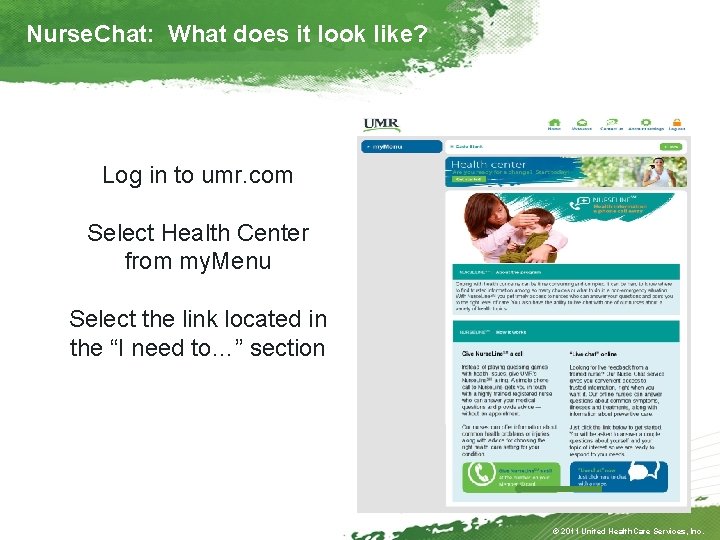
Nurse. Chat: What does it look like? Log in to umr. com Select Health Center from my. Menu Select the link located in the “I need to…” section © 2011 United Health. Care Services, Inc.
Treatment Decision Support 22 © 2011 United Health. Care Services, Inc.
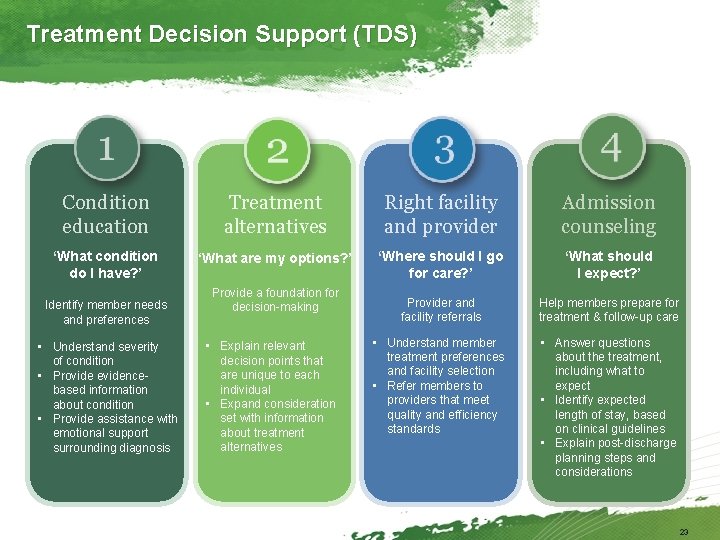
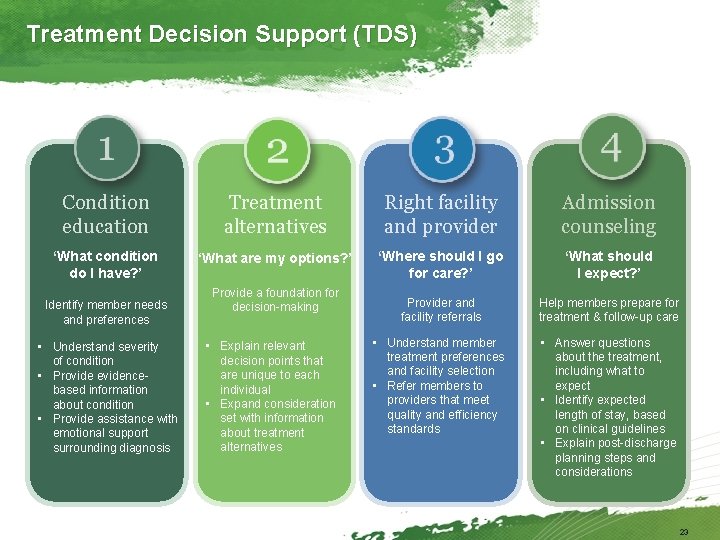
Treatment Decision Support (TDS) Condition education Treatment alternatives Right facility and provider Admission counseling ‘What condition do I have? ’ ‘What are my options? ’ ‘Where should I go for care? ’ ‘What should I expect? ’ Provider and facility referrals Help members prepare for treatment & follow-up care • Understand member treatment preferences and facility selection • Refer members to providers that meet quality and efficiency standards • Answer questions about the treatment, including what to expect • Identify expected length of stay, based on clinical guidelines • Explain post-discharge planning steps and considerations Identify member needs and preferences • Understand severity of condition • Provide evidencebased information about condition • Provide assistance with emotional support surrounding diagnosis Provide a foundation for decision-making • Explain relevant decision points that are unique to each individual • Expand consideration set with information about treatment alternatives 23
In Closing… Flyers available electronically on the One-Foth Homepage>Member Resources>Benefits or www. foth. com/benefits. Plan Advisor: 877 -852 -2545 Thank you for your time and attention! 24