Ultrafiltration Control using Hematocrit Monitoring 2013 ANNA North

- Slides: 19
Ultrafiltration Control using Hematocrit Monitoring 2013 ANNA North Carolina Statewide Symposium and the Southeastern Kidney Council NC Annual Meeting “Unique Challenges for the Nephrology Professional” Kimberly F. Clarkson, MSN, RN, CNN May 22, 2013
Objectives • Describe blood volume monitoring • Identify trend and graph development during hemodialysis • Evaluate nursing assessment considerations to decrease intradialytic mortality
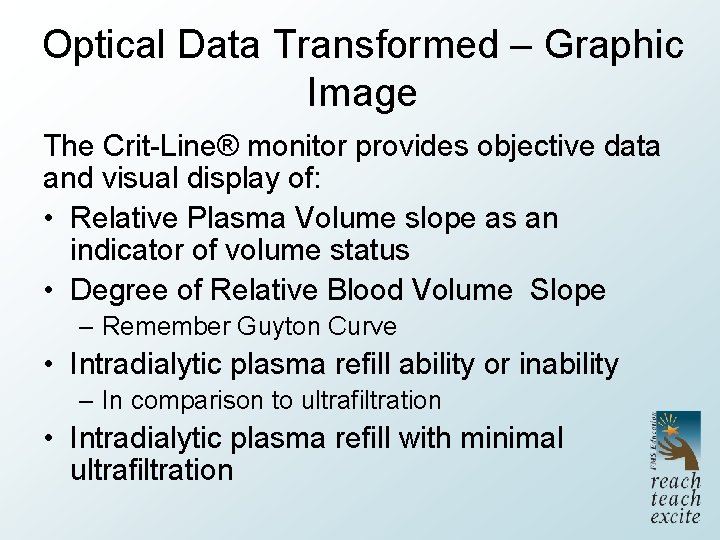
Relative Blood Volume Monitoring • Measures hematocrit in arterial blood – Crit-Line® Technology • Optical transmission detecting blood volume changes – Blood volume change – surrogate marker for vascular refilling – Increase in hematocrit relative to decrease in fluid removal • Interface display of changes • Affords a “window” into intravascular space Davenport, 2009
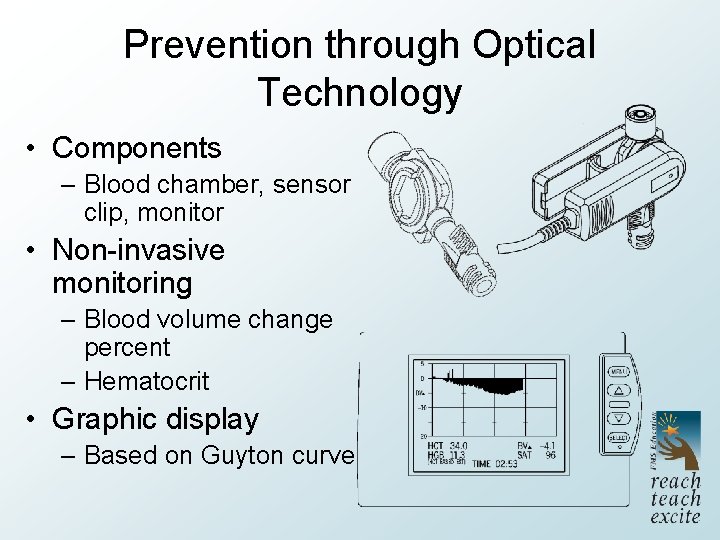
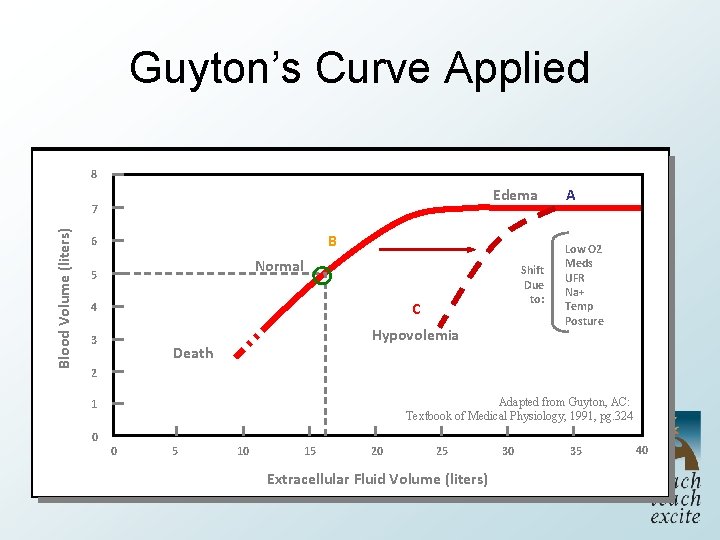
Prevention through Optical Technology • Components – Blood chamber, sensor clip, monitor • Non-invasive monitoring – Blood volume change percent – Hematocrit • Graphic display – Based on Guyton curve
Guyton’s Curve • Dr. Guyton (September 8, 1919 - April 3, 2003) – Physiologist; primarily circulatory system – Cardiac output related to peripheral circulation – Demonstrated oxygen demand regulated cardiac output • Overturned previous conventional wisdom – Heart itself does not control output – Developed graphic representation • Fundamental base in medical school • Guyton Curve Hall, 2003
Fluid Volume Distribution • Volume distribution; 70 kilogram male example – Intracellular • Approximately 23 L – Extracellular • Approximately 17 L – Intravascular • Approximately 5 L; cannot accommodate > 7 L
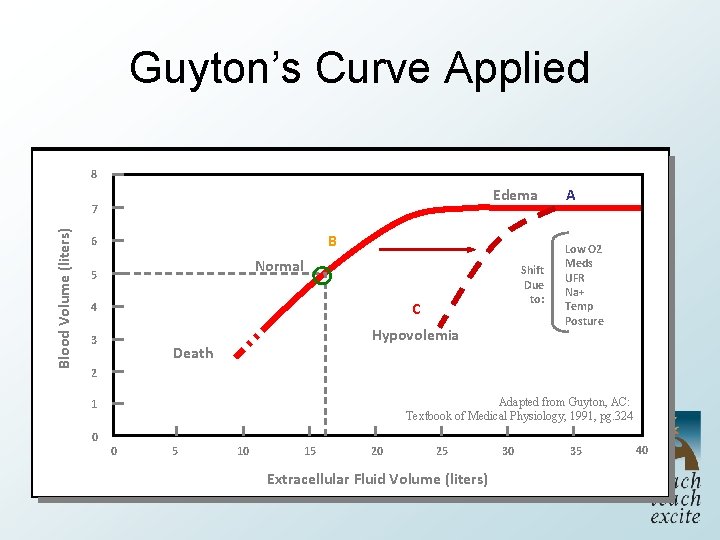
Guyton’s Curve Applied 8 8 Edema Blood. Volume (liters) Blood 7 7 6 6 B Normal 55 Shift Due to: 4 4 C 3 3 Hypovolemia Death 2 2 Low O 2 Meds UFR Na+ Temp Posture Adapted from Guyton, AC: Textbook of Medical Physiology, 1991, pg. 324 1 1 00 A 0 0 55 10 10 15 15 20 20 25 25 Extracellular Fluid Volume (liters) Extracellular 30 30 35 35 40 40
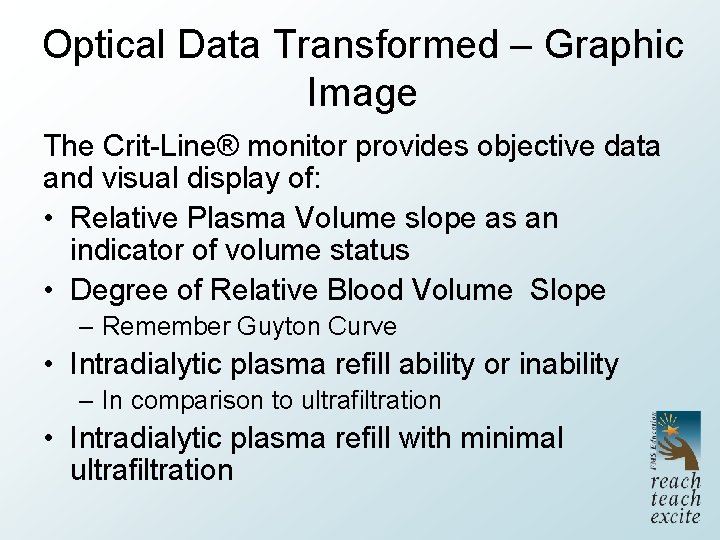
Optical Data Transformed – Graphic Image The Crit-Line® monitor provides objective data and visual display of: • Relative Plasma Volume slope as an indicator of volume status • Degree of Relative Blood Volume Slope – Remember Guyton Curve • Intradialytic plasma refill ability or inability – In comparison to ultrafiltration • Intradialytic plasma refill with minimal ultrafiltration
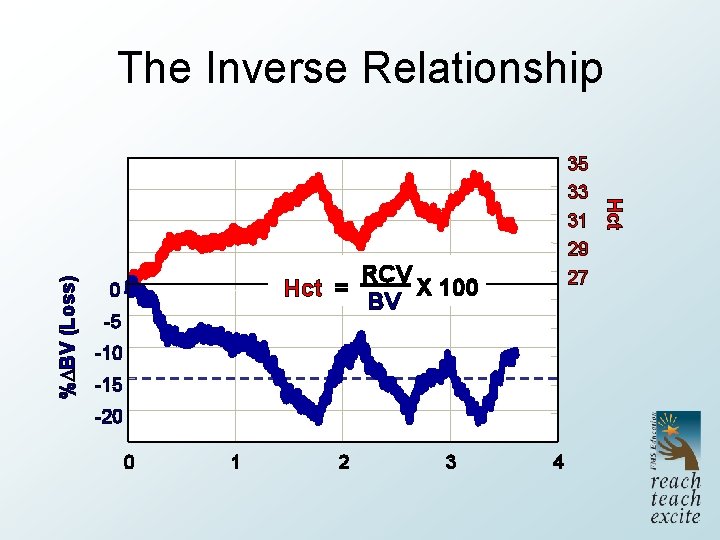
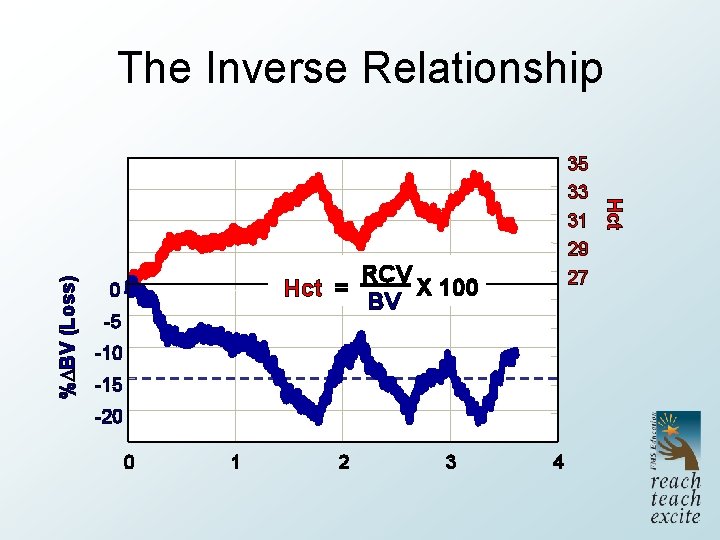
35 33 31 29 27 RCV X 100 Hct = BV 0 -5 -10 -15 -20 0 1 2 3 4 Hct % BV (Loss) The Inverse Relationship
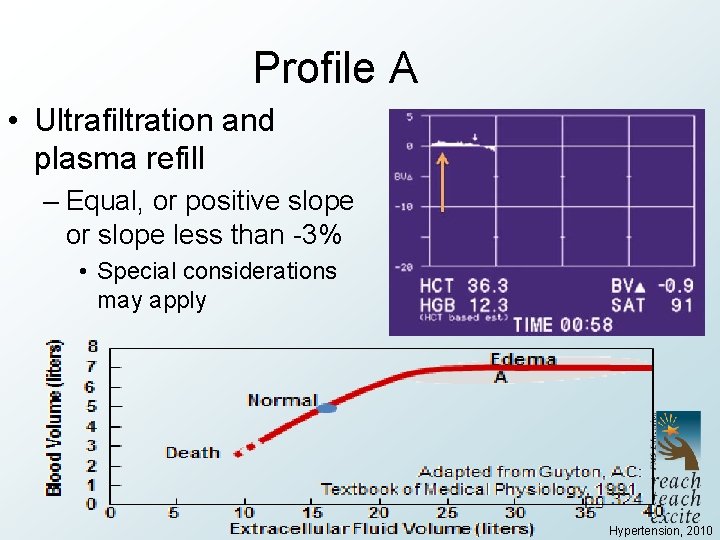
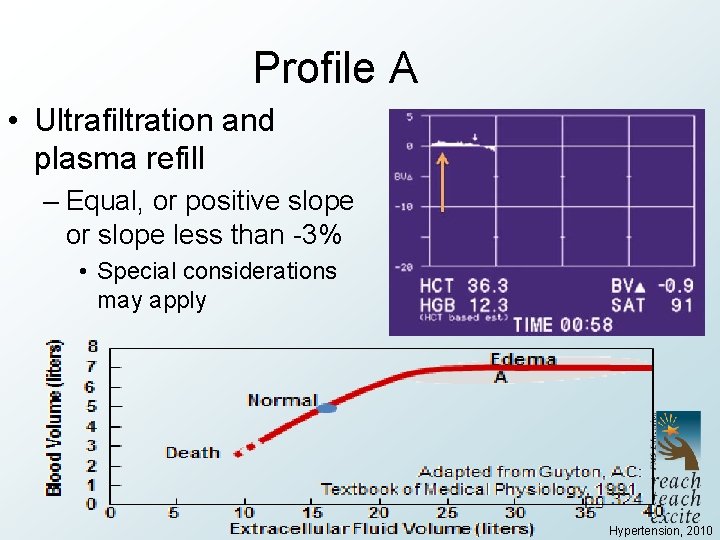
Profile A • Ultrafiltration and plasma refill – Equal, or positive slope or slope less than -3% • Special considerations may apply Hypertension, 2010
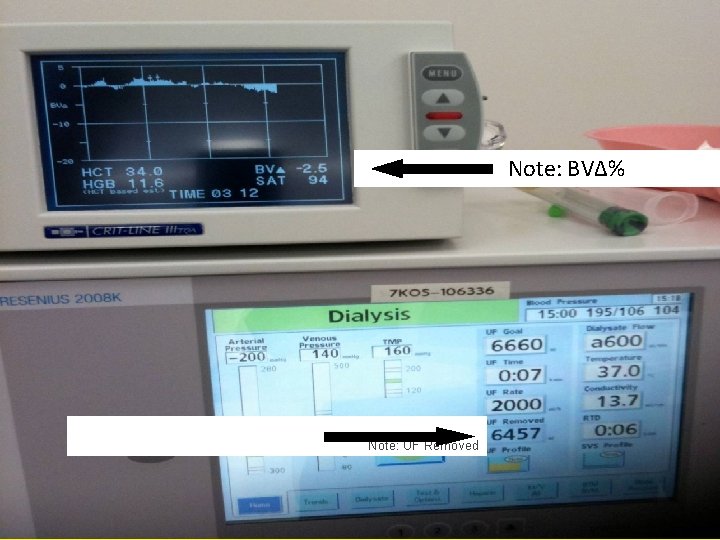
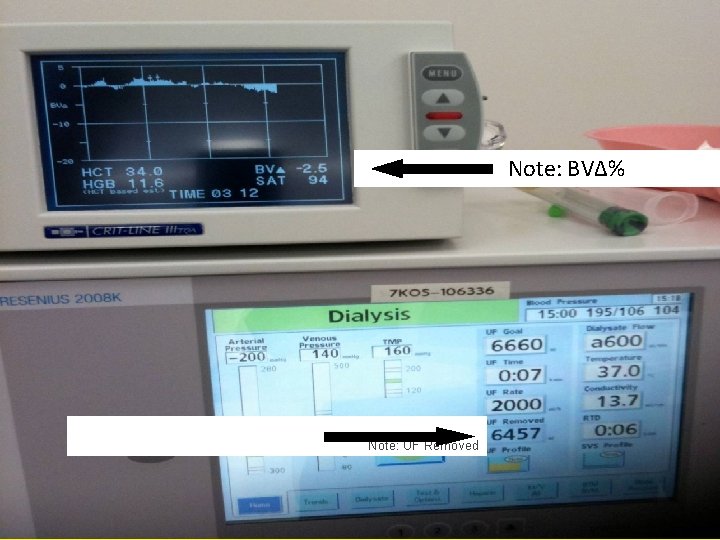
Note: BV∆% Note: UF Removed RPV Principles 11
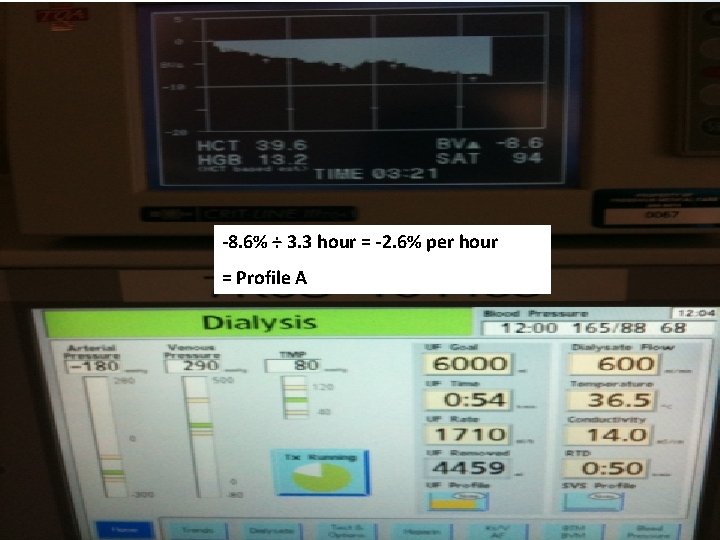
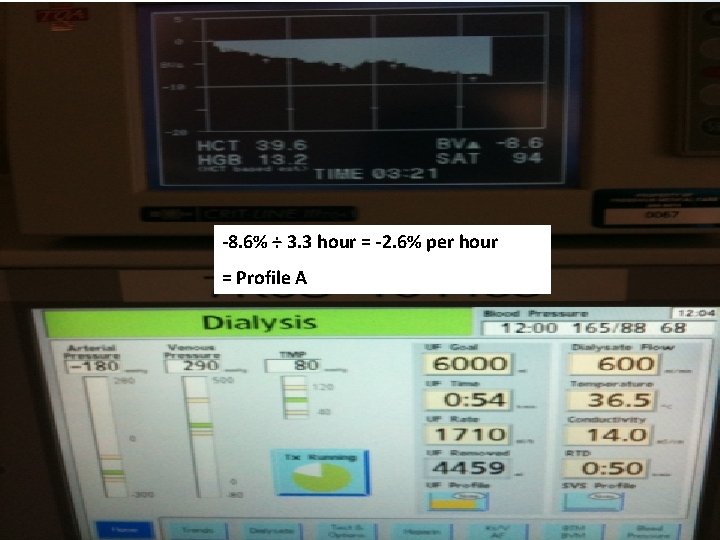
-8. 6% ÷ 3. 3 hour = -2. 6% per hour = Profile A RPV Principles 12
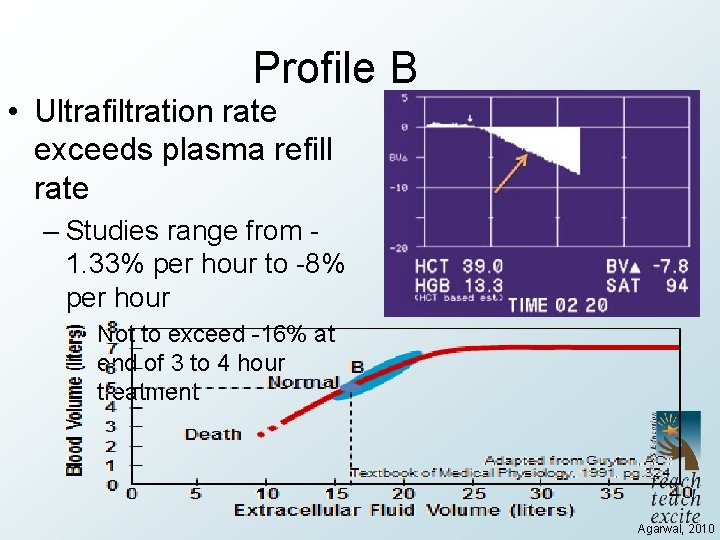
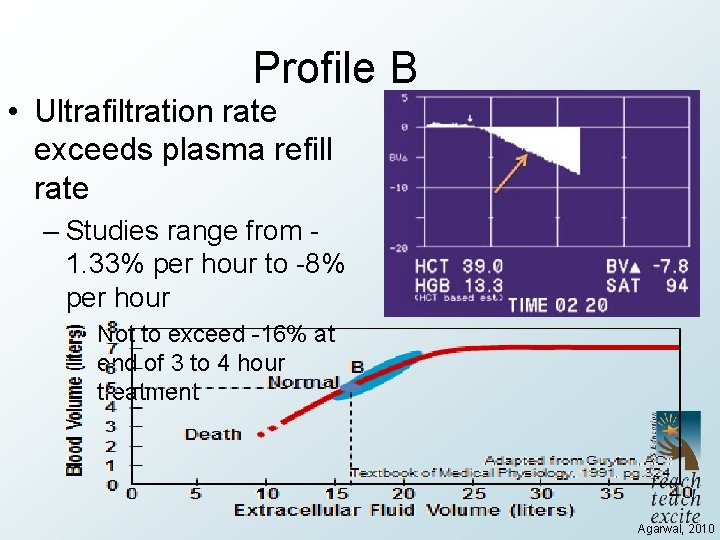
Profile B • Ultrafiltration rate exceeds plasma refill rate – Studies range from 1. 33% per hour to -8% per hour • Not to exceed -16% at end of 3 to 4 hour treatment Agarwal, 2010
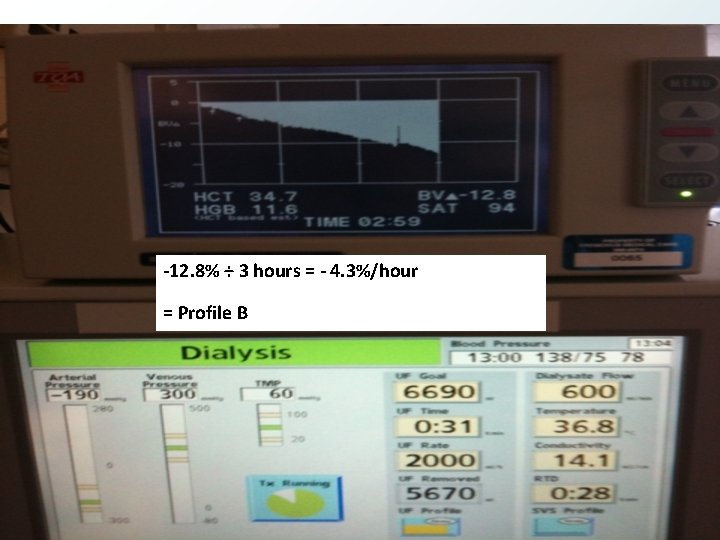
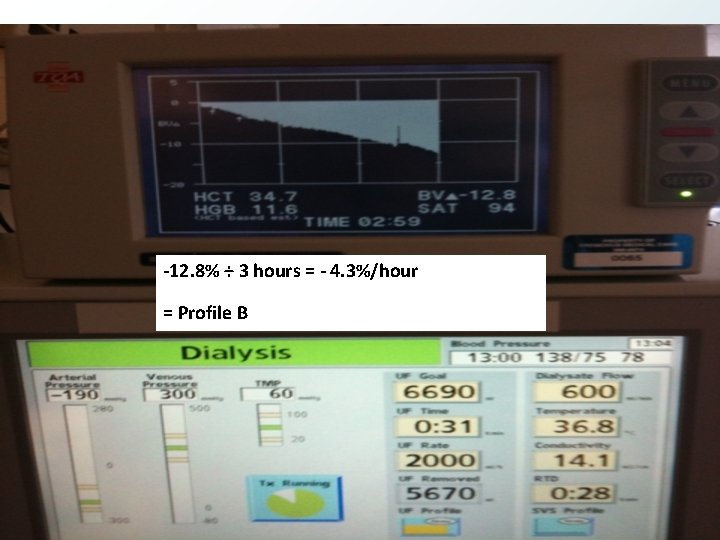
-12. 8% ÷ 3 hours = - 4. 3%/hour = Profile B RPV Principles 14
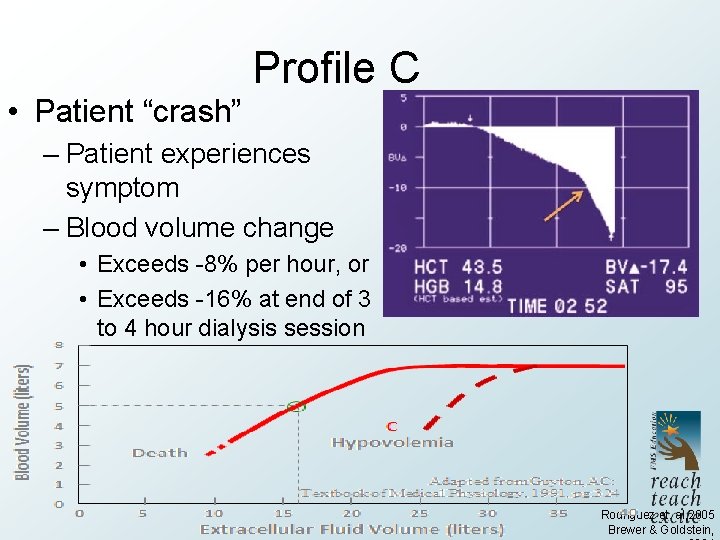
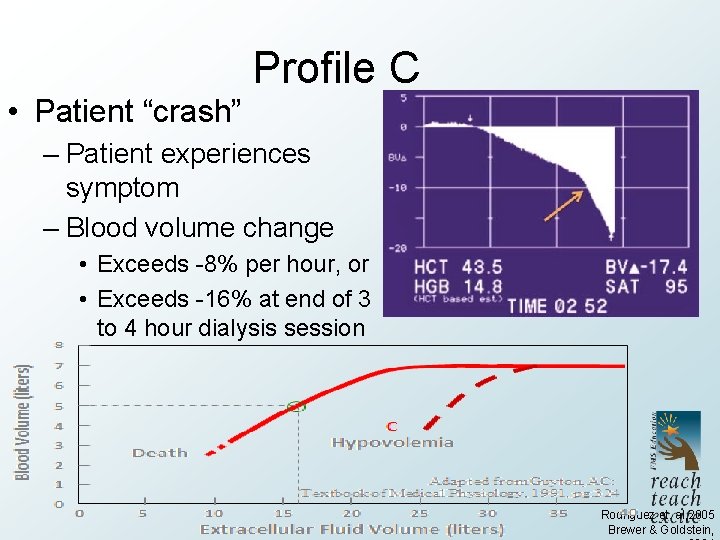
Profile C • Patient “crash” – Patient experiences symptom – Blood volume change • Exceeds -8% per hour, or • Exceeds -16% at end of 3 to 4 hour dialysis session Rodriguez et. al, 2005 Brewer & Goldstein,
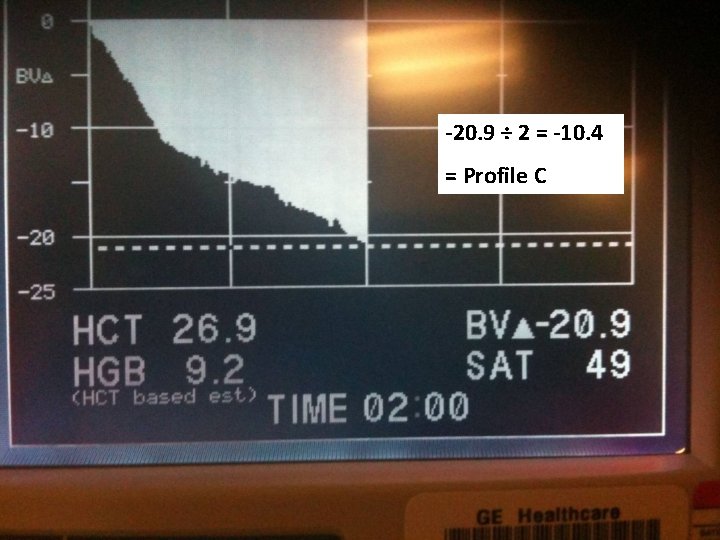
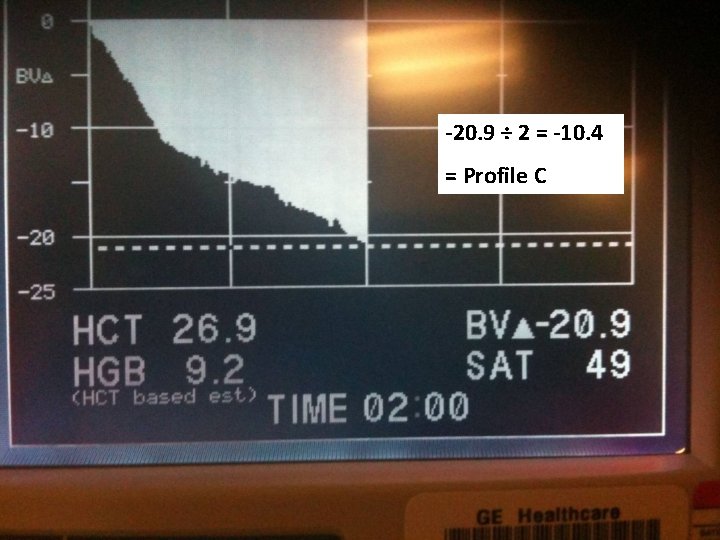
-20. 9 ÷ 2 = -10. 4 = Profile C RPV Principles 16

Prevent Treatment Complications E – Electrolytes V – Volume removed–ultrafiltration A – Anemia/albumin/allergies L – Lying back, feet on floor – position U – Urinary output A – Anti-hypertensives or other meds T – Temperature I – Ideal dry weight O – Oxygenation of tissues N – Nurse responsibility
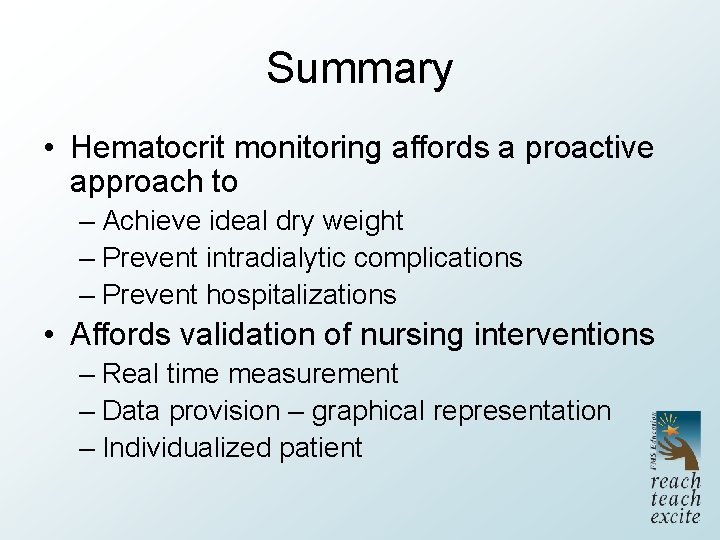
Summary • Hematocrit monitoring affords a proactive approach to – Achieve ideal dry weight – Prevent intradialytic complications – Prevent hospitalizations • Affords validation of nursing interventions – Real time measurement – Data provision – graphical representation – Individualized patient
References