Ulcerative Colitis Definition It is a recurrent ulcerative


- Slides: 20
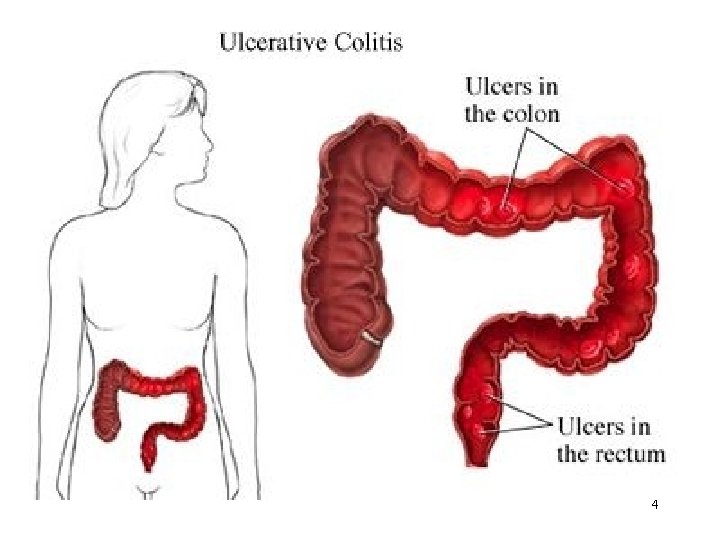
Ulcerative Colitis Definition It is a recurrent ulcerative and inflammatory disease of the mucosal layer of the colon and rectum. It is a serious disease systemic complications high mortality rate Incidence Peak – 30 to 50 years of age Pathophysiology Affects the superficial mucosa of the colon 1 multiple ulcerations
Diffuse inflammation, desquamation of the colonic epithelium Ulcers may bleed Lesions are continuous Disease begins in the rectum and may involve the entire colon The bowel narrows shortens and thickens because of muscular hypertrophy and fat deposits The inflammation may spread into the muscularis, inhibiting its ability to contract toxic megacolon distension of the colon 2
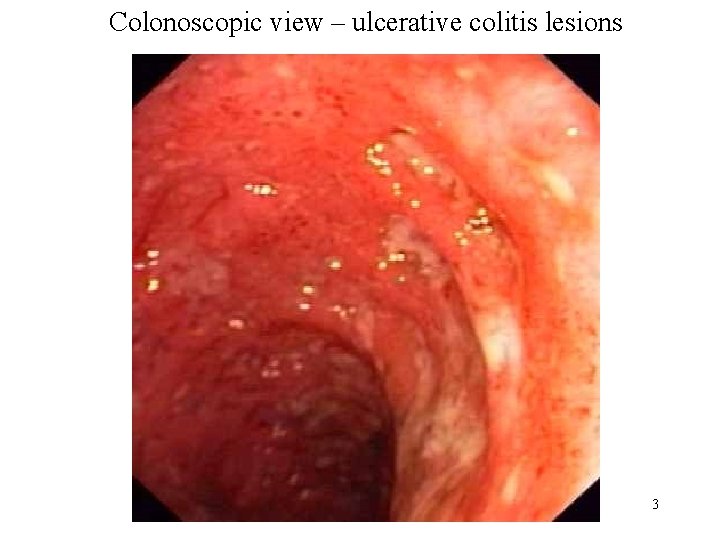
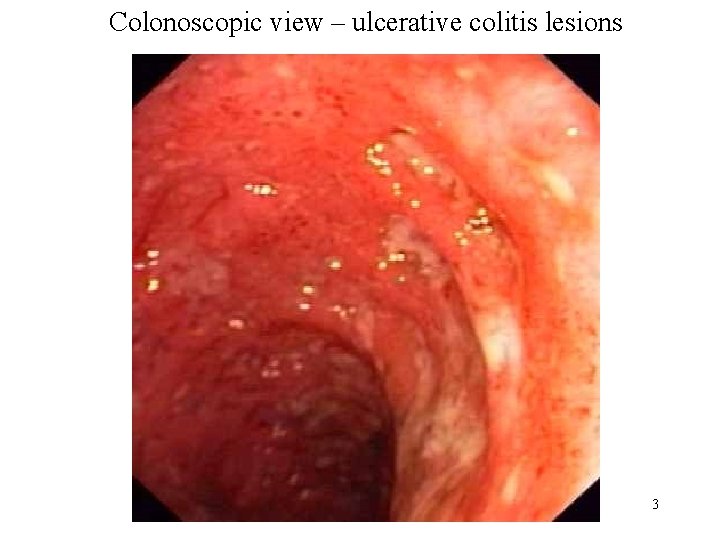
Colonoscopic view – ulcerative colitis lesions 3
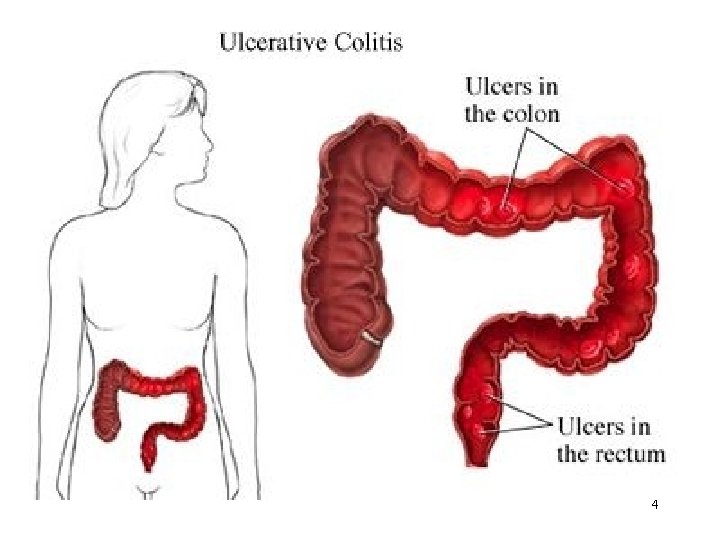
4
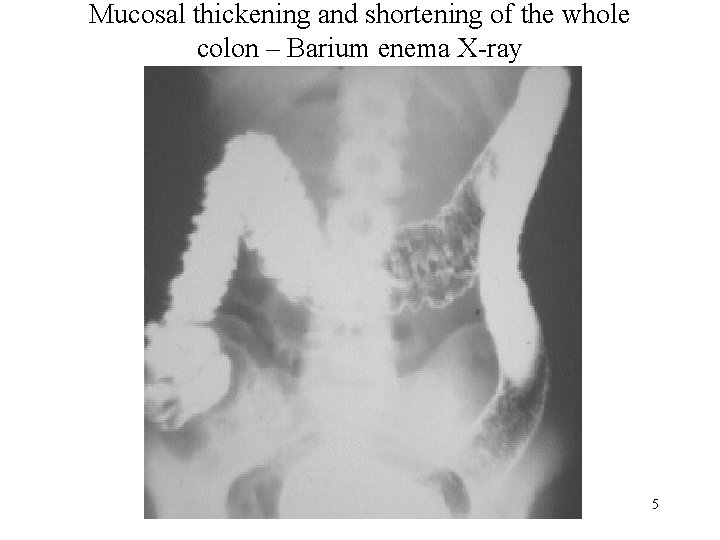
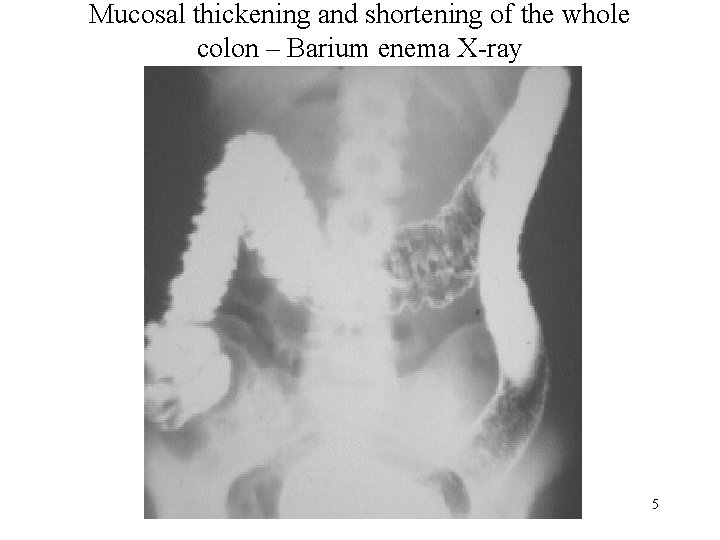
Mucosal thickening and shortening of the whole colon – Barium enema X-ray 5
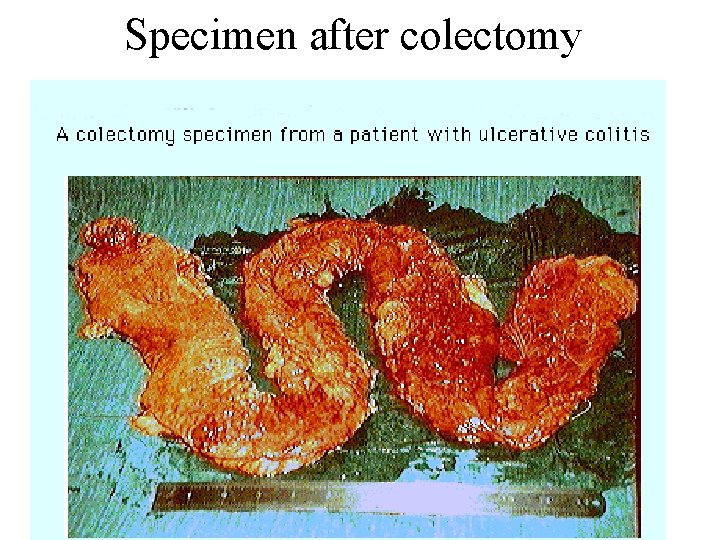
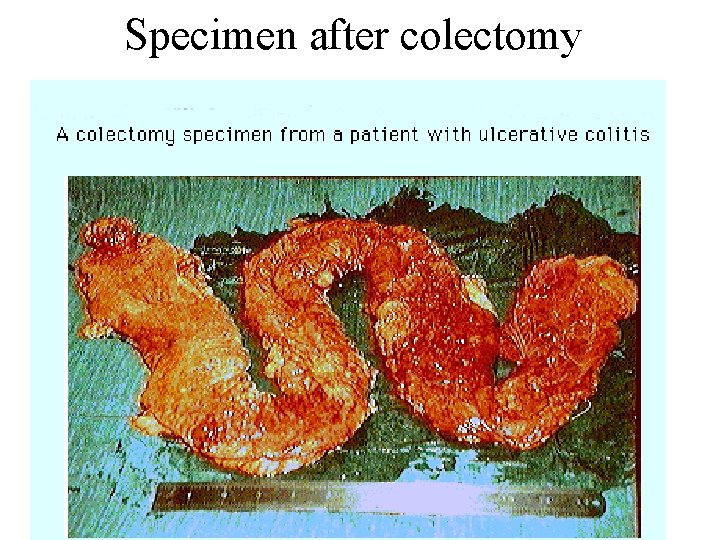
Specimen after colectomy 6
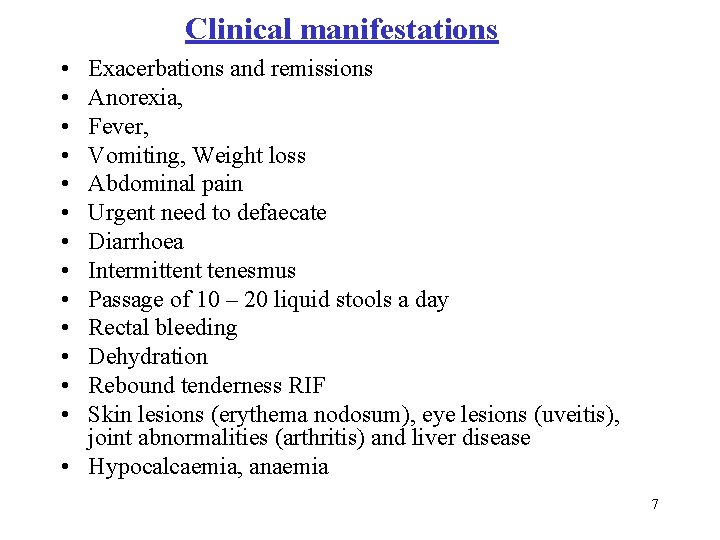
Clinical manifestations • • • • Exacerbations and remissions Anorexia, Fever, Vomiting, Weight loss Abdominal pain Urgent need to defaecate Diarrhoea Intermittent tenesmus Passage of 10 – 20 liquid stools a day Rectal bleeding Dehydration Rebound tenderness RIF Skin lesions (erythema nodosum), eye lesions (uveitis), joint abnormalities (arthritis) and liver disease • Hypocalcaemia, anaemia 7
Investigations • Hb – may be low • TC – raised • ESR – raised • Albumin level – low • Electrolyte imbalance + • Sigmoidoscopy • Barium enema Mucosal inflammation, friability, exudate and ulcerations 8
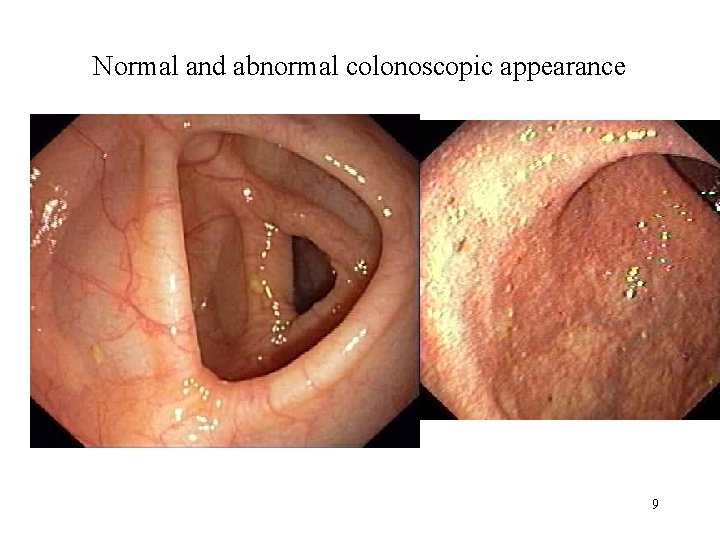
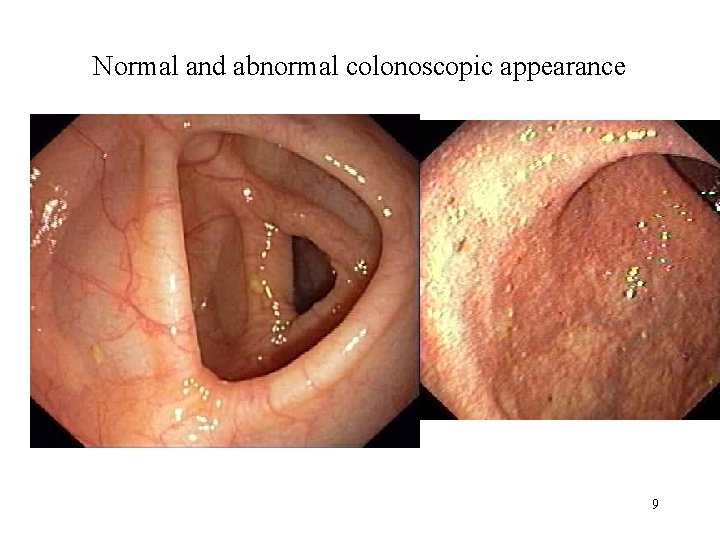
Normal and abnormal colonoscopic appearance 9
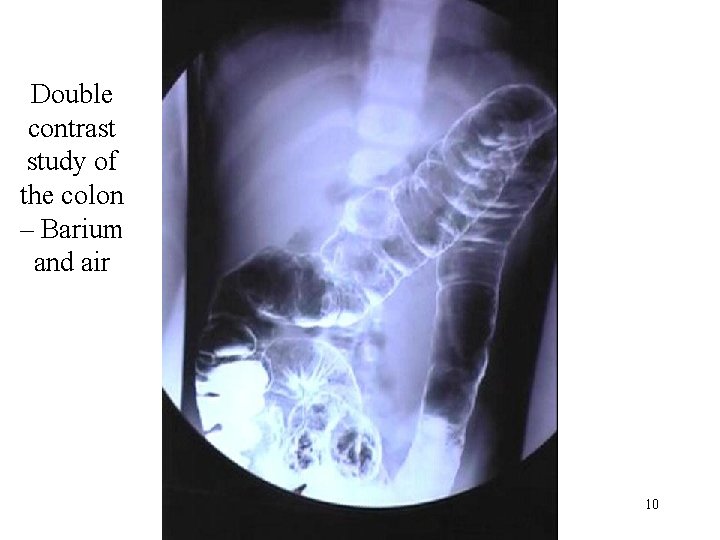
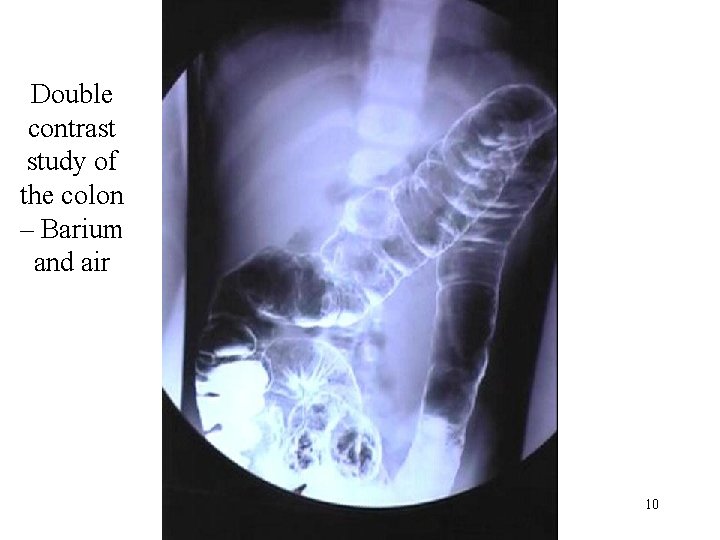
Double contrast study of the colon – Barium and air 10
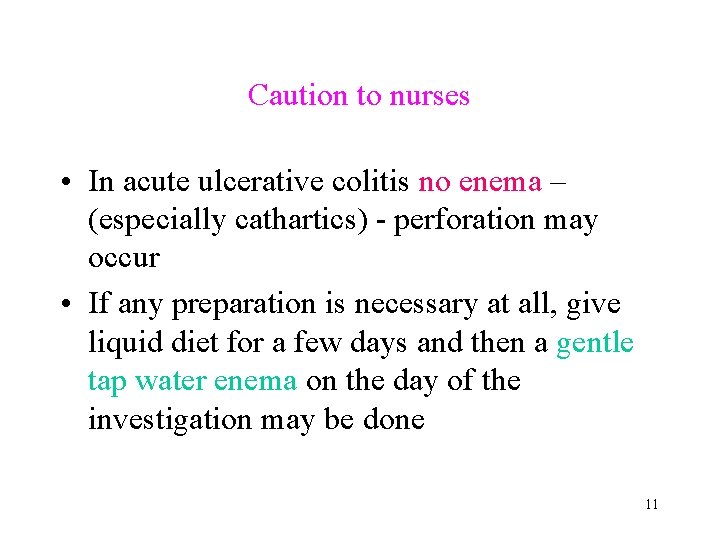
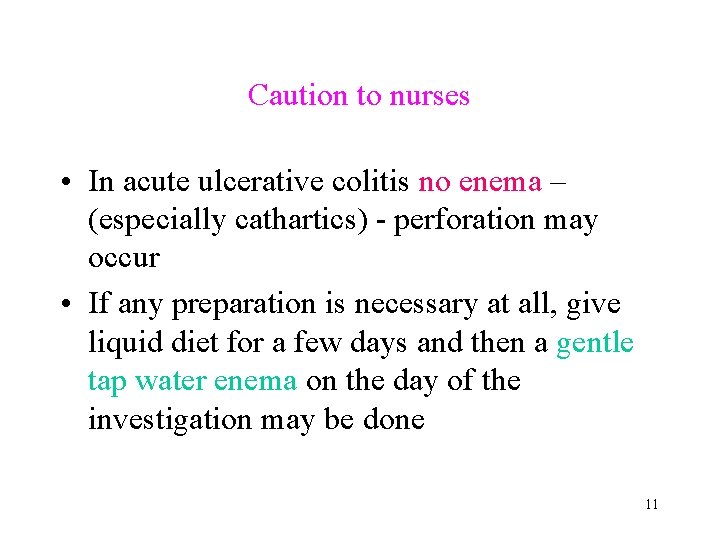
Caution to nurses • In acute ulcerative colitis no enema – (especially cathartics) - perforation may occur • If any preparation is necessary at all, give liquid diet for a few days and then a gentle tap water enema on the day of the investigation may be done 11
complications • • Toxic megacolon Perforation – high mortality Bleeding as a result of ulceration Highly vascular granulation tissue pseudo polyps 12
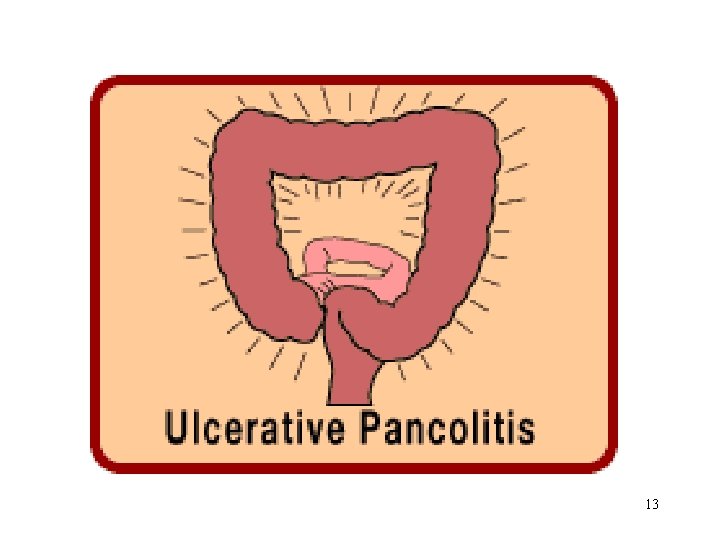
13
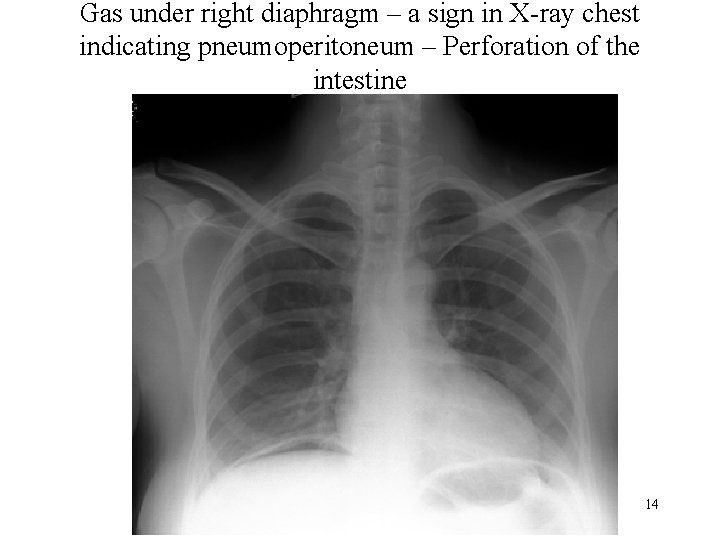
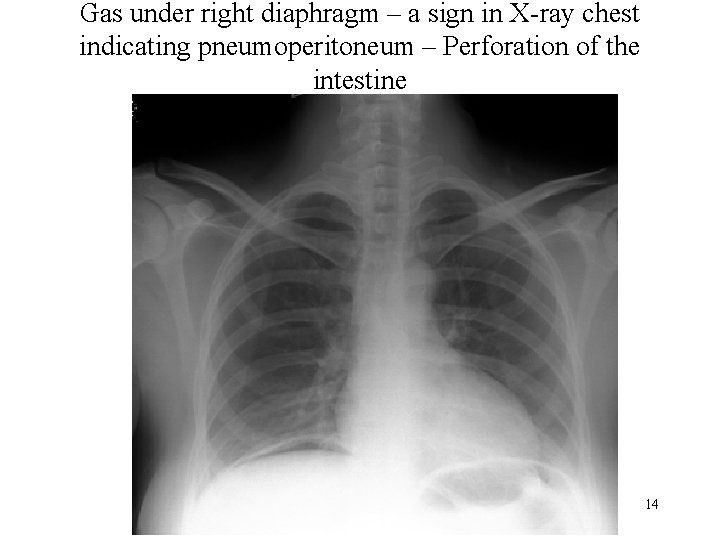
Gas under right diaphragm – a sign in X-ray chest indicating pneumoperitoneum – Perforation of the intestine 14
Management Medical treatment • Suppress inappropriate immune responses • Reduce inflammation • Provide rest to the diseased bowel • Nutritional therapy 15
Nutritional therapy • • • Oral fluids Low residue, high -protein, high calorie diet Vitamin supplements Iron replacement Correction of fluid and electrolyte imbalance by IV fluids • Avoid milk • Avoid cold foods and smoking • Total parental nutrition may be needed 16
Pharamacologic Therapy • • Sedatives Antidiarrhoeals Antiperistaltic drugs Sulphonamides such as sulfasalazine, sulfisoxazole • Antibiotics for infection like abscesses, perforations, peritonitis • Parenteral adrenocorticotropic hormone (ACTH) Beware of complications. • New topical and oral aminosalicylates (e. g. mesalamine, olsalazine are very effective in treatment. ) • Immunosuppressants used to reduce the dosage of 17 corticoids and to prevent recurrences.
Surgical Treatment • Strictureplasty • Resection and anastomosis a) Segmental colectomy with anastomosis b) Total colectomy and ileostomy 18

19

20