UHS Inc ICD10 CMPCS Physician Education Obstetrics and
UHS, Inc. ICD-10 -CM/PCS Physician Education Obstetrics and Gynecology 1
ICD-10 Implementation • October 1, 2015 – Compliance date for implementation of ICD-10 -CM (diagnoses) and ICD-10 -PCS (procedures) – Ambulatory and physician services provided on or after 10/1/15 – Inpatient discharges occurring on or after 10/1/15 • ICD-10 -CM (diagnoses) will be used by all providers in every health care setting • ICD-10 -PCS (procedures) will be used only for hospital claims for inpatient hospital procedures – ICD-10 -PCS will not be used on physician claims, even those for inpatient visits 2
Why ICD-10 Current ICD-9 Code Set is: – Outdated: 30 years old – Current code structure limits amount of new codes that can be created – Has obsolete groupings of disease families – Lacks specificity and detail to support: • Accurate anatomical positions • Differentiation of risk & severity • Key parameters to differentiate disease manifestations 3
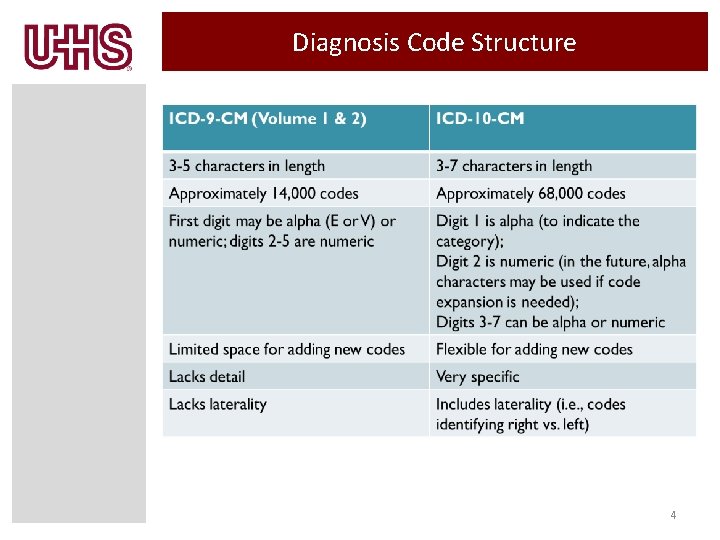
Diagnosis Code Structure 4
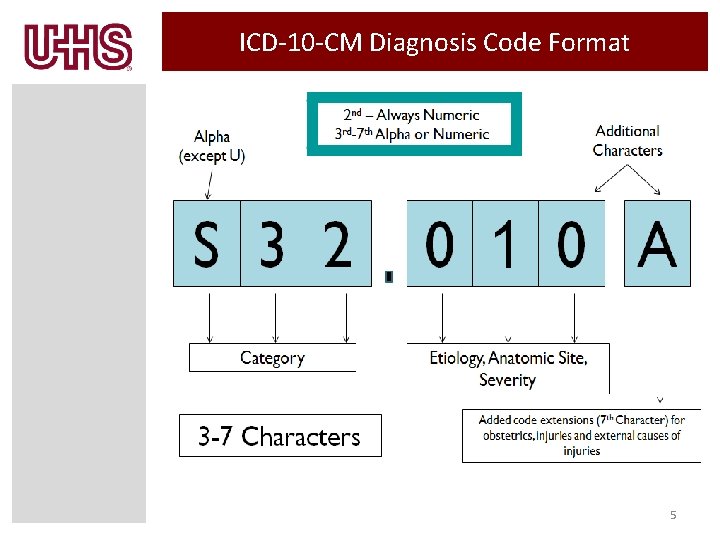
ICD-10 -CM Diagnosis Code Format 5
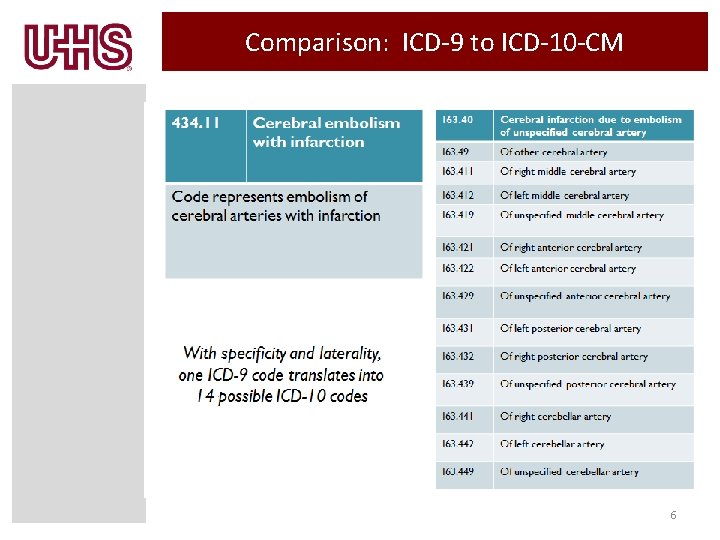
Comparison: ICD-9 to ICD-10 -CM 6
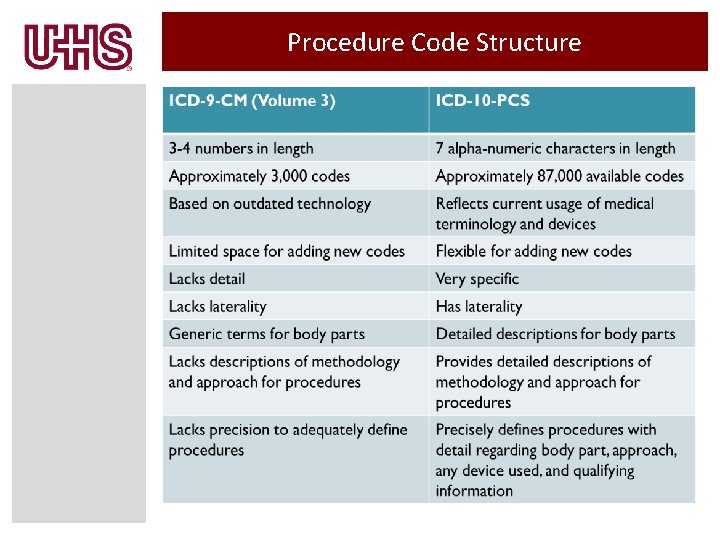
Procedure Code Structure
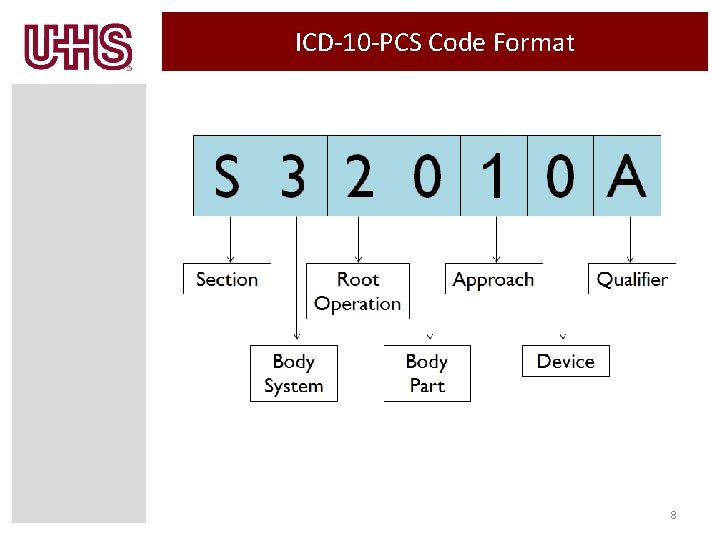
ICD-10 -PCS Code Format 8
ICD-10 Changes Everything! • ICD-10 is a Business Function Change, not just another code set change. • ICD-10 Implementation will impact everyone: – Registration, Nurses, Managers, Lab, Clinical Areas, Billing, Physicians, and Coding • How is ICD-10 going to change what you do? 9
ICD-10 -CM/PCS Documentation Tips 10
ICD-10 Provider Impact • Clinical documentation is the foundation of successful ICD 10 Implementation • Golden Rule of Documentation – If it isn’t documented by the physician, it didn’t happen – If it didn’t happen, it can’t be billed • The purpose in documentation is to tell the story of what was performed and what is diagnosed accurately and thoroughly reflecting the condition of the patient – what services were rendered and what is the severity of illness • The key word is SPECIFICITY – Granularity – Laterality • Complete and concise documentation allows for accurate coding and reimbursement 11
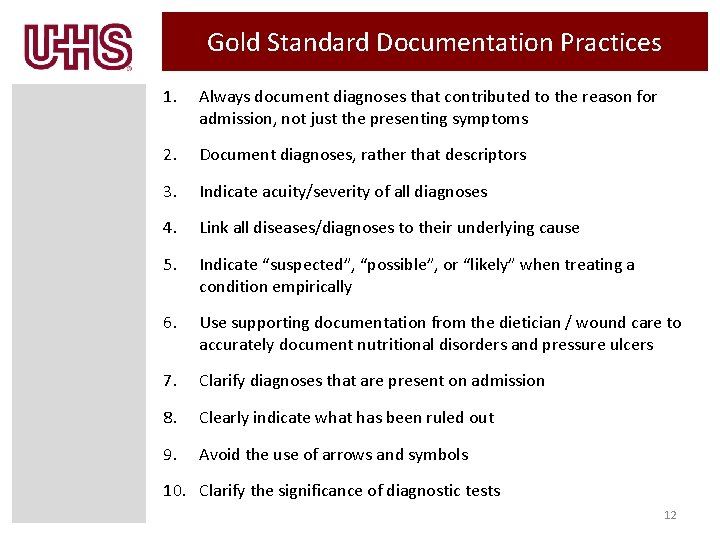
Gold Standard Documentation Practices 1. Always document diagnoses that contributed to the reason for admission, not just the presenting symptoms 2. Document diagnoses, rather that descriptors 3. Indicate acuity/severity of all diagnoses 4. Link all diseases/diagnoses to their underlying cause 5. Indicate “suspected”, “possible”, or “likely” when treating a condition empirically 6. Use supporting documentation from the dietician / wound care to accurately document nutritional disorders and pressure ulcers 7. Clarify diagnoses that are present on admission 8. Clearly indicate what has been ruled out 9. Avoid the use of arrows and symbols 10. Clarify the significance of diagnostic tests 12
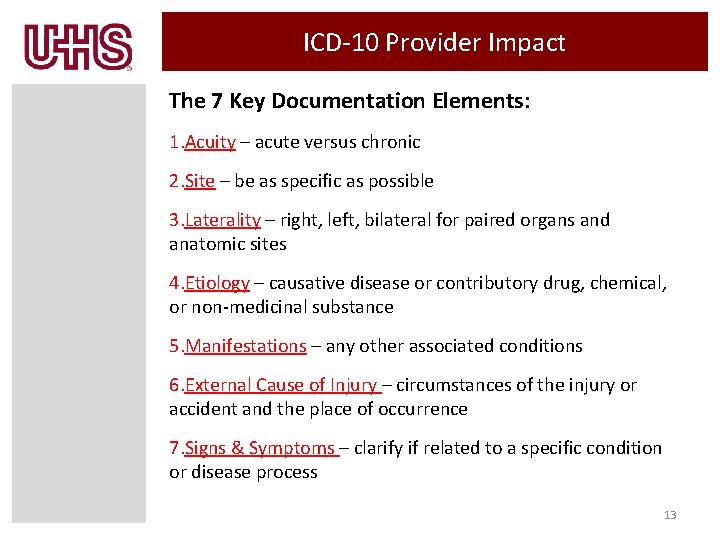
ICD-10 Provider Impact The 7 Key Documentation Elements: 1. Acuity – acute versus chronic 2. Site – be as specific as possible 3. Laterality – right, left, bilateral for paired organs and anatomic sites 4. Etiology – causative disease or contributory drug, chemical, or non-medicinal substance 5. Manifestations – any other associated conditions 6. External Cause of Injury – circumstances of the injury or accident and the place of occurrence 7. Signs & Symptoms – clarify if related to a specific condition or disease process 13
ICD-10 Documentation Tips Do not use symbols to indicate a disease. For example “↑lipids” means that a laboratory result indicates the lipids are elevated – or “↑BP” means that a blood pressure reading is high These are not the same as hyperlipidemia or hypertension 14
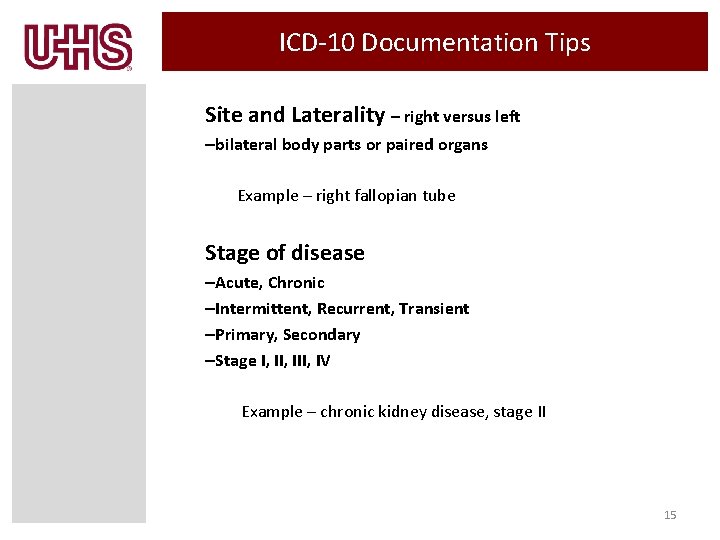
ICD-10 Documentation Tips Site and Laterality – right versus left –bilateral body parts or paired organs Example – right fallopian tube Stage of disease –Acute, Chronic –Intermittent, Recurrent, Transient –Primary, Secondary –Stage I, III, IV Example – chronic kidney disease, stage II 15
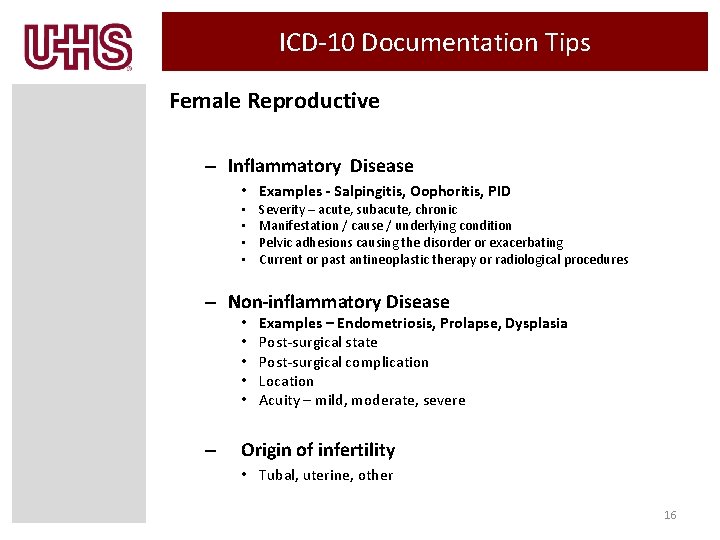
ICD-10 Documentation Tips Female Reproductive – Inflammatory Disease • Examples - Salpingitis, Oophoritis, PID • • Severity – acute, subacute, chronic Manifestation / cause / underlying condition Pelvic adhesions causing the disorder or exacerbating Current or past antineoplastic therapy or radiological procedures – Non-inflammatory Disease • • • – Examples – Endometriosis, Prolapse, Dysplasia Post-surgical state Post-surgical complication Location Acuity – mild, moderate, severe Origin of infertility • Tubal, uterine, other 16
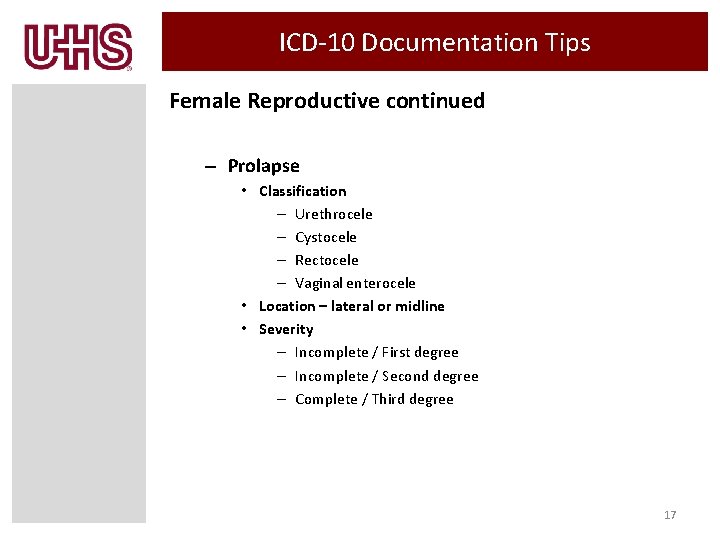
ICD-10 Documentation Tips Female Reproductive continued – Prolapse • Classification – Urethrocele – Cystocele – Rectocele – Vaginal enterocele • Location – lateral or midline • Severity – Incomplete / First degree – Incomplete / Second degree – Complete / Third degree 17
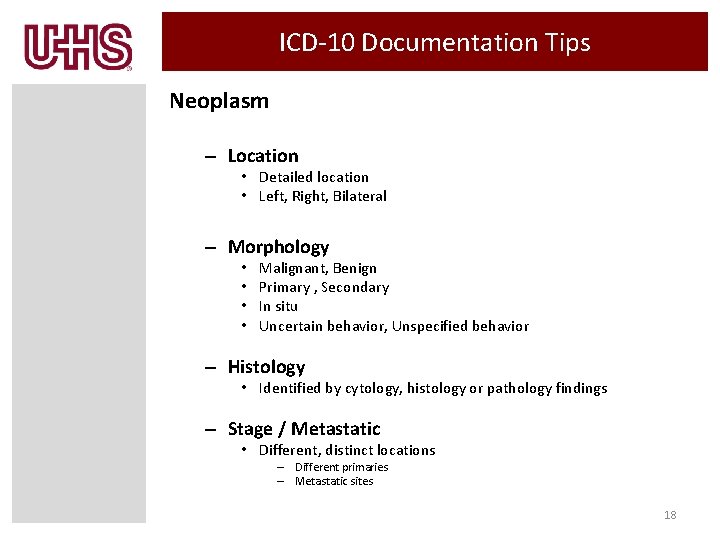
ICD-10 Documentation Tips Neoplasm – Location • Detailed location • Left, Right, Bilateral – Morphology • • Malignant, Benign Primary , Secondary In situ Uncertain behavior, Unspecified behavior – Histology • Identified by cytology, histology or pathology findings – Stage / Metastatic • Different, distinct locations – Different primaries – Metastatic sites 18
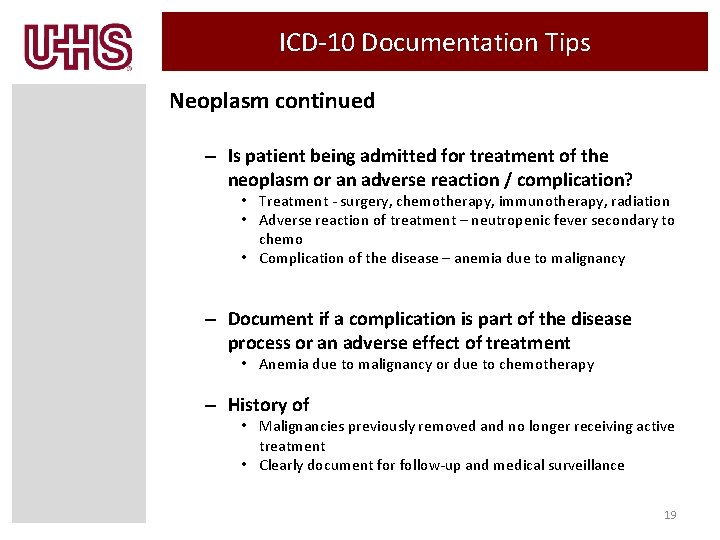
ICD-10 Documentation Tips Neoplasm continued – Is patient being admitted for treatment of the neoplasm or an adverse reaction / complication? • Treatment - surgery, chemotherapy, immunotherapy, radiation • Adverse reaction of treatment – neutropenic fever secondary to chemo • Complication of the disease – anemia due to malignancy – Document if a complication is part of the disease process or an adverse effect of treatment • Anemia due to malignancy or due to chemotherapy – History of • Malignancies previously removed and no longer receiving active treatment • Clearly document for follow-up and medical surveillance 19
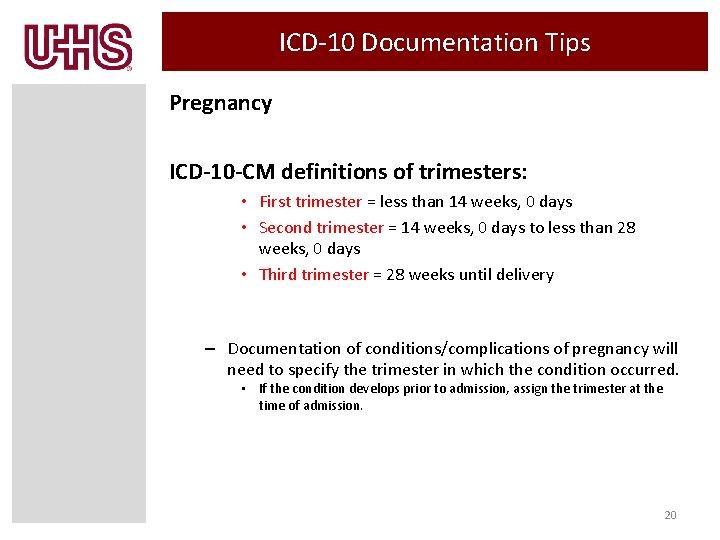
ICD-10 Documentation Tips Pregnancy ICD-10 -CM definitions of trimesters: • First trimester = less than 14 weeks, 0 days • Second trimester = 14 weeks, 0 days to less than 28 weeks, 0 days • Third trimester = 28 weeks until delivery – Documentation of conditions/complications of pregnancy will need to specify the trimester in which the condition occurred. • If the condition develops prior to admission, assign the trimester at the time of admission. 20
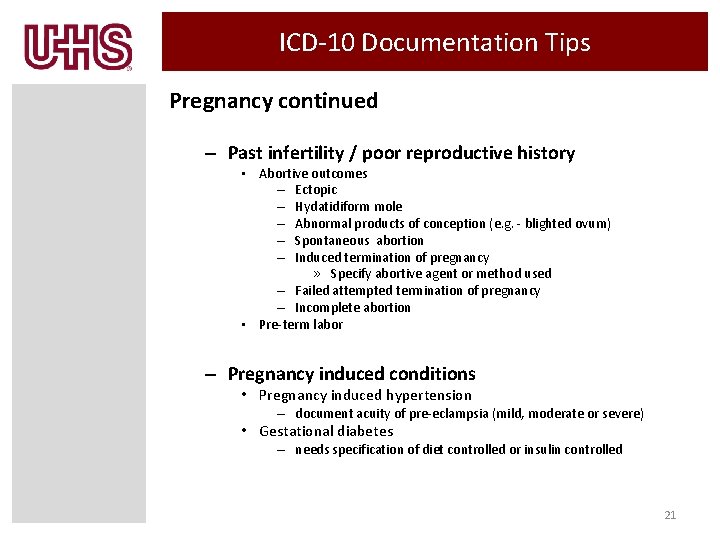
ICD-10 Documentation Tips Pregnancy continued – Past infertility / poor reproductive history • Abortive outcomes – Ectopic – Hydatidiform mole – Abnormal products of conception (e. g. - blighted ovum) – Spontaneous abortion – Induced termination of pregnancy » Specify abortive agent or method used – Failed attempted termination of pregnancy – Incomplete abortion • Pre-term labor – Pregnancy induced conditions • Pregnancy induced hypertension – document acuity of pre-eclampsia (mild, moderate or severe) • Gestational diabetes – needs specification of diet controlled or insulin controlled 21
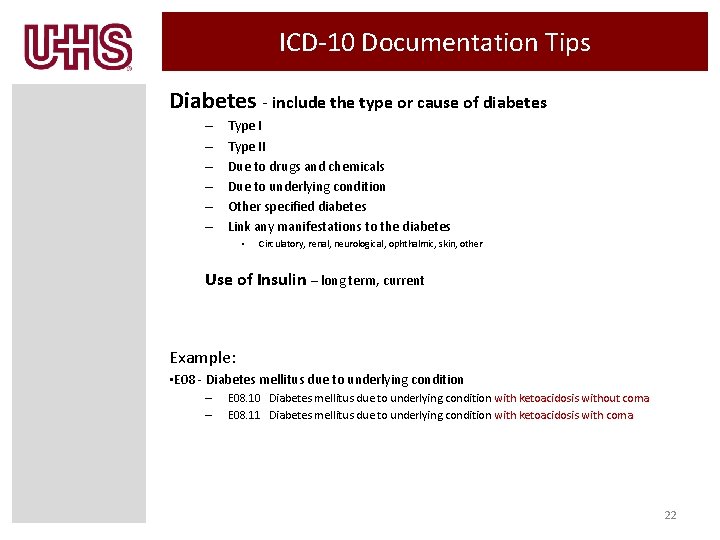
ICD-10 Documentation Tips Diabetes - include the type or cause of diabetes – – – Type II Due to drugs and chemicals Due to underlying condition Other specified diabetes Link any manifestations to the diabetes • Circulatory, renal, neurological, ophthalmic, skin, other Use of Insulin – long term, current Example: • E 08 - Diabetes mellitus due to underlying condition – – E 08. 10 Diabetes mellitus due to underlying condition with ketoacidosis without coma E 08. 11 Diabetes mellitus due to underlying condition with ketoacidosis with coma 22
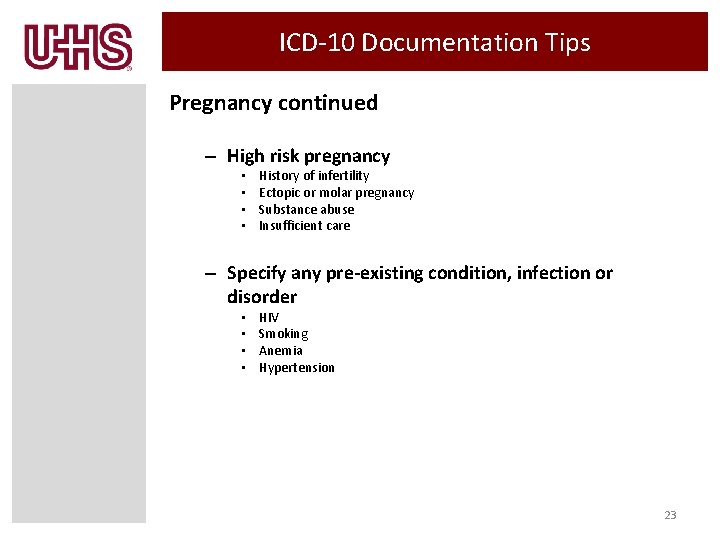
ICD-10 Documentation Tips Pregnancy continued – High risk pregnancy • • History of infertility Ectopic or molar pregnancy Substance abuse Insufficient care – Specify any pre-existing condition, infection or disorder • • HIV Smoking Anemia Hypertension 23
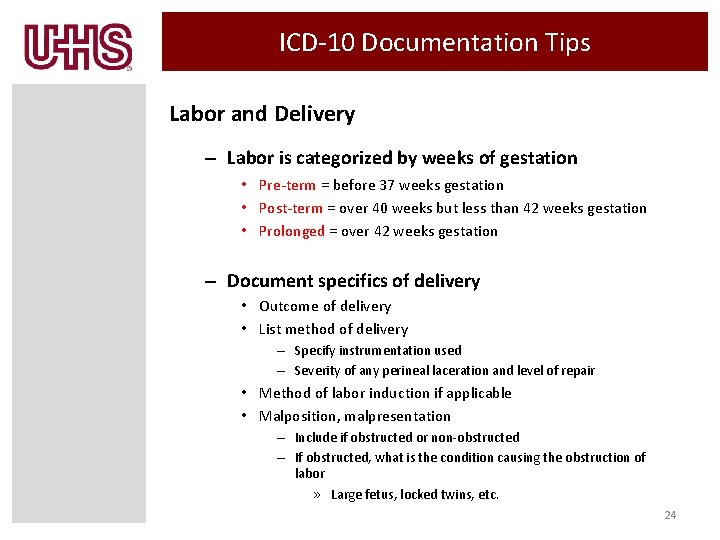
ICD-10 Documentation Tips Labor and Delivery – Labor is categorized by weeks of gestation • Pre-term = before 37 weeks gestation • Post-term = over 40 weeks but less than 42 weeks gestation • Prolonged = over 42 weeks gestation – Document specifics of delivery • Outcome of delivery • List method of delivery – Specify instrumentation used – Severity of any perineal laceration and level of repair • Method of labor induction if applicable • Malposition, malpresentation – Include if obstructed or non-obstructed – If obstructed, what is the condition causing the obstruction of labor » Large fetus, locked twins, etc. 24
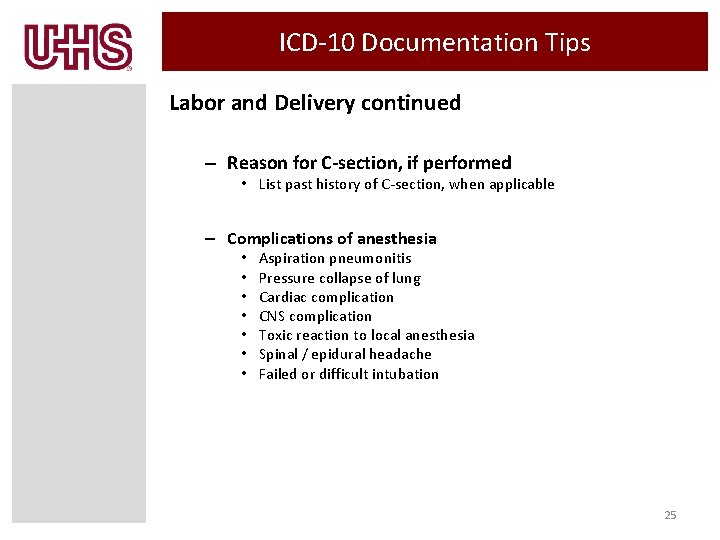
ICD-10 Documentation Tips Labor and Delivery continued – Reason for C-section, if performed • List past history of C-section, when applicable – Complications of anesthesia • • Aspiration pneumonitis Pressure collapse of lung Cardiac complication CNS complication Toxic reaction to local anesthesia Spinal / epidural headache Failed or difficult intubation 25
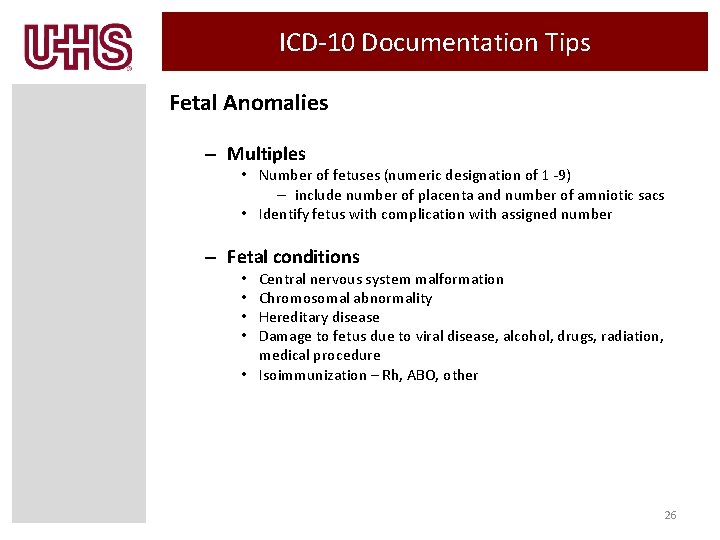
ICD-10 Documentation Tips Fetal Anomalies – Multiples • Number of fetuses (numeric designation of 1 -9) – include number of placenta and number of amniotic sacs • Identify fetus with complication with assigned number – Fetal conditions Central nervous system malformation Chromosomal abnormality Hereditary disease Damage to fetus due to viral disease, alcohol, drugs, radiation, medical procedure • Isoimmunization – Rh, ABO, other • • 26
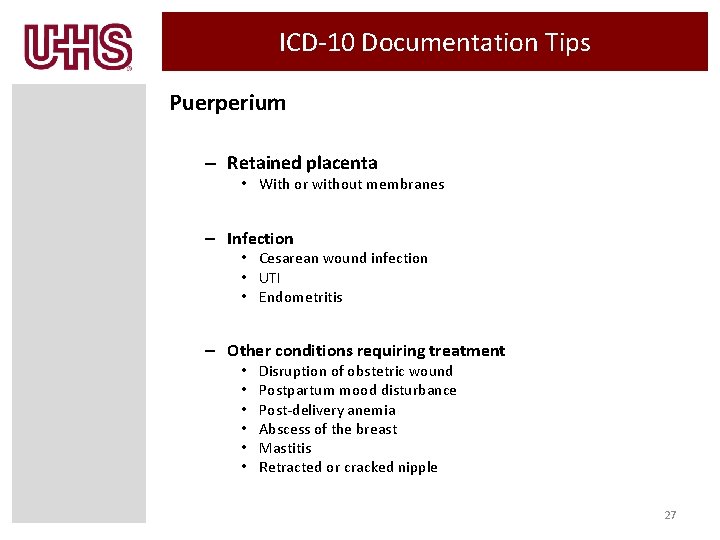
ICD-10 Documentation Tips Puerperium – Retained placenta • With or without membranes – Infection • Cesarean wound infection • UTI • Endometritis – Other conditions requiring treatment • • • Disruption of obstetric wound Postpartum mood disturbance Post-delivery anemia Abscess of the breast Mastitis Retracted or cracked nipple 27
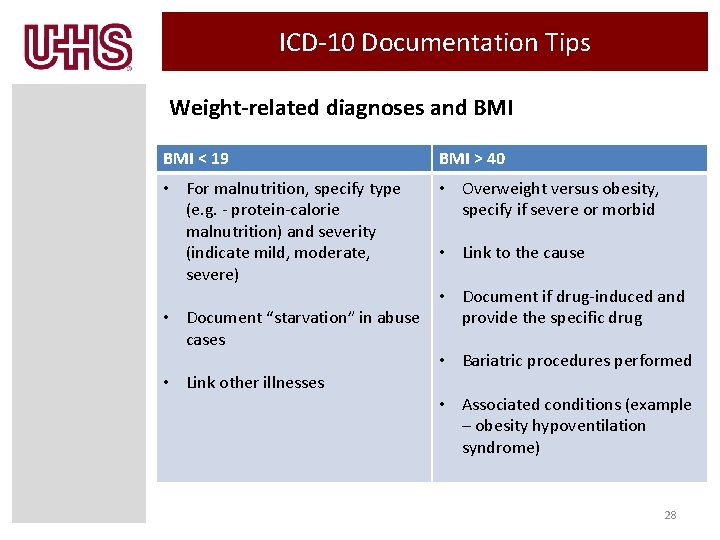
ICD-10 Documentation Tips Weight-related diagnoses and BMI < 19 BMI > 40 • For malnutrition, specify type (e. g. - protein-calorie malnutrition) and severity (indicate mild, moderate, severe) • Overweight versus obesity, specify if severe or morbid • Document “starvation” in abuse cases • Link other illnesses • Link to the cause • Document if drug-induced and provide the specific drug • Bariatric procedures performed • Associated conditions (example – obesity hypoventilation syndrome) 28
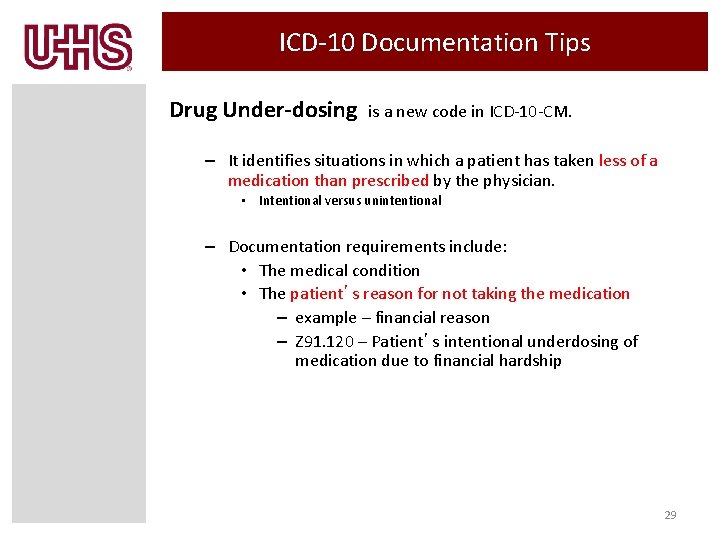
ICD-10 Documentation Tips Drug Under-dosing is a new code in ICD-10 -CM. – It identifies situations in which a patient has taken less of a medication than prescribed by the physician. • Intentional versus unintentional – Documentation requirements include: • The medical condition • The patient’s reason for not taking the medication – example – financial reason – Z 91. 120 – Patient’s intentional underdosing of medication due to financial hardship 29
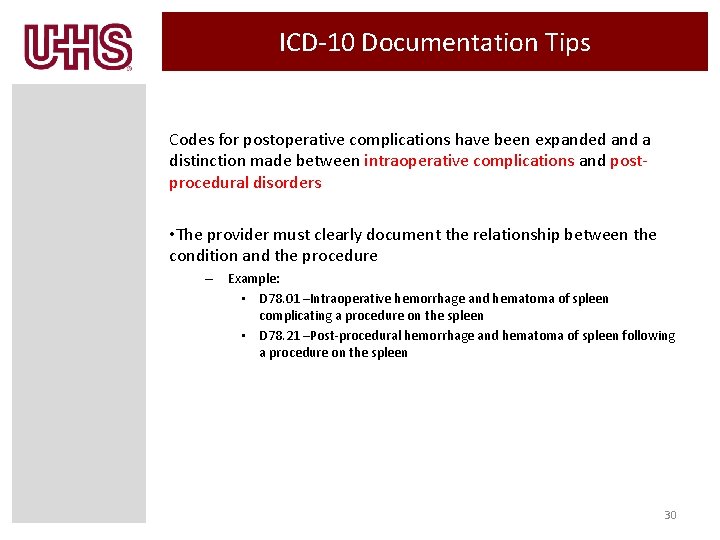
ICD-10 Documentation Tips Codes for postoperative complications have been expanded and a distinction made between intraoperative complications and postprocedural disorders • The provider must clearly document the relationship between the condition and the procedure – Example: • D 78. 01 –Intraoperative hemorrhage and hematoma of spleen complicating a procedure on the spleen • D 78. 21 –Post-procedural hemorrhage and hematoma of spleen following a procedure on the spleen 30
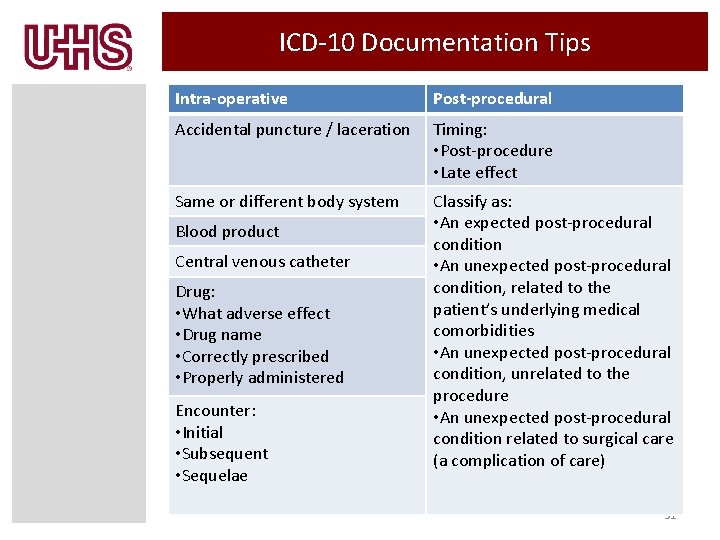
ICD-10 Documentation Tips Intra-operative Post-procedural Accidental puncture / laceration Timing: • Post-procedure • Late effect Same or different body system Classify as: • An expected post-procedural condition • An unexpected post-procedural condition, related to the patient’s underlying medical comorbidities • An unexpected post-procedural condition, unrelated to the procedure • An unexpected post-procedural condition related to surgical care (a complication of care) Blood product Central venous catheter Drug: • What adverse effect • Drug name • Correctly prescribed • Properly administered Encounter: • Initial • Subsequent • Sequelae 31
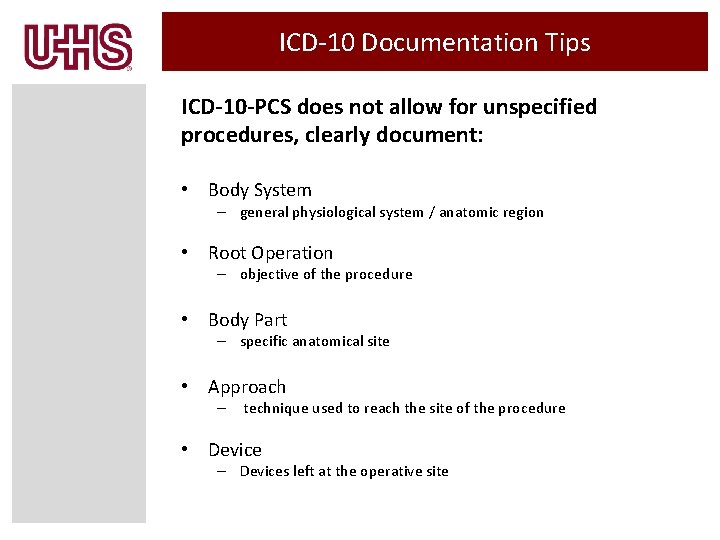
ICD-10 Documentation Tips ICD-10 -PCS does not allow for unspecified procedures, clearly document: • Body System – general physiological system / anatomic region • Root Operation – objective of the procedure • Body Part – specific anatomical site • Approach – technique used to reach the site of the procedure • Device – Devices left at the operative site
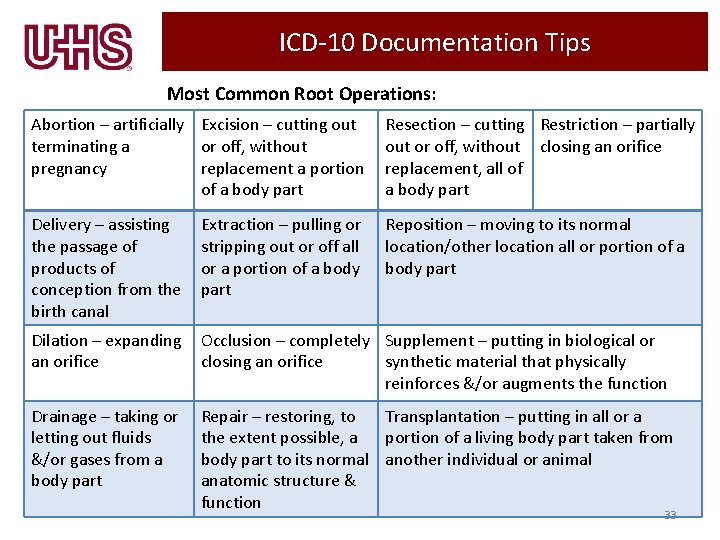
ICD-10 Documentation Tips Most Common Root Operations: Abortion – artificially Excision – cutting out terminating a or off, without pregnancy replacement a portion of a body part Resection – cutting Restriction – partially out or off, without closing an orifice replacement, all of a body part Delivery – assisting the passage of products of conception from the birth canal Extraction – pulling or stripping out or off all or a portion of a body part Reposition – moving to its normal location/other location all or portion of a body part Dilation – expanding an orifice Occlusion – completely Supplement – putting in biological or closing an orifice synthetic material that physically reinforces &/or augments the function Drainage – taking or letting out fluids &/or gases from a body part Repair – restoring, to Transplantation – putting in all or a the extent possible, a portion of a living body part taken from body part to its normal another individual or animal anatomic structure & function 33
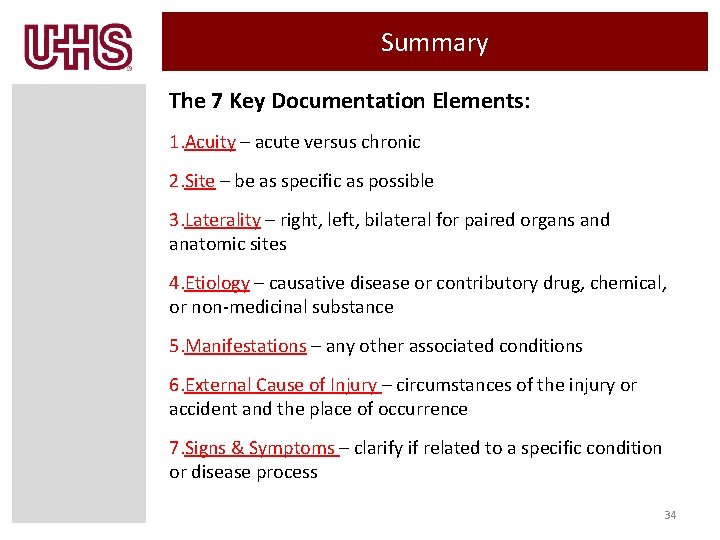
Summary The 7 Key Documentation Elements: 1. Acuity – acute versus chronic 2. Site – be as specific as possible 3. Laterality – right, left, bilateral for paired organs and anatomic sites 4. Etiology – causative disease or contributory drug, chemical, or non-medicinal substance 5. Manifestations – any other associated conditions 6. External Cause of Injury – circumstances of the injury or accident and the place of occurrence 7. Signs & Symptoms – clarify if related to a specific condition or disease process 34
- Slides: 34