UGS MODULE Candidiasis By Prof Dr Zainalabideen A
UGS MODULE Candidiasis By Prof. Dr. Zainalabideen A. Al- Abdulla, MRCPI, DTM&H. , Ph. D. , FRCPath. (U. K. )
Learning objectives 1. Describe the morphology of Candida albicans, its pathogenesis and the association between the immune system & fungal infections. 2. Briefly describe clinical presentation and the nature of the vaginal discharge. 3. Describe laboratory methods of diagnosis as well as drugs used for treatment.
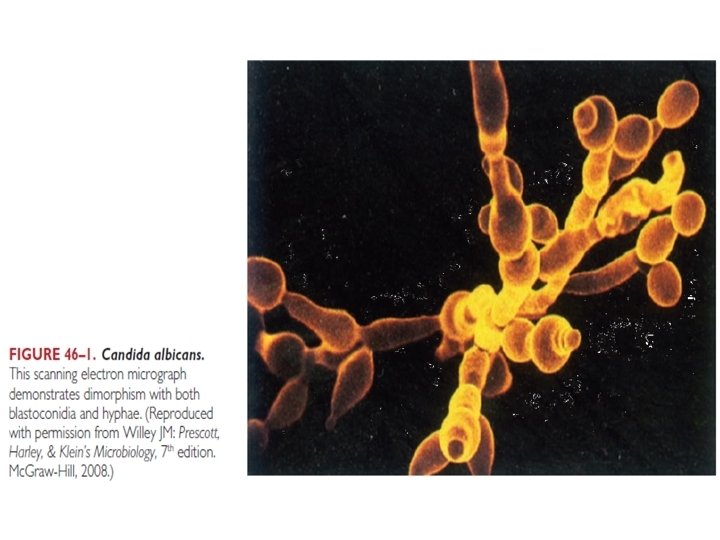
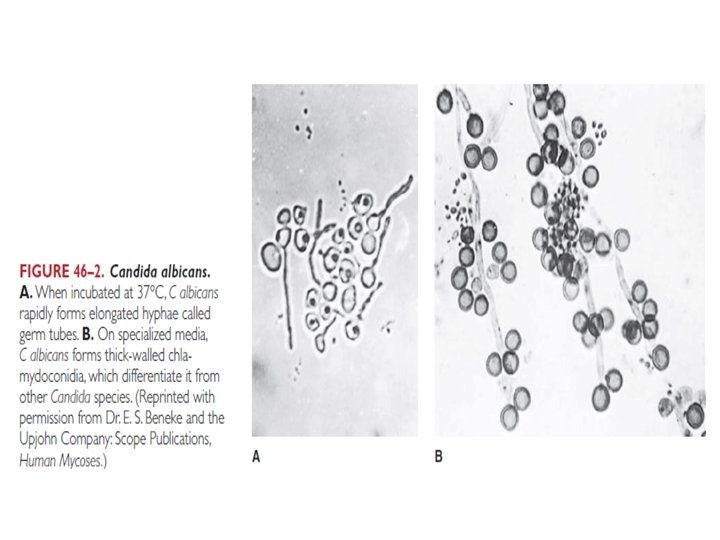
Candida: General Characteristics • Budding, round, or oval yeast cells • May form Hyphae such as during infections • Cell wall: Chitin and carbohydrates (CHO) • Species identification: Biochemical, enzymatic, morphologic, CHO assimilation, fermentation, hyphae, germ tubes and chlamydoconidia • Grow on Sabouraud’s agar, and blood agar: - Smooth, white, 2 -4 mm colonies - Candida albicans: Is germ tube positive
Candida albicans • Forms: - Yeast with budding (Blastoconidia) - Hyphae triggered by: Temp. 37 o. C, p. H # When attached to yeast as sprouts “outgrow” are called Germ Tubes # Hyphae may develop terminal thick-walled “Chlamydoconidia” - Elongated forms with restrictions (Pseudo-hyphae) • Cell wall: Includes surface mannoproteins
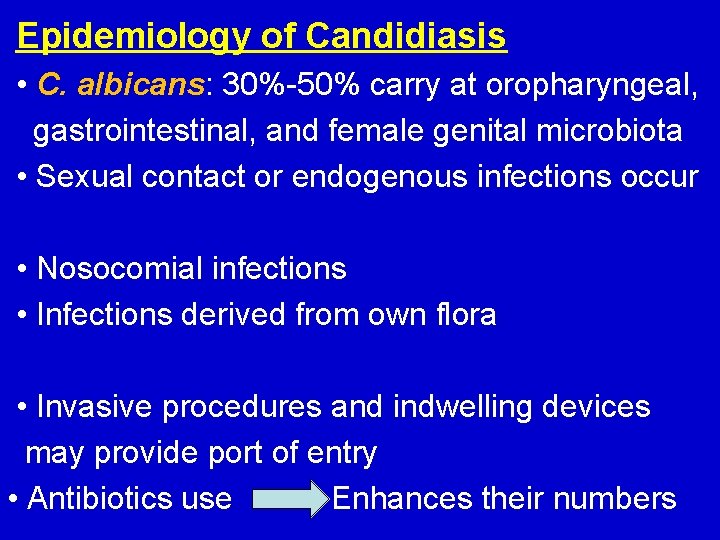
Epidemiology of Candidiasis • C. albicans: 30%-50% carry at oropharyngeal, gastrointestinal, and female genital microbiota • Sexual contact or endogenous infections occur • Nosocomial infections • Infections derived from own flora • Invasive procedures and indwelling devices may provide port of entry • Antibiotics use Enhances their numbers
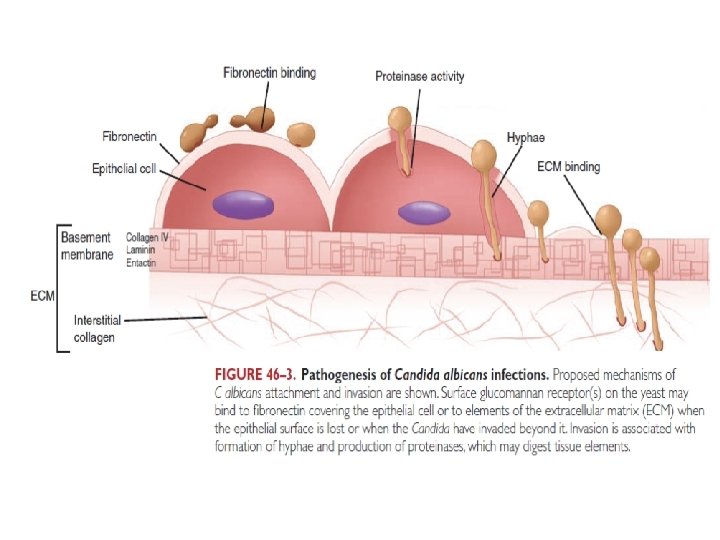
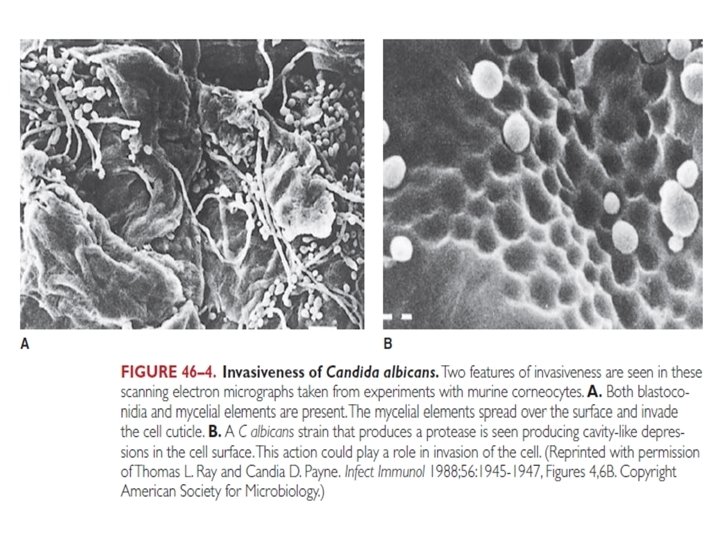
Pathogenesis • Hyphae form during invasion superficially or deep • Strong attachment to epithelium is via surface hyphal wall protein (Hwp 1) on germ tube/hyphae • Glucomanan receptors of Candida bind to fibronectin of epithelial cells (by yeast form) or extracellular matrix (ECM) as collagen, laminin and intactin e. g. by hyphal form during invasion. cont. /…
Cont. /…. Pathogenesis • Proteinases, phospholipases: For invasion - Aspartic proteinases (Sap): Digest keratin, and collagen: # Sap tissue specific, e. g. GIT, vaginal # Produced by hyphae, e. g. during invasion • Able to form biofilm (yeast and hyphae). Cont. /. . .
Cont. /… pathogenesis • Mechanisms of evasion of innate immunity: - Masking from TLRs - Degradation of surface Cb 3 Surface proteins resembling CR 2, CR 3 (confusing phagocytosis), e. g. high glucose - Hyphal growth inside phagocytes leads to death of these cells • Susceptibility increased by antibiotics, steroids, leukopenia, AIDS, chemotherapy, devices, DM
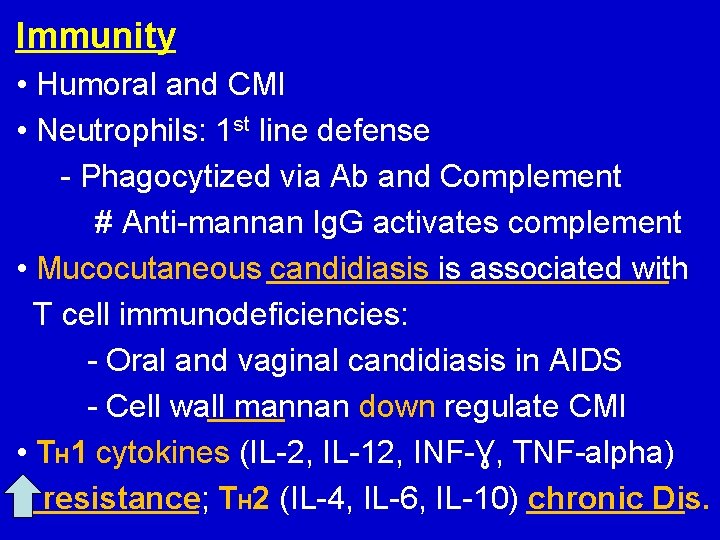
Immunity • Humoral and CMI • Neutrophils: 1 st line defense - Phagocytized via Ab and Complement # Anti-mannan Ig. G activates complement • Mucocutaneous candidiasis is associated with T cell immunodeficiencies: - Oral and vaginal candidiasis in AIDS - Cell wall mannan down regulate CMI • TH 1 cytokines (IL-2, IL-12, INF-Ɣ, TNF-alpha) resistance; TH 2 (IL-4, IL-6, IL-10) chronic Dis.
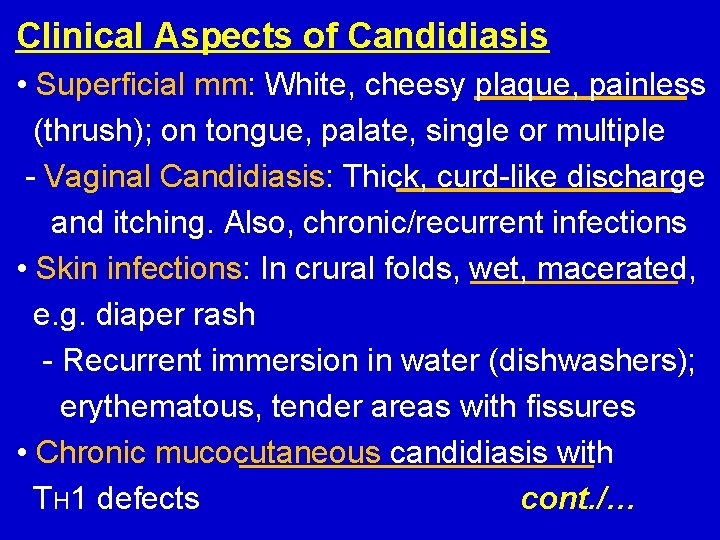
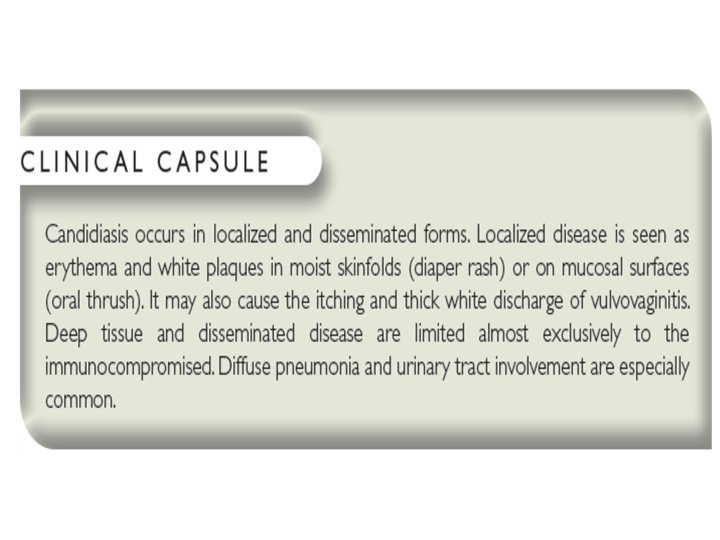
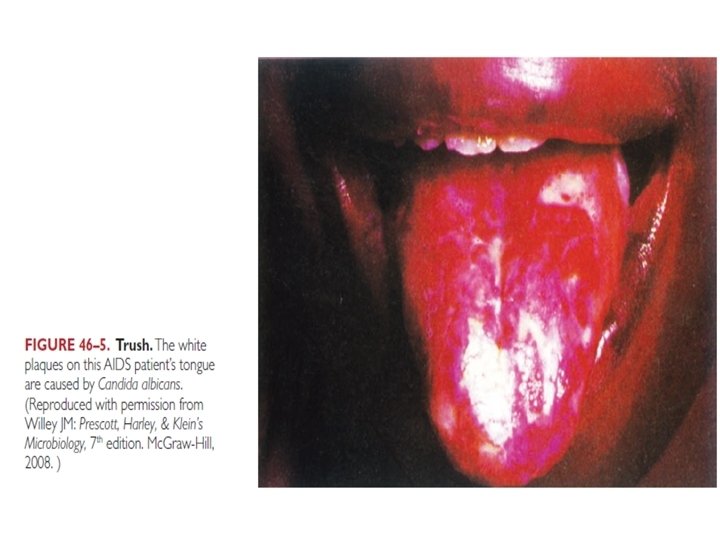
Clinical Aspects of Candidiasis • Superficial mm: White, cheesy plaque, painless (thrush); on tongue, palate, single or multiple - Vaginal Candidiasis: Thick, curd-like discharge and itching. Also, chronic/recurrent infections • Skin infections: In crural folds, wet, macerated, e. g. diaper rash - Recurrent immersion in water (dishwashers); erythematous, tender areas with fissures • Chronic mucocutaneous candidiasis with TH 1 defects cont. /…

Thrush Vulvovaginal candidiasis Diaper Rash Chronic mucocutaneous candidiasis
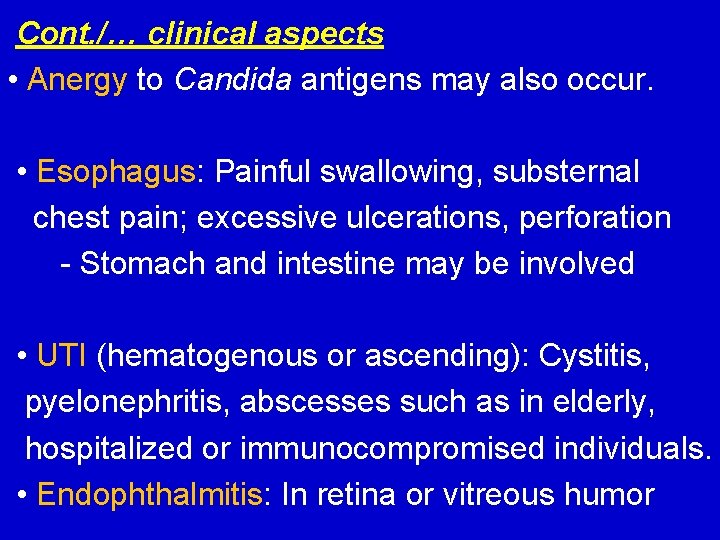
Cont. /… clinical aspects • Anergy to Candida antigens may also occur. • Esophagus: Painful swallowing, substernal chest pain; excessive ulcerations, perforation - Stomach and intestine may be involved • UTI (hematogenous or ascending): Cystitis, pyelonephritis, abscesses such as in elderly, hospitalized or immunocompromised individuals. • Endophthalmitis: In retina or vitreous humor
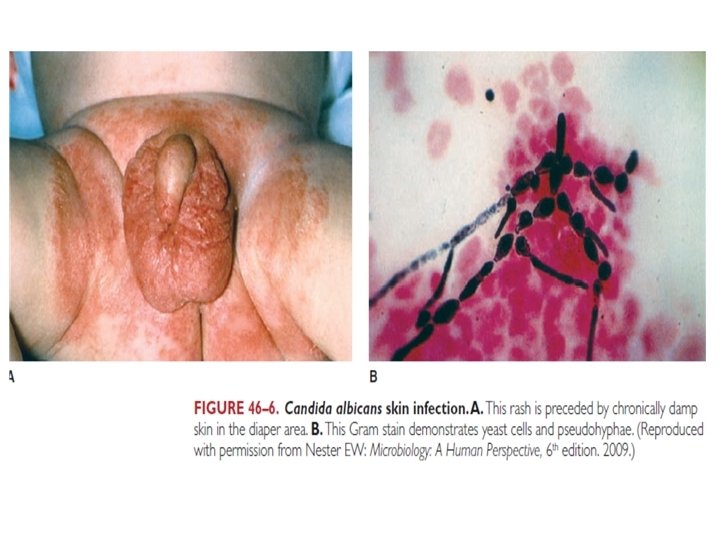

Candidal Intertrigo
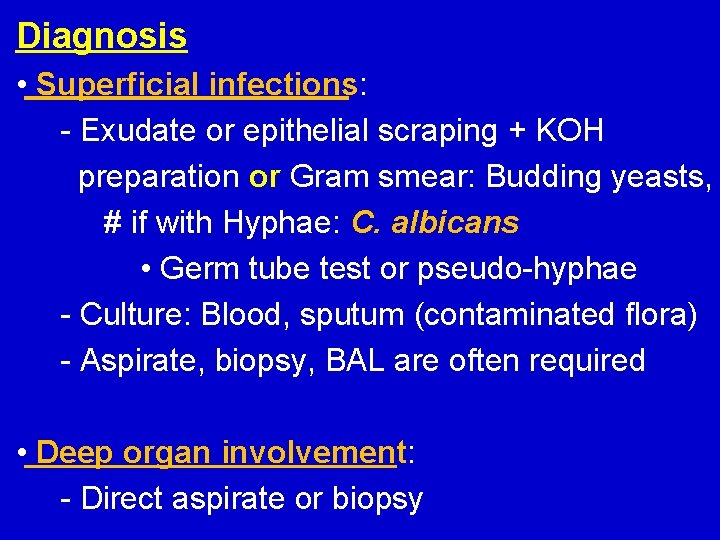
Diagnosis • Superficial infections: - Exudate or epithelial scraping + KOH preparation or Gram smear: Budding yeasts, # if with Hyphae: C. albicans • Germ tube test or pseudo-hyphae - Culture: Blood, sputum (contaminated flora) - Aspirate, biopsy, BAL are often required • Deep organ involvement: - Direct aspirate or biopsy
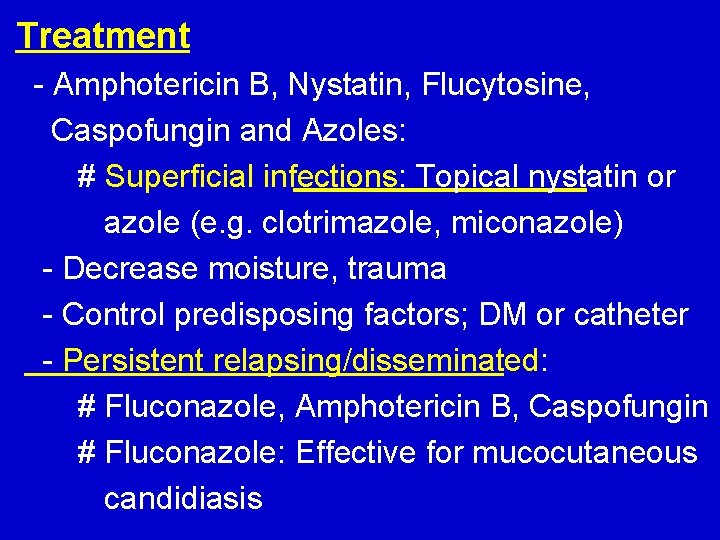
Treatment - Amphotericin B, Nystatin, Flucytosine, Caspofungin and Azoles: # Superficial infections: Topical nystatin or azole (e. g. clotrimazole, miconazole) - Decrease moisture, trauma - Control predisposing factors; DM or catheter - Persistent relapsing/disseminated: # Fluconazole, Amphotericin B, Caspofungin # Fluconazole: Effective for mucocutaneous candidiasis
Other Candida Species - Candida tropicalis: Indwelling catheter - Candida glabrata: Has no hyphae; part of GIT, and genital microbiota: # May cause UTI and fungemia - Treatment: Similar to C. albicans, but C. glabrata is more resistant to Fluconazole
- Slides: 23