UCSF Congenital Cardiac Anesthesia Tutorials Tetralogy of Fallot





- Slides: 14
UCSF Congenital Cardiac Anesthesia Tutorials Tetralogy of Fallot for Cardiac Anaesthesia 1 William C K Ng
acknowledgements 2
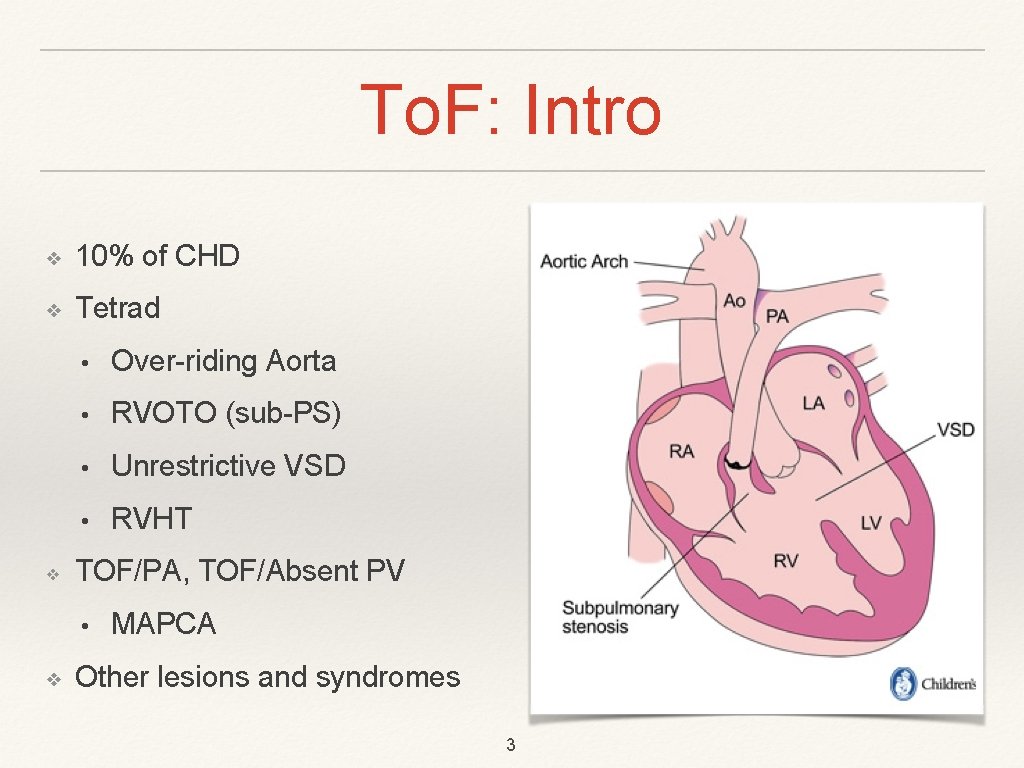
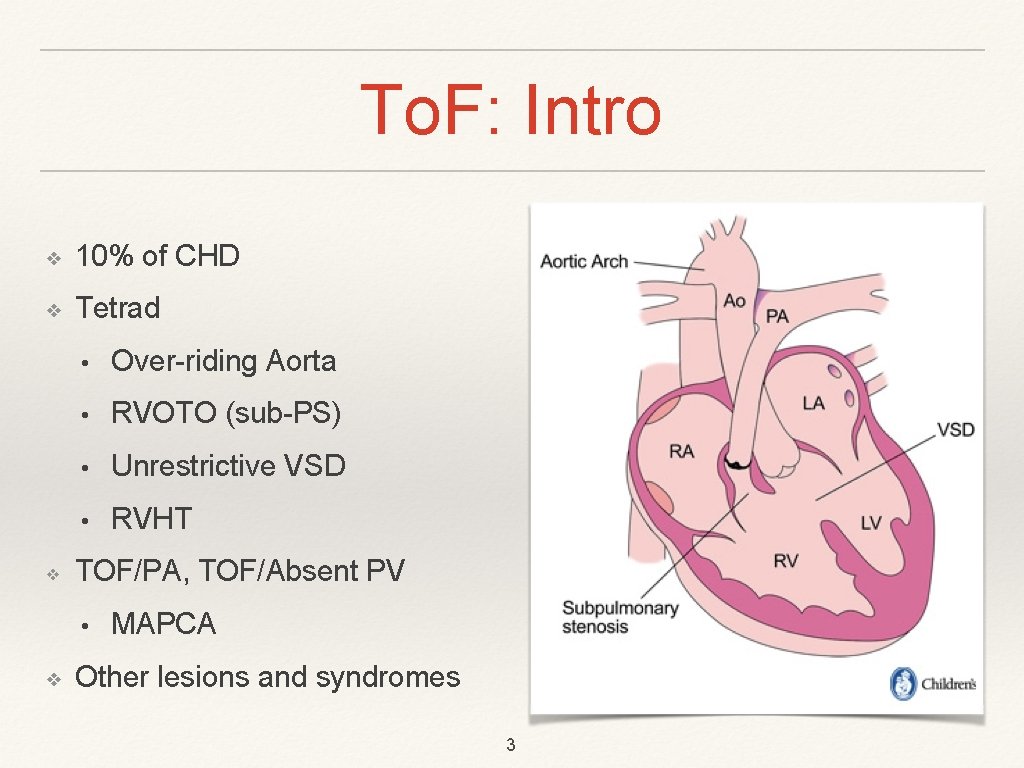
To. F: Intro ❖ 10% of CHD ❖ Tetrad ❖ • Over-riding Aorta • RVOTO (sub-PS) • Unrestrictive VSD • RVHT TOF/PA, TOF/Absent PV • ❖ MAPCA Other lesions and syndromes 3

History, Examination, Investigations ❖ Prenatal diagnosis vs. Postnatal diagnosis - more obvious when PDA is closed. • Cyanosis • Syndromes • Chest ❖ ECG: RAD ❖ CXR: “clog-shaped” heart Cœur en sabot. 4

Consequences and associations of To. F ❖ Biventricular origin of Aorta ❖ HT RVOT ❖ PA hypoplasia or PV absence, and consequences of each ❖ Other ❖ • PV dysplasia • RAA with mirror branching • Coronary pathways: LAD from RCA Syndromes: VACTERL, CHARGE, Alagille, 22 q 11 deletion, Trisomy 21 5
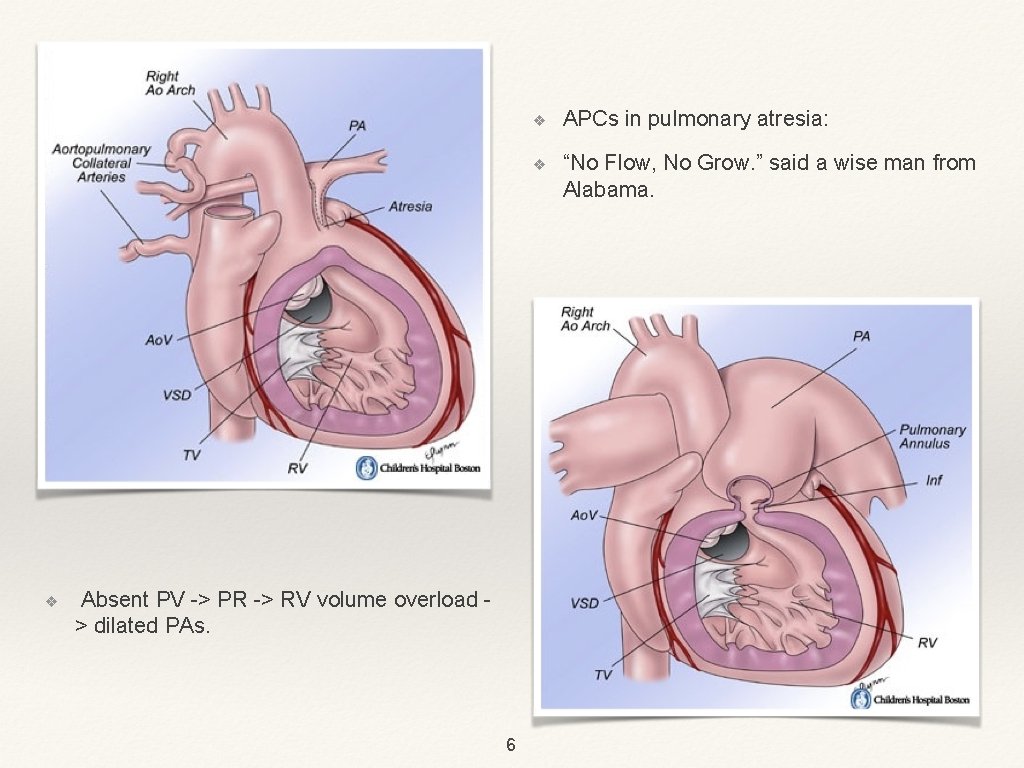
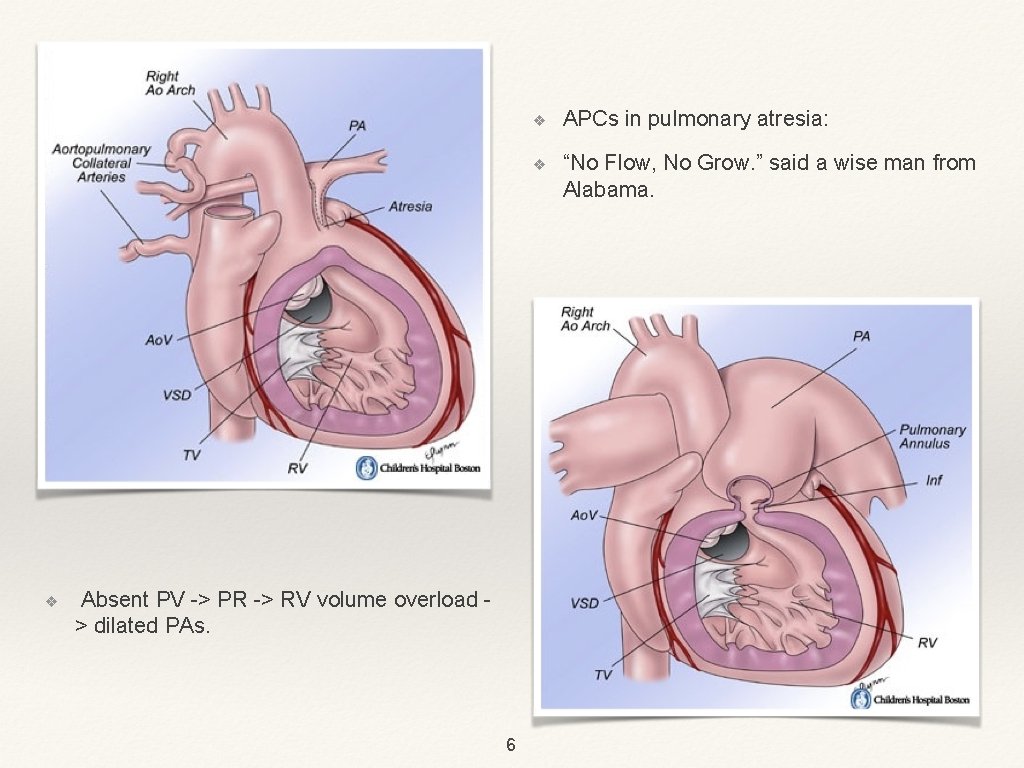
❖ Absent PV -> PR -> RV volume overload > dilated PAs. 6 ❖ APCs in pulmonary atresia: ❖ “No Flow, No Grow. ” said a wise man from Alabama.

• • • RVOTO and dynamic changes VSD: number, location, size (unrestricted) Coronaries Other abnormalities Function and dynamic changes 7 Echocardiograp hy
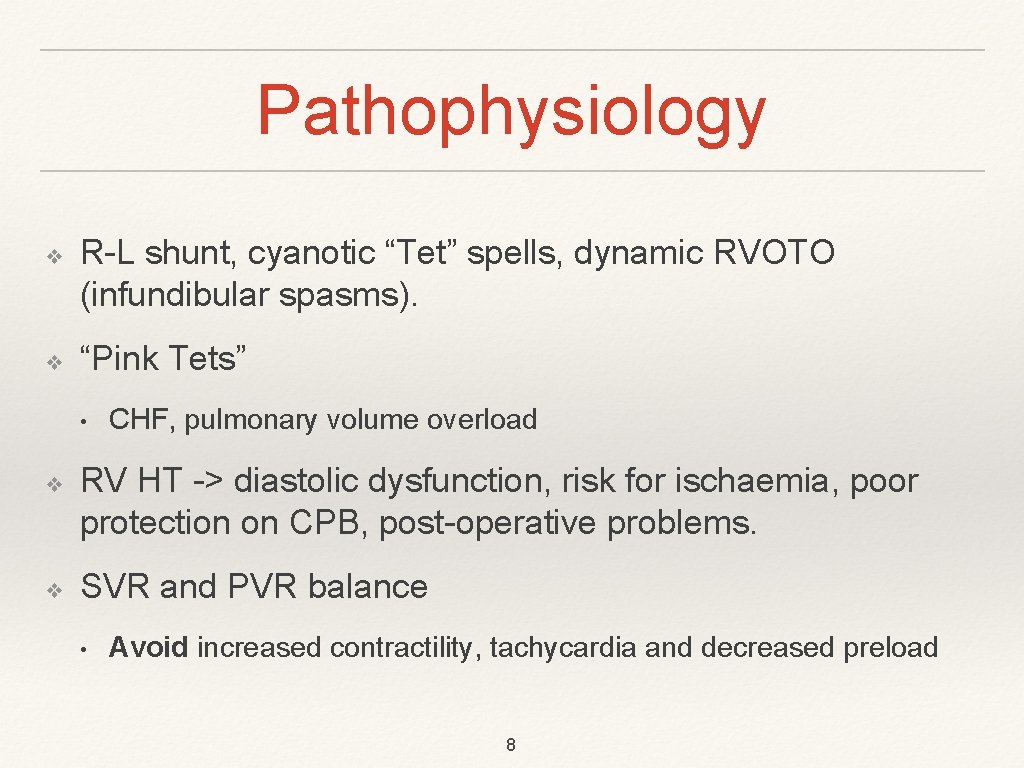
Pathophysiology ❖ ❖ R-L shunt, cyanotic “Tet” spells, dynamic RVOTO (infundibular spasms). “Pink Tets” • ❖ ❖ CHF, pulmonary volume overload RV HT -> diastolic dysfunction, risk for ischaemia, poor protection on CPB, post-operative problems. SVR and PVR balance • Avoid increased contractility, tachycardia and decreased preload 8
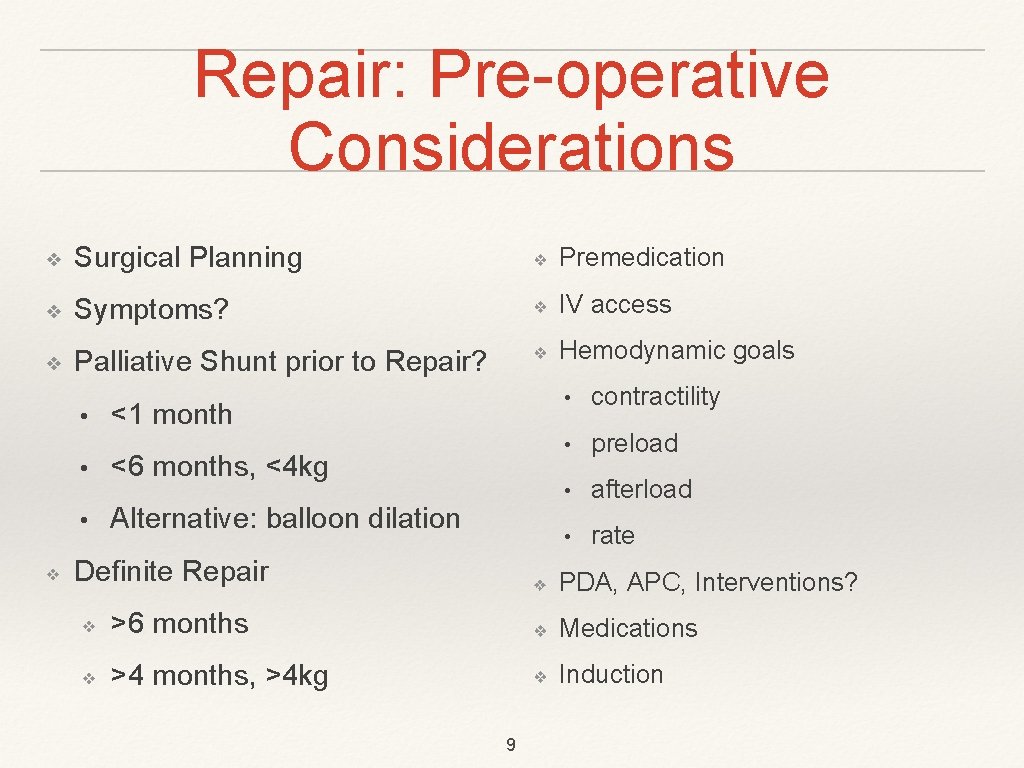
Repair: Pre-operative Considerations ❖ Surgical Planning ❖ Premedication ❖ Symptoms? ❖ IV access ❖ Palliative Shunt prior to Repair? ❖ Hemodynamic goals • ❖ <1 month • <6 months, <4 kg • Alternative: balloon dilation Definite Repair • contractility • preload • afterload • rate ❖ PDA, APC, Interventions? ❖ >6 months ❖ Medications ❖ >4 months, >4 kg ❖ Induction 9

Repair: Intraoperative Considerations ❖ ❖ PVR • ❖ ❖ • O 2, CO 2, p. H Perfusion Pressure • ❖ RV, LV Surgical Goals: • Relief of RVOTO • VSD repair • Preservation of RV function ❖ Morales et al. on Right Infundibular sparing 10 IM/IV: Ketamine, Fentanyl, Rocuronium, low-dose Sevoflurane Monitoring • NIRS • Invasive monitoring and CVC Rescue drugs, fluid, maneouvres ❖ ❖ ❖ Induction dangers, access and plan B alpha, IVF, beta-blocker, sevoflurane, abdominal pressure, position Maintenance ❖ Fentanyl ❖ Fast-track
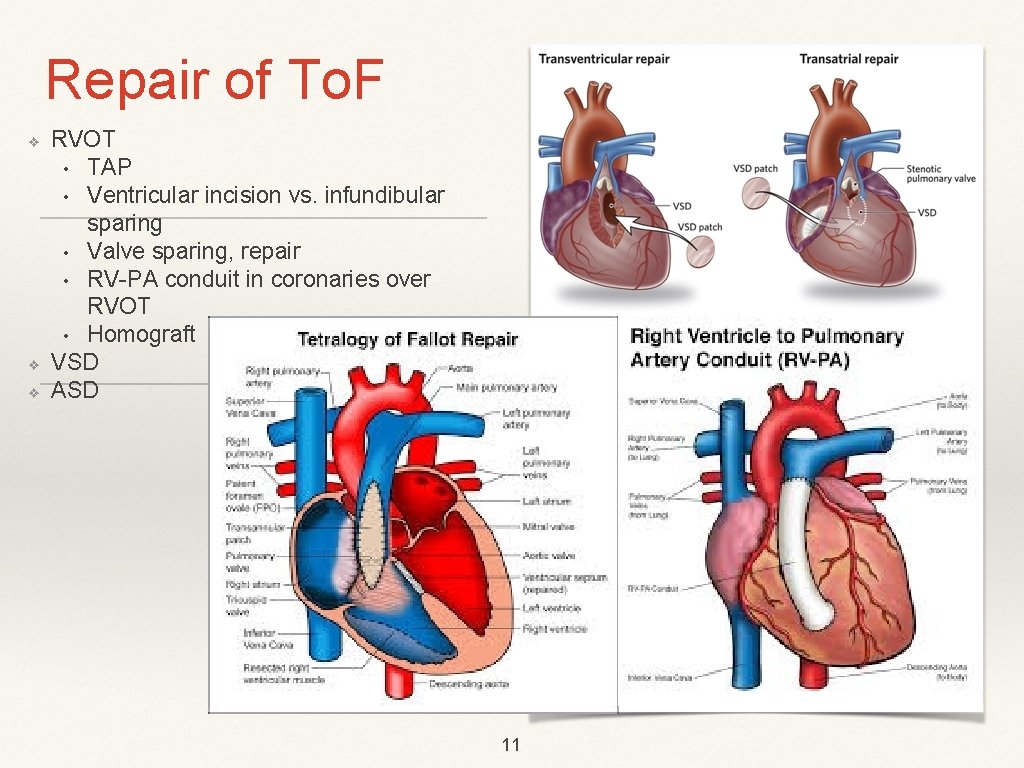
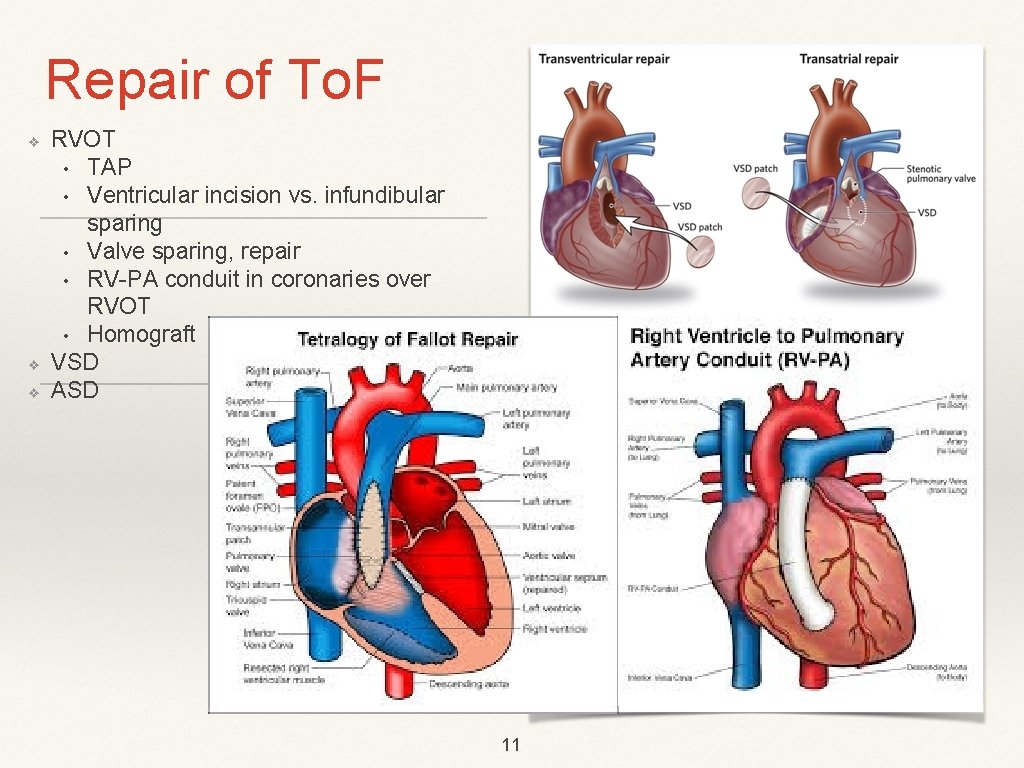
Repair of To. F ❖ ❖ ❖ RVOT • TAP • Ventricular incision vs. infundibular sparing • Valve sparing, repair • RV-PA conduit in coronaries over RVOT • Homograft VSD ASD 11

Post-operative and Late considerations ❖ RV function ❖ ❖ ❖ ❖ Inotropes, filling & RAp, PVR RVp: LVp (<0. 75) Disposition Conduction system (VSD); JET (10%) Cardiac Catherization • Pulmonary rehabilitation • BDs, Stents, APCs ❖ Redo: RV-PA conduit, PVR ❖ Mortality ❖ Shunt: physiological, post-op ventilation; thrombosis, stenosis ❖ Ventricular incision, TA patch and complications Predictors on CMR (LV CS, RV LS) Morbidity ❖ Ventricular function, ET ❖ Atrial Tachyarrhythmias (atrial dilation), VT ❖ Residual VSDs (>3 mm) ❖ QRS >180 s and PVR ❖ PBF: too much/little ❖ Aortic Dilation 12
To. F and non-Cardiac Surgery ❖ Pre-repair? Hemodynamic goals: C. R. A. P. ❖ Un-repaired with cyanosis? ❖ Earlier repairs with Transannuloplasty: PR and RV dilation ❖ Post-repair: • Function on history • Echo assessment, RVOT, PV, RV • PA: anatomy and haemodynamics • EPS: atrial tachy-arrhythmias (AF) • Role of CMR (see. Ezzat et al. ) 13
To. F: Key Points ❖ Most common form of cyanotic heart disease ❖ Hemodynamic Management Goals ❖ Unrepaired: PVR vs. SVR ❖ Repaired: ❖ ❖ Induction ❖ Post-op. complications ❖ Cath-lab pulmonary rehabilitation ❖ Late outcomes BTS: another time 14
 Tetralogy of fallot mnemonic
Tetralogy of fallot mnemonic Down syndrome physical exam
Down syndrome physical exam 5 cyanotic congenital heart disease
5 cyanotic congenital heart disease Tof pathophysiology
Tof pathophysiology Pink tof vs blue tof
Pink tof vs blue tof Tet spell
Tet spell Peds vital signs
Peds vital signs Tetralogy of fallot tet spell
Tetralogy of fallot tet spell Transportation of great arteries
Transportation of great arteries Ucsf cardiac anesthesia
Ucsf cardiac anesthesia Paramembranous vsd
Paramembranous vsd Anesthesia for cardiac tamponade
Anesthesia for cardiac tamponade Encuclillamiento tetralogia de fallot
Encuclillamiento tetralogia de fallot Tetralogia de fallot componentes
Tetralogia de fallot componentes Hipoksik hecme nedir
Hipoksik hecme nedir