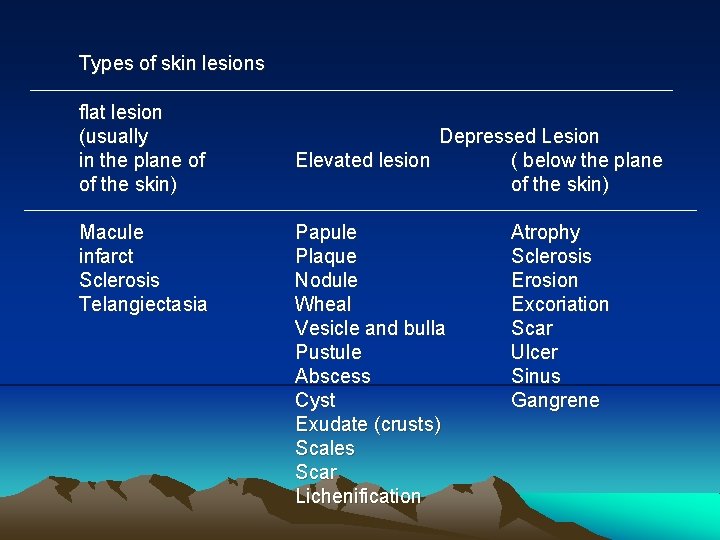
Types of skin lesions flat lesion usually in
- Slides: 18
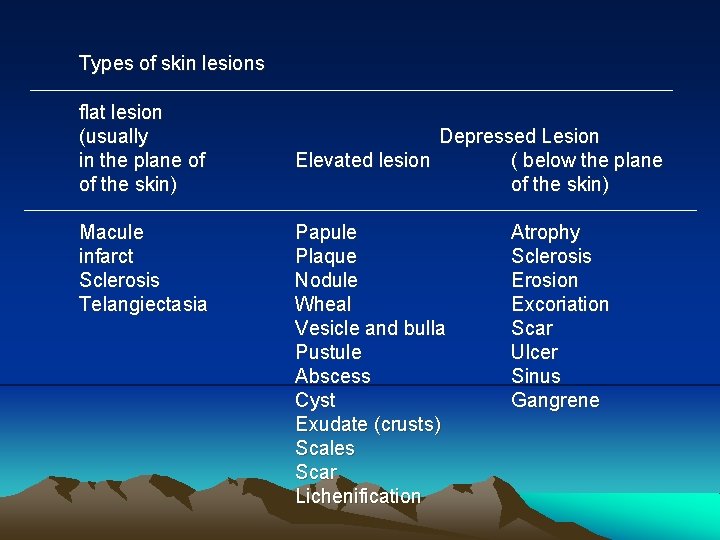
Types of skin lesions flat lesion (usually in the plane of of the skin) Macule infarct Sclerosis Telangiectasia Depressed Lesion Elevated lesion ( below the plane of the skin) Papule Plaque Nodule Wheal Vesicle and bulla Pustule Abscess Cyst Exudate (crusts) Scales Scar Lichenification Atrophy Sclerosis Erosion Excoriation Scar Ulcer Sinus Gangrene
The Structure of Skin Lesions and Fundamentals of Diagnosis
An Approach to Dermatologic Diagnosis
1. Initial clinical impression: I. Does the patient appear ill? II. Physical examination—detailed examination of skin, hair, nails, and mucous membranes
A. Four cardinal features 1. Type of lesion: macule, papule, nodule, vesicle, etc. ? 2. Shape of individual lesions: annular, iris, arciform, linear, round, oval, umbilicated, etc. ? 3. Arrangement of multiple lesions: isolated, scattered, grouped, herpetiform, zosteriform, annular, arciform, linear, reticular, etc. ?
4. Distribution to be sure to examine scalp, mouth, palms, and soles) a. Extent of involvement: circumscribed, regional, generalized, universal? What percentage of the body surface is involved (the palm is roughly equivalent to 1%)? b. Pattern: symmetry, exposed areas, sites of pressure, intertriginous areas? c. Characteristic location: flexural, extensor, intertriginous, glabrous, palms and soles, dermatomal, trunk, lower extremities, exposed areas, etc. ?
B. Three major characteristics 1. Color a. If diffuse: red, brown, gray-blue, white, blue, orange-yellow, etc. ; or if circumscribed: red. violaceous, orange, yellow, lilac, livid, brown, black, blue, gray, white, etc. ? b. Does color blanch with pressure (diascopy test)? c. Wood's lamp examination of pigmentary alterations: Is contrast enhanced
2. Consistency and feel of lesion: soft, doughy, firm, hard, "infiltrated, " dry, moist, mobile, tender? 3. Anatomic component(s) of skin primarily affected: Is the process epidermal, subcutaneous, appendageal. or a combination of these?
III. General physical examination as indicated by clinical presentation and differential diagnosis, with particular attention to vital signs, lymphadenopathy, hepatomegaly, splenomegaly, joints. IV. History of skin lesions. Seven key questions:
A. When did it start? B. Does it itch, burn, or hurt? C. Where on the body did it start? D. How has it spread? (Pattern of spread) E. How have individual lesions changed? (Evolution) F. Provocative factors? G. Previous treatment(s)?
V. General history of present illness as indicated by clinical situation, with particular attention to constitutional and prodromal symptoms. A. Acute illness syndrome (fever, sweats, chills, headache, nausea, vomiting, etc. )? B. Chronic illness syndrome (fatigue, anorexia, weight loss, malaise)?
VI. Review of systems as indicated by clinical situation, with particular attention to possible connections between cutaneous signs and diseases of other organ systems (e. g. , rheumatic complaints: myalgias, arthralgias. Raynaud's phenomenon, sicca symptoms).
VII. Past medical history A. Operations B. Illnesses C. Allergies, especially drug-allergies D. Medications (present and past) E. Habits (smoking, alcohol intake, drug abuse) F. Atopic history (asthma, hay fever, eczema)
VIII. Family medical history (particularly of skin disorders and of atopy) IX. Social history, with particular reference to occupation, hobbies, exposures, travel. X. Sexual history XI. Laboratory studies
A. Special procedures 1. Biopsy for histopathologic and other analyses, if indicated, e. g. , electron microscopy, immuno fluorescence. With inflammatory nodules, obtain tissue to be minced for bacterial and fungal cultures as well.
2. Gram's stain of crusts, scales, or exudate. 3. KOH prep for yeast or fungi. 4. Cytologic preparation (Tzanck smear) in vesicular and bullous eruptions: direct smear of base for giant cells (seen in herpes simplex or varicella-zoster).
5. Bacteriologic, viral, and fungal cultures as indicated. 6. Wood's lamp examination of urine for porphyrins and of hair and skin for fluorescence, and for changes in pigmentation. 7. Scraping for scabies mite. 8. Patch tests 9. Acetowhitening
B. General: hematology, chemistry, urmalysis, serologic tests (e. g. STS ANA), stool examination, and imaging studies. • Xll. Final diagnosis: reexamination over time, and more than one biopsy may be required for definitive diagnosis.