Types of Secretory Glands Single Cell mucous cells
- Slides: 39
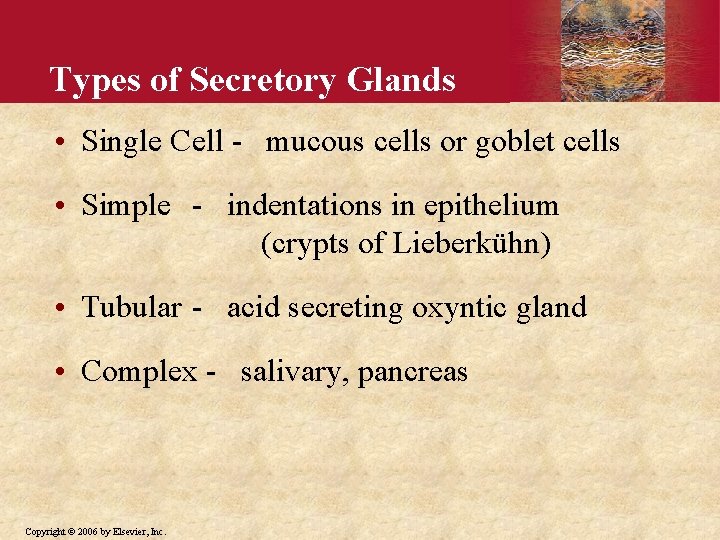
Types of Secretory Glands • Single Cell - mucous cells or goblet cells • Simple - indentations in epithelium (crypts of Lieberkühn) • Tubular - acid secreting oxyntic gland • Complex - salivary, pancreas Copyright © 2006 by Elsevier, Inc.
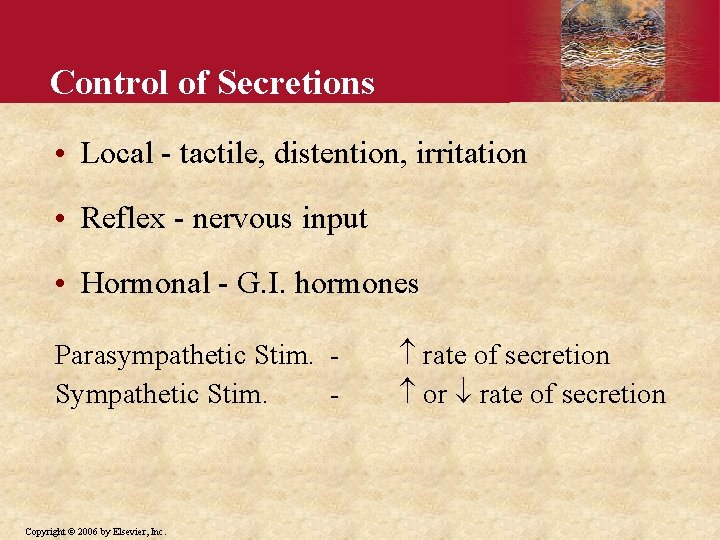
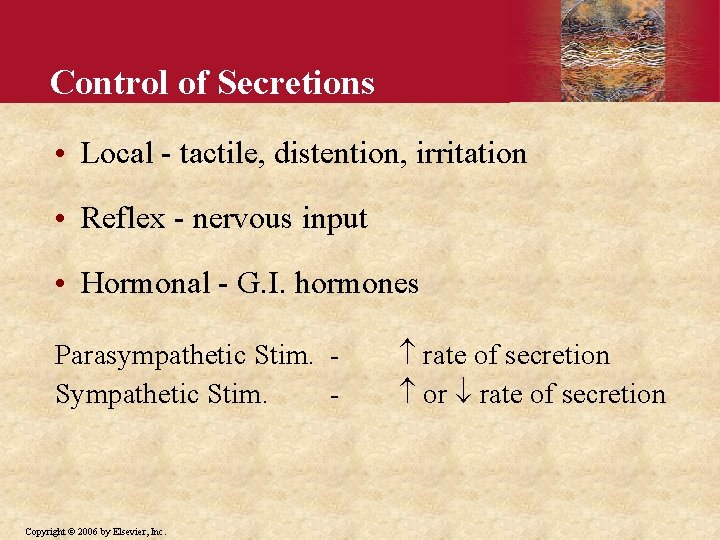
Control of Secretions • Local - tactile, distention, irritation • Reflex - nervous input • Hormonal - G. I. hormones Parasympathetic Stim. Sympathetic Stim. - Copyright © 2006 by Elsevier, Inc. rate of secretion or rate of secretion
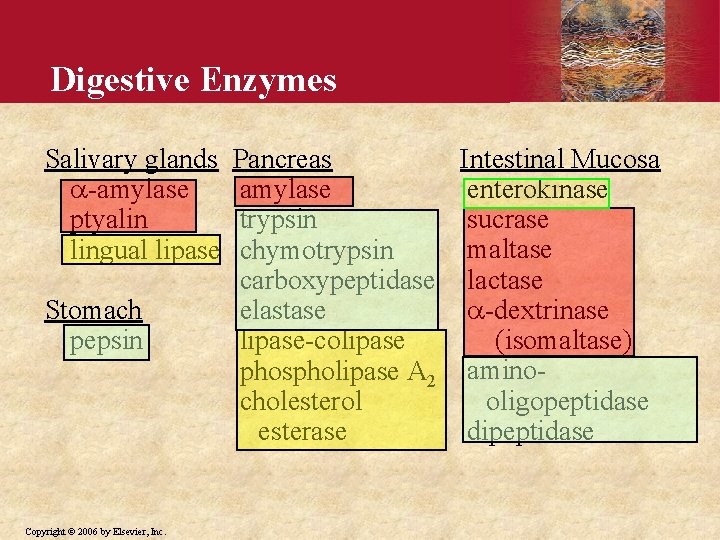
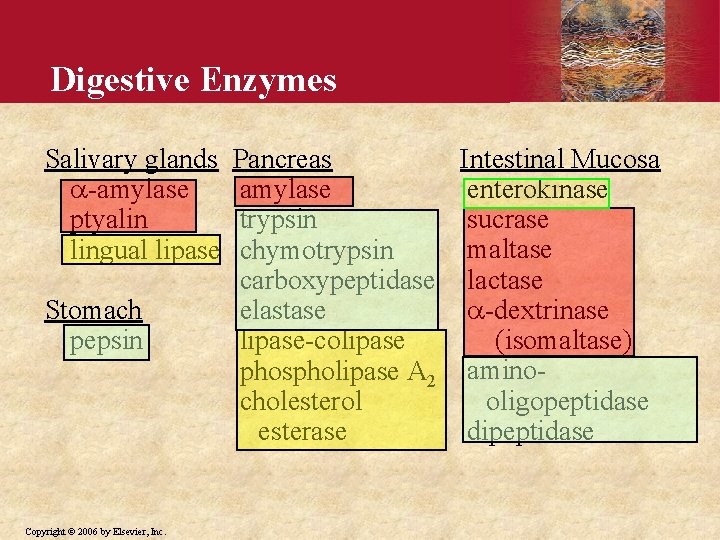
Digestive Enzymes Salivary glands -amylase ptyalin lingual lipase Stomach pepsin Copyright © 2006 by Elsevier, Inc. Intestinal Mucosa Pancreas enterokinase amylase sucrase trypsin maltase chymotrypsin carboxypeptidase lactase -dextrinase elastase (isomaltase) lipase-colipase phospholipase A 2 aminooligopeptidase cholesterol dipeptidase esterase
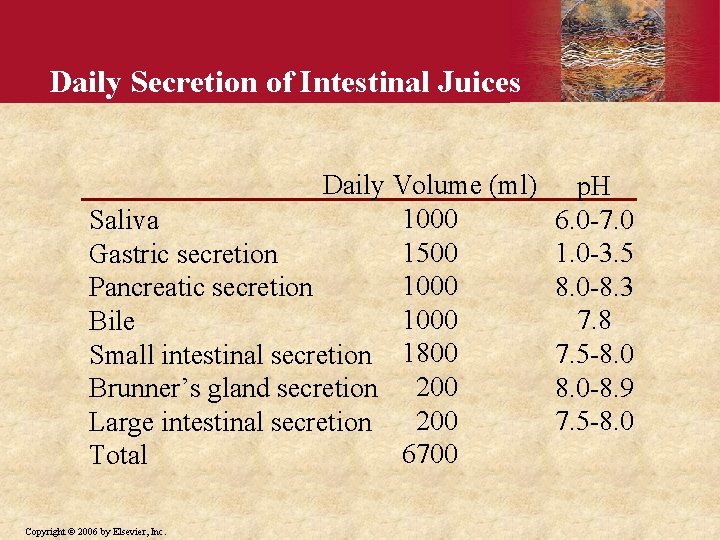
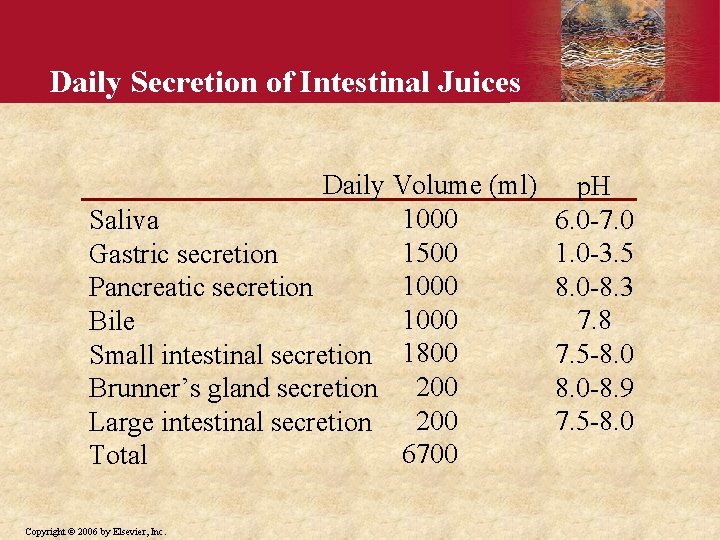
Daily Secretion of Intestinal Juices Daily Volume (ml) 1000 Saliva 1500 Gastric secretion 1000 Pancreatic secretion 1000 Bile Small intestinal secretion 1800 Brunner’s gland secretion 200 Large intestinal secretion 6700 Total Copyright © 2006 by Elsevier, Inc. p. H 6. 0 -7. 0 1. 0 -3. 5 8. 0 -8. 3 7. 8 7. 5 -8. 0 -8. 9 7. 5 -8. 0
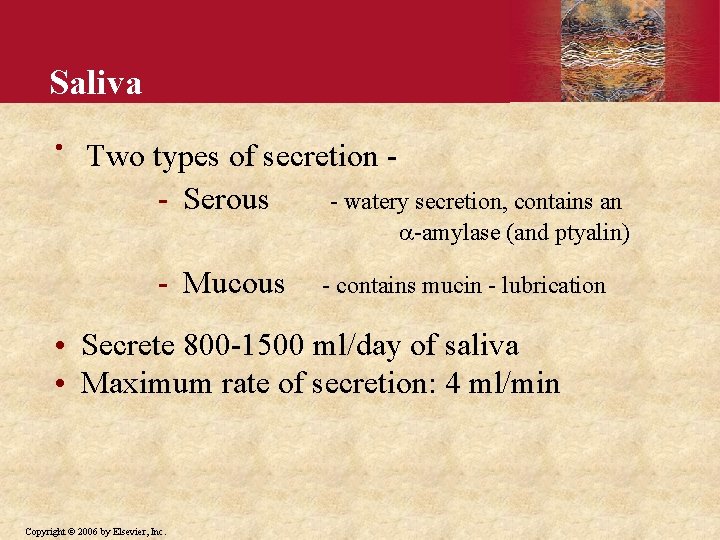
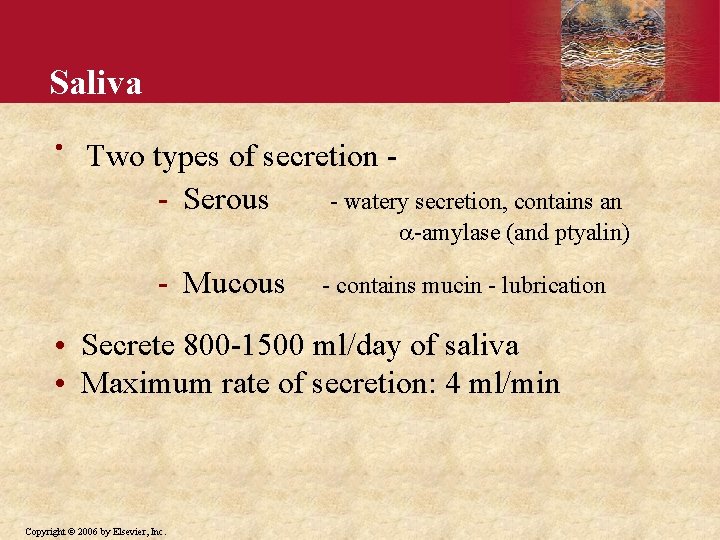
Saliva • Two types of secretion - Serous - watery secretion, contains an -amylase (and ptyalin) - Mucous - contains mucin - lubrication • Secrete 800 -1500 ml/day of saliva • Maximum rate of secretion: 4 ml/min Copyright © 2006 by Elsevier, Inc.
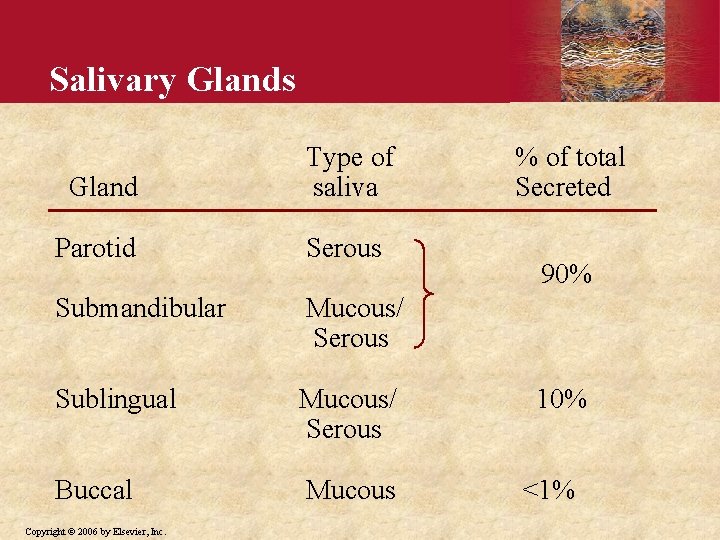
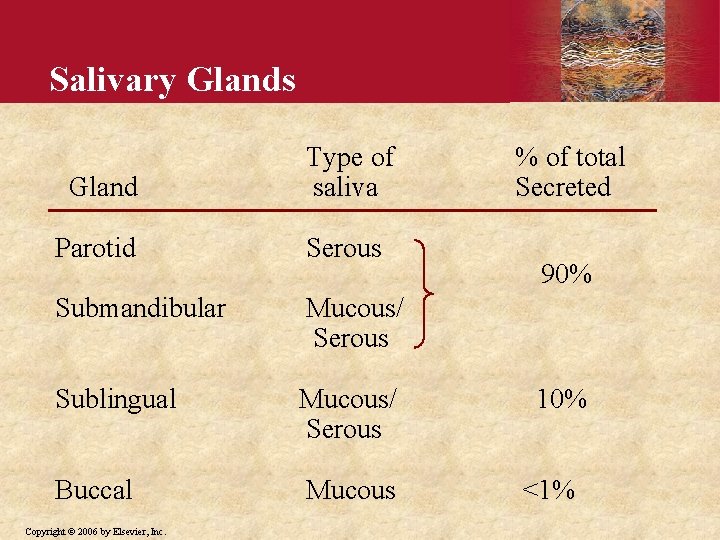
Salivary Glands Gland Type of saliva Parotid Serous Submandibular Mucous/ Serous Sublingual Mucous/ Serous Buccal Mucous Copyright © 2006 by Elsevier, Inc. % of total Secreted 90% 10% <1%
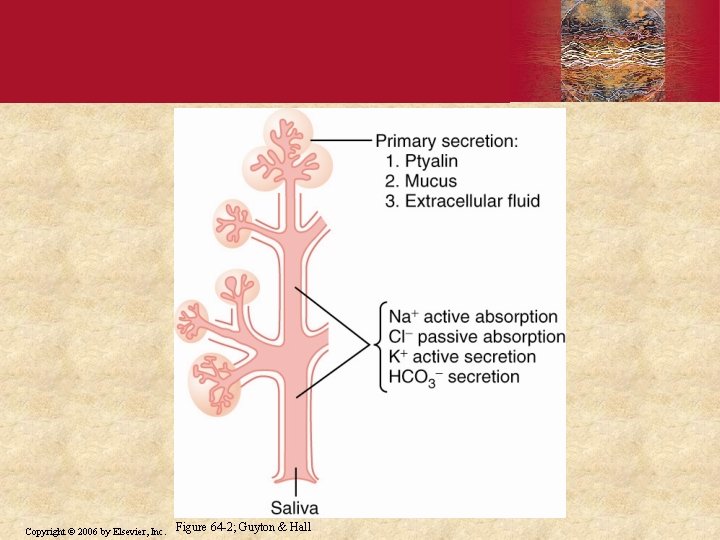
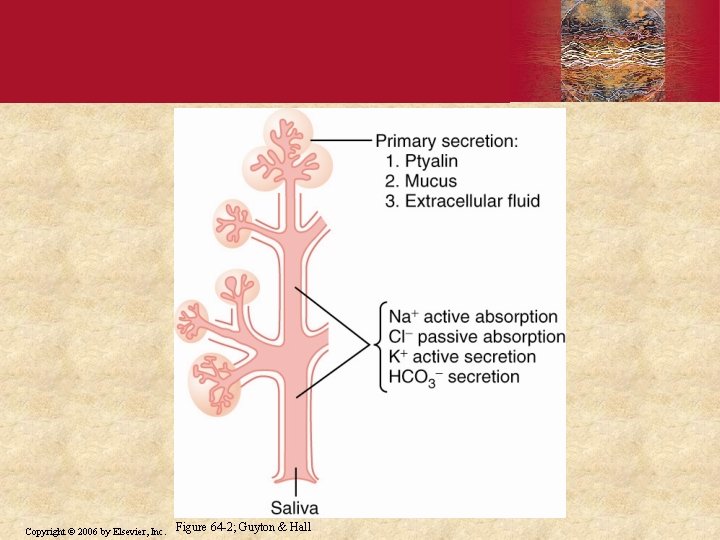
Copyright © 2006 by Elsevier, Inc. Figure 64 -2; Guyton & Hall
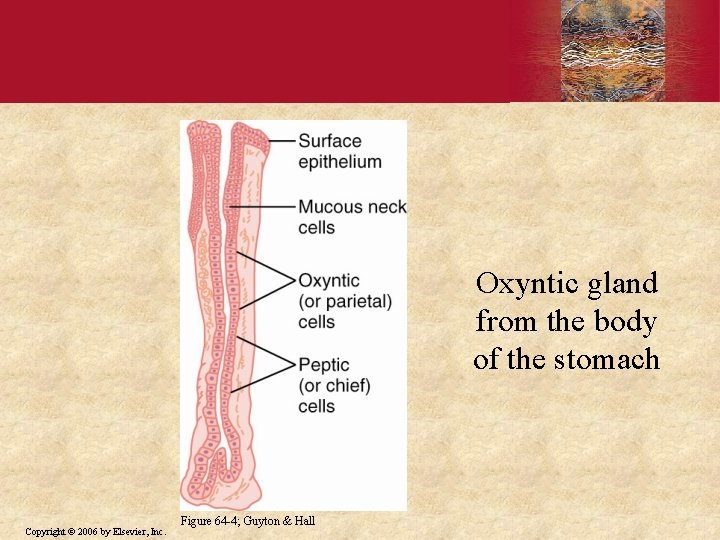
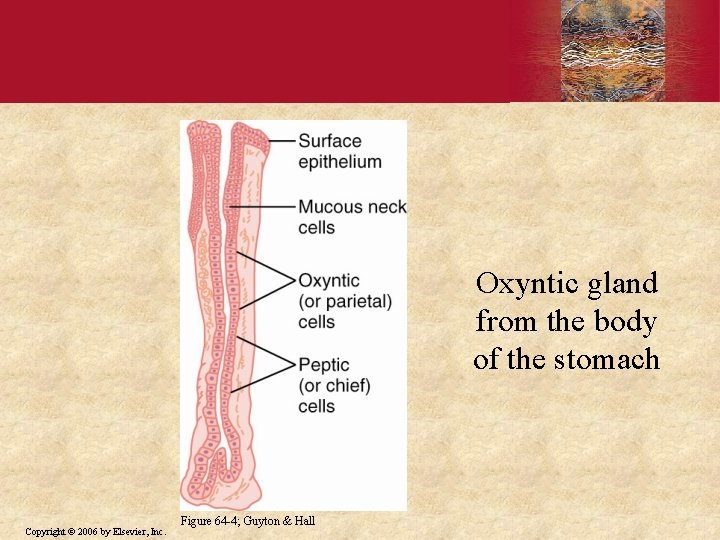
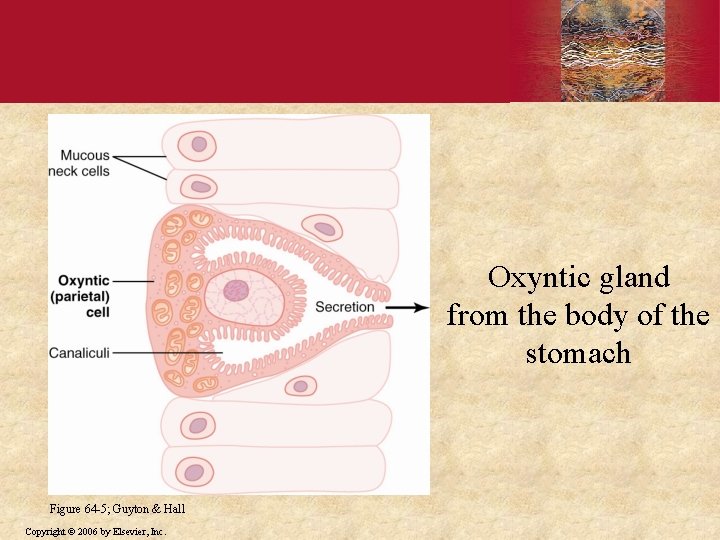
Oxyntic gland from the body of the stomach Copyright © 2006 by Elsevier, Inc. Figure 64 -4; Guyton & Hall
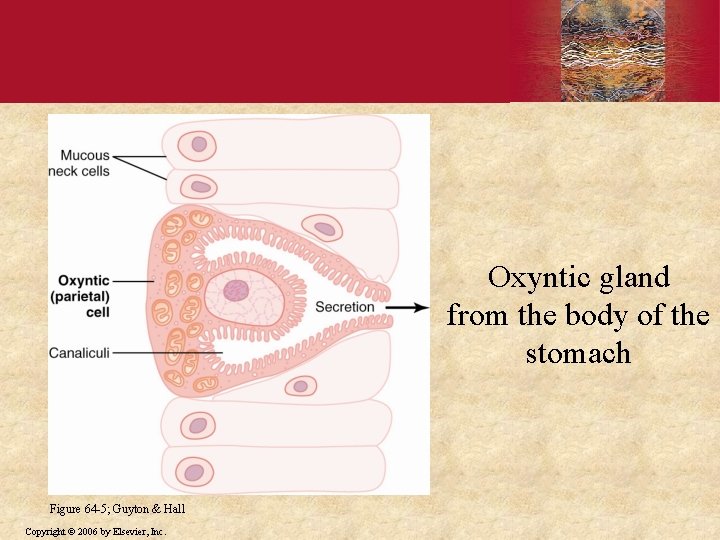
Oxyntic gland from the body of the stomach Figure 64 -5; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
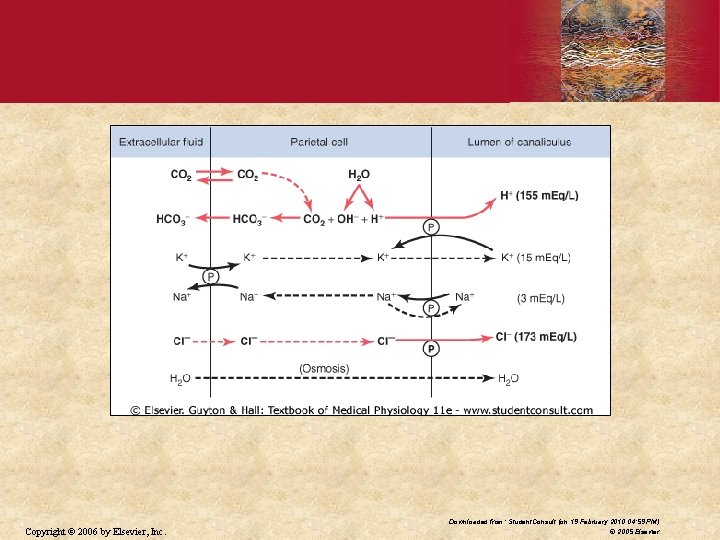
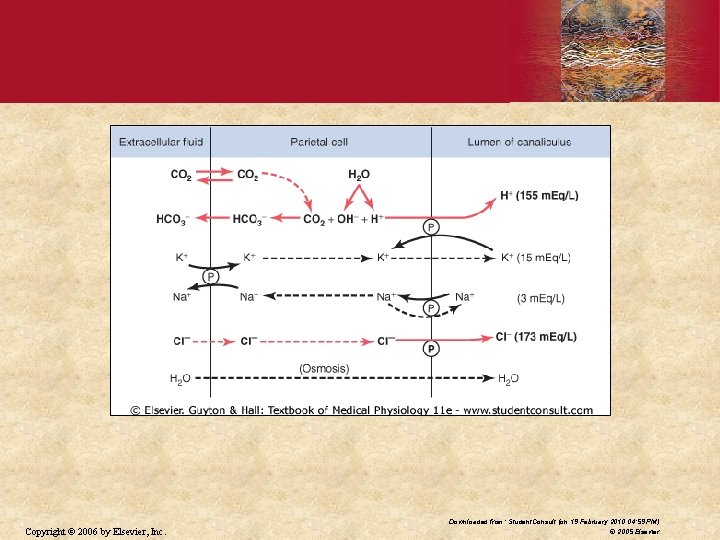
Copyright © 2006 by Elsevier, Inc. Downloaded from: Student. Consult (on 19 February 2010 04: 59 PM) © 2005 Elsevier
Gastric Acid • Three major functions - Bacteriostatic - Converts pepsinogen to pepsin - Begins protein digestion (with pepsin) Copyright © 2006 by Elsevier, Inc.
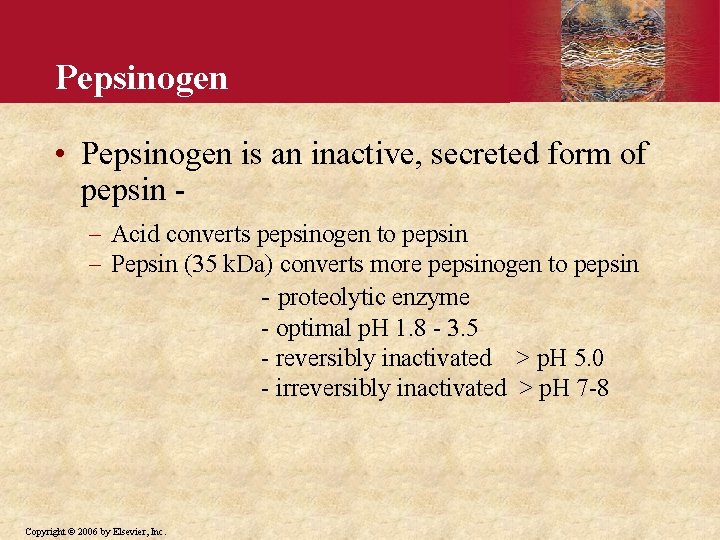
Pepsinogen • Pepsinogen is an inactive, secreted form of pepsin Acid converts pepsinogen to pepsin Pepsin (35 k. Da) converts more pepsinogen to pepsin - proteolytic enzyme - optimal p. H 1. 8 - 3. 5 - reversibly inactivated > p. H 5. 0 - irreversibly inactivated > p. H 7 -8 Copyright © 2006 by Elsevier, Inc.
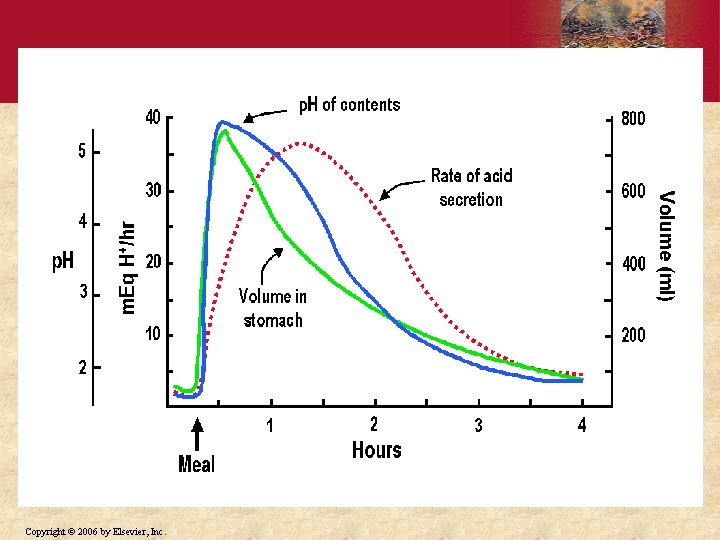
Copyright © 2006 by Elsevier, Inc.
Peptic Ulcers • Peptic ulcers occur when damaging effects of acid and pepsin overcome ability of mucosa to protect itself Gastric ulcers - main problem is decreased ability of mucosa to protect itself Duodenal ulcers - main problem is exposure to increased amounts of acid and pepsin Copyright © 2006 by Elsevier, Inc.
Treatment of Peptic Ulcers • Antacids • H 2 receptor blockers - Rantidine (Zantac) - Cimetidine (Tagamet) • Proton pump inhibitors - Omeparazole (Prilosec) • Antibiotics • Surgical (rare) Copyright © 2006 by Elsevier, Inc. - vagotomy - antrectomy
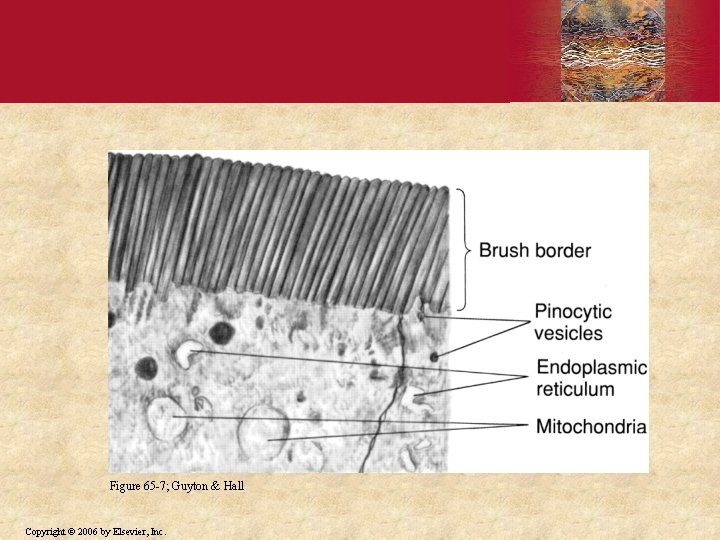
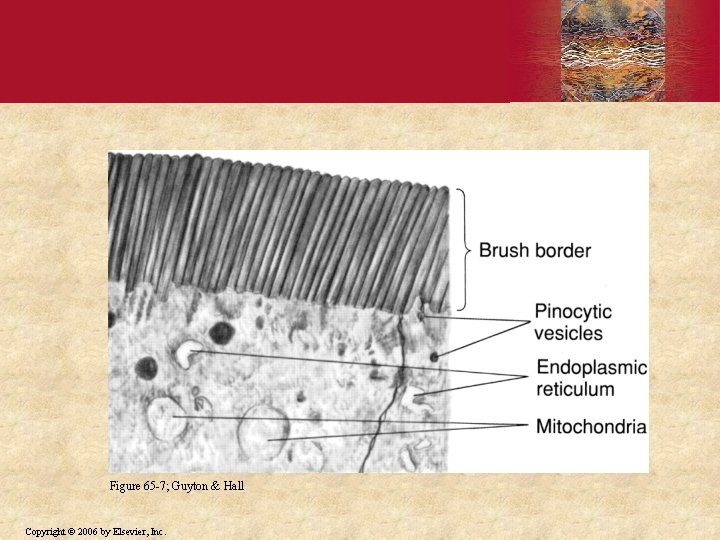
Figure 65 -7; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
Pancreas • As chyme floods into small intestine two things must happen: Acid must be neutralized to prevent damage to duodenal mucosa Macromolecular nutrients - proteins, fats and starch must be broken down much further so their constituents can be absorbed Copyright © 2006 by Elsevier, Inc.
Pancreas • Pancreas plays vital role in accomplishing both objectives Digestive enzymes for all food types Bicarbonate solution to neutralize acid chyme Copyright © 2006 by Elsevier, Inc.
Internal Structure of Pancreas • Compound gland with structure similar to salivary gland • Acini - grape-like clusters of cells that store and secrete digestive enzymes • Ducts - secrete bicarbonate Intercalated ducts - receive secretions from acini Intralobular ducts - receive fluid from intercalated ducts Copyright © 2006 by Elsevier, Inc.
Enzymes for Protein Digestion • Proteolytic enzymes - Trypsin Cleaves proteins to polypeptides - Chymotrypsin - Carboxypeptidase Copyright © 2006 by Elsevier, Inc. Cleaves polypeptides to AA
Enzymes for Carbohydrate Digestion • Pancreatic amylase - starches - glycogen to disaccharides Copyright © 2006 by Elsevier, Inc.
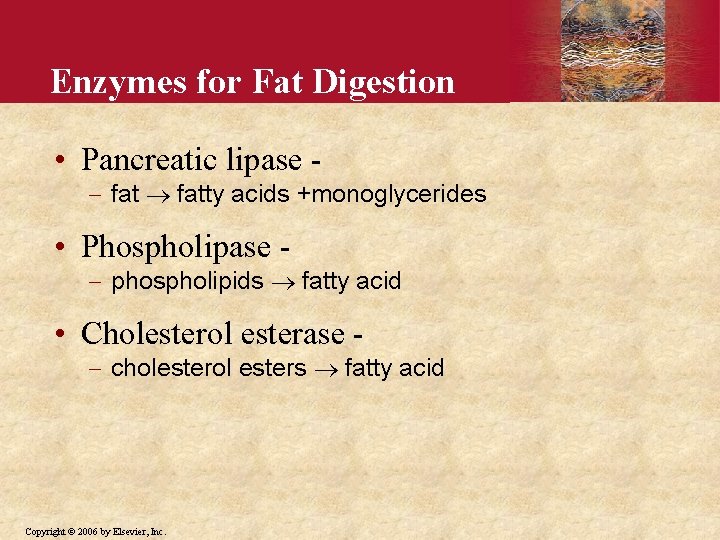
Enzymes for Fat Digestion • Pancreatic lipase - fatty acids +monoglycerides • Phospholipase - phospholipids fatty acid • Cholesterol esterase - cholesterol esters fatty acid Copyright © 2006 by Elsevier, Inc.
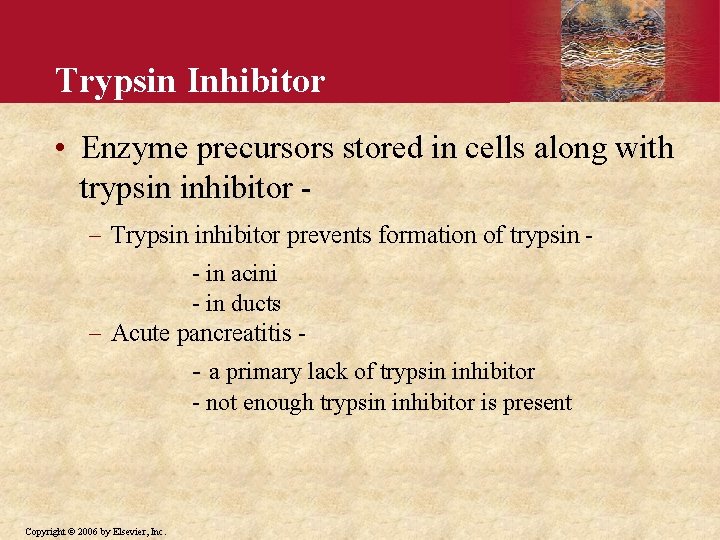
Why Doesn’t the Pancreas Digest Itself? • Pancreatic proteolytic enzymes are stored and secreted in an inactive form - (also, a trypsin inhibitor is present in cells) trypsinogen chymotrypsinogen trypsin procarboxypeptidase Copyright © 2006 by Elsevier, Inc. chymotrypsin carboxypeptidase
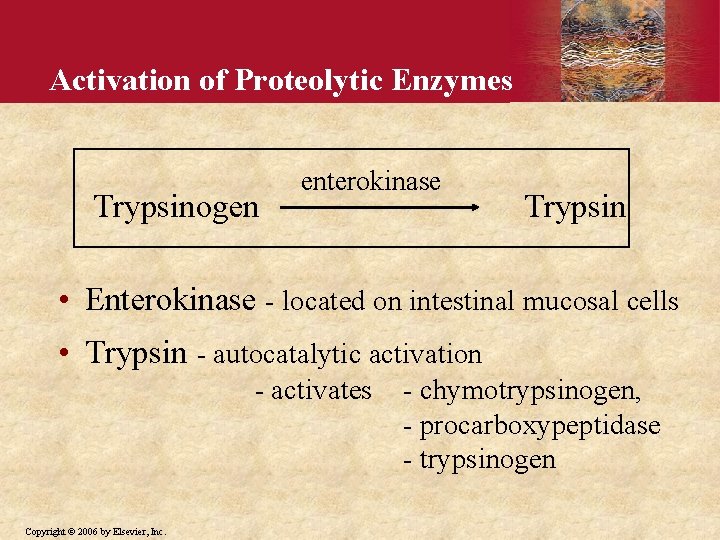
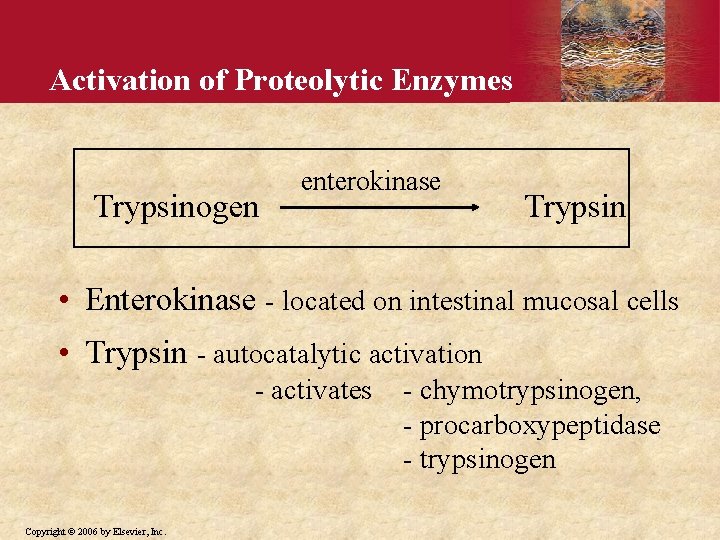
Activation of Proteolytic Enzymes Trypsinogen enterokinase Trypsin • Enterokinase - located on intestinal mucosal cells • Trypsin - autocatalytic activation - activates Copyright © 2006 by Elsevier, Inc. - chymotrypsinogen, - procarboxypeptidase - trypsinogen
Trypsin Inhibitor • Enzyme precursors stored in cells along with trypsin inhibitor Trypsin inhibitor prevents formation of trypsin - in acini - in ducts Acute pancreatitis - - a primary lack of trypsin inhibitor - not enough trypsin inhibitor is present Copyright © 2006 by Elsevier, Inc.
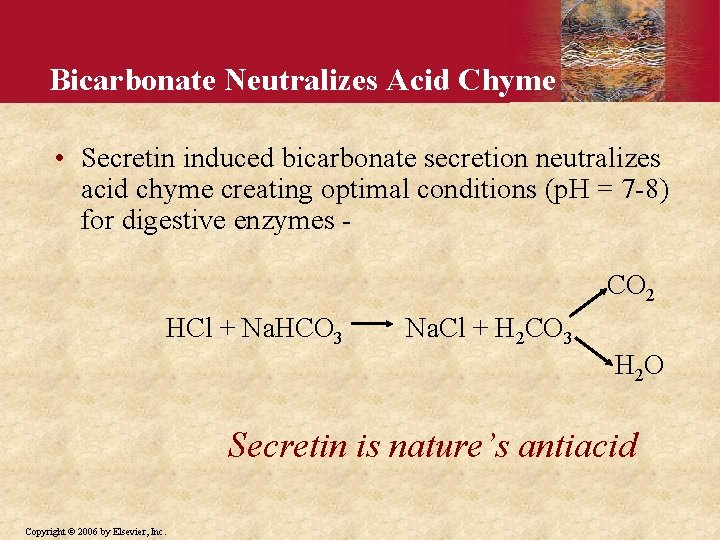
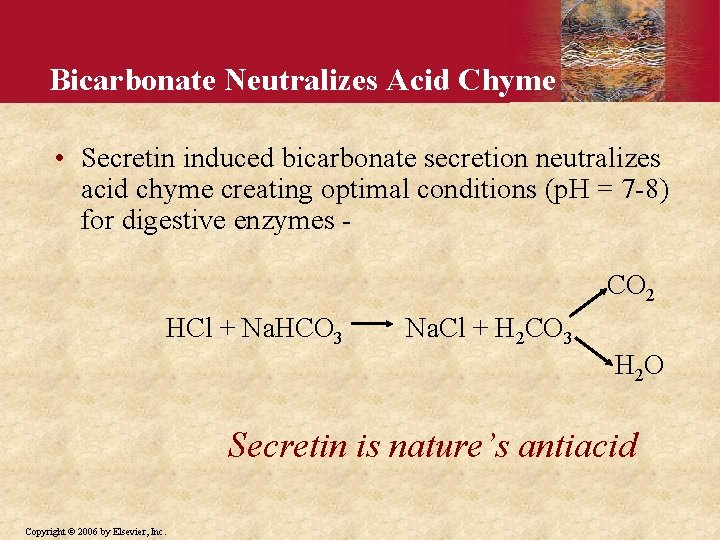
Bicarbonate Neutralizes Acid Chyme • Secretin induced bicarbonate secretion neutralizes acid chyme creating optimal conditions (p. H = 7 -8) for digestive enzymes CO 2 HCl + Na. HCO 3 Na. Cl + H 2 CO 3 H 2 O Secretin is nature’s antiacid Copyright © 2006 by Elsevier, Inc.
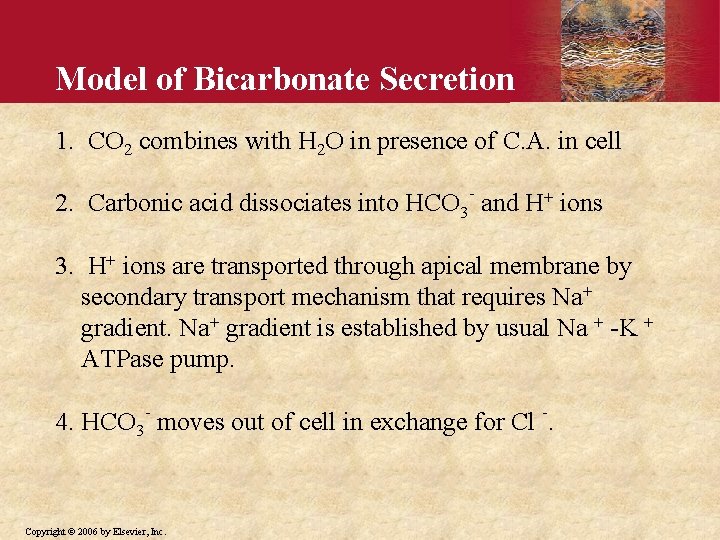
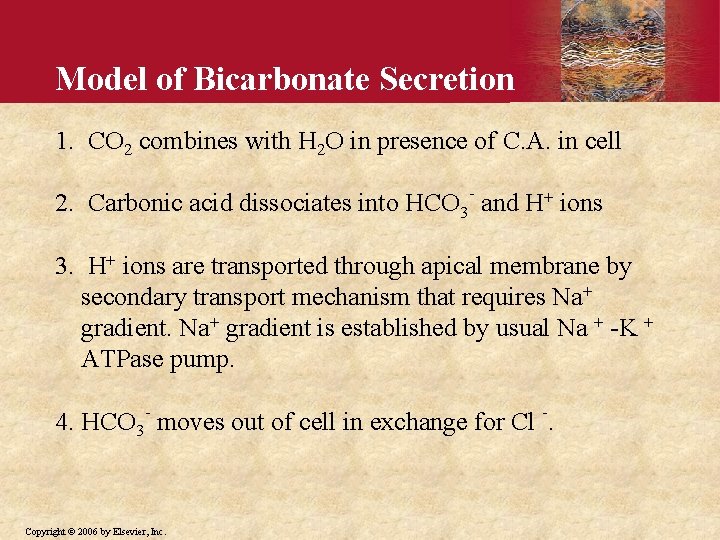
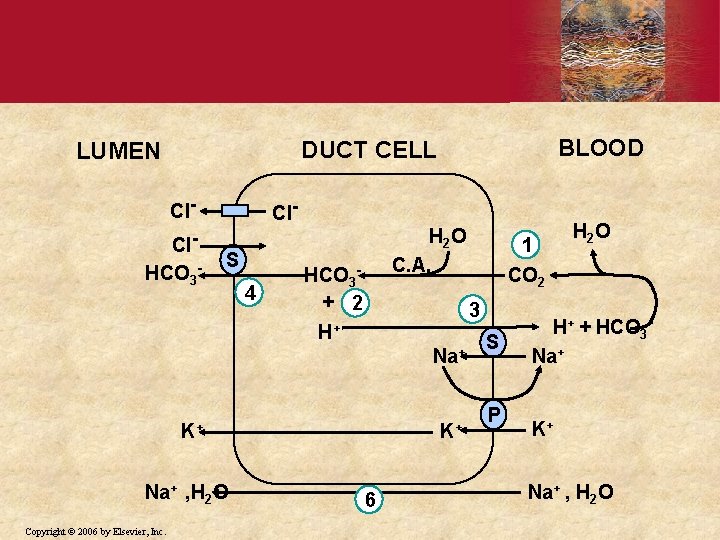
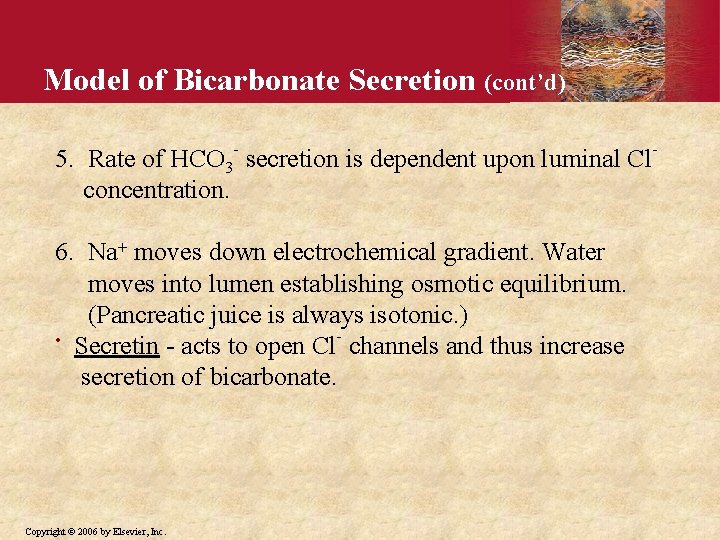
Model of Bicarbonate Secretion 1. CO 2 combines with H 2 O in presence of C. A. in cell 2. Carbonic acid dissociates into HCO 3 - and H+ ions 3. H+ ions are transported through apical membrane by secondary transport mechanism that requires Na+ gradient is established by usual Na + -K + ATPase pump. 4. HCO 3 - moves out of cell in exchange for Cl -. Copyright © 2006 by Elsevier, Inc.
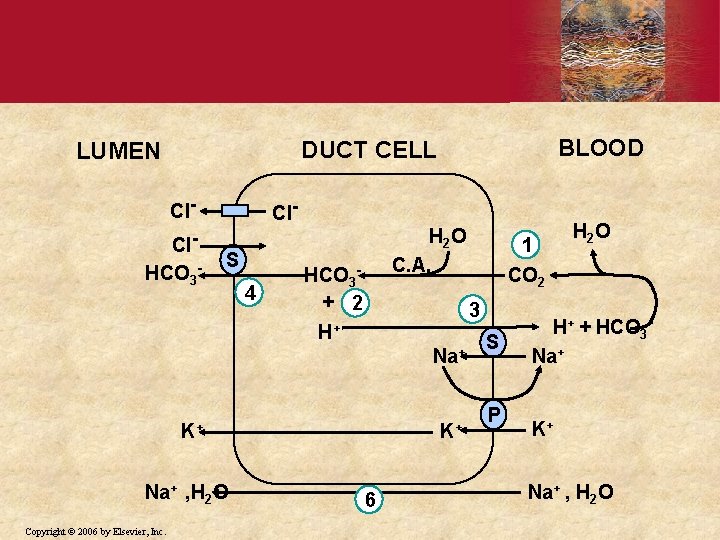
BLOOD DUCT CELL LUMEN Cl. HCO 3 - Cl. S 4 H 2 O C. A. HCO 3+ 2 Na+ K+ Copyright © 2006 by Elsevier, Inc. CO 2 3 H+ Na+ , H 2 O 1 K+ 6 H 2 O S P H+ + HCO 3 Na+ K+ Na+ , H 2 O
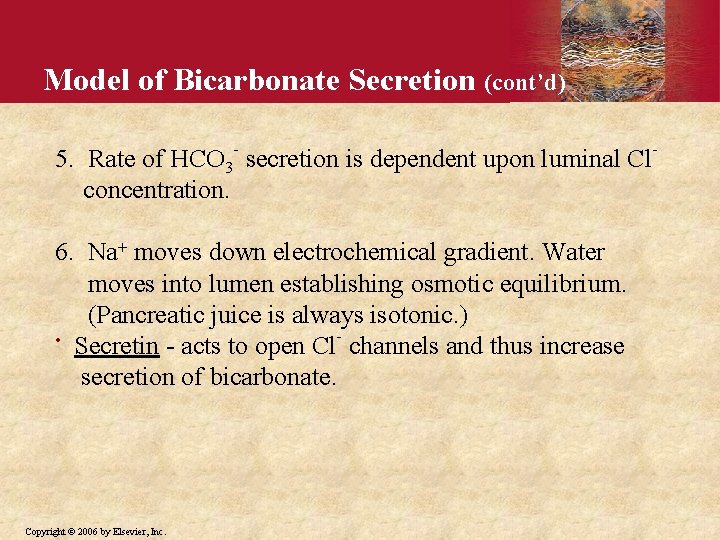
Model of Bicarbonate Secretion (cont’d) 5. Rate of HCO 3 - secretion is dependent upon luminal Clconcentration. 6. Na+ moves down electrochemical gradient. Water moves into lumen establishing osmotic equilibrium. (Pancreatic juice is always isotonic. ) • Secretin - acts to open Cl- channels and thus increase secretion of bicarbonate. Copyright © 2006 by Elsevier, Inc.
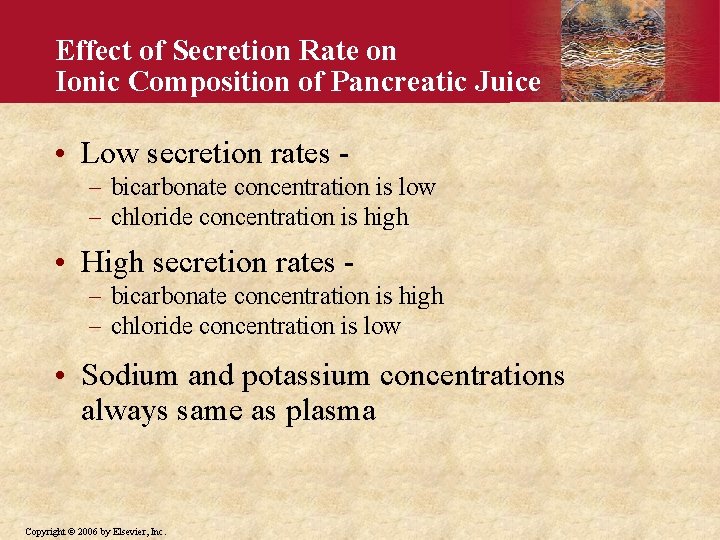
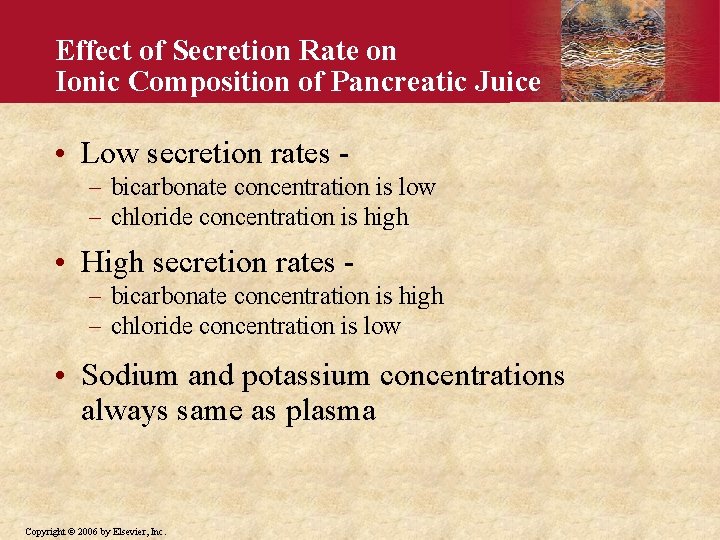
Effect of Secretion Rate on Ionic Composition of Pancreatic Juice • Low secretion rates - bicarbonate concentration is low chloride concentration is high • High secretion rates - bicarbonate concentration is high chloride concentration is low • Sodium and potassium concentrations always same as plasma Copyright © 2006 by Elsevier, Inc.
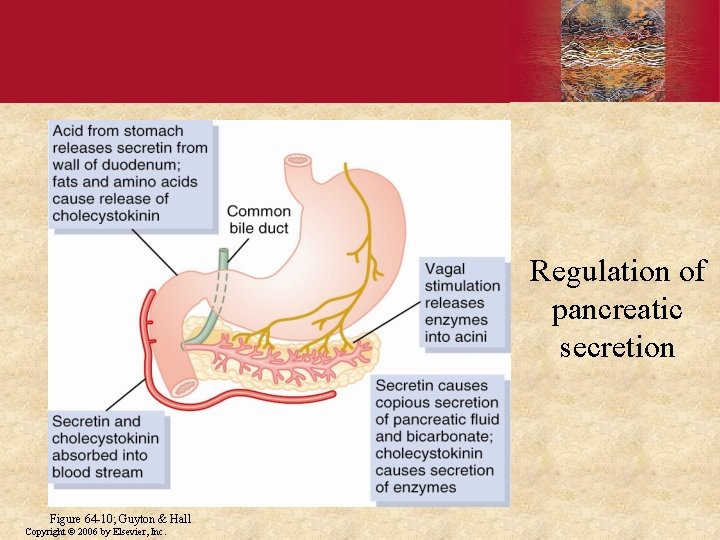
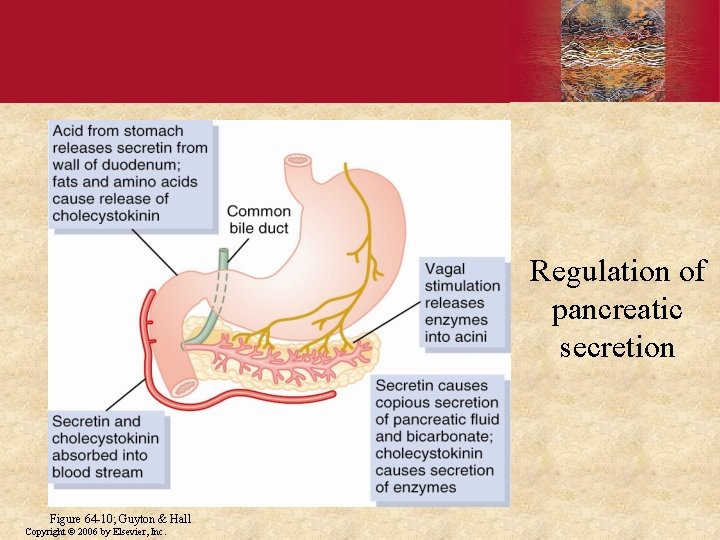
Regulation of pancreatic secretion Figure 64 -10; Guyton & Hall Copyright © 2006 by Elsevier, Inc.
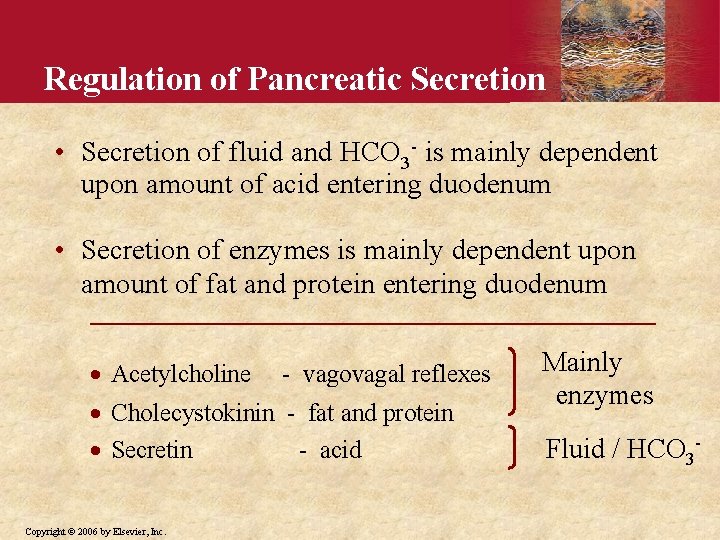
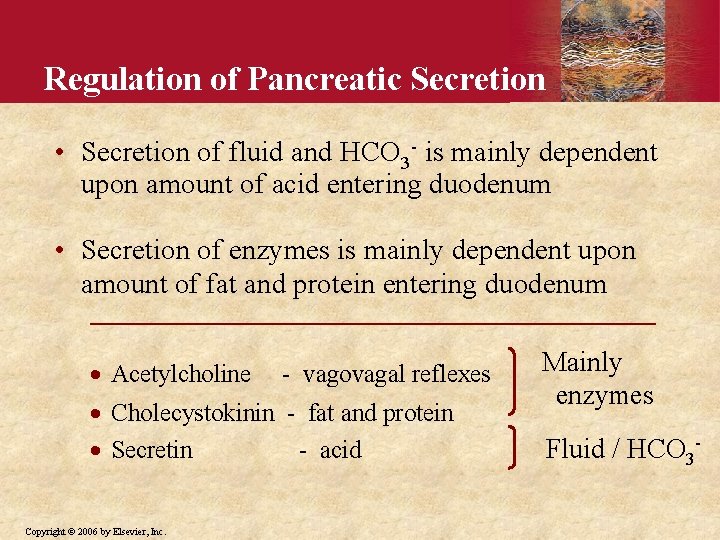
Regulation of Pancreatic Secretion • Secretion of fluid and HCO 3 - is mainly dependent upon amount of acid entering duodenum • Secretion of enzymes is mainly dependent upon amount of fat and protein entering duodenum · Acetylcholine - vagovagal reflexes · Cholecystokinin - fat and protein · Secretin - acid Copyright © 2006 by Elsevier, Inc. Mainly enzymes Fluid / HCO 3 -
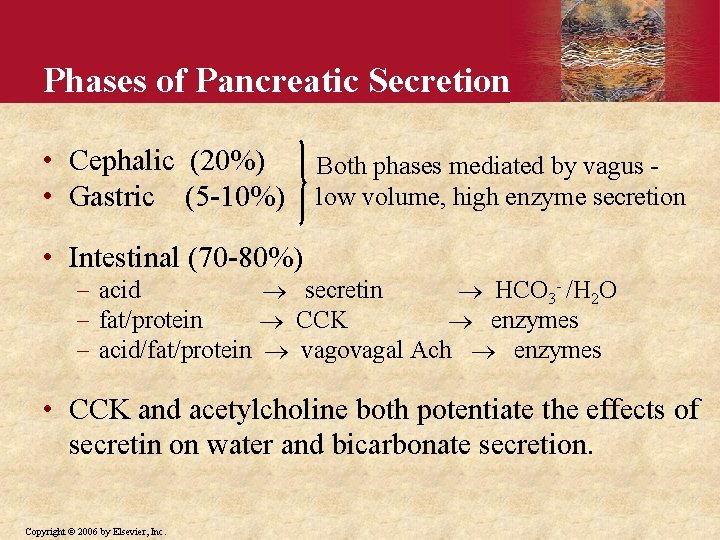
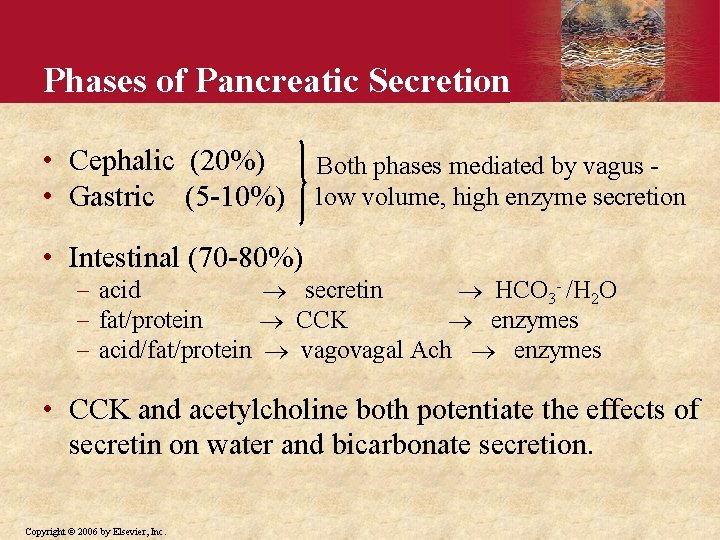
Phases of Pancreatic Secretion • Cephalic (20%) • Gastric (5 -10%) Both phases mediated by vagus low volume, high enzyme secretion • Intestinal (70 -80%) acid secretin HCO 3 - /H 2 O fat/protein CCK enzymes acid/fat/protein vagovagal Ach enzymes • CCK and acetylcholine both potentiate the effects of secretin on water and bicarbonate secretion. Copyright © 2006 by Elsevier, Inc.
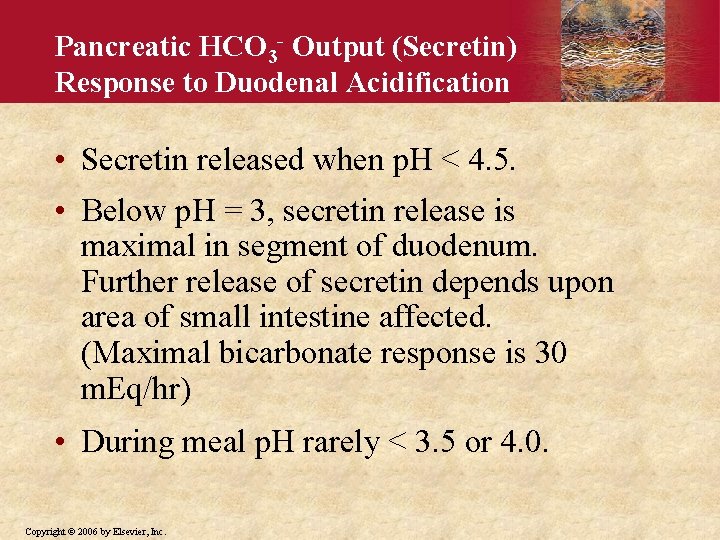
Pancreatic HCO 3 - Output (Secretin) Response to Duodenal Acidification • Secretin released when p. H < 4. 5. • Below p. H = 3, secretin release is maximal in segment of duodenum. Further release of secretin depends upon area of small intestine affected. (Maximal bicarbonate response is 30 m. Eq/hr) • During meal p. H rarely < 3. 5 or 4. 0. Copyright © 2006 by Elsevier, Inc.
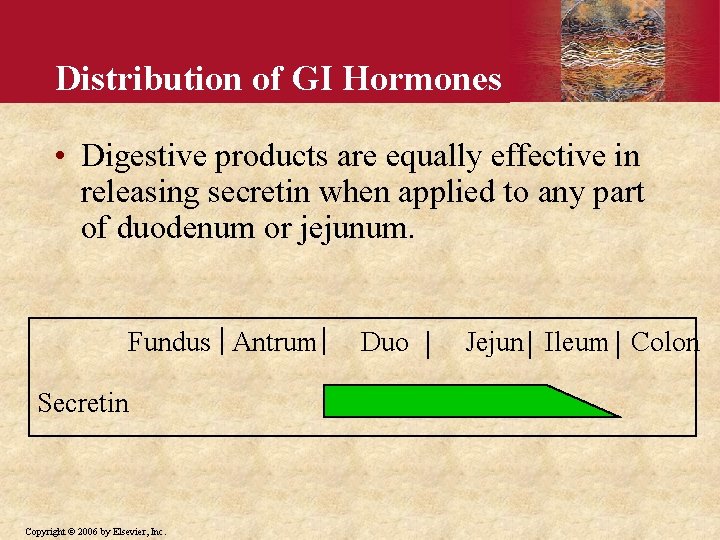
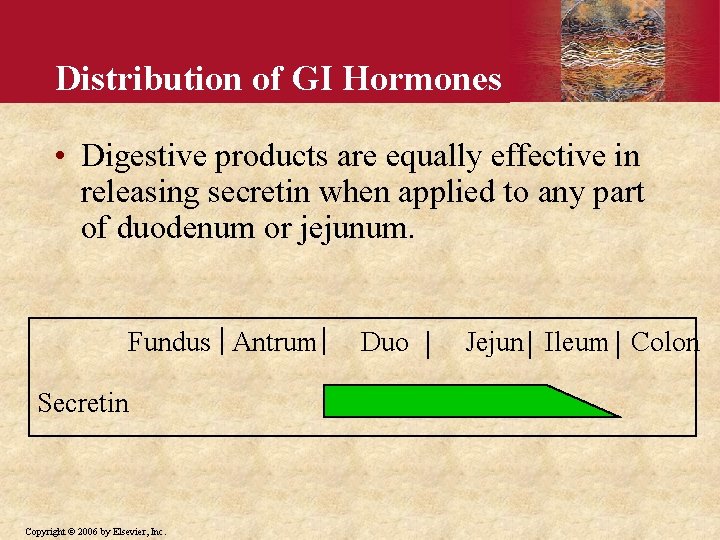
Distribution of GI Hormones • Digestive products are equally effective in releasing secretin when applied to any part of duodenum or jejunum. Fundus Antrum Secretin Copyright © 2006 by Elsevier, Inc. Duo Jejun Ileum Colon
Pancreatic Failure • Digestion is abnormal when pancreas fails to secrete normal amounts of enzymes. Pancreatitis Removal of pancreatic head - malignancy • Without pancreatic enzymes - 60% fat not absorbed (steatorrhea) 30 -40% protein and carbohydrates not absorbed Copyright © 2006 by Elsevier, Inc.
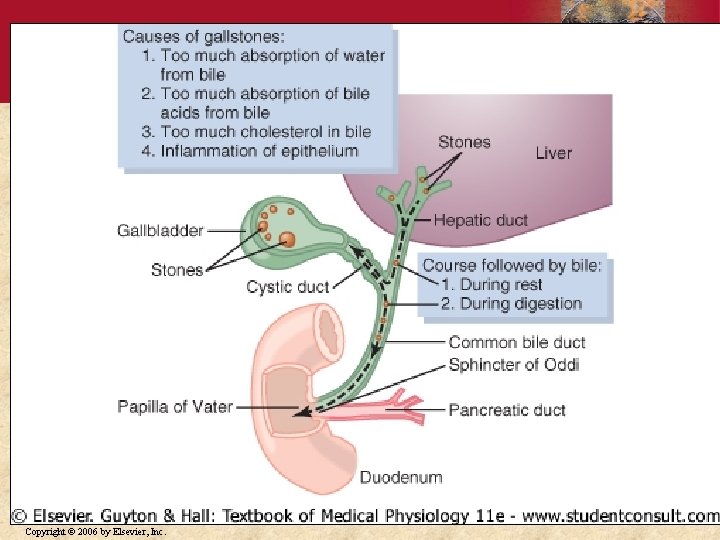
Pancreatitis • Pancreatitis means inflammation of pancreas. Autodigestion theory can explain condition. • Chronic pancreatitis - (multiple shared causes) alcohol - most common cause in adults cystic fibrosis - most common cause in children • Acute pancreatitis - (multiple shared causes) gallstones Copyright © 2006 by Elsevier, Inc. - most common cause
Secretion Failure in Cystic Fibrosis • CF patients lack chloride transporter at apical membrane. • Watery ductal secretion decreases which concentrates acinar secretions in ducts. • Precipitation of proteinaceous secretions block ducts and can destroy gland by autodigestion. Copyright © 2006 by Elsevier, Inc.
Copyright © 2006 by Elsevier, Inc.