Types and etiologies of CNS infections classified by

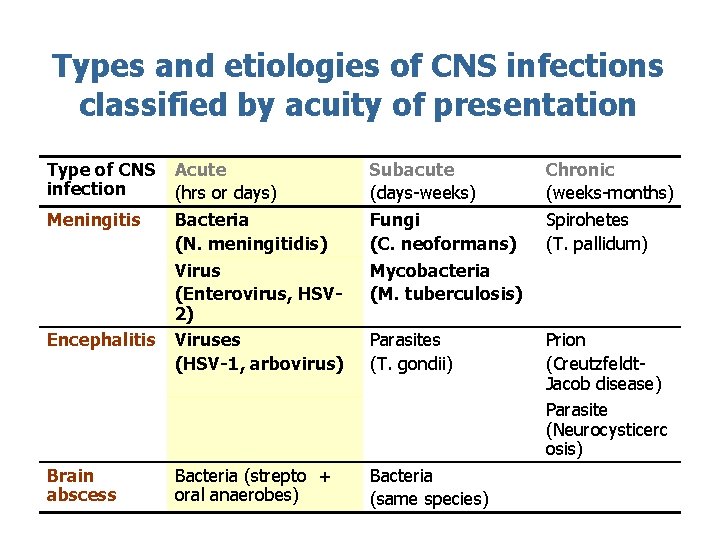
Types and etiologies of CNS infections classified by acuity of presentation Type of CNS infection Meningitis Encephalitis Brain abscess Acute (hrs or days) Bacteria (N. meningitidis) Virus (Enterovirus, HSV 2) Viruses (HSV-1, arbovirus) Subacute (days-weeks) Fungi (C. neoformans) Mycobacteria (M. tuberculosis) Chronic (weeks-months) Spirohetes (T. pallidum) Parasites (T. gondii) Prion (Creutzfeldt. Jacob disease) Parasite (Neurocysticerc osis) Bacteria (strepto + oral anaerobes) Bacteria (same species)
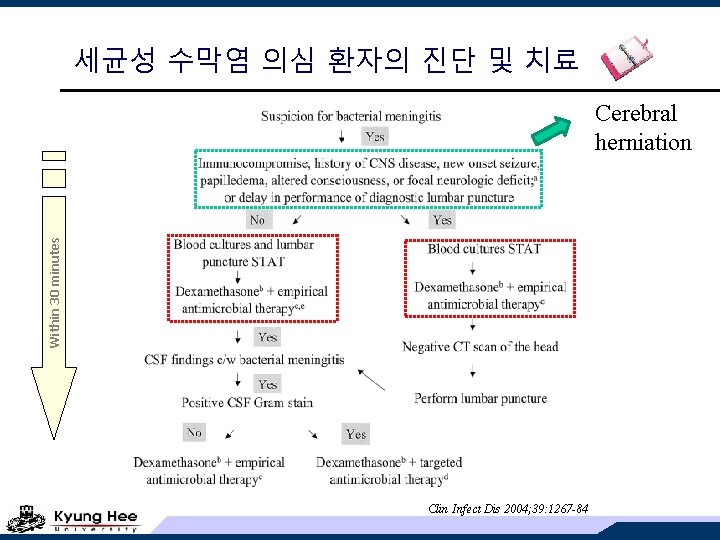
세균성 수막염 의심 환자의 진단 및 치료 Within 30 minutes Cerebral herniation Clin Infect Dis 2004; 39: 1267 -84
CSF tapping • CSF WBC 750/m. L (poly 90%) • CSF protein 550 mg/L • CSF glucose 20 mg/L
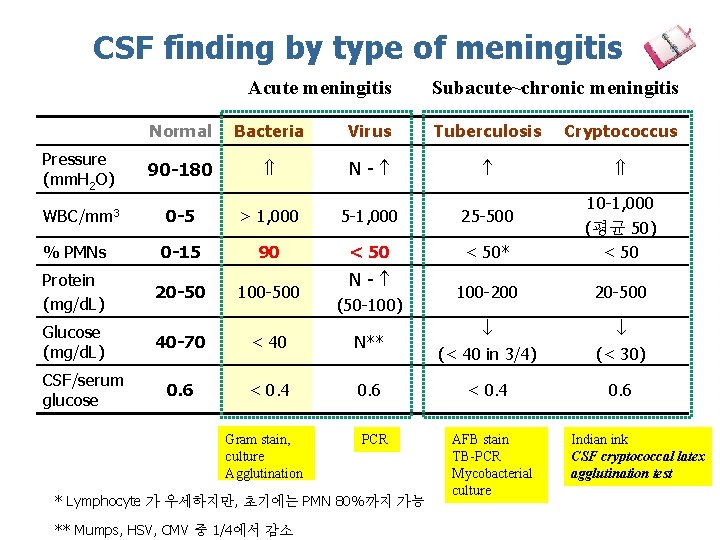
CSF finding by type of meningitis Acute meningitis Subacute~chronic meningitis Normal Bacteria Virus Tuberculosis Cryptococcus Pressure (mm. H 2 O) 90 -180 N- WBC/mm 3 0 -5 > 1, 000 5 -1, 000 25 -500 % PMNs 0 -15 90 < 50* 10 -1, 000 (평균 50) < 50 Protein (mg/d. L) 20 -50 100 -500 100 -200 20 -500 Glucose (mg/d. L) 40 -70 < 40 N** (< 40 in 3/4) (< 30) 0. 6 < 0. 4 0. 6 CSF/serum glucose Gram stain, culture Agglutination N- (50 -100) PCR * Lymphocyte 가 우세하지만, 초기에는 PMN 80%까지 가능 ** Mumps, HSV, CMV 중 1/4에서 감소 AFB stain TB-PCR Mycobacterial culture Indian ink CSF cryptococcal latex agglutination test
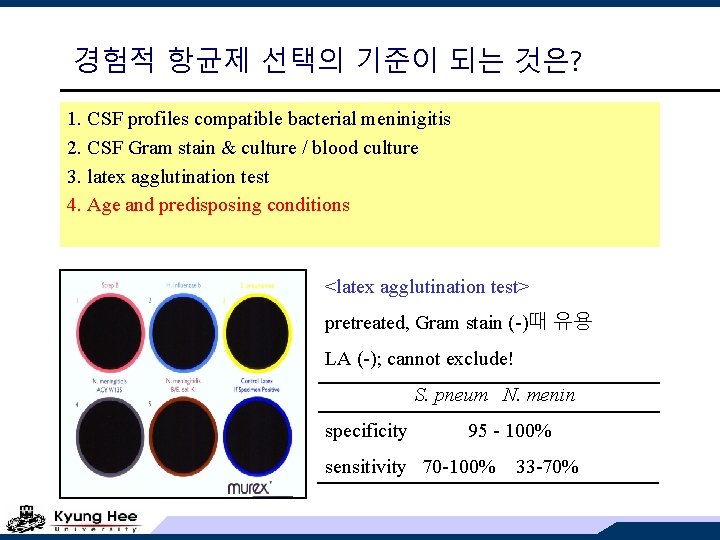
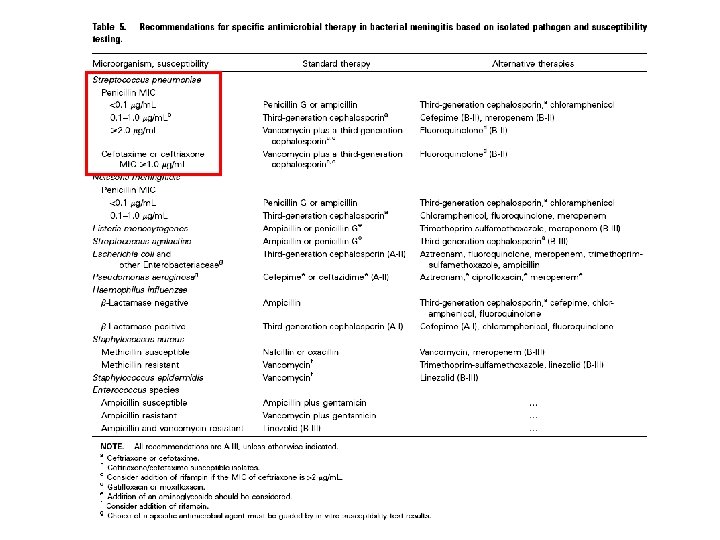
경험적 항균제 선택의 기준이 되는 것은? 1. CSF profiles compatible bacterial meninigitis 2. CSF Gram stain & culture / blood culture 3. latex agglutination test 4. Age and predisposing conditions <latex agglutination test> pretreated, Gram stain (-)때 유용 LA (-); cannot exclude! S. pneum N. menin specificity 95 - 100% sensitivity 70 -100% 33 -70%
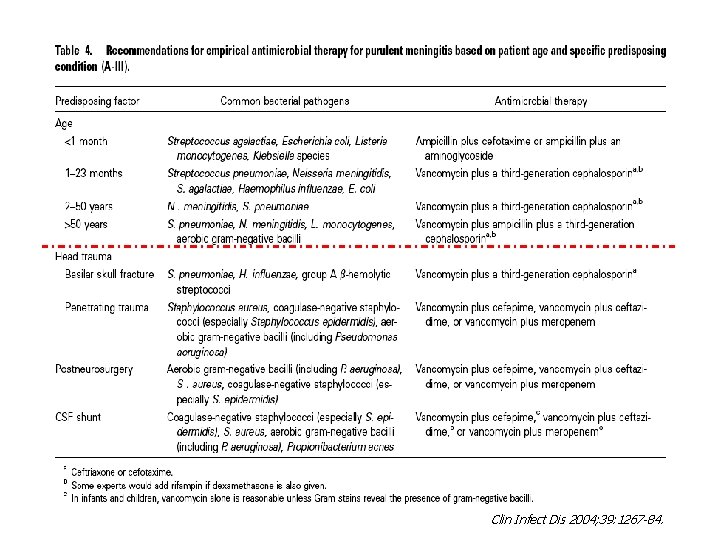
Clin Infect Dis 2004; 39: 1267 -84.
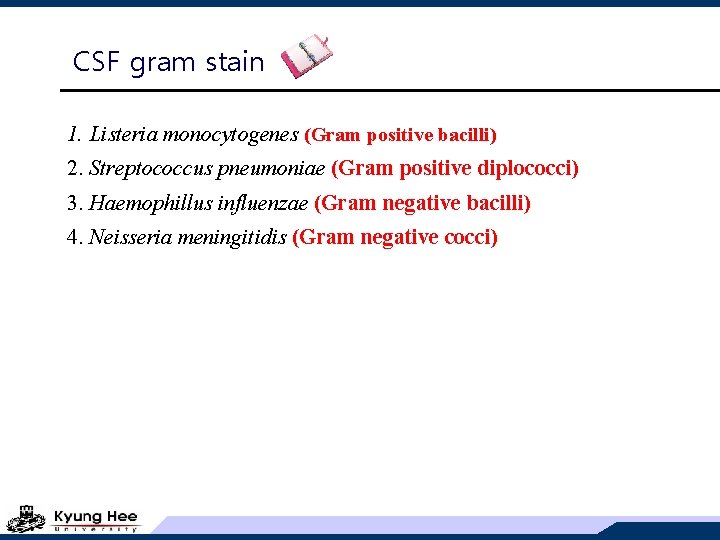
CSF gram stain 1. Listeria monocytogenes (Gram positive bacilli) 2. Streptococcus pneumoniae (Gram positive diplococci) 3. Haemophillus influenzae (Gram negative bacilli) 4. Neisseria meningitidis (Gram negative cocci)
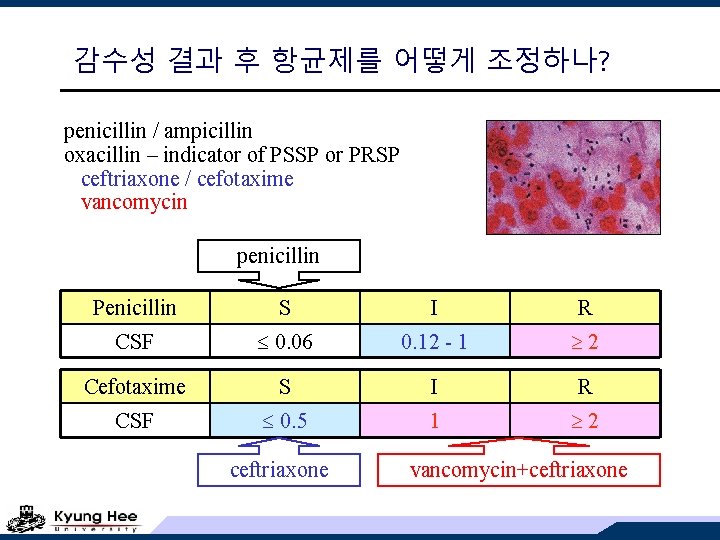
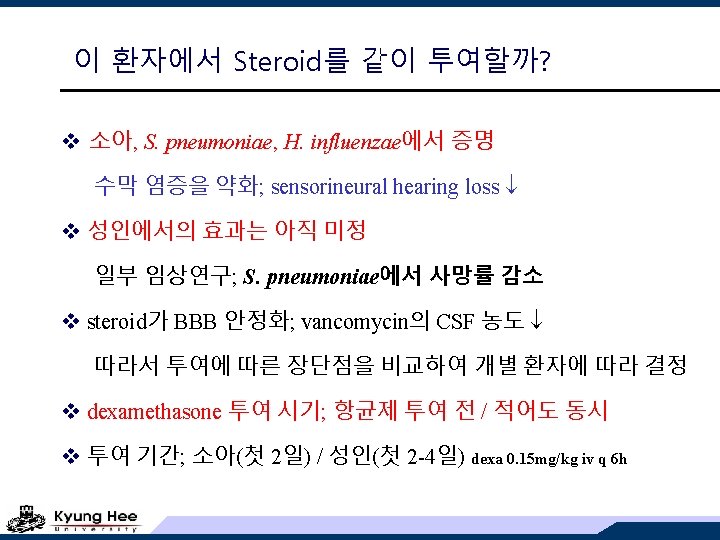
감수성 결과 후 항균제를 어떻게 조정하나? penicillin / ampicillin oxacillin – indicator of PSSP or PRSP ceftriaxone / cefotaxime vancomycin penicillin Penicillin S I R CSF 0. 06 0. 12 - 1 2 Cefotaxime S I R CSF 0. 5 1 2 ceftriaxone vancomycin+ceftriaxone
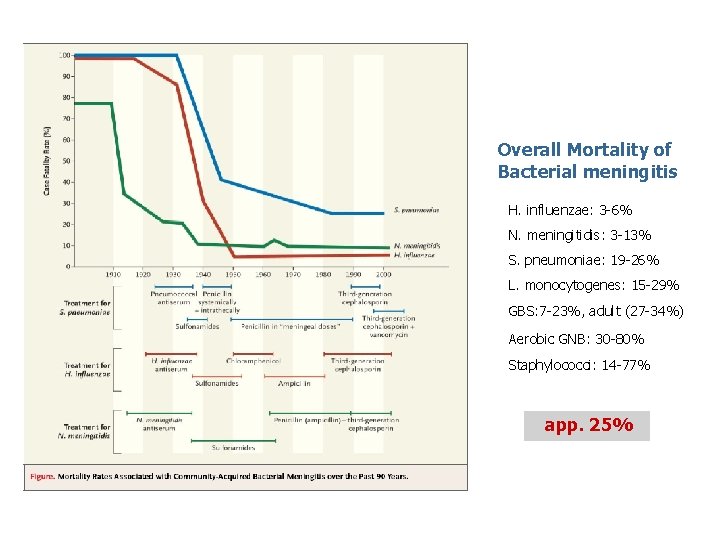
Overall Mortality of Bacterial meningitis H. influenzae: 3 -6% N. meningitidis: 3 -13% S. pneumoniae: 19 -26% L. monocytogenes: 15 -29% GBS: 7 -23%, adult (27 -34%) Aerobic GNB: 30 -80% Staphylococci: 14 -77% app. 25%

이 환자의 피부 발진 Purpura fulminans
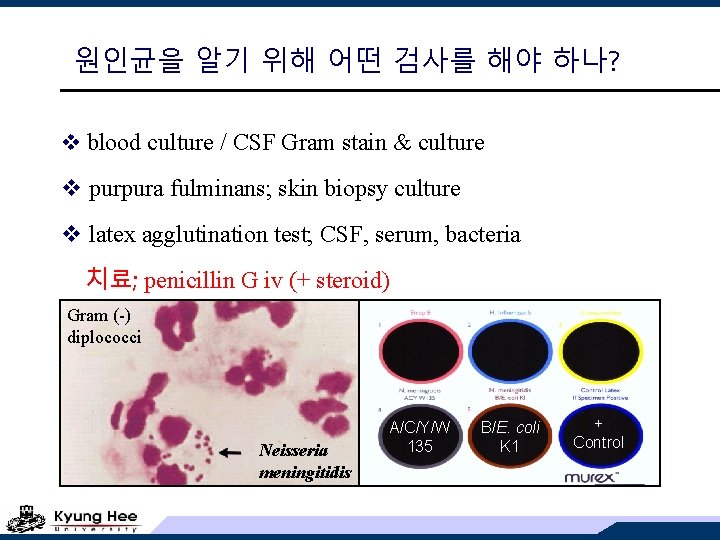
원인균을 알기 위해 어떤 검사를 해야 하나? v blood culture / CSF Gram stain & culture v purpura fulminans; skin biopsy culture v latex agglutination test; CSF, serum, bacteria 치료; penicillin G iv (+ steroid) Gram (-) diplococci Neisseria meningitidis A/C/Y/W 135 B/E. coli K 1 + Control
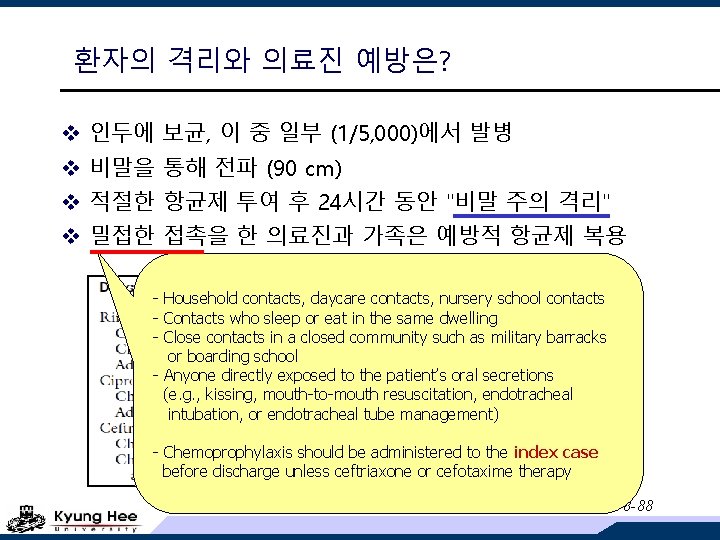
환자의 격리와 의료진 예방은? v 인두에 보균, 이 중 일부 (1/5, 000)에서 발병 v 비말을 통해 전파 (90 cm) v 적절한 항균제 투여 후 24시간 동안 "비말 주의 격리" v 밀접한 접촉을 한 의료진과 가족은 예방적 항균제 복용 - Household contacts, daycare contacts, nursery school contacts - Contacts who sleep or eat in the same dwelling - Close contacts in a closed community such as military barracks or boarding school - Anyone directly exposed to the patient’s oral secretions (e. g. , kissing, mouth-to-mouth resuscitation, endotracheal intubation, or endotracheal tube management) - Chemoprophylaxis should be administered to the index case before discharge unless ceftriaxone or cefotaxime therapy NEJM 2001; 344: 1378 -88
Neisseria meningitidis v 13 serogroups; A/B/C/Y/W 135 - nearly all diseases v A (C); third-world countries v B & C; industrialized (90% in US) v endemic rates are low but epidemics ! v meningitis, septicemia, septic shock with MOF v mortality is still > 10% (septicemia 40%) No other infection so quickly kills ! 사망자 1/2은 첫 증상 후 24시간 내 사망 사망자 1/3은 입원 후 6시간 내 사망 생존자의 11~19%는 후유증이 남음
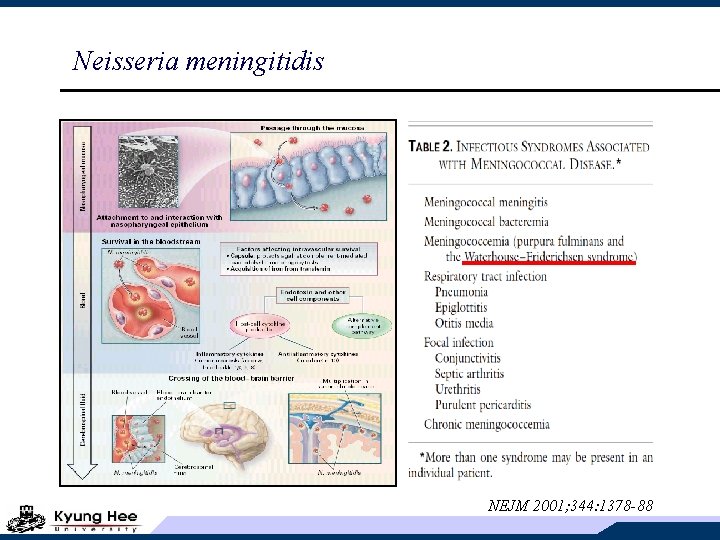
Neisseria meningitidis NEJM 2001; 344: 1378 -88
우리나라의 신고 현황 법정전염병 신고율 27% K J Epidemiol 1996 91 92 93 94 95 96 97 98 99 2000 CDMR, KCDC
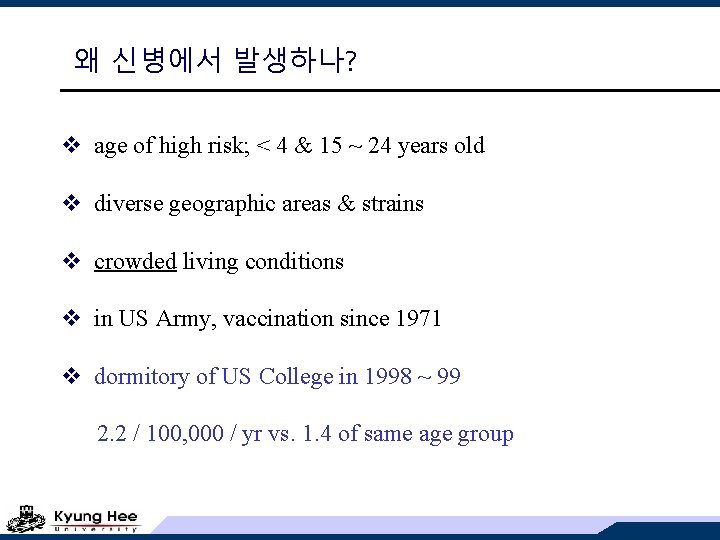
왜 신병에서 발생하나? v age of high risk; < 4 & 15 ~ 24 years old v diverse geographic areas & strains v crowded living conditions v in US Army, vaccination since 1971 v dormitory of US College in 1998 ~ 99 2. 2 / 100, 000 / yr vs. 1. 4 of same age group
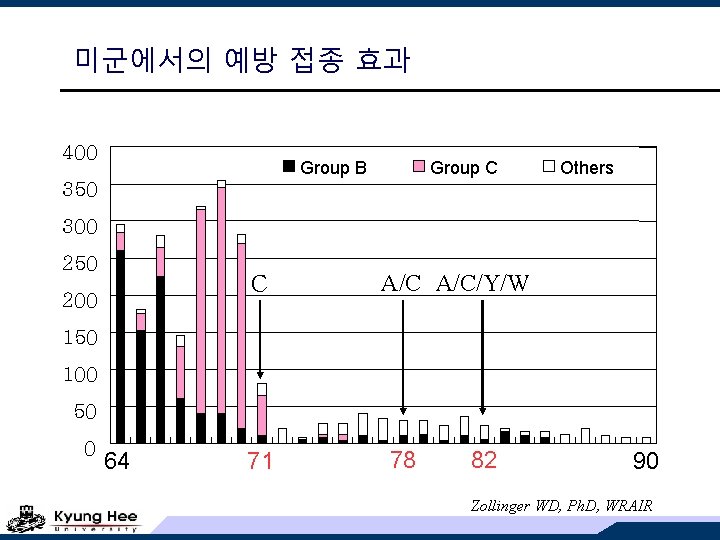
미군에서의 예방 접종 효과 400 Group B Group C Others 350 300 250 C 200 A/C/Y/W 150 100 50 0 64 71 78 82 90 Zollinger WD, Ph. D, WRAIR
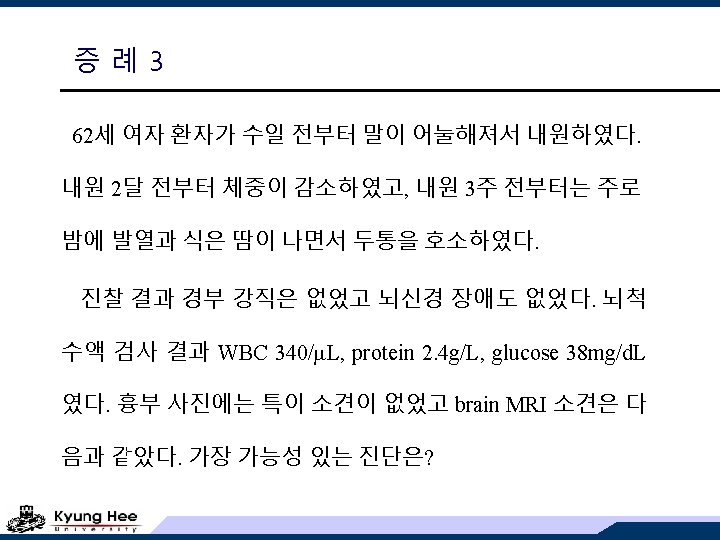
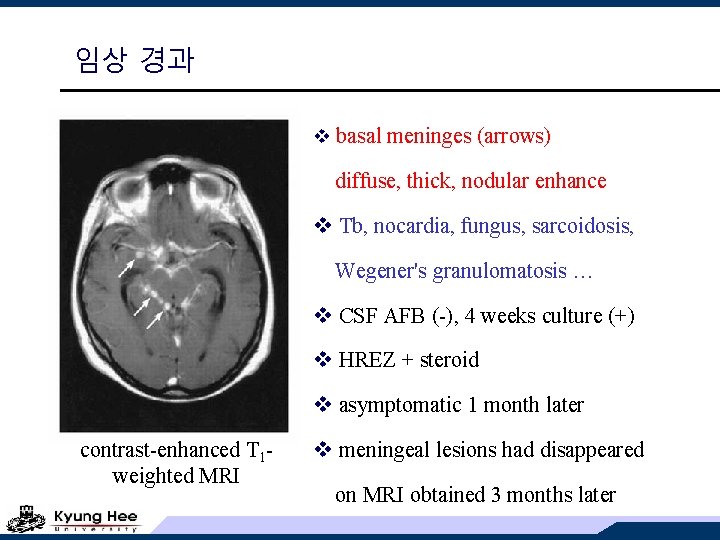
임상 경과 v basal meninges (arrows) diffuse, thick, nodular enhance v Tb, nocardia, fungus, sarcoidosis, Wegener's granulomatosis … v CSF AFB (-), 4 weeks culture (+) v HREZ + steroid v asymptomatic 1 month later contrast-enhanced T 1 weighted MRI v meningeal lesions had disappeared on MRI obtained 3 months later
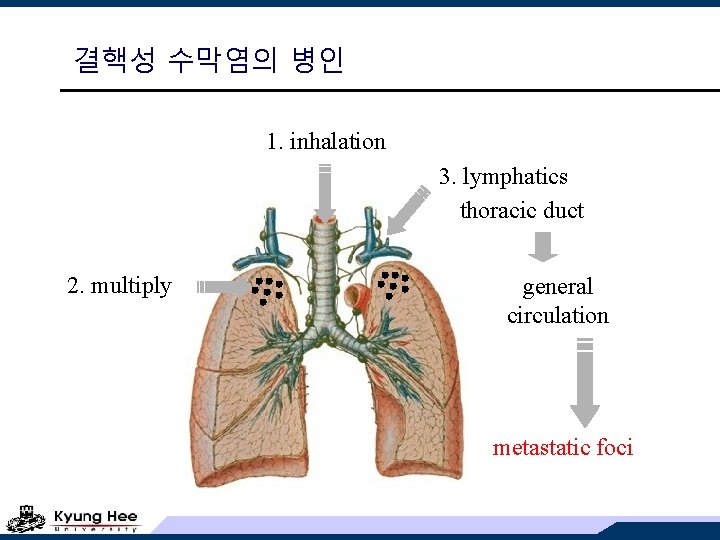
결핵성 수막염의 병인 1. inhalation 3. lymphatics thoracic duct 2. multiply general circulation metastatic foci
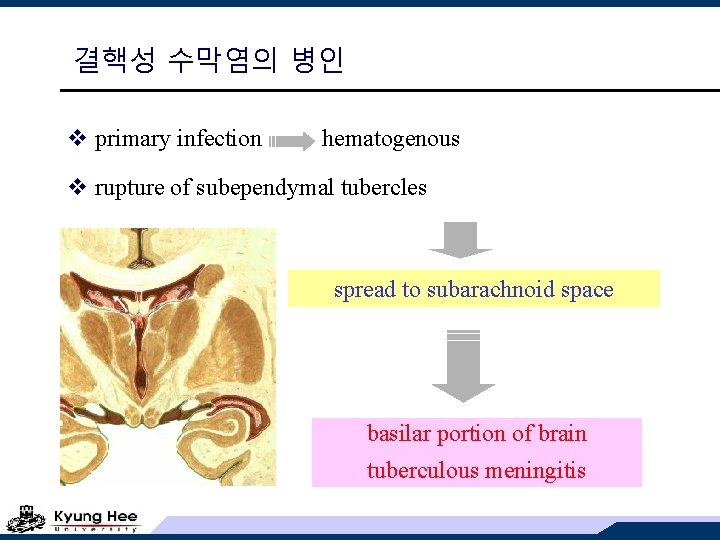
결핵성 수막염의 병인 v primary infection hematogenous v rupture of subependymal tubercles spread to subarachnoid space basilar portion of brain tuberculous meningitis
결핵성 수막염의 임상적 발현 v subacute to chronic (at least 4 weeks) v fever, headache, night sweat, weight loss, malaise, lethargy … v infarct, SOL, hydrocephalus headache, vomiting, confusion, seizure v cranial nerve involvement IV (trochlear) > II, III, VIII
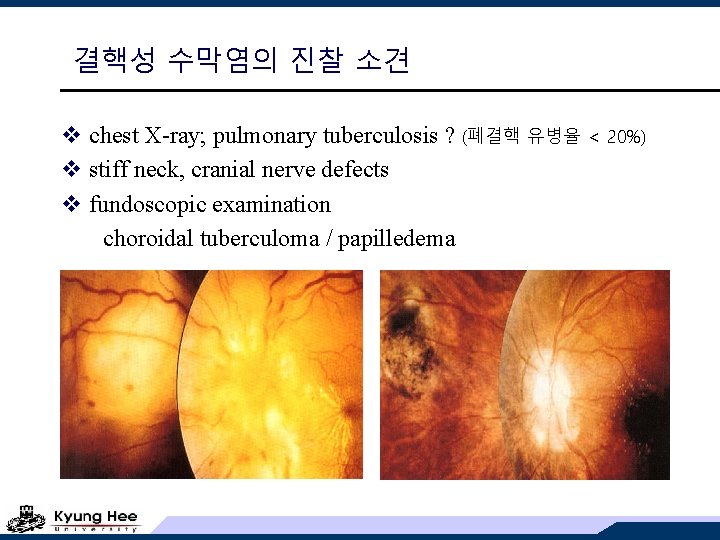
결핵성 수막염의 진찰 소견 v chest X-ray; pulmonary tuberculosis ? (폐결핵 유병율 < 20%) v stiff neck, cranial nerve defects v fundoscopic examination choroidal tuberculoma / papilledema
결핵성 수막염의 진단 v 확진이 매우 어렵다 - 의심해야 진단할 수 있다. v CSF 소견 fungal, partially treated bacterial meningitis와 비슷 gross; clear or slightly opaque overnight stand; small wisp-like pellicle WBC; 100 -500/ L (PMN to MN) protein; elevated glucose; < 45 -50 mg/dl (< 1/2 serum level) v CSF AFB smear (10 -22%) / culture (50 -80%) v PCR sensitivity (27 -85%) / specificity (95 -100%)
결핵성 수막염의 치료 v prompt chemotherapy is important ! v INH / RFP / EMB / PZA v 12 months; meningitis, miliary, bone/joint v Cb tuberculomas; enlarge during chemo. Tx. v Steroid adjunctive therapy large, well-designed studies; not available ! Pd 60 mg/d for 1 -2 wks, then taper over 4 -6 wks stage 2; confusion or focal neurologic signs stage 3; stuporous or para- / hemiplegia consider CSF protein > 1, 000 mg/d. L (d/t spinal block)
- Slides: 35