Type A Type B 80 1520 Overdose toxicity
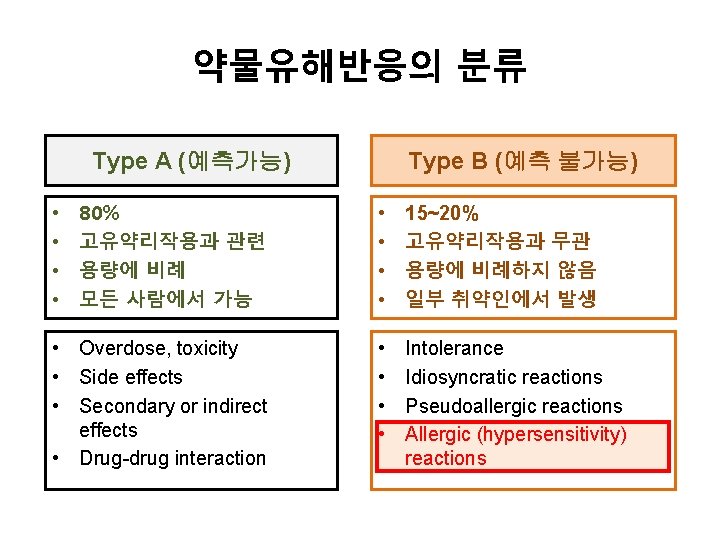
약물유해반응의 분류 Type A (예측가능) Type B (예측 불가능) 80% 고유약리작용과 관련 용량에 비례 모든 사람에서 가능 • • 15~20% 고유약리작용과 무관 용량에 비례하지 않음 일부 취약인에서 발생 • Overdose, toxicity • Side effects • Secondary or indirect effects • Drug-drug interaction • • Intolerance Idiosyncratic reactions Pseudoallergic reactions Allergic (hypersensitivity) reactions • •

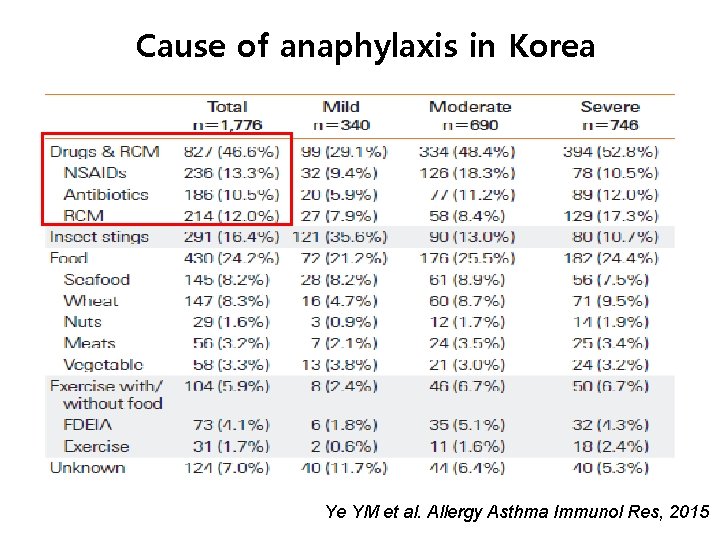
Cause of anaphylaxis in Korea Ye YM et al. Allergy Asthma Immunol Res, 2015
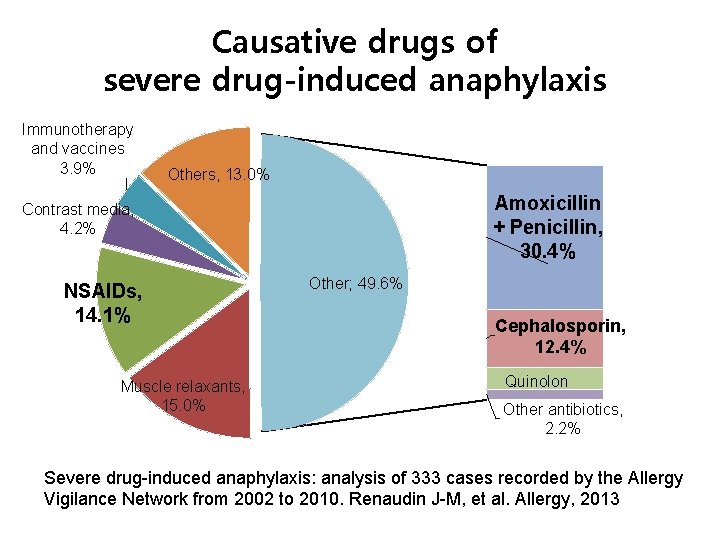
Causative drugs of severe drug-induced anaphylaxis Immunotherapy and vaccines 3. 9% Others, 13. 0% Amoxicillin + Penicillin, 30. 4% Contrast media, 4. 2% NSAIDs, 14. 1% Muscle relaxants, 15. 0% Other; 49. 6% Cephalosporin, 12. 4% Quinolone, , 4, 6% Other antibiotics, 2. 2% Severe drug-induced anaphylaxis: analysis of 333 cases recorded by the Allergy Vigilance Network from 2002 to 2010. Renaudin J-M, et al. Allergy, 2013
Beta-lactam antibiotics Allergy
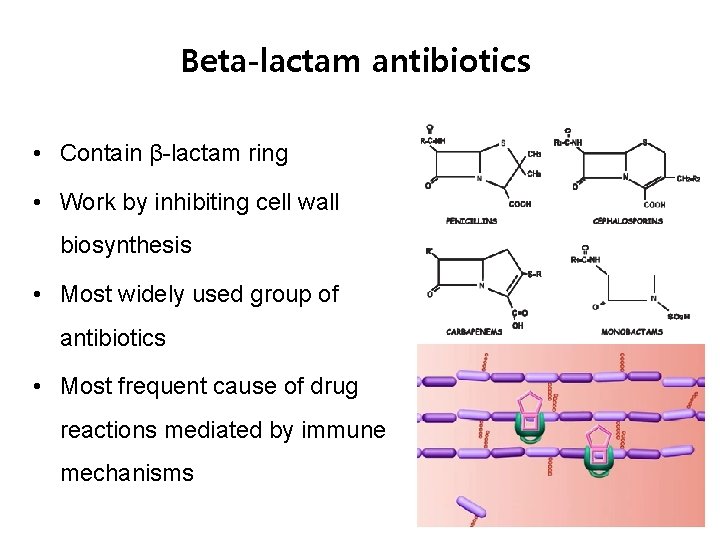
Beta-lactam antibiotics • Contain β-lactam ring • Work by inhibiting cell wall biosynthesis • Most widely used group of antibiotics • Most frequent cause of drug reactions mediated by immune mechanisms
Allergy to penicillin “claimed” vs. “real” • Reaction by underlying illness • Predictable other type of adverse reaction rather than allergic • Allergenicity lost over time • Lack of understanding drug allergy • Alternate broad-spectrum antibiotics – cost – multidrug-resistant bacteria
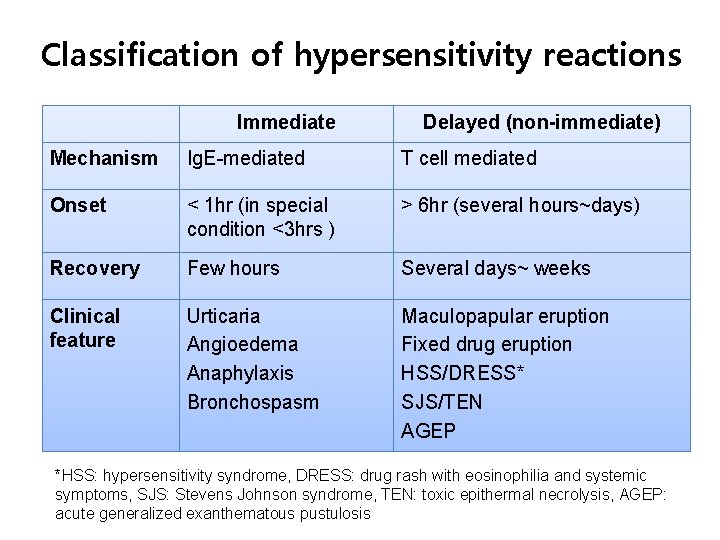
Classification of hypersensitivity reactions Immediate Delayed (non-immediate) Mechanism Ig. E-mediated T cell mediated Onset < 1 hr (in special condition <3 hrs ) > 6 hr (several hours~days) Recovery Few hours Several days~ weeks Clinical feature Urticaria Angioedema Anaphylaxis Bronchospasm Maculopapular eruption Fixed drug eruption HSS/DRESS* SJS/TEN AGEP *HSS: hypersensitivity syndrome, DRESS: drug rash with eosinophilia and systemic symptoms, SJS: Stevens Johnson syndrome, TEN: toxic epithermal necrolysis, AGEP: acute generalized exanthematous pustulosis
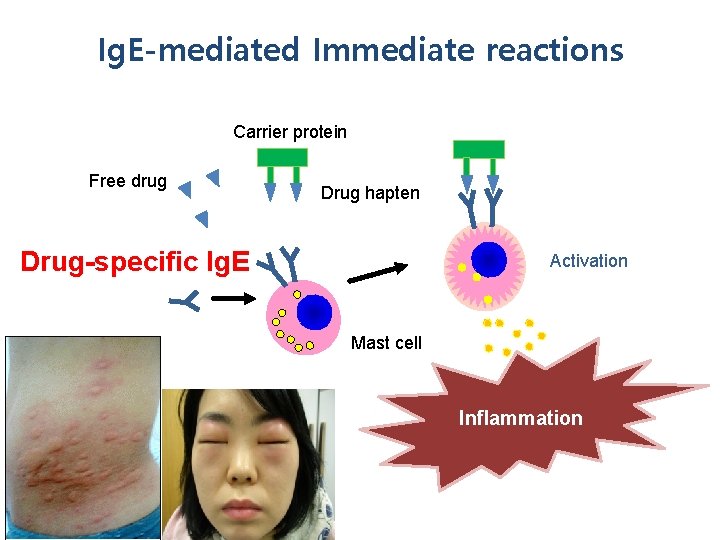
Ig. E-mediated Immediate reactions Carrier protein Free drug Drug hapten Drug-specific Ig. E Activation Mast cell Inflammatory mediators and cytokines Inflammation

T cell-mediated delayed eruptions
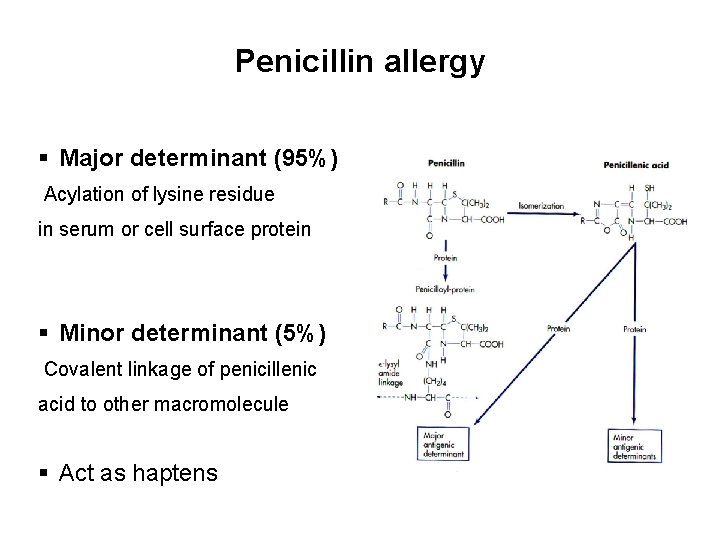
Penicillin allergy § Major determinant (95%) Acylation of lysine residue in serum or cell surface protein § Minor determinant (5%) Covalent linkage of penicillenic acid to other macromolecule § Act as haptens
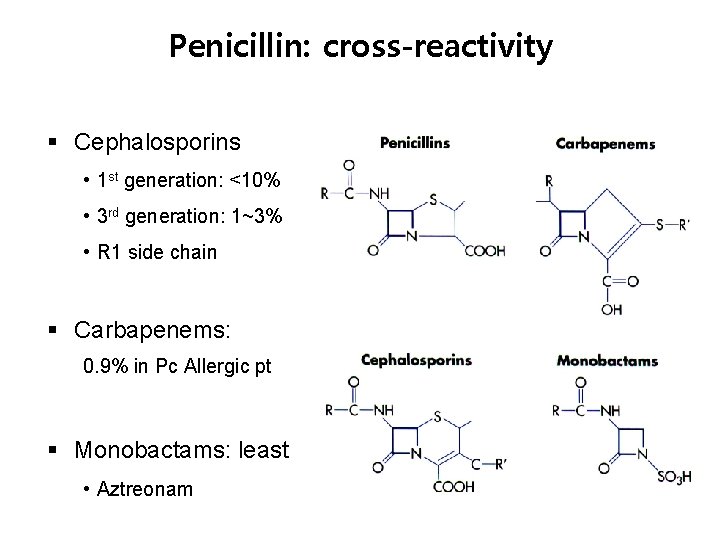
Penicillin: cross-reactivity § Cephalosporins • 1 st generation: <10% • 3 rd generation: 1~3% • R 1 side chain § Carbapenems: 0. 9% in Pc Allergic pt § Monobactams: least • Aztreonam
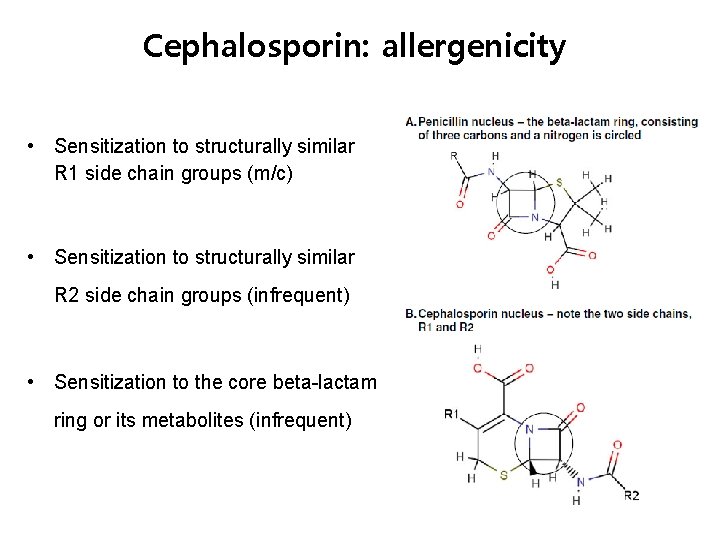
Cephalosporin: allergenicity • Sensitization to structurally similar R 1 side chain groups (m/c) • Sensitization to structurally similar R 2 side chain groups (infrequent) • Sensitization to the core beta-lactam ring or its metabolites (infrequent)
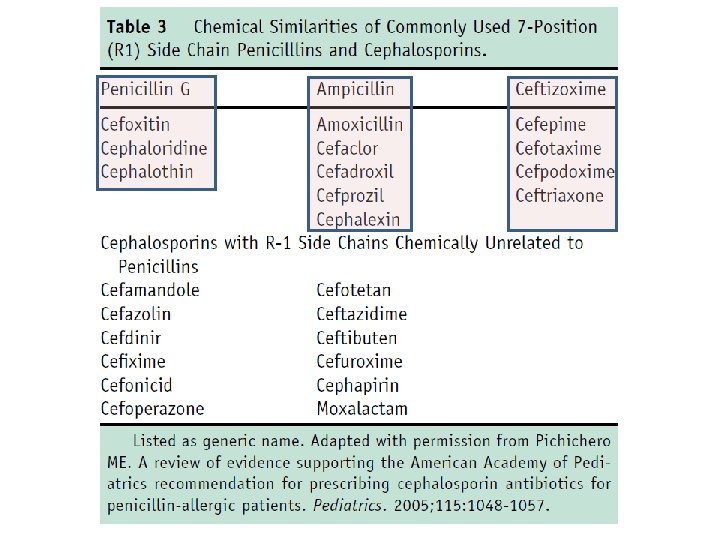
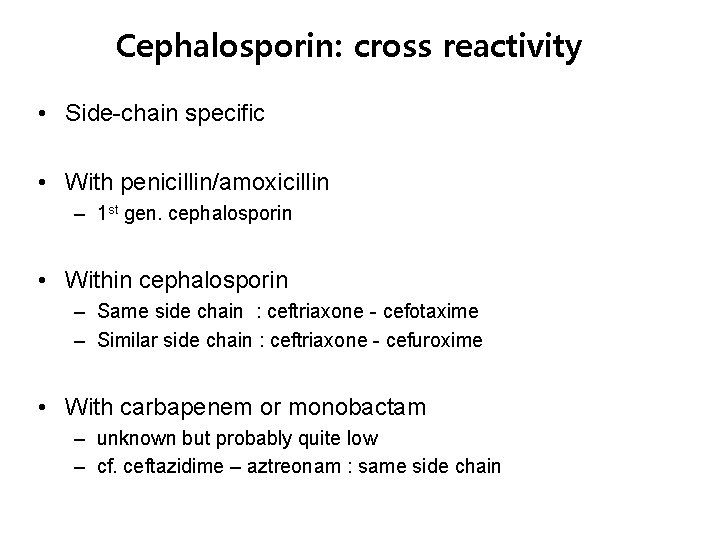
Cephalosporin: cross reactivity • Side-chain specific • With penicillin/amoxicillin – 1 st gen. cephalosporin • Within cephalosporin – Same side chain : ceftriaxone - cefotaxime – Similar side chain : ceftriaxone - cefuroxime • With carbapenem or monobactam – unknown but probably quite low – cf. ceftazidime – aztreonam : same side chain
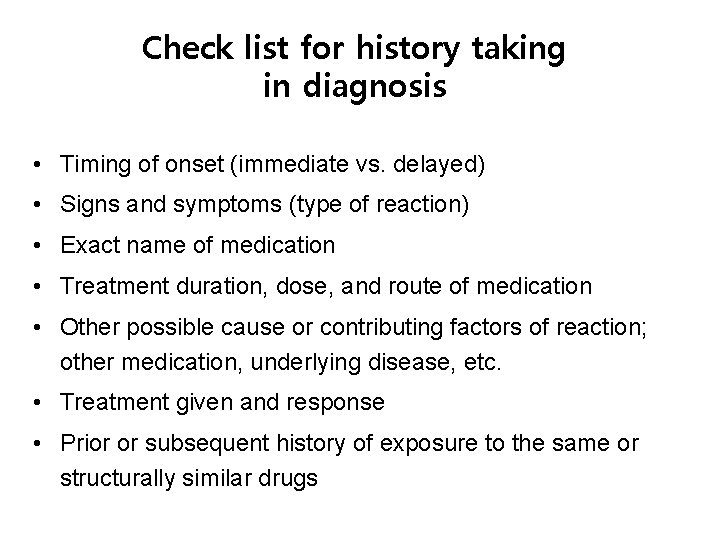
Check list for history taking in diagnosis • Timing of onset (immediate vs. delayed) • Signs and symptoms (type of reaction) • Exact name of medication • Treatment duration, dose, and route of medication • Other possible cause or contributing factors of reaction; other medication, underlying disease, etc. • Treatment given and response • Prior or subsequent history of exposure to the same or structurally similar drugs
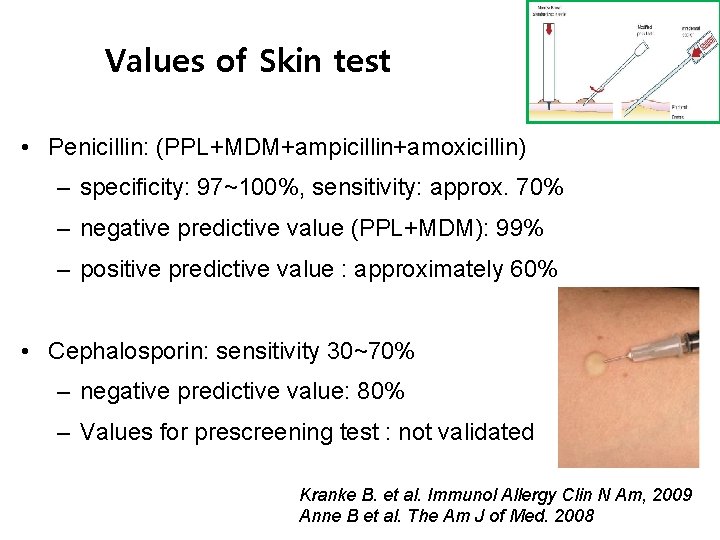
Values of Skin test • Penicillin: (PPL+MDM+ampicillin+amoxicillin) – specificity: 97~100%, sensitivity: approx. 70% – negative predictive value (PPL+MDM): 99% – positive predictive value : approximately 60% • Cephalosporin: sensitivity 30~70% – negative predictive value: 80% – Values for prescreening test : not validated Kranke B. et al. Immunol Allergy Clin N Am, 2009 Anne B et al. The Am J of Med. 2008
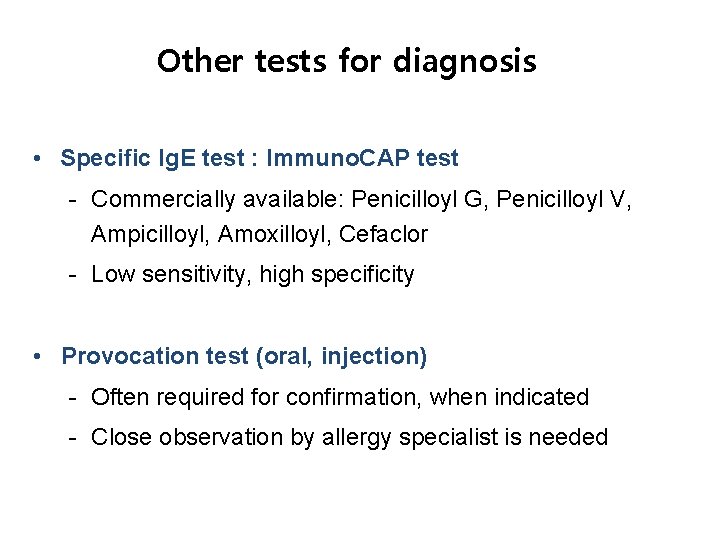
Other tests for diagnosis • Specific Ig. E test : Immuno. CAP test - Commercially available: Penicilloyl G, Penicilloyl V, Ampicilloyl, Amoxilloyl, Cefaclor - Low sensitivity, high specificity • Provocation test (oral, injection) - Often required for confirmation, when indicated - Close observation by allergy specialist is needed
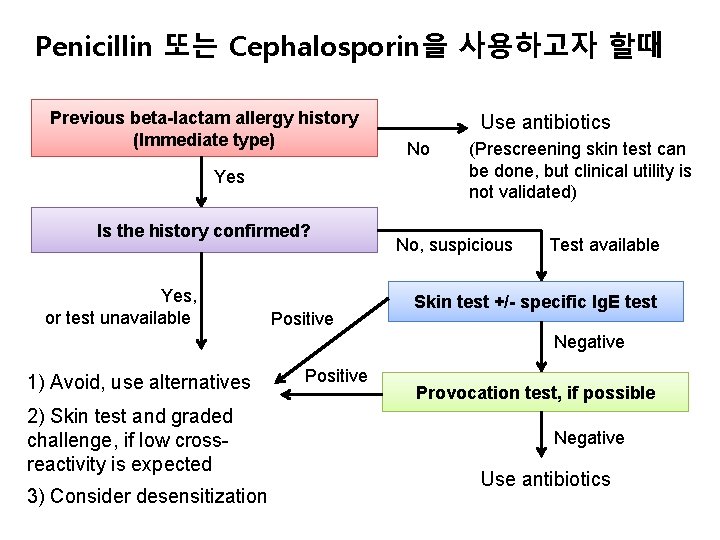
Penicillin 또는 Cephalosporin을 사용하고자 할때 Previous beta-lactam allergy history (Immediate type) Yes Is the history confirmed? Yes, or test unavailable Positive Use antibiotics No (Prescreening skin test can be done, but clinical utility is not validated) No, suspicious Test available Skin test +/- specific Ig. E test Negative 1) Avoid, use alternatives 2) Skin test and graded challenge, if low crossreactivity is expected 3) Consider desensitization Positive Provocation test, if possible Negative Use antibiotics
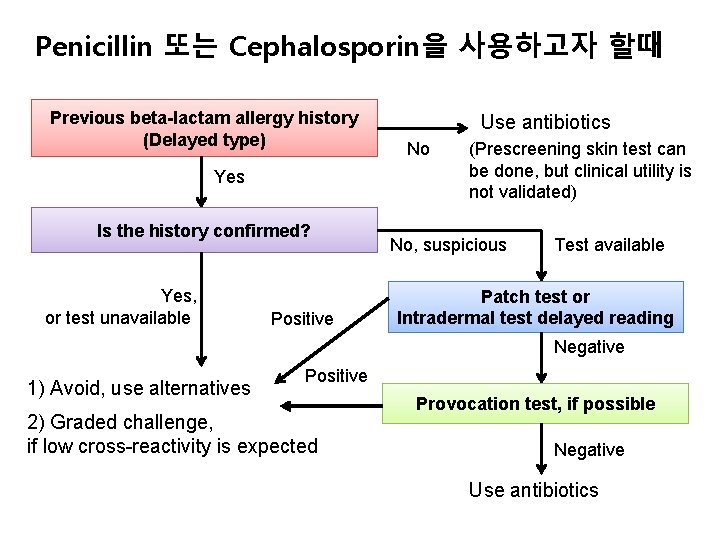
Penicillin 또는 Cephalosporin을 사용하고자 할때 Previous beta-lactam allergy history (Delayed type) Yes Is the history confirmed? Yes, or test unavailable Positive Use antibiotics No (Prescreening skin test can be done, but clinical utility is not validated) No, suspicious Test available Patch test or Intradermal test delayed reading Negative 1) Avoid, use alternatives Positive 2) Graded challenge, if low cross-reactivity is expected Provocation test, if possible Negative Use antibiotics
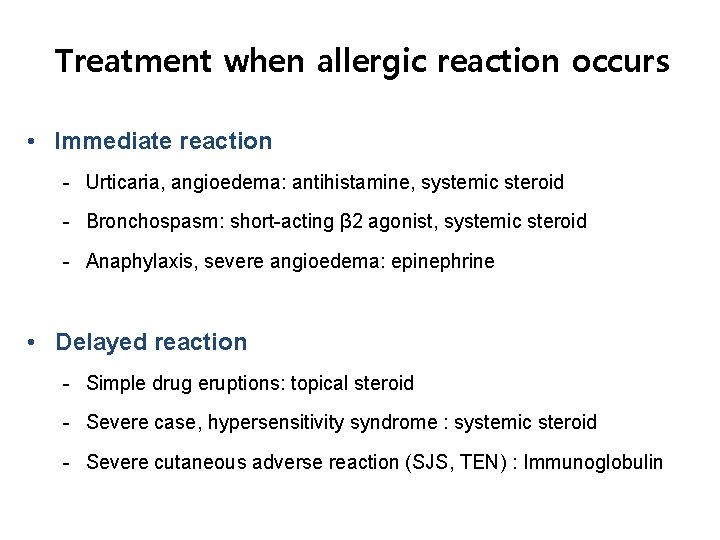
Treatment when allergic reaction occurs • Immediate reaction - Urticaria, angioedema: antihistamine, systemic steroid - Bronchospasm: short-acting β 2 agonist, systemic steroid - Anaphylaxis, severe angioedema: epinephrine • Delayed reaction - Simple drug eruptions: topical steroid - Severe case, hypersensitivity syndrome : systemic steroid - Severe cutaneous adverse reaction (SJS, TEN) : Immunoglobulin
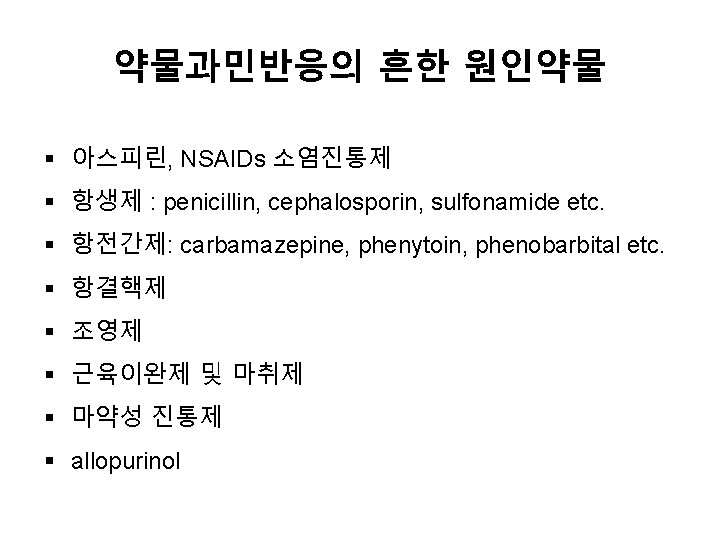
NSAIDs Hypersensitivity
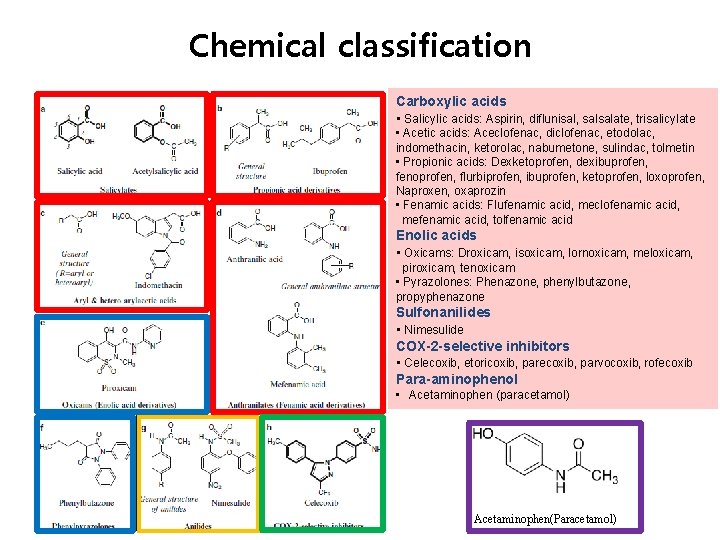
Chemical classification Carboxylic acids • Salicylic acids: Aspirin, diflunisal, salsalate, trisalicylate • Acetic acids: Aceclofenac, diclofenac, etodolac, indomethacin, ketorolac, nabumetone, sulindac, tolmetin • Propionic acids: Dexketoprofen, dexibuprofen, fenoprofen, flurbiprofen, ibuprofen, ketoprofen, loxoprofen, Naproxen, oxaprozin • Fenamic acids: Flufenamic acid, meclofenamic acid, mefenamic acid, tolfenamic acid Enolic acids • Oxicams: Droxicam, isoxicam, lornoxicam, meloxicam, piroxicam, tenoxicam • Pyrazolones: Phenazone, phenylbutazone, propyphenazone Sulfonanilides • Nimesulide COX-2 -selective inhibitors • Celecoxib, etoricoxib, parecoxib, parvocoxib, rofecoxib Para-aminophenol • Acetaminophen (paracetamol) Acetaminophen(Paracetamol)
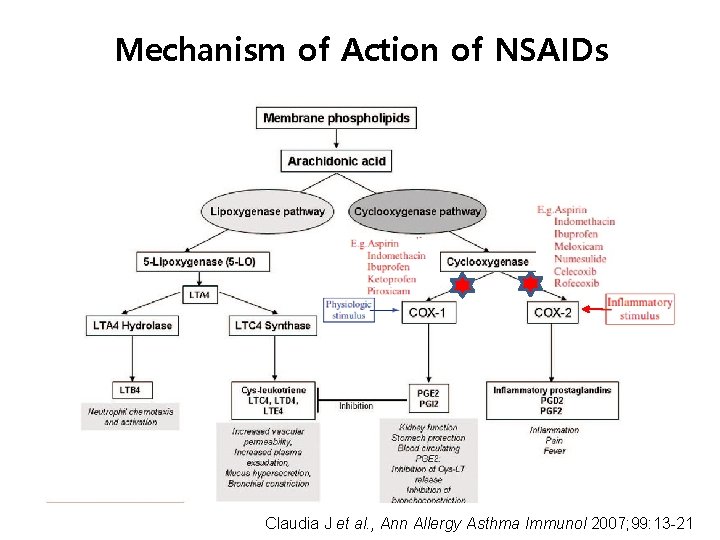
Mechanism of Action of NSAIDs Claudia J et al. , Ann Allergy Asthma Immunol 2007; 99: 13 -21
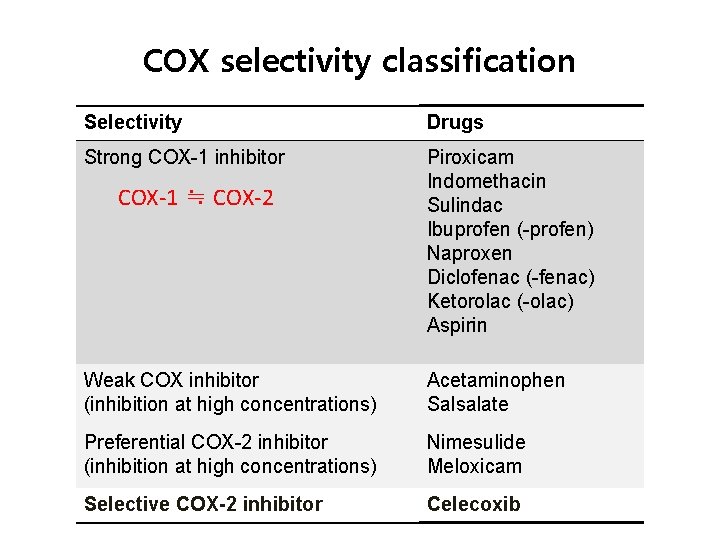
COX selectivity classification Selectivity Drugs Strong COX-1 inhibitor Piroxicam Indomethacin Sulindac Ibuprofen (-profen) Naproxen Diclofenac (-fenac) Ketorolac (-olac) Aspirin COX-1 ≒ COX-2 Weak COX inhibitor (inhibition at high concentrations) Acetaminophen Salsalate Preferential COX-2 inhibitor (inhibition at high concentrations) Nimesulide Meloxicam Selective COX-2 inhibitor Celecoxib
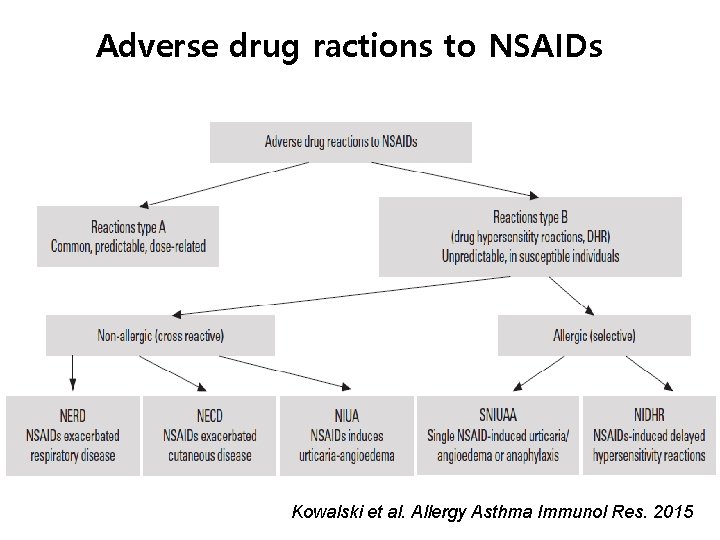
Adverse drug ractions to NSAIDs Kowalski et al. Allergy Asthma Immunol Res. 2015
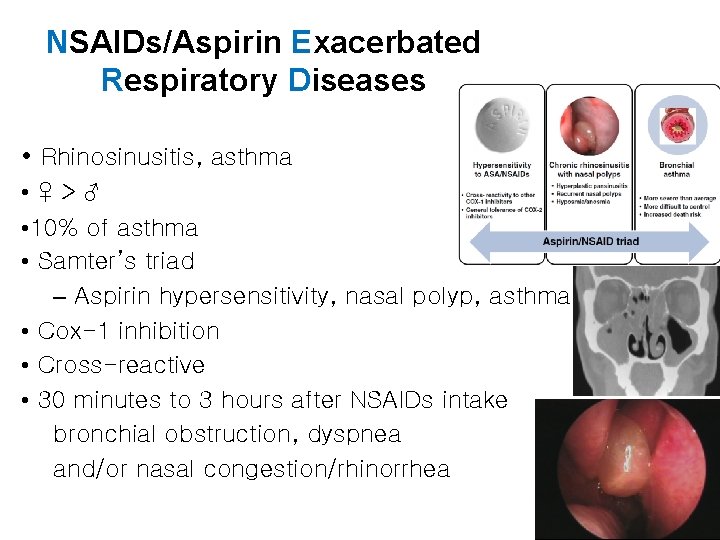
NSAIDs/Aspirin Exacerbated Respiratory Diseases • Rhinosinusitis, asthma • ♀>♂ • 10% of asthma • Samter’s triad – Aspirin hypersensitivity, nasal polyp, asthma • Cox-1 inhibition • Cross-reactive • 30 minutes to 3 hours after NSAIDs intake bronchial obstruction, dyspnea and/or nasal congestion/rhinorrhea
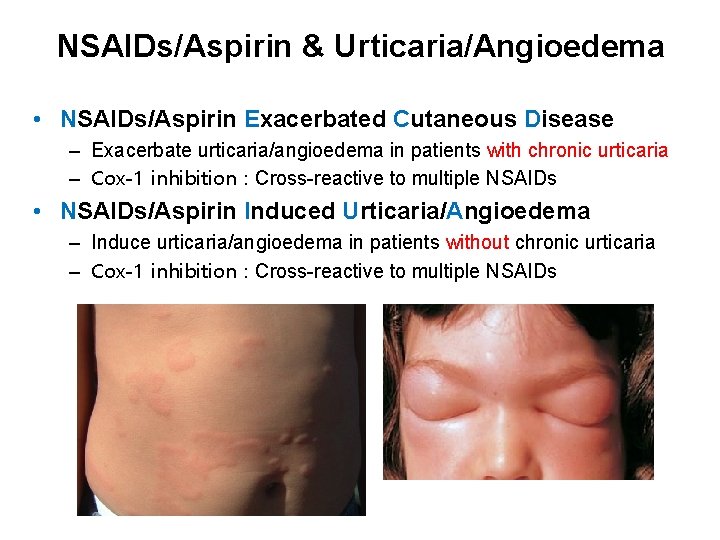
NSAIDs/Aspirin & Urticaria/Angioedema • NSAIDs/Aspirin Exacerbated Cutaneous Disease – Exacerbate urticaria/angioedema in patients with chronic urticaria – Cox-1 inhibition : Cross-reactive to multiple NSAIDs • NSAIDs/Aspirin Induced Urticaria/Angioedema – Induce urticaria/angioedema in patients without chronic urticaria – Cox-1 inhibition : Cross-reactive to multiple NSAIDs
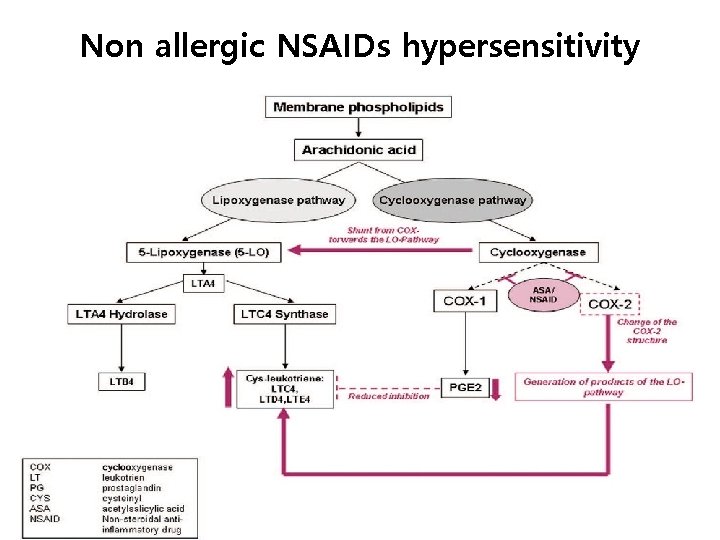
Non allergic NSAIDs hypersensitivity
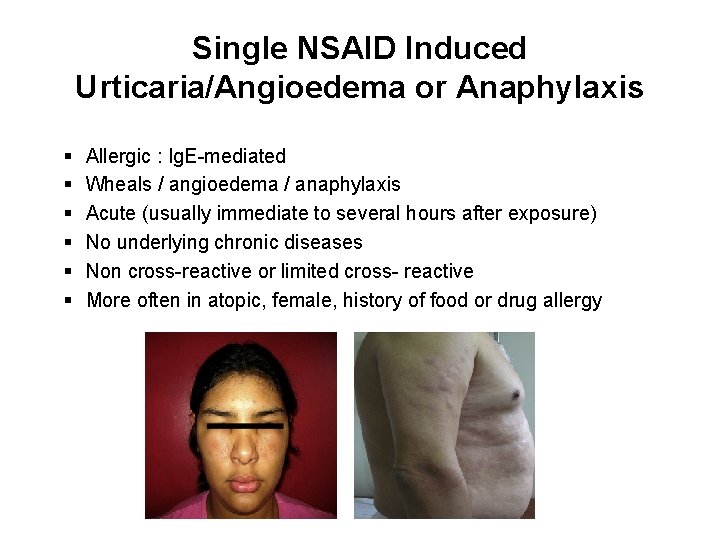
Single NSAID Induced Urticaria/Angioedema or Anaphylaxis § § § Allergic : Ig. E-mediated Wheals / angioedema / anaphylaxis Acute (usually immediate to several hours after exposure) No underlying chronic diseases Non cross-reactive or limited cross- reactive More often in atopic, female, history of food or drug allergy
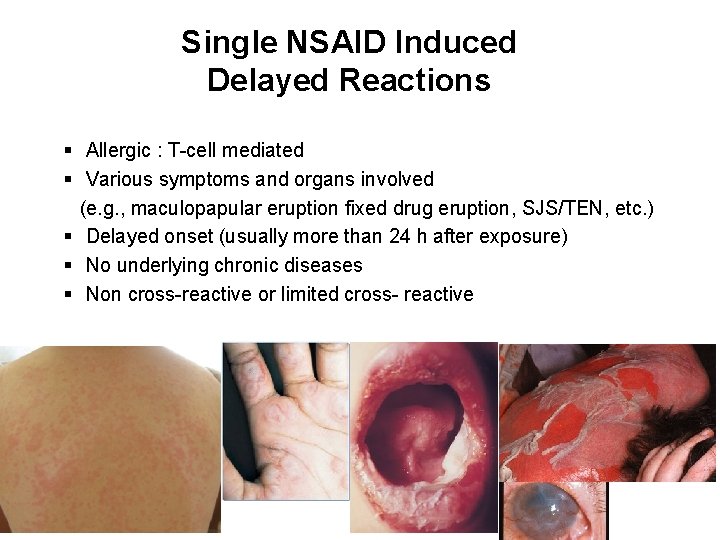
Single NSAID Induced Delayed Reactions § Allergic : T-cell mediated § Various symptoms and organs involved (e. g. , maculopapular eruption fixed drug eruption, SJS/TEN, etc. ) § Delayed onset (usually more than 24 h after exposure) § No underlying chronic diseases § Non cross-reactive or limited cross- reactive
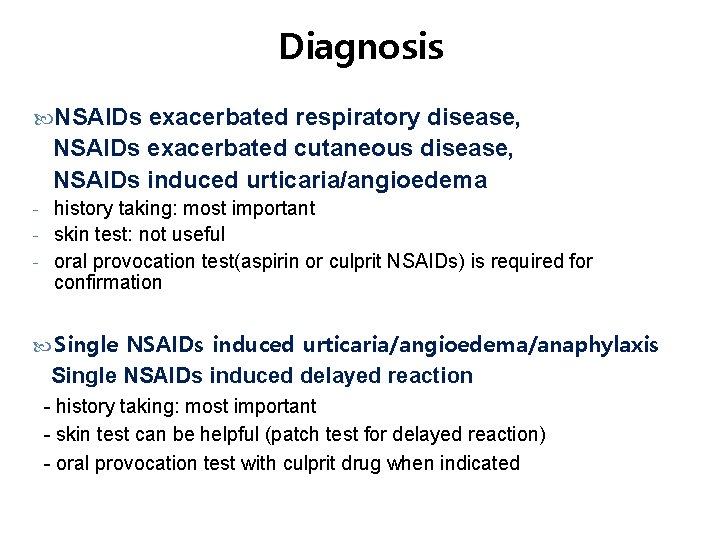
Diagnosis NSAIDs exacerbated respiratory disease, NSAIDs exacerbated cutaneous disease, NSAIDs induced urticaria/angioedema - history taking: most important - skin test: not useful - oral provocation test(aspirin or culprit NSAIDs) is required for confirmation Single NSAIDs induced urticaria/angioedema/anaphylaxis Single NSAIDs induced delayed reaction - history taking: most important - skin test can be helpful (patch test for delayed reaction) - oral provocation test with culprit drug when indicated
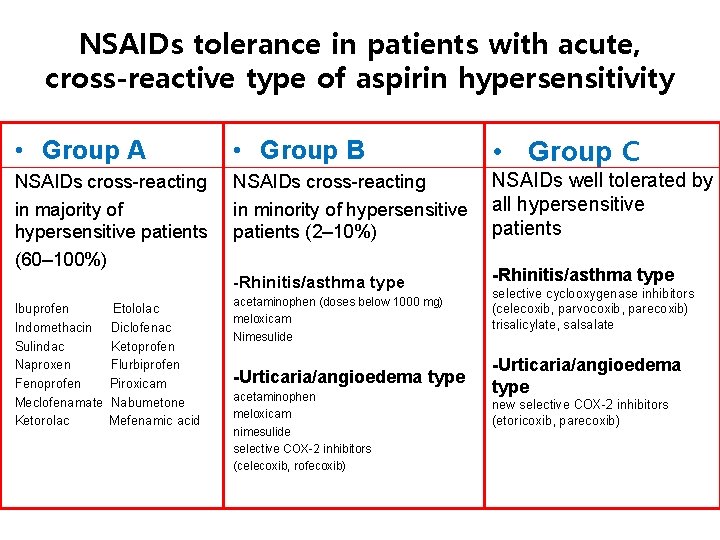
NSAIDs tolerance in patients with acute, cross-reactive type of aspirin hypersensitivity • Group A • Group B • Group C NSAIDs cross-reacting in majority of hypersensitive patients (60– 100%) NSAIDs cross-reacting in minority of hypersensitive patients (2– 10%) NSAIDs well tolerated by all hypersensitive patients -Rhinitis/asthma type Ibuprofen Indomethacin Sulindac Naproxen Fenoprofen Meclofenamate Ketorolac Etololac Diclofenac Ketoprofen Flurbiprofen Piroxicam Nabumetone Mefenamic acid acetaminophen (doses below 1000 mg) meloxicam Nimesulide -Urticaria/angioedema type acetaminophen meloxicam nimesulide selective COX-2 inhibitors (celecoxib, rofecoxib) selective cyclooxygenase inhibitors (celecoxib, parvocoxib, parecoxib) trisalicylate, salsalate -Urticaria/angioedema type new selective COX-2 inhibitors (etoricoxib, parecoxib)
- Slides: 38