Type 2 Diabetes Outcomes Interventions in the Hospitalized
Type 2 Diabetes: Outcomes & Interventions in the Hospitalized African American Patient Zanetta Randolph University of Central Florida
So…. Who Is Involved? The effects of type 2 diabetes mellitus, span all cultures, age groups, ethnicities and sexual orientations. The implications of this disease, however, have been shown to wreak a disproportionate havoc amongst the specific population subset of adult African Americans, hospitalized throughout all levels of care. African Americans are 1. 6 times more likely to have diabetes compared to their Caucasian counterparts (Gumbs, 2012). In a recently published study, Healy, Black, Harris, Lorenz and Dungan (2013) found that of 2, 265 patients included in the study, a higher percentage of readmittance to the hospital setting existed amongst African American patients when compared to whites. The study marks higher readmission rates among African Americans at both 30 day and 180 day timeframes.
Is It Even a Valid Concern? According to Kim, Ross, Melkus, Zhao, and Boockvar (2010) in a study examining the scheduled and unscheduled hospital readmission rates among diabetic patients in California, African Americans were more likely to be readmitted than both Caucasians and Hispanics for unscheduled hospital readmissions. In 7. 21% of those readmissions, diabetes with unspecified complications was the cause for a return trip to the hospital within 30 days, second only to congestive heart failure (Kim et. al. , 2010). READMISSION COSTS MONEY!!!! 2012 Estimates show that diabetes (type 1 and 2) costs the U. S. nearly $245 BILLION DOLLARS in direct and indirect costs (CDC, 2014).
Now…What’s the Issue? PROBLEM STATEMENT African American diabetic patients experience poorer selfmanagement ability and a higher frequency of hospital readmissions when compared to their Caucasian counterparts as a result of patient education deficits, underutilization of racially conducive learning styles, and minimal attention devoted to evaluating patient perception of type 2 diabetes mellitus.
So…. Why Would A Nurse Care? ? • Nurses are at the bedside caring for these patients. Nurses are the frontline providers of patient care, advocacy and education!!!! • Nurses can enforce change and do it utilizing evidence based practice!! • Decreased readmission leads to better patient outcomes, increased institutional integrity, and decreased hospital expenses.
So…What’s The Plan For Patient Education Deficits ? BEEF UP THE EDUCATION!! African Americans (definitely not exclusively) need more than just discharge pamphlets with information from the floor nurse that pertains to basic skills such as operating a glucose monitor, injecting insulin into an orange to practice before injecting themselves, or a small list of symptoms pertaining to hypoglycemia and hyperglycemia. Healy, Black, Harris, Lorenz and Dungan (2013) found that focused education including not only the above, but also a patient curriculum based on American Diabetes Association approved material, DVD’s, flow sheets and checklists, evaluation of patient comprehension and response, an assessment of followup needs, as well as demonstration kits and conversation maps saw an associated 34% reduction in all-cause readmission odds at the end of 30 days, and a decrease of 20% by 180 days.
What About The Problem of Underutilization of Racially Conducive Learning Styles? ? Consider the inclusion of religion/spirituality in learning materials &/or education opportunities. African American religious traditions and spirituality are major coping mechanisms for the African American patient and can provide comfort for many during disturbing experiences (Boyd-Franklin, 2010). Religion/ spirituality utilized in whole person care- Increases odds of patient resorting to health seeking behaviors and the patient being motivated to learn and grow. Include internet usage as one of the major sources used in African American bedside education. According to Moussa, Sherrod and Choi (2013), lower diabetes literacy levels along with a lack of access to sound diabetes information may be among the factors that lead to poorer management of the illness within African American patients. This may in part be a result of reliance on traditional pamphlets, booklets and other text only sources of diabetic literature. Computer and internet usage among African Americans was explored by utilizing two distinct studies. It was concluded that, instead of the traditional methods, the African American population was more apt to utilize computers to access health information via the internet (Moussa et al. , 2013) Within the study, which was conducted at Winston Salem State University School of Health and Sciences, Moussa et al states that research led to the development of an internet program called the e. Care We Care Program, in which positive interactions among African American patients were seen (2013) The study provides examples of what measures could be initially instituted in the inpatient setting, especially with the increased use of in room web-television education networks being installed in hospital patient rooms.
Lastly, there is the issue of… minimal attention devoted to evaluating patient perception of type 2 diabetes mellitus Consider the patient’s perception of type 2 diabetes and ability to manage!!! Perception of the patient affects adherence, confidence and faith. The nurse must work alongside each specific patient and encourage patient competence through validation, and positive feedback. The way people think influences the way they feel, positively or negatively, so then positive thinking can relieve the depressive state and or related discomforts (Alves- Apostolo & Kolcaba, 2009). The patient will be capable of making decisions and taking responsibility for development of daily activities consistent with good control of type 2 diabetes after acting alongside health professionals, particularly nurses (Baggio et. al. 2013).
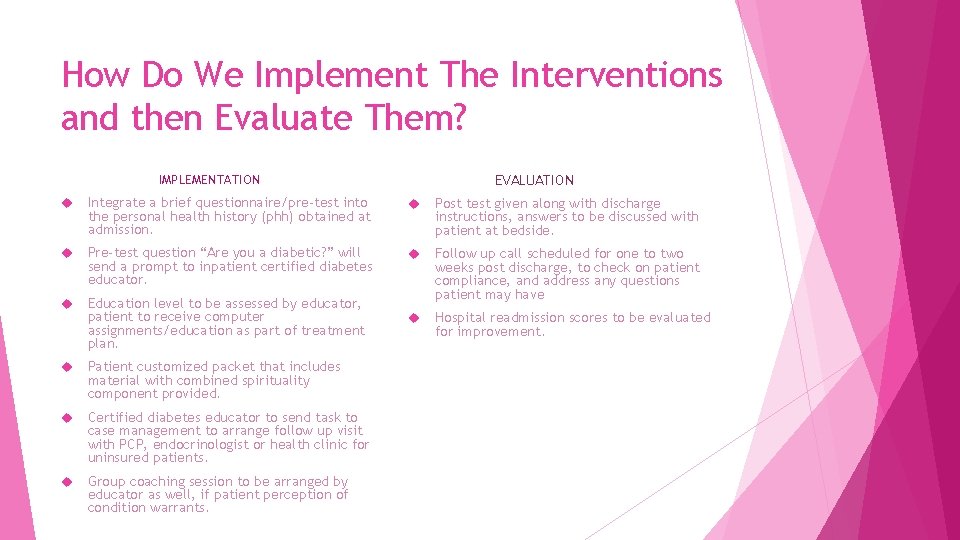
How Do We Implement The Interventions and then Evaluate Them? EVALUATION IMPLEMENTATION Integrate a brief questionnaire/pre-test into the personal health history (phh) obtained at admission. Post test given along with discharge instructions, answers to be discussed with patient at bedside. Pre-test question “Are you a diabetic? ” will send a prompt to inpatient certified diabetes educator. Education level to be assessed by educator, patient to receive computer assignments/education as part of treatment plan. Follow up call scheduled for one to two weeks post discharge, to check on patient compliance, and address any questions patient may have Hospital readmission scores to be evaluated for improvement. Patient customized packet that includes material with combined spirituality component provided. Certified diabetes educator to send task to case management to arrange follow up visit with PCP, endocrinologist or health clinic for uninsured patients. Group coaching session to be arranged by educator as well, if patient perception of condition warrants.
REFERENCES Apóstolo, J. , & Kolcaba, K. (2009). The effects of guided imagery on comfort, depression, anxiety, and stress of psychiatric inpatients with depressive disorders. Archives of Psychiatric Nursing, 23(6), 403 -411. doi: 10. 1016/j. apnu. 2008. 12. 003 Baggio, S. , Aparecida Sales, C. , Silva Marcon, S. , & Lima Santos, A. (2013). Perception of people suffering from diabetes regarding the disease and the reasons for hospital readmission: a descriptive study. Online Brazilian Journal of Nursing, 12(3), 501 -510. Boyd-Franklin, N. (2010). Incorporating spirituality and religion into the treatment of African-american clients. The Counseling Psychologist. 38(7) 976– 1000. doi: 10. 1177/0011000010374881 Centers for disease control. (2014). National diabetes statistics report, 2014. Retrieved from: http: //www. cdc. gov/diabetes/pubs/statsreport 14/national-diabetes-report-web. pdf Gumbs, J. (2012). Relationship between diabetes self-management education and self-care behaviors among African American women with Type 2 diabetes. Journal of Cultural Diversity, 19(1), 18 -22. Healy, S. , Black, D. , Harris, C. , Lorenz, A. , & Dungan, K. (2013). Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care, 36(10), 2960 -2967. doi: 10. 2337/dc 13 -0108 Kim, H. , Ross, J. , Melkus, G. , Zhao, Z. , & Boockvar, K. (2010). Scheduled and unscheduled `hospital readmissions among diabetic patients. American Journal of Managed Care, 16 (10): 760 -767 Moussa, M. , Sherrod, D. , & Choi, J. (2013). An e-health intervention for increasing diabetes knowledge in African Americans. International Journal of Nursing Practice, 1936 -43. doi: 10. 1111/ijn. 12167
- Slides: 10