Turbinectomy By Carly Winegar Anatomy Nasal Turbinates Nasal
Turbinectomy By Carly Winegar
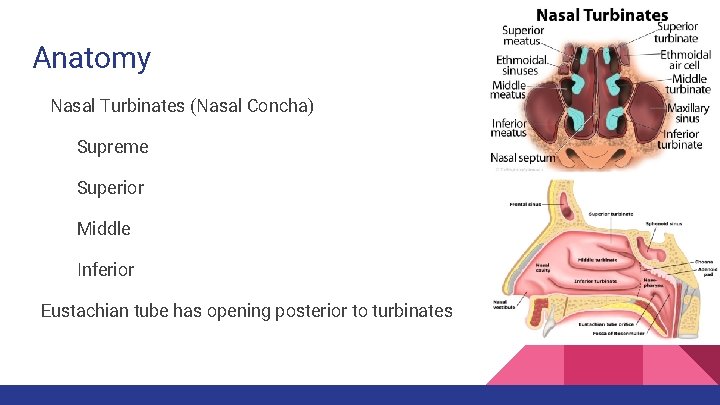
Anatomy Nasal Turbinates (Nasal Concha) Supreme Superior Middle Inferior Eustachian tube has opening posterior to turbinates
Physiology Forces air to flow steadily around the largest possible surface area of nasal mucosa to clean and warm the inhaled air to prepare it for the lungs Ciliated mucous membrane with shallow blood supply Bodies first line of defense against particles in inhaled air Erectile tissue that causes nasal congestion or decongestion
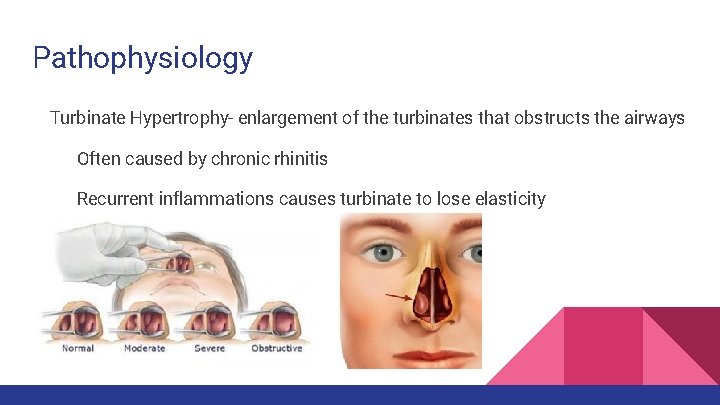
Pathophysiology Turbinate Hypertrophy- enlargement of the turbinates that obstructs the airways Often caused by chronic rhinitis Recurrent inflammations causes turbinate to lose elasticity
Diagnostic Exams Direct visual exam of the nasal passage Mirror Examination Sinuscopy History and Physical to determine which method will be used
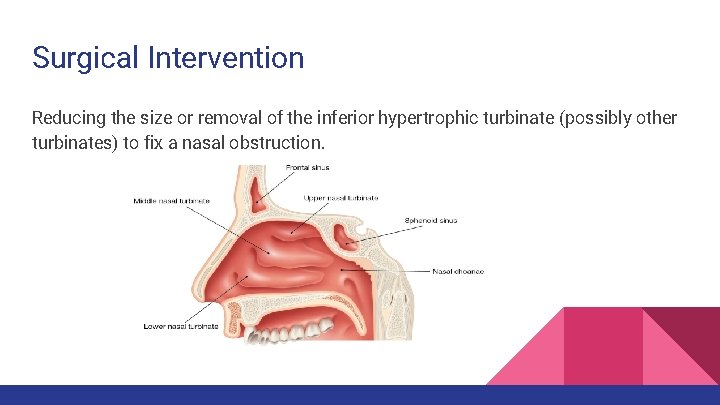
Surgical Intervention Reducing the size or removal of the inferior hypertrophic turbinate (possibly other turbinates) to fix a nasal obstruction.

Special Considerations May be performed in conjunction with other nasal procedures such as septoplasty, rhinoplasty, or sinus surgery. Be familiar with the methods used by your facility and your surgeon’s preference: Electrocautery Sclerosing agents Radiofrequency ablation Cryosurgery Argon Plasma surgery Laser Turbinectomy

Anesthesia General Anesthesia Local Anesthesia
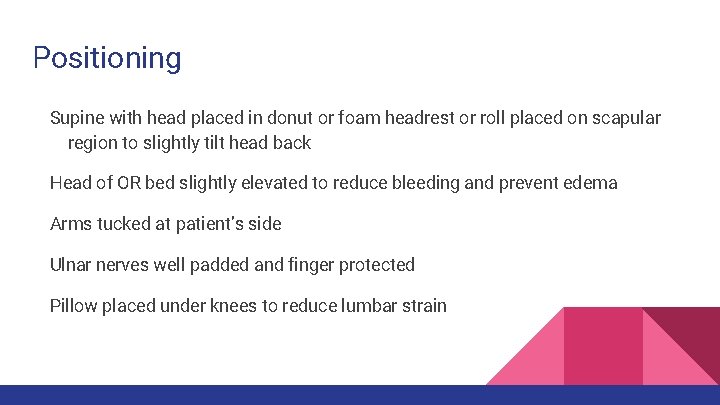
Positioning Supine with head placed in donut or foam headrest or roll placed on scapular region to slightly tilt head back Head of OR bed slightly elevated to reduce bleeding and prevent edema Arms tucked at patient’s side Ulnar nerves well padded and finger protected Pillow placed under knees to reduce lumbar strain
Skin Prep begins at the upper lip and extends to hairlines and beyond the chin Removal of facial hair usually not necessary
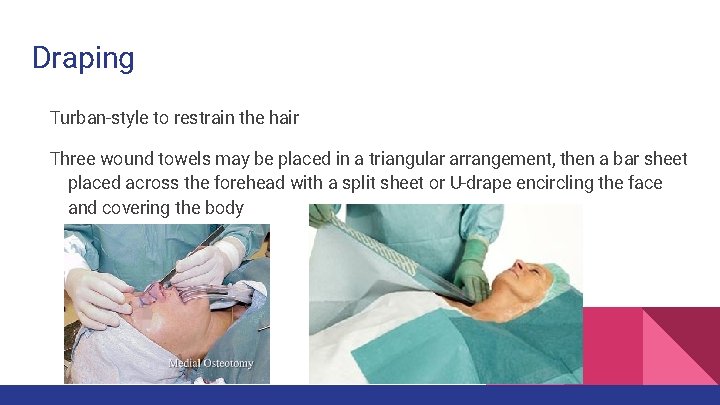
Draping Turban-style to restrain the hair Three wound towels may be placed in a triangular arrangement, then a bar sheet placed across the forehead with a split sheet or U-drape encircling the face and covering the body
Incision No incisions made to enter nasal cavity Submucosal incision through lining of the nose
Supplies Medicine cups Local syringes Two 25 or 27 -gauge needles Long cotton tip applicators Packing materials Local anesthetic Topical anesthetic (Cocaine 4%) Protective eyewear for the patient
Equipment Headlamp ESU Bipolar unit Insulated ESU with suction attachment Laser (if doing laser method) Carbon Dioxide Nd: YAG Diode lasers
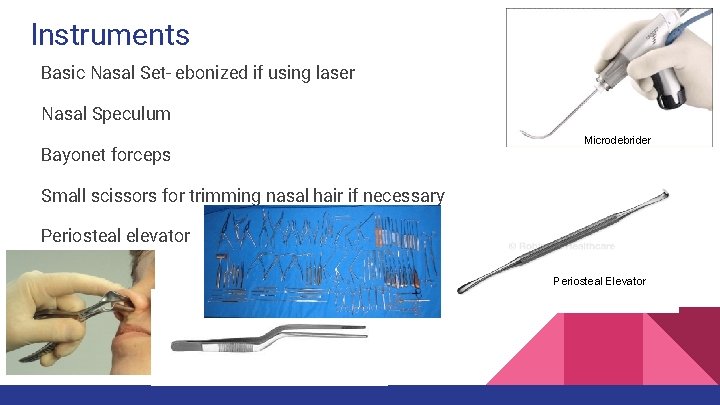
Instruments Basic Nasal Set- ebonized if using laser Nasal Speculum Bayonet forceps Microdebrider Small scissors for trimming nasal hair if necessary Periosteal elevator Microdebrider Periosteal Elevator
Inferior Turbinectomy Steps • Submucosal approach is used • The nasal mucosa along the edge of affected turbinate is incised • A periosteal elevator is placed underneath the turbinate, elevating and fracturing it medially (referred to as infracturing) • Angled scissors and rongeur are used to excise the bone and soft tissue of the turbinate • Insulated electrocautery is used for hemostasis and suction followed by nasal packing
Microdebrider Turbinectomy • A small tube is inserted through a small submucosal incision within the nose • The microdebrider is inserted into the turbinate • A CT-guided imaging system is used to assist the surgeon in viewing the surgical site • The microdebrider is activated with the use of a foot pedal and it quickly and accurately removes the turbinate without damaging surrounding tissue
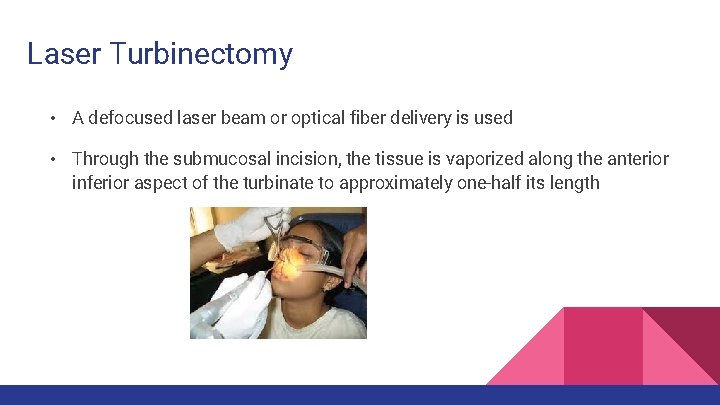
Laser Turbinectomy • A defocused laser beam or optical fiber delivery is used • Through the submucosal incision, the tissue is vaporized along the anterior inferior aspect of the turbinate to approximately one-half its length
Counts Initial Count When closing submucosa Final Count
Dressing Materials Nose packed with gauze Dry or impregnated with ointment (antibiotic or vaseline) to prevent crusting and infection and aid in removal Patient provided with mustache-style dressing that may be secured with tape or tied around patient’s head Patient forewarned before procedure that packing may be uncomfortable and will require breathing through mouth
Specimen Care No specimen unless turbinate is removed- send to pathology
Prognosis Usually done on an outpatient basis Responsible person drives patient home and stay with them for next 24 hours A visit to the doctor’s office on the first or second postoperative day may be necessary to remove packing
Complications Hemorrhaging Postoperative dryness or crusting Postoperative SSI Formation of adhesions Conchal bone necrosis
Wound Class/ Management Class II: Clean- Contaminated
- Slides: 24