Tuberculosis in children Part One By Malak Shaheen
Tuberculosis in children Part One By Malak Shaheen (MD, Ph. D Pediatrics)
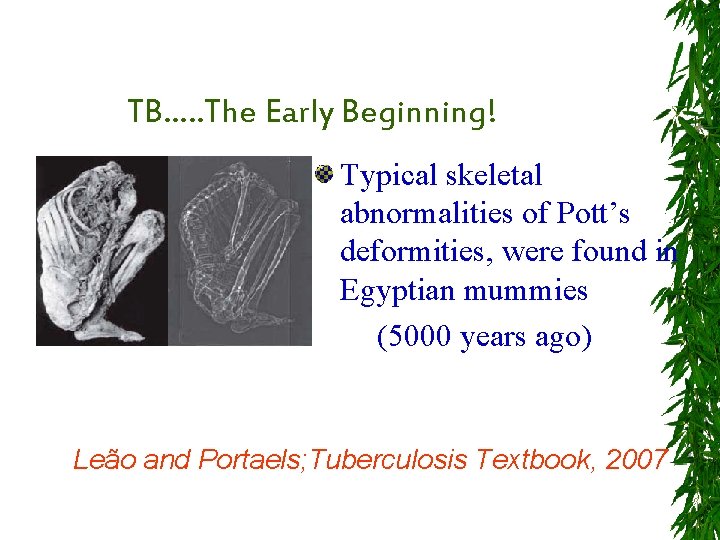
TB…. . The Early Beginning! Typical skeletal abnormalities of Pott’s deformities, were found in Egyptian mummies (5000 years ago) Leão and Portaels; Tuberculosis Textbook, 2007

TB…. . The Early Beginning! In 1890, about eight years after the discovery of the tubercle bacillus, Robert Koch (1843 -1910) announced a cure for TB. He obtained a heat-inactivated filtrate from cultures of M. tuberculosis. This product, known as “Koch's Old Tuberculin”,
However, TB patients who received tuberculin had generalized systemic reactions , in contrast to people without TB, who did not develop this violent reaction. These observations were the basis for the proposal of the use of tuberculin as a diagnostic test
In 1934, Florence Siebert made a simple protein precipitate of the old tuberculin and named it purified protein derivative (PPD)
Childhood Tuberculosis The Invisible Enemy Part 2 By Malak Shaheen (MD, Ph. D Pediatrics)
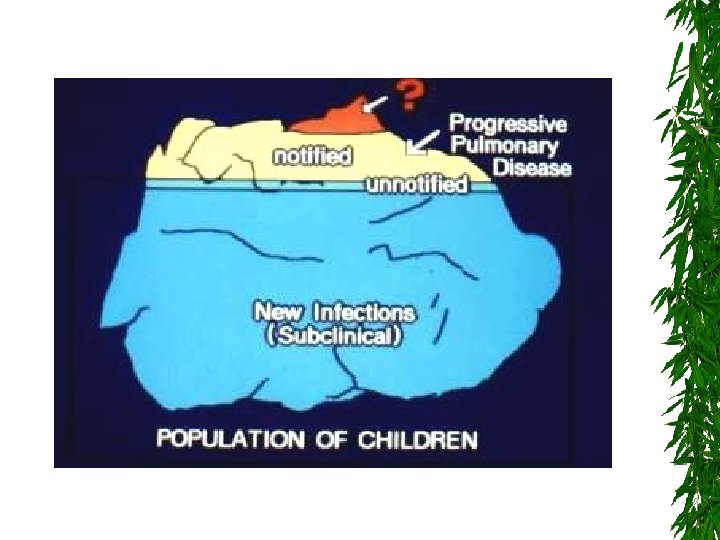
Why invisible ?
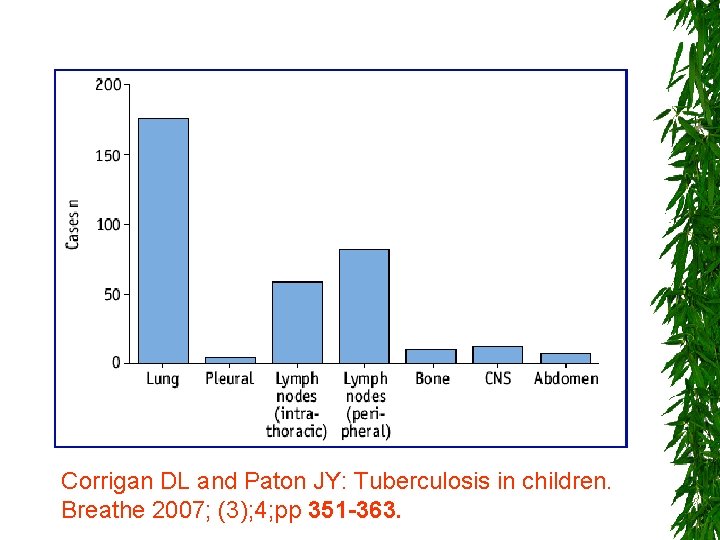
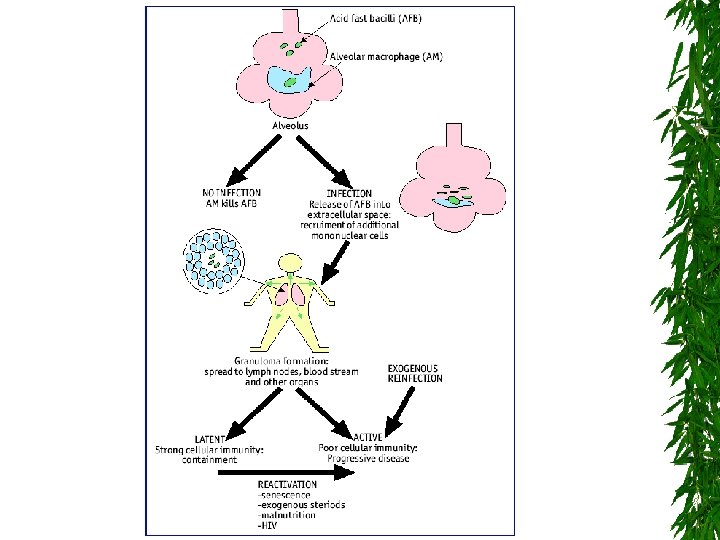
Corrigan DL and Paton JY: Tuberculosis in children. Breathe 2007; (3); 4; pp 351 -363.
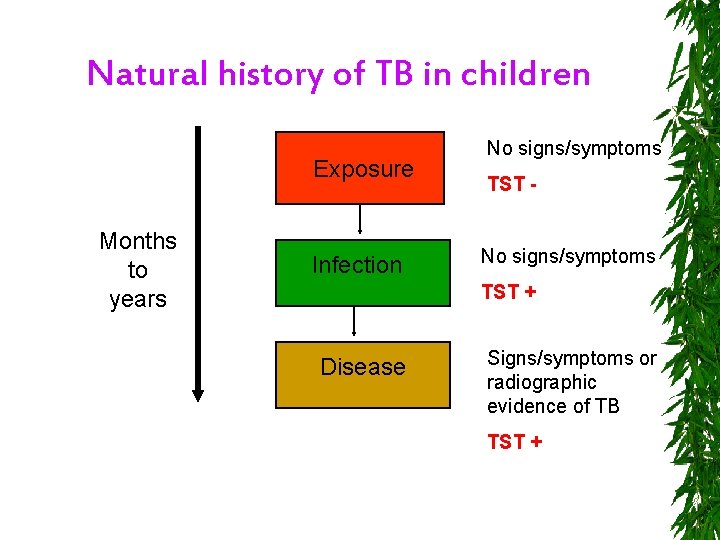
Natural history of TB in children Exposure Months to years Infection No signs/symptoms TST + Disease Signs/symptoms or radiographic evidence of TB TST +

More challenges ……. MDR HIV Children
Invisible – How to tackle ?
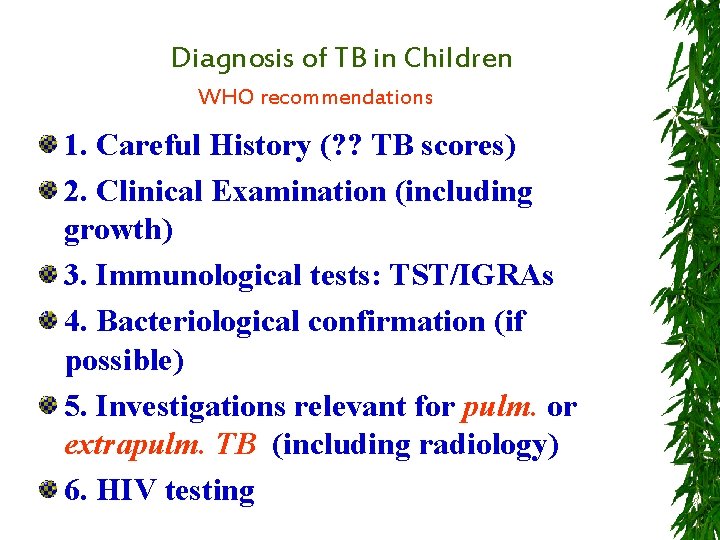
Diagnosis of TB in Children WHO recommendations 1. Careful History (? ? TB scores) 2. Clinical Examination (including growth) 3. Immunological tests: TST/IGRAs 4. Bacteriological confirmation (if possible) 5. Investigations relevant for pulm. or extrapulm. TB (including radiology) 6. HIV testing
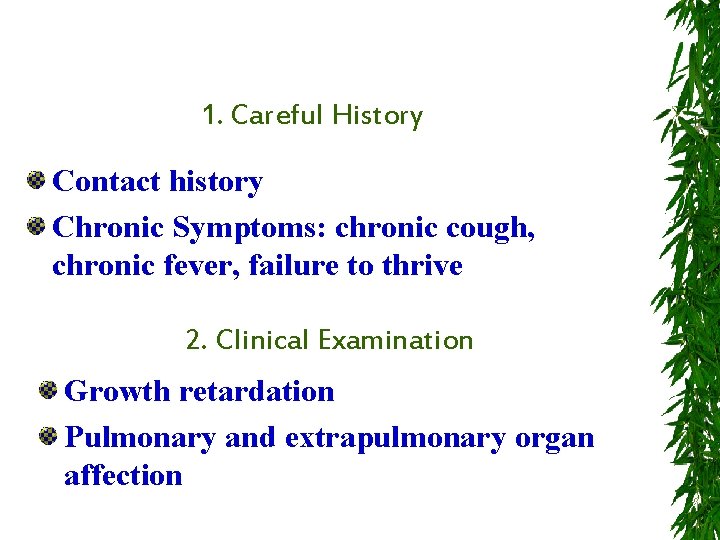
1. Careful History Contact history Chronic Symptoms: chronic cough, chronic fever, failure to thrive 2. Clinical Examination Growth retardation Pulmonary and extrapulmonary organ affection
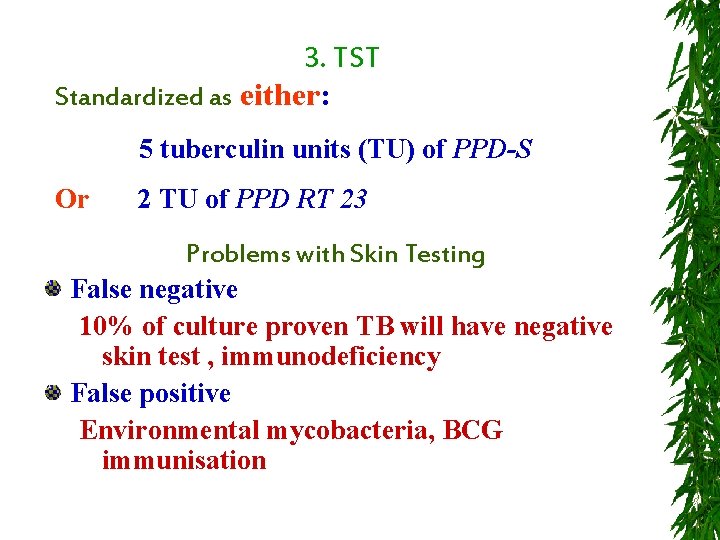
3. TST Standardized as either: 5 tuberculin units (TU) of PPD-S Or 2 TU of PPD RT 23 Problems with Skin Testing False negative 10% of culture proven TB will have negative skin test , immunodeficiency False positive Environmental mycobacteria, BCG immunisation
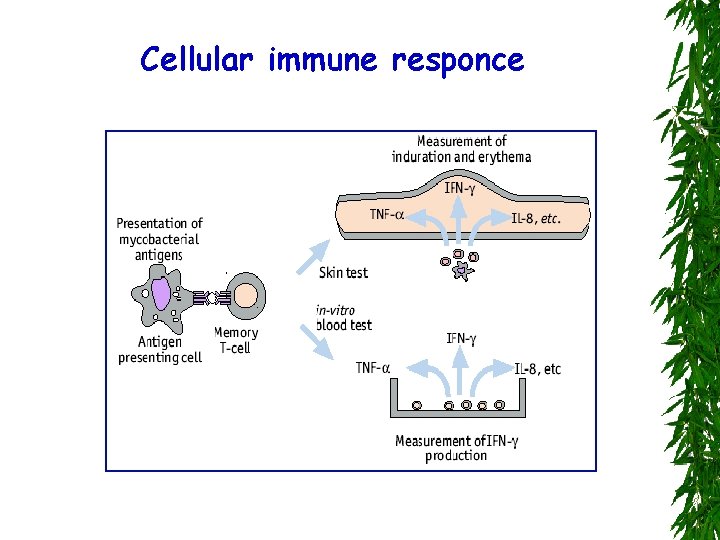
Cellular immune responce
TST: How to perform in children? Standardized as either: 5 tuberculin units (TU) of PPD-S Or 2 TU of PPD RT 23 Techniques with Skin Testing Heaf gun test Mantoux intradermal test
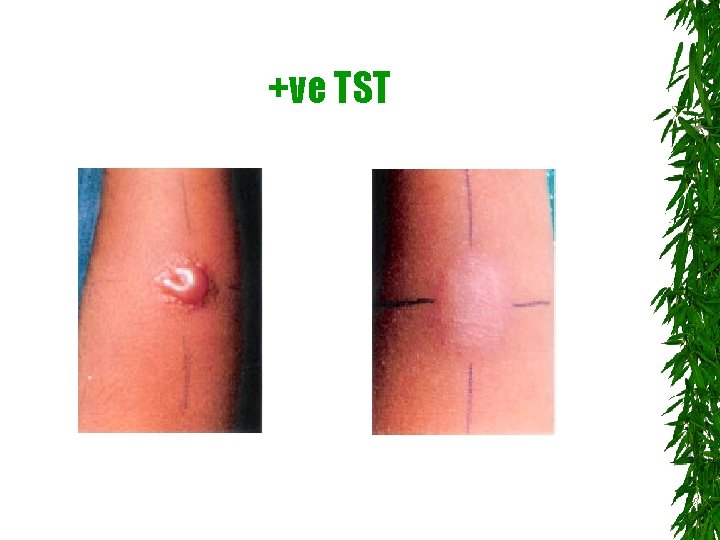
+ve TST
Challenges with T. Skin Testing False negative 10% of culture proven TB will have negative skin test , immunodeficiency False positive Environmental mycobacteria, BCG immunization Difficult Technique and Interpretation
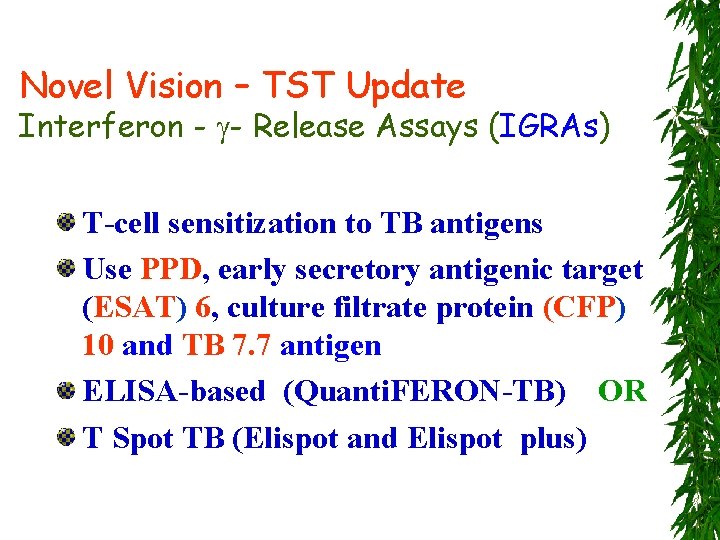
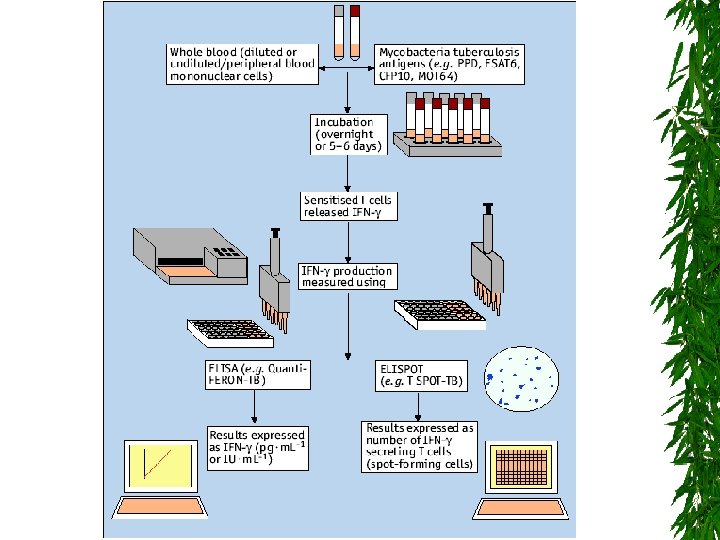
Novel Vision – TST Update Interferon - - Release Assays (IGRAs) T-cell sensitization to TB antigens Use PPD, early secretory antigenic target (ESAT) 6, culture filtrate protein (CFP) 10 and TB 7. 7 antigen ELISA-based (Quanti. FERON-TB) OR T Spot TB (Elispot and Elispot plus)
Applications 1. Diagnosis of active TB disease 2. Distinguish between M tuberculosis and NTM 3. Differentiate M tuberculosis from BCG 4. Latent infection TB infection 5. Monitor treatment
4. Bacteriological Confirmation First: Obtain appropriate samples for smear microscopy, culture and histopathology if possible. Samples could be; Sputum, gastric lavage, induced sputum, peripheral LN, pleural fluid, CSF, ascitic tap, joint tap, pericardial tap …. . etc
Microscopic Smear Easy, inexpensive and fast Ziehl-Neelsen (ZN) stain Fluorochrome stains (auramine-rhodamine) better than ZN Ba et al Int J Tuberc Lung Dis 1999; 3: 1101 -05 Sputum induction with nebulised 3% saline showed a better yield Zar et al Lancet 2005 365: 130 -4
Conventional Cultures Lowenstein-Jensen media Up to 3 weeks for positive growth Yield from extra-pulmonary sites lower (<50%)
Recent! Automated Liquid Media Various automated liquid media available (BACTEC 460, MGIT) Have faster turn around times (1 -2 weeks vs 3 -4 weeks) and higher recovery rates than solid media
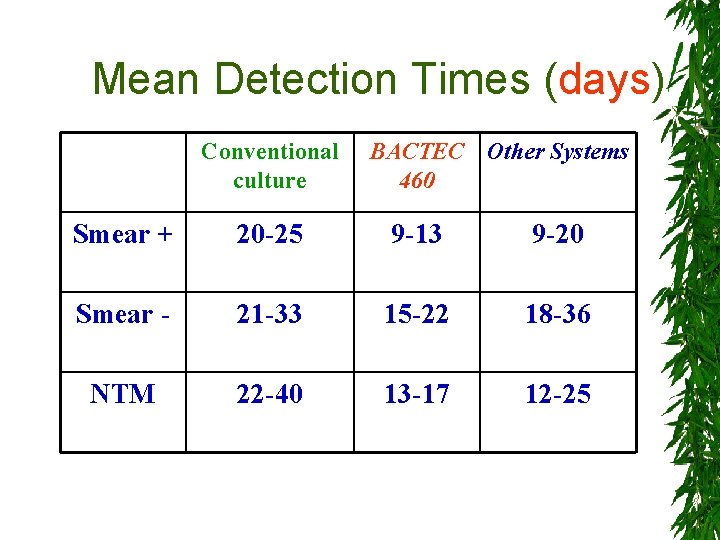
Mean Detection Times (days) Conventional culture BACTEC Other Systems 460 Smear + 20 -25 9 -13 9 -20 Smear - 21 -33 15 -22 18 -36 NTM 22 -40 13 -17 12 -25
5. Investigations relevant for suspected TB Flexible Bronchoscopy Endobronchial disease Luminal obstruction Sample collection Bronchoscopy samples have lower yield than 3 gastric aspirates
Nucleic Acid Amplification Techniques Sensitivity 40% and specificity 80% in children. False positives (NTM) and false negative (pauci-bacillary disease) Lower sensitivity with extrapulmonary samples Molecular probes for rifampicin resistance (mutations rpo. B gene) Molecular typing (RFLP, VNTR, MIRU) for epidemiological investigation
Diagnostic Accuracy of Chest X-rays Sensitivity of 60% in adults with culture confirmed TB Sensitivity of 40% and specificity of 74% in children De Villliers 2004 Australasian Radiology 2004; 48: 148 -153 Lower sensitivity in HIV positive adults (and children? )
CT Scan • Helpful in identifying hilar lymphadenopathy (more than 50% of children with normal chest x-ray) • Inter observer variability especially in differentiating thymus • Andronikou et al Pediatr Radiol 2005; 35: 425 -28 • High resolution and spiral CT imaging
Magnetic Resonance Imaging Useful in distinguishing different tissue characteristics e. g. fibrosis versus inflammation Useful for extrapulmonary disease especially bone/joint

Treatment
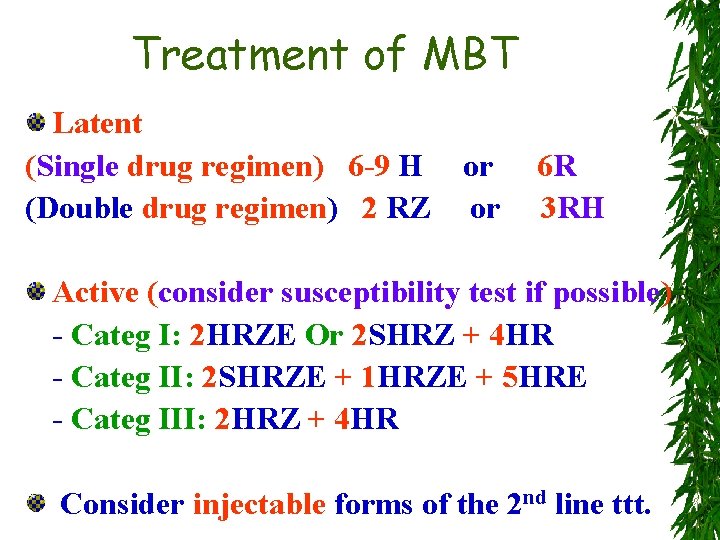
Treatment of MBT Latent (Single drug regimen) 6 -9 H (Double drug regimen) 2 RZ or or 6 R 3 RH Active (consider susceptibility test if possible) - Categ I: 2 HRZE Or 2 SHRZ + 4 HR - Categ II: 2 SHRZE + 1 HRZE + 5 HRE - Categ III: 2 HRZ + 4 HR Consider injectable forms of the 2 nd line ttt.

Special Considerations
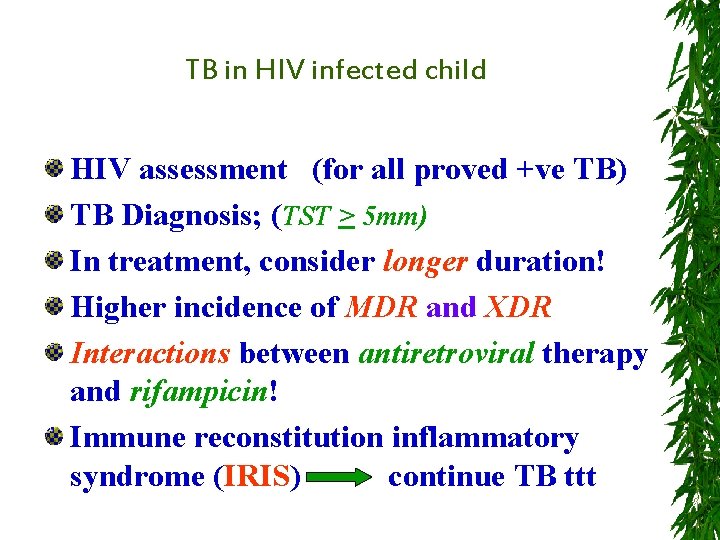
TB in HIV infected child HIV assessment (for all proved +ve TB) TB Diagnosis; (TST > 5 mm) In treatment, consider longer duration! Higher incidence of MDR and XDR Interactions between antiretroviral therapy and rifampicin! Immune reconstitution inflammatory syndrome (IRIS) continue TB ttt
Prophylaxis
For HIV children (if CD 4 < 100/mm) Azithromycin or clarithromycin (3 -6 Months) For TB contact (if < 5 years or immunosuppressed) 6 -9 H or 6 R or 9 -12 EFq
Hospital infection control measures (isolation, sterilization, physical barriers, …. . ) Index case findings Managing contacts (chemoprophylaxis) Family survey Negative pressure rooms Care giver with particulate respirators
Better treatment of TB in Children Criteria of drug resistant TB in Children (? ) WHO (2014)
What do we want to achieve in TB care? Targets “TB elimination by 2050” 44
START: Better Diagnosis of TB in Children Optimal sample collection Improved laboratory procedures Better imaging techniques Immune-based diagnostics
46
TB or not TB; that is the question !
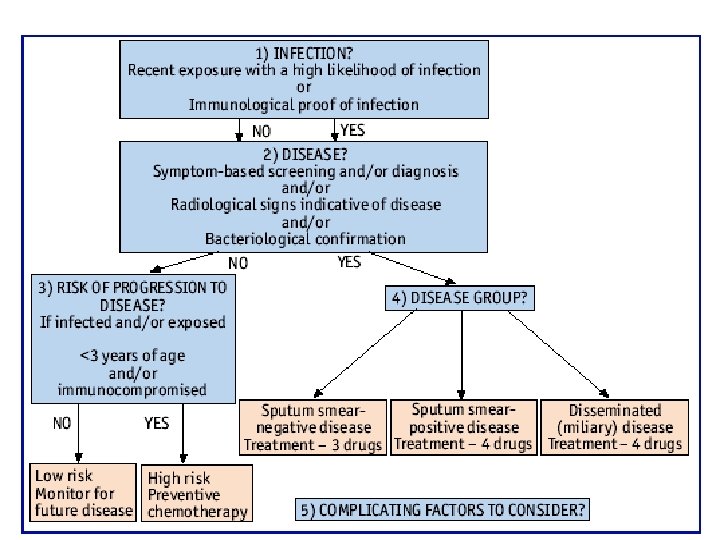
Evidence of TBNET consensus 2009 report 1) Children are more likely to develop tuberculosis than adults after exposure to an active case, hence contact screening and chemoprophylaxis are particularly important (evidence B).
2) The diagnosis of latent infection with M. tuberculosis in children relies on history of exposure, positivity of the tuberculin skin test and exclusion of clinical symptoms and radiological findings consistent with active tuberculosis (evidence B).
3) The positive and negative predictive value of IGRAs remains to be established in children (evidence D). 4) Latency, as assayed by the tuberculin skin test and IGRA, is a state of persistent mycobacteria-specific T-cell responses in the absence of clinical evidence for tuberculosis disease (evidence A).
5) Whether latent tuberculosis infection depends on the presence of living mycobacteria is presently unclear (evidence A). 6) The tuberculin skin test and IGRAs measure ‘‘lasting tuberculosis immune responses’’ and not ‘‘latent tuberculosis infection’’ (evidence A).
7) The tuberculin skin test and IGRAs cannot discriminate active from latent infection (evidence A). 8) In general, tuberculin skin test and IGRA results correlate poorly, mainly because of positive tuberculin skin test results in individuals vaccinated with BCG (evidence A).
9) IGRAs may be superior to the tuberculin skin test in identifying contacts at risk of developing tuberculosis (evidence C).
10) Contact children aged less than 5 yrs in particular should be started on chemoprophylaxis, independent of their tuberculin skin test result (evidence B). 11) Chemoprophylactic or preventive regimes are identical in adults and children, but the dose needs to be adjusted according to weight (evidence B).
Further Practice …. Pediatric TB cases
Further Readings …. www. Tuberculosis. Textbook. com
Further Readings …. WHO 2014
Further Readings …. First edition - 2008
Summary of TB in Children 2014

Thank You childshaheen@yahoo. com
- Slides: 61