Tuberculosis Dr Hamed AlZoubi Faculty of Medicine University
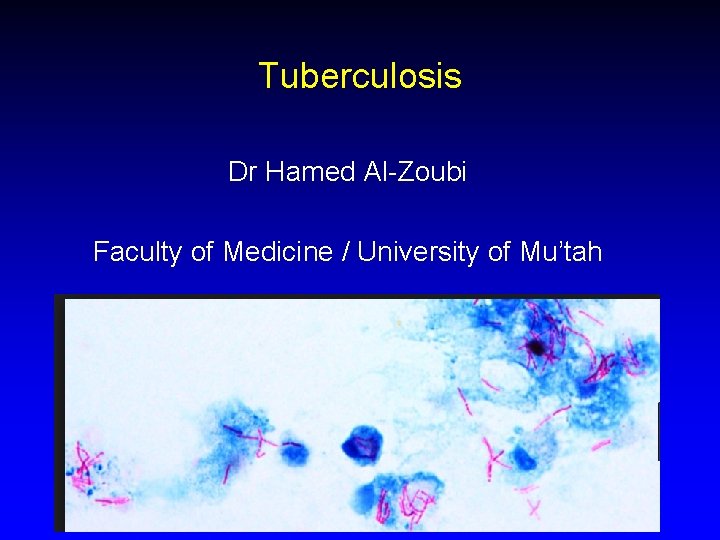
Tuberculosis Dr Hamed Al-Zoubi Faculty of Medicine / University of Mu’tah
Outline • • • Introduction Classification and structure Pathogenesis Manifestations Diagnosis • Environmental TB
Burden • Most common cause of infectious disease–related mortality worldwide • 2 billions cases worldwide • 9 -10 million new cases yearly • 1 -2 million deaths yearly • Main concern: immunocompromised, HIV; MDR
Mycobacterium Tuberculosis Complex Major human pathogens: 1. Mycobacterium tuberculosis (M. tuberculosis) 2. M. Africanum 3. M. Bovis 4. M. microtii: smooth growth on culture • Aerobic, non motile acid fast bacilli. • UV, Alcohol, aldehydes - sensitive • Alkaline acid and ammonia - resistant
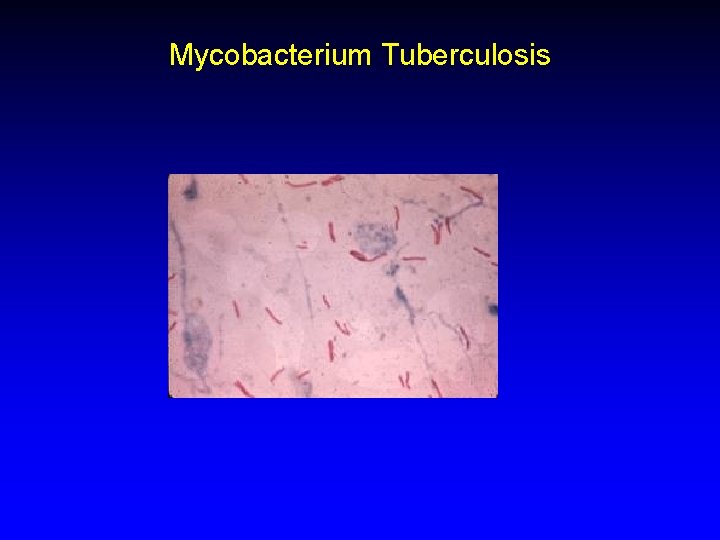
Mycobacterium Tuberculosis
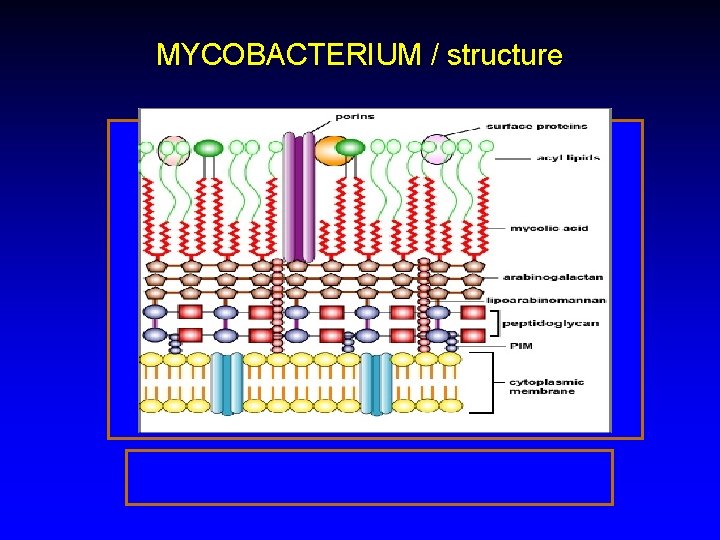
MYCOBACTERIUM / structure
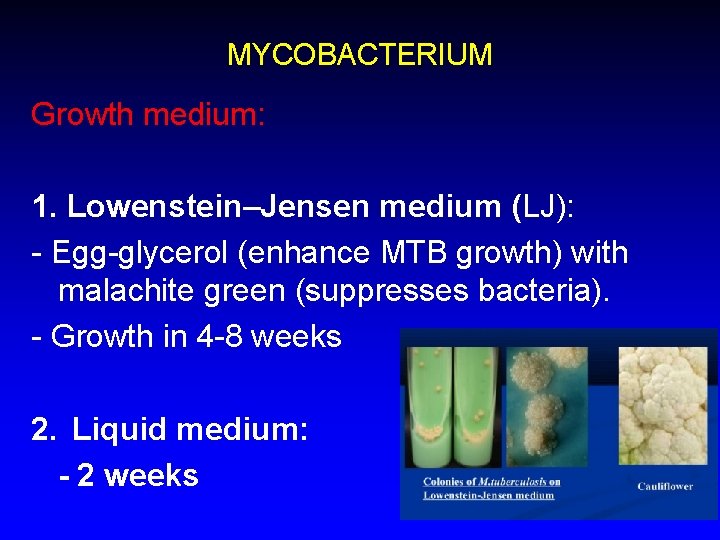
MYCOBACTERIUM Growth medium: 1. Lowenstein–Jensen medium (LJ): - Egg-glycerol (enhance MTB growth) with malachite green (suppresses bacteria). - Growth in 4 -8 weeks 2. Liquid medium: - 2 weeks
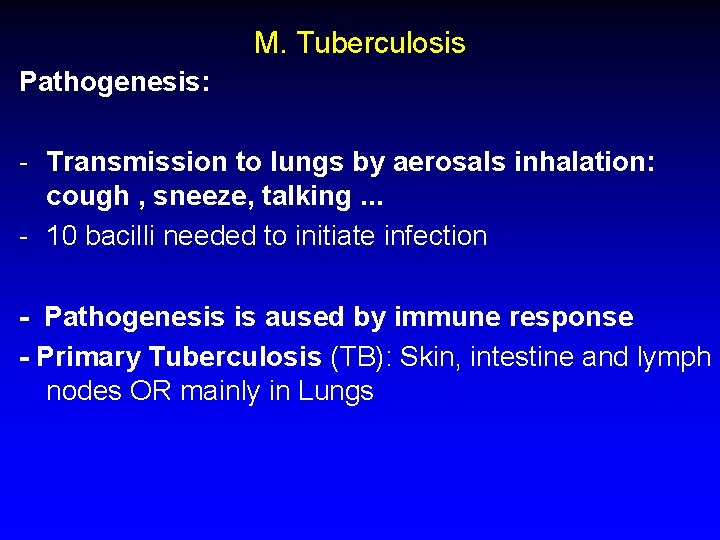
M. Tuberculosis Pathogenesis: - Transmission to lungs by aerosals inhalation: cough , sneeze, talking. . . - 10 bacilli needed to initiate infection - Pathogenesis is aused by immune response - Primary Tuberculosis (TB): Skin, intestine and lymph nodes OR mainly in Lungs
M. Tuberculosis • Lung: Primary TB: usually asymptomatic - Macrophages 1 in alveoli engulf the bacteria - Macrophages migrate To hilar lymph nodes > tubercle (rarely miliary TB in immunocompromised) - Tubercle is attacked by Macrophages 2 (acts by O 2 consumption) > surrounding the lesion in a granuloma (gohn focus) that will become necrotic (caseation) and followed by calcification > latent.
M. Tuberculosis • 90% of primary infections > latent • 10% of primary > secondary TB > meningitis, pott’s disease, urogenital and skin involvement (s. t milliary TB if opened into a blood vessel > disseminated) • Latent • Reactivation of latency or re-infection in immunocomp. Malnourished. . . > Develops into post primary TB (secondary) and usually occurs in the apex of the lung
MYCOBACTERIUM Clinically: • The following factors increase the likelihood that a patient will have tuberculosis (TB): • HIV infection • History of prior TB treatment • TB exposure, Travel to or emigration from a TB endemic area e. g India, South east Africa. . • Homelessness, poverty, malnutrition
MYCOBACTERIUM • Classic features associated with active TB are as follows: • Cough • Weight loss/anorexia • Fever • Night sweats • Hemoptysis (coughing blood) • Chest pain
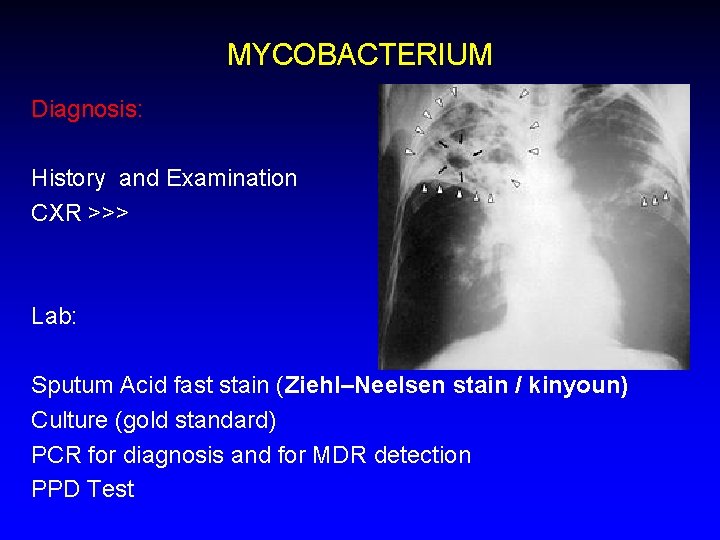
MYCOBACTERIUM Diagnosis: History and Examination CXR >>> Lab: Sputum Acid fast stain (Ziehl–Neelsen stain / kinyoun) Culture (gold standard) PCR for diagnosis and for MDR detection PPD Test
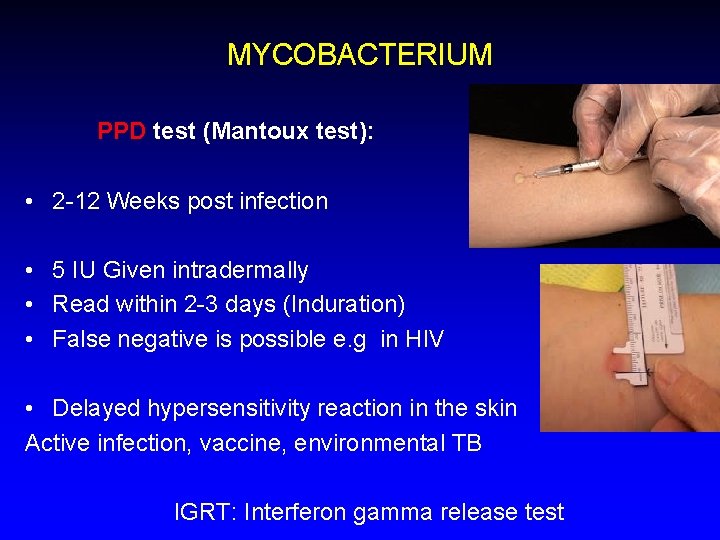
MYCOBACTERIUM PPD test (Mantoux test): • 2 -12 Weeks post infection • 5 IU Given intradermally • Read within 2 -3 days (Induration) • False negative is possible e. g in HIV • Delayed hypersensitivity reaction in the skin Active infection, vaccine, environmental TB IGRT: Interferon gamma release test
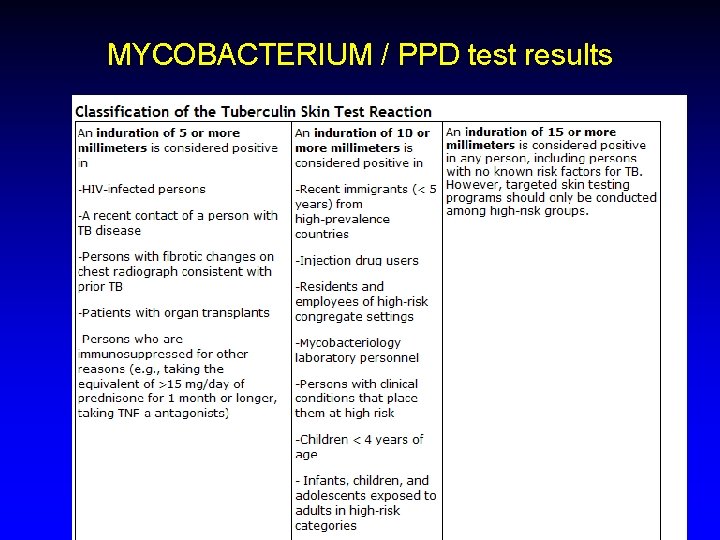
MYCOBACTERIUM / PPD test results
MYCOBACTERIUM Management - principles: Isolation: ? Combination, directly observed therapy (DOT) (1 st line anti TB) RIFINA 6 months +Ethambutol and Pyrazinamide first 2 months 2 nd line treatment in MDR: Macrolides, Fluroquinilones, aminoglycosides, cycloserine. . . 3 rd line treatment: Linezolid, rifabutin, arginine, vitamin D. .
Prevention: BCG life attenuated vaccine: • Bacillus Calmette Guerin - Life attenuated from M. bovis • Contraindications?
Environmental mycobacterium • four groups of mycobacteria associated with human disease classified according to their production of yellow or orange pigment and their rate of growth. • divided into: 1. photochromogens, which develop pigment in (or after exposure to) light 2. scotochromogens, which become pigmented in the dark 3. non-chromogens and rapid growers. Ø visible growth on Löwenstein-Jensen medium within 1 week on subculture
Environmental mycobacterium • Photochromogens: • M. marinum: • The cause of a warty skin infection • Known as swimming pool granuloma or fish tank granuloma. • It grows poorly, if at all, at 37°C, and cultures from skin lesions should be incubated at 33°C.
Environmental mycobacterium/ Scotochromogens • Most slowly growing scotochromogen isolated from sputum or urine are of no clinical significance. • Example on significant isolates: M. scrofulaceum is associated principally with scrofula or cervical lymphadenitis, but also causes pulmonary disease.
Environmental mycobacterium • Non-chromogens: • 1. The most prevalent and important opportunistic pathogens are in a group known as the M. avium intracellulare complex (MAIC) • MAI > think of HIV • 2. M. ulcerans • a very slowly growing species that grows in vitro only at 31 -34°C. • the cause of Buruli ulcer; • it produces a toxin that causes tissue necrosis and is involved in the pathogenesis of the disease.
Environmental mycobacterium • 3. M. xenopi: • A thermophile that grows well at 45°C. • It is principally responsible for pulmonary lesions. • Most reported cases have been from London and south-east England northern France
practical • Acid fast bacilli and LJ medium • Other respiratory pathogens
The End
- Slides: 24