Triple Innominate Osteotomy for Perthes Disease Indications and











- Slides: 44

Triple Innominate Osteotomy for Perthes Disease: Indications and Technique V. Salil Upasani, MD Assistant Clinical Professor Department of Orthopedic Surgery Rady Children’s Hospital San Diego University of California San Diego 6 th Annual IPSG Meeting October 6, 2017
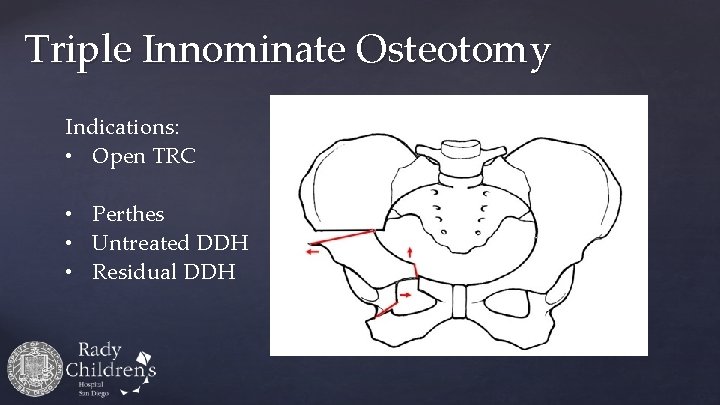
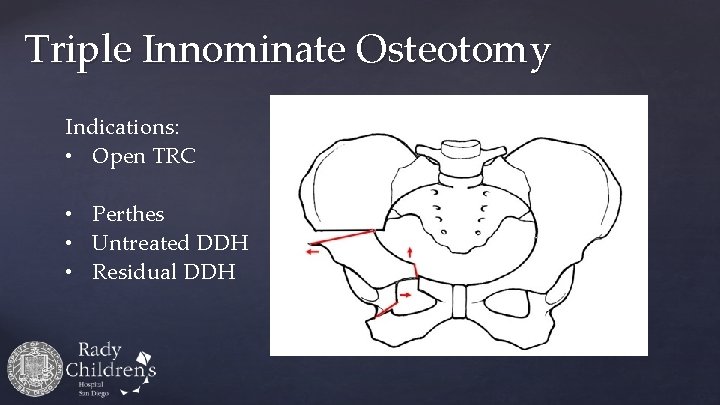
Triple Innominate Osteotomy Indications: • Open TRC • Perthes • Untreated DDH • Residual DDH
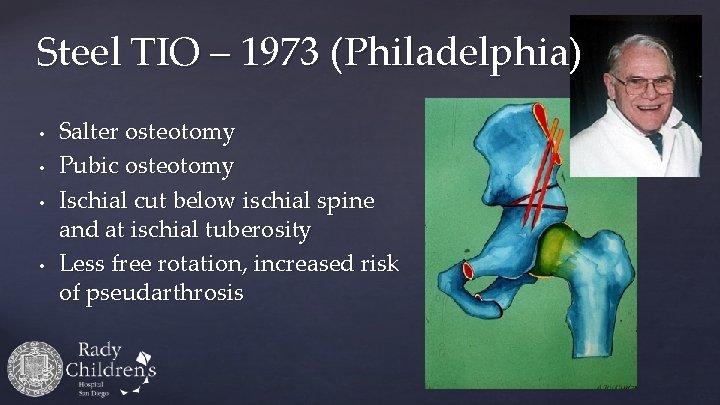
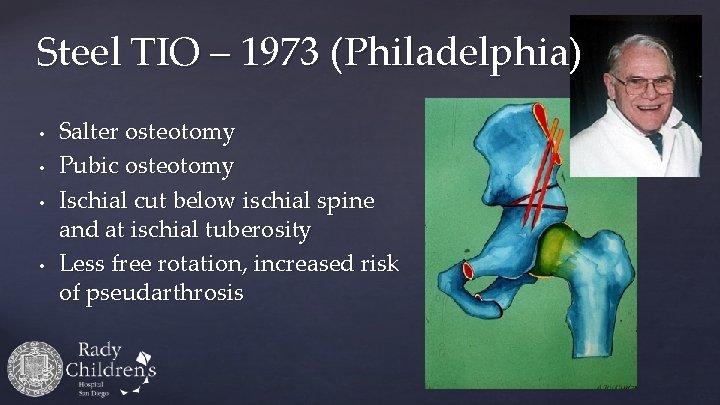
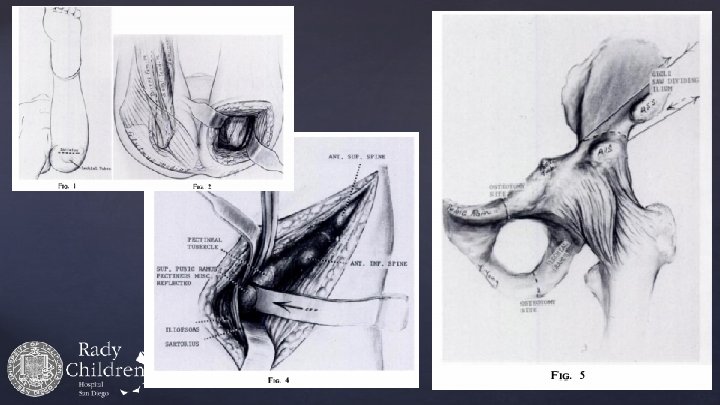
Steel TIO – 1973 (Philadelphia) • • Salter osteotomy Pubic osteotomy Ischial cut below ischial spine and at ischial tuberosity Less free rotation, increased risk of pseudarthrosis
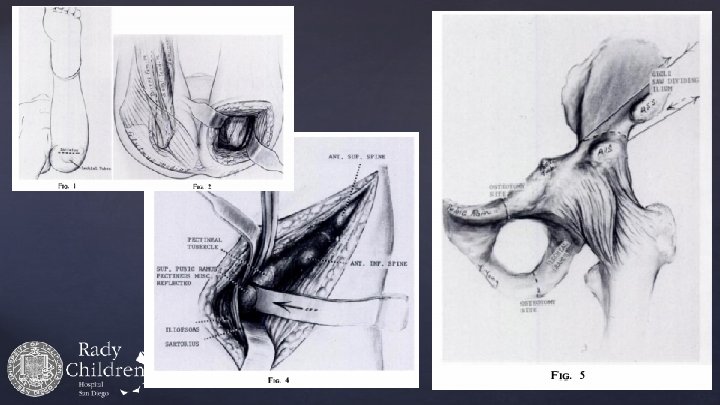
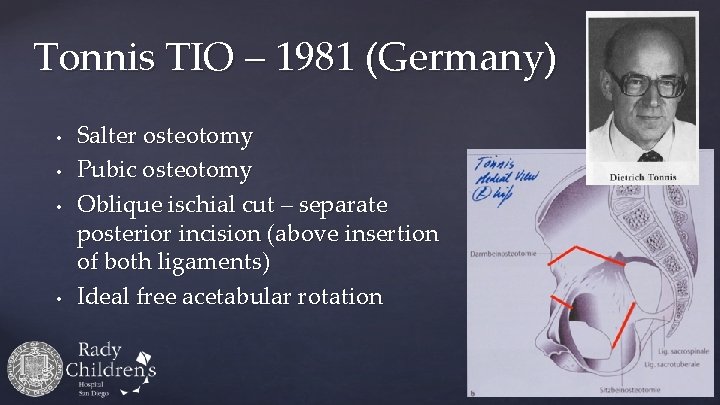
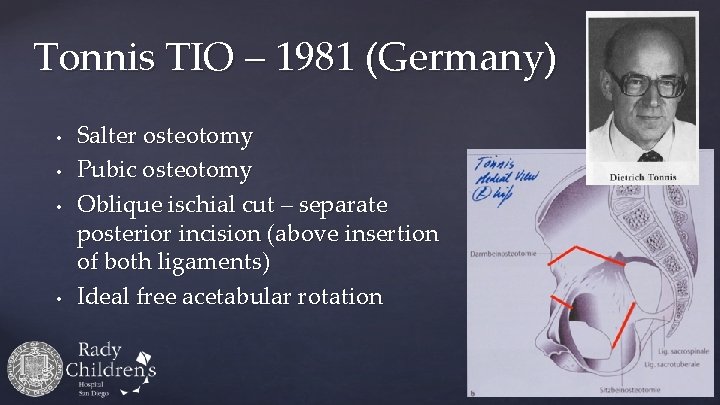
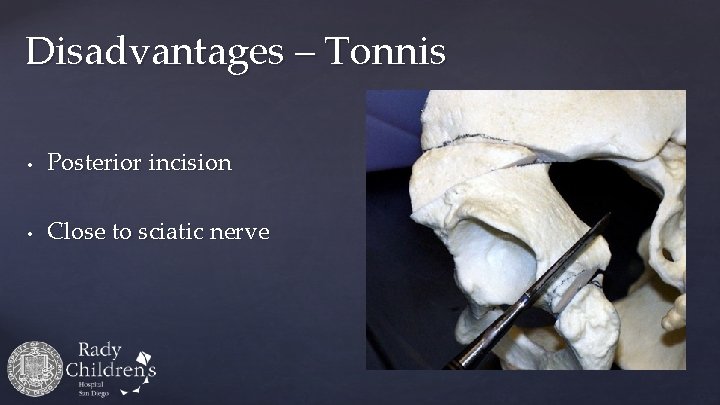
Tonnis TIO – 1981 (Germany) • • Salter osteotomy Pubic osteotomy Oblique ischial cut – separate posterior incision (above insertion of both ligaments) Ideal free acetabular rotation
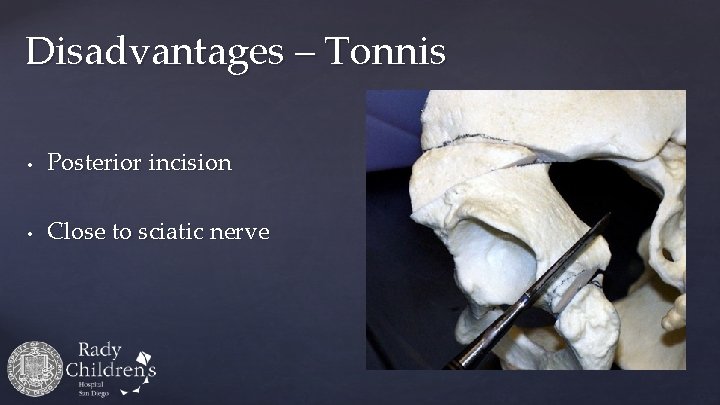
Disadvantages – Tonnis • Posterior incision • Close to sciatic nerve
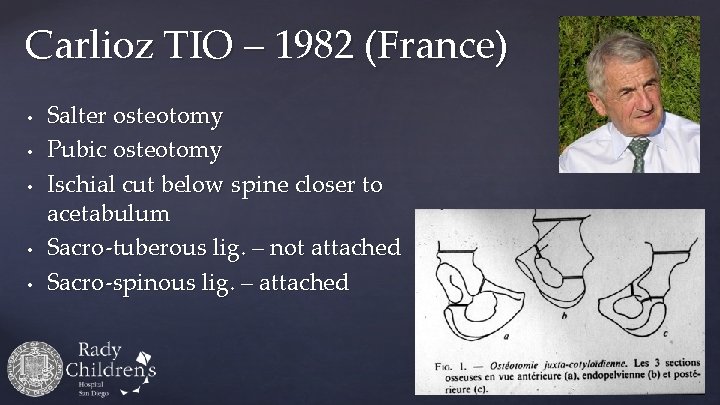
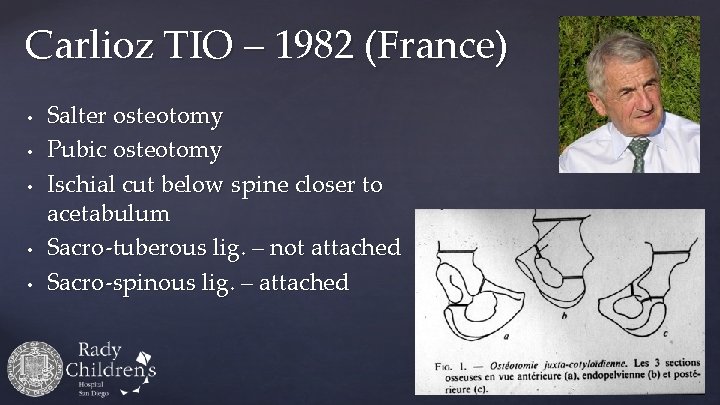
Carlioz TIO – 1982 (France) • • • Salter osteotomy Pubic osteotomy Ischial cut below spine closer to acetabulum Sacro-tuberous lig. – not attached Sacro-spinous lig. – attached

Video
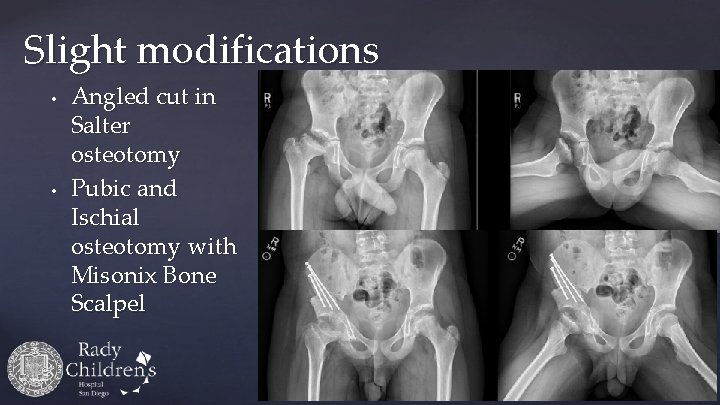
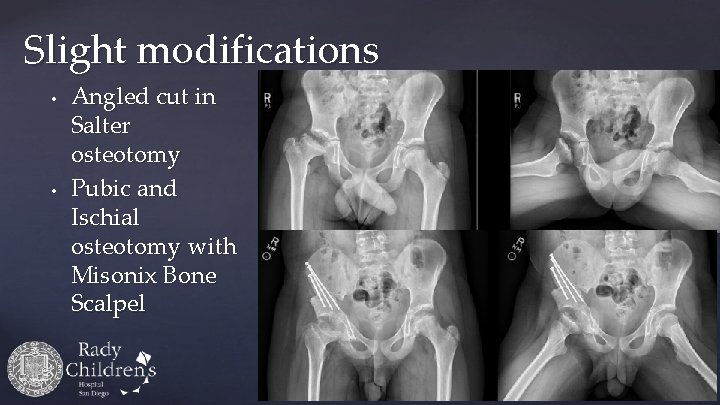
Slight modifications • • Angled cut in Salter osteotomy Pubic and Ischial osteotomy with Misonix Bone Scalpel

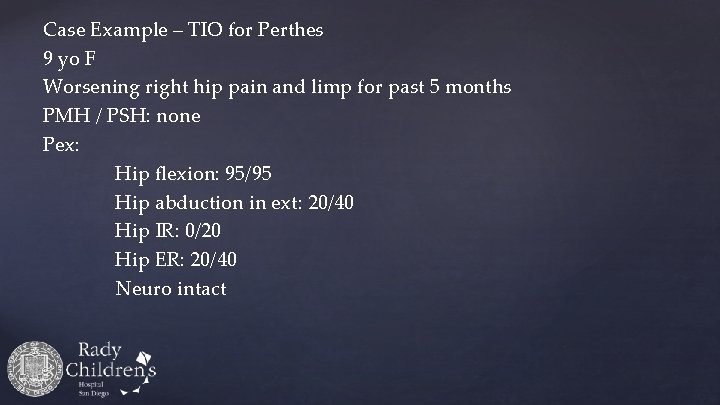
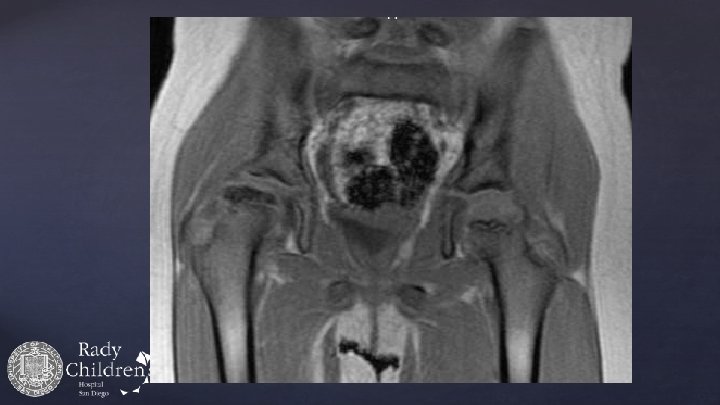
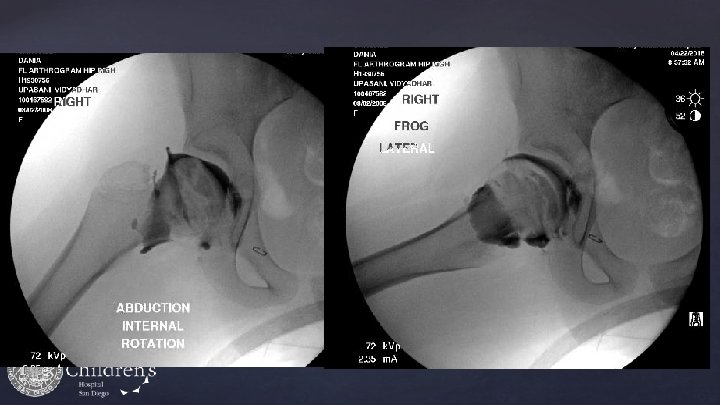
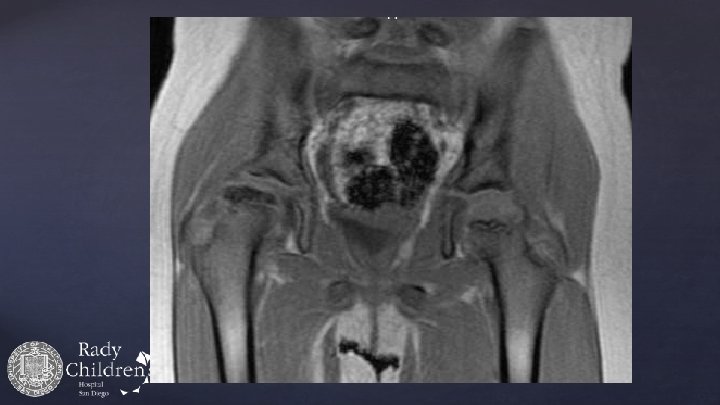
Case Example – TIO for Perthes 9 yo F Worsening right hip pain and limp for past 5 months PMH / PSH: none Pex: Hip flexion: 95/95 Hip abduction in ext: 20/40 Hip IR: 0/20 Hip ER: 20/40 Neuro intact

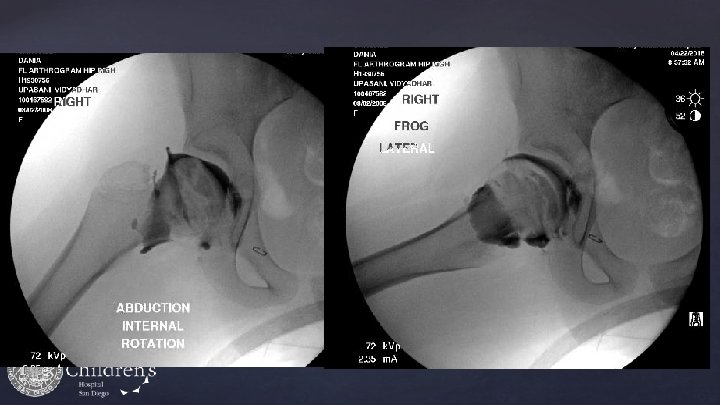

Post-op
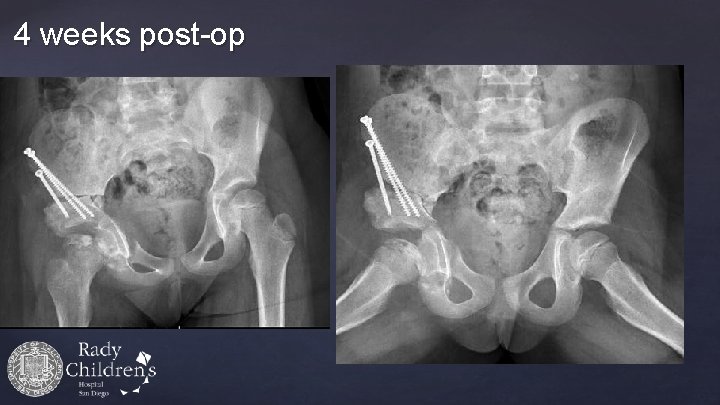
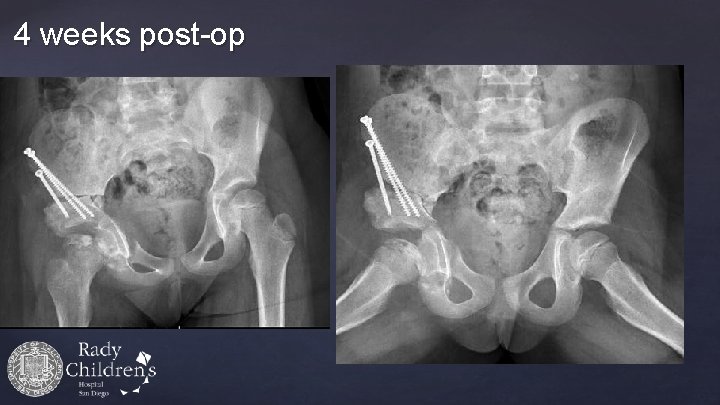
4 weeks post-op
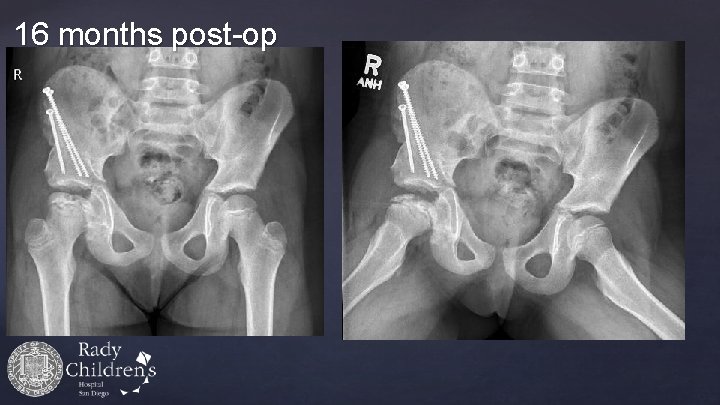
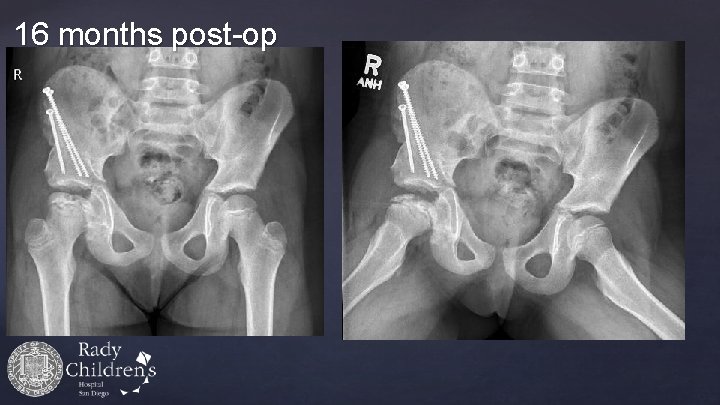
16 months post-op

Pre-op Post-op
Advanced Containment with the Triple Innominate Osteotomy for LCPD: Outcomes According to Age versus Disease Chronology Matthew Stepanovich, MD Vidyadhar V. Upasani, MD James D. Bomar, MPH Dennis R. Wenger, MD JPO 2015 Dec 17
Purpose • To evaluate the outcomes of triple innominate osteotomy (TIO) in Perthes disease • Based on disease chronology and severity • • Age Modified Elizabethtown – Joseph et al Catterall Lateral pillar – Herring et al
Methods • Retrospective chart and radiographic review 54 patients (56 hips) Inclusion: • All patients with LCPD treated with TIO • Single institution – 1995 -2011 • Minimum 2 -year follow-up Exclusion: Non LCP AVN / Concomitant femoral osteotomy • • •

Methods – Patient Classification • Disease chronology • • • Chronological age Modified Elizabethtown Disease severity • • Catterall Lateral Pillar
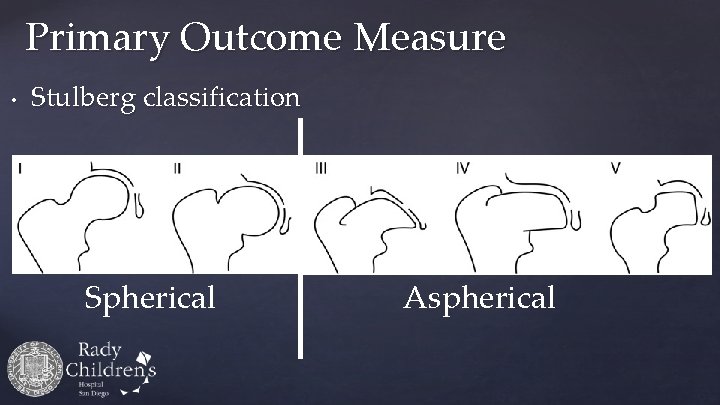
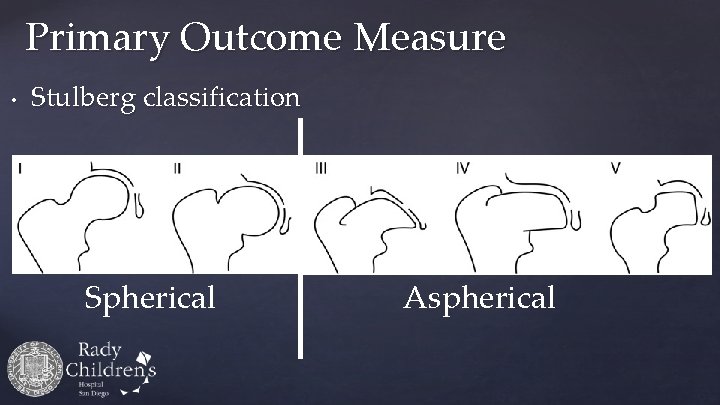
Primary Outcome Measure • Stulberg classification Spherical Aspherical
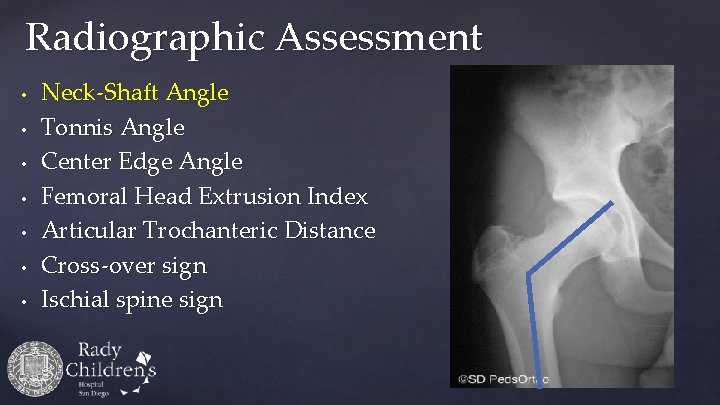
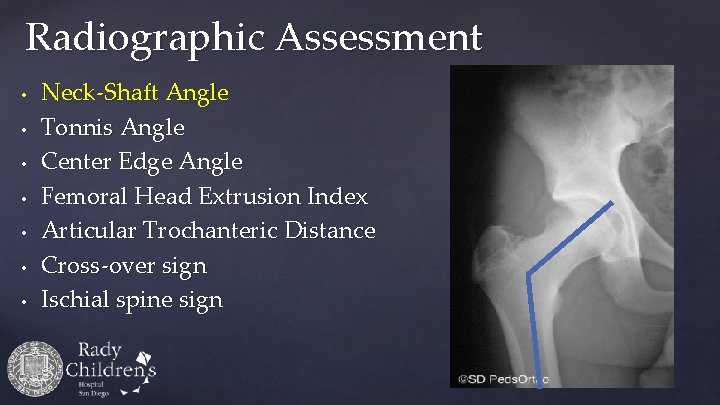
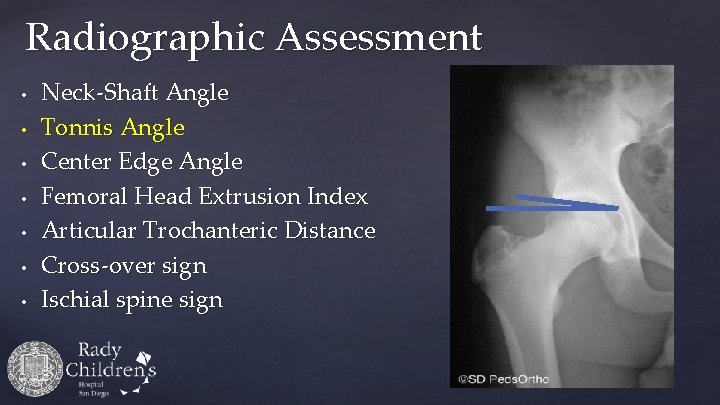
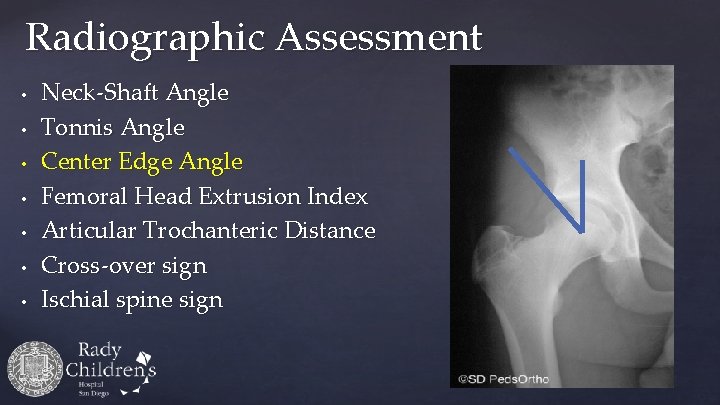
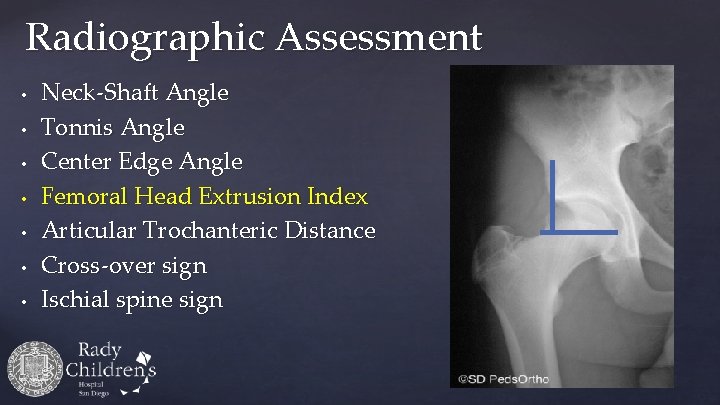
Radiographic Assessment • • Neck-Shaft Angle Tonnis Angle Center Edge Angle Femoral Head Extrusion Index Articular Trochanteric Distance Cross-over sign Ischial spine sign
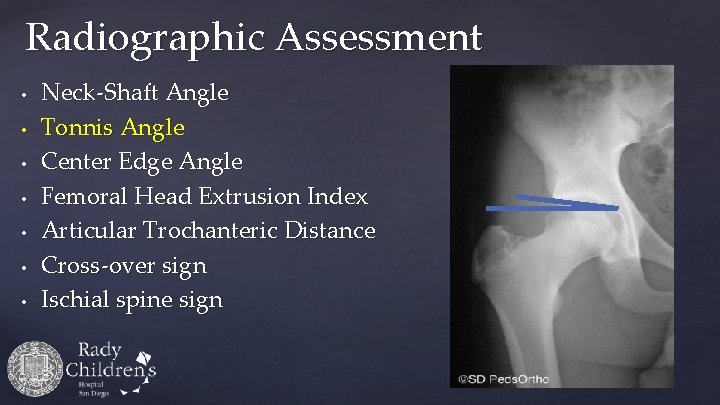
Radiographic Assessment • • Neck-Shaft Angle Tonnis Angle Center Edge Angle Femoral Head Extrusion Index Articular Trochanteric Distance Cross-over sign Ischial spine sign
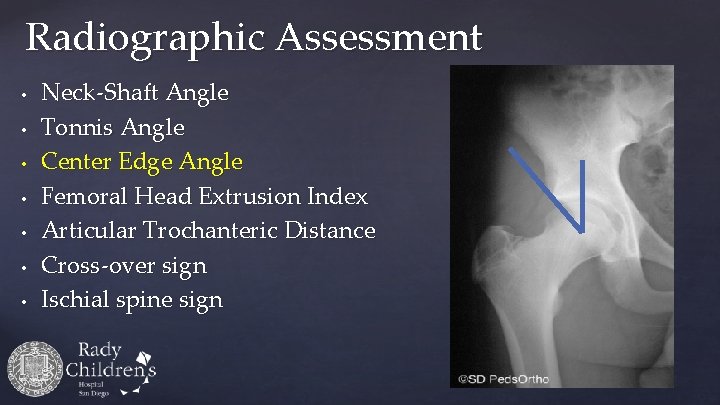
Radiographic Assessment • • Neck-Shaft Angle Tonnis Angle Center Edge Angle Femoral Head Extrusion Index Articular Trochanteric Distance Cross-over sign Ischial spine sign
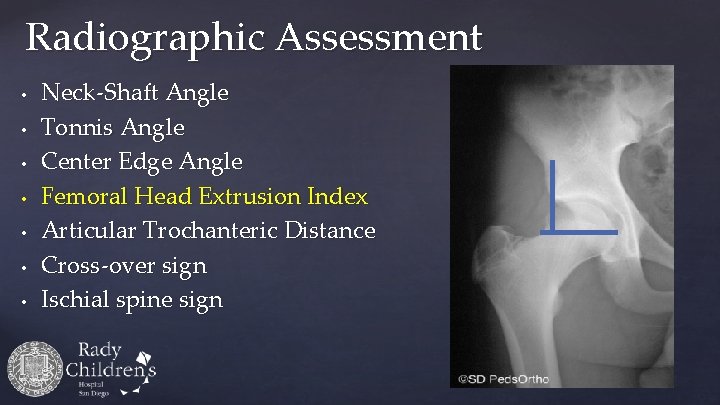
Radiographic Assessment • • Neck-Shaft Angle Tonnis Angle Center Edge Angle Femoral Head Extrusion Index Articular Trochanteric Distance Cross-over sign Ischial spine sign

Radiographic Assessment • • Neck-Shaft Angle Tonnis Angle Center Edge Angle Femoral Head Extrusion Index Articular Trochanteric Distance Cross-over sign Ischial spine sign

Radiographic Assessment • • Neck-Shaft Angle Tonnis Angle Center Edge Angle Femoral Head Extrusion Index Articular Trochanteric Distance Cross-over sign Ischial spine sign
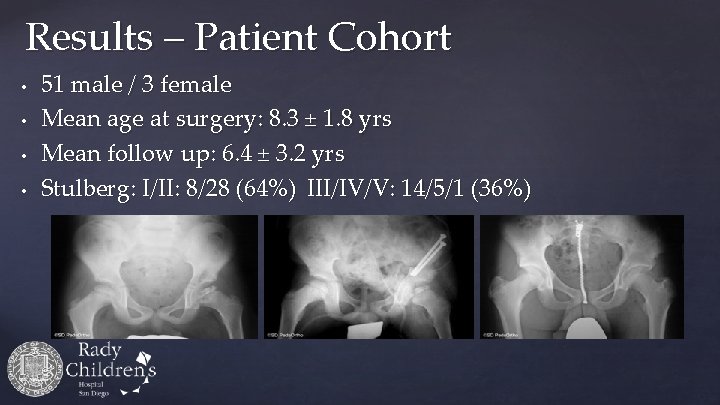
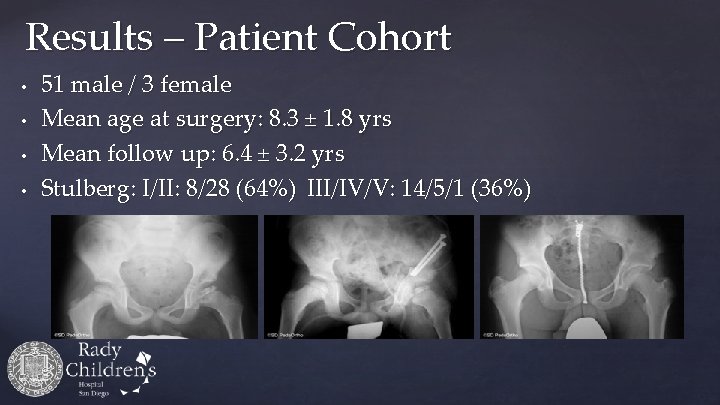
Results – Patient Cohort • • 51 male / 3 female Mean age at surgery: 8. 3 ± 1. 8 yrs Mean follow up: 6. 4 ± 3. 2 yrs Stulberg: I/II: 8/28 (64%) III/IV/V: 14/5/1 (36%)
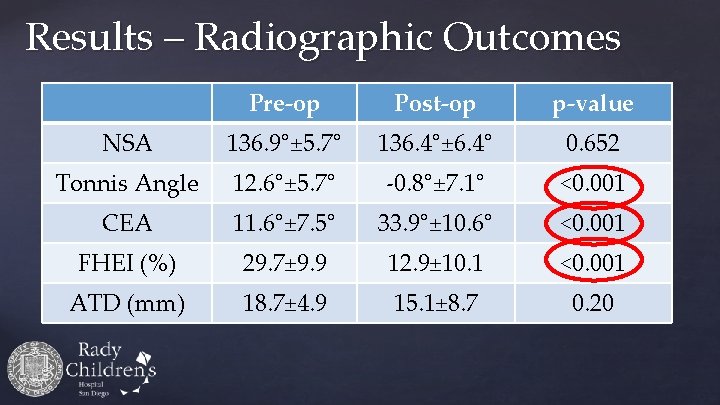
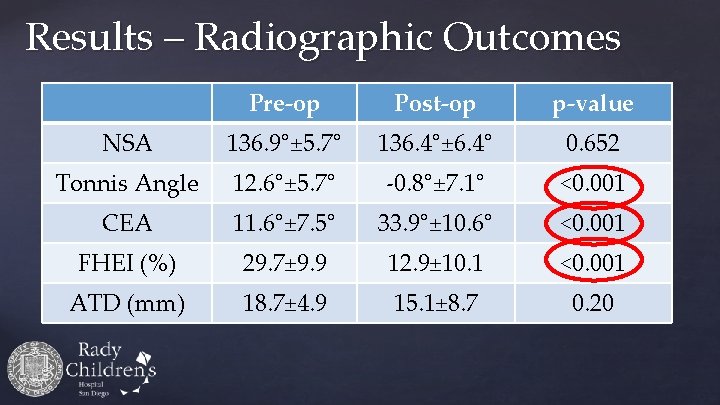
Results – Radiographic Outcomes Pre-op Post-op p-value NSA 136. 9°± 5. 7° 136. 4°± 6. 4° 0. 652 Tonnis Angle 12. 6°± 5. 7° -0. 8°± 7. 1° <0. 001 CEA 11. 6°± 7. 5° 33. 9°± 10. 6° <0. 001 FHEI (%) 29. 7± 9. 9 12. 9± 10. 1 <0. 001 ATD (mm) 18. 7± 4. 9 15. 1± 8. 7 0. 20

Results – Stulberg by Age
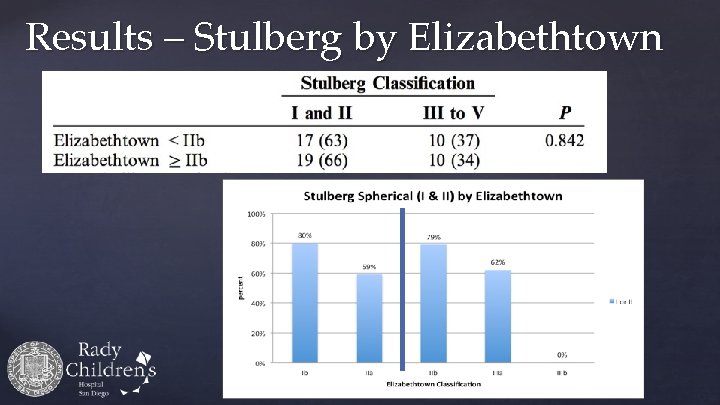
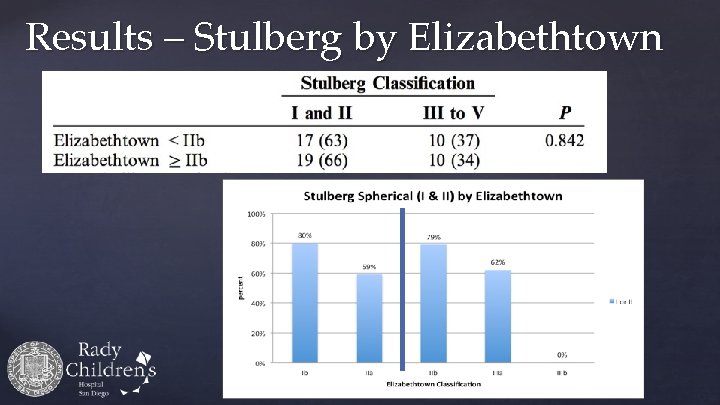
Results – Stulberg by Elizabethtown
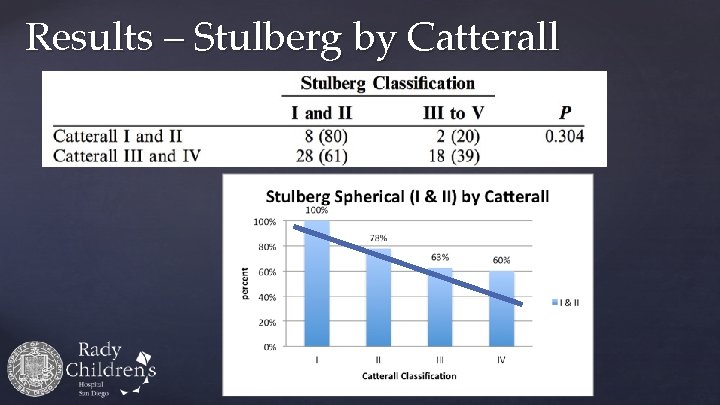
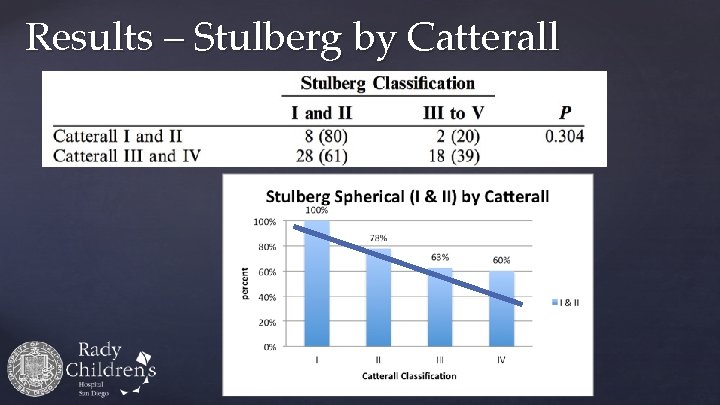
Results – Stulberg by Catterall
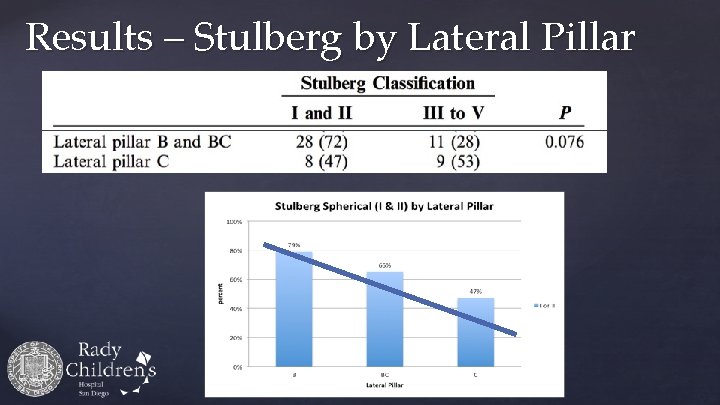
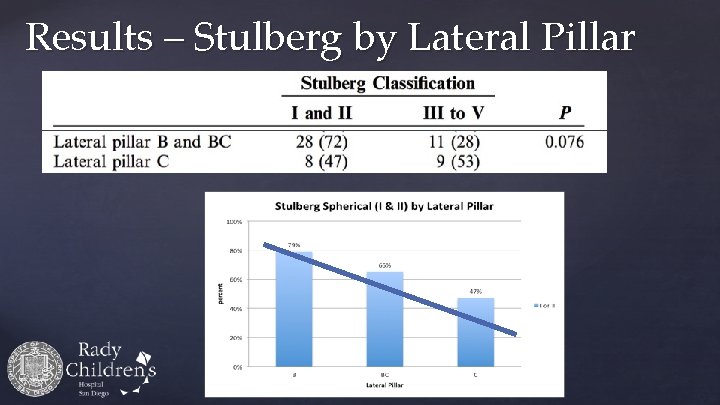
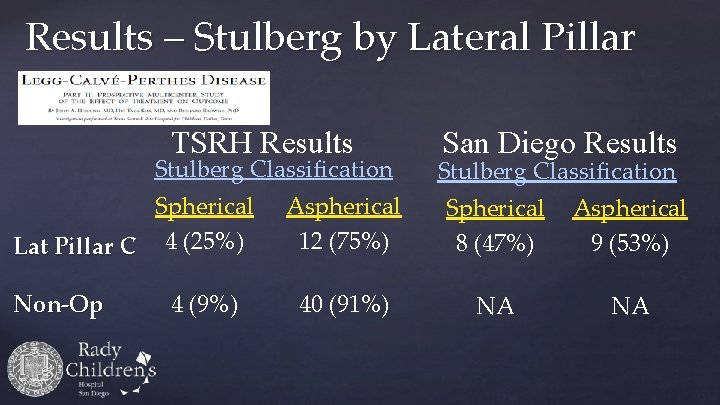
Results – Stulberg by Lateral Pillar
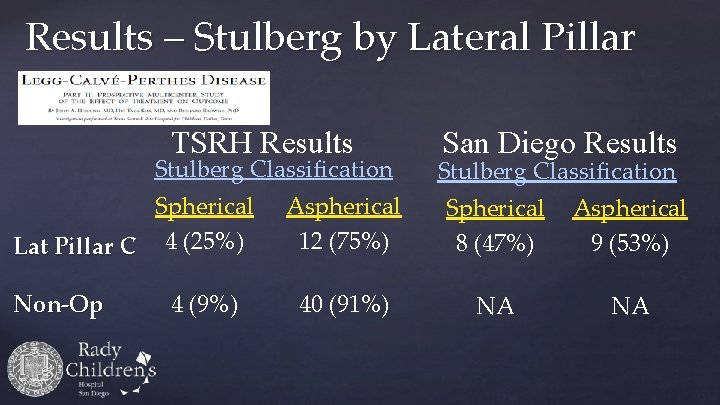
Results – Stulberg by Lateral Pillar TSRH Results Stulberg Classification Spherical Lat Pillar C 4 (25%) Non-Op 4 (9%) San Diego Results Stulberg Classification Aspherical 12 (75%) Spherical 8 (47%) Aspherical 9 (53%) 40 (91%) NA NA

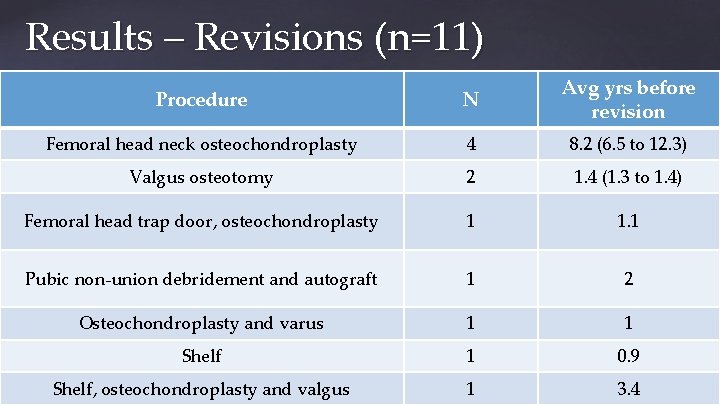
Results – Complications • • Impingement: 8 (14%) Undercoverage: 2 (4%) Non-union: 1 (2%) Revision surgery: 11 (20%)
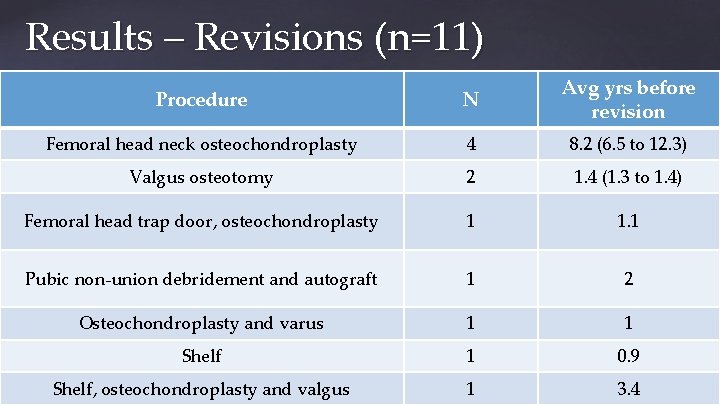
Results – Revisions (n=11) Procedure N Avg yrs before revision Femoral head neck osteochondroplasty 4 8. 2 (6. 5 to 12. 3) Valgus osteotomy 2 1. 4 (1. 3 to 1. 4) Femoral head trap door, osteochondroplasty 1 1. 1 Pubic non-union debridement and autograft 1 2 Osteochondroplasty and varus 1 1 Shelf 1 0. 9 Shelf, osteochondroplasty and valgus 1 3. 4
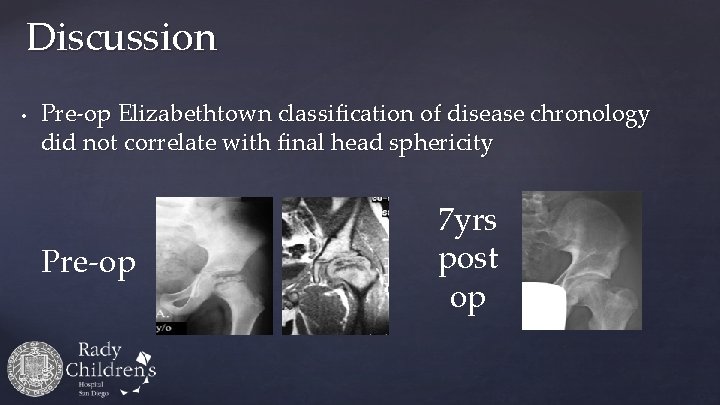
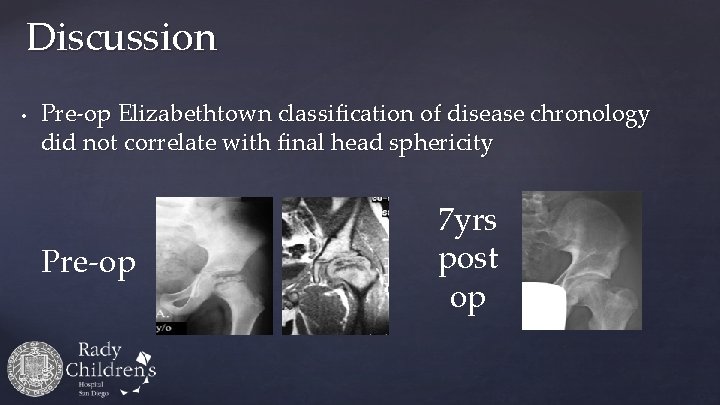
Discussion • Pre-op Elizabethtown classification of disease chronology did not correlate with final head sphericity Pre-op 7 yrs post op
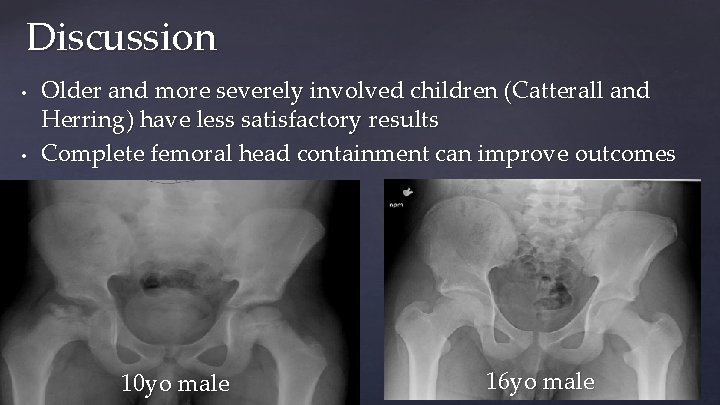
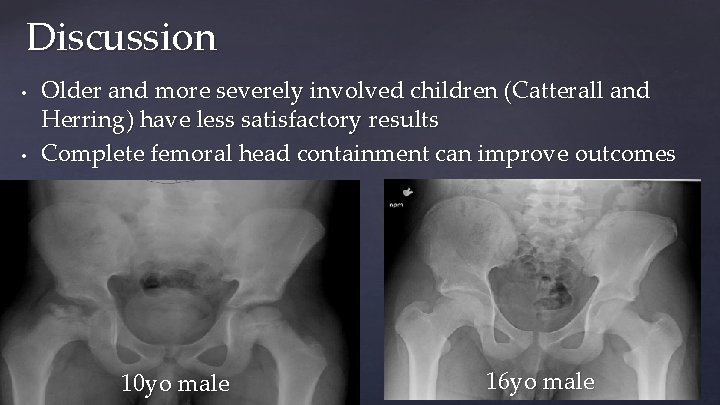
Discussion • • Older and more severely involved children (Catterall and Herring) have less satisfactory results Complete femoral head containment can improve outcomes 10 yo male 16 yo male
Discussion Perthes is a… May not respond to a…
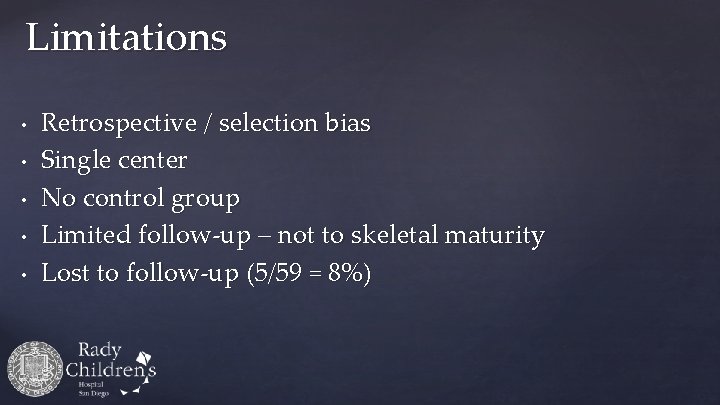
Limitations • • • Retrospective / selection bias Single center No control group Limited follow-up – not to skeletal maturity Lost to follow-up (5/59 = 8%)
Take Home Points • • Containment should still be considered for older and more severely affected Perthes patients Triple innominate osteotomy – viable technique Primary complication: over-containment (FAI) Future research: not just a mechanical solution
Thank You