Trench Foot CAUSES OF TRENCH FOOT v Prolonged









- Slides: 23
Trench Foot
CAUSES OF TRENCH FOOT v Prolonged exposure to damp, , cold conditions v Poor foot hygiene v Does Not require freezing temperatures v It can take less than a day of exposure for Trench Foot to develop
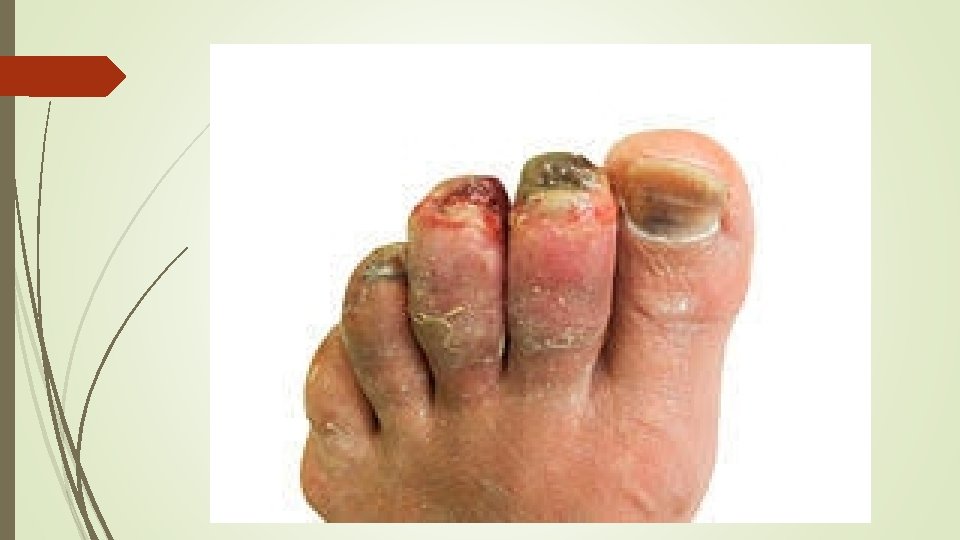
SYMPTOMS v Can affect any part of the foot v Cold, swollen, blotchy or white/grey color v Numbness, painful, prickly, or heavy feeling in foot v Tingling and/or itching sensation v The foot may be red, dry, and painful after it becomes warm v Blisters may form, followed by skin and tissue dying and falling off v In severe cases, untreated trench foot can involve the toes, heel, or entire foot



ADVANCED STAGE



TREATMENT v Thoroughly clean & dry the feet: Use an anti-bacterial, anti-fungal dressing and air the feet regularly v Gently re-warm feet to improve circulation: Warm the feed for approximately five minutes at a time either by soaking in warm (not hot) water or using heat packs. v Potassium permanganate foot bath: Can help draw fluid out of the affected area v Use dry, clean socks daily: Do Not wear socks while sleeping v Amputation: In severe cases where gangrene has set in, amputation is required v Seek medical treatment for advanced stages
Prevention v Wear clean, dry socks: Change socks frequently if in damp conditions v Use Polypropylene sock liners: draws moisture away from the feet v Don’t wear socks in bed: allow feet to “air” v Keep feet clean: wash and dry feet daily v Apply talcum powder or Vaseline: to keep moisture away v Ensure shoes fit well: avoid too loose or tight fitting shoes v Ensure footwear is dry: alternate footwear daily to ensure they are dry out fully; Avoid synthetic materials: e. g. rubber and vinyl v Control excessive perspiration: Use drying agents like aluminum chloride
FROSTBITE
CAUSES v. Wearing clothing not sutiable for the conditions v. Exposure to cold and wind for extended periods v. Risk increases as air temperature falls below 5 degrees F, even with low wind v. In wind chill of minus 16 F, Frostbite can occur on exposed skin in less than 30 minutes v. Touching materials such as ice, cold packs, or frozen metal
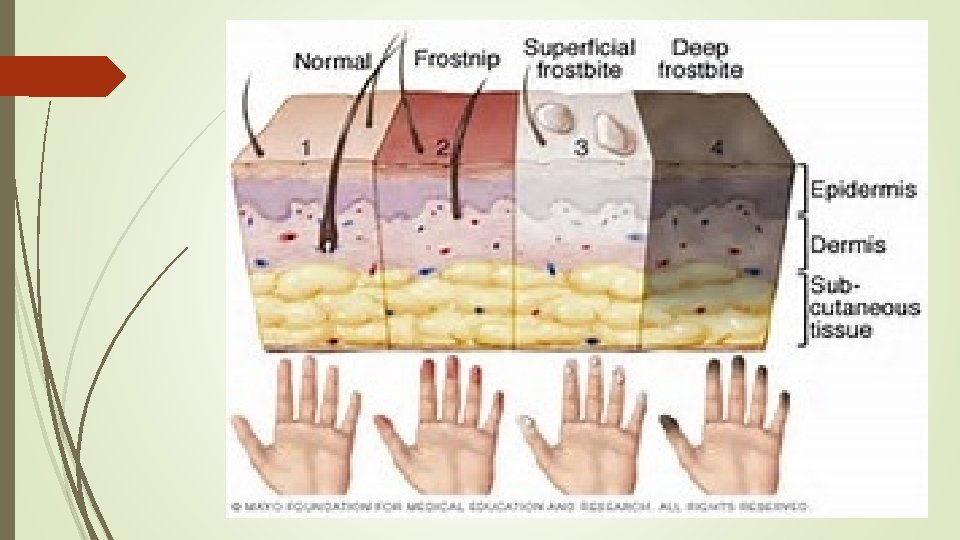
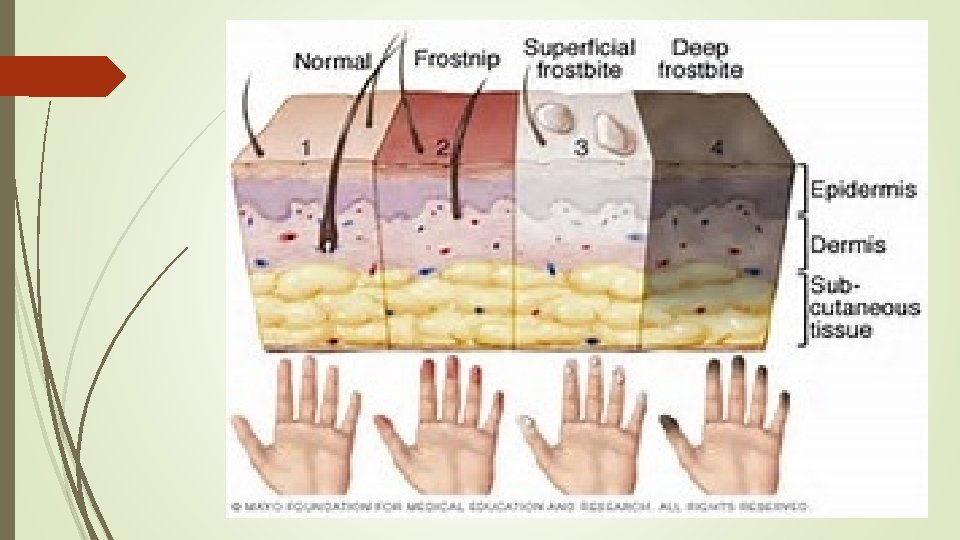
STAGE ONE v Frostnip – First Stage of frostbite Mild - Pale skin or red and feels very cold - Continued exposure leads to prickling and numbness - As the skin warms, may feel pain and tingling

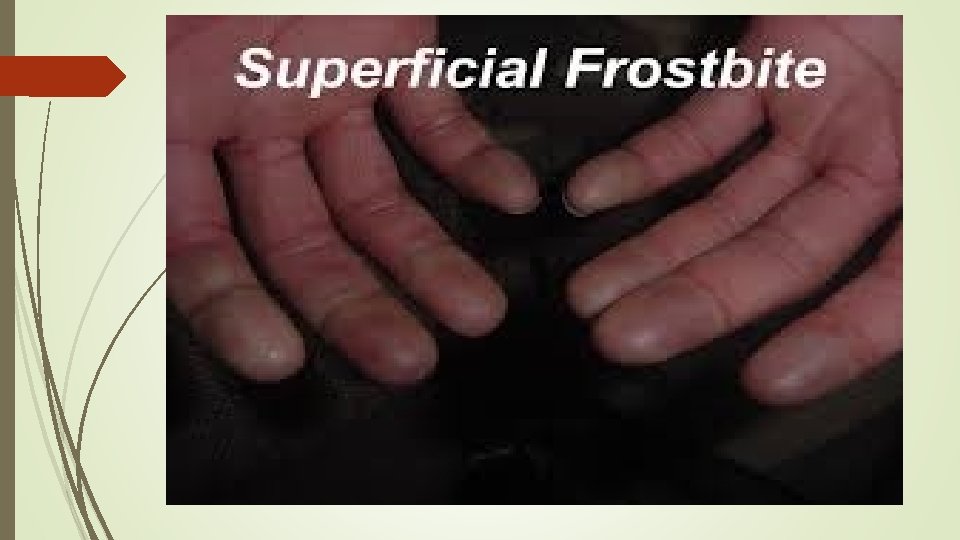
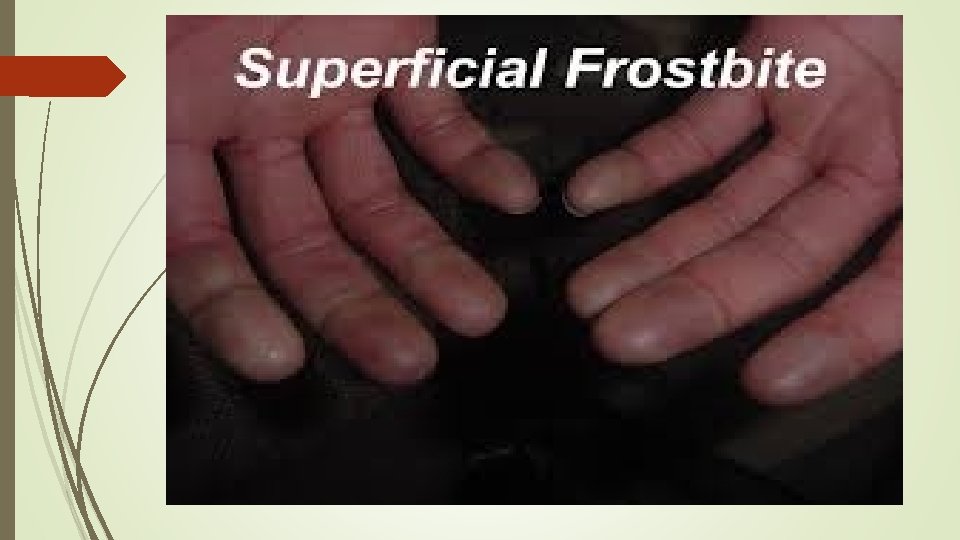
STAGE TWO v Superficial Frostbite - Reddened skin that turns white or pale - The skin may remain soft, but some ice crystals may form in the tissue - Skin may begin to feel warm—a sign of serious skin involvement - Rewarming at this stage, skin surface may appear mottled, blue, or purple - May notice stinging, burning, and swelling - Fluid-filled blister may appear 24 -36 hours after rewarming the skin
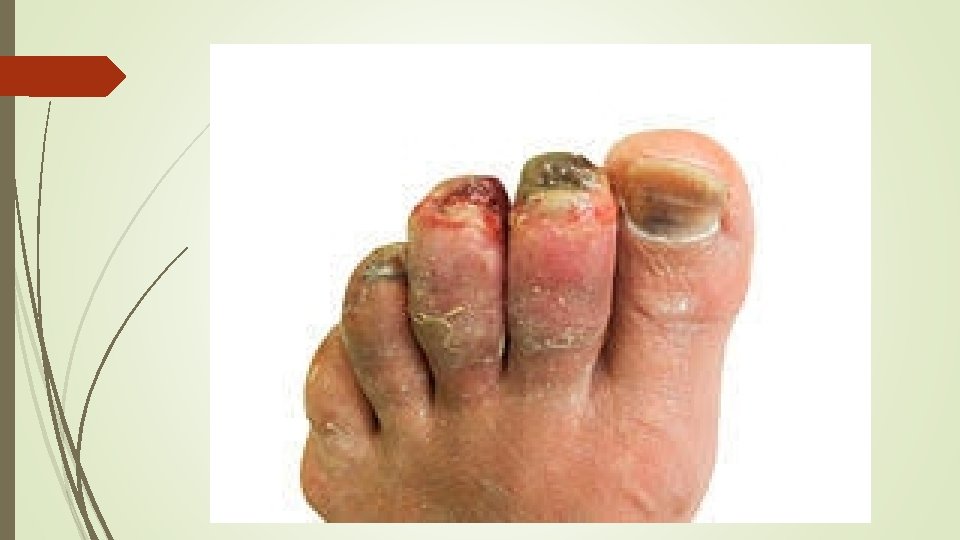
Frostbite v Severe (deep) frostbite - Affects all skin layers, and tissues below; no circulation to skin - Numbness - Losing all sensation of cold, pain, or discomfort - Joints or muscles may no longer work - Large blisters form in 24 -36 hours after rewarming - Followed by area turning black and hard as the tissue dies

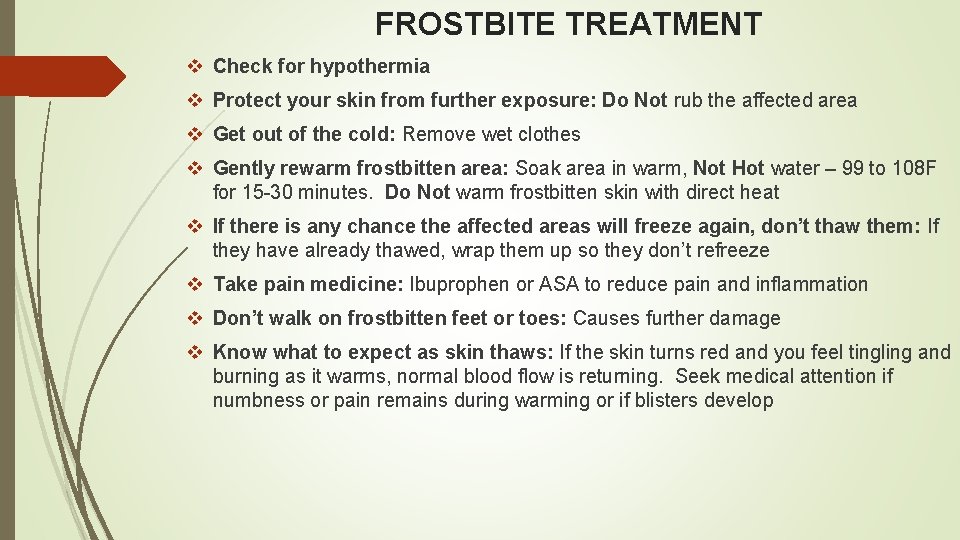
FROSTBITE TREATMENT v Check for hypothermia v Protect your skin from further exposure: Do Not rub the affected area v Get out of the cold: Remove wet clothes v Gently rewarm frostbitten area: Soak area in warm, Not Hot water – 99 to 108 F for 15 -30 minutes. Do Not warm frostbitten skin with direct heat v If there is any chance the affected areas will freeze again, don’t thaw them: If they have already thawed, wrap them up so they don’t refreeze v Take pain medicine: Ibuprophen or ASA to reduce pain and inflammation v Don’t walk on frostbitten feet or toes: Causes further damage v Know what to expect as skin thaws: If the skin turns red and you feel tingling and burning as it warms, normal blood flow is returning. Seek medical attention if numbness or pain remains during warming or if blisters develop

www. cc 27 bn. weebly. com