Treatment of Early Malignant Rectal Polyp Dr KP

- Slides: 39
Treatment of Early Malignant Rectal Polyp Dr KP Tsui Department of Surgery Tseung Kwan O Hospital
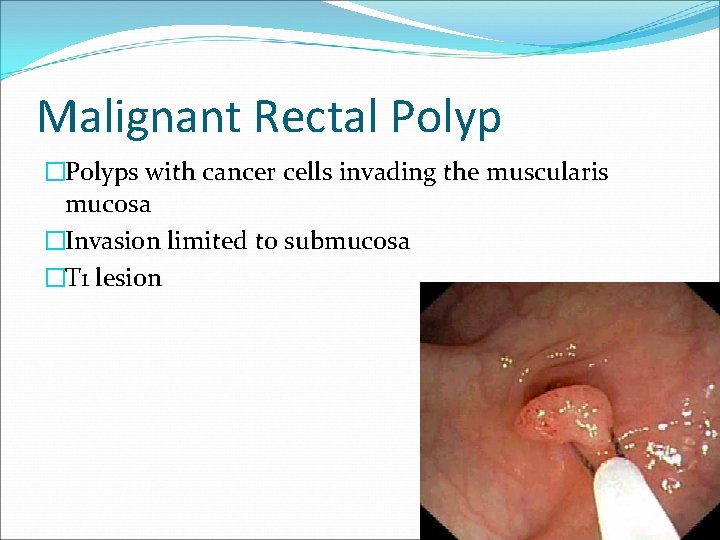
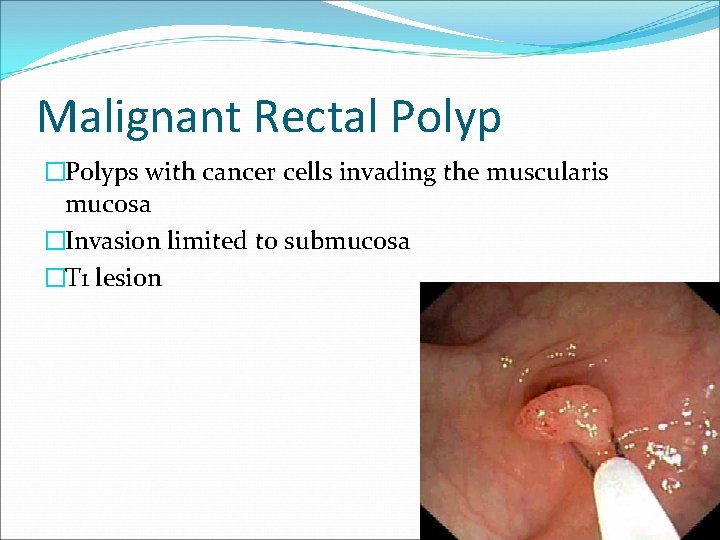
Malignant Rectal Polyp �Polyps with cancer cells invading the muscularis mucosa �Invasion limited to submucosa �T 1 lesion
�Incidence of malignant colorectal polyps as a proportion of all adenomas removed varies between 2. 6 and 9. 7%. �Average 4. 7% Sobin L, Wittekind C (eds). TNM classification of Malignant Tumours (6 th Edition). Wiler-Liss: New York, 2002.
�Size most important determinant factor determining risk of malignant transformation within a polyp �> 1 cm: 38. 5% �> 42 mm: 78. 9% Tytherleigh et al. BJS 2008; 95: 409 -423
�Villous adenomas have highest risk of malignancy at 29. 8% �Tubular adenomas have lowest at 3. 9% Tytherleigh et al. BJS 2008; 95: 409 -423
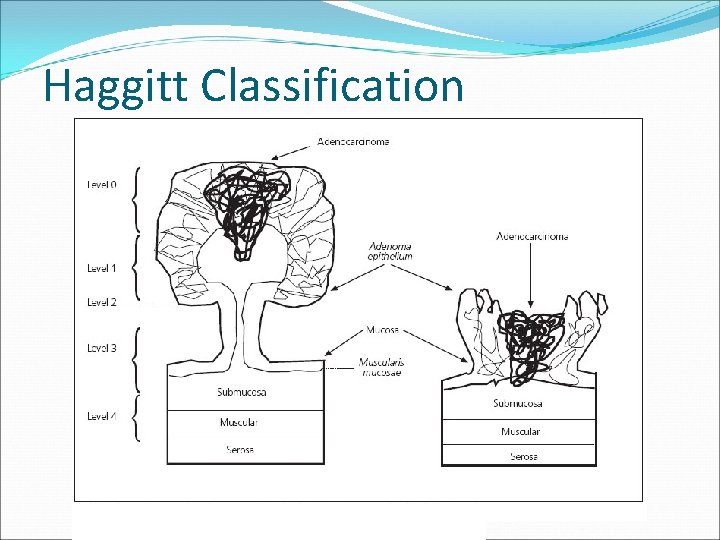
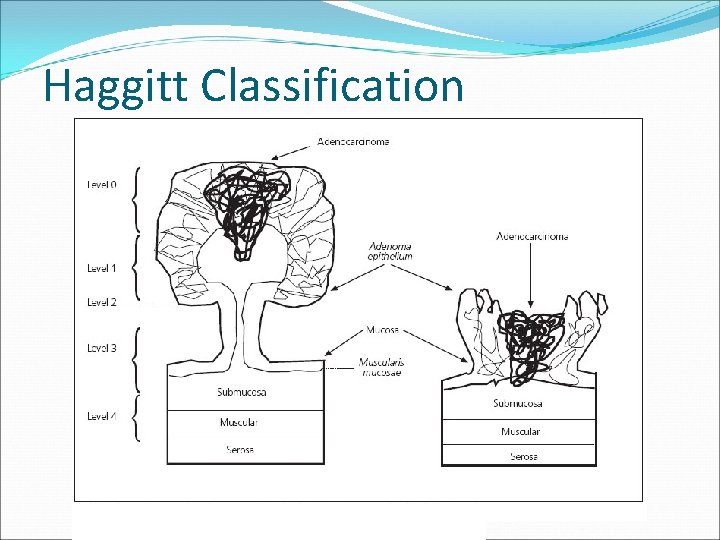
Haggitt Classification
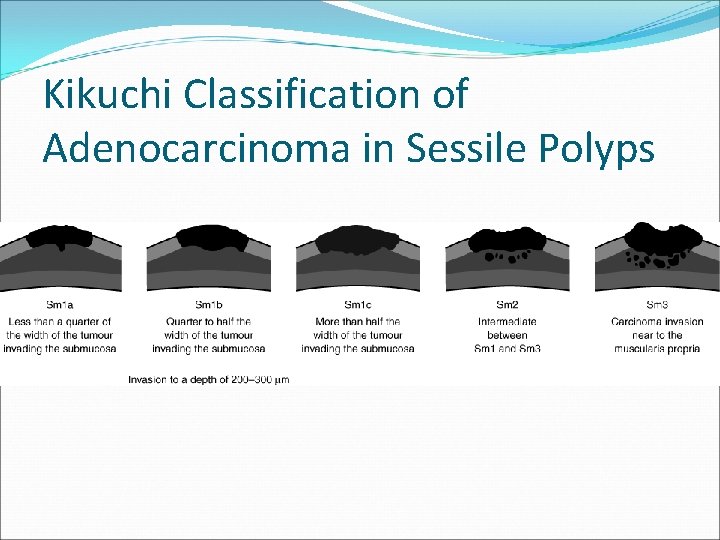
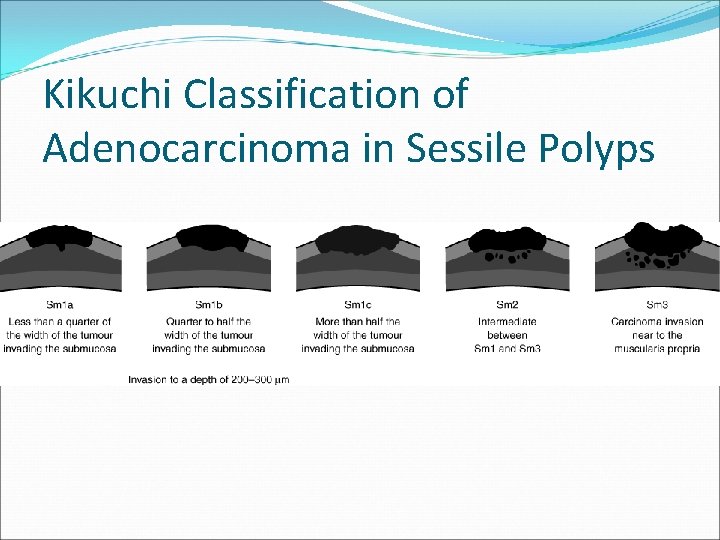
Kikuchi Classification of Adenocarcinoma in Sessile Polyps
Treatment �Staging �Histological Assessment
Clinical Scenario 1 Colonoscopy: 2 cm rectal polyp (5 cm from anal verge) Biopsy: adenocarcinoma
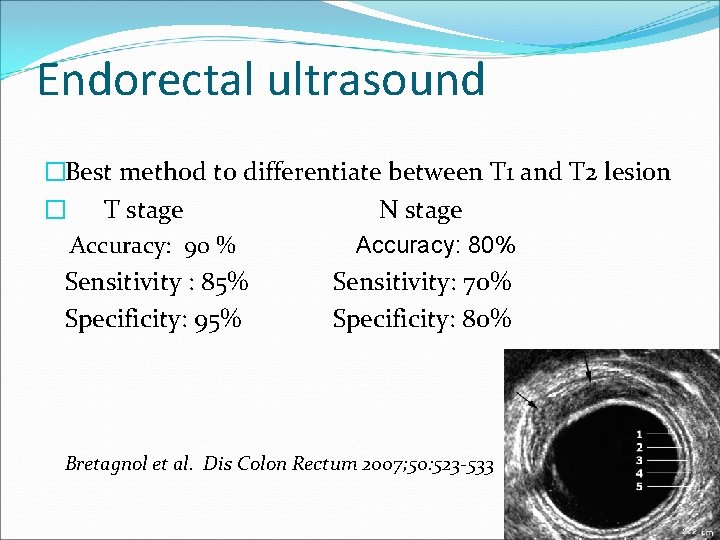
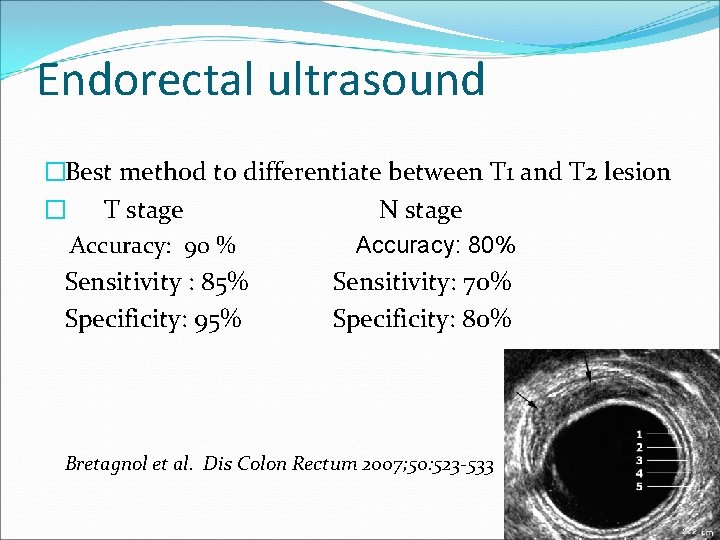
Endorectal ultrasound �Best method to differentiate between T 1 and T 2 lesion � T stage N stage Accuracy: 90 % Accuracy: 80% Sensitivity : 85% Sensitivity: 70% Specificity: 95% Specificity: 80% Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533
�Can assess residual tumor after polypectomy �Follow up after local excision Hernandez De Anda et al. Dis Colon Rectum 2004; 47: 818– 824
Limitations �Operator dependent �Upper rectal lesions �Tumor stenosis �Peritumoral fibrosis and inflammatory tissue �Effect of radiotherapy or hemorrhage after biopsy
Pelvic MRI �Overall T stage accuracy 59 -95% �T 1, 2 lesion (vs ERUS) - Similar sensitivities - Lower specificity (69%) �N stage - Comparable to EUS �Can evaluate entire pelvis Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533 Tytherleigh et al. BJS 2008; 95: 409 -423
CT abdomen + pelvis �Distant metastases �Low accuracy for T staging, 52 – 94% and N stage, 54 -70% Alexandre Jin Bok Audi Chang et al. Journal of Surgical Education; Vol 65: Number 1 Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533
PET �Limited role for local and regional staging �Sensitivities for lymph node metastases 22 -29% Abdel-Nabi H, Doerr RJ, Lamonica DM, et al. Radiology. 1998; 206: 755 -760
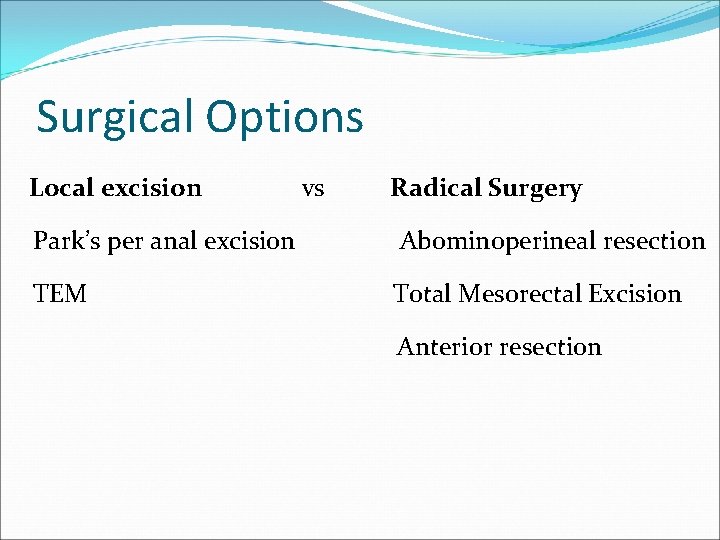
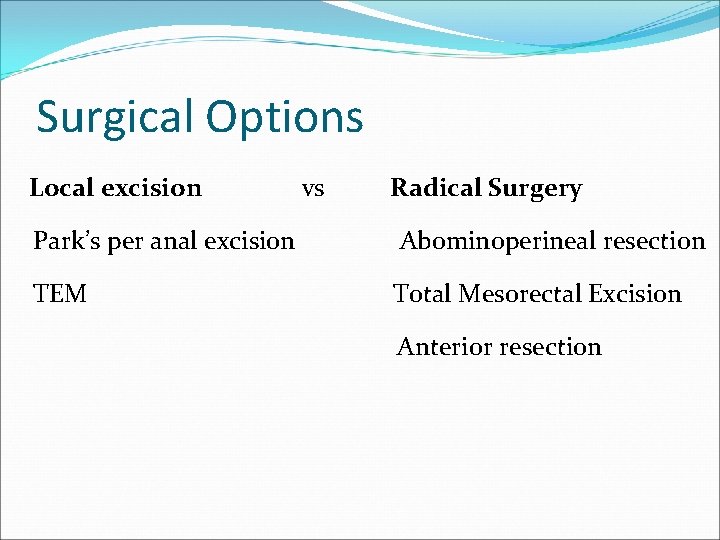
Surgical Options Local excision vs Radical Surgery Park’s per anal excision Abominoperineal resection TEM Total Mesorectal Excision Anterior resection
Local Excision �Opportunity of cure with less detriment �Sphincter preservation �Less morbidity and mortality �Less sexual or urinary dysfunction
Park’s per anal excision - Aid of anal retractors - 6 -10 cm of anal margin - Full thickness excision - At least 1 cm margin - Defect usually closed with absorbable sutures
Transanal endoscopic microsurgery �Rectoscope �Usually below peritoneal reflection �Full thickness excision �Excision margin of 1 cm �Difficult for lesions within 6 cm

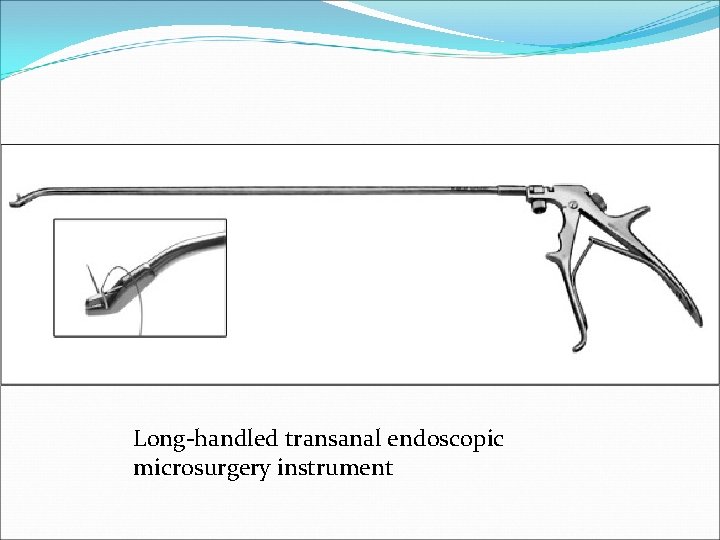
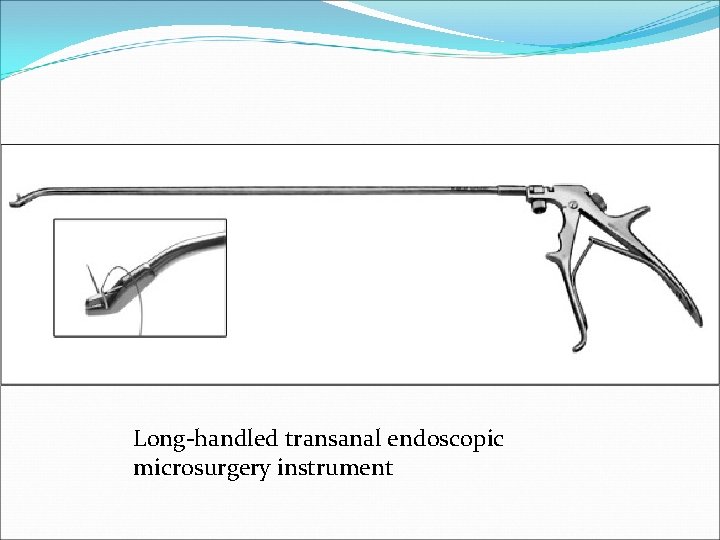
Long-handled transanal endoscopic microsurgery instrument
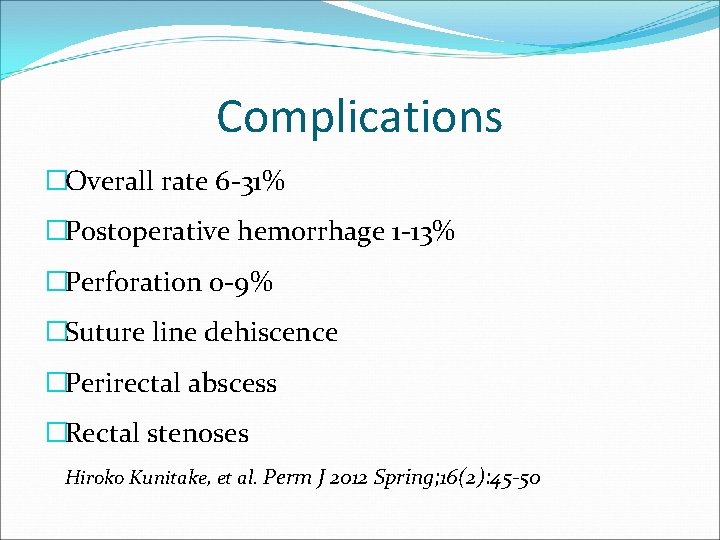
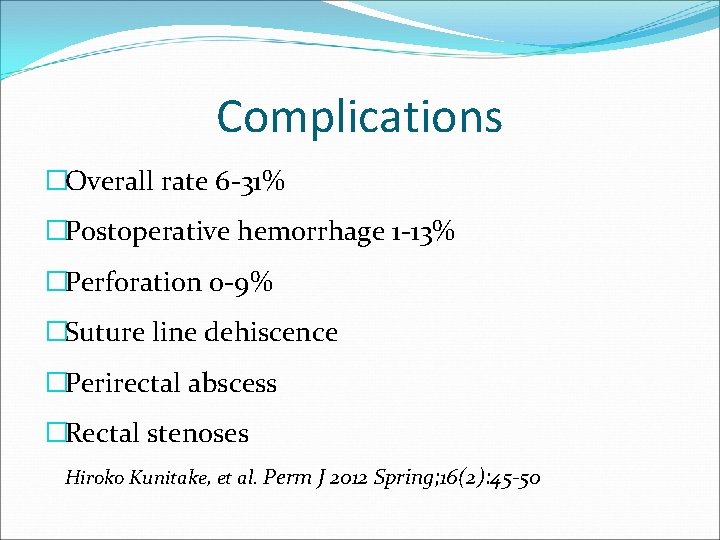
Complications �Overall rate 6 -31% �Postoperative hemorrhage 1 -13% �Perforation 0 -9% �Suture line dehiscence �Perirectal abscess �Rectal stenoses Hiroko Kunitake, et al. Perm J 2012 Spring; 16(2): 45 -50
Local Excision Vs Radical Surgery
�Generally accepted that local excision, by either endoscopic polypectomy or transanal surgery is adequate treatment for low risk ERC Tytherleigh et al. BJS 2008; 95: 409 -423
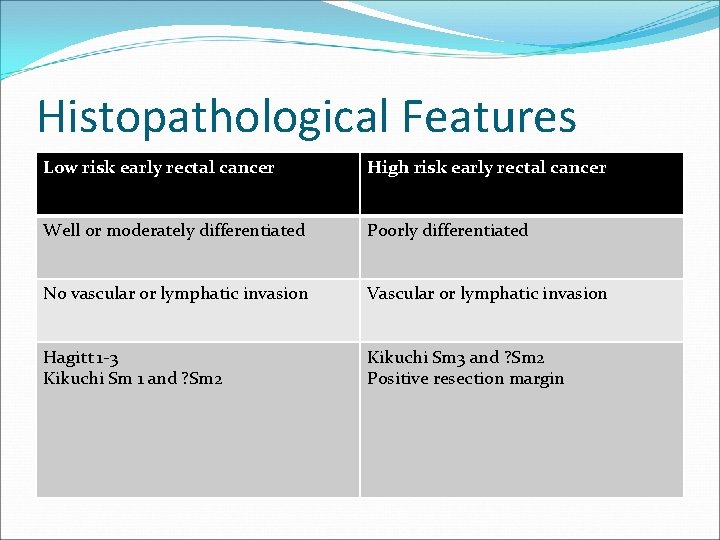
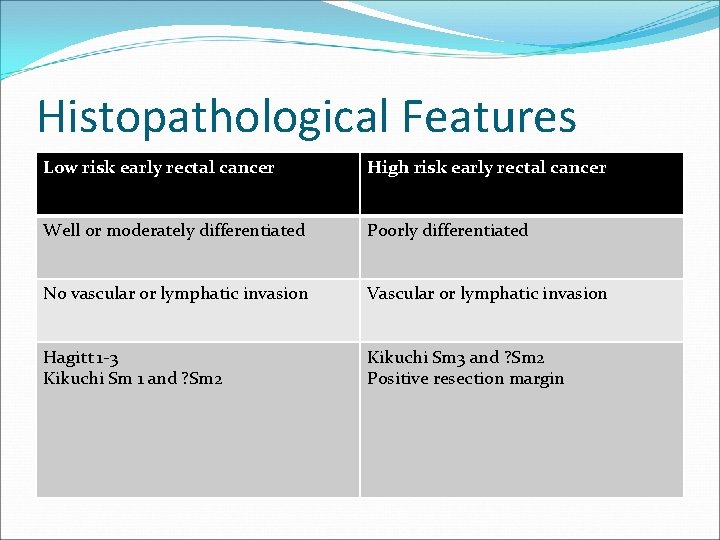
Histopathological Features Low risk early rectal cancer High risk early rectal cancer Well or moderately differentiated Poorly differentiated No vascular or lymphatic invasion Vascular or lymphatic invasion Hagitt 1 -3 Kikuchi Sm 1 and ? Sm 2 Kikuchi Sm 3 and ? Sm 2 Positive resection margin
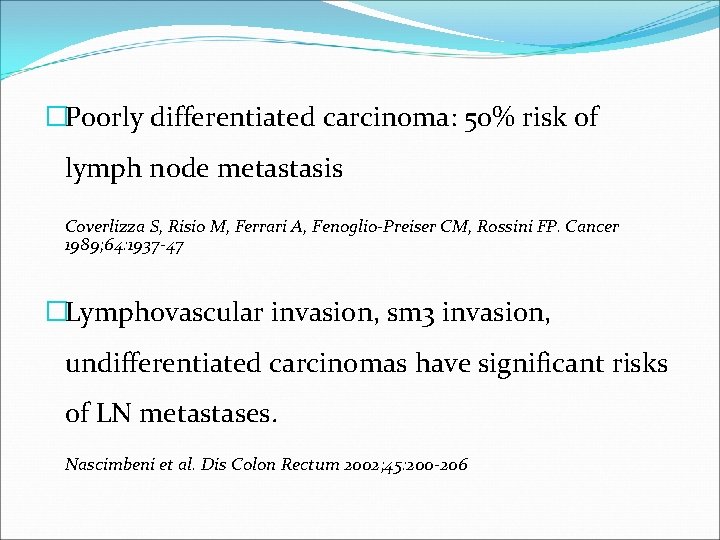
�Poorly differentiated carcinoma: 50% risk of lymph node metastasis Coverlizza S, Risio M, Ferrari A, Fenoglio-Preiser CM, Rossini FP. Cancer 1989; 64: 1937 -47 �Lymphovascular invasion, sm 3 invasion, undifferentiated carcinomas have significant risks of LN metastases. Nascimbeni et al. Dis Colon Rectum 2002; 45: 200 -206
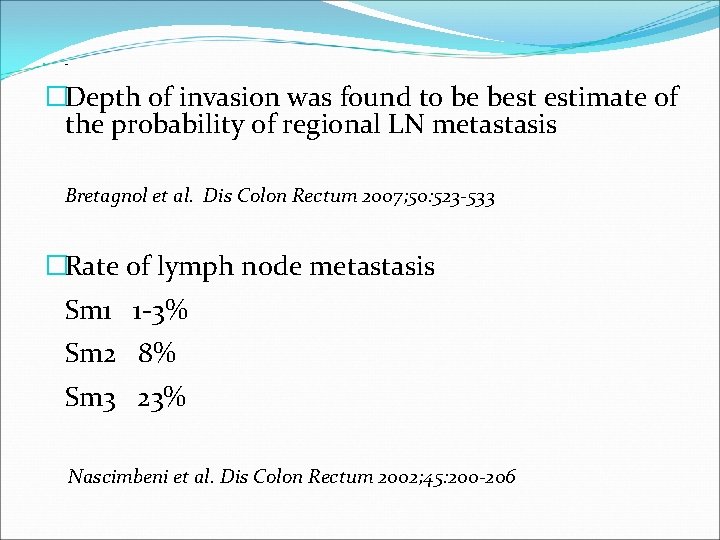
� Des. �Depth of invasion was found to be best estimate of the probability of regional LN metastasis Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533 �Rate of lymph node metastasis Sm 1 1 -3% Sm 2 8% Sm 3 23% Nascimbeni et al. Dis Colon Rectum 2002; 45: 200 -206
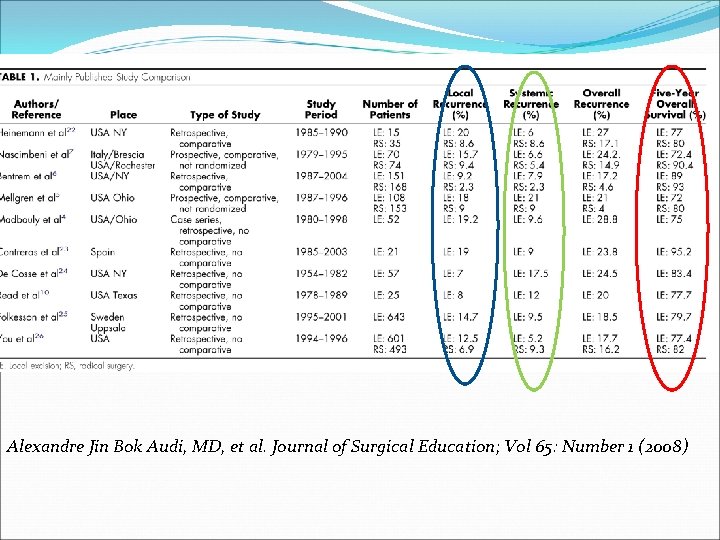
Optimal choice of surgery �The role of local excision as a curative procedure has been questioned due to inferior outcome in some long term follow up series. Alexandre Jin Bok Audi, MD, et al. Journal of Surgical Education; Vol 65: Number 1 (2008)
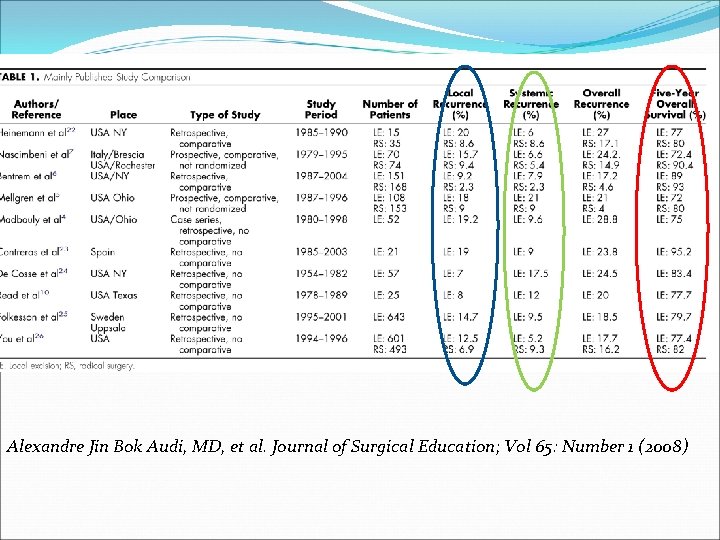
Alexandre Jin Bok Audi, MD, et al. Journal of Surgical Education; Vol 65: Number 1 (2008)
�Most literature data are based on case reports or small series with no standard criteria for patient selection
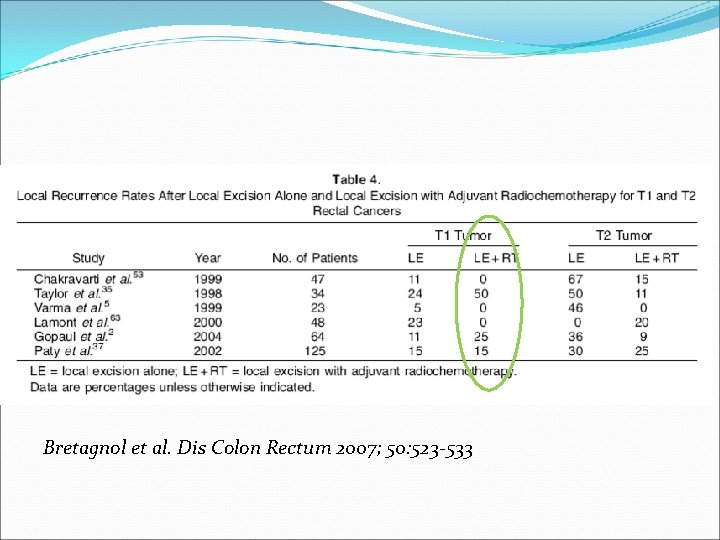
Adjuvant chemoradiotherapy �May be beneficial �Recommended for high risk T 1 lesions, assuming further surgery is not an option Tytherleigh et al. BJS 2008; 95: 409 -423
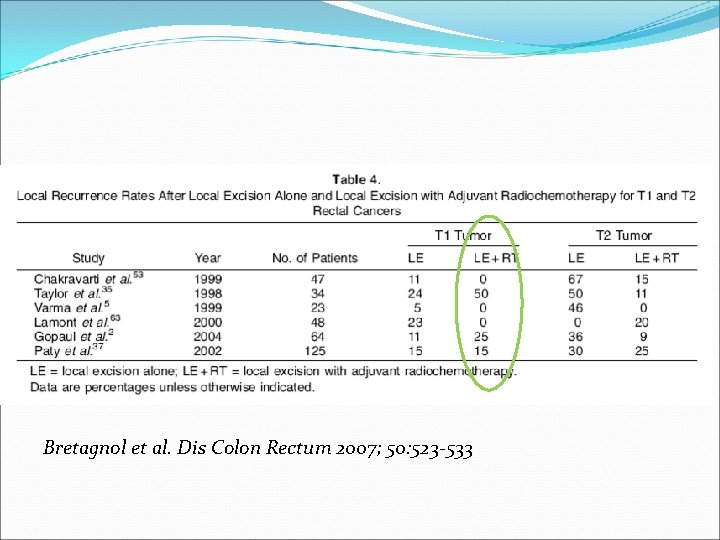
Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533
Limitations �Most retrospective studies �Lack of controlled data �No defined protocol for chemotherapy
Salvage surgery �Between 56 and 100% of recurrence suitable for salvage surgery �May not offer same outcomes as initial treatment �Should not be delayed in case of recurrence Tytherleigh et al. BJS 2008; 95: 409 -423
Clinical Scenario 2 �Colonoscopic polypectomy of rectal polyp �Pathology: adenocarcinoma
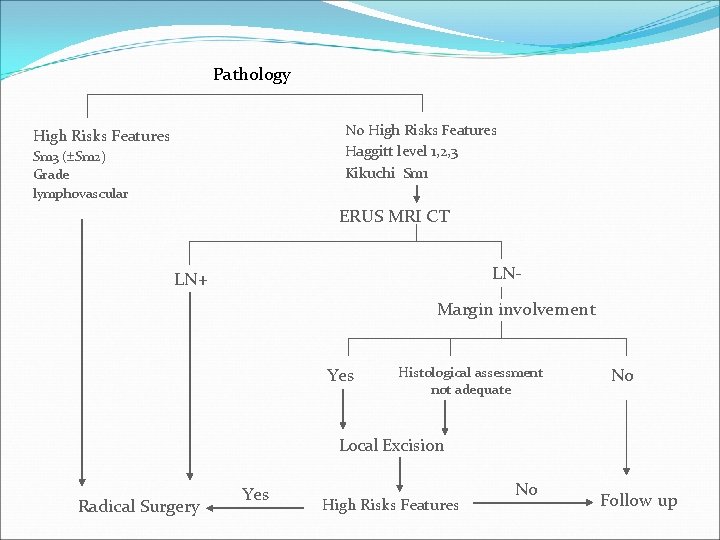
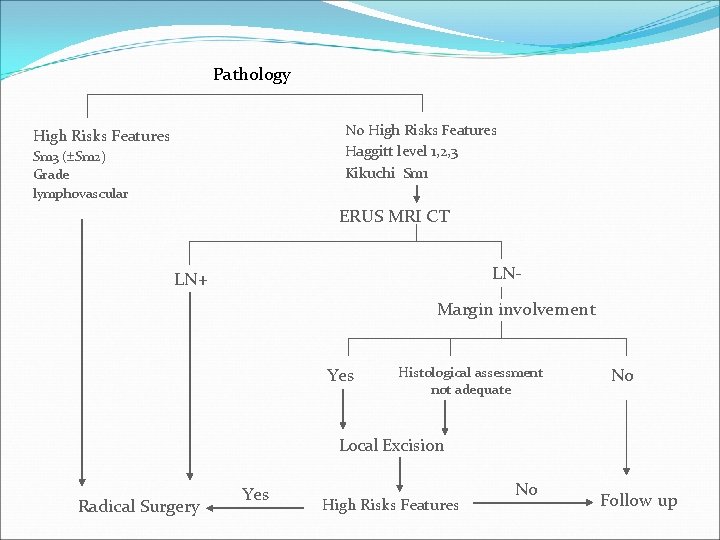
Pathology No High Risks Features Haggitt level 1, 2, 3 Kikuchi Sm 1 High Risks Features Sm 3 ( Sm 2) Grade lymphovascular ERUS MRI CT LN- LN+ Margin involvement Yes Histological assessment not adequate No Local Excision Radical Surgery Yes High Risks Features No Follow up
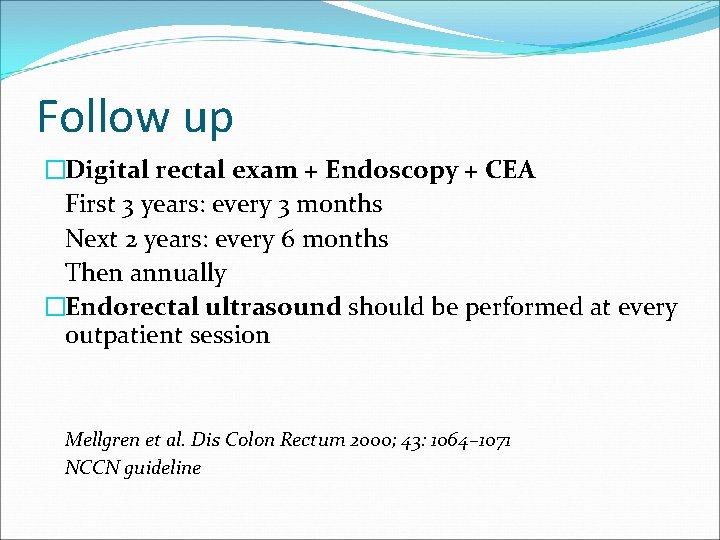
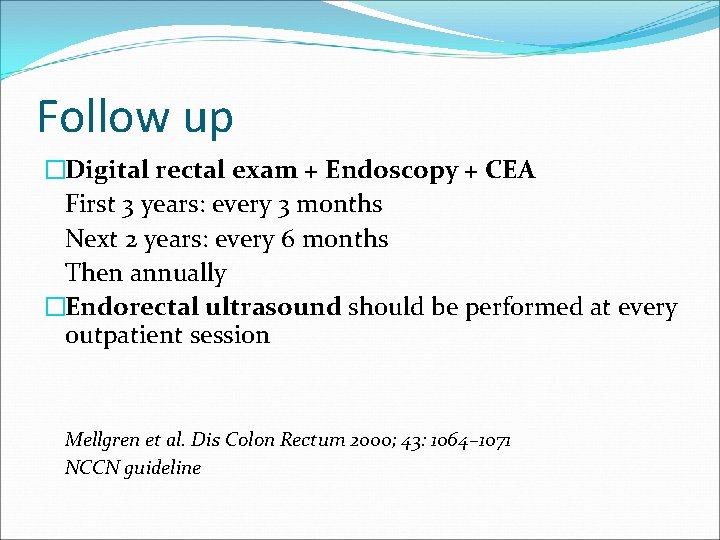
Follow up �Digital rectal exam + Endoscopy + CEA First 3 years: every 3 months Next 2 years: every 6 months Then annually �Endorectal ultrasound should be performed at every outpatient session Mellgren et al. Dis Colon Rectum 2000; 43: 1064– 1071 NCCN guideline
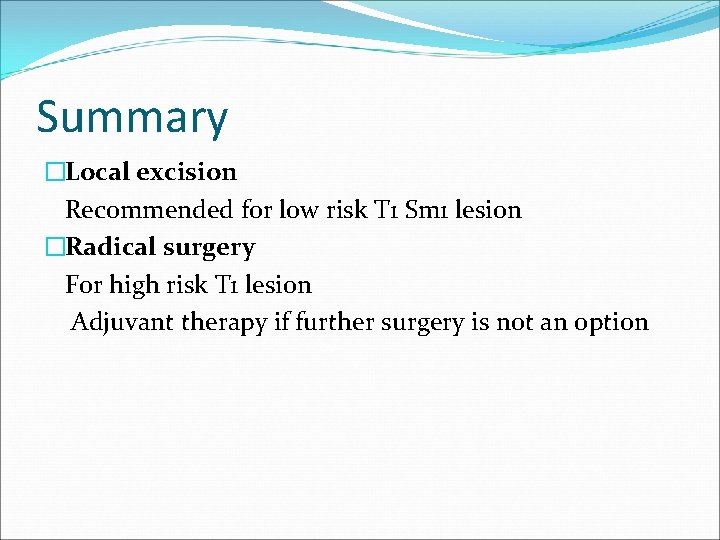
Summary �Local excision Recommended for low risk T 1 Sm 1 lesion �Radical surgery For high risk T 1 lesion Adjuvant therapy if further surgery is not an option
�Recurrence Diagnose early for salvage surgery �Follow up Endoscopic surveillance of rectum and scar