Treatment of AcneII Classification of Acne Grade of






- Slides: 39
Treatment of Acne-II
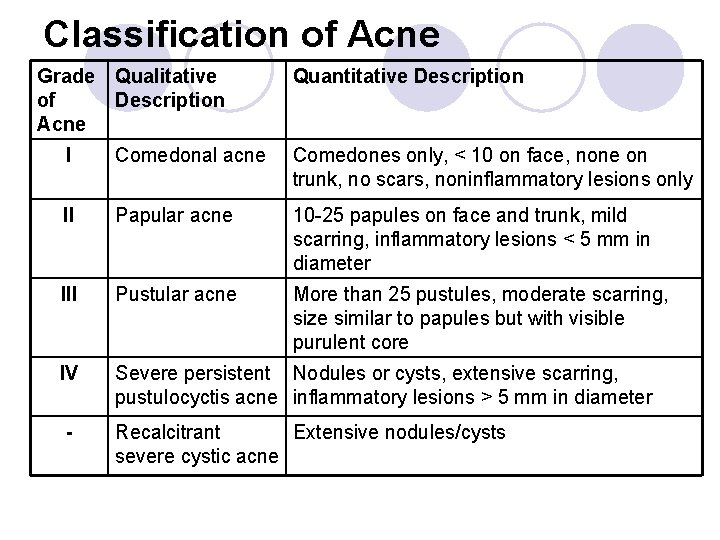
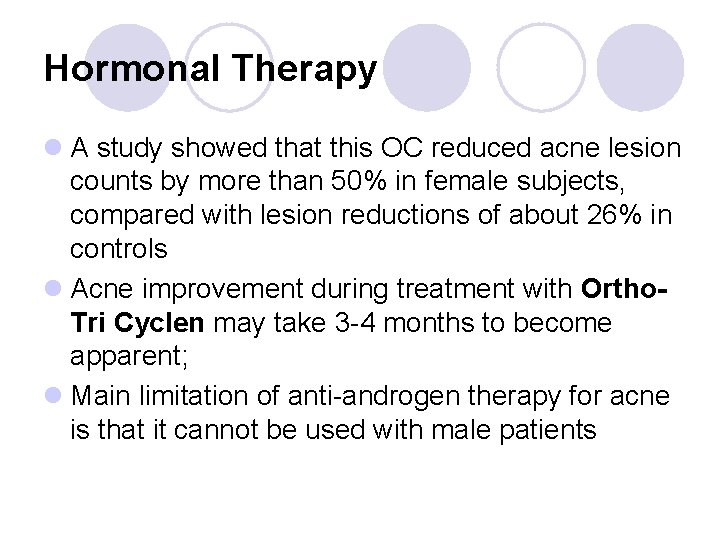
Classification of Acne Grade of Acne Qualitative Description Quantitative Description I Comedonal acne Comedones only, < 10 on face, none on trunk, no scars, noninflammatory lesions only II Papular acne 10 -25 papules on face and trunk, mild scarring, inflammatory lesions < 5 mm in diameter III Pustular acne More than 25 pustules, moderate scarring, size similar to papules but with visible purulent core IV Severe persistent Nodules or cysts, extensive scarring, pustulocyctis acne inflammatory lesions > 5 mm in diameter - Recalcitrant Extensive nodules/cysts severe cystic acne
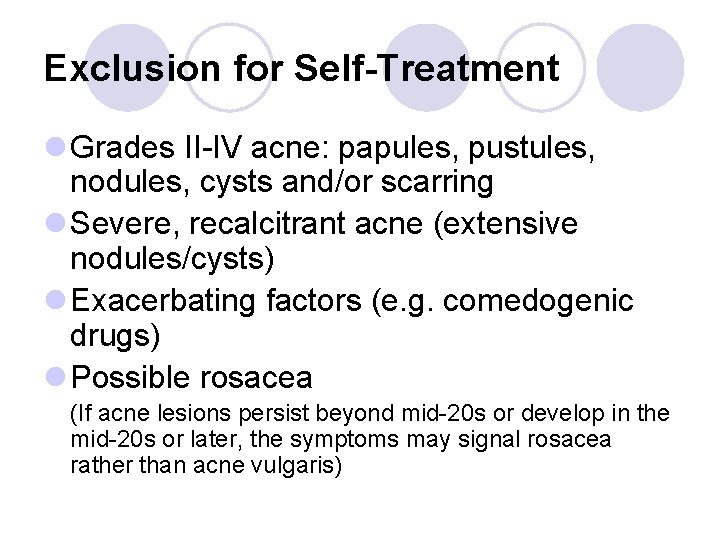
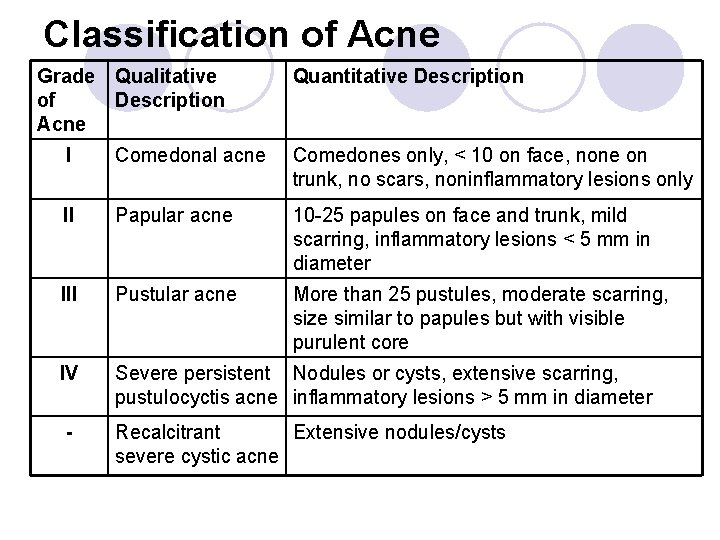
Exclusion for Self-Treatment l Grades II-IV acne: papules, pustules, nodules, cysts and/or scarring l Severe, recalcitrant acne (extensive nodules/cysts) l Exacerbating factors (e. g. comedogenic drugs) l Possible rosacea (If acne lesions persist beyond mid-20 s or develop in the mid-20 s or later, the symptoms may signal rosacea rather than acne vulgaris)

Pustular - an oral antibiotic would be best: Comedonal acne - topical treatment appropriate:

Severe acne treated with Isotretinoin: A) Before treatment: B) After 5 months
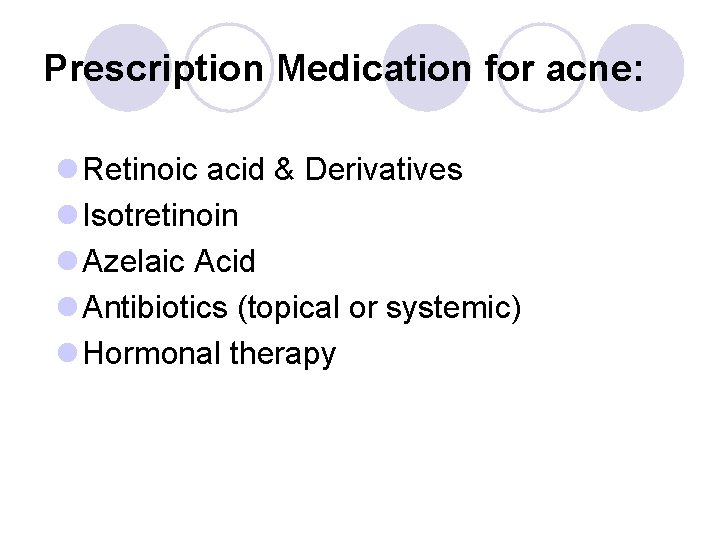
Prescription Medication for acne: l Retinoic acid & Derivatives l Isotretinoin l Azelaic Acid l Antibiotics (topical or systemic) l Hormonal therapy
Retinoic Acid & Derivatives l Retinoic acid (tretinoin) is the acid form of vitamin A l 13 -cis-retinoic acid (isotretinoin) is analog of retinoic acid effective when given orally l Retinoic acid insoluble in water; susceptible to oxidation and ester formation particularly when exposed to light; l Topically applied retinoic acid remains chiefly in the epidermis (< 10% absorbed)
Retinoic Acid & Derivatives l The small quantities absorbed following a topical application are metabolized by the liver and excreted in bile and urine; l Retinoic acid has several effects on epithelial tissues (lysosomes, PG-E 2, c. AMP, c. GMP and RNA polymerase) l Action in acne: (1) decreased cohesion between epidermal cells (2) increased epidermal cell turnover. l This results in expulsion of open comedones and transformation of closed comedones into open ones
Retinoic Acid & Derivatives l Retinoic acid is applied initially in a concentration sufficient to induce slight erythema with mild peeling l If too much irritaion is produced, decrease concentration or frequency of application; l During the first 4 -6 weeks of therapy, comedones not previously evident may appear l However, with continued therapy, the lesions will clear, and in 8 -12 weeks optimal clinical improvement should occur l (Retin-A Micro): timed release formulation with tretinoin containing microspheres. Less irritating

Retinoic Acid & Derivatives l Prolonged use of tretinoin promotes : (1) dermal collagen synthesis (2) new blood vessel formation (3) thickening of the epidermis Which helps diminish fine lines and wrinkles l Renova (0. 05% cream): specially formulated for this purpose
Retinoic Acid & Derivatives The most common adverse effects (topical): 1. erythema, dryness: first few weeks of use, but resolve with continued therapy; 2. May increase tumerogenic potential of UV radiation (in animals). Thus, patients are advised to minimize or avoid sun exposure and use protective sunscreen 3. Allergic contact dermatitis: rare

Retin-A dryness and irritation
Adapalene (Differin) l A derivative of naphathoic acid that resembles retinoic acid in structure and effects l Applied 0. 1% gel once daily l Unlike tretinoin: 1. photochemically stable 2. less irritating l Most effective: mild to moderate acne vulgaris

Treatment with Adpalene gel
Tazarotene (Tazorac) l Acetylenic retinoid l 0. 1% gel l Treatment of mild to moderately severe facial acne l Should not be used by pregnant women (pregnancy risk factor=X) l Contraceptive counseling in women of childbearing age.
Isotretinoin (Accutane) l A synthetic retinoid currently restricted to the treatment of severe cystic acne that is recalcitrant to standard therapies; l Well absorbed to circulation, extensively bound to plasma albumin, l elimination half-life of 21 hrs (parent drug), 21 -24 hrs (metabolite) l MOA: inhibits sebaceous gland size and function …. details
MOA- isotretenoin: l Isotretinoin prevents the formation of new comedos and resultant inflammatory lesions by: 1. decreasing the size and secretions of the sebaceous glands, 2. normalizing follicular keratinization, and 3. exerting anti-inflammatory effects. l Sebum production is reduced by at least 90% through competitive inhibition of retinol dehydrogenase-4, the enzyme that mediates the skin's production of dihydrotestosterone androstenedione.
Isotretinoin (Accutane) Dose: l 0. 5 -2 mg/kg/day, given orally in two divided doses daily for 4 -5 months; l If severe cystic acne persists following this initial treatment, a second course of therapy may be initiated after 2 months; l The skin would be sensitive during treatment. Patient is at high risk for abnormal healing and development of excessive granulation following procedures (e. g. piercing, tatoos, epilation)
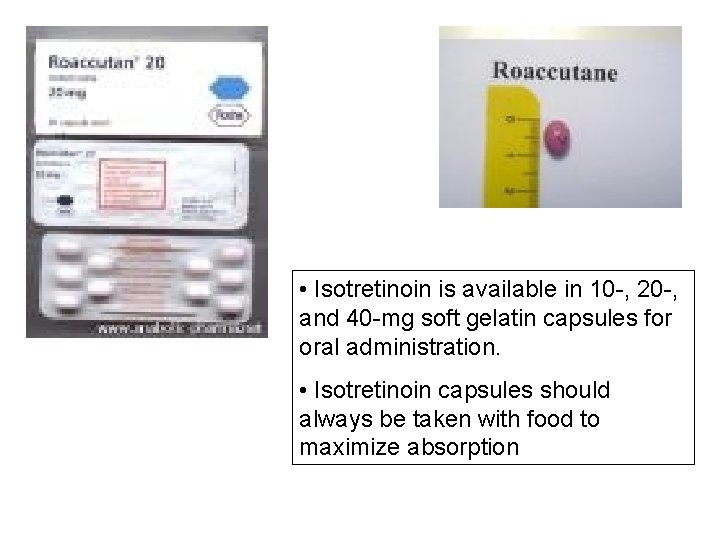
• Isotretinoin is available in 10 -, 20 -, and 40 -mg soft gelatin capsules for oral administration. • Isotretinoin capsules should always be taken with food to maximize absorption
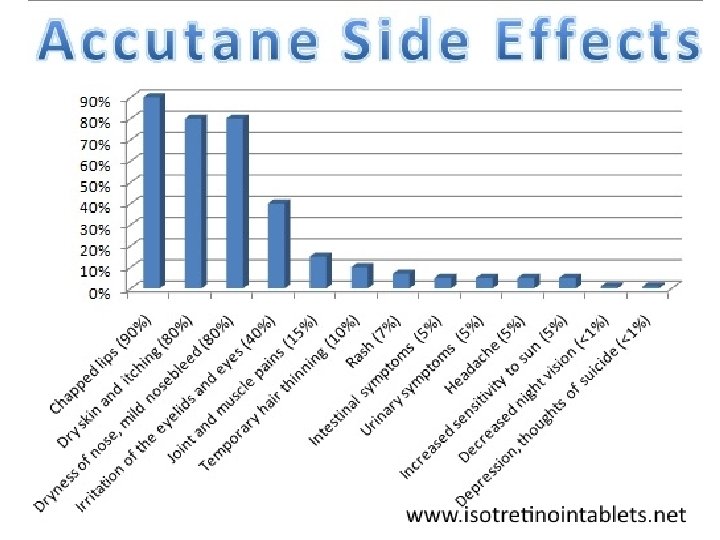
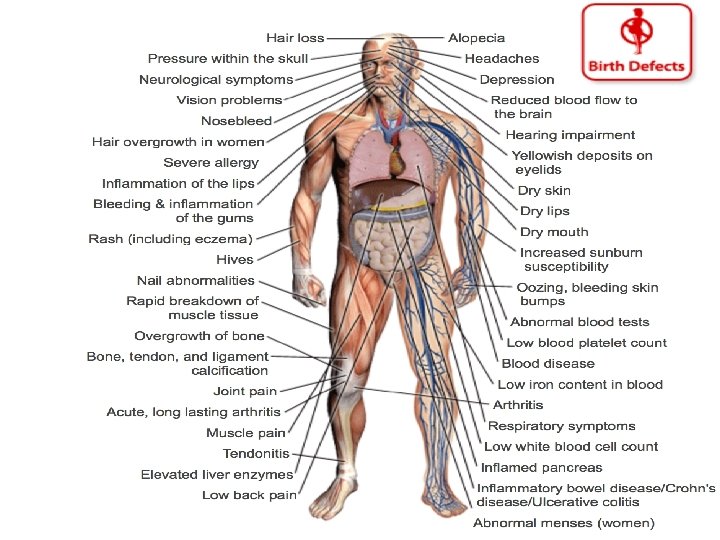
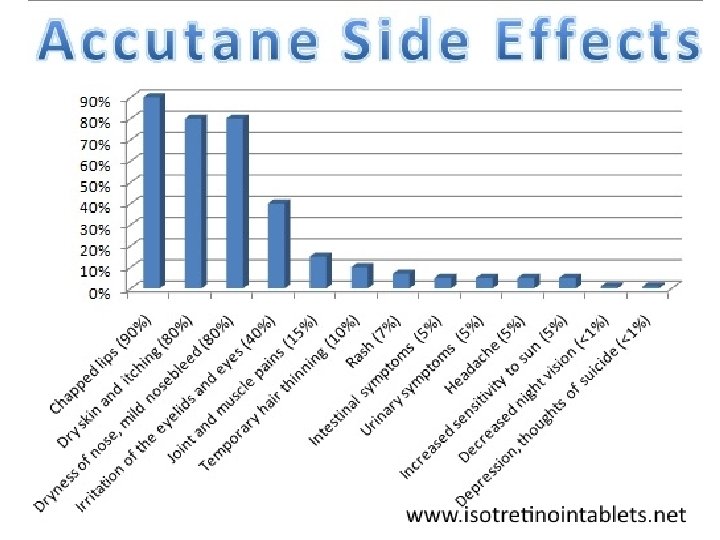
Isotretinoin (Accutane) Adverse Effects Common adverse effects (resemble hypervitaminosis A): l Dryness and itching of skin and mucous membranes l Less common: Headache, corneal opacities, pseudotumpr cerebri inflammatory bowel disease, anorexia, alopecia, muscle and joint pains l These effects are all reversible on discontinuation of therapy.
Isotretinoin (Accutane) Adverse Effects l Skeletal hyperostosis has been observed in patients receiving isotretinoin l Premature closure of epiphyses noted in children treated with this medication l Lipid abnormalities (triglycerides, HDL) are frequent l Depression, psychosis, aggressiveness or violent behavior & rarely suicidal thoughts (discontinuation MAY NOT be sufficient) l Teratogenecity
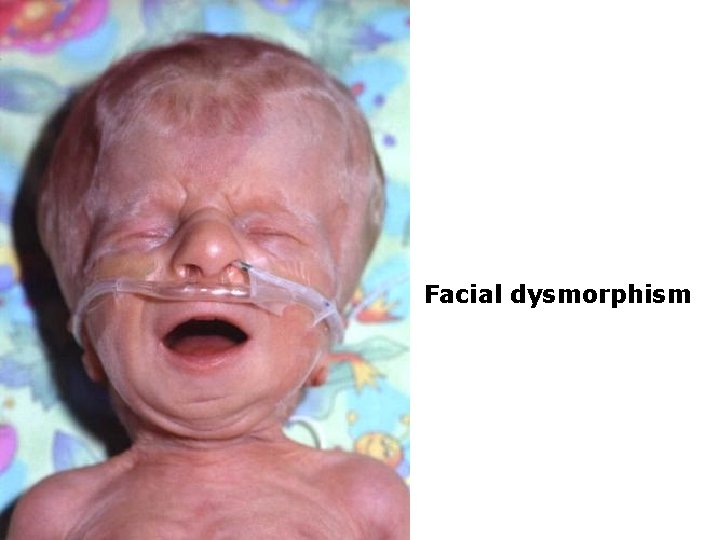
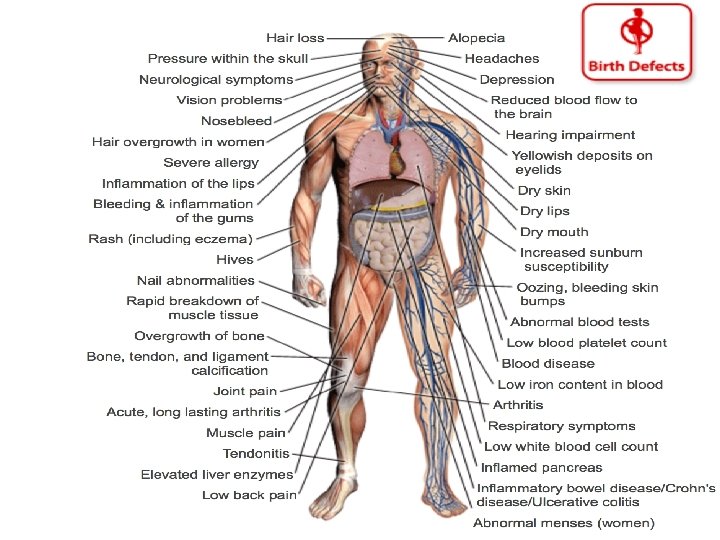
Teratogenecity l the skull, ears, and eyes and include facial dysmorphia and cleft palate. l Internal abnormalities affecting the thymus gland, central nervous system, cardiovascular system, and parathyroid gland (hormone deficiency) are recognized. l In some cases, these abnormalities have resulted in fetal death. l Nursing mothers should not receive isotretinoin.
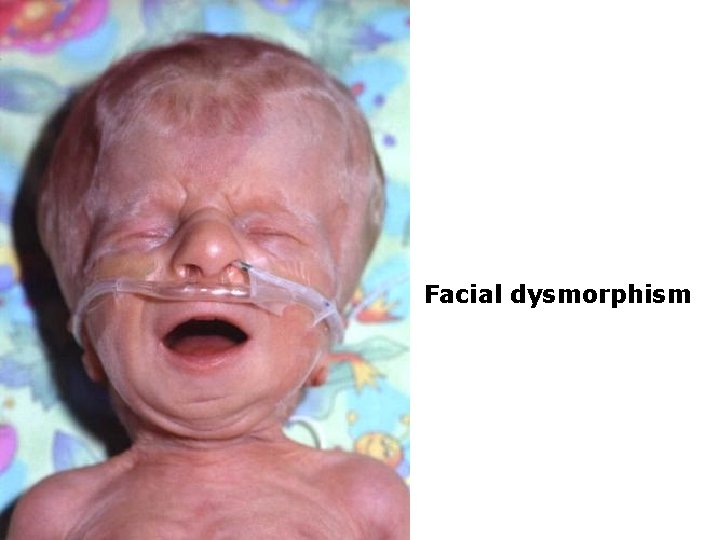
Facial dysmorphism

Cleft palate
Isotretinoin (Accutane) Teratogenecity 1. Women of childbearing age must use an effective form of contraception for at least 1 month before; throughout isotretinoin therapy, and for one or more menstrual cycles following discontinuance of therapy 2. A serum pregnancy test must be obtained within 2 weeks before starting therapy 3. Therapy should be initiated only on the second or third day after the next normal menstrual period
Isotretinoin (Accutane) Monitoring parameters: 1. CBC with differential & platelet count, baseline sed. rate, glucose, 2. Pregnancy tests 3. Lipids: prior to treatment & at weekly or biweekly intervals until response to treatment is established 4. Liver function tests: prior to treatment & at weekly or biweekly intervals until response to treatment is established 5. Creatine Phosphokinase 6. Blood Glucose
Azelaic Acid (Azelex) l l 1. 2. l l l Straight chain saturated dicarboxylic acid; effective in the treatment of acne vulgaris; Its mechanism of action not fully determined. However, studies shown: Antimicrobial activity against P acnes In vitro inhibition of the conversion of testosterone to dihydrotestosterone Initial therapy: once daily application of 20% cream to affected areas for 1 week. Then twice daily thereafter Mild irritation with redness and dryness of the skin during the first week of treatment Clinical improvement 6 -8 weeks of continuous therapy
Topical Antibiotics l Commonly prescribed: erythromycin and clindamycin alone or in combination with benzoyl peroxide l MOA: (1) bactericidal activity against P acnes. (2) may also have anti-inflammatory effect l Topical antibiotics are not comedolytic, l Bacterial resistance may develop to any of these agents. l The development of resistance is lessened if topical antibiotics are used in combination with benzoyl peroxide
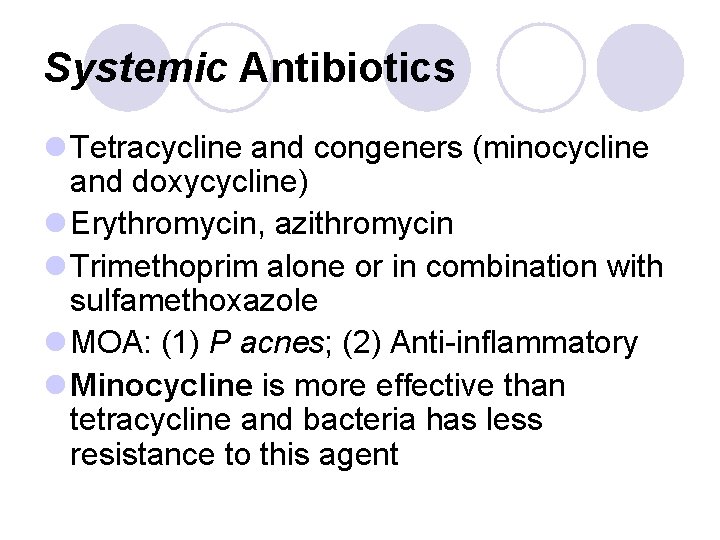
Systemic Antibiotics l Tetracycline and congeners (minocycline and doxycycline) l Erythromycin, azithromycin l Trimethoprim alone or in combination with sulfamethoxazole l MOA: (1) P acnes; (2) Anti-inflammatory l Minocycline is more effective than tetracycline and bacteria has less resistance to this agent
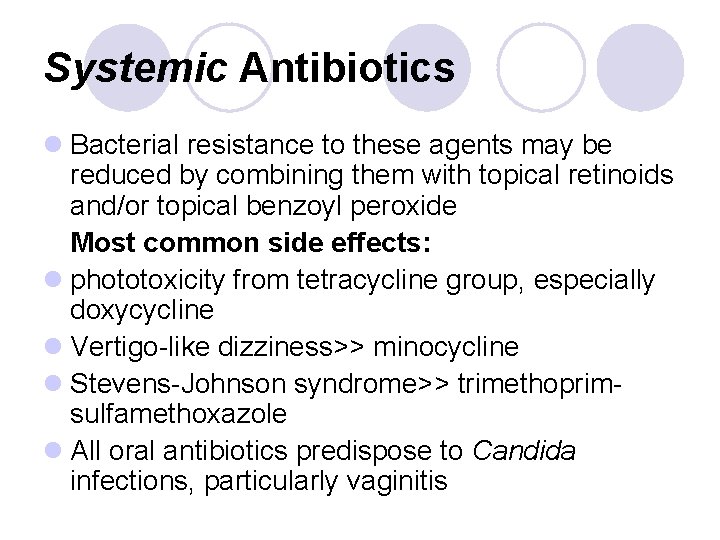
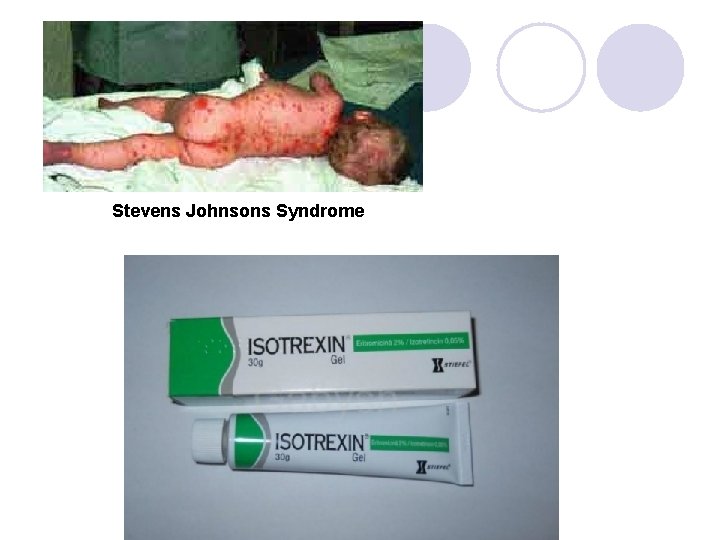
Systemic Antibiotics l Bacterial resistance to these agents may be reduced by combining them with topical retinoids and/or topical benzoyl peroxide Most common side effects: l phototoxicity from tetracycline group, especially doxycycline l Vertigo-like dizziness>> minocycline l Stevens-Johnson syndrome>> trimethoprimsulfamethoxazole l All oral antibiotics predispose to Candida infections, particularly vaginitis
Stevens Johnsons Syndrome
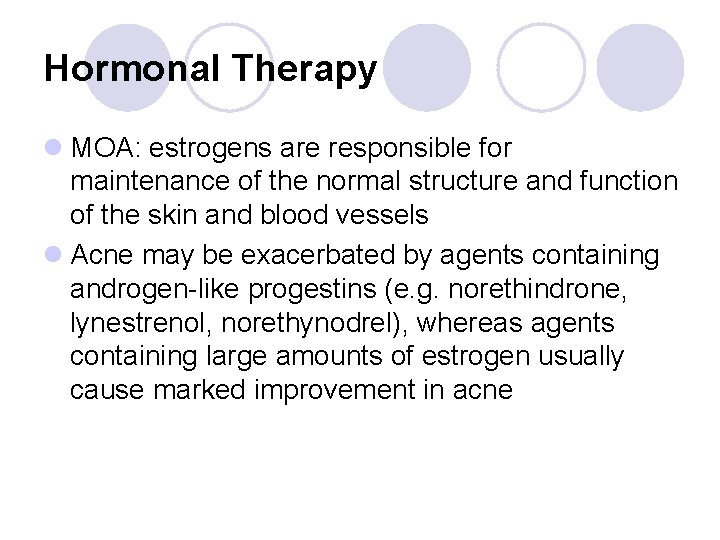
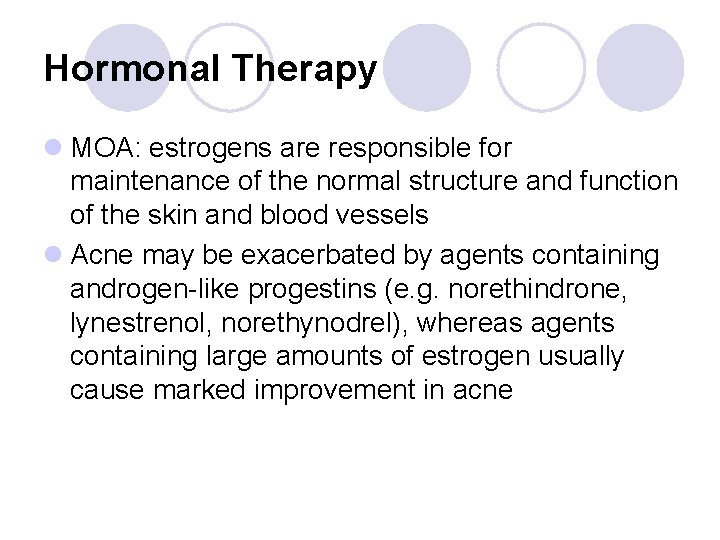
Hormonal Therapy l MOA: estrogens are responsible for maintenance of the normal structure and function of the skin and blood vessels l Acne may be exacerbated by agents containing androgen-like progestins (e. g. norethindrone, lynestrenol, norethynodrel), whereas agents containing large amounts of estrogen usually cause marked improvement in acne
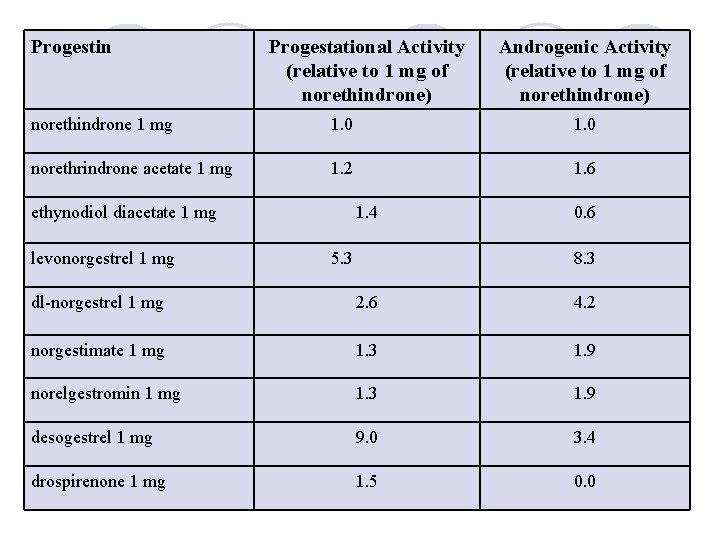
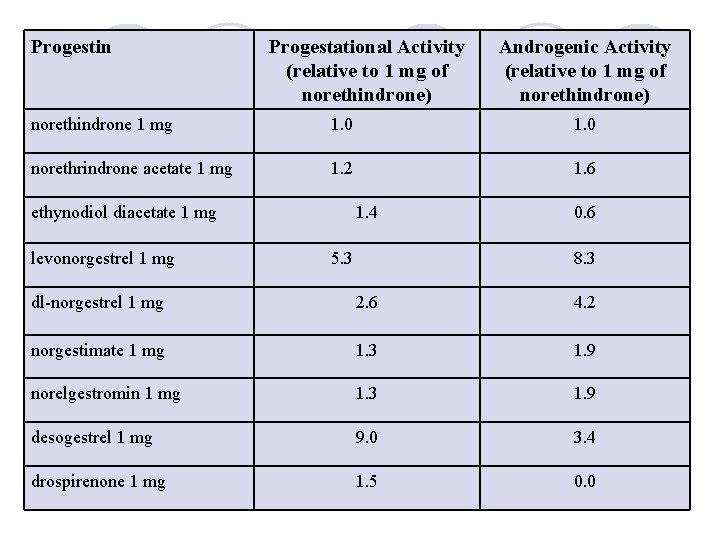
Progestin Progestational Activity (relative to 1 mg of norethindrone) Androgenic Activity (relative to 1 mg of norethindrone) norethindrone 1 mg 1. 0 norethrindrone acetate 1 mg 1. 2 1. 6 ethynodiol diacetate 1 mg levonorgestrel 1 mg 1. 4 5. 3 0. 6 8. 3 dl-norgestrel 1 mg 2. 6 4. 2 norgestimate 1 mg 1. 3 1. 9 norelgestromin 1 mg 1. 3 1. 9 desogestrel 1 mg 9. 0 3. 4 drospirenone 1 mg 1. 5 0. 0
Ethinyl estradiol + Drospirenone
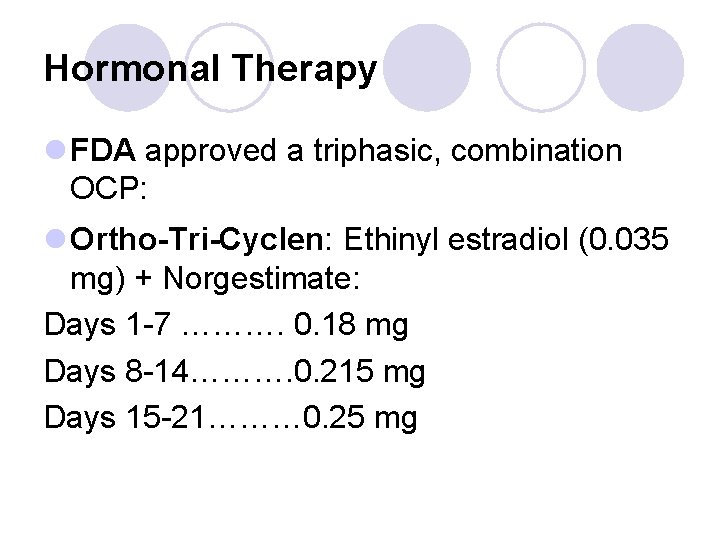
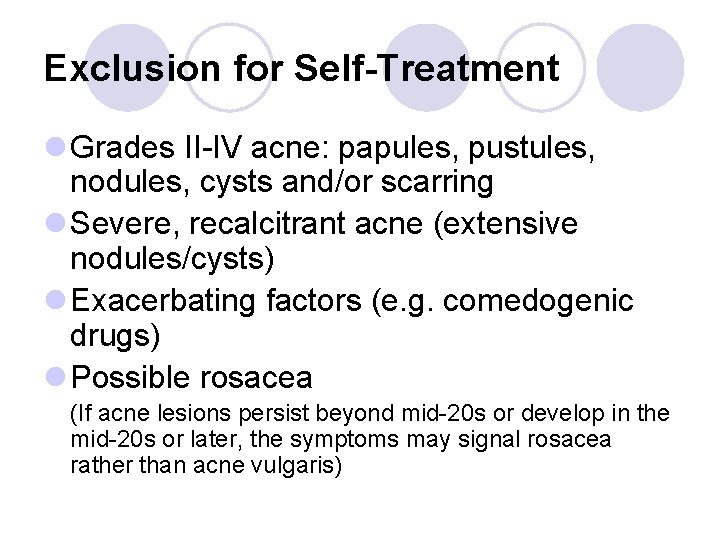
Hormonal Therapy l FDA approved a triphasic, combination OCP: l Ortho-Tri-Cyclen: Ethinyl estradiol (0. 035 mg) + Norgestimate: Days 1 -7 ………. 0. 18 mg Days 8 -14………. 0. 215 mg Days 15 -21……… 0. 25 mg
Hormonal Therapy l A study showed that this OC reduced acne lesion counts by more than 50% in female subjects, compared with lesion reductions of about 26% in controls l Acne improvement during treatment with Ortho. Tri Cyclen may take 3 -4 months to become apparent; l Main limitation of anti-androgen therapy for acne is that it cannot be used with male patients