Treatment of Acne What is acne l Acne



- Slides: 46

Treatment of Acne
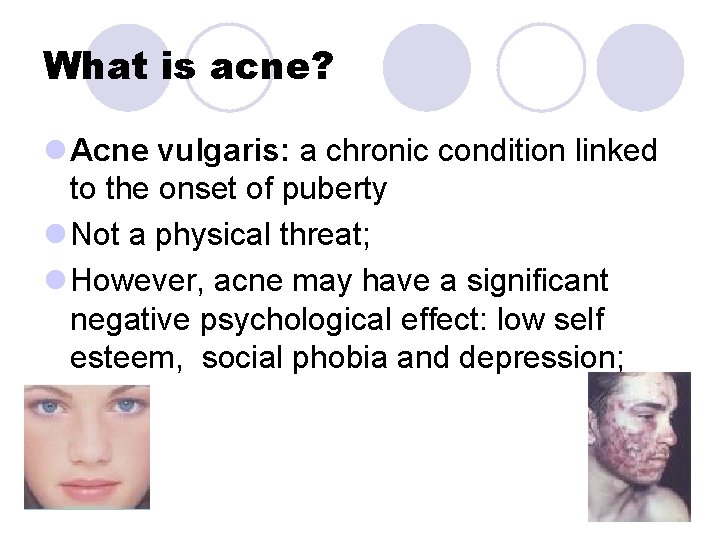
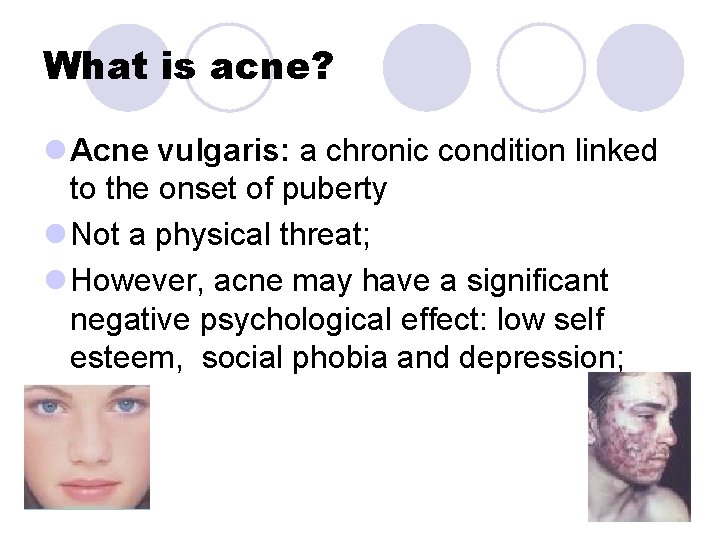
What is acne? l Acne vulgaris: a chronic condition linked to the onset of puberty l Not a physical threat; l However, acne may have a significant negative psychological effect: low self esteem, social phobia and depression;
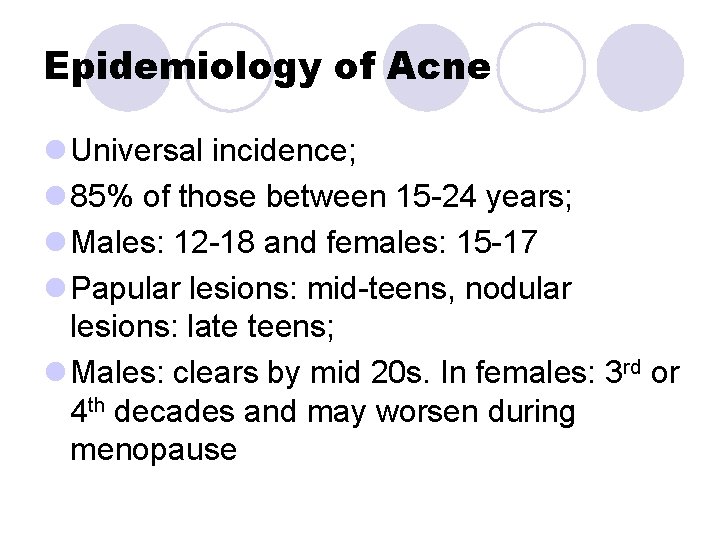
Epidemiology of Acne l Universal incidence; l 85% of those between 15 -24 years; l Males: 12 -18 and females: 15 -17 l Papular lesions: mid-teens, nodular lesions: late teens; l Males: clears by mid 20 s. In females: 3 rd or 4 th decades and may worsen during menopause
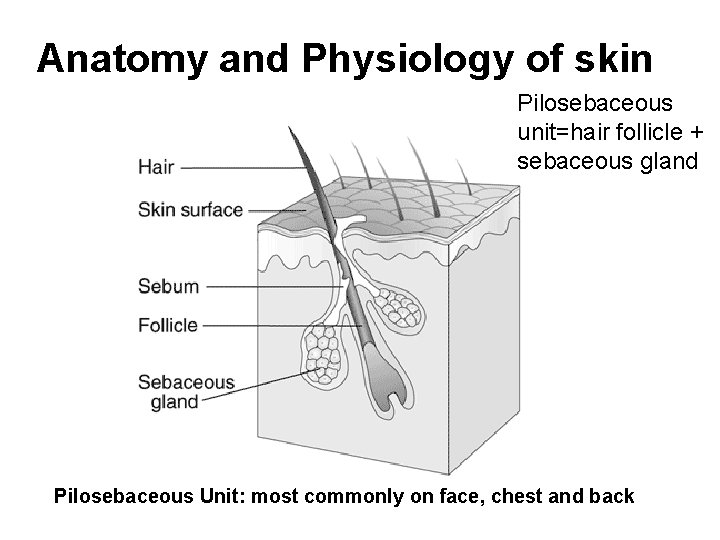
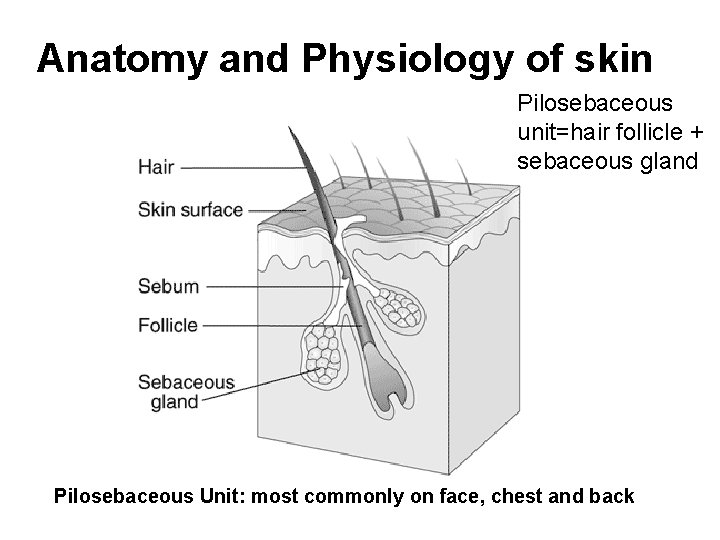
Anatomy and Physiology of skin Pilosebaceous unit=hair follicle + sebaceous gland Pilosebaceous Unit: most commonly on face, chest and back

Scalp folliculitis “Acne necrotica miliaris”
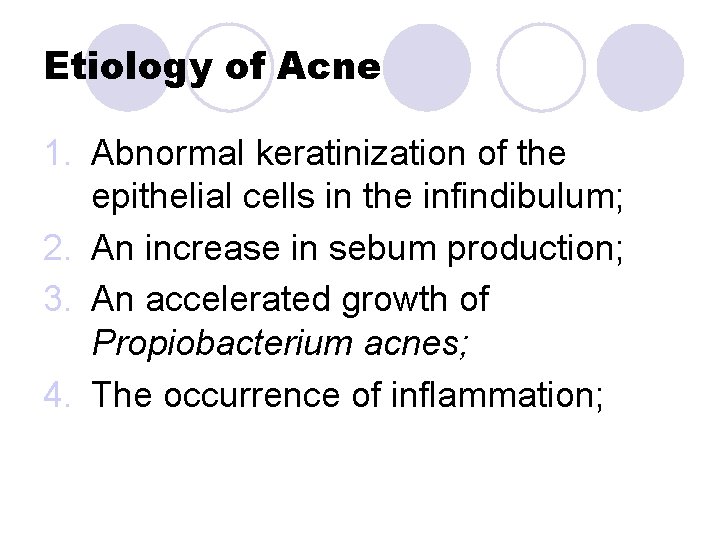
Etiology of Acne 1. Abnormal keratinization of the epithelial cells in the infindibulum; 2. An increase in sebum production; 3. An accelerated growth of Propiobacterium acnes; 4. The occurrence of inflammation;
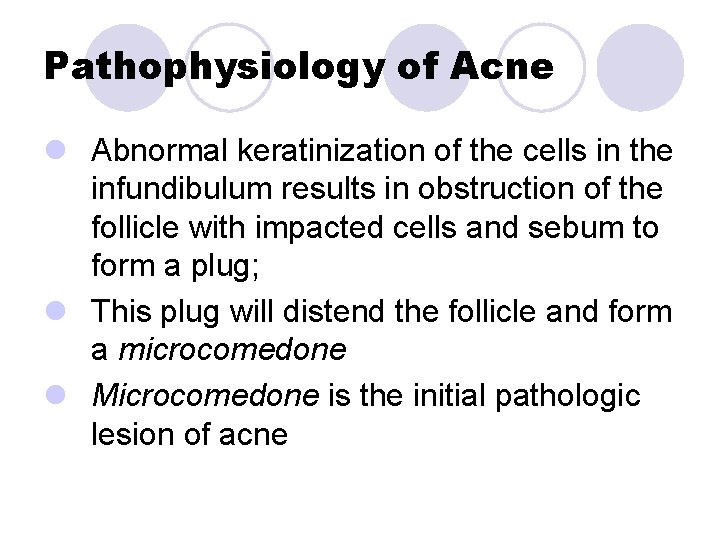
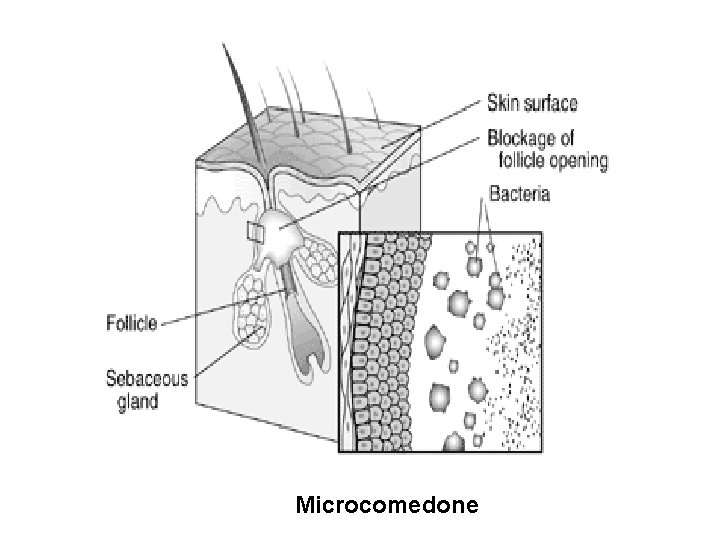
Pathophysiology of Acne l Abnormal keratinization of the cells in the infundibulum results in obstruction of the follicle with impacted cells and sebum to form a plug; l This plug will distend the follicle and form a microcomedone l Microcomedone is the initial pathologic lesion of acne
Microcomedone
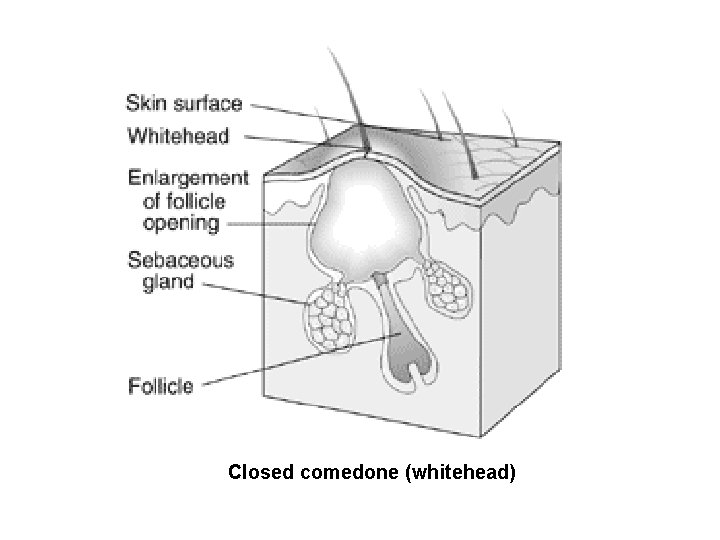
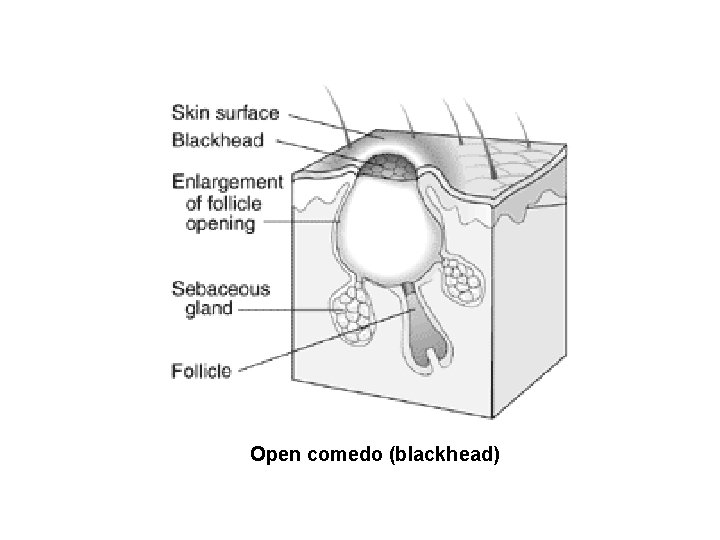
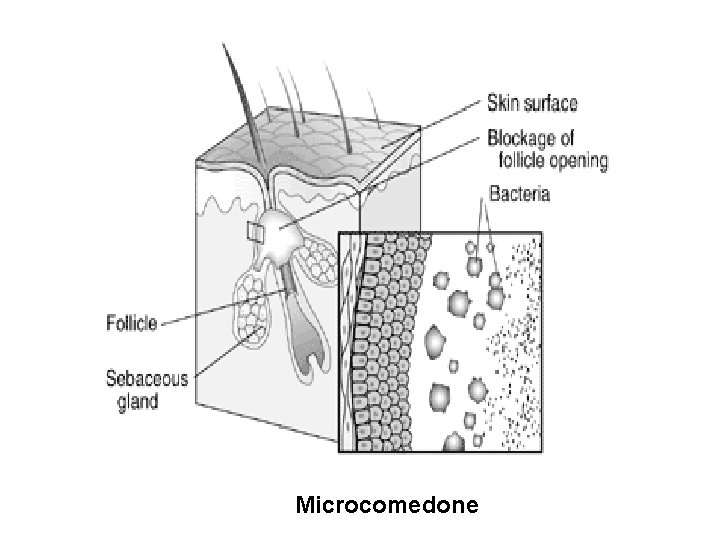
Pathophysiology of Acne l As more sebum accumulate, the microcomedone enlarges and becomes visible as a closed comedo, or white head l The whitehead: is a small pale nodule just beneath the skin surface that may form a precursor for other acne lesions l An open comedo (blackhead) occurs: when the desquamated epithelial cells and sebum accumulate behind the plug and the orifice of the follicular canal becomes distended, allowing the plug to protrude l The tip of the plug may darken because of melanin NOT dirt;
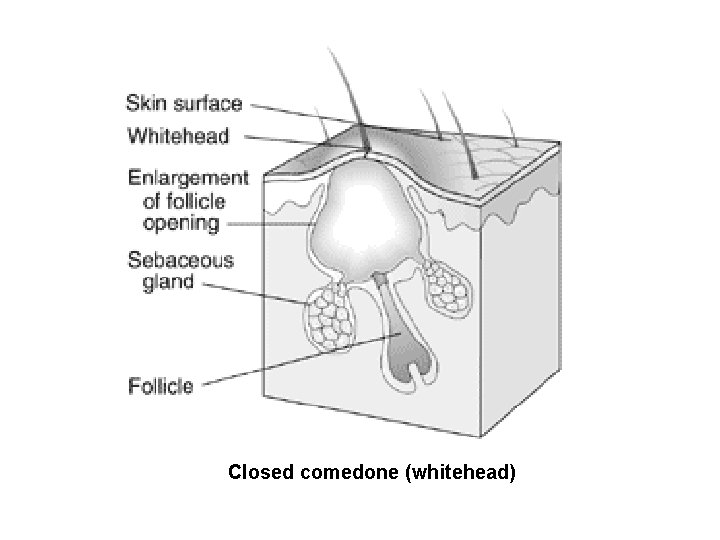
Closed comedone (whitehead)
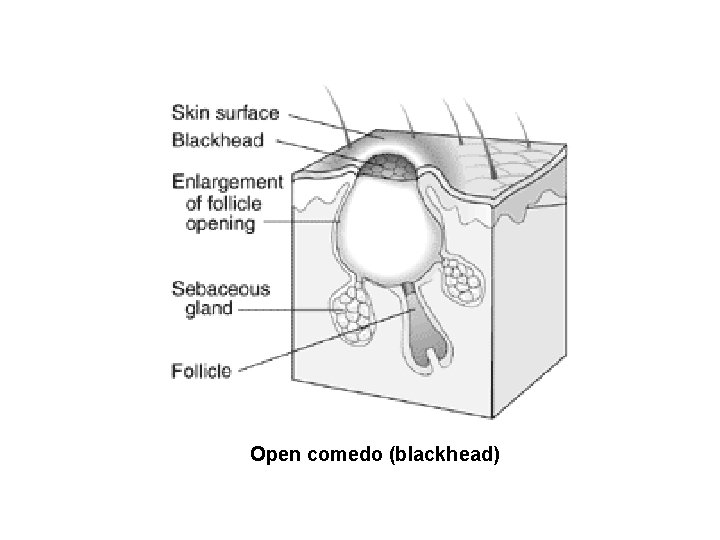
Open comedo (blackhead)
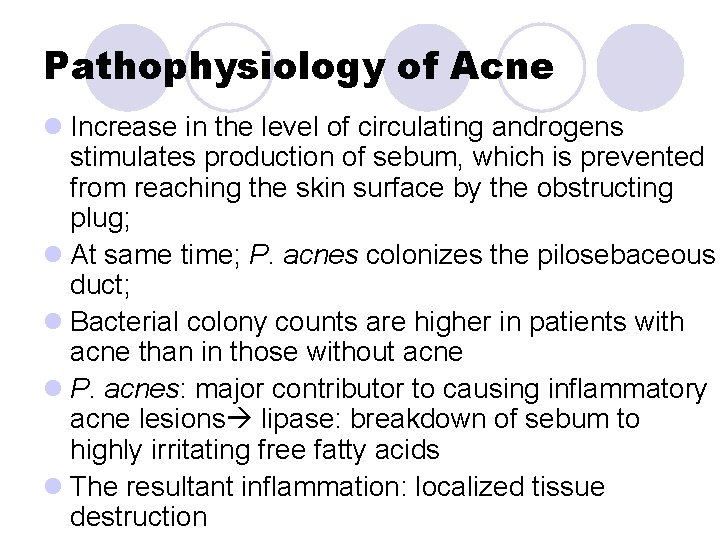
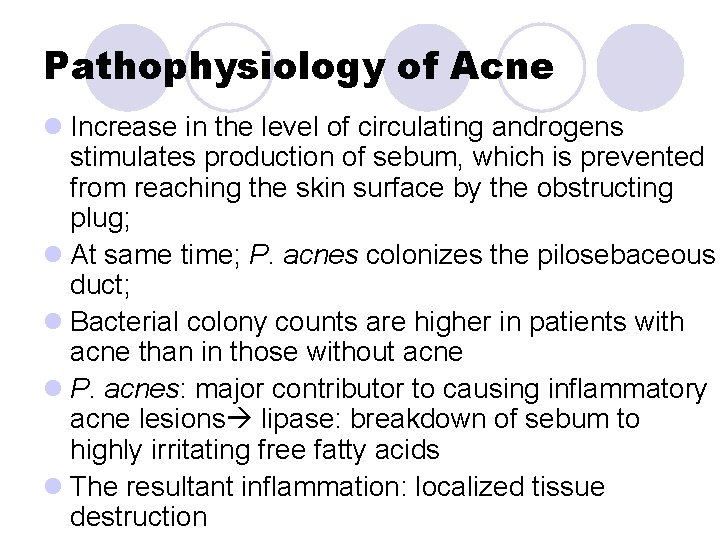
Pathophysiology of Acne l Increase in the level of circulating androgens stimulates production of sebum, which is prevented from reaching the skin surface by the obstructing plug; l At same time; P. acnes colonizes the pilosebaceous duct; l Bacterial colony counts are higher in patients with acne than in those without acne l P. acnes: major contributor to causing inflammatory acne lesions lipase: breakdown of sebum to highly irritating free fatty acids l The resultant inflammation: localized tissue destruction
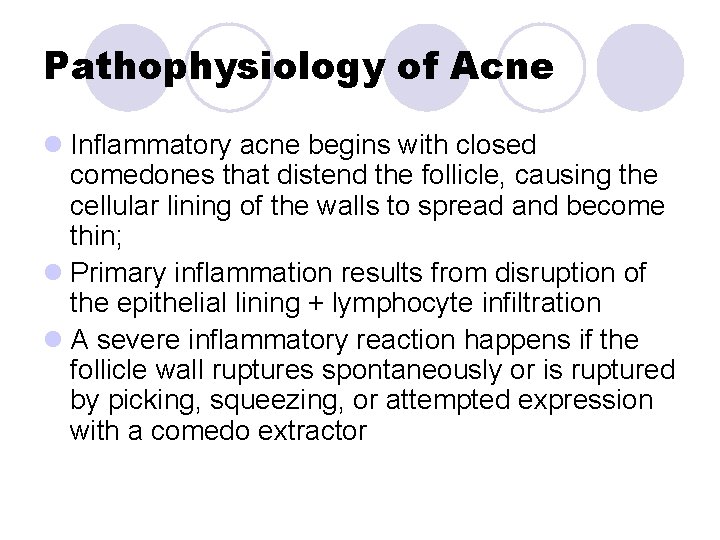
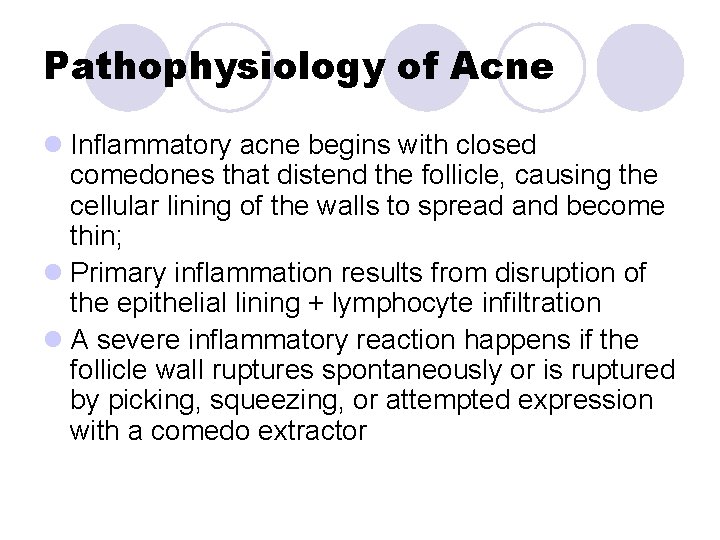
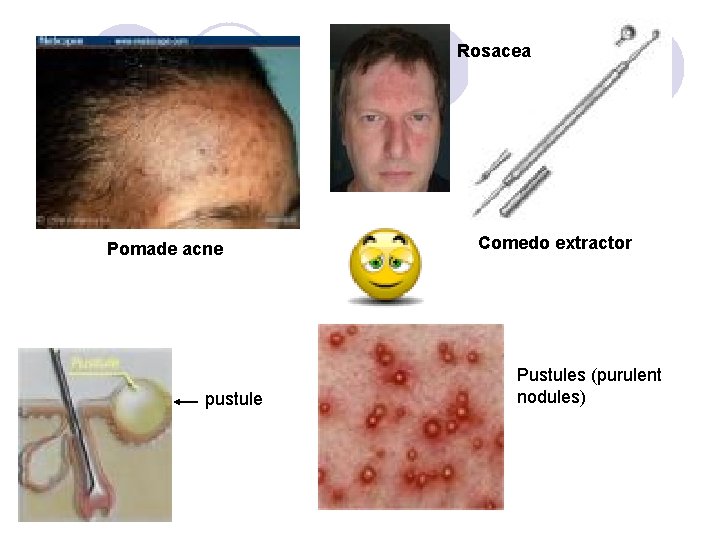
Pathophysiology of Acne l Inflammatory acne begins with closed comedones that distend the follicle, causing the cellular lining of the walls to spread and become thin; l Primary inflammation results from disruption of the epithelial lining + lymphocyte infiltration l A severe inflammatory reaction happens if the follicle wall ruptures spontaneously or is ruptured by picking, squeezing, or attempted expression with a comedo extractor
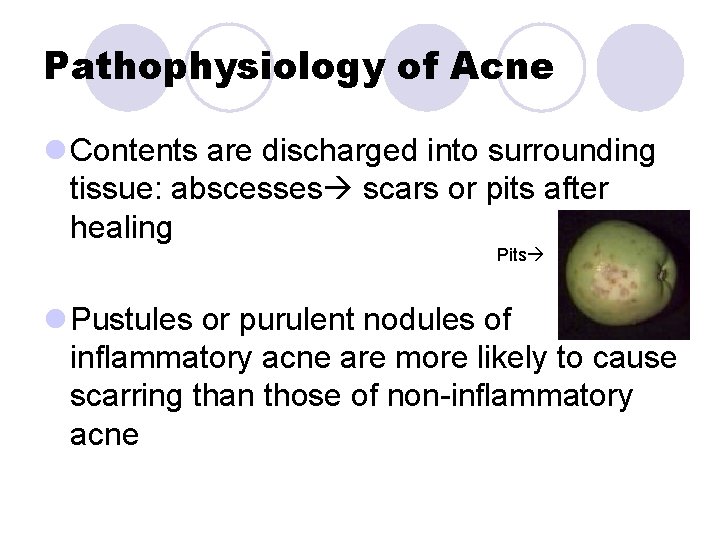
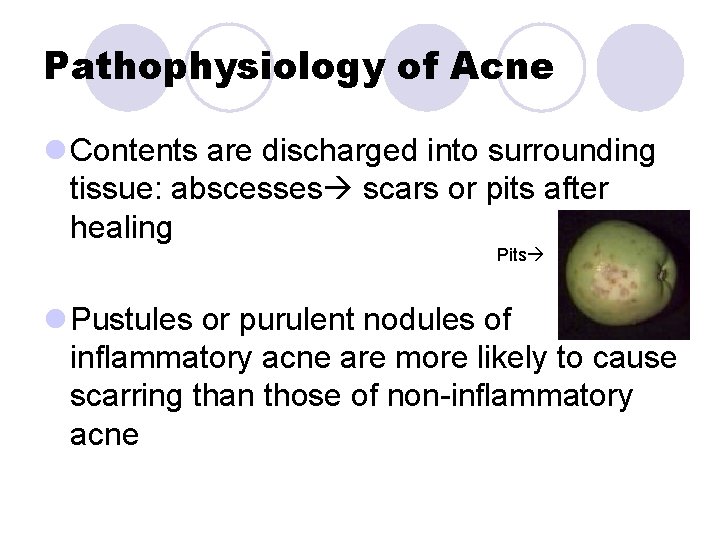
Pathophysiology of Acne l Contents are discharged into surrounding tissue: abscesses scars or pits after healing Pits l Pustules or purulent nodules of inflammatory acne are more likely to cause scarring than those of non-inflammatory acne
Exacerbating Factors for Acne l Several factors are known to exacerbate existing acne or cause periodic flare-ups of acne in some patients; l Some may have control over, while others not (e. g. heredity); l Factors: environmental and physical factors, cosmetic use, hormonal factors and medication use
Environmental & Physical 1. Hydration: decreases size of duct orifice and prevents loosening of comedone. e. g. high humidity environment or prolonged sweating and occlusive clothing 2. Irritation and friction (acne mechanica): may increase symptoms of acne. E. g. occlusive clothing, headbands, helmets, resting chin or cheek on hand etc 3. Occupational acne: exposure to dirt, vaporized cooking oils, or certain industrial chemicals
Cosmetic Use l Acne cosmetica: mild form of acne on the face, cheek and chin; l Typically: closed, non-inflammatory comedones; l Occurs as a result of using oil-based products on the skin that causes occlusion of the pilosebaceous unit; l Oil-based cosmetics may exacerbate acne or even induce it; l Moisturizers or tanning oils may contain comedogenic oils (e. g. lanolin, mineral oil, cocoa butter)
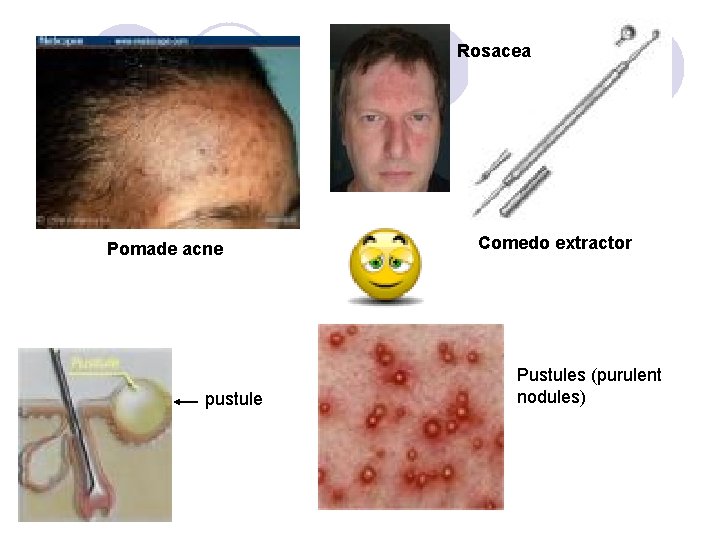
Rosacea Pomade acne pustule Comedo extractor Pustules (purulent nodules)
Emotional Factors l Severe or prolonged periods of stress may exacerbate acne; however they do not induce acne! l Mechanism is not known Hormonal Factors l Many women with acne experience a premenstrual flare-up of symptoms (i. e. ovulation, pregnancy). l OCP with high androgenic progestin are implicated in the production of acne
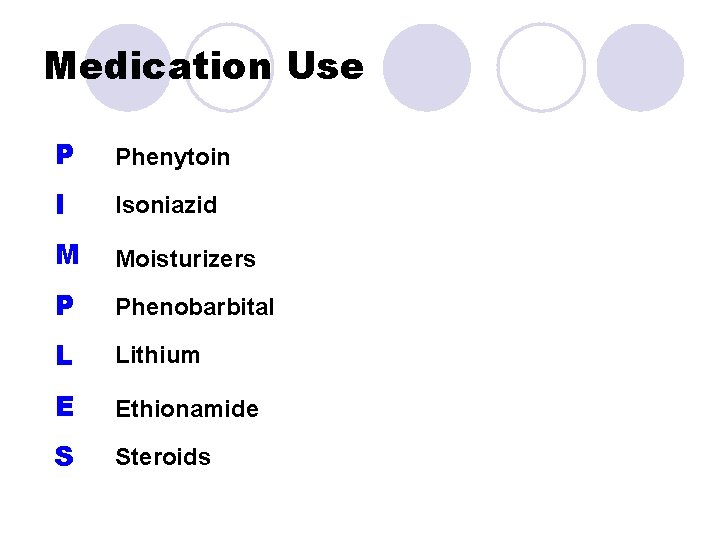
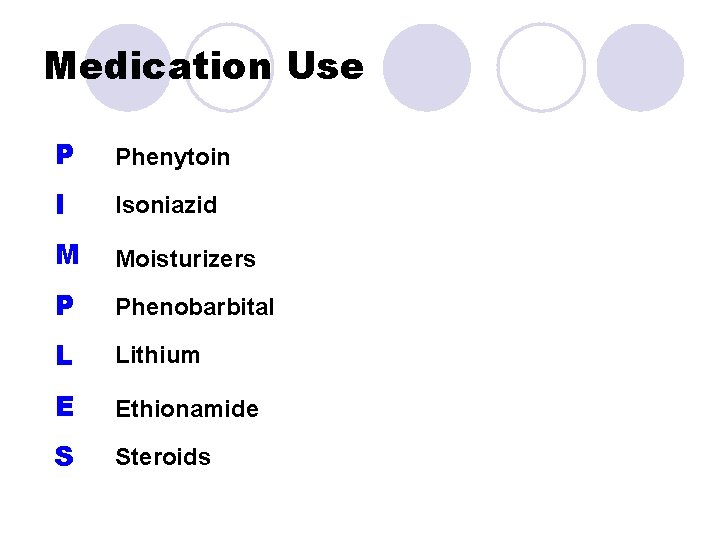
Medication Use P Phenytoin I Isoniazid M Moisturizers P Phenobarbital L Lithium E Ethionamide S Steroids
Unsubstantiated Etiologic Factors l Little evidence supports link between: diet and acne; l A rule of thumb: people should be advised to avoid any particular food that seems to exacerbate their acne; l Excessive scrubbing in attempt to open blocked pores may exacerbate rather than improve acne
“I know you're never supposed to squeeze a zit, but I'm not about to leave the house with a major eruption on my face. Isn't there any good way to pop it? ” !!!!!
Can I pop a pimple? !! l Opinion differs (Some say popping a pimple can scar, others say it can't scar) l Most: lancing and gently squeezing pimples that are at the surface and white will usually not lead to scarring. l However, trying to squeeze and pop a pimple which is still below the surface may lead to major problems.
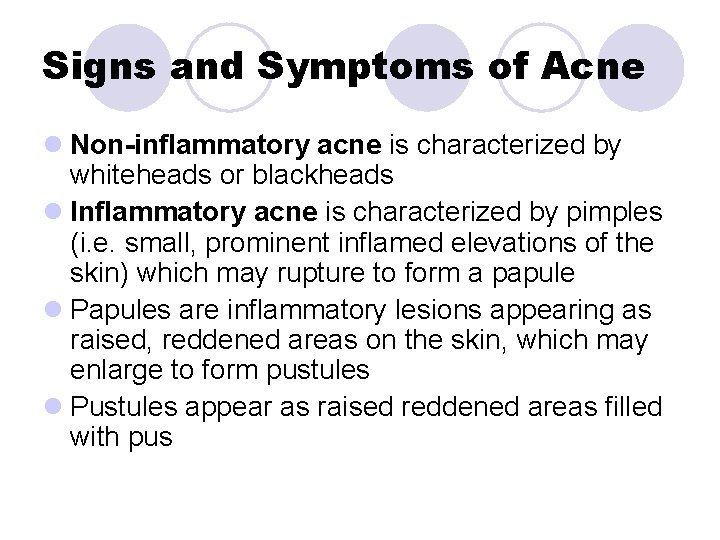
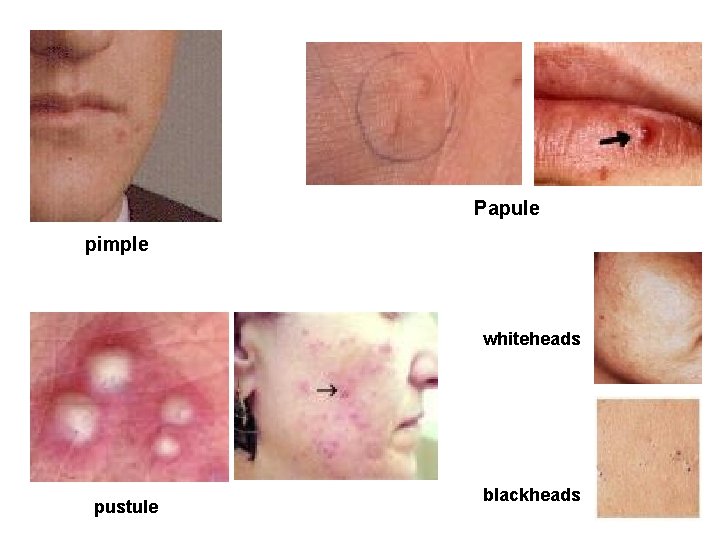
Signs and Symptoms of Acne l Non-inflammatory acne is characterized by whiteheads or blackheads l Inflammatory acne is characterized by pimples (i. e. small, prominent inflamed elevations of the skin) which may rupture to form a papule l Papules are inflammatory lesions appearing as raised, reddened areas on the skin, which may enlarge to form pustules l Pustules appear as raised reddened areas filled with pus
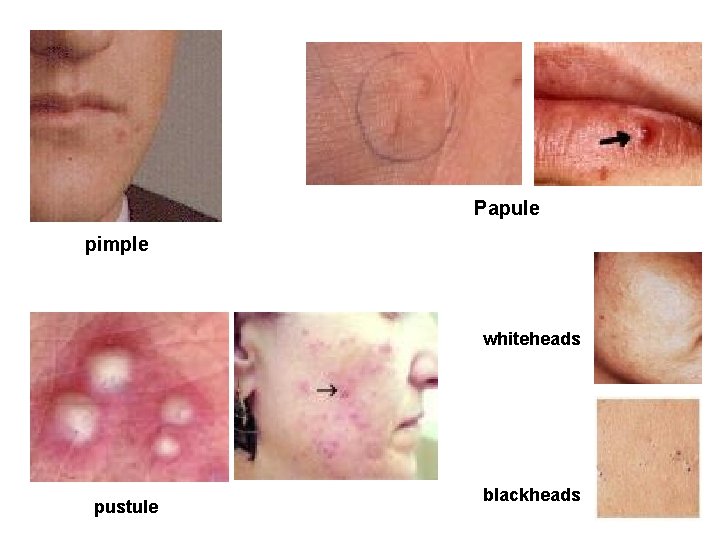
Papule pimple whiteheads pustule blackheads

Very severe acne, cystic acne, acne conglobata
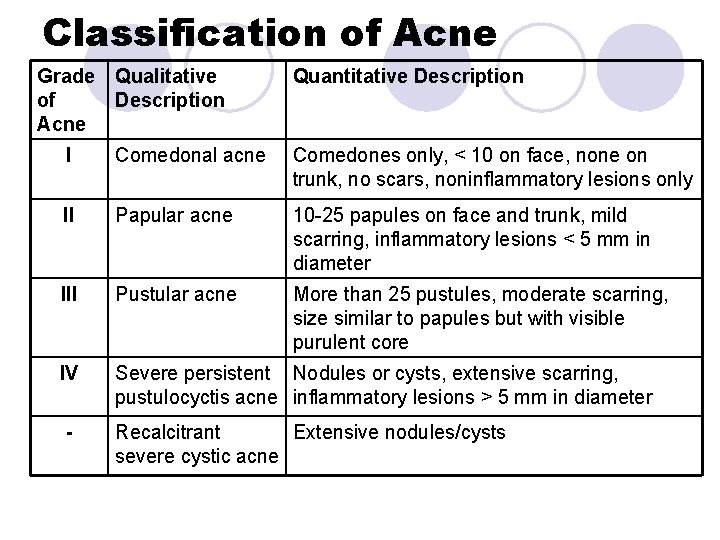
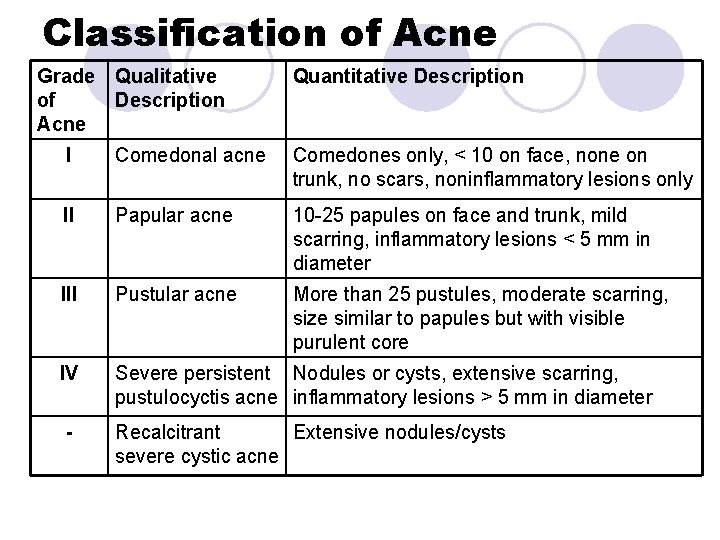
Classification of Acne Grade of Acne Qualitative Description Quantitative Description I Comedonal acne Comedones only, < 10 on face, none on trunk, no scars, noninflammatory lesions only II Papular acne 10 -25 papules on face and trunk, mild scarring, inflammatory lesions < 5 mm in diameter III Pustular acne More than 25 pustules, moderate scarring, size similar to papules but with visible purulent core IV Severe persistent Nodules or cysts, extensive scarring, pustulocyctis acne inflammatory lesions > 5 mm in diameter - Recalcitrant Extensive nodules/cysts severe cystic acne
Treatment of Acne Non-pharmacologic therapy l Cleansing of Skin l Minimize Exacerbating factors Pharmacologic Therapy
Pharmacologic Therapy l. Benzoyl Peroxide l. Salicylic acid l. Sulfur-Resorcinol combination products l. Alpha-hydroxy acids
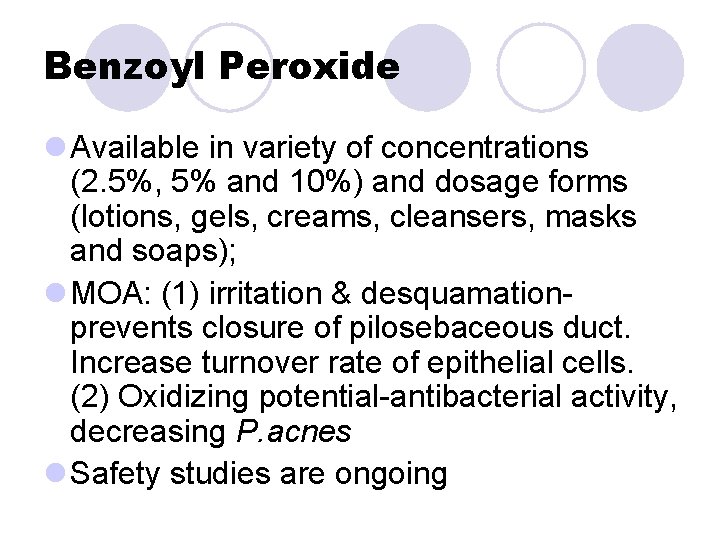
Benzoyl Peroxide l Available in variety of concentrations (2. 5%, 5% and 10%) and dosage forms (lotions, gels, creams, cleansers, masks and soaps); l MOA: (1) irritation & desquamationprevents closure of pilosebaceous duct. Increase turnover rate of epithelial cells. (2) Oxidizing potential-antibacterial activity, decreasing P. acnes l Safety studies are ongoing
Benzoyl Peroxide l The most effective and widely used OTC drug for non-inflammatory acne; l Clinical response to all concentrations is similar in reducing the number of inflammatory lesions l Different formulations are not equivalent: alcohol gel is superior to lotion of the same concentration; l Washes and cleansers: have little or no comedolytic effect
Benzoyl Peroxide l Adverse Effects: excessive dryness, peeling, some skin sloughing, erythema or edema lower concentrations must be used for shorter duration l Stinging/burning: non alarming unless persist or worsen l Precautions: (1) bleach hair, clothes, bed linens, (2)avoid excessive sun or sunlamps, (3) alcohol-based products (e. g. after shave lotion)( may exacerbate stinging/burning
Salicylic Acid l Available in wide range: 0. 5%-2% l A milder, less effective alternative for teretoin l MOA: acts as a surface keratolytic, mild comedolytic agent l When used in cleansing preparations: adjunctive treatment
Sulfur l Keratolytic and antibacterial (precipitated or colloidal) 3%-10% l Generally: accepted as effective in promoting the resolution of existing comedones, but, on continued use, may have a comedogenic effect l Alternative forms of sulfur: Na thiosulfate, Zn sulfide NGRSE l Applied in thin film to skin 3 times daily l Have noticeable color and odor
Sulfur-Resorcinol combination l 3 -8% sulfur with resorcinol 2% (enhances the effect of sulfur) l MOA: keratolytics, fostering cell turnover and desquamation l Resorcinol produces a reversible dark brown scale on some darker-skinned individuals
Alpha-hyrdoxy Acids l They occur naturally in sugar cane, fruits and milk products; l The most useful AHAs in dermatologic practice are glycolic acid, lactic acid and gluconic acid l MOA: facilitate desquamation of the stratum corneum. l Effective in treatment of comedonal acne
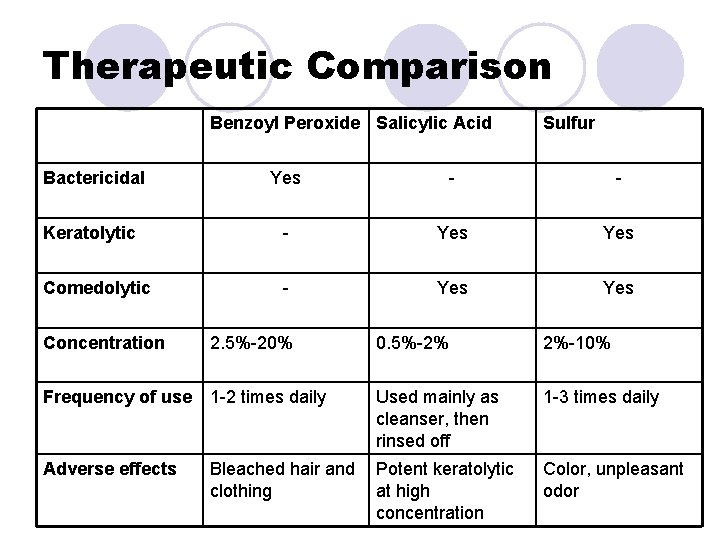
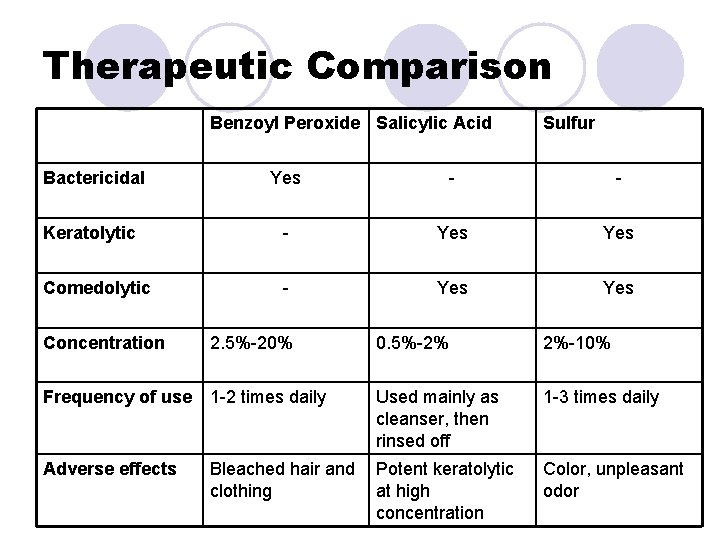
Therapeutic Comparison Benzoyl Peroxide Salicylic Acid Sulfur Bactericidal Yes - - Keratolytic - Yes Comedolytic - Yes Concentration 2. 5%-20% 0. 5%-2% 2%-10% Frequency of use 1 -2 times daily Used mainly as cleanser, then rinsed off 1 -3 times daily Adverse effects Potent keratolytic at high concentration Color, unpleasant odor Bleached hair and clothing
Product Selection Guidelines l Cosmetic appearance may influence compliance l Cleansers (bars, liquids, suspensions, lotions, creams, gels, and pads/wipes) are not of much value (WHY? ) l Lotions & creams with low fat content are intended to counteract drying (astringent effect) and peeling (keratolytic effect): alternative to more effective gels for dry sensitive skin or during winter weather
Patient Education: l The goal of self-treatment is to control mild acne, thus preventing more serious form from developing l Acne usually goes away on its own l Symptoms can usually be managed with diligent and long term treatment l Best approach is use cleansers and medications to keep skin ducts and orifices open
Patient Education: l Cleanse skin thoroughly but gently at least twice daily to produce a mild drying effect that loosens comedones, using soft wash cloth, warm water and facial soap without moisturizing oils l To prevent or minimize acne flare-ups, avoid or reduce exposure to environmental factors, such as dirt, dust, petroleum products, cooking oils or chemical irritants
Patient Education: l To prevent friction or irritation that may cause acne flare-ups, do not wear tightfitting clothes, headbands, or helmets, avoid resting the chin on the hand; l To minimise acne related to cosmetic use, do not use oil based cosmetics and shampoos
Patient Education: l To prevent excessive hydration of the skin, which can cause flare-ups, avoid areas of high humidity and do not wear tight fitting clothes that restrict air movement; l Try to maintain proper diet, although a link between diet and acne is not found; l Avoid stressful situations. Stress may play a role in acne flare-ups but it does not cause acne
Selected websites for acne information www. aad. org www. acne. org www. derm-infonet. com/acnenet www. facefacts. com www. fda. gov www. nlm. nih. gov/medlinepluse/acne. html www. rosacea. org www. Skincarephysicians. com/acnenet www. holisticonline. com/remedies/Acne. htm
Glossary: l Comedo: A plug of keratin and sebum within the dilated orifice of a hair follicle, frequently containing the bacteria Propionibacterium acnes, Staphylococcus albus and Pityrosporon ovale, also called blackhead. l Propiobacterium acnes: a gram positive anearobic rod found on the skin l Pustule: a vesicle or an elevation of the cuticle with an inflamed base, containing pus.
Glossary: l Blemish: Any mark of deformity or injury, whether physical or moral; anything; that diminishes beauty, or renders imperfect that which is otherwise well formed l Pimple: Any small acuminated elevation of the cuticle, whether going on to suppuration or not l Papule: A small circumscribed, superficial, solid elevation of the skin