TREATMENT MANAGEMENT OF SEVERE ACUTE PROTEINENERGY MALNUTRITION IN


- Slides: 27
TREATMENT & MANAGEMENT OF SEVERE ACUTE (PROTEIN-ENERGY) MALNUTRITION IN CHILDREN Global Health Fellowship Nutrition Module
Severe Malnutrition Medical & social disorder End result of chronic nutritional & emotional deprivation Management requires medical & social interventions
Underlying causes of poor diet & excess disease (UNICEF) Insufficient access to food Inadequate maternal & child care Poor environment Inadequate or lack of access to health services
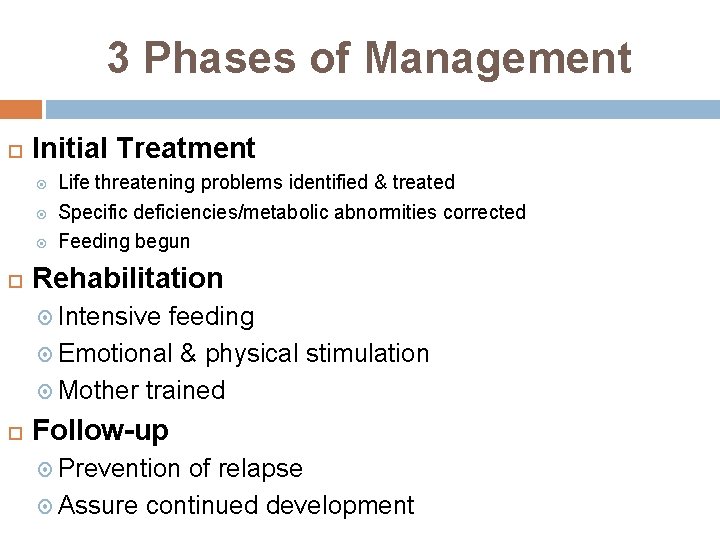
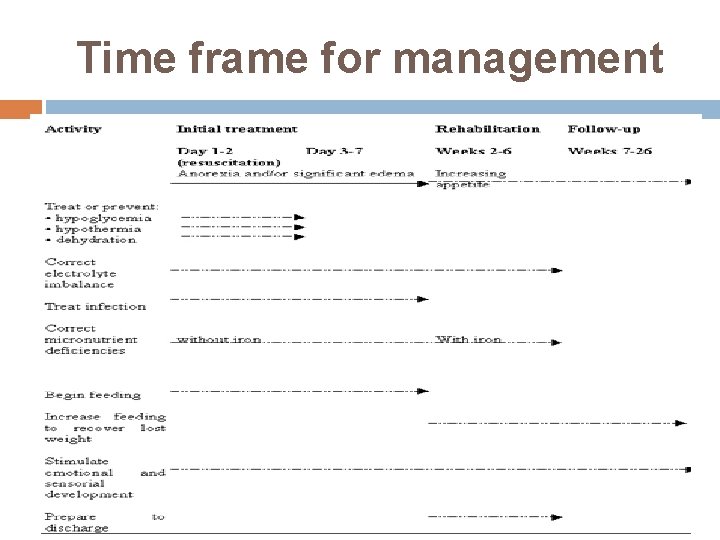
3 Phases of Management Initial Treatment Life threatening problems identified & treated Specific deficiencies/metabolic abnormities corrected Feeding begun Rehabilitation Intensive feeding Emotional & physical stimulation Mother trained Follow-up Prevention of relapse Assure continued development

Treatment Facilities Initial treatment & beginning of rehabilitation SAM with complication (anorexia, infection, dehydration) Residential care in special nutrition unit SAM w/out complications, s/p inpt has appetite. gaining weight, stable Nutritional rehabilitation center: day hospital, 1 ary health center CTC
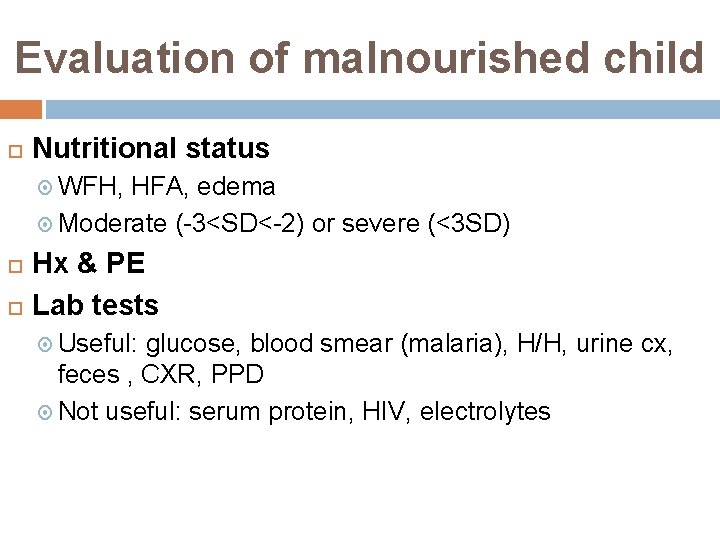
Evaluation of malnourished child Nutritional status WFH, HFA, edema Moderate (-3<SD<-2) or severe (<3 SD) Hx & PE Lab tests Useful: glucose, blood smear (malaria), H/H, urine cx, feces , CXR, PPD Not useful: serum protein, HIV, electrolytes
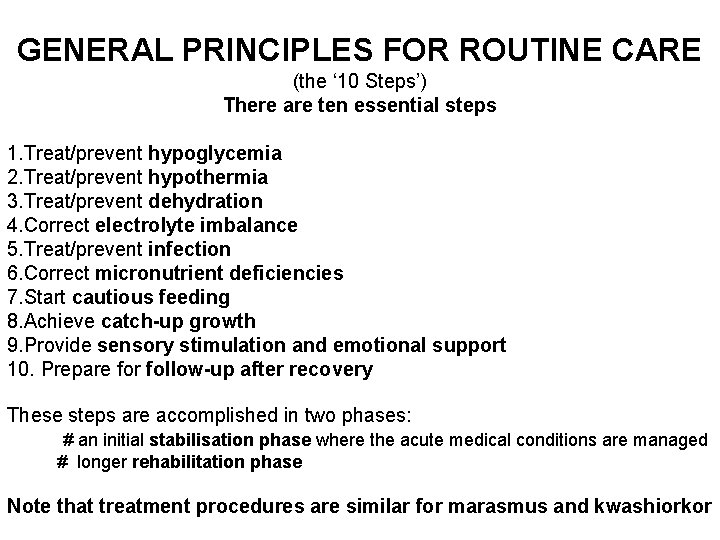
GENERAL PRINCIPLES FOR ROUTINE CARE (the ‘ 10 Steps’) There are ten essential steps 1. Treat/prevent hypoglycemia 2. Treat/prevent hypothermia 3. Treat/prevent dehydration 4. Correct electrolyte imbalance 5. Treat/prevent infection 6. Correct micronutrient deficiencies 7. Start cautious feeding 8. Achieve catch-up growth 9. Provide sensory stimulation and emotional support 10. Prepare for follow-up after recovery These steps are accomplished in two phases: # an initial stabilisation phase where the acute medical conditions are managed # longer rehabilitation phase Note that treatment procedures are similar for marasmus and kwashiorkor
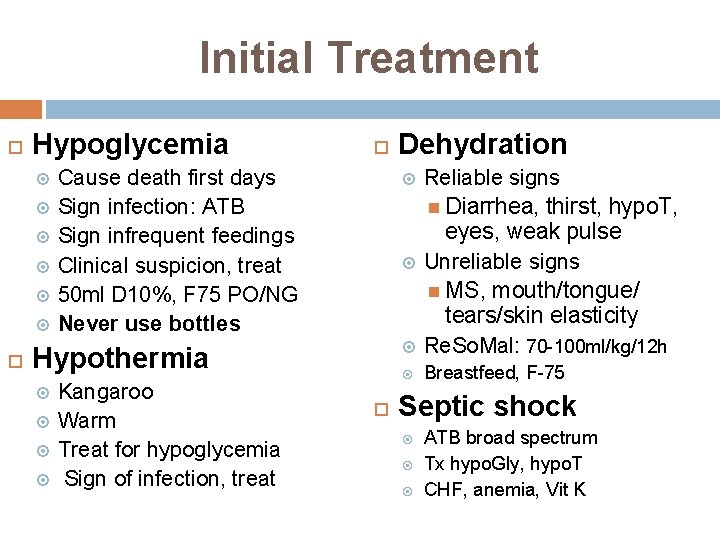
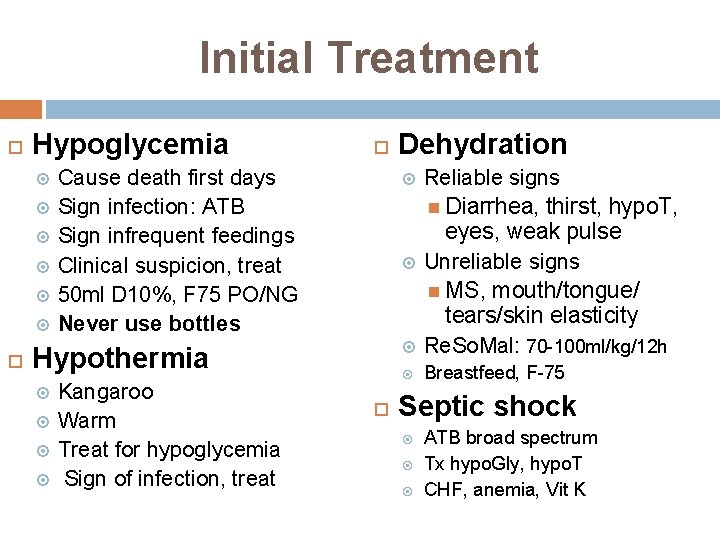
Initial Treatment Hypoglycemia Cause death first days Sign infection: ATB Sign infrequent feedings Clinical suspicion, treat 50 ml D 10%, F 75 PO/NG Never use bottles Kangaroo Warm Treat for hypoglycemia Sign of infection, treat Reliable signs Diarrhea, thirst, hypo. T, eyes, weak pulse Unreliable signs MS, mouth/tongue/ tears/skin elasticity Re. So. Mal: 70 -100 ml/kg/12 h Breastfeed, F-75 Hypothermia Dehydration Septic shock ATB broad spectrum Tx hypo. Gly, hypo. T CHF, anemia, Vit K
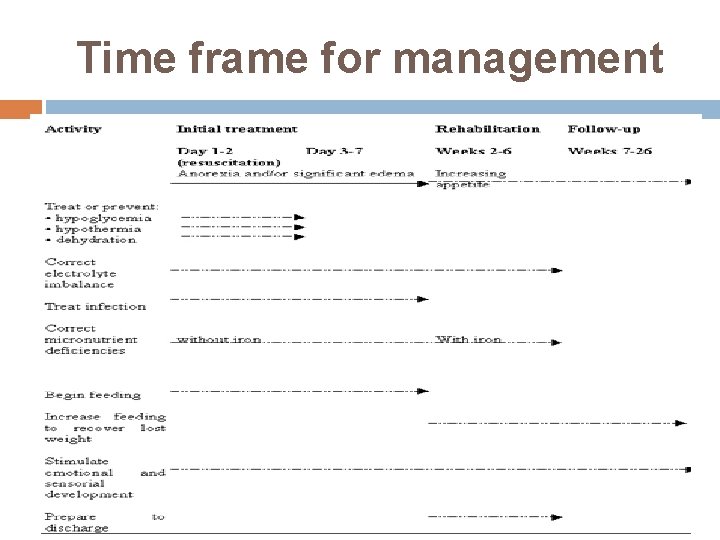
Time frame for management
Re. So. Mal Severely malnourished children K deficient, high Na levels Mg, Zn, copper deficiency Commercially available Dilute 1 packet of standard WHO ORS in 2 l water + 50 g of sucrose (25 g/l) + 40 ml (20 ml/l) mineral mix solution 5 ml/kg PO/NG q 30 min Cont till thirst & urine
Formula diets for severely malnourished children Impaired liver & intestinal function + infection Unable to tolerate usual amounts of dietary protein, fat, Na Diet low in above, hi in carbohydrates F-75 Food must be given in small amounts, frequently (PO/NG) 75 kcal or 315 kj/100 ml Initial phase treatment, 130 ml/kg/d Feed q 2 -3 hr (8 meals/d) F-100 100 kcal or 420 kj/100 ml Feed q 4 -5 h (5 -6 meals/d) Rehabilitation phase (appetite returned)
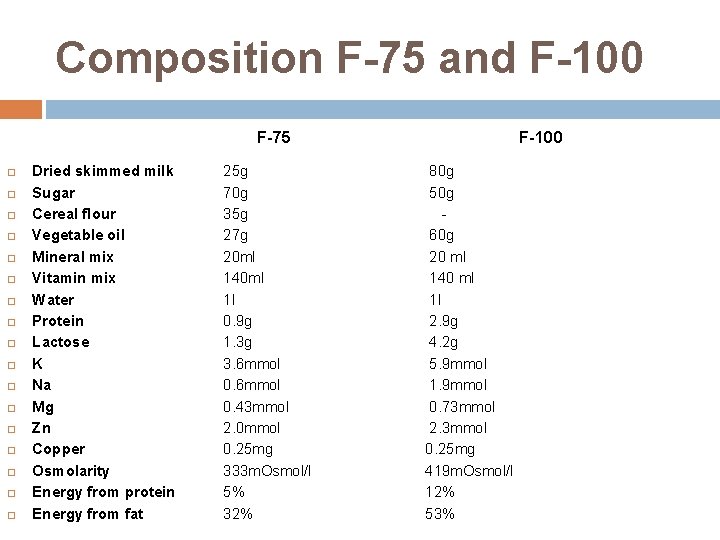
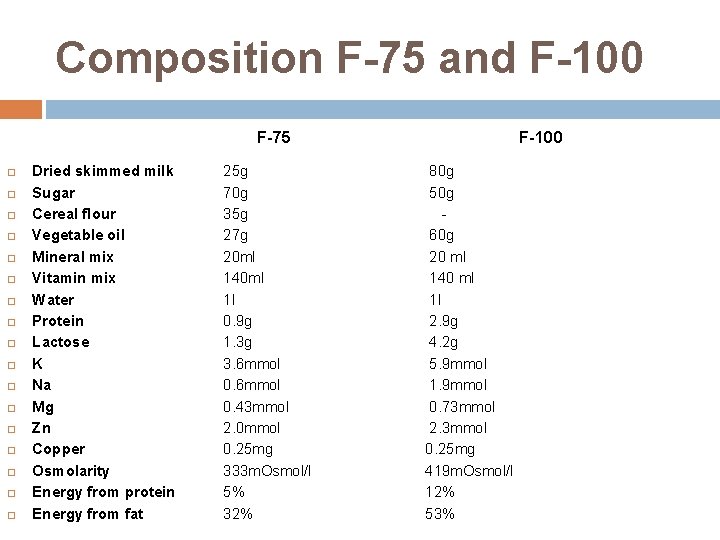
Composition F-75 and F-100 F-75 Dried skimmed milk Sugar Cereal flour Vegetable oil Mineral mix Vitamin mix Water Protein Lactose K Na Mg Zn Copper Osmolarity Energy from protein Energy from fat 25 g 70 g 35 g 27 g 20 ml 140 ml 1 l 0. 9 g 1. 3 g 3. 6 mmol 0. 43 mmol 2. 0 mmol 0. 25 mg 333 m. Osmol/l 5% 32% F-100 80 g 50 g 60 g 20 ml 140 ml 1 l 2. 9 g 4. 2 g 5. 9 mmol 1. 9 mmol 0. 73 mmol 2. 3 mmol 0. 25 mg 419 m. Osmol/l 12% 53%
Continue Breastfeeding
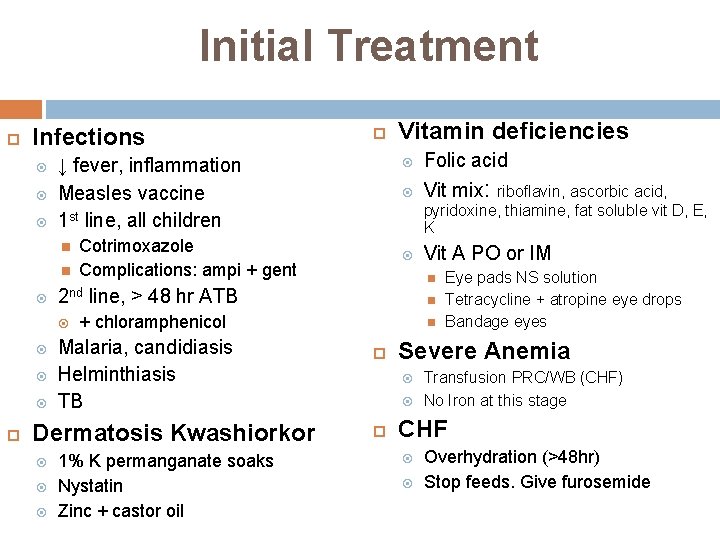
Initial Treatment Infections ↓ fever, inflammation Measles vaccine 1 st line, all children Cotrimoxazole Complications: ampi + gent Folic acid Vit mix: Vit A PO or IM Malaria, candidiasis Helminthiasis TB 1% K permanganate soaks Nystatin Zinc + castor oil riboflavin, ascorbic acid, pyridoxine, thiamine, fat soluble vit D, E, K + chloramphenicol Dermatosis Kwashiorkor Vitamin deficiencies 2 nd line, > 48 hr ATB Severe Anemia Eye pads NS solution Tetracycline + atropine eye drops Bandage eyes Transfusion PRC/WB (CHF) No Iron at this stage CHF Overhydration (>48 hr) Stop feeds. Give furosemide

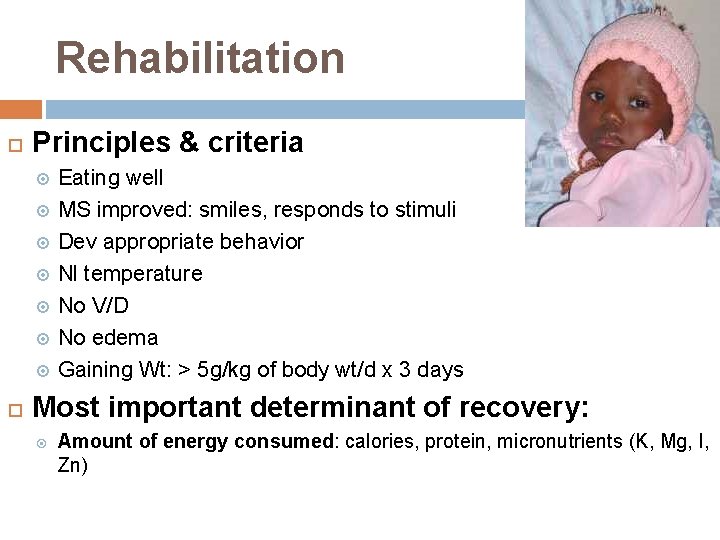
Rehabilitation Principles & criteria Eating well MS improved: smiles, responds to stimuli Dev appropriate behavior Nl temperature No V/D No edema Gaining Wt: > 5 g/kg of body wt/d x 3 days Most important determinant of recovery: Amount of energy consumed: calories, protein, micronutrients (K, Mg, I, Zn)
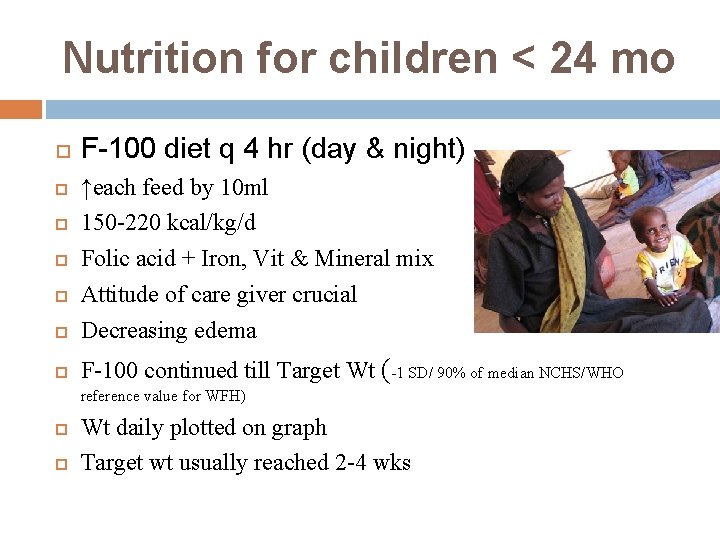
Nutrition for children < 24 mo F-100 diet q 4 hr (day & night) ↑each feed by 10 ml 150 -220 kcal/kg/d Folic acid + Iron, Vit & Mineral mix Attitude of care giver crucial Decreasing edema F-100 continued till Target Wt (-1 SD/ 90% of median NCHS/WHO reference value for WFH) Wt daily plotted on graph Target wt usually reached 2 -4 wks
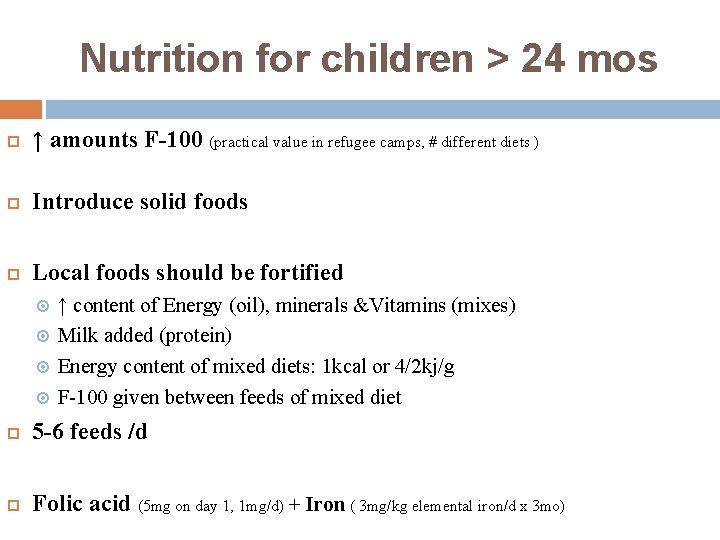
Nutrition for children > 24 mos ↑ amounts F-100 (practical value in refugee camps, # different diets ) Introduce solid foods Local foods should be fortified ↑ content of Energy (oil), minerals &Vitamins (mixes) Milk added (protein) Energy content of mixed diets: 1 kcal or 4/2 kj/g F-100 given between feeds of mixed diet 5 -6 feeds /d Folic acid (5 mg on day 1, 1 mg/d) + Iron ( 3 mg/kg elemental iron/d x 3 mo)
Emotional & physical stimulation 1 ary/2 ary prevention DD, MR, ED Start during rehabilitation Avoid sensory deprivation Maternal presence Environment Play activities, peer interactions Physical activities
Rehabilitation Parental teaching Correct feeding/food preparation practices, Stimulation, play, hygiene Treatment diarrhea, infections When to seek medical care Preparation for D/C Reintegration into family & community Prevent malnutrition recurrence
Criteria for D/C Child Mother WFH reached -1 SD Eating appropriate amount of diet that mother can prepare at home Gaining wt at normal or ↑rate Vit/mineral deficiencies treated/corrected Infections treated Full immunizations Able & willing to care for child Knows proper food preparation Knows appropriate toys & play for child Knows home treatment fever, diarrhea, ARI Health worker Able to ensure F/U child & support for mother
Follow up Child usually remains stunted w/ DD Prevention of recurrence severe malnutrition Strategy for tracing children F/U: 1, 2, 4 weeks, then 3 & 6 mos, then 2 x/yr till age 3 yrs WFH no less than -1 SD Assess overall health, feeding, play Immunizations, treatments, vitamin/minerals Record progress
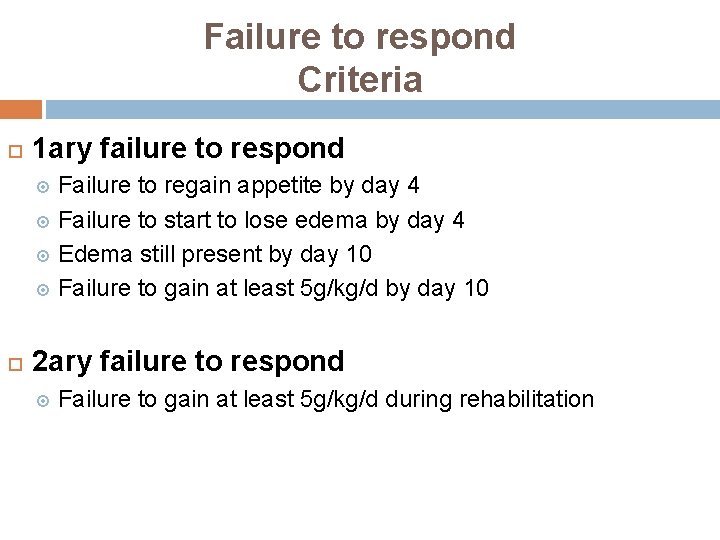
Failure to respond Criteria 1 ary failure to respond Failure to regain appetite by day 4 Failure to start to lose edema by day 4 Edema still present by day 10 Failure to gain at least 5 g/kg/d by day 10 2 ary failure to respond Failure to gain at least 5 g/kg/d during rehabilitation
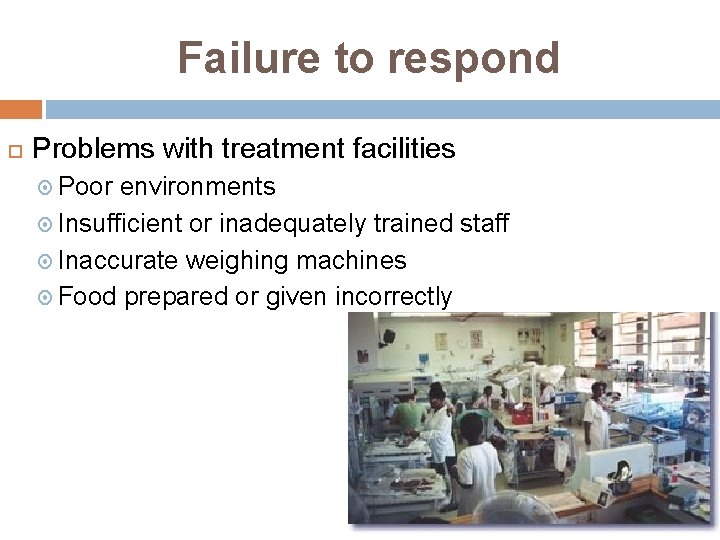
Failure to respond Problems with treatment facilities Poor environments Insufficient or inadequately trained staff Inaccurate weighing machines Food prepared or given incorrectly
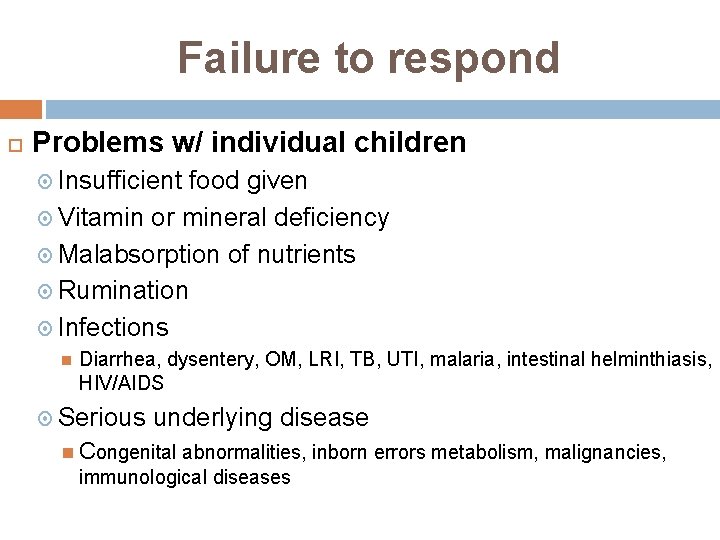
Failure to respond Problems w/ individual children Insufficient food given Vitamin or mineral deficiency Malabsorption of nutrients Rumination Infections Diarrhea, dysentery, OM, LRI, TB, UTI, malaria, intestinal helminthiasis, HIV/AIDS Serious underlying disease Congenital abnormalities, inborn errors metabolism, malignancies, immunological diseases
Fight Malnutrition