TREATING THE CERVICAL SPINE FOR HEADACHES CONCUSSION TMJ


- Slides: 37
TREATING THE CERVICAL SPINE FOR HEADACHES, CONCUSSION & TMJ Anne Keil PT, DPT In Motion Therapy August 8, 2020
*Objectives: *Understand the PT treatment based classification for the neck *Review the PT Clinical Practice Guideline for headaches *State the effect neck symptoms have in the PT Concussion CPG *Identify the contribution that neck treatment has to TMD *Identify postural taping techniques beneficial to the neck Anne Keil PT DPT In Motion Therapy August 8, 2020
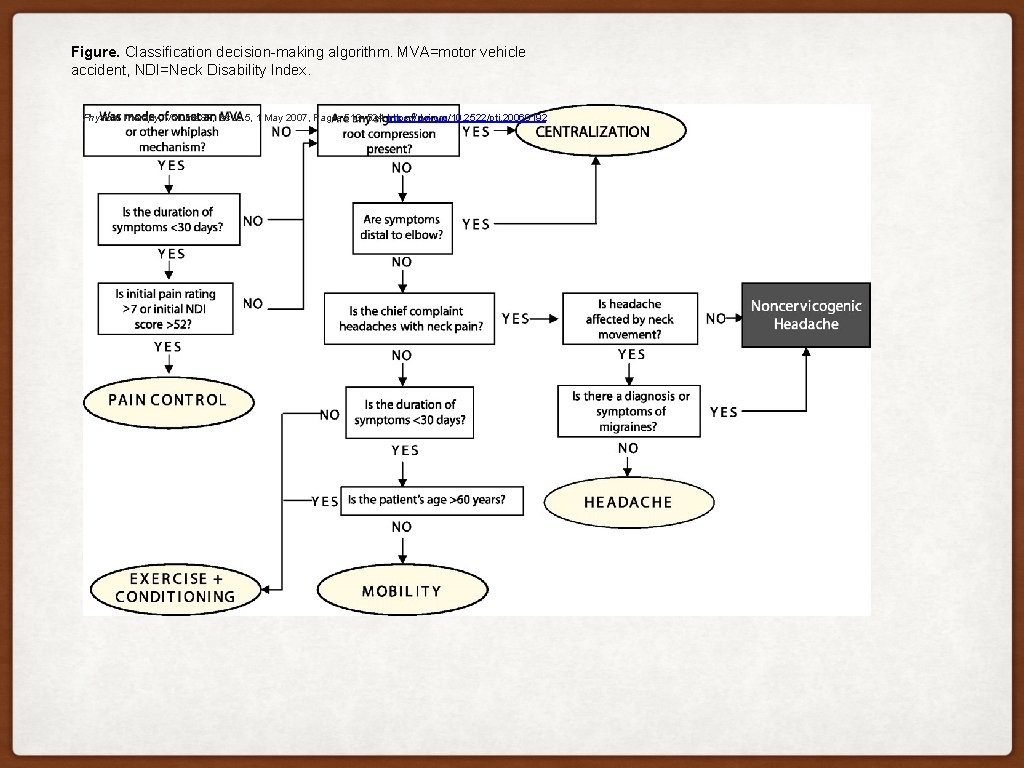
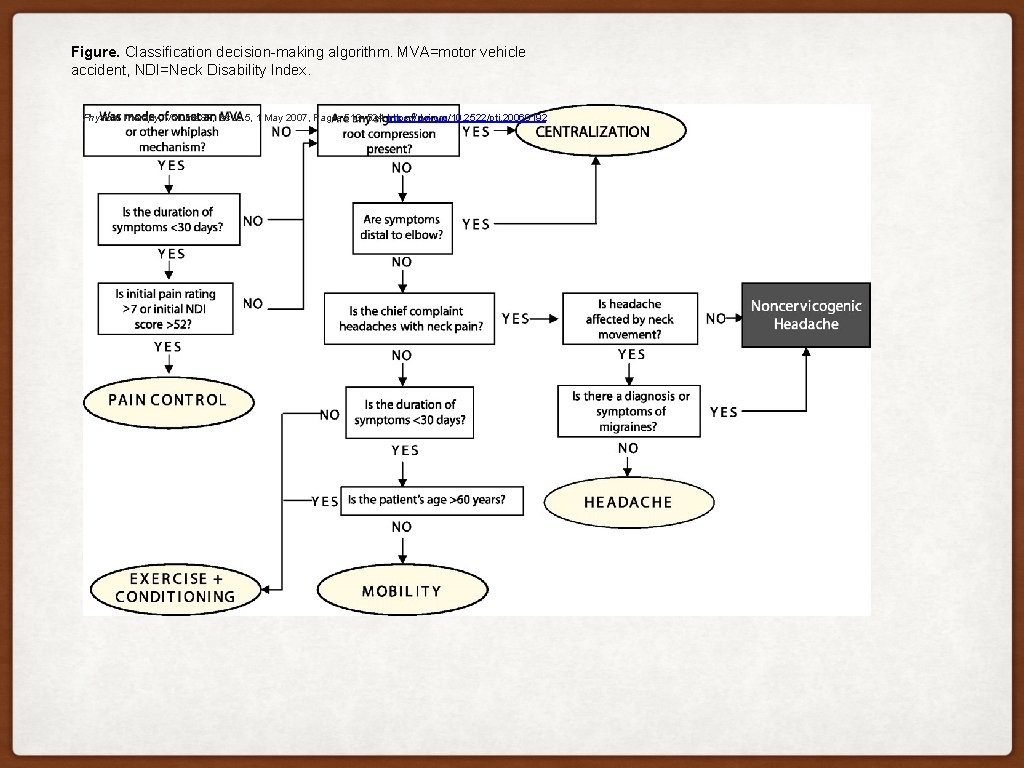
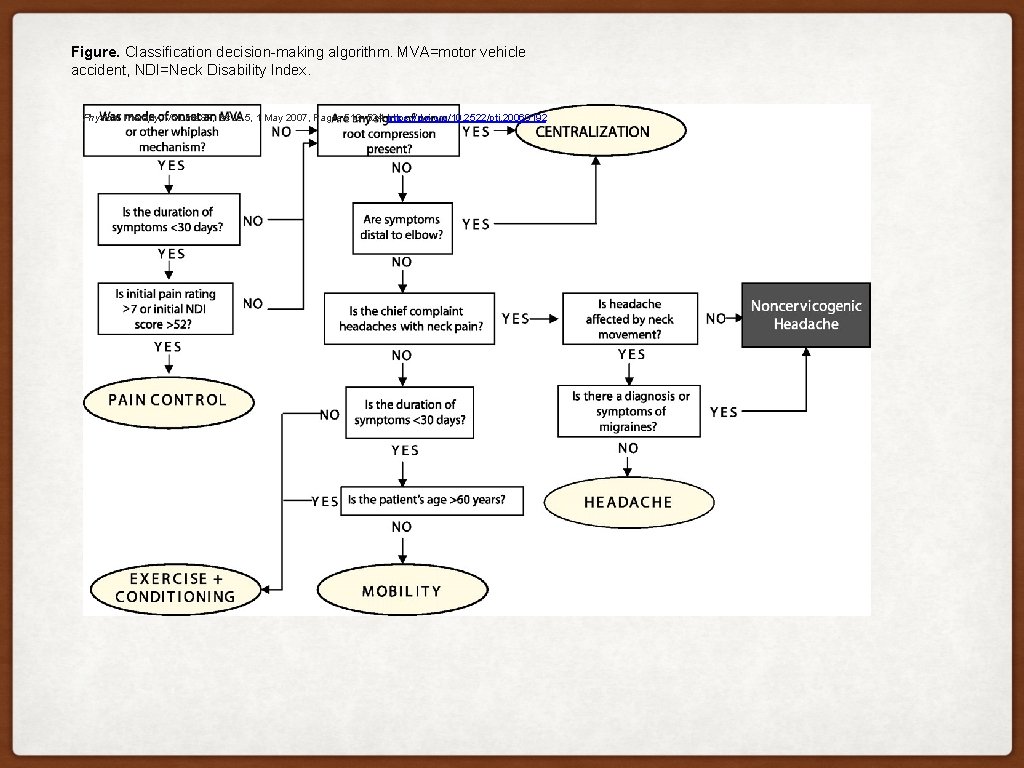
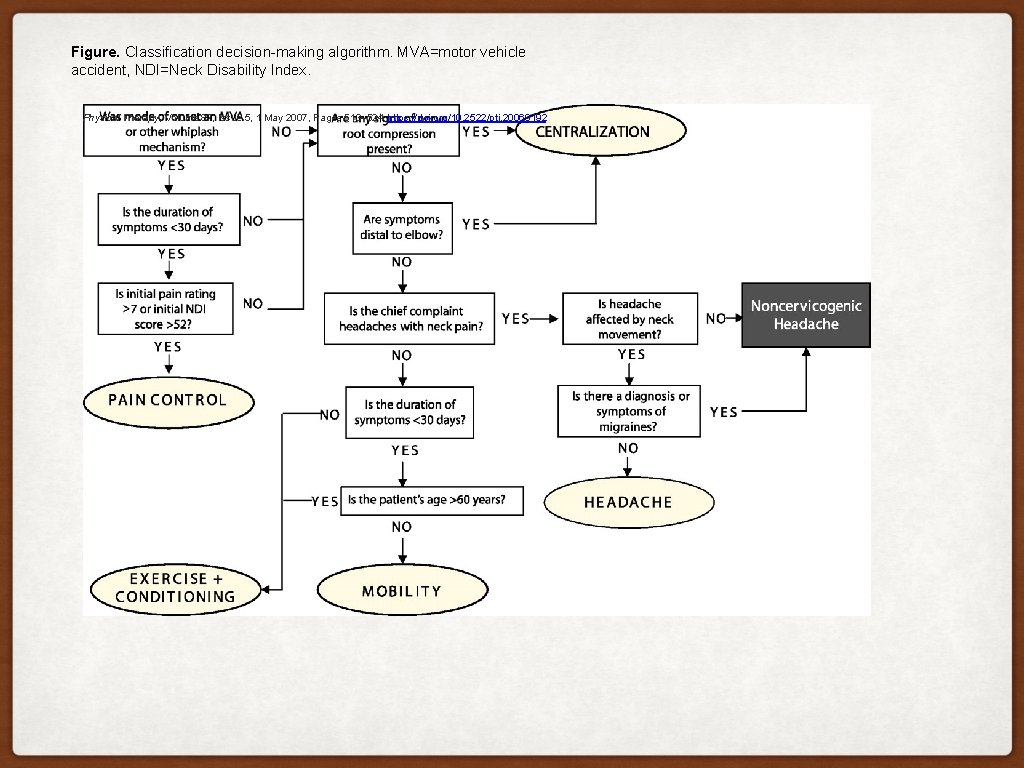
Figure. Classification decision-making algorithm. MVA=motor vehicle accident, NDI=Neck Disability Index. Physical Therapy, Volume 87, Issue 5, 1 May 2007, Pages 513– 524, https: //doi. org/10. 2522/ptj. 20060192
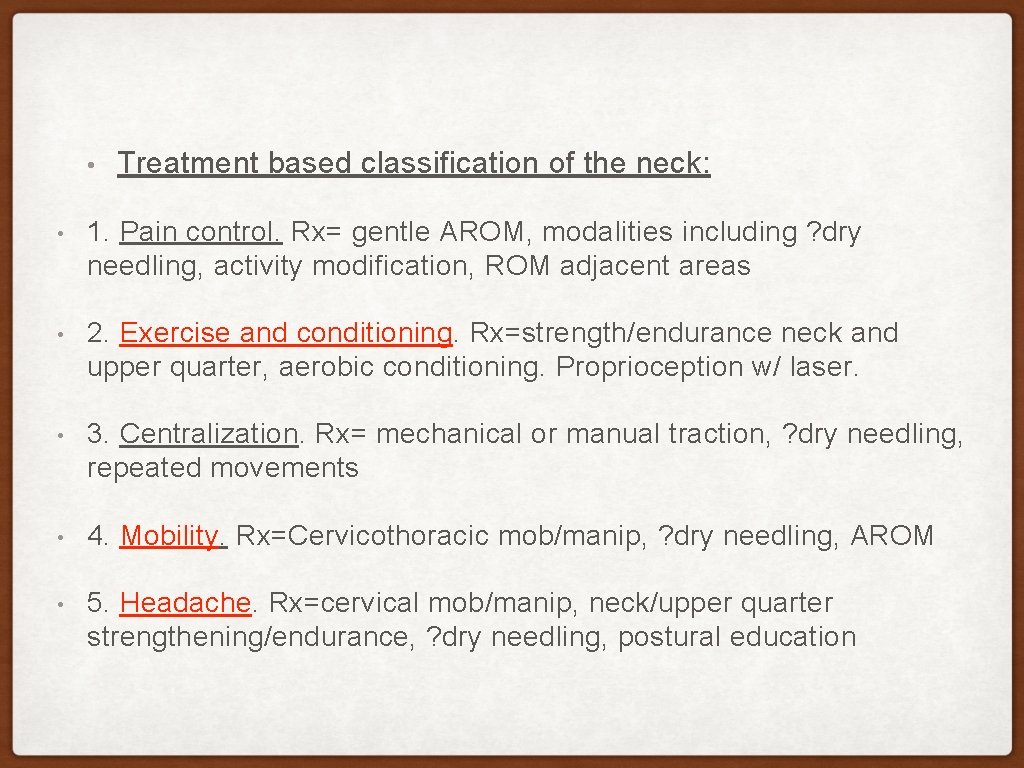
• Treatment based classification of the neck: • 1. Pain control. Rx= gentle AROM, modalities including ? dry needling, activity modification, ROM adjacent areas • 2. Exercise and conditioning. Rx=strength/endurance neck and upper quarter, aerobic conditioning • 3. Centralization. Rx= mechanical or manual traction (especially >age 55), ? dry needling, repeated movements, neural mobility • 4. Mobility. Rx=Cervicothoracic mob/manip, ? dry needling, AROM • 5. Headache. Rx=cervical mob/manip, neck/upper quarter strengthening/endurance, ? dry needling, postural education
1. THE CERVICAL SPINE AND ITS RELATIONSHIP TO HEADACHES
CERVICOGENIC HEADACHE: CLINICAL SUMMARY With cervicogenic headache, pain is referred to the head and/or face from the cervical spine. (Biondi, Bogduk) The pain is typically unilateral and starts in the cervical region. (Sjaastad et al) Headaches of cervical origin can share many common features with migraine and tension type headaches, making differential diagnosis a challenge. (Becker) When headaches are caused by dysfunction in the cervical spine, PTs play a critical role in the diagnosis and treatment of these patients.
PREVALENCE: CERVICOGENIC HEADACHE Prevalence of cervicogenic headache in the general population is estimated to be between 0. 4% and 2. 5%. Prevalence can reach as high as 20% in patients with chronic headache. (Biondi) Cervicogenic headache can be present in 54. 3% of persons with a cervical injury. (Haldman) 75% of persons with migraine headaches also fulfill criteria for Cervicogenic headache. (Haldman)
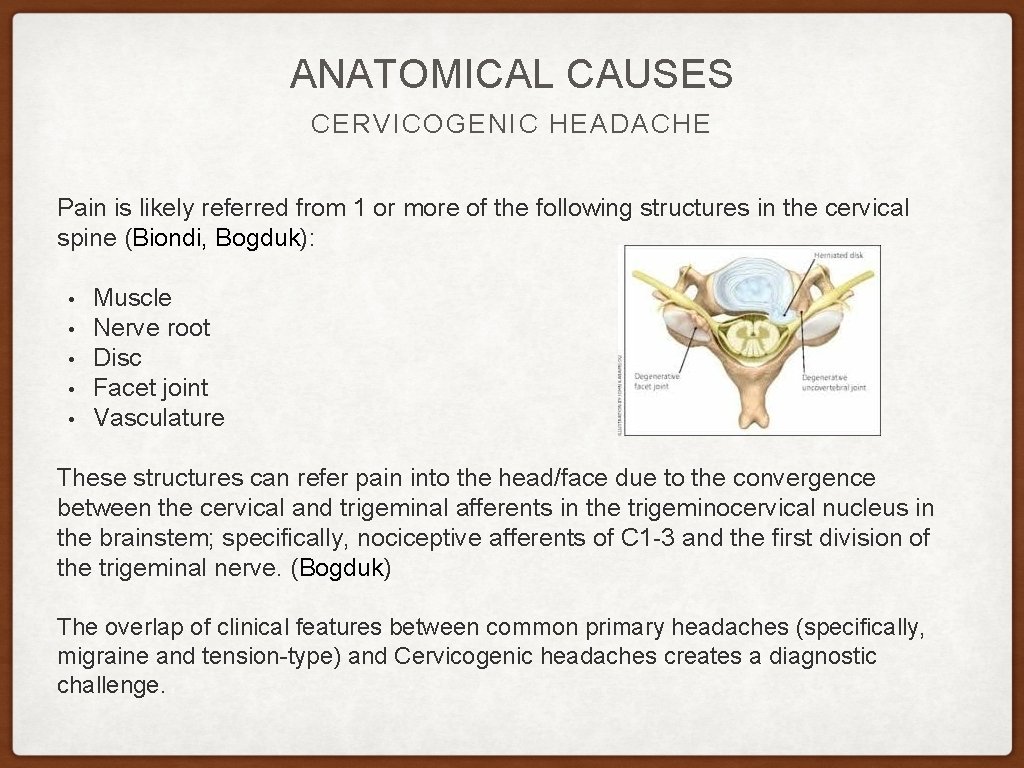
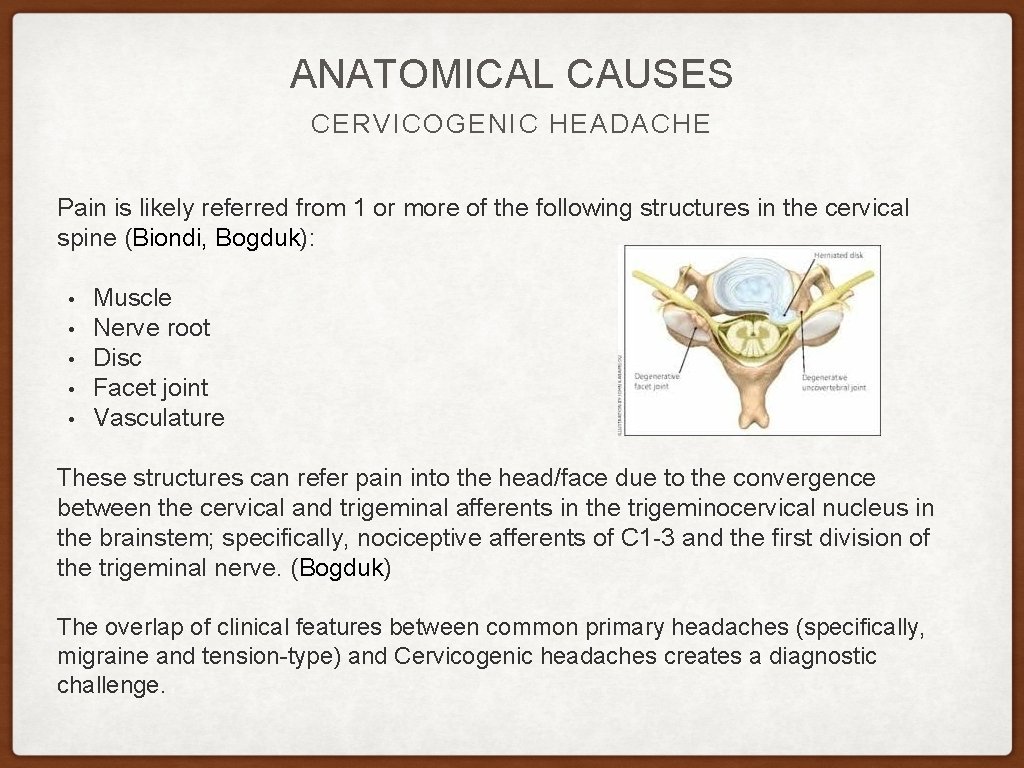
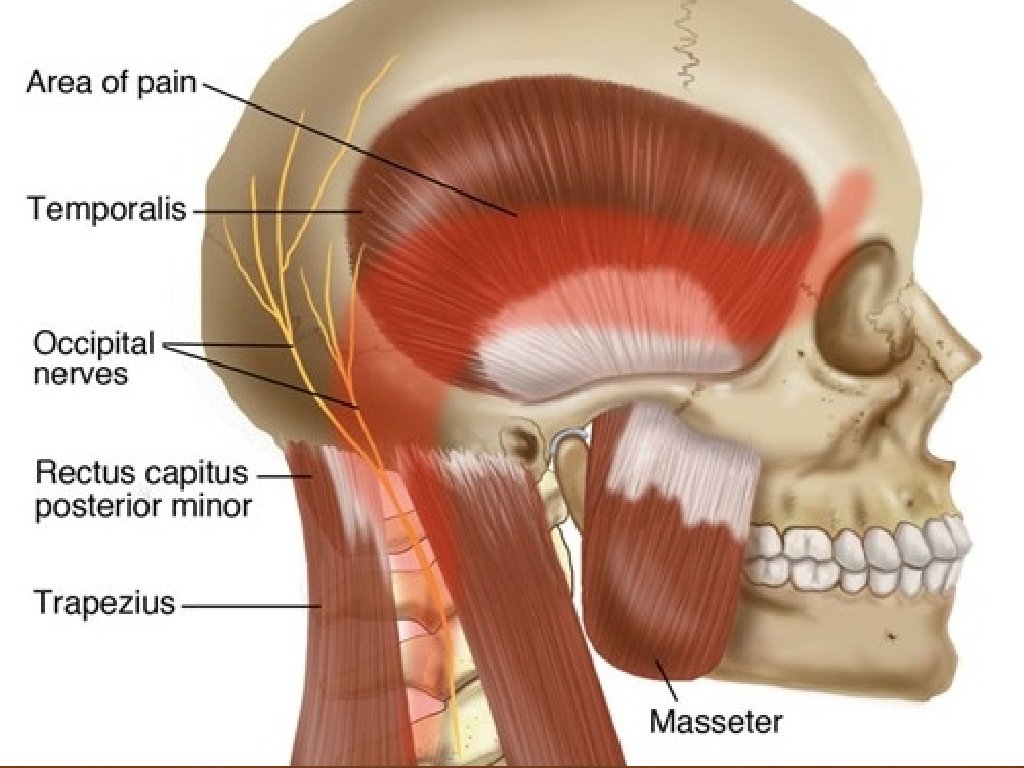
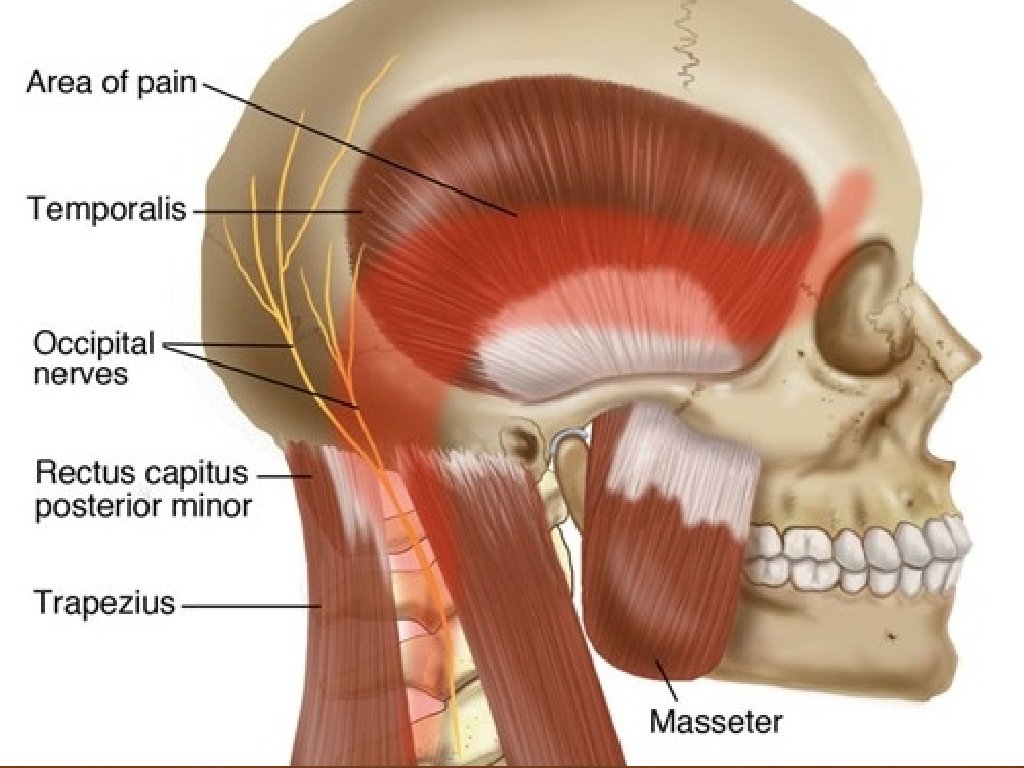
ANATOMICAL CAUSES CERVICOGENIC HEADACHE Pain is likely referred from 1 or more of the following structures in the cervical spine (Biondi, Bogduk): • • • Muscle Nerve root Disc Facet joint Vasculature These structures can refer pain into the head/face due to the convergence between the cervical and trigeminal afferents in the trigeminocervical nucleus in the brainstem; specifically, nociceptive afferents of C 1 -3 and the first division of the trigeminal nerve. (Bogduk) The overlap of clinical features between common primary headaches (specifically, migraine and tension-type) and Cervicogenic headaches creates a diagnostic challenge.
PRIMARY VS. SECONDARY HEADACHES Primary headaches • • • Are not associated with disease or structural neurologic abnormality Laboratory, imaging, physical, and neuro exams are generally normal Common diagnoses: migraine, tension-type headache, and cluster headaches Secondary headaches • • • Abnormal findings on clinical exam, imaging, and/or lab testing confirm diagnosis Headache attributed to: • Head and/or neck trauma • Cranial or cervical vascular disorder • Nonvascular intracranial disorder • A medication or its withdrawal • Ironically, medications used to treat HAs can cause medication-overuse • Headaches • Common medication-overuse headache causing meds include • ergotamines, triptans (both are migraine meds), analgesics, and opioids Infection Disorder of homeostasis Psychiatric disorder
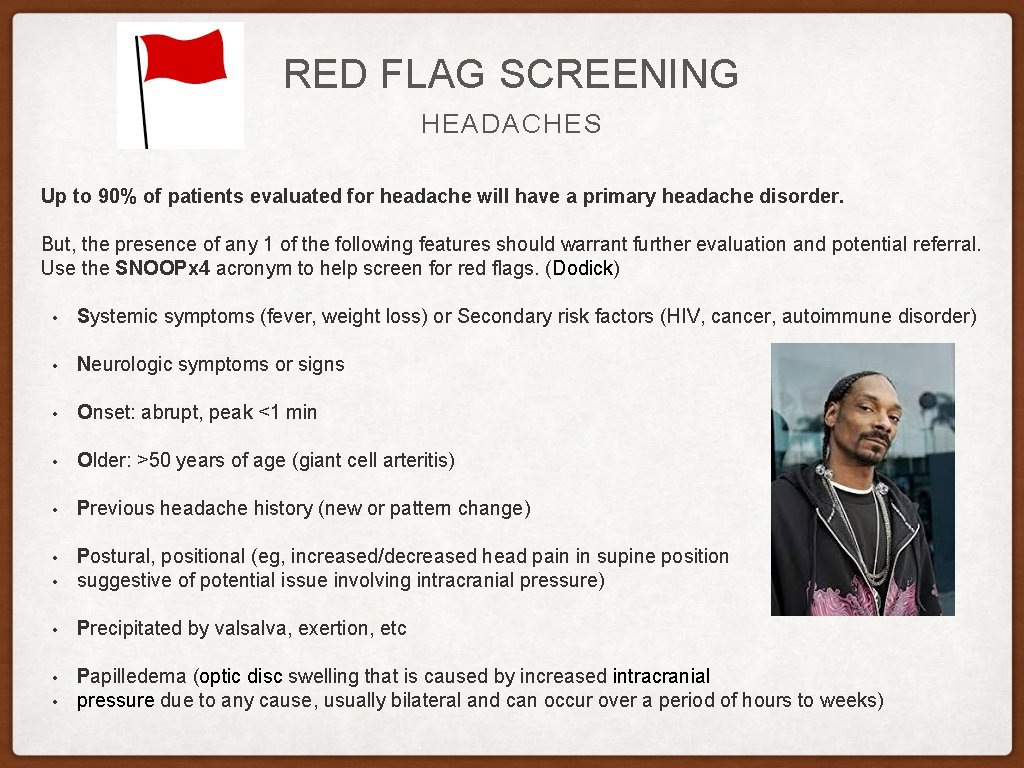
RED FLAG SCREENING HEADACHES Up to 90% of patients evaluated for headache will have a primary headache disorder. But, the presence of any 1 of the following features should warrant further evaluation and potential referral. Use the SNOOPx 4 acronym to help screen for red flags. (Dodick) • Systemic symptoms (fever, weight loss) or Secondary risk factors (HIV, cancer, autoimmune disorder) • Neurologic symptoms or signs • Onset: abrupt, peak <1 min • Older: >50 years of age (giant cell arteritis) • Previous headache history (new or pattern change) • • Postural, positional (eg, increased/decreased head pain in supine position suggestive of potential issue involving intracranial pressure) • Precipitated by valsalva, exertion, etc • Papilledema (optic disc swelling that is caused by increased intracranial pressure due to any cause, usually bilateral and can occur over a period of hours to weeks) •
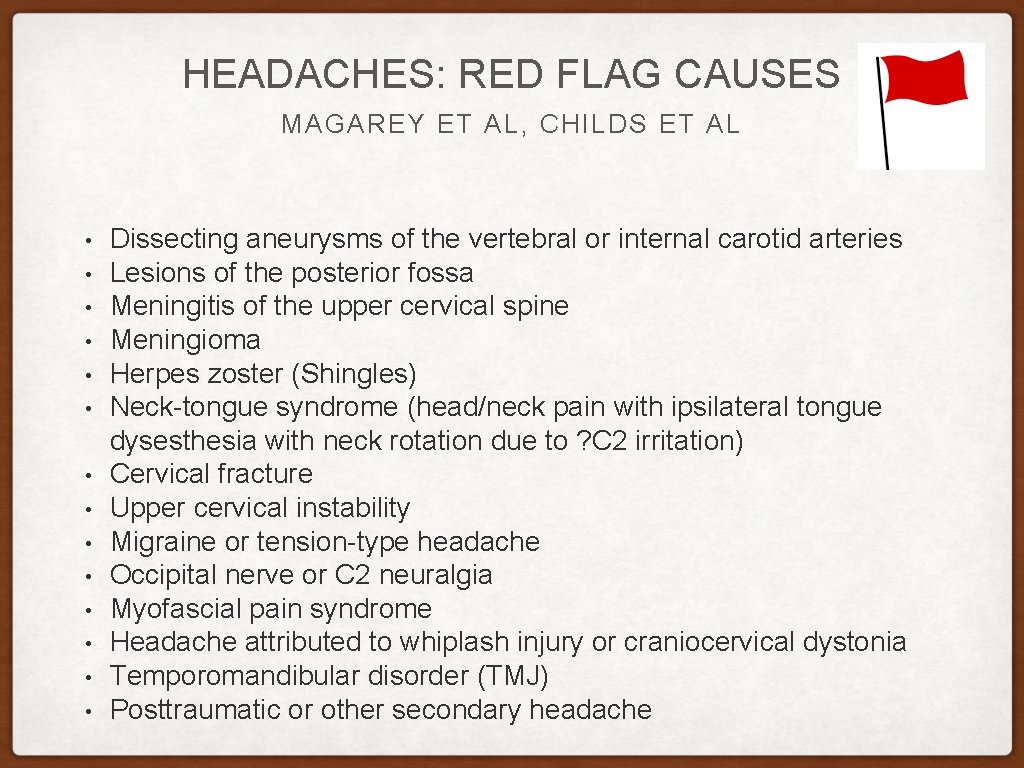
HEADACHES: RED FLAG CAUSES MAGAREY ET AL, CHILDS ET AL • • • • Dissecting aneurysms of the vertebral or internal carotid arteries Lesions of the posterior fossa Meningitis of the upper cervical spine Meningioma Herpes zoster (Shingles) Neck-tongue syndrome (head/neck pain with ipsilateral tongue dysesthesia with neck rotation due to ? C 2 irritation) Cervical fracture Upper cervical instability Migraine or tension-type headache Occipital nerve or C 2 neuralgia Myofascial pain syndrome Headache attributed to whiplash injury or craniocervical dystonia Temporomandibular disorder (TMJ) Posttraumatic or other secondary headache
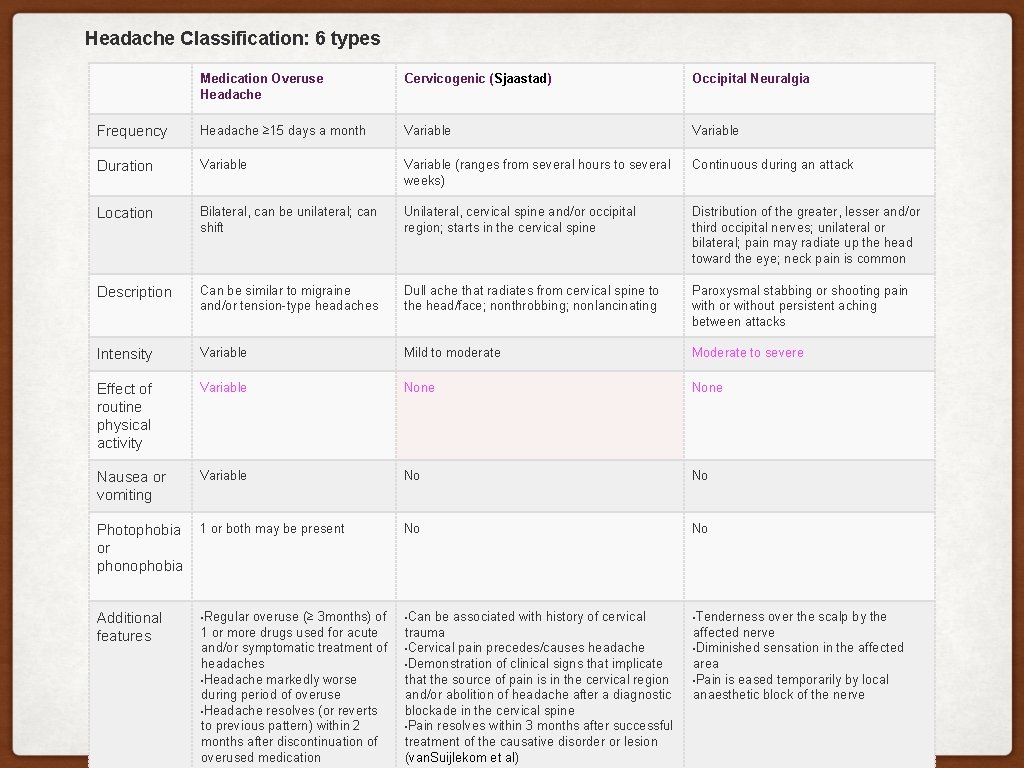
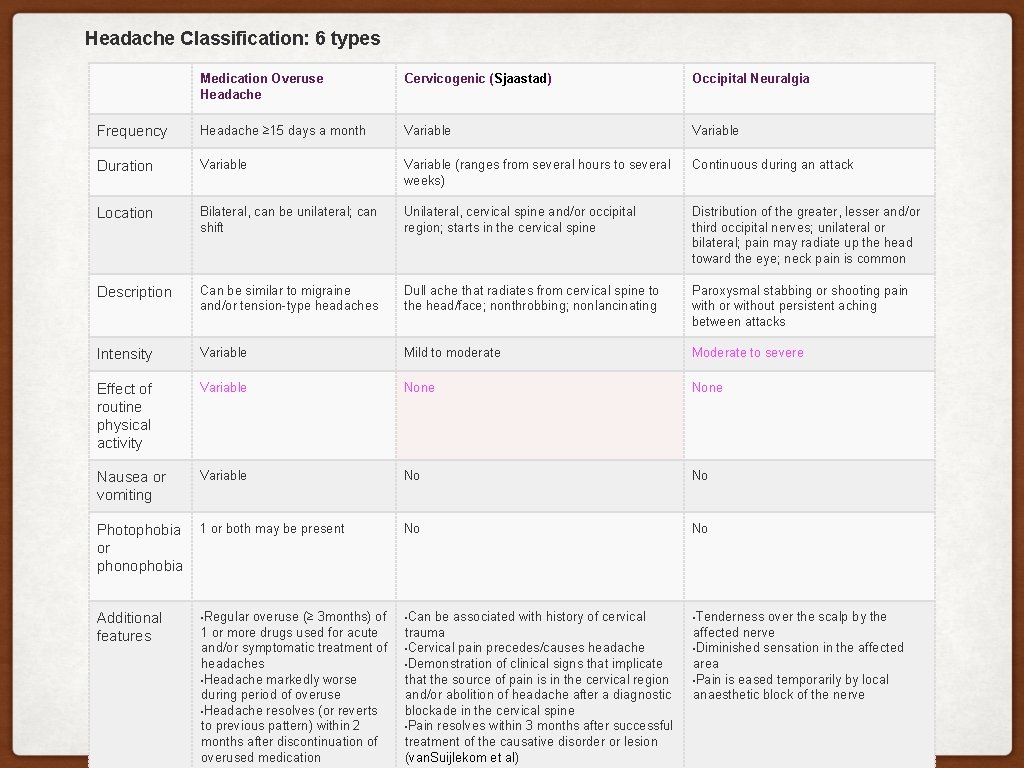
Headache Classification: 6 types Medication Overuse Headache Cervicogenic (Sjaastad) Occipital Neuralgia Frequency Headache ≥ 15 days a month Variable Duration Variable (ranges from several hours to several weeks) Continuous during an attack Location Bilateral, can be unilateral; can shift Unilateral, cervical spine and/or occipital region; starts in the cervical spine Distribution of the greater, lesser and/or third occipital nerves; unilateral or bilateral; pain may radiate up the head toward the eye; neck pain is common Description Can be similar to migraine and/or tension-type headaches Dull ache that radiates from cervical spine to the head/face; nonthrobbing; nonlancinating Paroxysmal stabbing or shooting pain with or without persistent aching between attacks Intensity Variable Mild to moderate Moderate to severe Effect of routine physical activity Variable None Nausea or vomiting Variable No No Photophobia 1 or both may be present or phonophobia No No • Regular overuse (≥ 3 months) of • Can be associated with history of cervical • Tenderness over the scalp by the 1 or more drugs used for acute and/or symptomatic treatment of headaches • Headache markedly worse during period of overuse • Headache resolves (or reverts to previous pattern) within 2 months after discontinuation of overused medication trauma • Cervical pain precedes/causes headache • Demonstration of clinical signs that implicate that the source of pain is in the cervical region and/or abolition of headache after a diagnostic blockade in the cervical spine • Pain resolves within 3 months after successful treatment of the causative disorder or lesion (van. Suijlekom et al) affected nerve • Diminished sensation in the affected area • Pain is eased temporarily by local anaesthetic block of the nerve Additional features
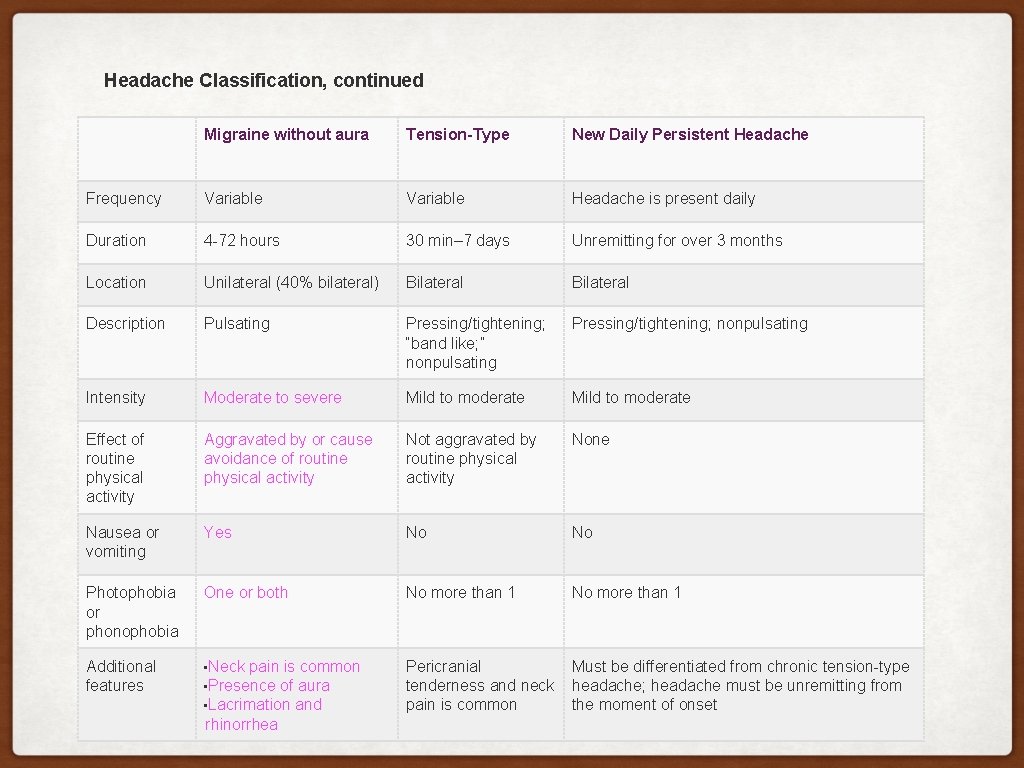
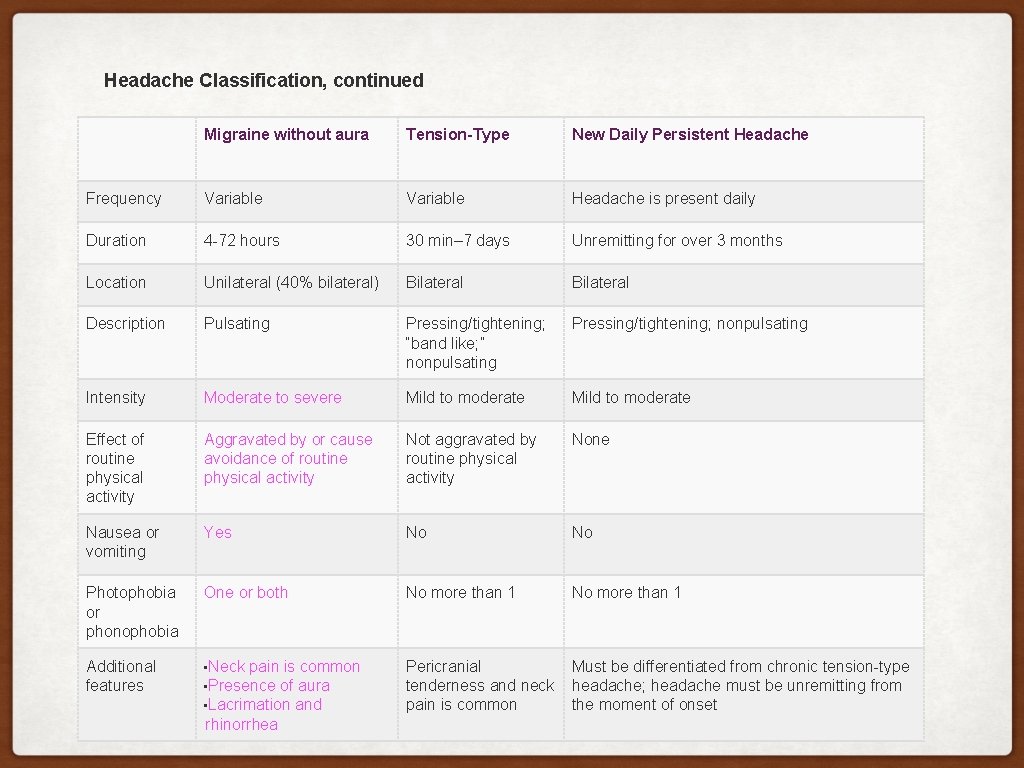
Headache Classification, continued Migraine without aura Tension-Type New Daily Persistent Headache Frequency Variable Headache is present daily Duration 4 -72 hours 30 min– 7 days Unremitting for over 3 months Location Unilateral (40% bilateral) Bilateral Description Pulsating Pressing/tightening; “band like; ” nonpulsating Pressing/tightening; nonpulsating Intensity Moderate to severe Mild to moderate Effect of routine physical activity Aggravated by or cause avoidance of routine physical activity Not aggravated by routine physical activity None Nausea or vomiting Yes No No Photophobia or phonophobia One or both No more than 1 Additional features • Neck pain is common Pericranial Must be differentiated from chronic tension-type tenderness and neck headache; headache must be unremitting from pain is common the moment of onset • Presence of aura • Lacrimation and rhinorrhea

CERVICAL EXAM CERVICOGENIC HEADACHE 1. Cervical spine AROM (Zito & Jull) • Findings typical= Decreased AROM into flexion and extension, AA rotation, cervical flexion-rotation test (Zito & Jull, • Ogince et al) 2. Cervical spine palpation: tight suboccipitals and facet joints C 1 -3 on the symptomatic side (Biondi, Bogduk, Sjaagstad) 3. Joint mobility assessment of upper cervical (C 0 -3): impaired mobility (Zito & Jull, Jull) 4. Deep neck flexor endurance testing (Zito & Jull, Jull). • The endurance test for the short neck flexors has been found to have acceptable reliability (de. Koning et al) • Patient is in a hook lying position with hands on the abdomen, cued to perform maximum craniocervical flexion • and maintain this while lifting the head/neck approximately 2. 5 cm off the table (Domenech et al). 10 mm Hg • Mean normative values = 39 sec for men and 29 sec for women (Domenech et al) 5. During muscle length testing, typically limited mobility of (Zito & Jull): • Upper trapezius • Levator scapulae • Scalenes • Suboccipital extensors • Pectoralis major and minor 6. Manual muscle testing (Jull): • Lower and middle trapezius • Serratus anterior • Anterior and posterior cervical spine
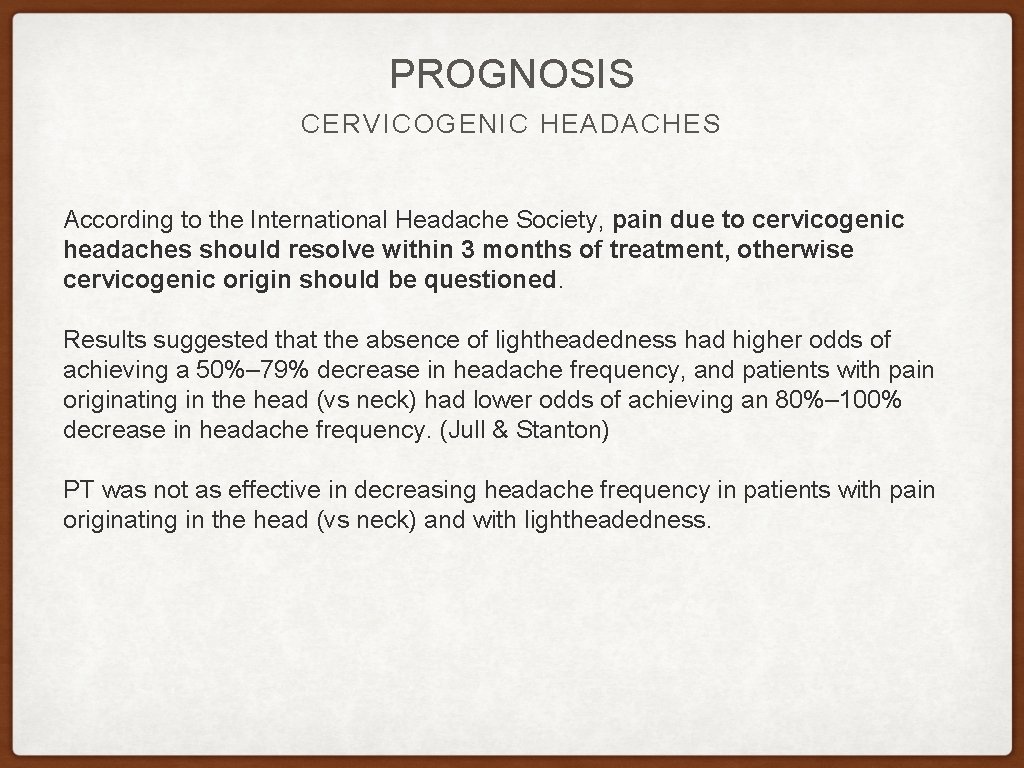
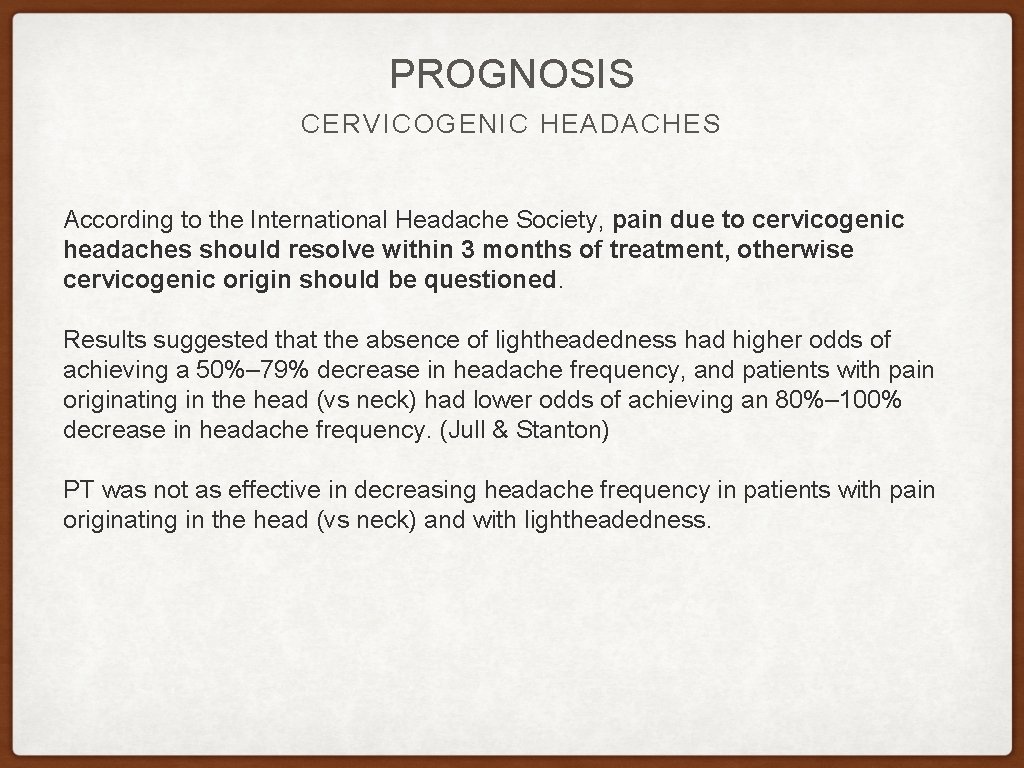
PROGNOSIS CERVICOGENIC HEADACHES According to the International Headache Society, pain due to cervicogenic headaches should resolve within 3 months of treatment, otherwise cervicogenic origin should be questioned. Results suggested that the absence of lightheadedness had higher odds of achieving a 50%– 79% decrease in headache frequency, and patients with pain originating in the head (vs neck) had lower odds of achieving an 80%– 100% decrease in headache frequency. (Jull & Stanton) PT was not as effective in decreasing headache frequency in patients with pain originating in the head (vs neck) and with lightheadedness.
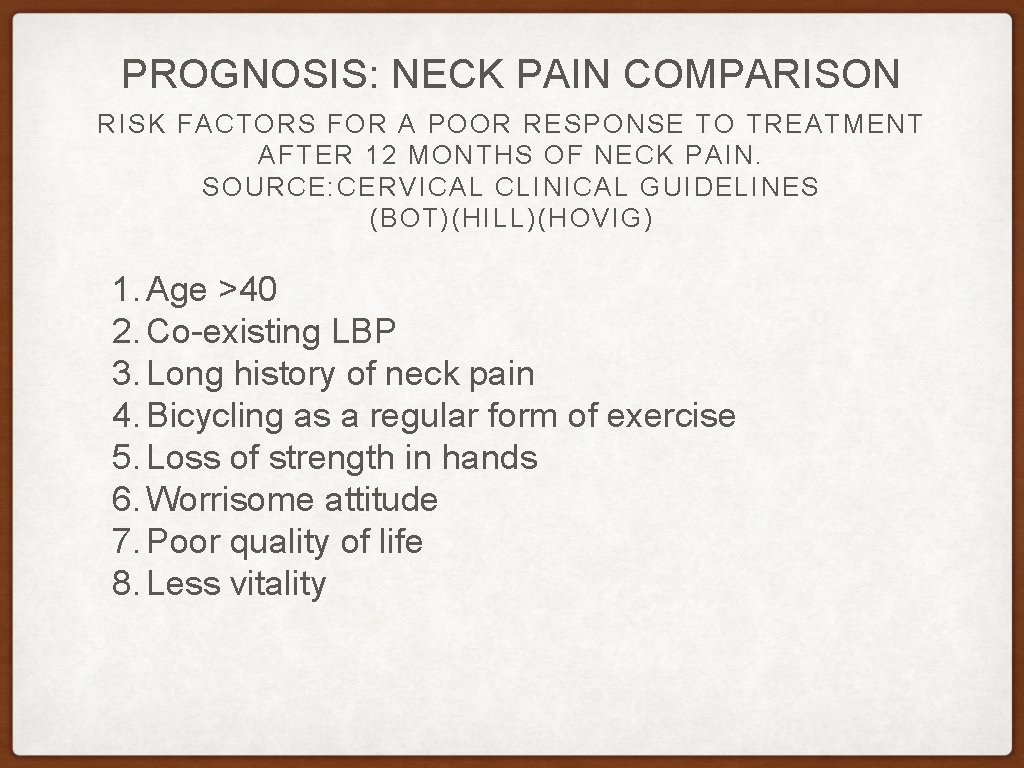
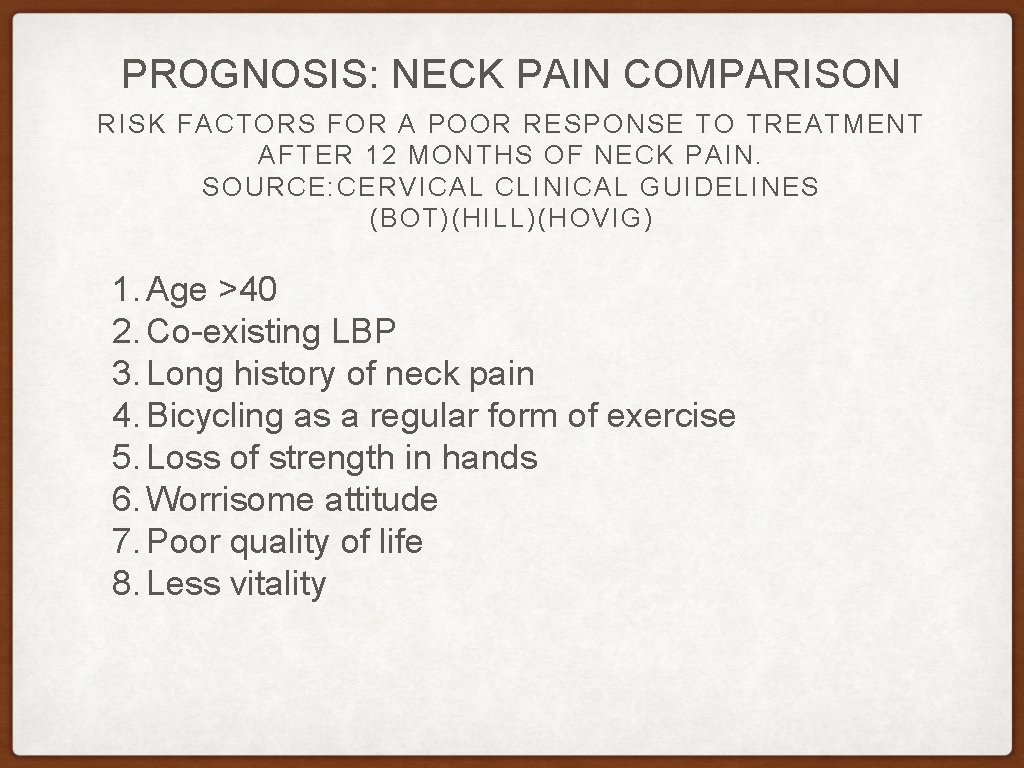
PROGNOSIS: NECK PAIN COMPARISON RISK FACTORS FOR A POOR RESPONSE TO TREATMENT AFTER 12 MONTHS OF NECK PAIN. SOURCE: CERVICAL CLINICAL GUIDELINES (BOT)(HILL)(HOVIG) 1. Age >40 2. Co-existing LBP 3. Long history of neck pain 4. Bicycling as a regular form of exercise 5. Loss of strength in hands 6. Worrisome attitude 7. Poor quality of life 8. Less vitality

CERVICOGENIC HEADACHE TREATMENT: FOLLOW TREATMENT BASED CLASSIFICATION Racicki et al’s systematic review assessed the effectiveness of PT treatment for cervicogenic headache found 6 randomized controlled trials of good quality. Interventions included cervical mobilization/manipulati Exercise alone was found to reduce the frequency of headaches. Similarly, cervical spine mobilization and manipulation decreased the frequency and intensity of headaches, but a combination of cervical mobil duration. (Racicki et al) This suggests implementing a combination of cervical/thoracic spine manual therapy and exercise. Focus: deep neck flexor, serratus anterior and lower trapezius endurance training.
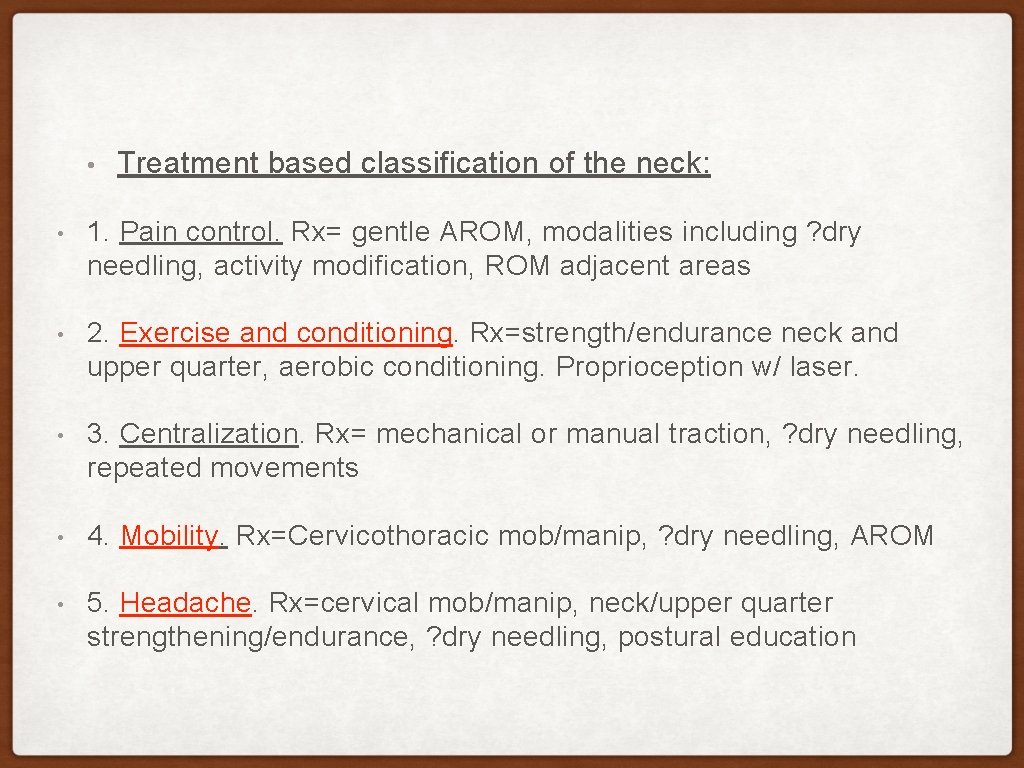
• Treatment based classification of the neck: • 1. Pain control. Rx= gentle AROM, modalities including ? dry needling, activity modification, ROM adjacent areas • 2. Exercise and conditioning. Rx=strength/endurance neck and upper quarter, aerobic conditioning. Proprioception w/ laser. • 3. Centralization. Rx= mechanical or manual traction, ? dry needling, repeated movements • 4. Mobility. Rx=Cervicothoracic mob/manip, ? dry needling, AROM • 5. Headache. Rx=cervical mob/manip, neck/upper quarter strengthening/endurance, ? dry needling, postural education
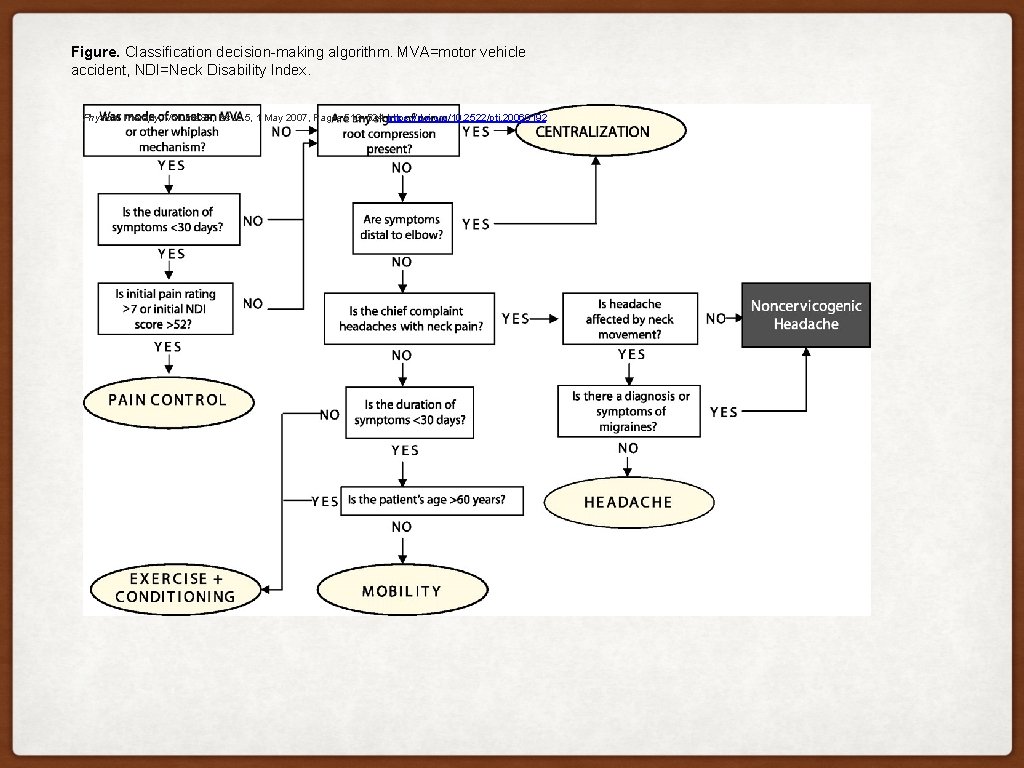
Figure. Classification decision-making algorithm. MVA=motor vehicle accident, NDI=Neck Disability Index. Physical Therapy, Volume 87, Issue 5, 1 May 2007, Pages 513– 524, https: //doi. org/10. 2522/ptj. 20060192
2. CERVICAL SPINE AND CONCUSSION
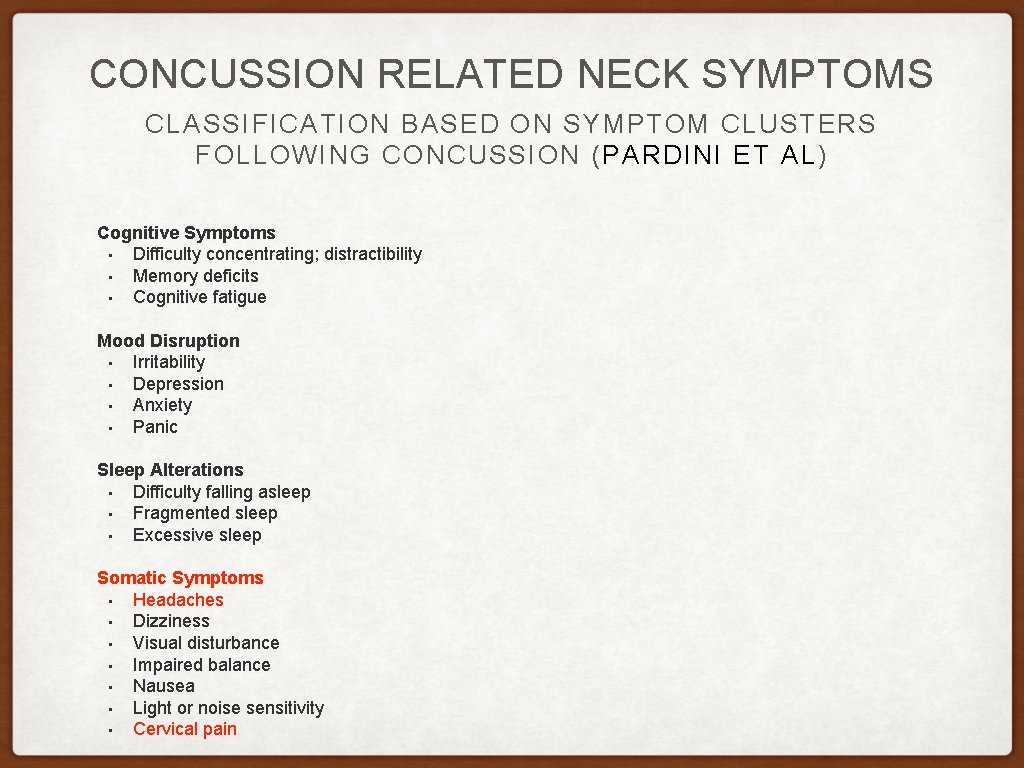
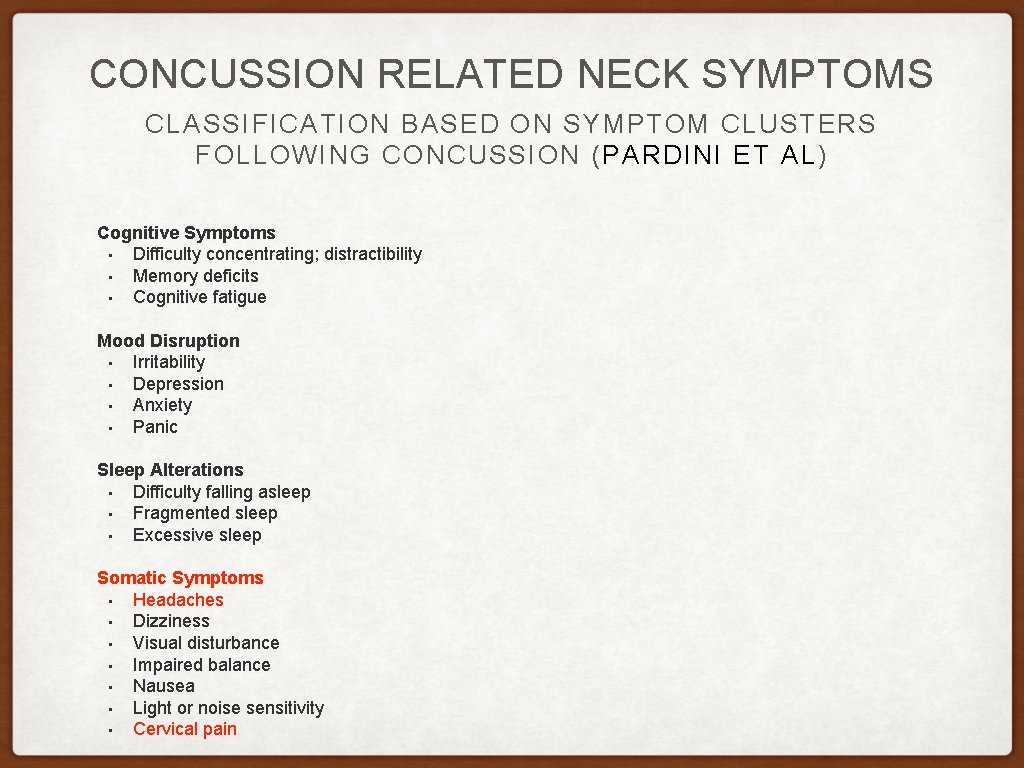
CONCUSSION RELATED NECK SYMPTOMS CLASSIFICATION BASED ON SYMPTOM CLUSTERS FOLLOWING CONCUSSION ( PARDINI ET AL) Cognitive Symptoms • Difficulty concentrating; distractibility • Memory deficits • Cognitive fatigue Mood Disruption • Irritability • Depression • Anxiety • Panic Sleep Alterations • Difficulty falling asleep • Fragmented sleep • Excessive sleep Somatic Symptoms • Headaches • Dizziness • Visual disturbance • Impaired balance • Nausea • Light or noise sensitivity • Cervical pain
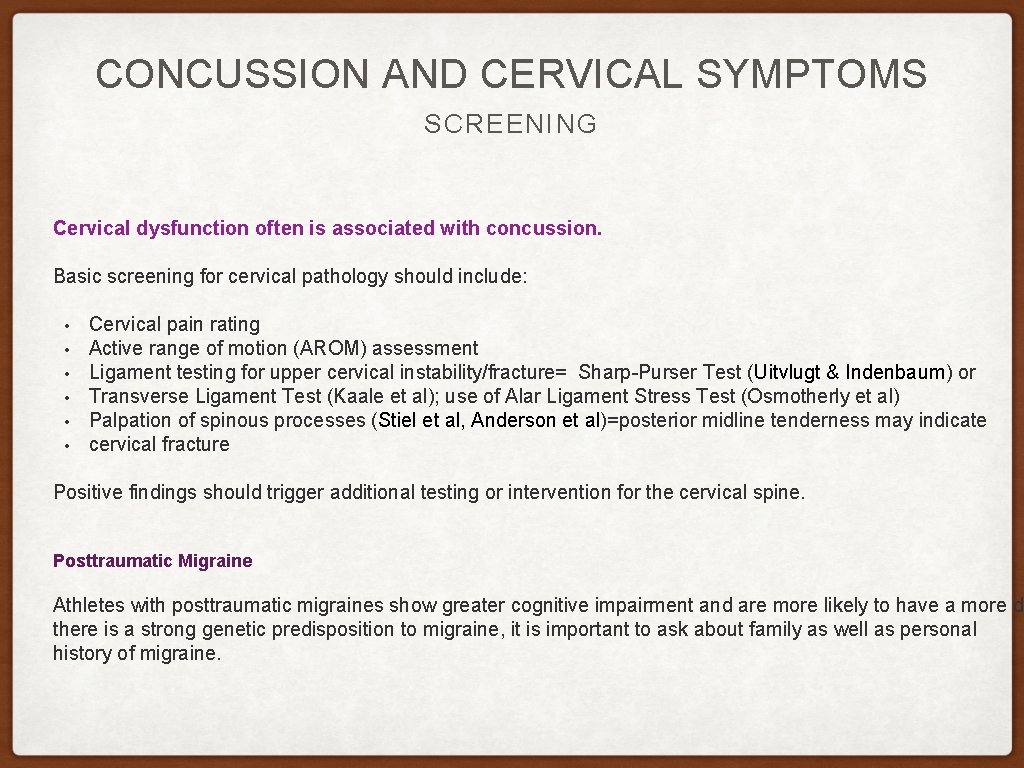
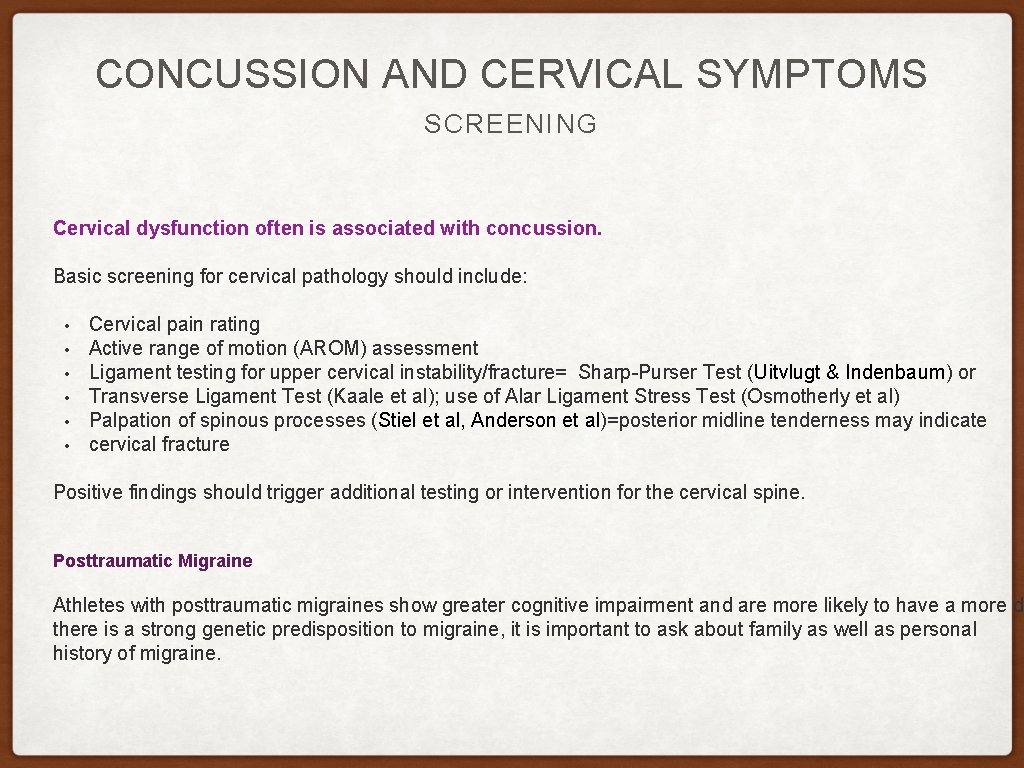
CONCUSSION AND CERVICAL SYMPTOMS SCREENING Cervical dysfunction often is associated with concussion. Basic screening for cervical pathology should include: • • • Cervical pain rating Active range of motion (AROM) assessment Ligament testing for upper cervical instability/fracture= Sharp-Purser Test (Uitvlugt & Indenbaum) or Transverse Ligament Test (Kaale et al); use of Alar Ligament Stress Test (Osmotherly et al) Palpation of spinous processes (Stiel et al, Anderson et al)=posterior midline tenderness may indicate cervical fracture Positive findings should trigger additional testing or intervention for the cervical spine. Posttraumatic Migraine Athletes with posttraumatic migraines show greater cognitive impairment and are more likely to have a more de there is a strong genetic predisposition to migraine, it is important to ask about family as well as personal history of migraine.
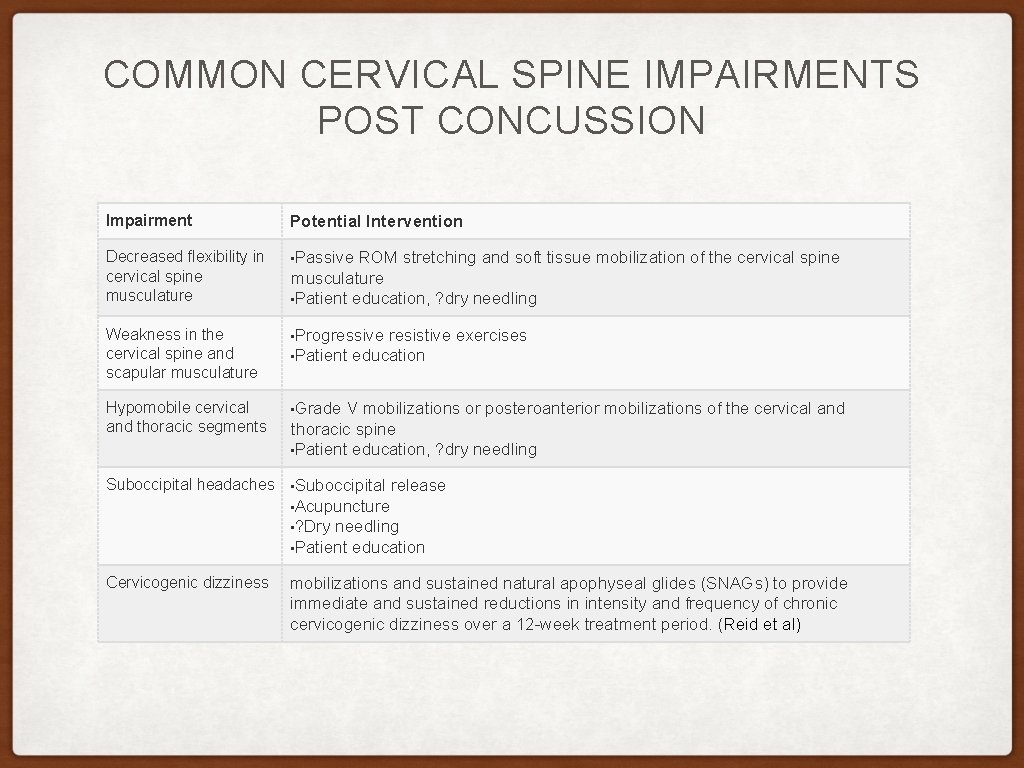
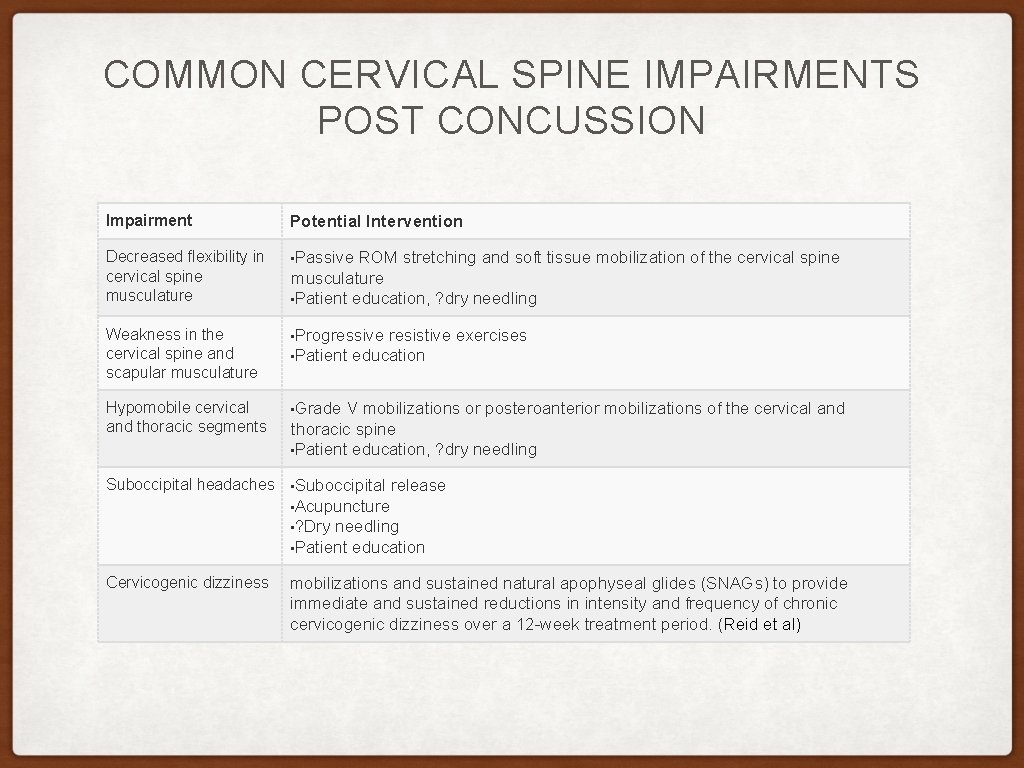
COMMON CERVICAL SPINE IMPAIRMENTS POST CONCUSSION Impairment Potential Intervention Decreased flexibility in cervical spine musculature • Passive ROM stretching and soft tissue mobilization of the cervical spine Weakness in the cervical spine and scapular musculature • Progressive resistive exercises Hypomobile cervical and thoracic segments • Grade V mobilizations or posteroanterior mobilizations of the cervical and musculature • Patient education, ? dry needling • Patient education thoracic spine • Patient education, ? dry needling Suboccipital headaches • Suboccipital release • Acupuncture • ? Dry needling • Patient education Cervicogenic dizziness mobilizations and sustained natural apophyseal glides (SNAGs) to provide immediate and sustained reductions in intensity and frequency of chronic cervicogenic dizziness over a 12 -week treatment period. (Reid et al)
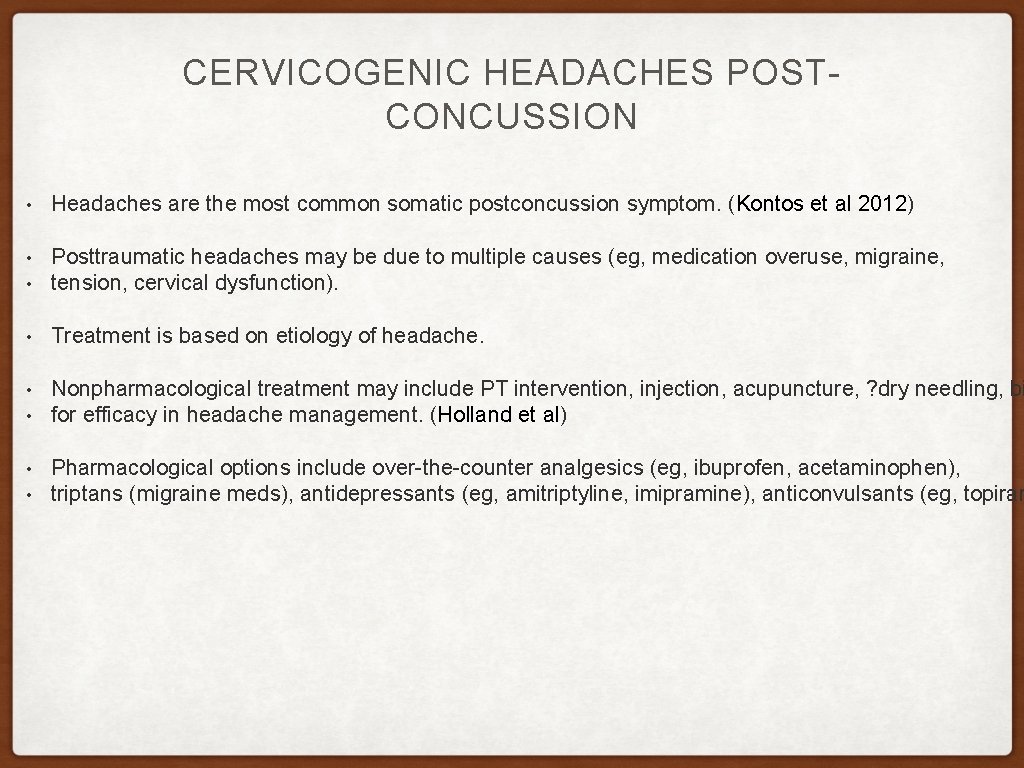
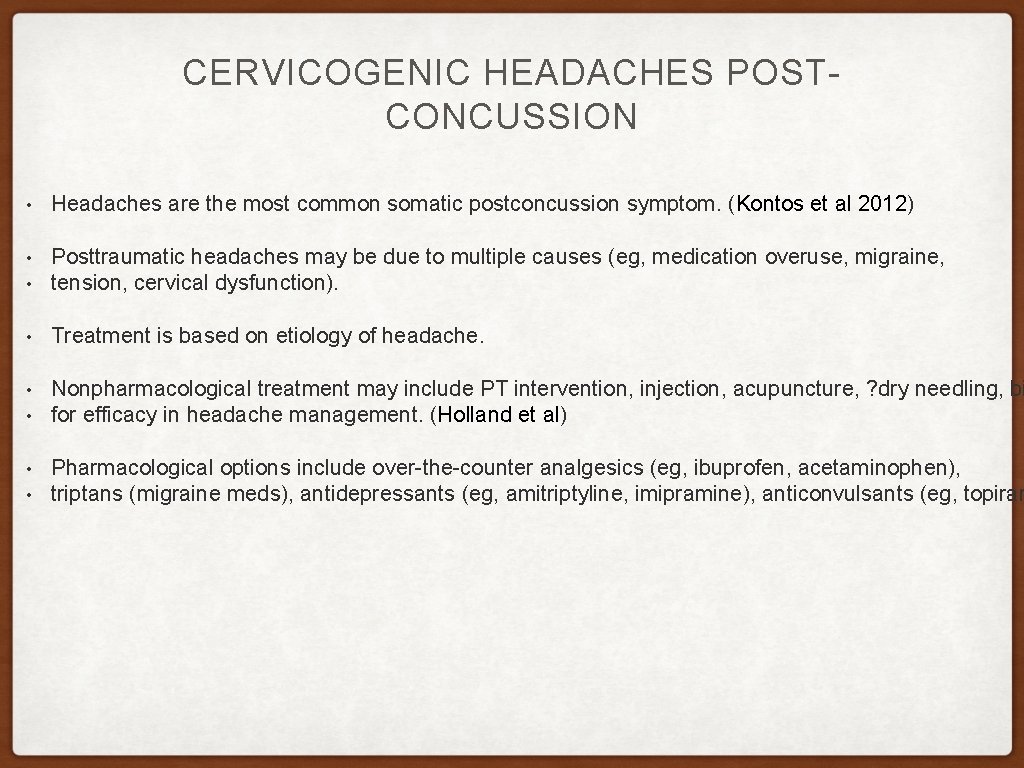
CERVICOGENIC HEADACHES POSTCONCUSSION • Headaches are the most common somatic postconcussion symptom. (Kontos et al 2012) • • Posttraumatic headaches may be due to multiple causes (eg, medication overuse, migraine, tension, cervical dysfunction). • Treatment is based on etiology of headache. • Nonpharmacological treatment may include PT intervention, injection, acupuncture, ? dry needling, bi for efficacy in headache management. (Holland et al) • • • Pharmacological options include over-the-counter analgesics (eg, ibuprofen, acetaminophen), triptans (migraine meds), antidepressants (eg, amitriptyline, imipramine), anticonvulsants (eg, topiram
3. CERVICAL SPINE AND TEMPOROMANDIBULAR DISORDERS
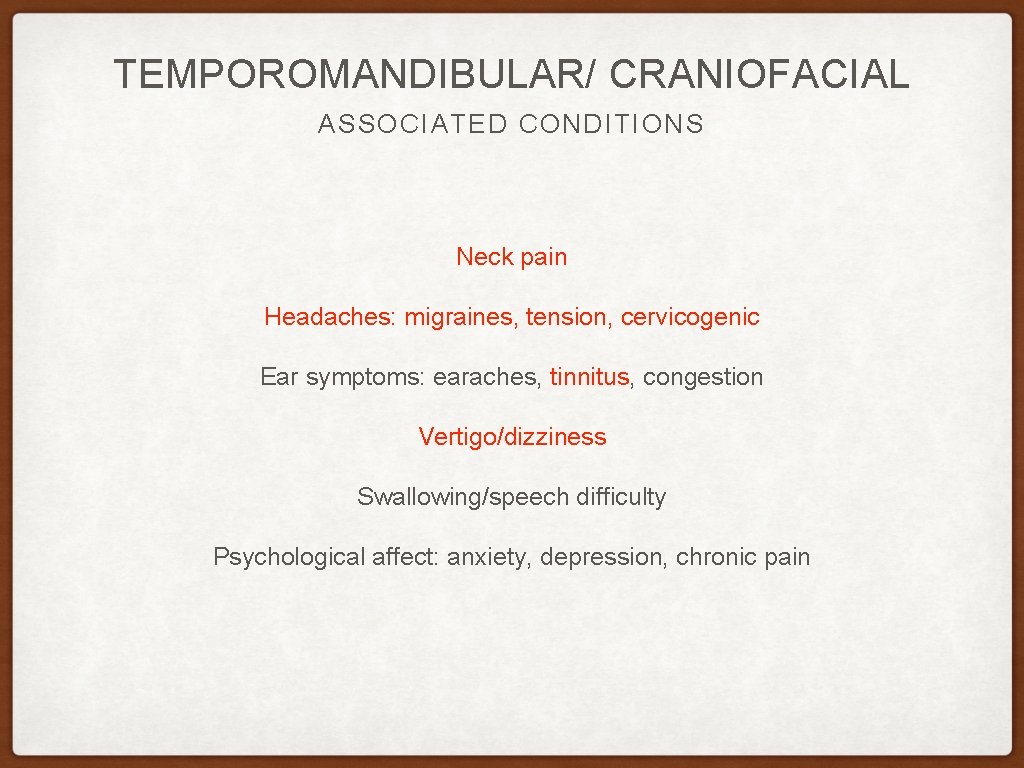
TEMPOROMANDIBULAR/ CRANIOFACIAL ASSOCIATED CONDITIONS Neck pain Headaches: migraines, tension, cervicogenic Ear symptoms: earaches, tinnitus, congestion Vertigo/dizziness Swallowing/speech difficulty Psychological affect: anxiety, depression, chronic pain
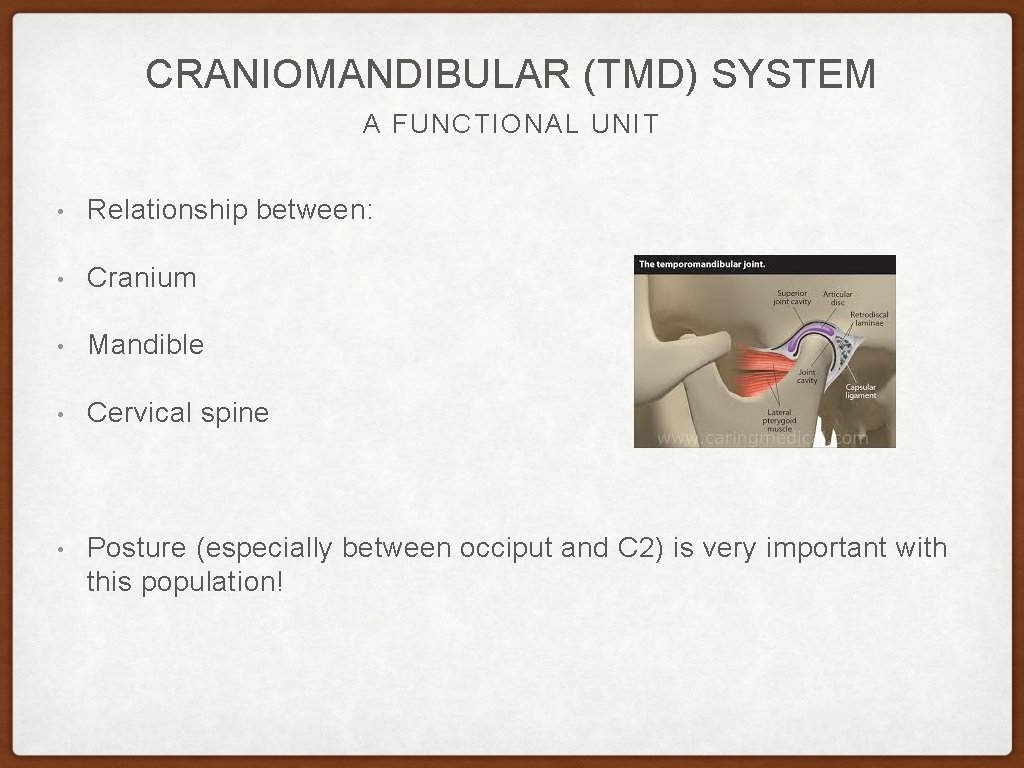
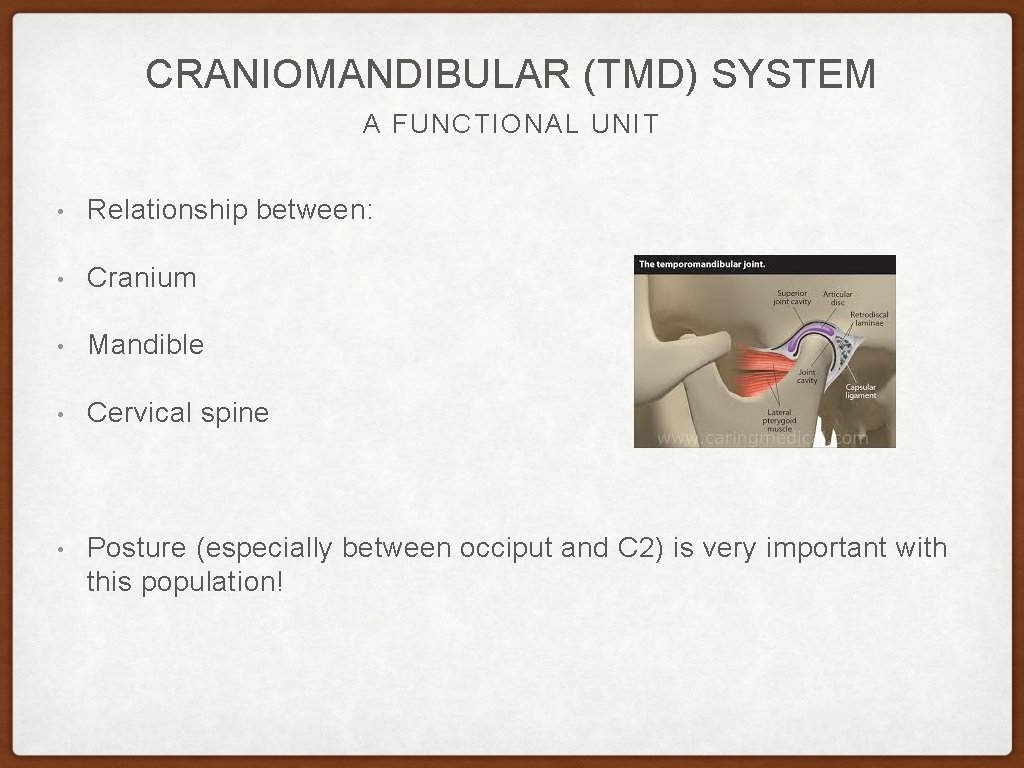
CRANIOMANDIBULAR (TMD) SYSTEM A FUNCTIONAL UNIT • Relationship between: • Cranium • Mandible • Cervical spine • Posture (especially between occiput and C 2) is very important with this population!
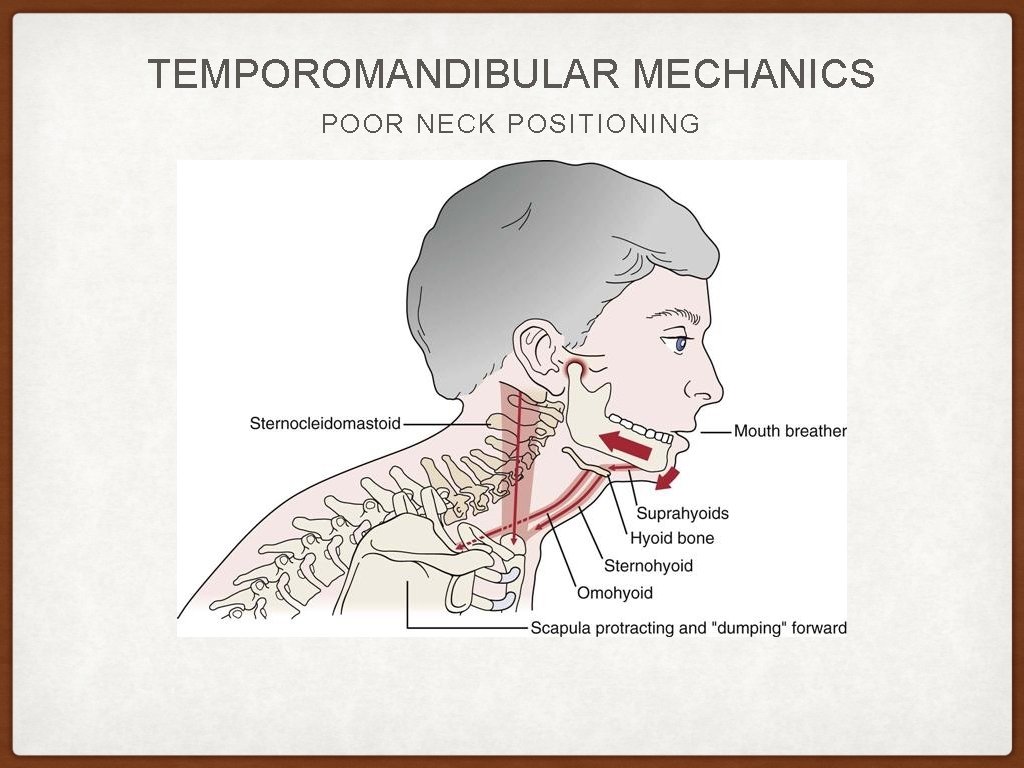
TEMPOROMANDIBULAR DISORDER (TMD) THE BASICS - 2: 1 prevalence female: male. Prevalent in those with hypermobility (54%) - TMD average of onset is 32 - Posture of the sub cranial and cervical spine, especially forward head position can effect TMJ ROM, the path of the mandible with opening/closing, and Aberrant muscle activity (Goldstein et al)(Huggare) - Only 15% of TMD dysfunction are related to teeth/occlusive issues, the majority Are biomechanical issues - - The sub cranial functional space (between the occiput and C 2 spinous process should be a minimum of 2 fingers (not less than 20 mm). Lab: practice this.
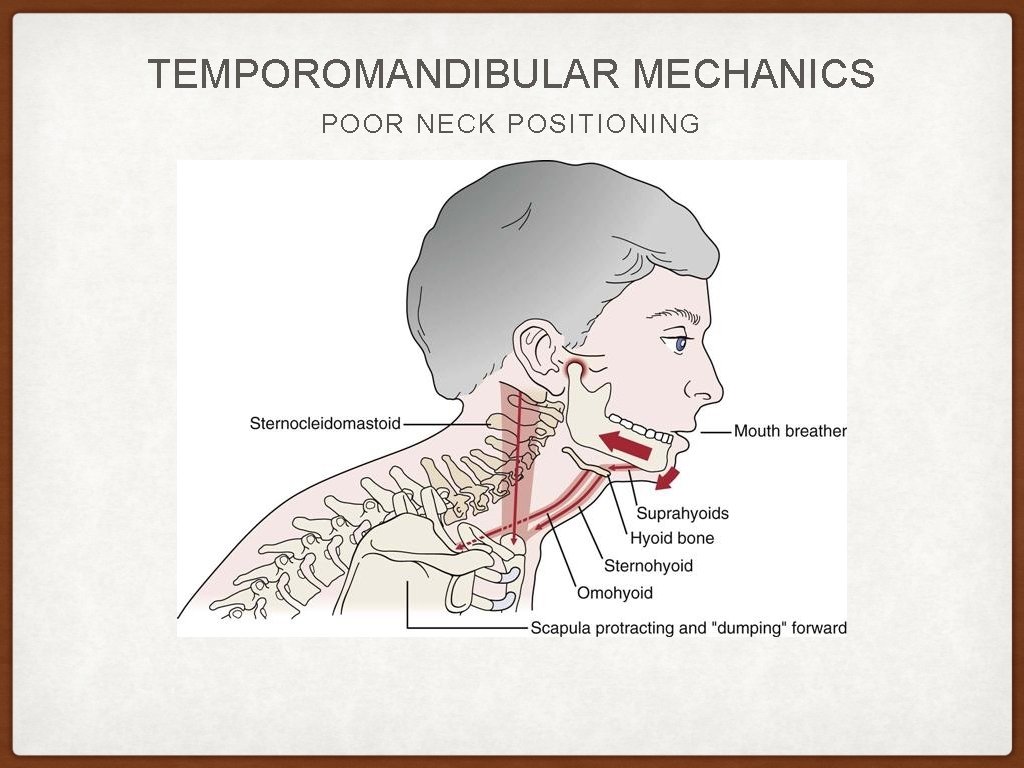
TEMPOROMANDIBULAR MECHANICS POOR NECK POSITIONING
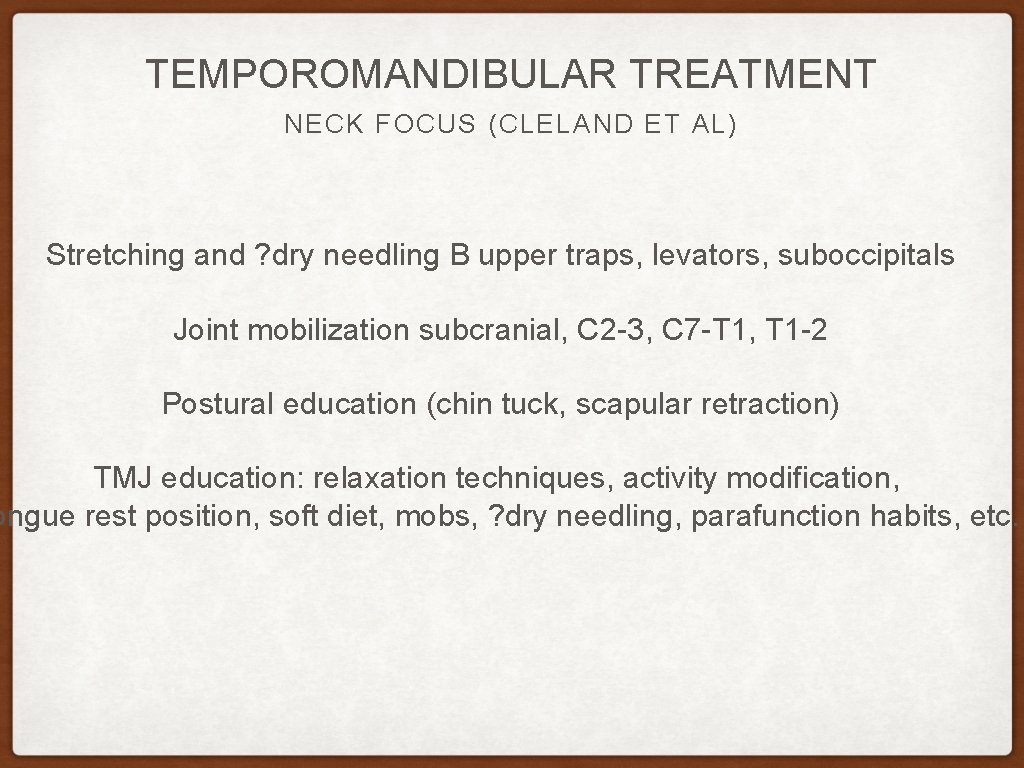
TEMPOROMANDIBULAR TREATMENT NECK FOCUS (CLELAND ET AL) Stretching and ? dry needling B upper traps, levators, suboccipitals Joint mobilization subcranial, C 2 -3, C 7 -T 1, T 1 -2 Postural education (chin tuck, scapular retraction) TMJ education: relaxation techniques, activity modification, ongue rest position, soft diet, mobs, ? dry needling, parafunction habits, etc.
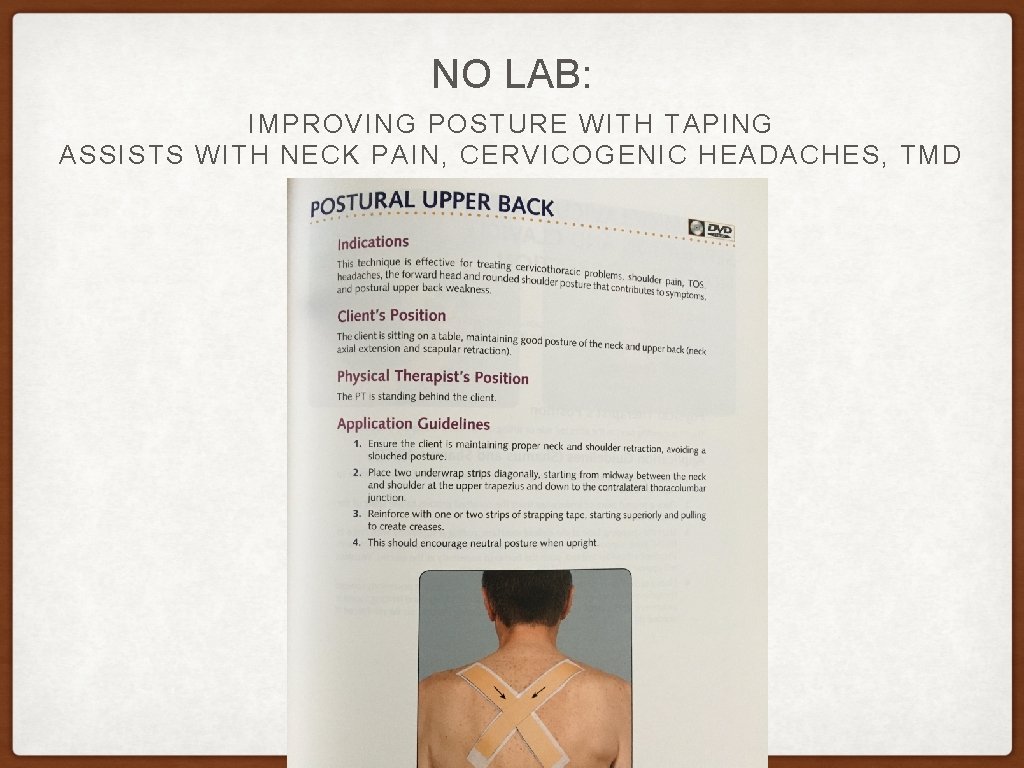
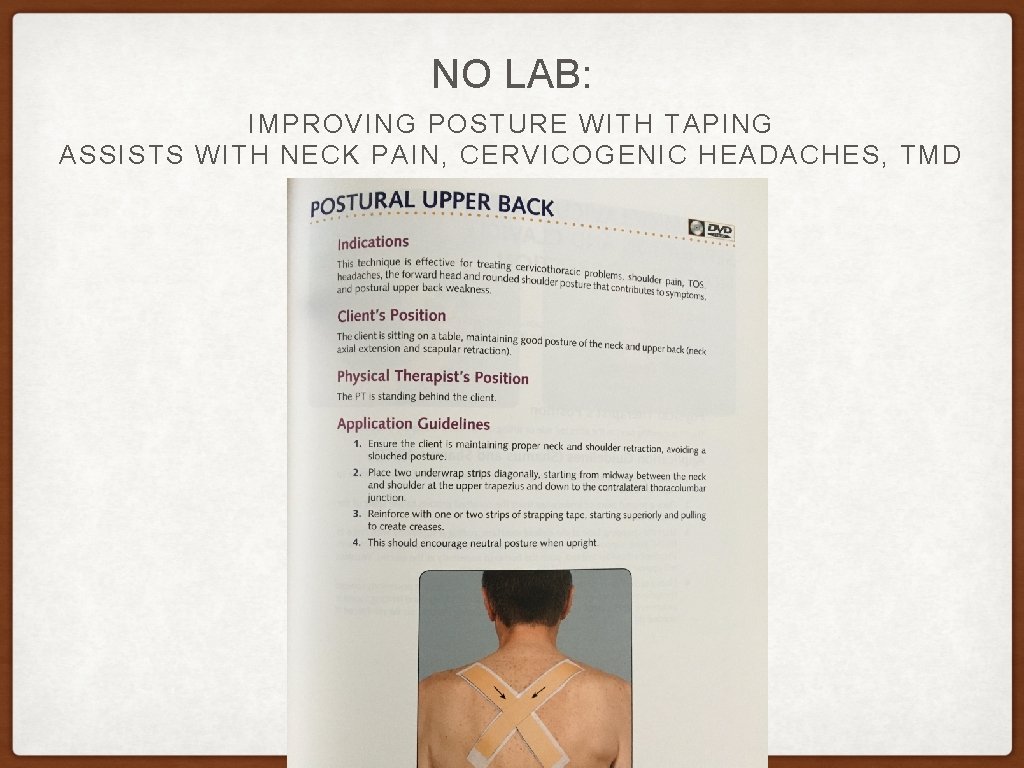
NO LAB: IMPROVING POSTURE WITH TAPING ASSISTS WITH NECK PAIN, CERVICOGENIC HEADACHES, TMD
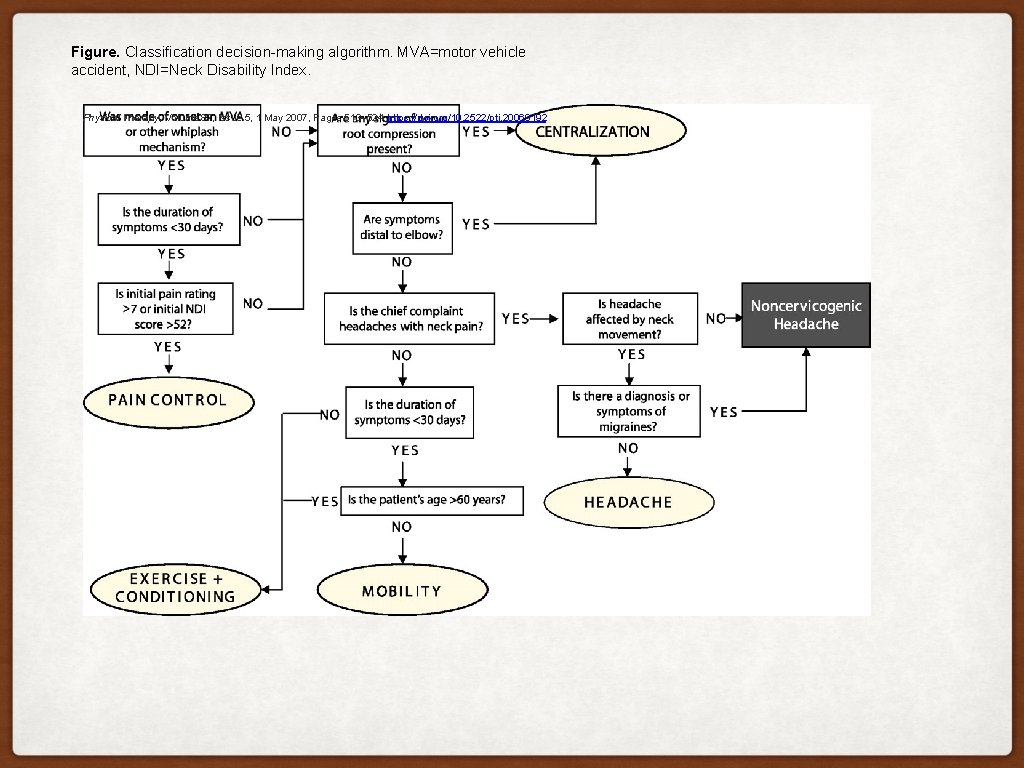
Figure. Classification decision-making algorithm. MVA=motor vehicle accident, NDI=Neck Disability Index. Physical Therapy, Volume 87, Issue 5, 1 May 2007, Pages 513– 524, https: //doi. org/10. 2522/ptj. 20060192
PT CONTINUING EDUCATION QUESTIONS • Name the 5 treatment based classifications of the cervical spine? pain, exercise & conditioning, mobility, centralization, headache • Which type of headache worsens with activity? Migraine without aura, medication overuse headache • Can TMD issues cause headaches? Yes • True or false: Cervical dysfunction is common with concussion? T
THANK YOU! QUESTIONS?
References: Biondi DM. Cervicogenic headache: a review of diagnostic and treatment strategies. J Am Osteopath Assoc. 2005; 105(4 Suppl 2): 16 S– 22 S. Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol. 2009; 8: 959– 968. Sjaastad O, Fredriksen A, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. Headache. 1998; 38: 442– 445. Becker WJ. Cervicogenic headache: evidence that the neck is a pain generator. Headache. 2010; 50: 699– 705. Haldman S, Dagenais S. Cervicogenic headaches: a critical review. Spine J. 2001; 1: 31– 46. van Suijlekom HA, Lame I, Stomp-van den Berg SG, et al. Quality of life of patients with cervicogenic headache: a comparision with control subjects and patients with migraine or tension-type headache. Headache. 2003; 43: 1034– 1041. Magarey ME, Rebbeck T, Coughlan B, et al. Pre-manipulative testing of the cervical spine review, revision and new clinical guidelines. Man Ther. 2004; 9: 95– 108. Childs JD, Flynn TW, Fritz JM, et al. Screening for vertebrobasilar insufficiency in patients with neck pain: manual therapy decision-making in the presence of uncertainty. J Orthop Sports Phys Ther. 2005; 35: 300– 306. Dodick DW. Occipital nerve stimulation for chronic cluster headache. Adv Stud Med. 2003; 3(6 C): S 550–S 555. Zito G, Jull GA. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man Ther. 2006; 11: 118– 129. Ogince M, Hall T, Robinson K, Blackmore AM. The diagnostic validity of the cervical flexion-rotation test in C 1/2 -related cervicogenic headache. Man Ther. 2007; 12: 256– 262. Jull G. Management of cervical headache. Man Ther. 1997; 2: 182– 190. de Koning CH, van den Heuvel SP, Staal JB, et al. Clinimatric evaluation of methods to measure muscle functioning in patients with non-specific neck pain: a systematic review. BMC Musculoskelet Disord. 2008; 9: 142. Domenech MA, Sizer PS, Dedrick GS, et al. The deep neck flexor endurance test: normative data scores in healthy adults. PM R. 2011; 3: 105– 110. International Headache Society. The international classification of headache disorders, 3 rd ed. (Beta version). http: //ihs-classification. org/en/. Accessed June 9, 2017. Jull GA, Stanton WR. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalagia. 2004; 25: 101– 108. Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine (Phila Pa 1976). 2002; 27: 1835– 1843. Racicki S, Gerwin S, Di. Claudio S, et al. Conservative physical therapy treatment management for the treatment of cervicogenic headache: a systematic review. J Manip Ther. 2013; 21: 113– 124.
Sigman & Landel, Cervicogenic Headache Clinical Summary, 6/12/17 accessed from PTnow. org Mucha & Troutman-Enseki, Concussion Clinical Summary, 1/30/15 accessed from PTnow. org Uitvlugt G, Indenbaum S. Clinical assessment of atlantoaxial instability using the Sharp-Purser test. Arthritis Rheum. Jul 1988; 31(7): 918 -922. Pub. Med Abstract. Kaale BR, Krakenes J, Albrektsen G, Wester K. Clinical assessment techniques for detecting ligament and membrane injuries in the upper cervical spine region: a comparison with MRI results. Man Ther. 2008; 13(5): 397 -403. Pub. Med Abstract. Osmotherly PG, Rivett DA, Rowe LJ. Construct validity for clinical tests for Alar ligament integrity: an evaluation using magnetic resonance imaging. Phys Ther. 2012; 92: 718 -725. Free Article. Stiel IG, Wells GA, Vandemheem KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001; 286(15): 1841 -1848. Free Article. Pub. Med Abstract. Anderson PA, Gugala Z, Lindsey RW, Schoenfeld AJ, Harris MB. Clearing the cervical spine in the blunt trauma patient. J Am Acad Orthop Surg. 2010; 18(3): 149 -159. Pub. Med Abstract. Kontos AP, Elbin RJ, Lau B, et al. Posttraumatic migraine as a predictor of recovery and cognitive impairment after sport-related concussion. Am J Sports Med. 2013; 41(7): 1497 -1504. Pub. Med Abstract. Mihalik JP, Register-Mihalik J, Kerr ZY, Marshall SW, Mc. Crea MC, Guskiewicz KM. Recovery of posttraumatic migraine characteristics in patients after mild traumatic brain injury. Am J Sports Med. 2013; 41(7): 1490 -1496. Pub. Med Abstract. Mihalik JP, Stump JE, Collins MW, Lovell MR, Field M, Maroon JC. Posttraumatic migraine characteristics in athletes following sports-related concussion. J Neurosurg. 2005; 102(5): 850 -855. Pub. Med Abstract. Pardini J, Stump J, Lovell MR, Collins MW, Moritz K, Fu F. The Post-concussion symptom scale (PCSS): a factor analysis [abstract]. Br J Sports Med. 2004; 38: 661 -662. Conference Abstract. [Scroll to #032. ] Kontos AP, Elbin RJ, Schatz P, et al. A revised factor structure for the post-concussion symptom scale: baseline and postconcussion factors. Am J Sports Med. 2012; 40(10): 2375 -2384. Pub. Med Abstract. Holland S, Silberstein SD, Freitag F, et al. Evidence-based guideline update; NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012; 78(17): 1346 -1353. Free. Article. | Pub. Med Abstract. Conidi FX. Sports-related concussion: the role of the headache specialist. Headache. 2012; 52 Suppl 1: 15 -21. | Pub. Med Abstract. Reid SA, Rivett DA, Katekar MG, Callister R. Comparison of mulligan sustained natural apophyseal glides and maitland mobilizations for treatment of cervicogenic dizziness: a randomized Craniofacial 2, Seminar manual. University of St Augustine 1/18.