Treating High Cholesterol because Cheeseburgers and Fries Still
Treating High Cholesterol because Cheeseburgers and Fries Still Exist!!!! By Nancy Dagefoerde MSN, FNP-BC
Objectives • Describe how to interpret the cholesterol guidelines and identify patient populations that qualify for treatment. • Describe the use of statins and non statins in the treatment of elevated cholesterol levels. • Describe common statin intolerance effects and how to address them in practice.
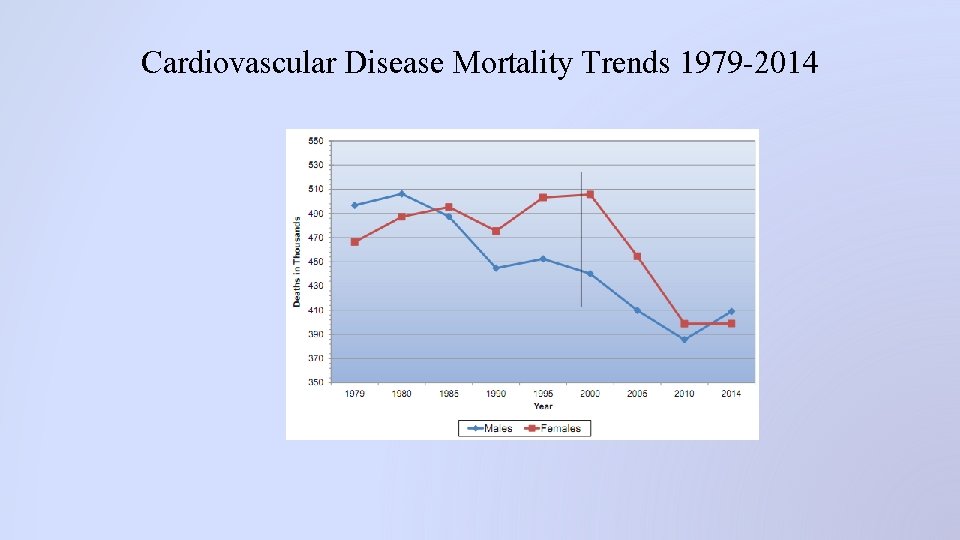
Cardiovascular Disease Mortality Trends 1979 -2014
Cardiovascular Disease Statistics 2018 • • • Cardiovascular disease accounts for 836, 546 deaths in the US per year which is 1 of every 3 deaths 2, 300 Americans die of CV disease each day: 1 every 38 seconds About 92. 1 million Americans live with some form of CV disease Coronary Heart Disease remains the leading cause of death (1 in 7 deaths) Total direct medical costs of CVD are projected to increase to $749 billion in 2035 Hear disease and stroke statistics 2018 update: a report from the American Heart Association. Circulation. DOI: 10. 1161
Cholesterol Statistics 2018 • About 94. 6 million or 39. 7% of American adults have a total cholesterol of 200 mg/d. L or higher • About 28. 5 million or 11. 9% of American adults have a total cholesterol of 240 mg/d. L or higher • 1 in 3 American adults have high levels of LDL cholesterol • 18. 7% of American adults have low levels of HDL cholesterol January 31, 2018. Circulation. DOI: 10. 1161/CIR.
Screening • Adults should have a lipid panel measured at least every 5 years starting at age 20 – Rescreen in 5 years if at goal or if not at goal treat according to the guidelines • Children should have a lipid panel once at age 9 -11 and again at age 17 -21 according to the American Academy of Pediatrics – Screen earlier 2 years to 10 years of age if positive family history of dyslipidemia or premature CVD risk factors, medical conditions such as organ transplant, lupus, nephrotic syndrome, or treatment for HIV
2013 ACC/AHA Guidelines for Cholesterol Management to Reduce Cardiovascular Risk • NCEP dates back to 1988 directed by the NHLBI( last update 2004) • Guiding principle is that an elevated cholesterol is the a root cause of ASCVD events based on review of large scale RCT’s • Treatment with past guidelines has led to progressive reduction in ASCVD morbidity and mortality in the last decade. • For all guidelines remember individual decision making for all patients. Stone. NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA guidelines on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults. J Am Col Cardiology, 2013.
Recommendations • Lifestyle modification is the foundation – Mediterranean or DASH nutrition plans – Regular exercise (150 minutes a week, 60 minutes a day is better) – Smoking Cessation: Quit Line 866 -784 -8937 – Treat Hypertension – Treat elevated blood sugars – Maintain healthy weight • Statin therapy is the next level of care
Recommendations for Pediatric Patients – Lifestyle modifications – Treat greater than 8 years old with apheresis, statin, and Zetia. Refer if LDL > 500 – Treatment Goal is to lower LDL to 130 mg/d. L www. ncbi. nlm. nih. gov/articles www. aafp. org/afp/2010/0901

Four Major Statin Benefit Groups • Patients with known ASCVD • Patients with LDL values > 190 mg/dl • Diabetics aged 40 -75 with LDL > 70 mg/dl • Patients without diabetes or ASCVD but with a LDL 70 -189 mg/dl and age 40 -75 with a CV risk estimator score > 7. 5%
Other Factors that May be Considered • • • LDL > 160 mg/dl or genetic hyperlipidemia Family history of premature ASCVD C- reactive protein > 2 mg/L Coronary Calcium score > 300 Agatston units Ankle Brachial Index <. 9 Elevated lifetime risk of ASCVD
10 Year ASCVD Risk Calculator • • www. clincalc. com Iphone app: 2013 Pooled Cohort Equations ASCVD My. americanheart. org Itunes. apple. com
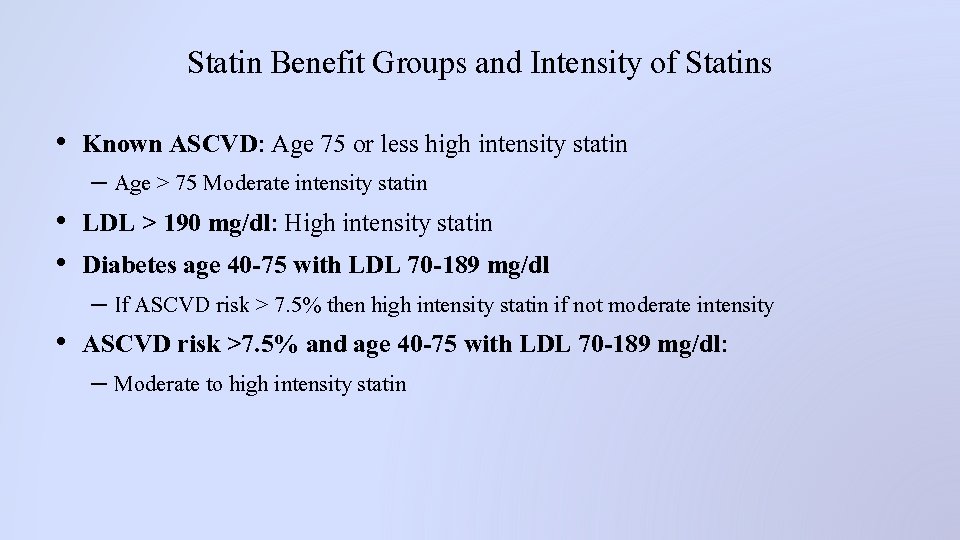
Statin Benefit Groups and Intensity of Statins • Known ASCVD: Age 75 or less high intensity statin – Age > 75 Moderate intensity statin • LDL > 190 mg/dl: High intensity statin • Diabetes age 40 -75 with LDL 70 -189 mg/dl – If ASCVD risk > 7. 5% then high intensity statin if not moderate intensity • ASCVD risk >7. 5% and age 40 -75 with LDL 70 -189 mg/dl: – Moderate to high intensity statin

High, Moderate, and Low Intensity Statin Therapy High Intensity Moderate Intensity Lowers LDL >50% Lowers LDL 30%-50% Lowers LDL <30% Atorvastatin 40 -80 mg Atorvastatin 10 -20 mg Simvastatin 10 mg Rosuvastatin 20 -40 mg Rosuvastatin 5 -10 mg Pravastatin 10 -20 mg Simvastatin 20 -40 mg Lovastatin 20 mg Pravastatin 40 -80 mg Fluvastatin 20 -40 mg Fluvastatin 40 -80 mg Pitavastatin 1 mg Lovastatin 40 mg Pitavastatin 2 -4 mg
Testing Needed Prior to Statin Initiation • • • Fasting Lipid Panel ALT CK (if indicated) Hemoglobin A 1 c (optional) TSH
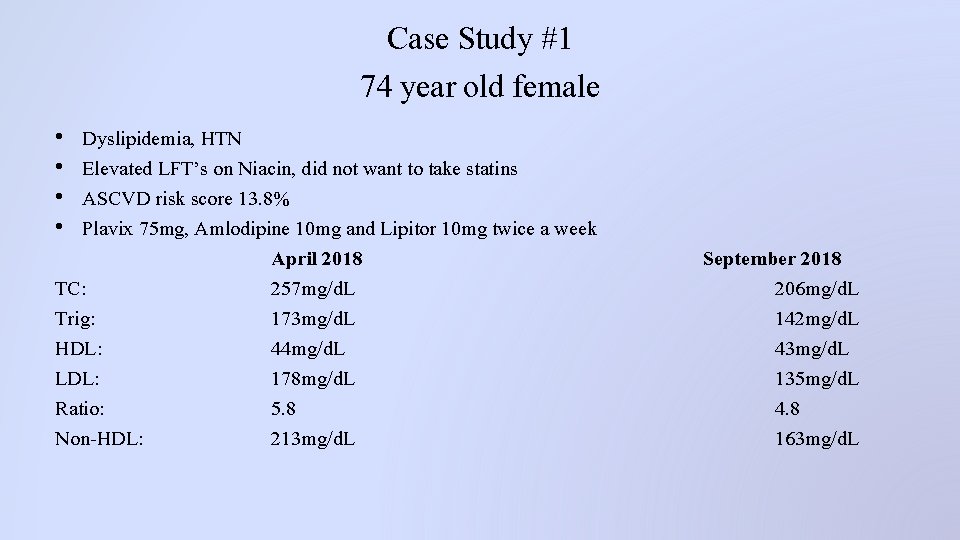
Case Study #1 74 year old female • • Dyslipidemia, HTN Elevated LFT’s on Niacin, did not want to take statins ASCVD risk score 13. 8% Plavix 75 mg, Amlodipine 10 mg and Lipitor 10 mg twice a week April 2018 TC: 257 mg/d. L Trig: 173 mg/d. L HDL: 44 mg/d. L LDL: 178 mg/d. L Ratio: 5. 8 Non-HDL: 213 mg/d. L September 2018 206 mg/d. L 142 mg/d. L 43 mg/d. L 135 mg/d. L 4. 8 163 mg/d. L
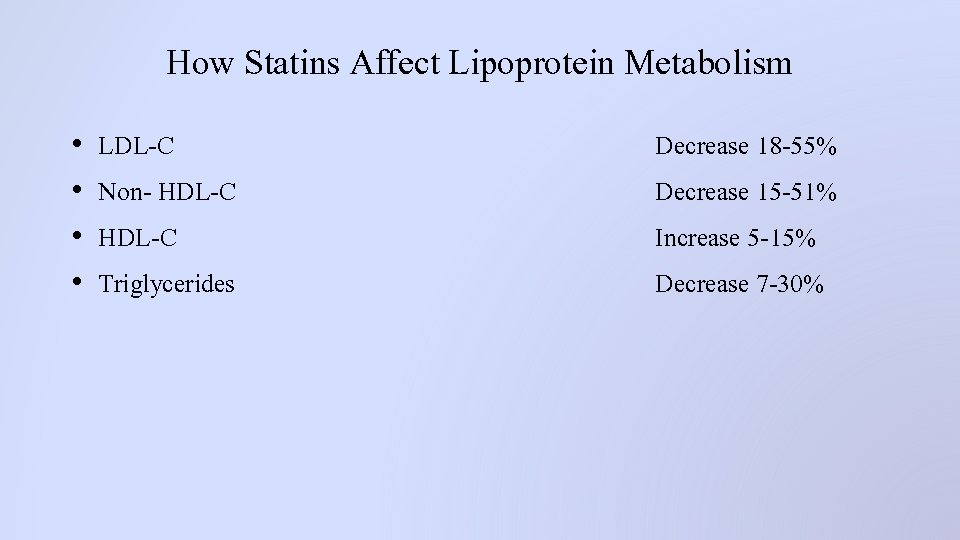
How Statins Affect Lipoprotein Metabolism • • LDL-C Non- HDL-C Triglycerides Decrease 18 -55% Decrease 15 -51% Increase 5 -15% Decrease 7 -30%
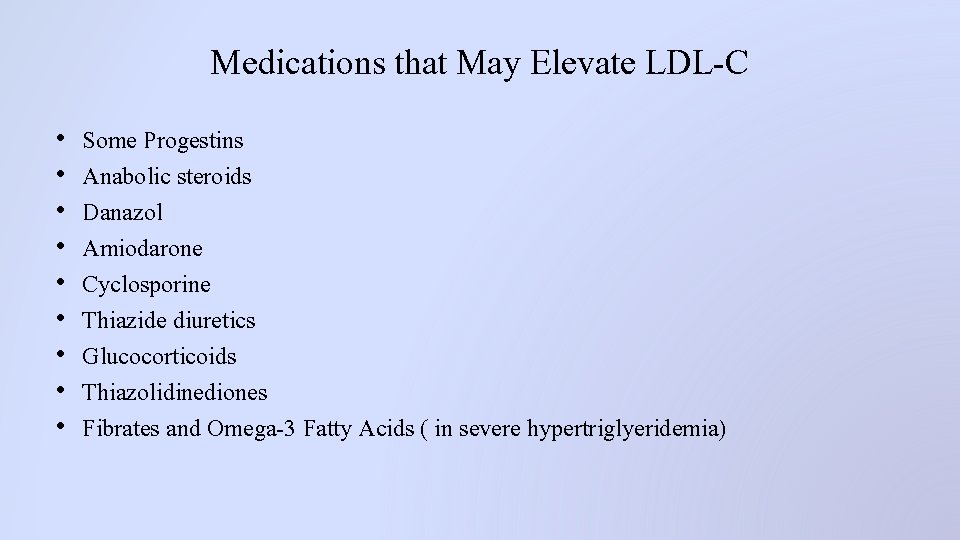
Medications that May Elevate LDL-C • • • Some Progestins Anabolic steroids Danazol Amiodarone Cyclosporine Thiazide diuretics Glucocorticoids Thiazolidinediones Fibrates and Omega-3 Fatty Acids ( in severe hypertriglyeridemia)
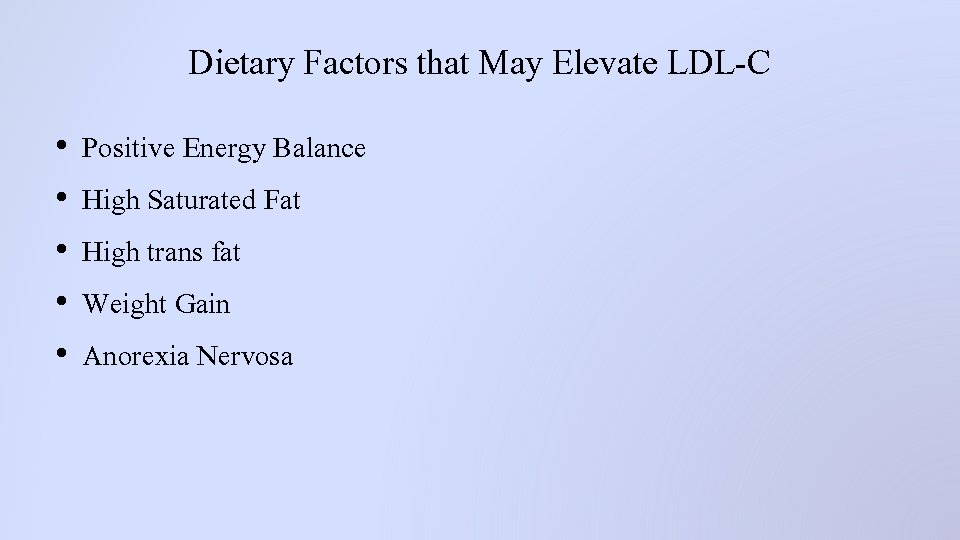
Dietary Factors that May Elevate LDL-C • • • Positive Energy Balance High Saturated Fat High trans fat Weight Gain Anorexia Nervosa

Diseases and Disorders that May Elevate LDL-C • • • Chronic Kidney Disease Nephrotic Syndrome Obstructive Liver Disease HIV infection Autoimmune disorders Hypothyroidism Pregnancy Polycystic ovary syndrome Menopause with declining estrogen levels
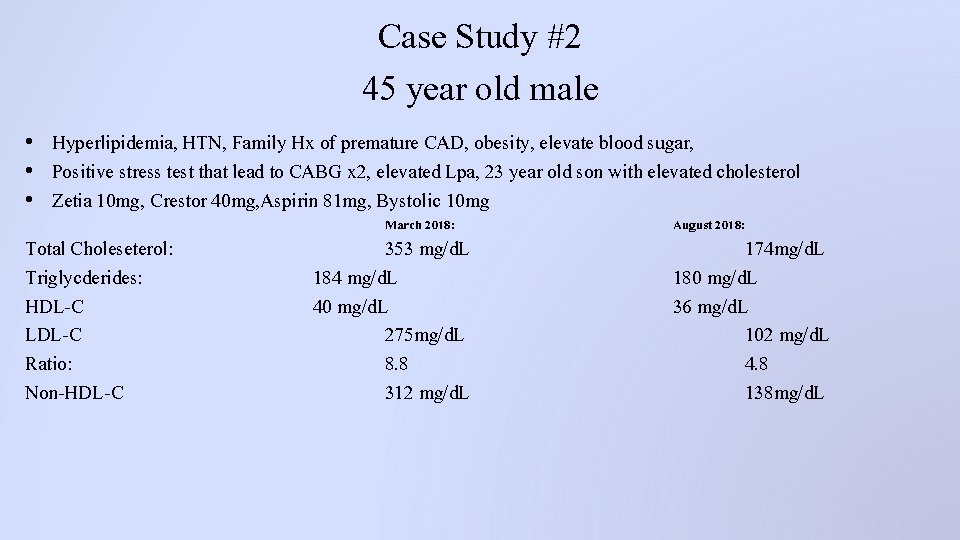
Case Study #2 45 year old male • Hyperlipidemia, HTN, Family Hx of premature CAD, obesity, elevate blood sugar, • Positive stress test that lead to CABG x 2, elevated Lpa, 23 year old son with elevated cholesterol • Zetia 10 mg, Crestor 40 mg, Aspirin 81 mg, Bystolic 10 mg March 2018: Total Choleseterol: Triglycderides: HDL-C LDL-C Ratio: Non-HDL-C 353 mg/d. L 184 mg/d. L 40 mg/d. L 275 mg/d. L 8. 8 312 mg/d. L August 2018: 174 mg/d. L 180 mg/d. L 36 mg/d. L 102 mg/d. L 4. 8 138 mg/d. L
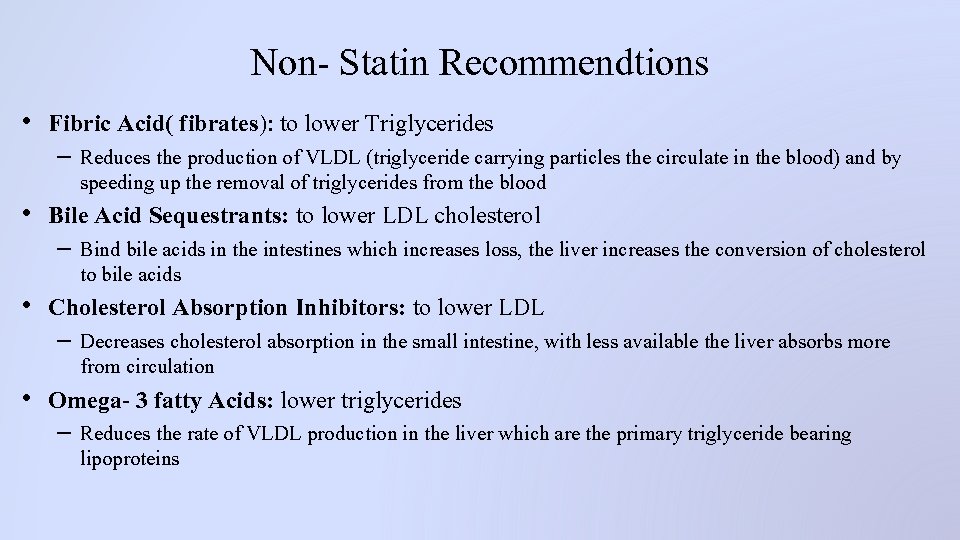
Non- Statin Recommendtions • Fibric Acid( fibrates): to lower Triglycerides – Reduces the production of VLDL (triglyceride carrying particles the circulate in the blood) and by speeding up the removal of triglycerides from the blood • Bile Acid Sequestrants: to lower LDL cholesterol – Bind bile acids in the intestines which increases loss, the liver increases the conversion of cholesterol to bile acids • Cholesterol Absorption Inhibitors: to lower LDL – Decreases cholesterol absorption in the small intestine, with less available the liver absorbs more from circulation • Omega- 3 fatty Acids: lower triglycerides – Reduces the rate of VLDL production in the liver which are the primary triglyceride bearing lipoproteins
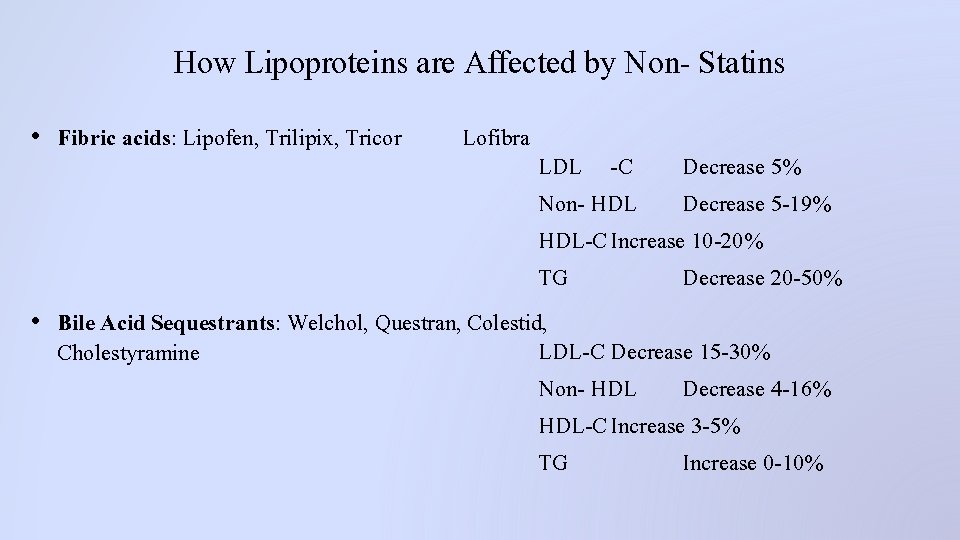
How Lipoproteins are Affected by Non- Statins • Fibric acids: Lipofen, Trilipix, Tricor Lofibra LDL -C Decrease 5% Non- HDL Decrease 5 -19% HDL-C Increase 10 -20% TG Decrease 20 -50% • Bile Acid Sequestrants: Welchol, Questran, Colestid, LDL-C Decrease 15 -30% Cholestyramine Non- HDL Decrease 4 -16% HDL-C Increase 3 -5% TG Increase 0 -10%
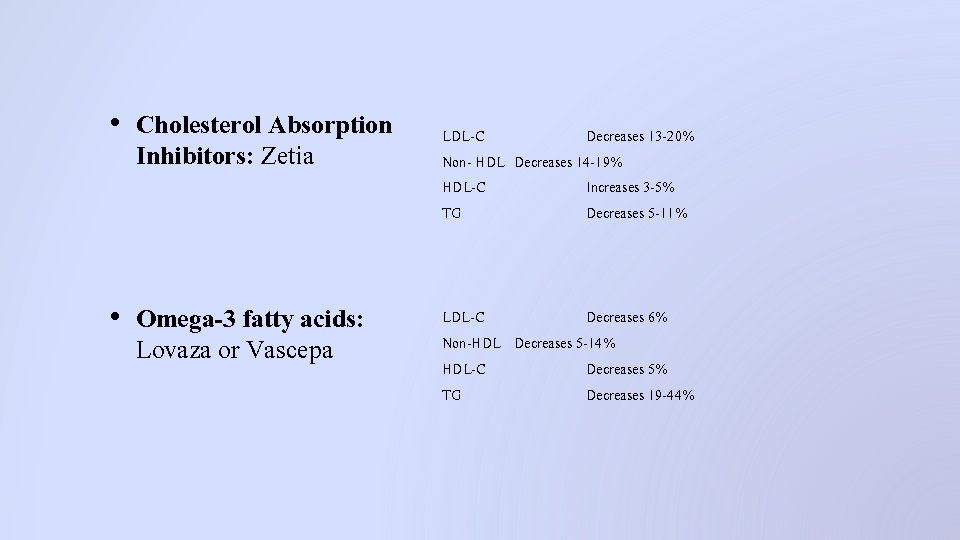
• Cholesterol Absorption Inhibitors: Zetia • Omega-3 fatty acids: Lovaza or Vascepa LDL-C Decreases 13 -20% Non- HDL Decreases 14 -19% HDL-C Increases 3 -5% TG Decreases 5 -11% LDL-C Decreases 6% Non-HDL Decreases 5 -14% HDL-C Decreases 5% TG Decreases 19 -44%

Medications that May Elevate Triglycerides • • • Oral estrogens Tamoxifen Raloxifene Retinoids Immunosuppressive drugs Interferon Beta Blockers Protease Inhibitors Thiazide Diuretics Glucocorticoids Rosiglitazone Bile Acid sequestrants
Dietary Characteristics that May Elevate Triglycerides • • Positive energy balance High glycemic load Excess alcohol Weight gain
Disorders that May Elevate Triglycerides • • • Chronic kidney disease Nephrotic Syndrome Diabetes mellitus Metabolic Syndrome HIV infection Autoimmune disorders Hypothyroidism Pregnancy Polycystic ovary syndrome Menopause
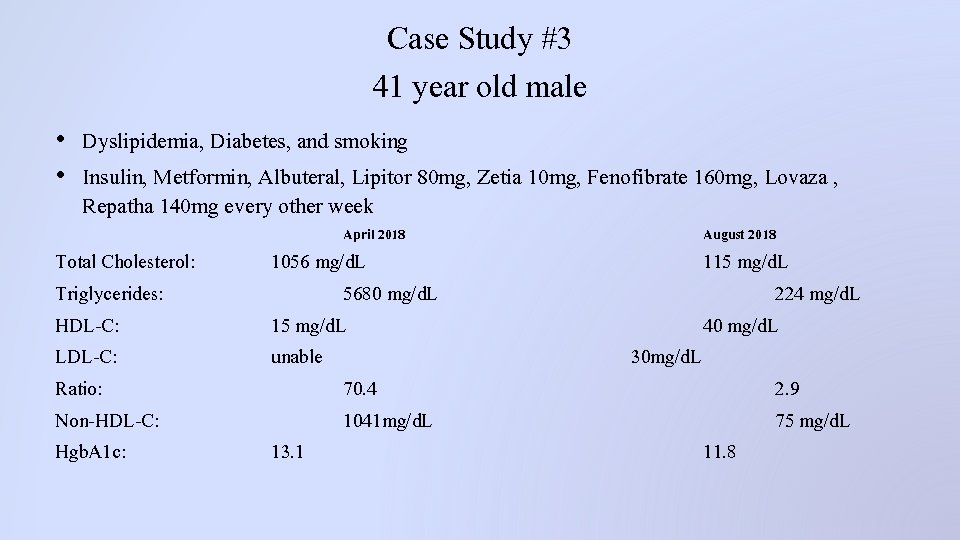
Case Study #3 41 year old male • Dyslipidemia, Diabetes, and smoking • Insulin, Metformin, Albuteral, Lipitor 80 mg, Zetia 10 mg, Fenofibrate 160 mg, Lovaza , Repatha 140 mg every other week April 2018 Total Cholesterol: Triglycerides: HDL-C: LDL-C: Ratio: Non-HDL-C: Hgb. A 1 c: 1056 mg/d. L 5680 mg/d. L 15 mg/d. L unable 70. 4 1041 mg/d. L 13. 1 August 2018 115 mg/d. L 224 mg/d. L 40 mg/d. L 30 mg/d. L 2. 9 75 mg/d. L 11. 8
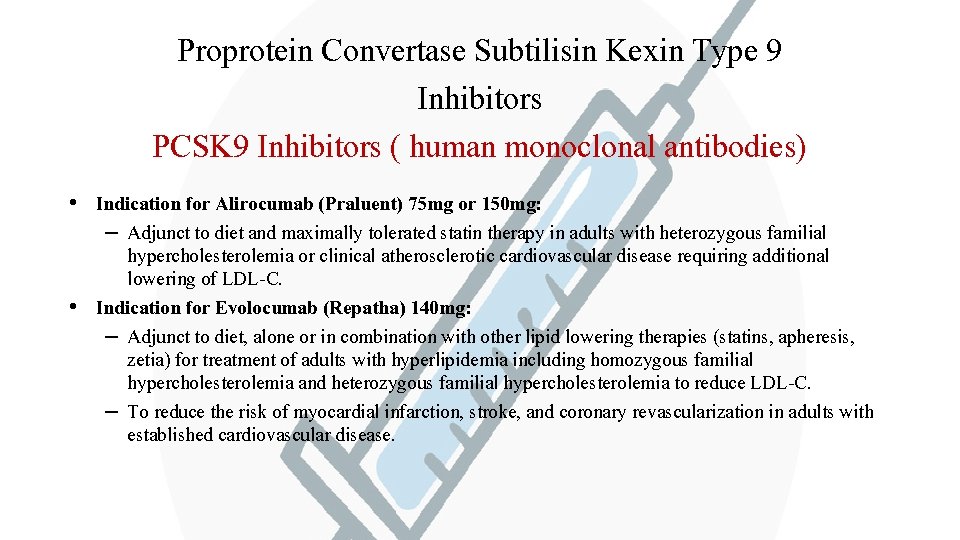
Proprotein Convertase Subtilisin Kexin Type 9 Inhibitors PCSK 9 Inhibitors ( human monoclonal antibodies) • Indication for Alirocumab (Praluent) 75 mg or 150 mg: – Adjunct to diet and maximally tolerated statin therapy in adults with heterozygous familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease requiring additional lowering of LDL-C. • Indication for Evolocumab (Repatha) 140 mg: – Adjunct to diet, alone or in combination with other lipid lowering therapies (statins, apheresis, zetia) for treatment of adults with hyperlipidemia including homozygous familial hypercholesterolemia and heterozygous familial hypercholesterolemia to reduce LDL-C. – To reduce the risk of myocardial infarction, stroke, and coronary revascularization in adults with established cardiovascular disease.
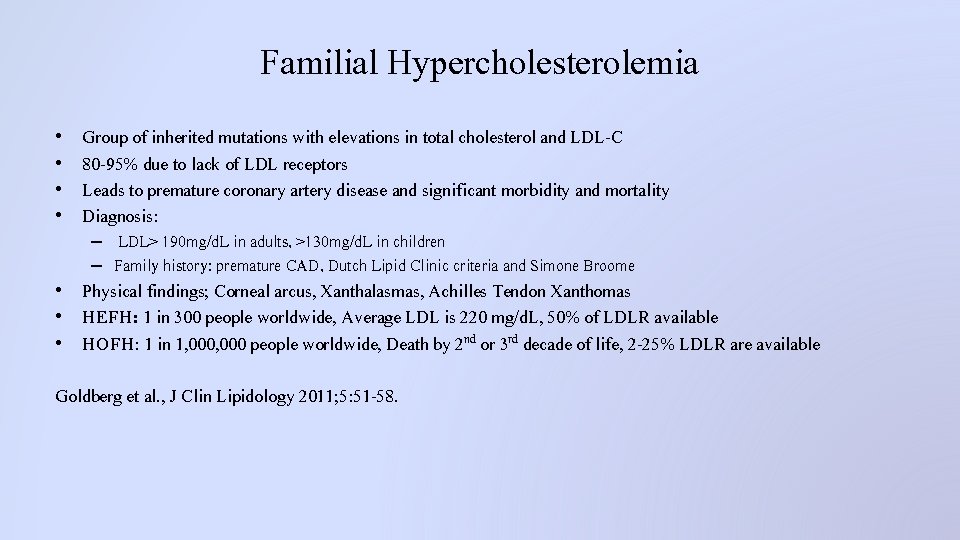
Familial Hypercholesterolemia • • Group of inherited mutations with elevations in total cholesterol and LDL-C 80 -95% due to lack of LDL receptors Leads to premature coronary artery disease and significant morbidity and mortality Diagnosis: – LDL> 190 mg/d. L in adults, >130 mg/d. L in children – Family history: premature CAD, Dutch Lipid Clinic criteria and Simone Broome • Physical findings; Corneal arcus, Xanthalasmas, Achilles Tendon Xanthomas • HEFH: 1 in 300 people worldwide, Average LDL is 220 mg/d. L, 50% of LDLR available • HOFH: 1 in 1, 000 people worldwide, Death by 2 nd or 3 rd decade of life, 2 -25% LDLR are available Goldberg et al. , J Clin Lipidology 2011; 5: 51 -58.
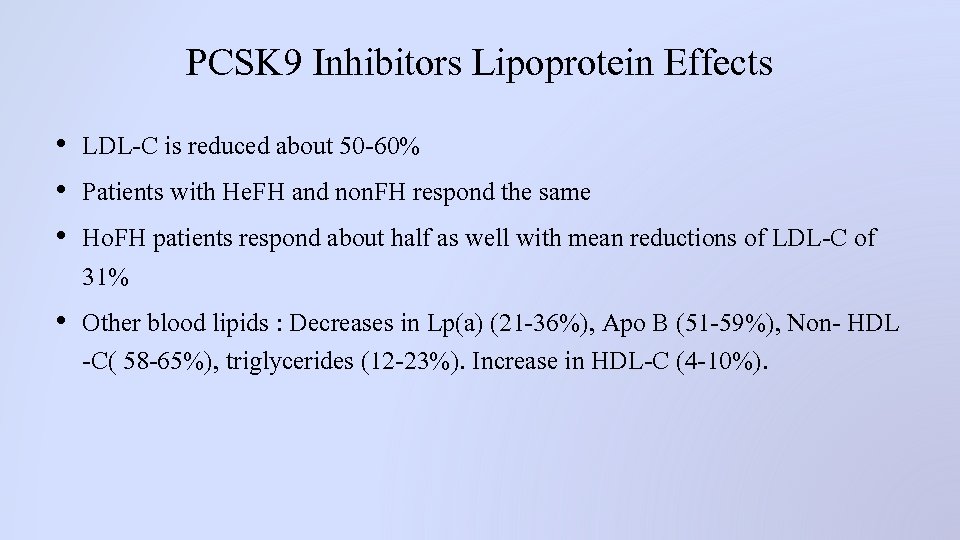
PCSK 9 Inhibitors Lipoprotein Effects • LDL-C is reduced about 50 -60% • Patients with He. FH and non. FH respond the same • Ho. FH patients respond about half as well with mean reductions of LDL-C of 31% • Other blood lipids : Decreases in Lp(a) (21 -36%), Apo B (51 -59%), Non- HDL -C( 58 -65%), triglycerides (12 -23%). Increase in HDL-C (4 -10%).
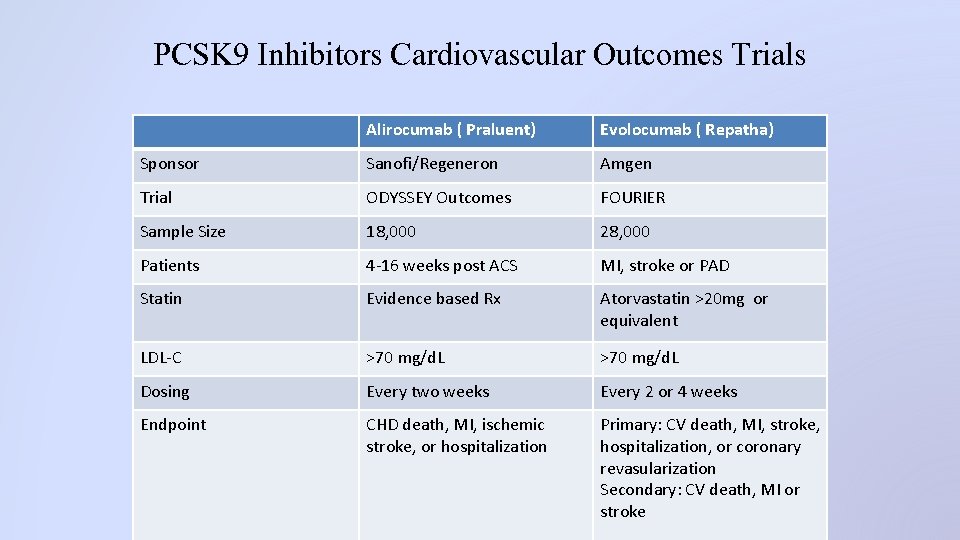
PCSK 9 Inhibitors Cardiovascular Outcomes Trials Alirocumab ( Praluent) Evolocumab ( Repatha) Sponsor Sanofi/Regeneron Amgen Trial ODYSSEY Outcomes FOURIER Sample Size 18, 000 28, 000 Patients 4 -16 weeks post ACS MI, stroke or PAD Statin Evidence based Rx Atorvastatin >20 mg or equivalent LDL-C >70 mg/d. L Dosing Every two weeks Every 2 or 4 weeks Endpoint CHD death, MI, ischemic stroke, or hospitalization Primary: CV death, MI, stroke, hospitalization, or coronary revasularization Secondary: CV death, MI or stroke
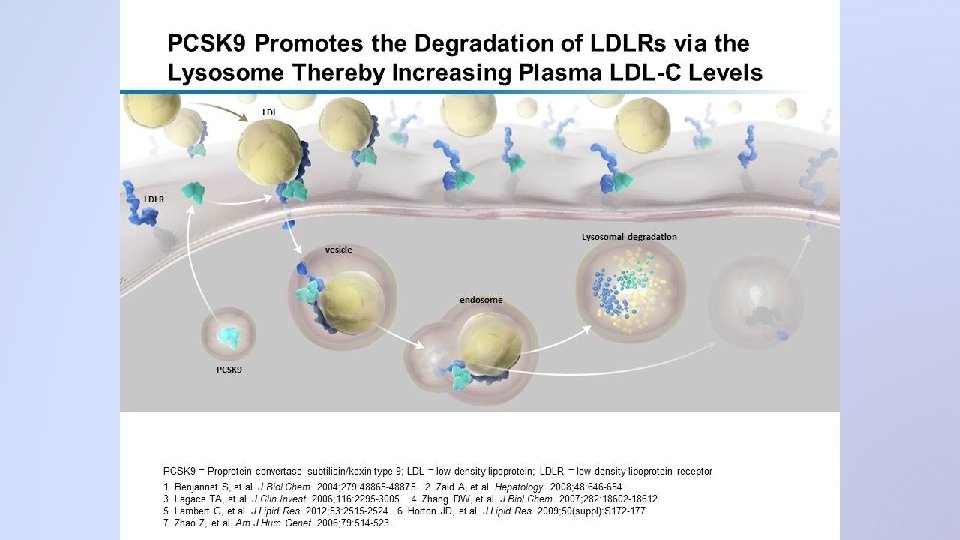
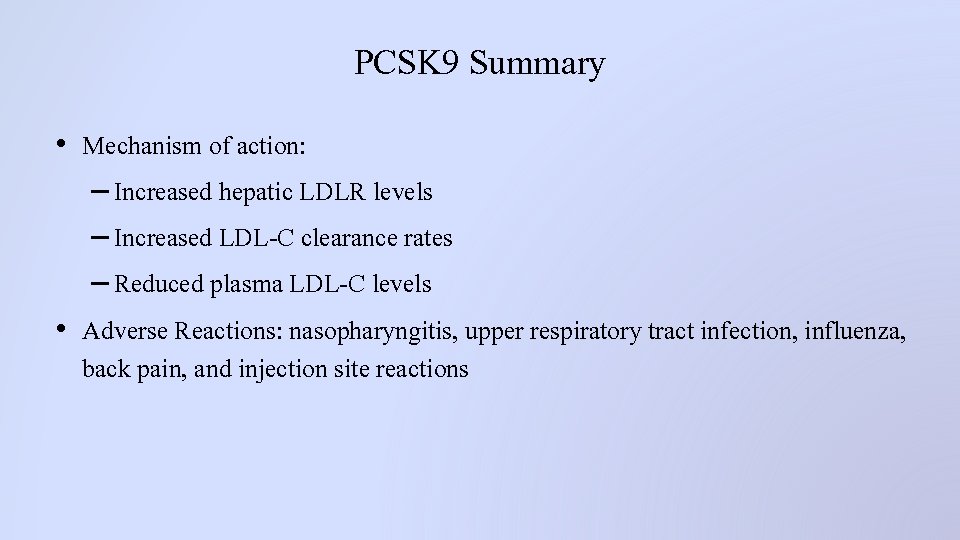
PCSK 9 Summary • Mechanism of action: – Increased hepatic LDLR levels – Increased LDL-C clearance rates – Reduced plasma LDL-C levels • Adverse Reactions: nasopharyngitis, upper respiratory tract infection, influenza, back pain, and injection site reactions
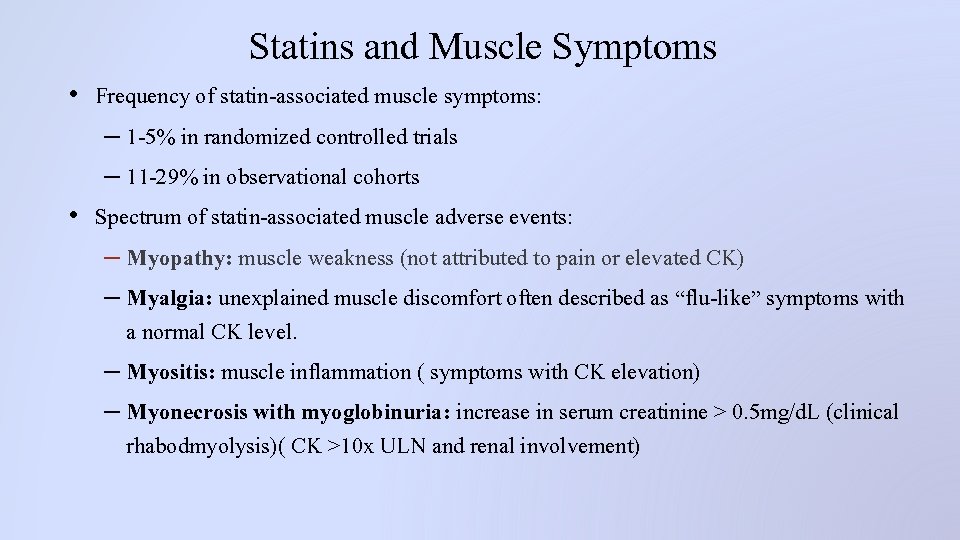
Statins and Muscle Symptoms • Frequency of statin-associated muscle symptoms: – 1 -5% in randomized controlled trials – 11 -29% in observational cohorts • Spectrum of statin-associated muscle adverse events: – Myopathy: muscle weakness (not attributed to pain or elevated CK) – Myalgia: unexplained muscle discomfort often described as “flu-like” symptoms with a normal CK level. – Myositis: muscle inflammation ( symptoms with CK elevation) – Myonecrosis with myoglobinuria: increase in serum creatinine > 0. 5 mg/d. L (clinical rhabodmyolysis)( CK >10 x ULN and renal involvement)
Options for Patients Intolerant to Multiple Statins • • • Lower the statin dose Switch to another statin Reduce the frequency to not daily Add on a non statin to the highest tolerable statin dose Measure and supplement with Vitamin D Adding Co enzyme Q 10
Statin Safety: ACC/AHA Guidelines • Use a moderate intensity statin if the following applies: – Renal or Hepatic impairment – Previous statin intolerance of muscle disorder – Unexplained ALT levels – Using other medications that affects statin metabolism – > 75 years old – Asian ancestry • CK not routinely done although it would be important for persons with a risk for adverse muscle events. Stone NJ et al. Circulation 2013, DOI: 19. 1161/01

ACC/AHA Statin Safety Recommendations • Mild to moderate muscle symptoms develop: – Discontinue statin to evaluate symptoms – Evaluate other conditions: hypothyroidism, reduced renal or hepatic function, rheumatologic disorders, steroid myopathy, vitamin D deficiency, primary muscle diseases – If symptoms resolve give the statin at a lower dose to assess causal relationship of muscle symptoms – If symptoms return at the lower dose, use a different statin at a lower dose

Monitoring Statin Therapy • Baseline lipid panel should be obtained with a second lipid panel in 4 -12 weeks after initiation of statin therapy • Then assessments should be every 3 -12 months as clinically indicated. • Dose and frequency can be increased as tolerated.
Cognitive Impairment and Statin Use • Statins have been associated with spontaneous reports of adverse cognitive effects such as amnesia, concentration difficulties, and confusion • Two large RCT’s (PROSPER and HPS) show no difference in cognition after many months being on a statin (42 months and 6 months) • At least 12 small RCT’s showed similar results • If a patient reports adverse cognitive effects: – Assess for other causes of change in cognitive function – Consider a trial of discontinuing the statin www. lipid. org
Statin Use and Liver and Kidney Dysfunction • Liver Function changes: – 1 -3% through RCT’s show liver function elevations – Liver function elevations may be due to other etiologies (fatty liver or hepatitis ) – 2012 FDA statin label change recommends liver function testing at baseline and then clinically as indicated. • Renal Function changes: – Possible proteinuria and or hematuria – Consider age, gender, size, frailty, other diseases, family history, excessive exercise, surgery, ETOH, obstructive liver disease, transplants, renal failure – Treatment that is related: high dose statins or interaction with other medications www. lipid. org
Drug to Drug Interactions affecting Renal Function • • • • Fibrates Macrolide Antibiotics Cyclosporines Protease Inhibitors Calcium Channel Blockers Nefazadone Amiodarone Alcohol Niacin Colchicine Digoxin Coumadin Azole Antifungal
Statin Diabetes Safety • Statin use is associated with a modest but statistically significant increase risk for new-onset type 2 diabetes mellitus 10% vs placebo • High Intensity increases risk more than Moderate Intensity statins • Risk is clearly more evident for those with major risk factors for diabetes • Cardiovascular benefits of statin therapy far outweigh the risk of diabetes • Recommendations: – Statin therapy should continue to decrease ASCVD event risk – Lifestyle modification should be emphasized – Patients with diabetes risk factors should be screened with fasting blood sugars or HGA 1 c prior to starting statin therapy and yearly thereafter www. lipid. org
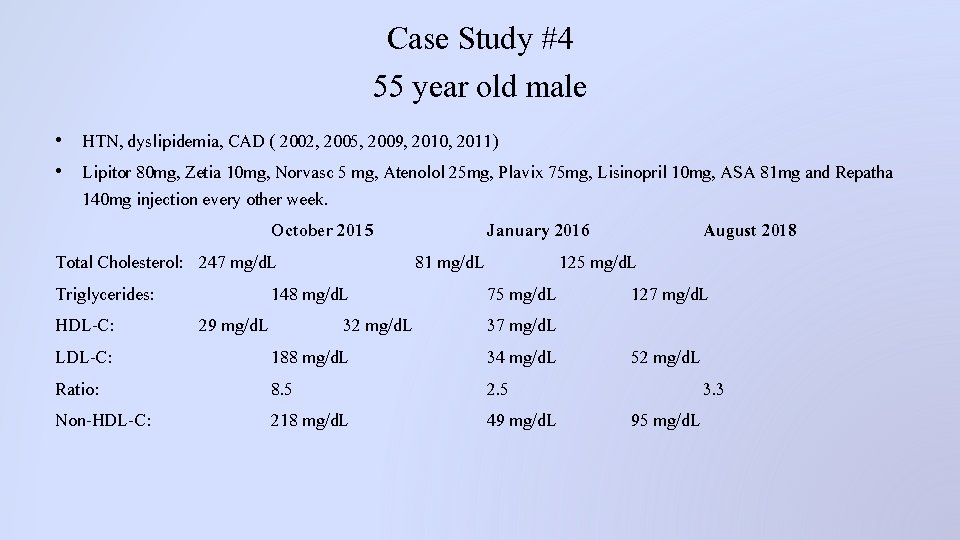
Case Study #4 55 year old male • HTN, dyslipidemia, CAD ( 2002, 2005, 2009, 2010, 2011) • Lipitor 80 mg, Zetia 10 mg, Norvasc 5 mg, Atenolol 25 mg, Plavix 75 mg, Lisinopril 10 mg, ASA 81 mg and Repatha 140 mg injection every other week. October 2015 January 2016 August 2018 Total Cholesterol: 247 mg/d. L 81 mg/d. L 125 mg/d. L Triglycerides: 148 mg/d. L 75 mg/d. L 127 mg/d. L HDL-C: 29 mg/d. L 32 mg/d. L 37 mg/d. L LDL-C: 188 mg/d. L 34 mg/d. L 52 mg/d. L Ratio: 8. 5 2. 5 3. 3 Non-HDL-C: 218 mg/d. L 49 mg/d. L 95 mg/d. L

Thank You!
- Slides: 46