Treating Chronic Depression Using Empirically Supported Treatments that











- Slides: 51
Treating Chronic Depression: Using Empirically Supported Treatments that Work Gary A. Sibcy, II, Ph. D Licensed Clinical Psychologist Professor: School of Behavior Sciences Center for Counselor Education and Family Development Liberty University gsibcy@Liberty. edu
Treating Depression �Question: “Don’t we have “effective” medical treatments for depression? ” �Depends on what you mean by “effective. ”
Depression �Major Depressive Disorder (MDD) is a relatively common psychiatric disorder, with a lifetime prevalence rate of 7% to 12% for men and 20% to 25% for women (Kessler et al 2003). �The annual cost of MDD in the U. S. was estimated at $ 83. 1 billion (Greenberg et al 2003) and the World Health Organization predicted it to be the second-leading cause of functional impairment and disability worldwide by 2020 (Murry and Lopez, 1996).
Depression �Although a number of effective psychiatric and psychological treatments have been developed, �a sizeable portion of patients have a chronic, treatmentresistant course of illness, �characterized by a failure to reach full-remission and continuing to exhibit substantial symptomology.

Depression �In clinical effectiveness studies with representative treatment samples, � 70% to 89% of patients fail to reach remission after relatively extend treatment courses of 8 to 12 months (Lin et al, 1997; Rost et al, 2002; Rush et al, 2004
STAR*D STUDY �In the largest real-world effectiveness study of MDD ever conducted, the Sequenced Treatment Alternatives to Relieve Depression (STAR*D), �A four-step treatment protocol was designed to treat patients to remission. �Each level of treatment lasted up to 12 weeks. All patients entered level I and if they achieved remission, they remained at the same level and were followed up to 1 year. � If they failed to reach remission, they were upgraded to the next level, offered different augmentation strategies
STAR*D STUDY � Of the 60% of patients who completed the study, 33% achieved remission at Level I, 57% at Level 2, and 63% and 67% achieved remission at Levels 3 and 4, respectively.
Upshot �The upshot of this study was that with each subsequent level of treatment, �fewer patients achieved remission, �with only about 10% of treatment resistant patients (i. e. those who failed to reach remission after levels 1 and 2) achieving remission after level 4. �Moreover, relapse rates increased with each treatment step: 40% in step 1, 53% in step 2, 65 % in step 3 and 71% in step 4 and the overall dropout rate was 40%.
Upshot �Thus a substantial proportion of patients fail to achieve remission (33% of those who remain in treatment over the course of 1 -year) and �the majority of treatment-resist patients relapse (65%71%) within 1 -year, even when continuing maintenance medication. �Consequently these results represent a need to develop alternative treatments that not only increases the proportion of patients achieving remission, but also reduces both relapse rates and dropout rates.
One Such Treatment �Cognitive Behavioral Analysis System of Psychotherapy �Specifically designed for Chronic, Refractory Depression—especially Early Onset
Characteristics of Chronic Depression �Long-standing history of Dysthymic Disorder, now Persistent Depressive Disorder with multiple, superimposed Major Depressive Episodes �Multiple Major Depressive episodes, each lasting several years �Some never fully recover and remain in partial remission �Many have comorbid disorders, including anxiety and personality disorders
Typical Treatment History �Long periods of untreated depression before seeking first treatment �Previously misdiagnosed �Antidepressant only at inadequate doses and/or length of treat �Those receiving therapy derived little to no benefit �Few will have received combined medication and psychotherapy
Characteristics of Chronic, Treatment Resistant Depression �Highly treatment resistant to nearly all treatment modes: �Medication �Psychotherapy � CBT � IPT � STDP
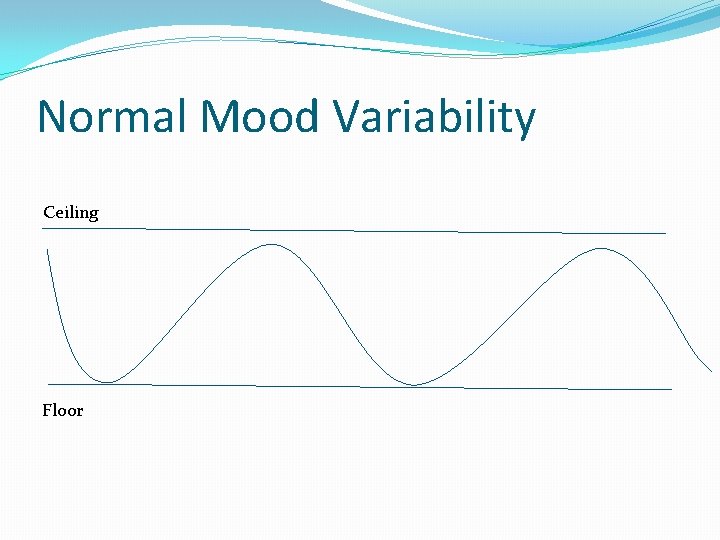
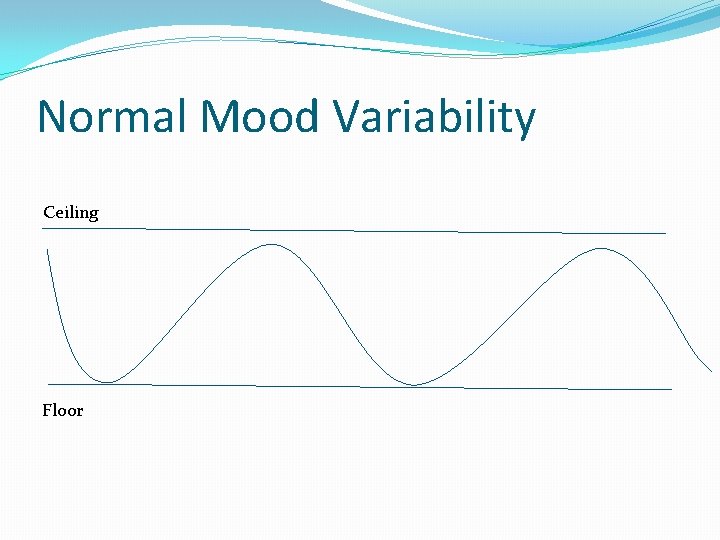
Normal Mood Variability Ceiling Floor
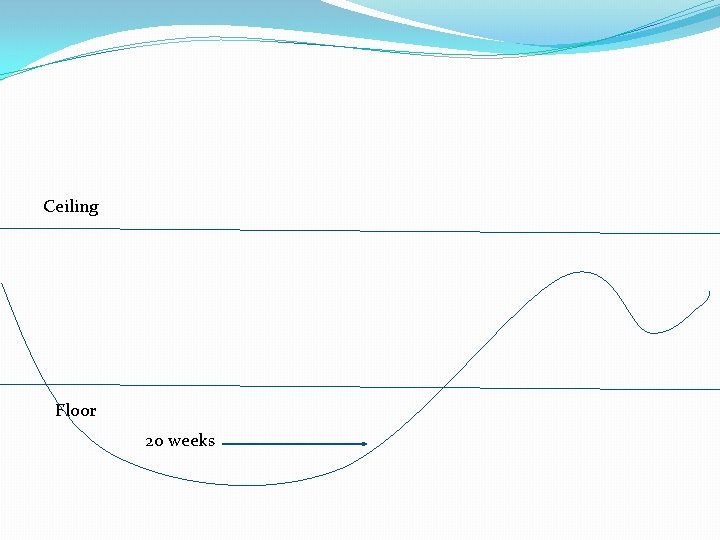
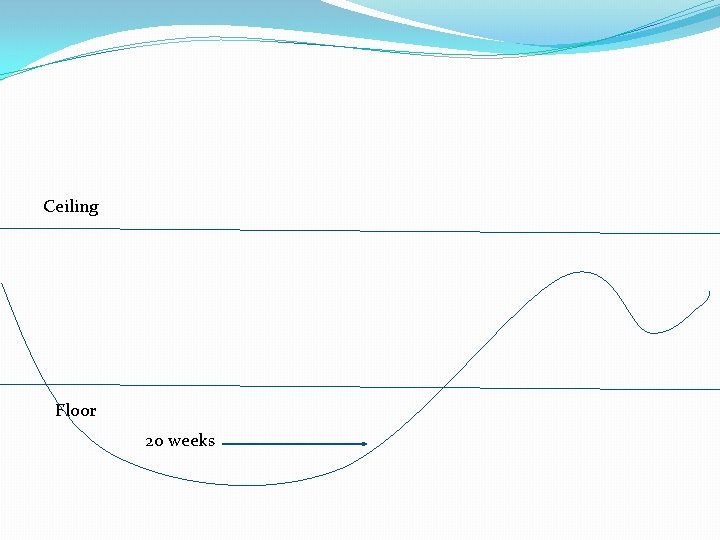
Ceiling Floor 20 weeks

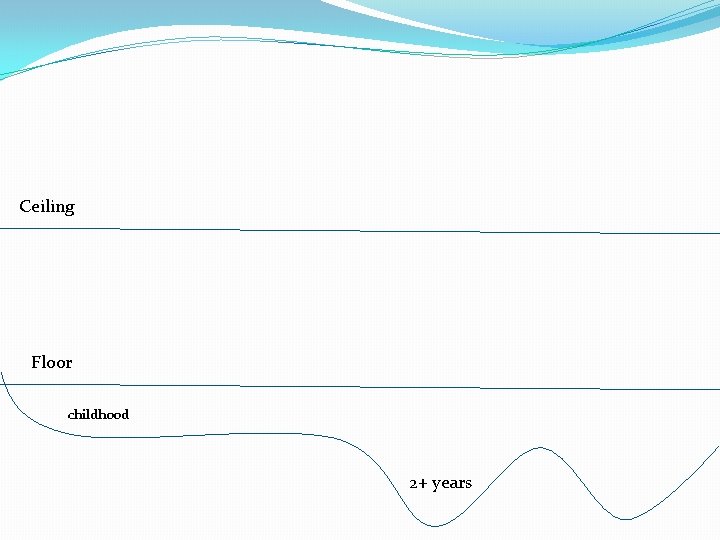
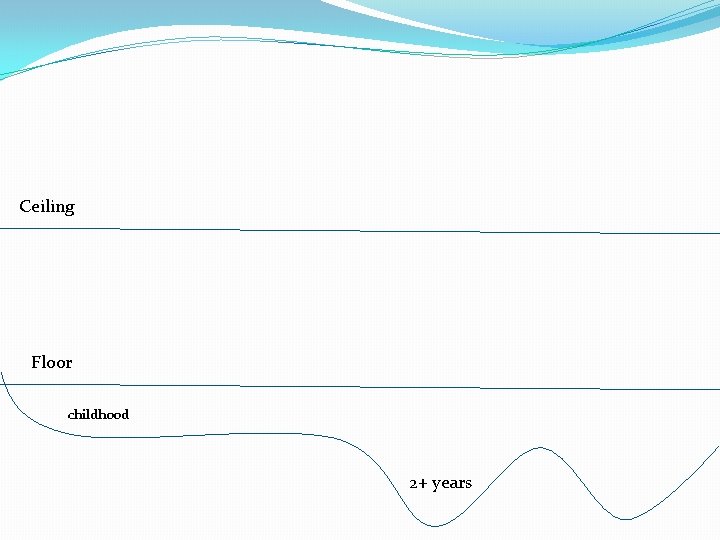
Ceiling Floor 2 + year
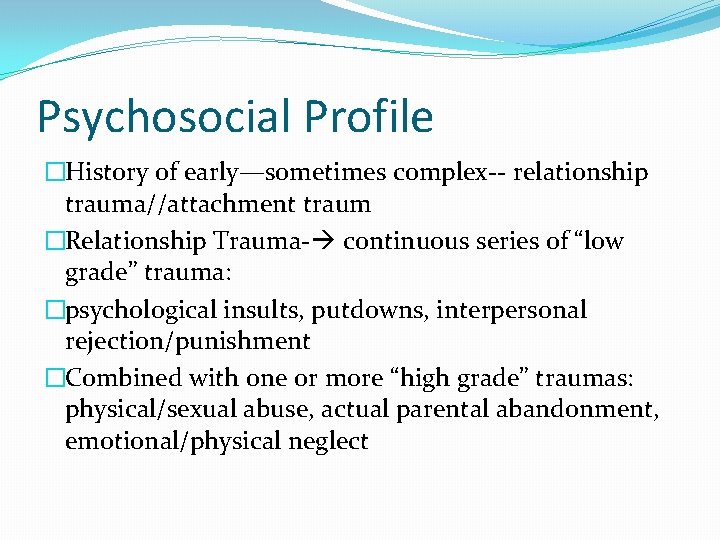
Ceiling Floor childhood 2+ years
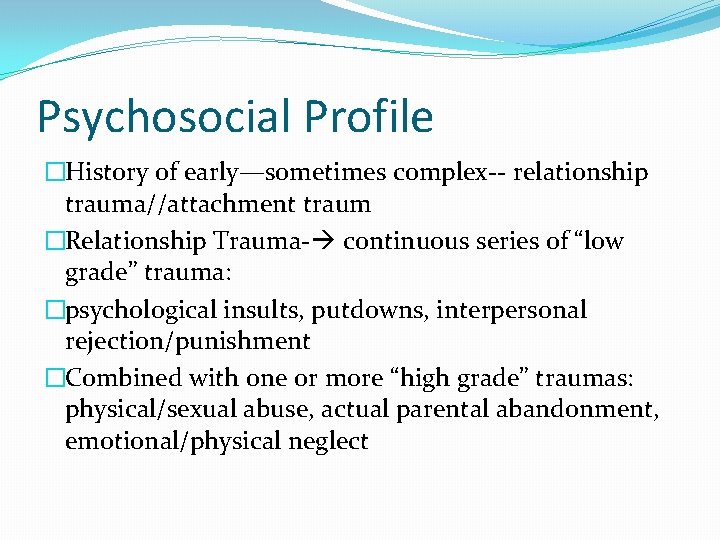
Psychosocial Profile �History of early—sometimes complex-- relationship trauma//attachment traum �Relationship Trauma- continuous series of “low grade” trauma: �psychological insults, putdowns, interpersonal rejection/punishment �Combined with one or more “high grade” traumas: physical/sexual abuse, actual parental abandonment, emotional/physical neglect
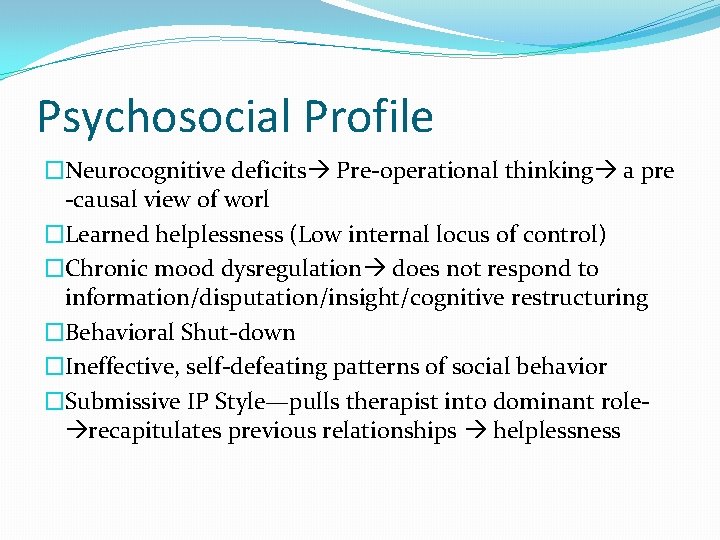
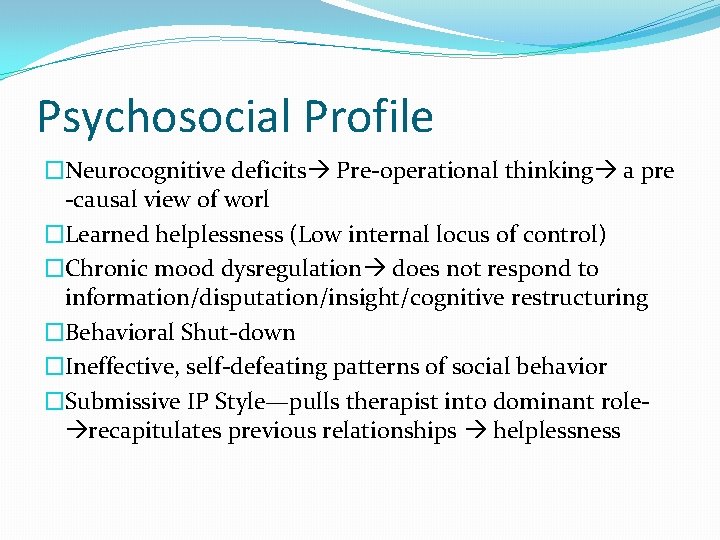
Psychosocial Profile �Neurocognitive deficits Pre-operational thinking a pre -causal view of worl �Learned helplessness (Low internal locus of control) �Chronic mood dysregulation does not respond to information/disputation/insight/cognitive restructuring �Behavioral Shut-down �Ineffective, self-defeating patterns of social behavior �Submissive IP Style—pulls therapist into dominant role recapitulates previous relationships helplessness
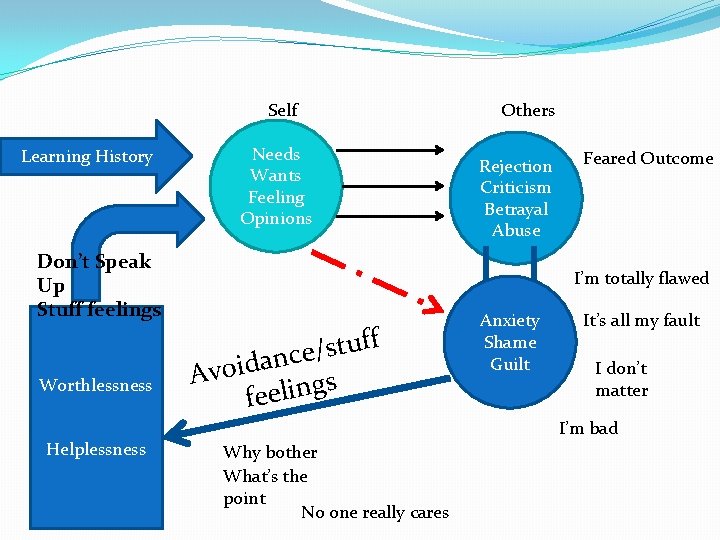
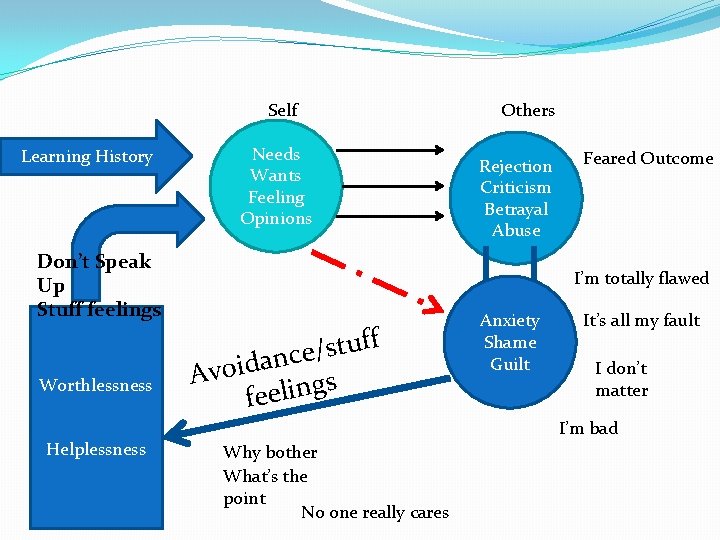
Self Learning History Don’t Speak Up Stuff feelings Worthlessness Helplessness Needs Wants Feeling Opinions Others Rejection Criticism Betrayal Abuse Feared Outcome I’m totally flawed f f u t s / e c n a d i Avo s g n i l e fe Anxiety Shame Guilt It’s all my fault I don’t matter I’m bad Why bother What’s the point No one really cares

e Learned Helplessness ls a n g Si in Bra Helplessness Sig n Bra als in I’m af Shut-down Energy Motivation Pleasure ur l i a I’m tired I’m worn out I’m use less Survival Mode Fight-Flight On-edge Irritable/angry Hypervigilant Something Bad is going to happen I’m going crazy I’m dying I can’t stand this
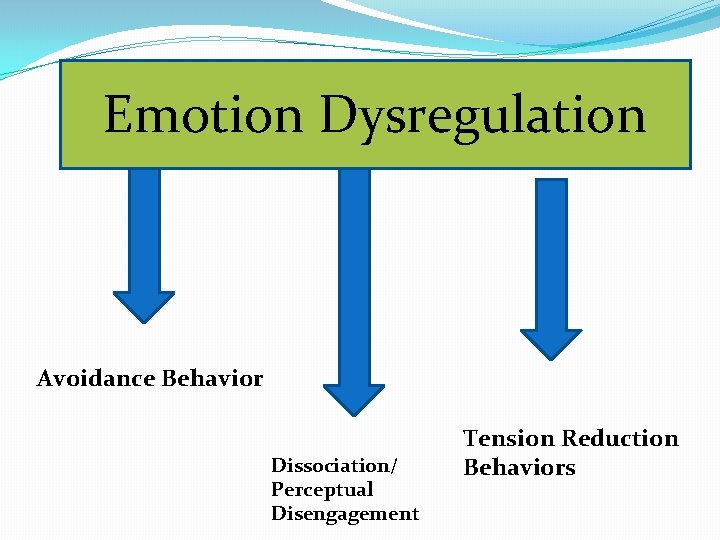
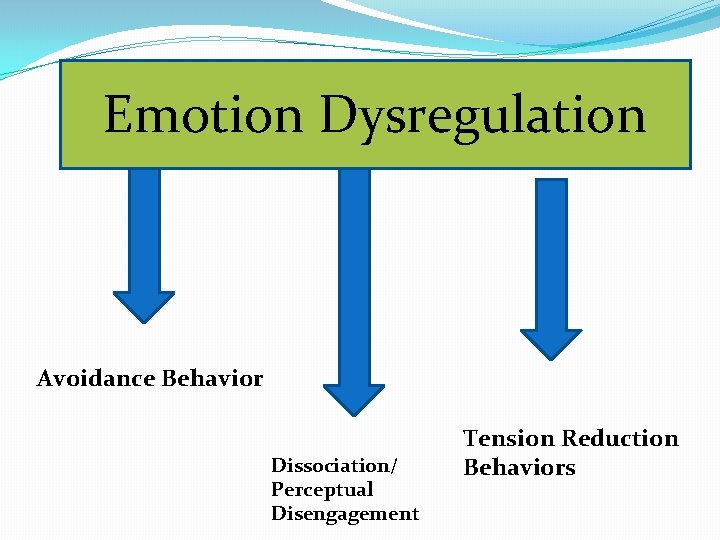
Emotion Dysregulation Avoidance Behavior Dissociation/ Perceptual Disengagement Tension Reduction Behaviors
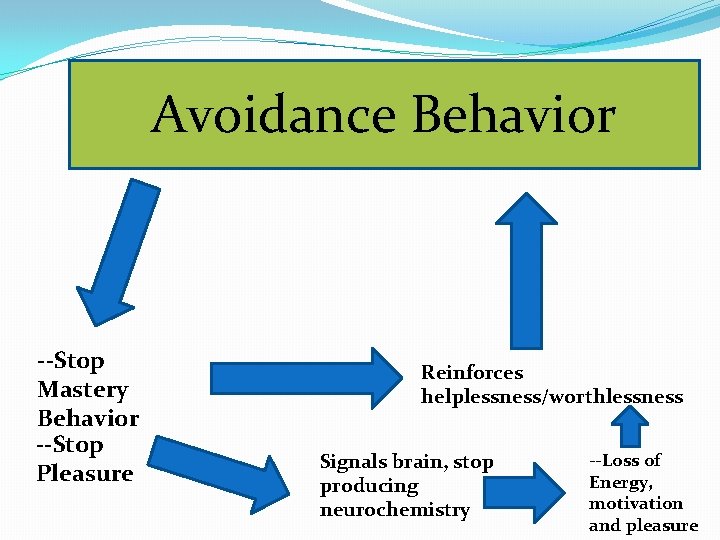
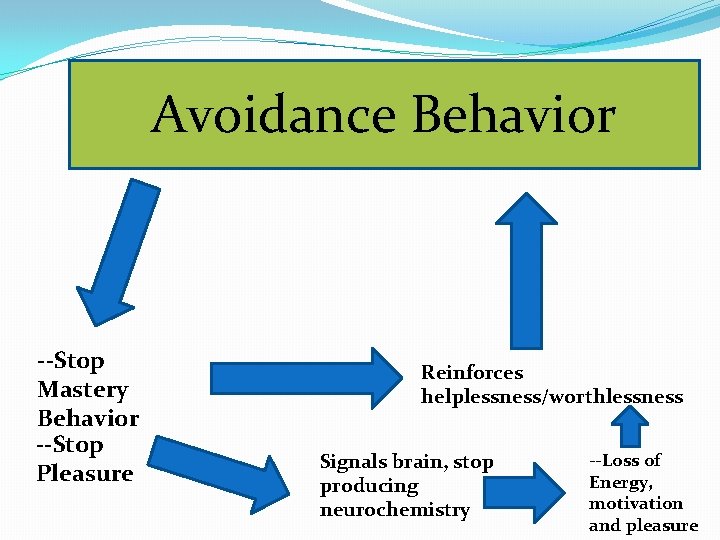
Avoidance Behavior --Stop Mastery Behavior --Stop Pleasure Reinforces helplessness/worthlessness Signals brain, stop producing neurochemistry --Loss of Energy, motivation and pleasure

Emotion Dysregulation Tension Reduction Behaviors Self mutilation Sexual acting out Suicide Fantasy Addictive Behavior
Psychosocial Profile � Mood Disorder learned and maintained by chronic and pervasive pattern of interpersonal avoidance. � Avoidance is fueled by attachment-based fear (i. e. , fear based on history of interpersonal learning in context of attachment relationships) where expression of self/attachment (wants, needs, emotions, and intentions) is repeated associated with attachment injuries and psychological insults delivered by attachment figures in the form of rejection, criticism, and blame. � Consequently, the person comes to associate the expression of self (including all attachment needs) with anxiety, shame, and guilt. A natural response to these feelings is avoidance behavior (stuffing of feelings). � This results in chronic feelings of worthlessness (“My feelings don’t matter”) and helplessness (“Nothing I do works so why try”). The biological consequence of these perceptions is the deactivation of motivation, energy, and pleasure (the brain is primarily and conservator of energy, thus when the perception is that nothing will work or change in turns off activation related neurotransmitters). It may also activate the brains survival mode, which results in chronic over-activation of the sympathetic nervous system, resulting in feelings of anxiety, tension, and irritability.
Neurocognitive Consequences �The neurobiological consequence of chronic emotion dysregulation is the disintegration of dendritic connections between PFC and various subcortical systems in limbic system, including hippocampus. �Degeneration of middle frontal areas of the brain and hippocampus impaired ability to attend to and contextualizing relationship events �Consequently, person relates in mindless fashion, repeating same old patterns of relationship experiences— ”Interpersonal Sameness” �Confirms feelings of hopelessness and helplessness �This interferes with the brains ability to form autobiographical memory and other neurocognitive deficits
Neurocognitive Deficits �These neurocognitive deficits are similar to deficits described in other research, including Theory of Mind, Mindsight, and Mentalization �Also similar to Piagetian concept of preoperational functioning: childlike ego-centric pattern of thinking where the individual is not influenced by external environment… �Failure of Perceptual Engagement—visually disengaged from social environment, using past experience to interpret present moment, thus creating the past in the present…continuous, interpersonal sameness.
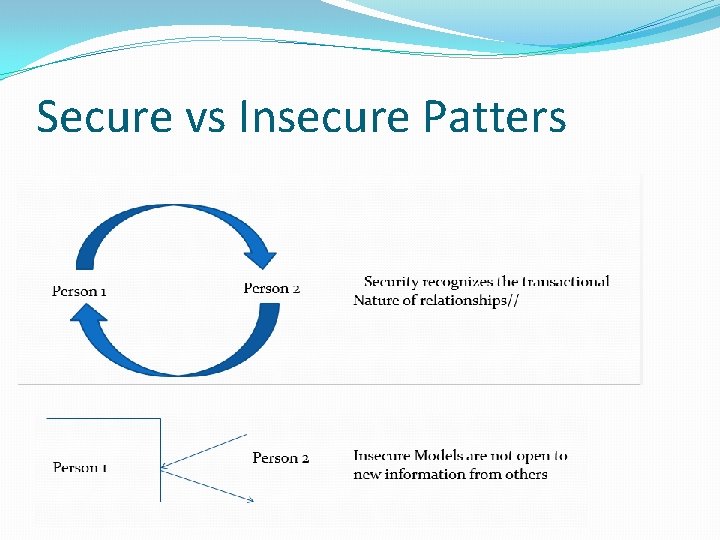
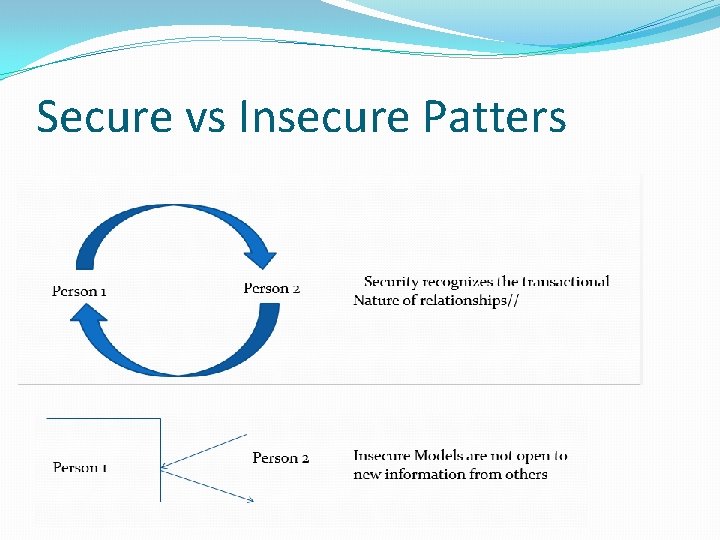
Secure vs Insecure Patters
No one appreciates what I do…why do I even help these people Thanks for all your help With the project Sure, anytime
Self-Defeating Patterns of Interpersonal Behavior �Fail to understand how they affect others and actually “pull” others into behaving exactly the way they expect others to behavior �They use the past to interpret the present �You keep getting the past in the present �Recapitulation of past in current relationship experiences

Dominance H o s t i l e Dominant Hostility Affiliation Dominant Friendly p o w e r Passive Hostility Affiliation Freindly Passivity F r i e n d l y
CBASP Treatment Components �The Significant Other History �Transference Hypothesis �Identification of “Hot Spot” �Disciplined Personal Involvement �Interpersonal Discrimination Exercises �Situation Analysis
Steps in Significant Other History �Identify Key Players �For each ask: �“what was/is it like being around this person? ” � Get examples of key words �“What has been the stamp this person has left on your life? �At the end Ask: �“Looking back on all these relationships, what is the affect you think they have had on who you are today. ”

Transference Hypothesis �Four Content Domains �Relational intimacy �Disclosure of private material �Mistakes �Feeling or expressing negative emotion �Formulate TH as highly probable interpersonal event (hot spots) which will trigger patient’s internal working model �Basic Model: �If I do x…Sibcy will…. .
Disciplined Personal Involvement/ Conditioned personal responsivity �Designed to penetrate patients interpersonal sameness through perceptual engagement �Confronting interpersonal behavior �Increasing Mentalization, understanding how his behavior effects others �Not using past to interpret the present �Usually will activate “Transference Hot Spot”
Interpersonal Discrimination Exercises �Hot spot activated �Draw attention to it �Ask how others would react to it �Ask how “you” reacted to it with them in session �Compare and contrast to past/others �Ask about implication for therapy �Ask about generalization to future
CBASP Situational Analysis �Uses Coping Survey Questionnaire �Two phases �Elicitation – SA used as an interpersonal, cognitive behavioral diagnostic tool �Remediation – Problematic behaviors are targeted for change and revised until new behaviors bring a desirable conclusion �Confronts avoidance and directs the patient’s attention to the interpersonal environment

CBASP Situational Analysis � Step 1: Describe what happened. (A brief “slice of time” with a beginning, an end, and a short story in between. ) � Step 2: Describe your interpretation of what happened (how did you “read” the situation? ). (A description of the process of the situation. ) � Step 3: Describe what you did during the situation (what you said/how you said it). (What someone else would have observed if they had been able to see you during this situation. ) � Step 4: Describe how the event came out for you (actual outcome). (Goes back to the end of the situation in Step 1) � Step 5: Describe how you wanted the event to come out for you (desired outcome). (Looking at the end point of this situation, what is the best you could do at that point? Remember, goals must be realistic and attainable. ) � Step 6: Was the desired outcome achieved? YES ___ NO ____ � Step 7: Why?
Situation Analysis �Situation�Interpretations�Behaviors�Actual Outcome�Desired Outcome�Did you get DO �Why?
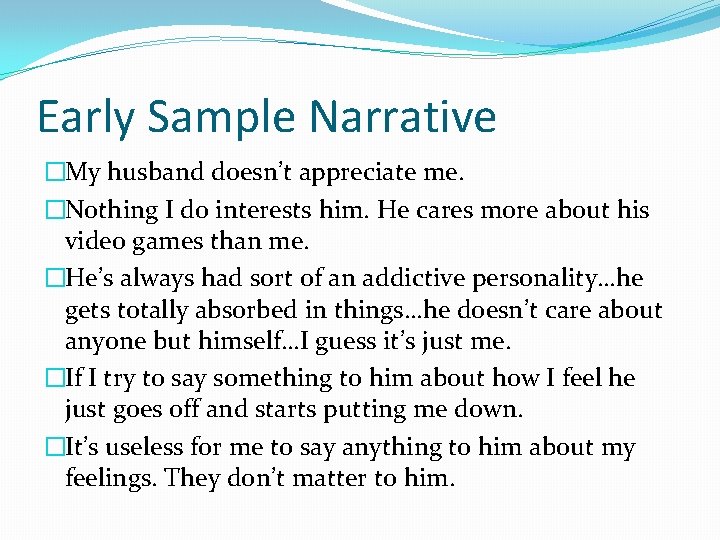
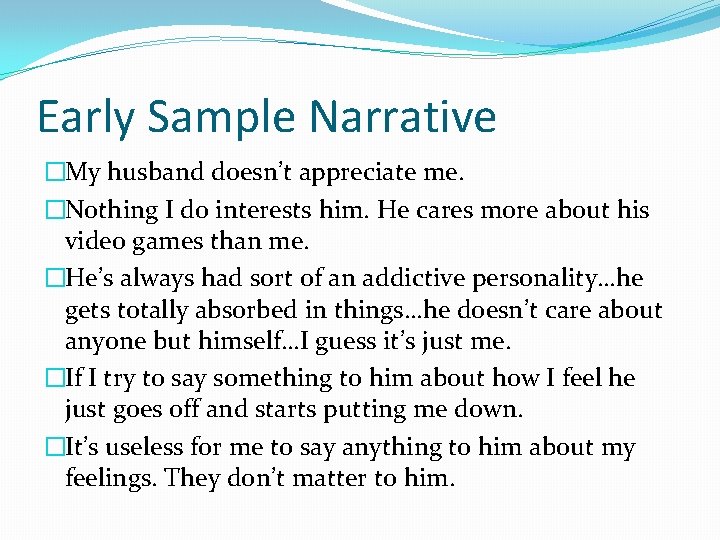
Early Sample Narrative �My husband doesn’t appreciate me. �Nothing I do interests him. He cares more about his video games than me. �He’s always had sort of an addictive personality…he gets totally absorbed in things…he doesn’t care about anyone but himself…I guess it’s just me. �If I try to say something to him about how I feel he just goes off and starts putting me down. �It’s useless for me to say anything to him about my feelings. They don’t matter to him.

Situation Analysis (session 6) �Situation: �At home eating dinner. �As soon as husband I finished dinner, he got up from the table and took his plate to sink. �Then he started to head down stairs. I asked him where he was going. �He said, “I think I’ll go play some war of aircraft. ” �I didn’t say anything but just nodded my head. �He turned and walked off downstairs.
SA (continue) �Interpretations: �He doesn’t love me �I must be such a bore �What’s the point…no one cares about what I need �Behavior: �I just nodded my head up and down and stared past him. Then I dropped it

SA continued �Actual Outcome: �I dropped it �Desired Outcome: �I want him to give up these stupid games �I want him to love me and care about me

SA �Revised DO: �To tell him: I really want to spend some time with you this evening…can we do that later? �Did you get DO? �No �Why? �I didn’t say anything to him
SA continued �Revise interpretations: �He doesn’t love me �I must be such a bore �What’s the point…no one cares about what I need �Revised Action Read: �Ask him to spend time; speak up �Be nice
Case Example: �Bill � 48 year-old accountant with chronic depression �Depressed his whole life �Numerous medications �Numerous therapists �Nothing helps
Sample Narrative �The other evening I decided to tell my husband my feelings about him spending so much time playing the video game. I told him that I felt he was addicted to the game and even told him there is research on how these games work like addictions. I also told him it was like he had a mistress and I couldn’t stand it anymore. He told me I was overreacting and that I blow everything out of proportion. He told me I needed to get a life. I just turned away and walked off.
What is the evidence �An FDA approved medication must demonstrate at least 2 large scale Randomized Controlled Treatment studies �Using clinically depressed patients who meet strict inclusion and exclusion criteria �Qualified patients were randomly assigned to one of two group: �Medication group �Placebo control group
Evidence �Depression is measured using standardized instruments– self report vs clinician rated �These are administered repeatedly over course of treatment to endpoint (usually 8 -12 weeks) �Usually use of fixed dose methods (e. g. , 20 mg Prozac). �Statistical Outcome: �Treatment group is compared to placebo to see if there was a “statistically significant difference” between treatment and control group (P<. 05)
The Problem �Statistical Significance does not equal Real Life Benefit �SS is affected by two factors �Number of people in the study �Everyone in the study is alike

An Integrative Model of Depression Behavioral Disturbances • Role Transitions • Loss/grief • Relationship disturbances • Loneliness • Type II Self Other/ world Genetics/biology X Early Relationship Experiences Negative Bias Insecure Working Models of Attachment X Social-Neuro-cognitive Skill Deficits Chronic Mood Dysregulation Future Focus Intervention