Treadmill Stress Testing for the Primary Care Physician
- Slides: 52
Treadmill Stress Testing for the Primary Care Physician Francis G. O’Connor, MD, MPH, FACSM Medical Director, Human Performance Lab Associate Professor of Family Medicine Uniformed Services University of the Health Sciences
Objectives Review essential Exercise Stress Test (EST) background, resources and terminology. Describe the performance of the EST. Describe common normal and abnormal responses to exercise testing. Discuss interpretation of the EST.
Exercise Stress Test Essentials
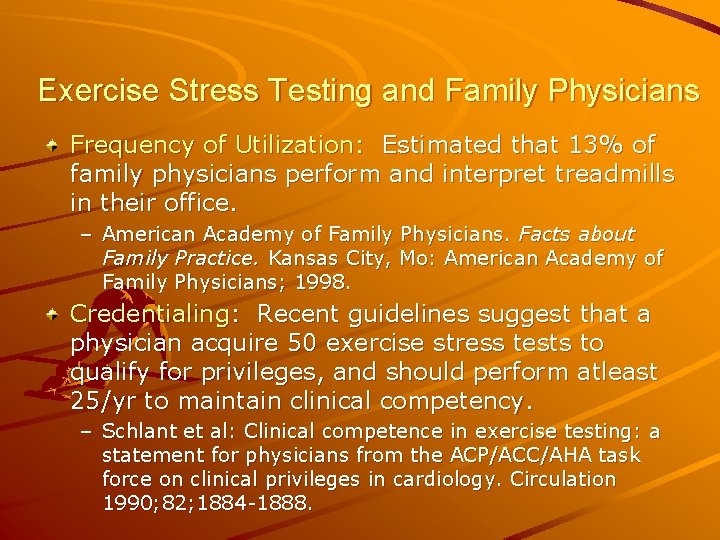
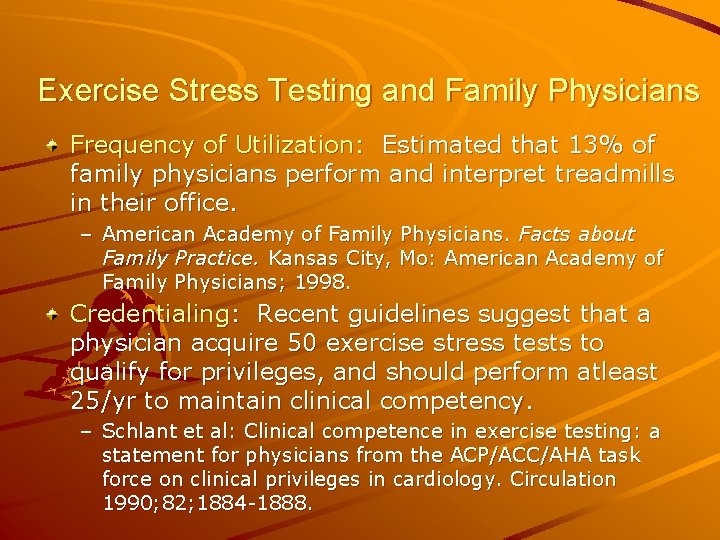
Exercise Stress Testing and Family Physicians Frequency of Utilization: Estimated that 13% of family physicians perform and interpret treadmills in their office. – American Academy of Family Physicians. Facts about Family Practice. Kansas City, Mo: American Academy of Family Physicians; 1998. Credentialing: Recent guidelines suggest that a physician acquire 50 exercise stress tests to qualify for privileges, and should perform atleast 25/yr to maintain clinical competency. – Schlant et al: Clinical competence in exercise testing: a statement for physicians from the ACP/ACC/AHA task force on clinical privileges in cardiology. Circulation 1990; 82; 1884 -1888.
Safety and Exercise Stress Testing The risk of death during or immediately after an exercise test is less than or equal to 0. 01%. The risk of an acute MI during or immediately after an exercise test is less than or equal to 0. 04%. The risk of a complication requiring hospitalization is less than or equal to 0. 2%.
References ACC/AHAQ Practice Guidelines – Fletcher GF et al: Exercise Standards: a statement for healthcare professionals from the American Heart Association Writing Group: Special Report. Circulation 1995; 91: 580 -615. – ACC/AHA Guidelines for Exercise Testing. A Report of the ACC/AHA Task Force on Practice Guidelines. JACC Vol. 30 (3): 260 -311. – Gibbons RJ et al: ACC/AHA 2002 guideline update for exercise testing: a report of the American College of Cardiology/American heart Association Task Force on Practice Guidelines 2002. www. acc. org/clinical/guidelines ACSM References – ACSM’s Guidelines for Exercise Testing and Prescription, Seventh Edition. – ACSM’s Resource Manual for Exercise Testing and Prescription, Seventh Edition.
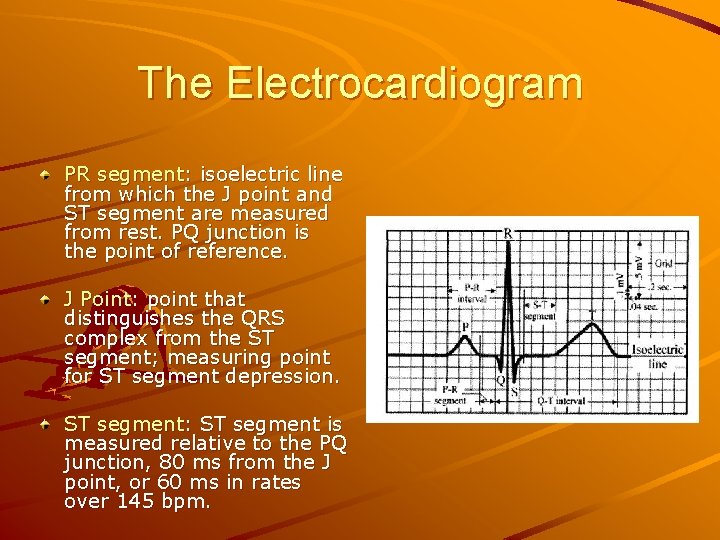
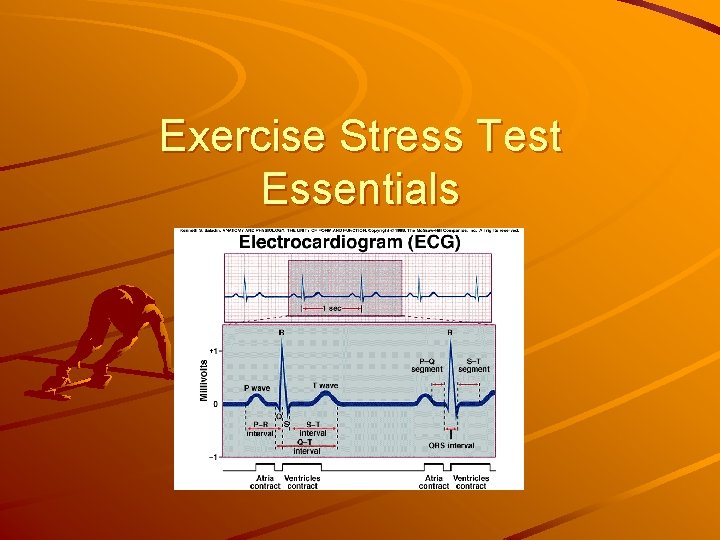
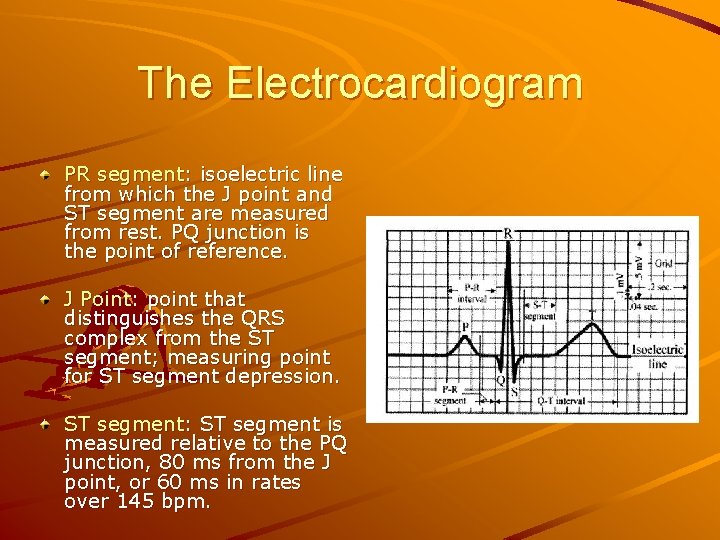
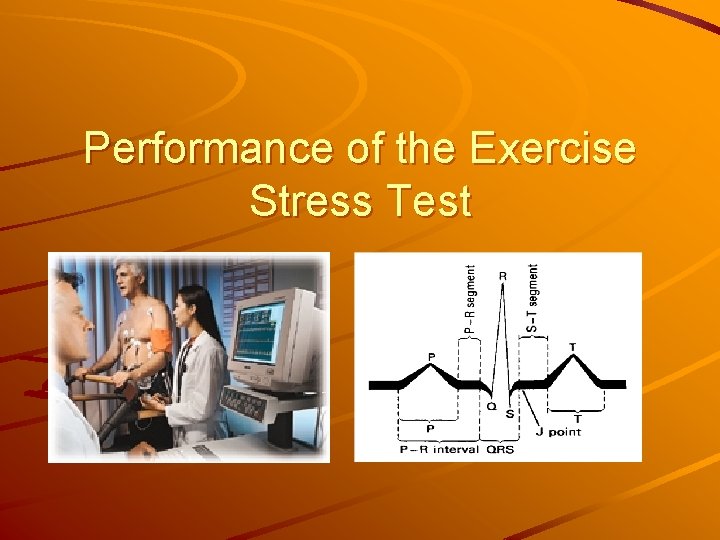
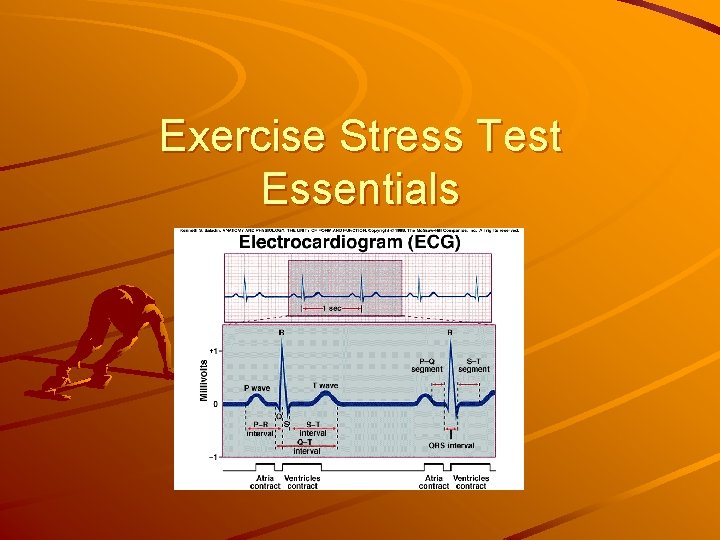
The Electrocardiogram PR segment: isoelectric line from which the J point and ST segment are measured from rest. PQ junction is the point of reference. J Point: point that distinguishes the QRS complex from the ST segment; measuring point for ST segment depression. ST segment: ST segment is measured relative to the PQ junction, 80 ms from the J point, or 60 ms in rates over 145 bpm.
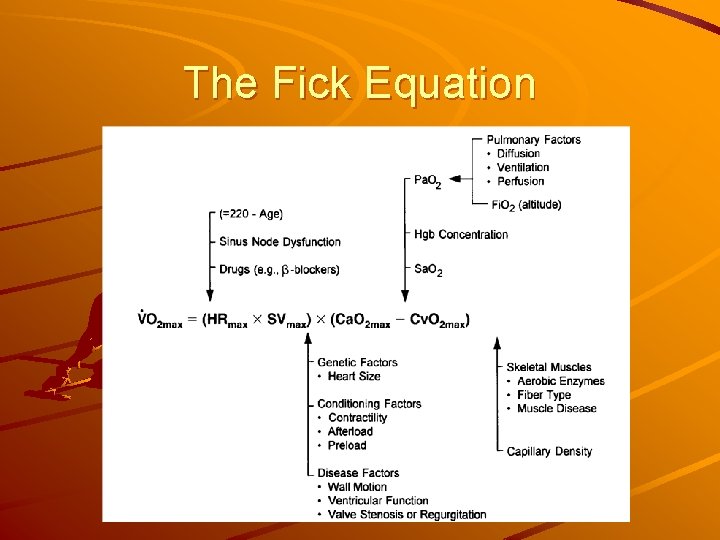
Exercise Physiology METs: oxygen uptake is conveniently expressed in METs; 3. 5 ml O 2/kg/min – 1 MET=rest; 5 MET=ADLs; 10 METs= medical therapy equivalent to CABG; 18 METS=elite athlete. Myocardial Oxygen Consumption: – Double product of HRx. SBP correlates with myocardial oxygen consumption. VO 2 MAX: – Fick Equation: VO 2 max = (HRmax x SV max) x (Ca. O 2 max – Cv. O 2 max) – Gold standard for aerobic fitness.
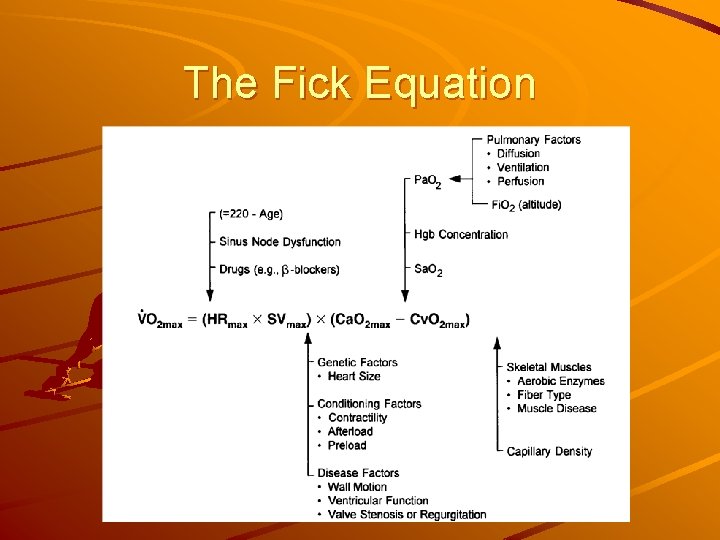
The Fick Equation
Performance of the Exercise Stress Test
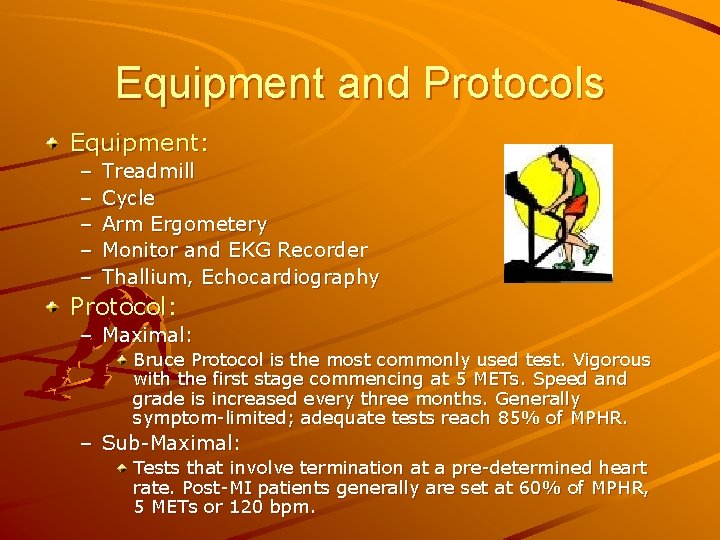
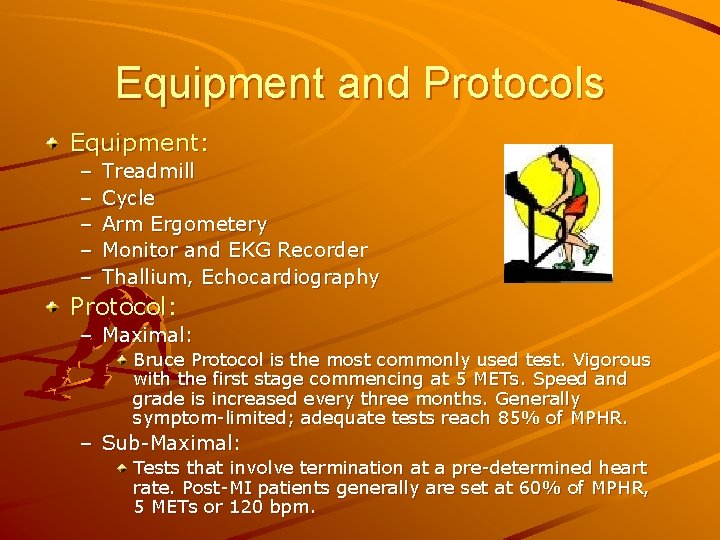
Equipment and Protocols Equipment: – – – Treadmill Cycle Arm Ergometery Monitor and EKG Recorder Thallium, Echocardiography Protocol: – Maximal: Bruce Protocol is the most commonly used test. Vigorous with the first stage commencing at 5 METs. Speed and grade is increased every three months. Generally symptom-limited; adequate tests reach 85% of MPHR. – Sub-Maximal: Tests that involve termination at a pre-determined heart rate. Post-MI patients generally are set at 60% of MPHR, 5 METs or 120 bpm.
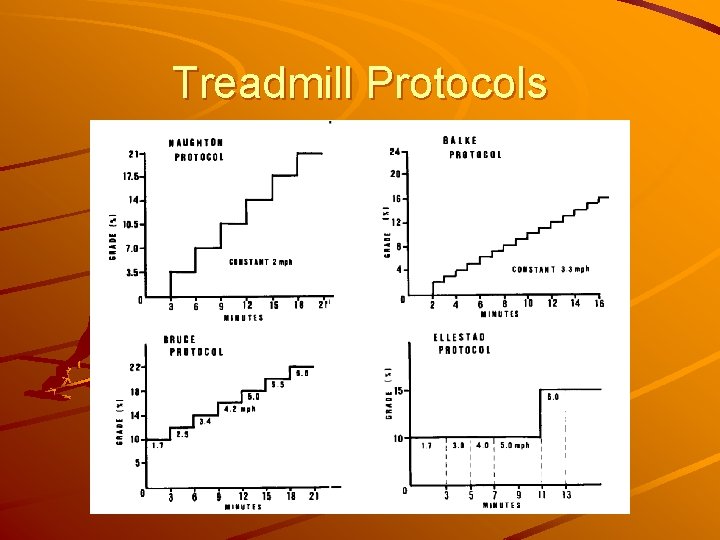
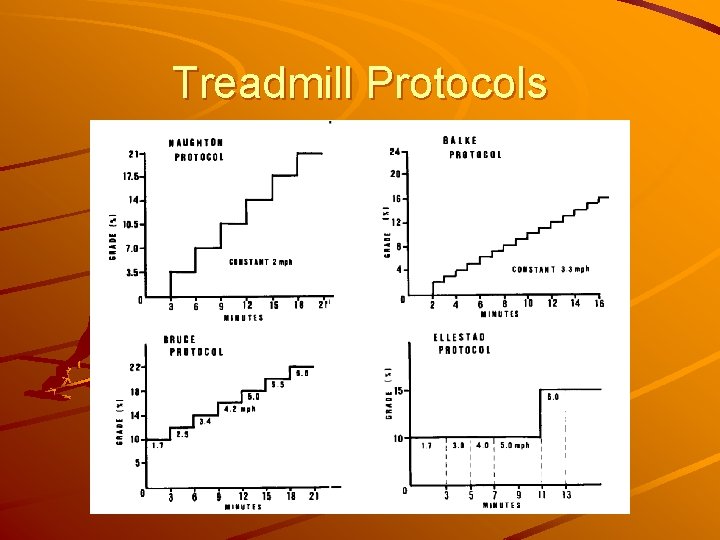
Treadmill Protocols
Indications ACC/AHA Guidelines for Exercise Testing – Class I: general consensus/evidence that testing is justified. – Class II: divergence of opinion on utility. IIa in favor; IIb less evidence. – Class III: agreement that testing is not warranted.
Indications: Diagnose Obstructive CAD Class I – Adult patients (including those with RBBB and 1 mm resting ST depression) with an intermediate pre-test probability of disease. Class IIa – Patients with vasospastic angina. Class IIb – Patients with a high or low pre-test probability of disease. – Patients with less than 1 mm ST depression and taking digoxin. – Patients with LVH by voltage and less than 1 mm of baseline ST depression. Class III – WPW; paced rhythm; >1 mm ST depression; LBBB.
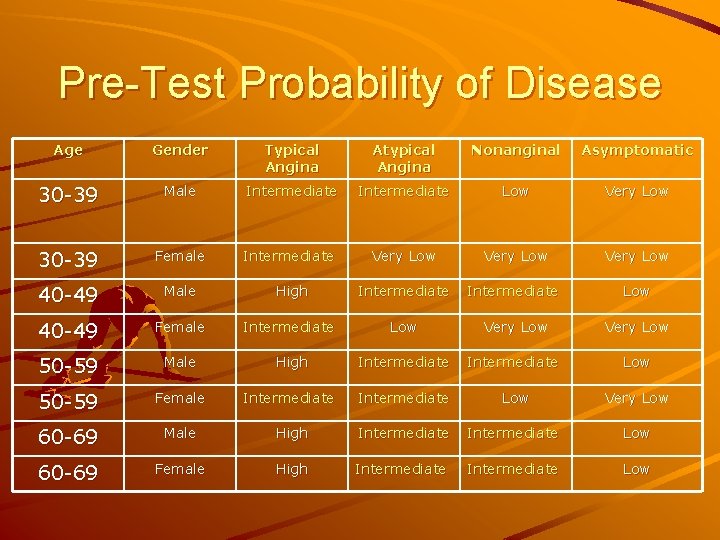
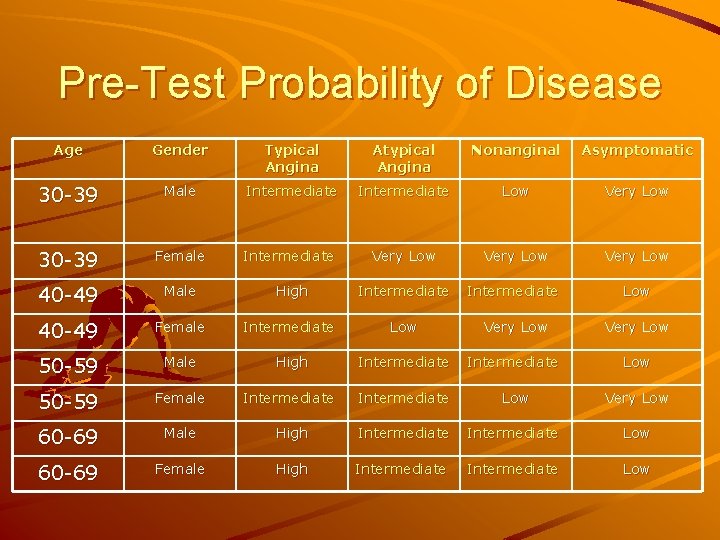
Pre-Test Probability of Disease Age Gender Typical Angina Atypical Angina Nonanginal Asymptomatic 30 -39 Male Intermediate Low Very Low 30 -39 Female Intermediate Very Low 40 -49 Male High Intermediate Low 40 -49 Female Intermediate Low Very Low 50 -59 Male High Intermediate Low 50 -59 Female Intermediate Low Very Low 60 -69 Male High Intermediate Low 60 -69 Female High Intermediate Low
ACSM Recommendations for Exercise Testing Prior to Exercise Participation CAD Risk Factors – FH: MI in 1 st degree male relative before 55; female before 65. – Smoker or quit within 6 months. – Hypertension – Hypercholesterolemia: TCHOL > 200; HDL <35; LDL > 130. – Impaired fasting glucose: >110. – Obesity: BMI >30. – Sedentary – HDL >60 is a negative risk factor. CAD Signs/Symptoms – Pain in the chest, neck, jaw, arms that may be due to ischemia – SOB at rest or exertion – Dizziness or syncope – Orthopnea/PND – Ankle edema – Claudication – Known heart murmur – Unusual fatigue or SOB with usual activities
ACSM Recommendations for Exercise Testing Prior to Exercise Participation Initial ACSM Risk Stratification – Low Risk: younger individuals who are asymptomatic and have no more than one risk factor. – Moderate Risk: older or those who meet the threshold for two or more risk factors. – High Risk: individual with signs or symptoms of CAD, or known cardiovascular, pulmonary, or metabolic disease Old versus Young – Men < 45 years of age; Women < 55. Moderate versus Vigorous Exercise – Moderate: 3 -6 METs, 40 to 60% maximal oxygen uptake. – Vigorous: >6 METs, or 60% maximal oxygen uptake.
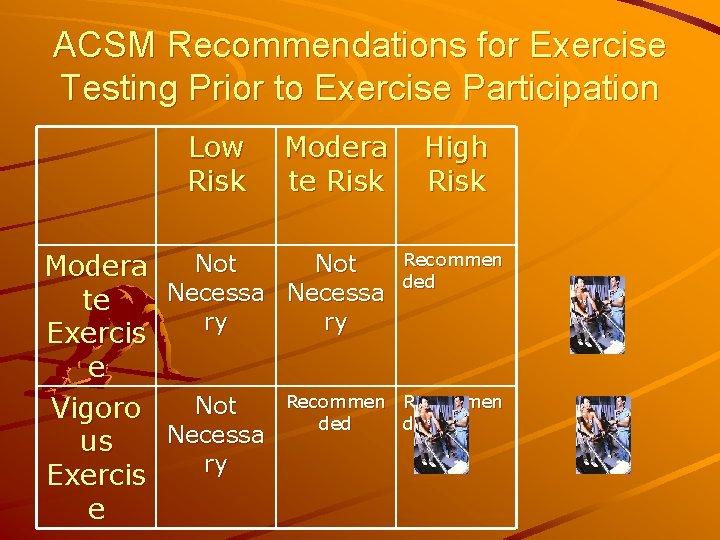
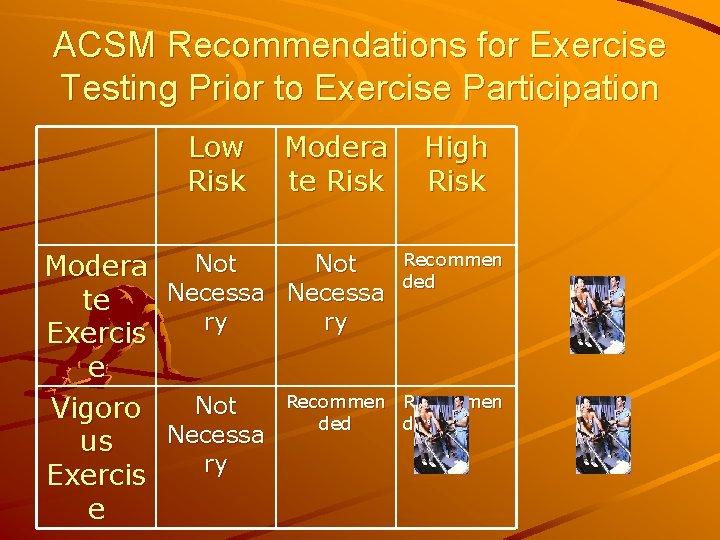
ACSM Recommendations for Exercise Testing Prior to Exercise Participation Low Risk Modera te Risk Not Modera Necessa te ry ry Exercis e Recommen Not Vigoro ded Necessa us ry Exercis e High Risk Recommen ded
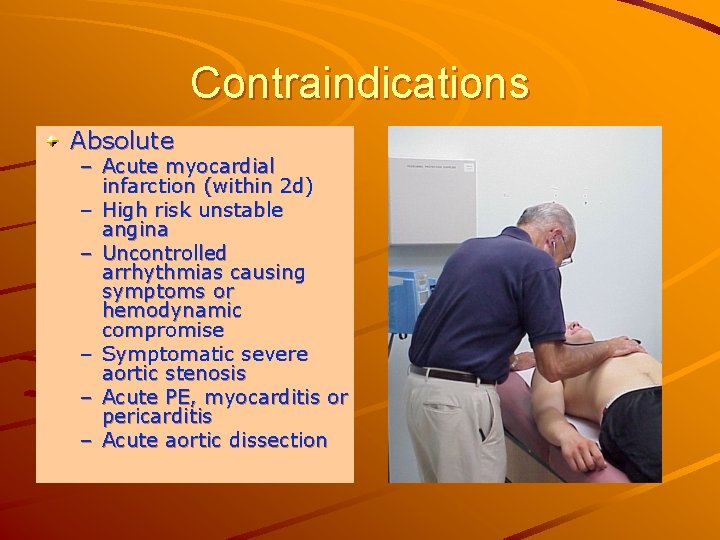
Contraindications Absolute – Acute myocardial infarction (within 2 d) – High risk unstable angina – Uncontrolled arrhythmias causing symptoms or hemodynamic compromise – Symptomatic severe aortic stenosis – Acute PE, myocarditis or pericarditis – Acute aortic dissection
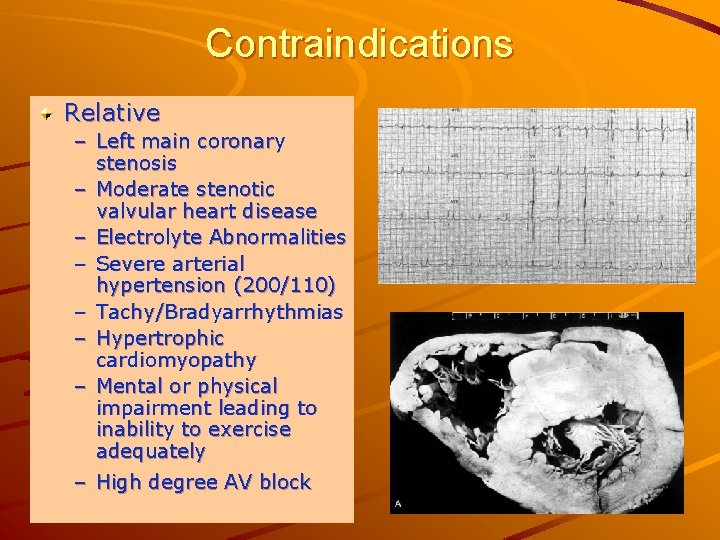
Contraindications Relative – Left main coronary stenosis – Moderate stenotic valvular heart disease – Electrolyte Abnormalities – Severe arterial hypertension (200/110) – Tachy/Bradyarrhythmias – Hypertrophic cardiomyopathy – Mental or physical impairment leading to inability to exercise adequately – High degree AV block
Special Considerations Medications – Beta blockers: blunt HR response; short acting held the day of the test; long acting held two days. – Calcium channel blockers: delay ischemia, decreasing sensitivity of the test. – Digoxin: produces abnormal ST depression with exercise. – Diuretics: may cause ST depression with hypokalemia. Conduction Disturbances – High degree AV block (Mobitz II and third degree block) should not be tested. – LBBB and WPW preclude interpretation of ischemia and should not be tested. Special Clinical Situations – Severe arthritis/Obesity: consider pharmacologic stress testing. – Hypertension: don’t test 200/120 – Q waves: in post MI pts, ST elevation can indicate a hypokinetic ventricle.
Physician Responsibilities During the Test Patient Evaluation and Clearance – Careful history of symptoms and past medical history; typical vs. atypical. – Risk factors – Family history – Informed Consent Physical Examination – – Vital signs Cardiovascular: murmurs, gallops – Lungs Selection of Protocol – – Maximal vs. Sub-Maximal Treadmill vs. Cycle
Performing the Test Preparing the Patient Monitoring the Patient Terminating the Test Recovery of the Patient
Preparing the Patient Instructions: – No eating two hours before test; no consumption of alcohol, caffeine, or tobacco three hrs before. – Comfortable clothing. – Medications determined by functional vs. diagnostic testing. Skin Preparation – Hair shaved; abrasive rub; “tap” test. Appropriate Blood Pressure cuff. Consent.
Preparing the Patient Pre-Test Checklist – Equipment and safety check – Informed Consent – Pre-test history and physical examination – Electrode skin preparation – Resting ECG reviewed – Standing ECG and BP – Patient Demonstration – Patient Questions
Monitoring the Patient Pre-Test – 12 lead ECG supine and standing. – BP supine and standing. Exercise – 12 lead last 15 sec of each stage. – BP and RPE at the end of each stage. Post-Test – 12 lead ECG immediately after exercise, then every 1 to 2 minutes until return to baseline. – BP: immediately after exercise, then every 1 to 2 minutes until return to baseline. – Follow symptoms. Borg RPE Scale – – – – 6 7 Very, very light 8 9 Very light 10 11 Fairly light 12 13 Somewhat hard 14 15 Hard 16 17 Very hard 18 19 Very, very hard 20
Terminating the Test All treadmill stress tests should be completed to a symptom-limited endpoint, if possible. 85% of maximal predicted heart rate is required to identify a test as adequate.
Indications for Test Termination Absolute – Drop in SBP of >10 mm. Hg from baseline, despite increased workload, when accompanied by other ischemia – Moderate to severe angina – Increasing ataxia, dizziness, or presyncope – Signs of poor perfusion – Technical difficulties – Subjects desire – Sustained Vtach – ST elevation in leads without diagnostic Q waves
Indications for Test Termination Relative – Drop in SBP of >10 mm. Hg from baseline, despite increased workload – ST depression >2 mm from baseline – Multifocal PVCs, triplets, SVT, heart block – Fatigue, shortness of breath, wheezing, leg cramps – Bundle branch block – Increasing chest pain – Hypertensive response
Recovery of the Patient Have the patient lie down and continuously observe. Auscultate for abnormal heart and lung sounds. Monitor until clinically stable and electrocardiogram has returned to normal. ECG changes in recovery just as ominous as those occurring during exercise.
Common Normal Responses to Exercise Testing Symptoms – Typical anginal symptoms can be produced by testing and increase the prognostic value of a test. – Symptoms, however, do not define a positive test, and define a test “suggestive of ischemia. ” – Opportunity for “anginal threshold” determination and use of Borg Scale for exercise prescription.
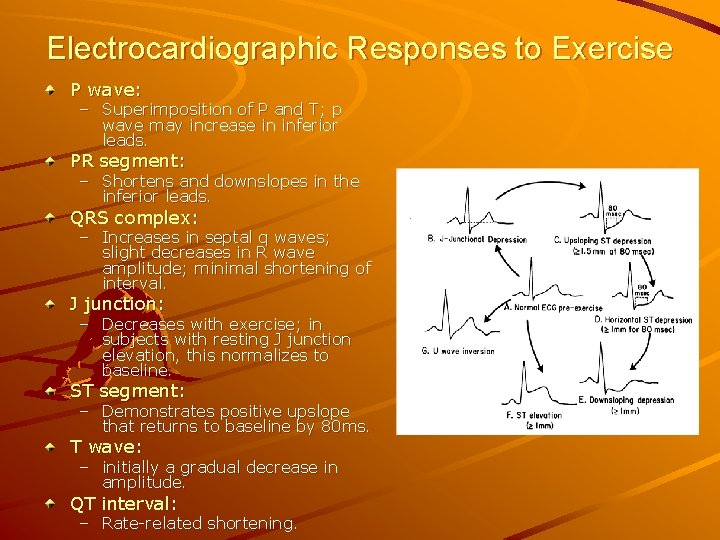
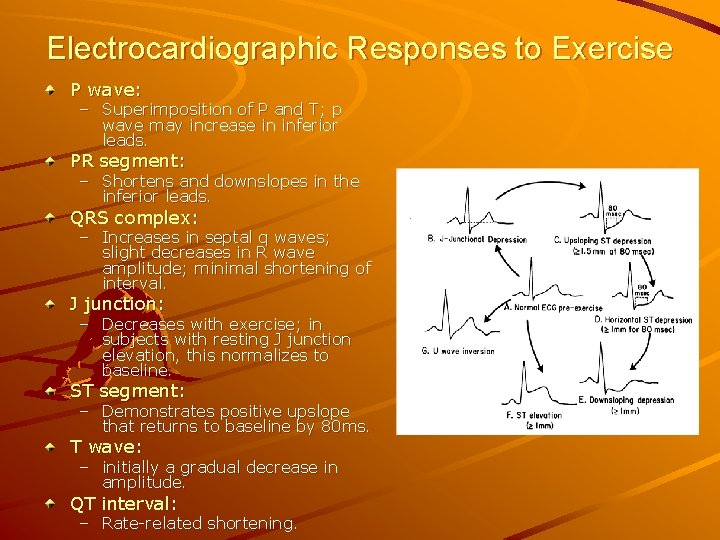
Electrocardiographic Responses to Exercise P wave: – Superimposition of P and T; p wave may increase in inferior leads. PR segment: – Shortens and downslopes in the inferior leads. QRS complex: – Increases in septal q waves; slight decreases in R wave amplitude; minimal shortening of interval. J junction: – Decreases with exercise; in subjects with resting J junction elevation, this normalizes to baseline. ST segment: – Demonstrates positive upslope that returns to baseline by 80 ms. T wave: – initially a gradual decrease in amplitude. QT interval: – Rate-related shortening.
Heart Rate Normal Heart Rate Response – Increase in HR as a result of vagal tone withdrawal. – Standard deviation for peak HR determination is 15 BPM. Chronotropic Incompetence – Peak heart rate less than 120 BPM. – Failure to achieve 85% of age-predicted maximum. Heart Rate Recovery
Heart Rate Recovery Following the GXT, patients walked for 2 minutes at 1. 5 mph and at a grade of 2. 5%. Heart rate recovery was the difference in heart rate at peak exercise and one minute into recovery; 12/min or less was considered abnormal. 9454 patients were followed for a median of 5 years; 20 % had abnormal heart rate recovery; they represented 8% of deaths vs. 2%; hazard ratio of 4. 16. Heart rate recovery is an independent predictor of mortality. Heart Rate Recovery and Treadmill Exercise Score as Predictors of Mortality in Patients Referred for Exercise ECG Nishime EO, et al: JAMA, September 20, 2000. Vo 284, No 11, 2000.
Blood Pressure Normal: – Systolic increases during exercise; returns to baseline by five to six minutes in recovery. Hypotensive Response to Exercise: – A drop in BP to baseline levels during exercise; poor prognosis. Hypertensive Response to Exercise: – Systolic greater than 220 mm. Hg, or rise in diastolic of > 10 mm. Hg, or Stage II age predicted 95% DBP. Singh et al: BP response during treadmill testing as a risk factor for new-onset hypertension. Circulation. 1999; 99: 1831 -1836. Blood Pressure in Recovery: – 3 Minute Systolic BP Ratio: SBP 3 min/ SBP Peak > 0. 91 is abnormal. Taylor et al: Postexercise systolic BP response: clinical application to the assessment of ischemic heart disease. American Family Physician. Vol 58(5).
Common Abnormal Responses to Exercise Stress Testing
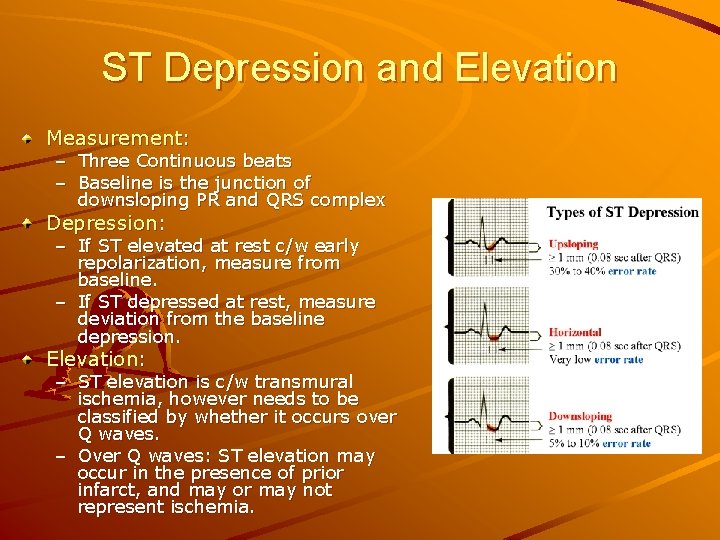
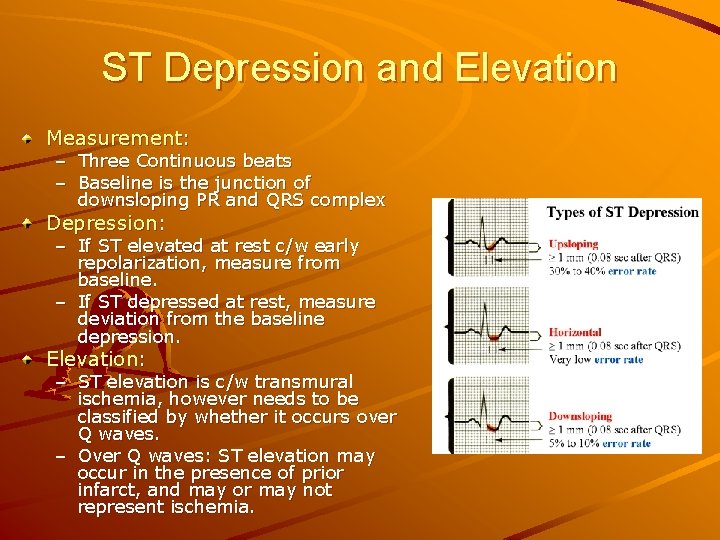
ST Depression and Elevation Measurement: – Three Continuous beats – Baseline is the junction of downsloping PR and QRS complex Depression: – If ST elevated at rest c/w early repolarization, measure from baseline. – If ST depressed at rest, measure deviation from the baseline depression. Elevation: – ST elevation is c/w transmural ischemia, however needs to be classified by whether it occurs over Q waves. – Over Q waves: ST elevation may occur in the presence of prior infarct, and may or may not represent ischemia.
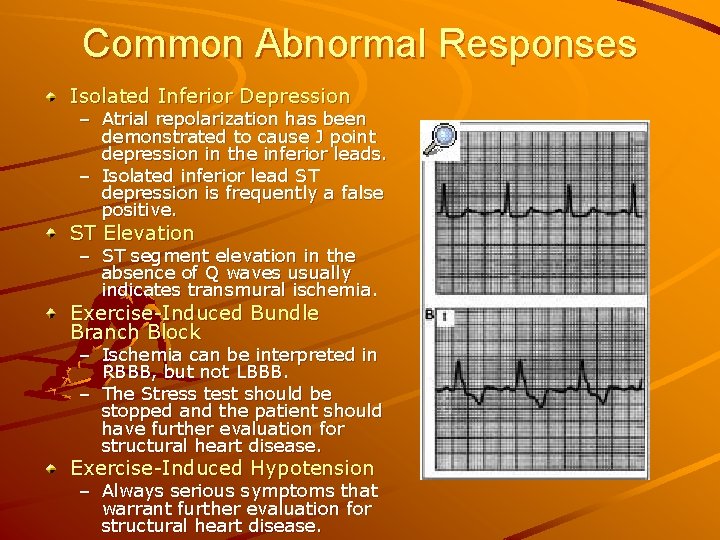
Common Abnormal Responses Isolated Inferior Depression – Atrial repolarization has been demonstrated to cause J point depression in the inferior leads. – Isolated inferior lead ST depression is frequently a false positive. ST Elevation – ST segment elevation in the absence of Q waves usually indicates transmural ischemia. Exercise-Induced Bundle Branch Block – Ischemia can be interpreted in RBBB, but not LBBB. – The Stress test should be stopped and the patient should have further evaluation for structural heart disease. Exercise-Induced Hypotension – Always serious symptoms that warrant further evaluation for structural heart disease.
Common Abnormal Responses Exercise-Induced Arrhythmias – Simple PVCs: not uncommon; low grade ectopy, unifocal, and infrequent PVCs during exercise do not increase risk. – Complex Arrhythmias: complex arrhythmias at low levels, in particular when associated with ischemia, warrant further evaluation. – Ventricular Tachycardia: require termination of the test, with prognosis based upon status of underlying heart disease. – Paroxysmal Atrial Tachycardia/PSVT: treated as patients who develop PSVT without exercise.
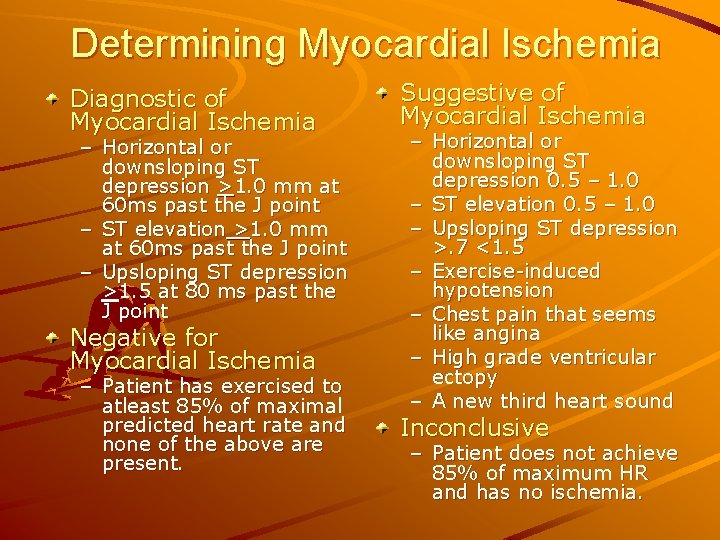
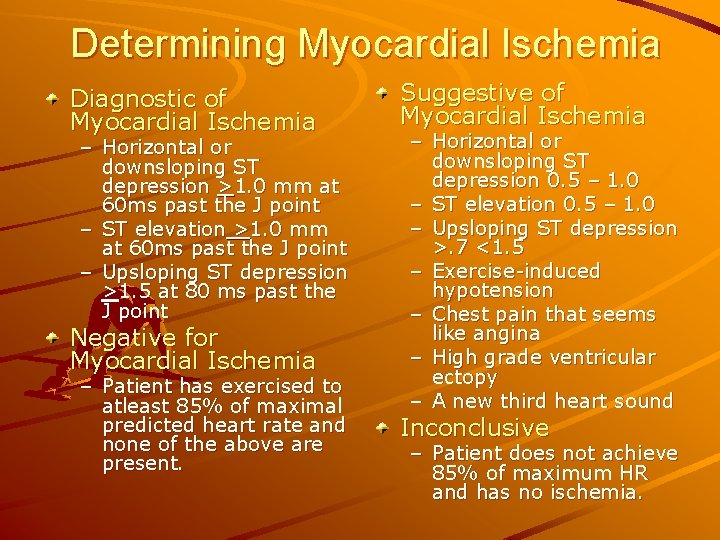
Determining Myocardial Ischemia Diagnostic of Myocardial Ischemia – Horizontal or downsloping ST depression >1. 0 mm at 60 ms past the J point – ST elevation >1. 0 mm at 60 ms past the J point – Upsloping ST depression >1. 5 at 80 ms past the J point Negative for Myocardial Ischemia – Patient has exercised to atleast 85% of maximal predicted heart rate and none of the above are present. Suggestive of Myocardial Ischemia – Horizontal or downsloping ST depression 0. 5 – 1. 0 – ST elevation 0. 5 – 1. 0 – Upsloping ST depression >. 7 <1. 5 – Exercise-induced hypotension – Chest pain that seems like angina – High grade ventricular ectopy – A new third heart sound Inconclusive – Patient does not achieve 85% of maximum HR and has no ischemia.
The Final Report First Paragraph: (General Summary) – Pt’s age, indication for testing, cardiac medications and protocol. – Baseline heart rate, BP and resting ECG findings. – Peak exercise data, BP, HR, peak METs, RPE and reason for stopping. – Description of abnormalities in ECG response, hemodynamics, dysrhythmias, or symptoms Second Paragraph: (Assessment) – – – Presence or absence of ischemia Normal or abnormal HR/BP response Presence of dysrhythmias Presence of symptoms Maximal aerobic capacity
Interpretation of the Exercise Stress Test
Bayes Theorem Theory of Conditional Probability – The predictive value of a test depends upon the descriptors of the test accuracy as well as the prevalence of disease in the population being tested. Patients with an abnormal test and a low pre-test probability of disease are at risk for a false-positive. Patients with a normal test and a high pre-test probability of disease are at risk for a false negative test. – The treadmill is thought to have a sensitivity of 70% and a specificity of 80% for diagnosing CAD.
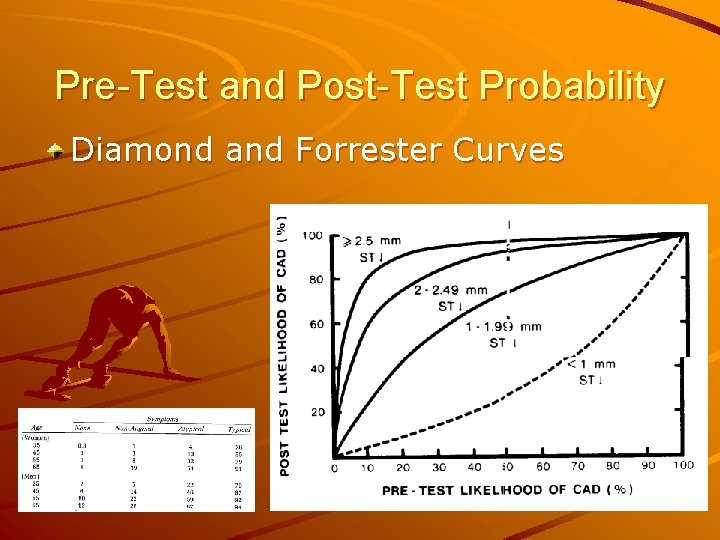
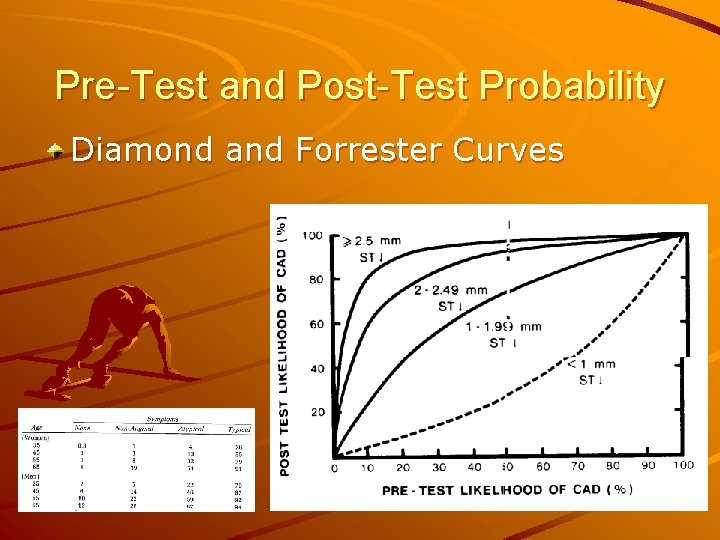
Pre-Test and Post-Test Probability Diamond and Forrester Curves
Common Errors False-Negative Tests – Failure to reach an adequate workload – Insufficient number of leads – Single vessel disease – Good collateral circulation – Technical or observer error False-Positive Tests – Pre-existing abnormal ECG – Cardiac hypertrophy – WPW and other conduction abnormalities – Drugs – Cardiomyopathy – Hypokalemia – Vasoregulatory abnormalities – Mitral valve prolapse – Pericardial disorders – Pectus excavatum – Coronary spasm – Anemia – Female gender – Observer error
Predicting Severity of Disease Electrocardiographic Responses – ST depression > 2. 5 mm – ST depression beginning at 5 METs or less – Downsloping ST depression or ST elevation – ST depression lasting more than 8 minutes into recovery – Serious dysrhythmias at a low heart rate – ST depression in more than 5 leads Nonelectrocardiographic Response – Chronotropic incompetence – Exercise-induced hypotension – Inability to exercise past 5 METs
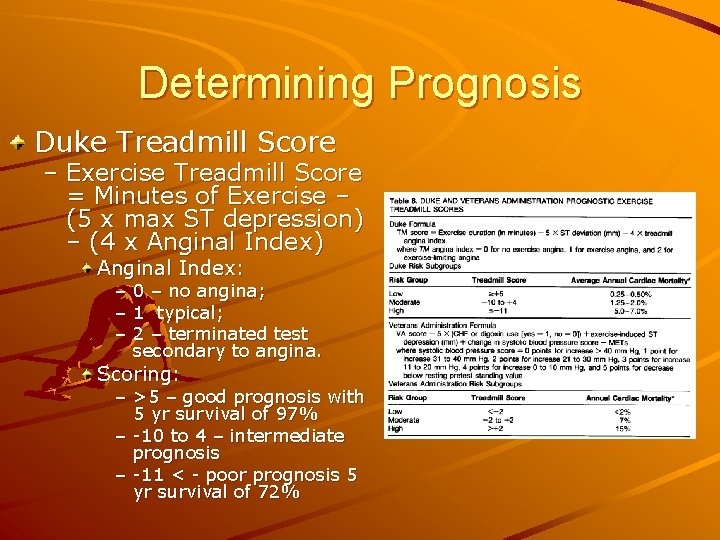
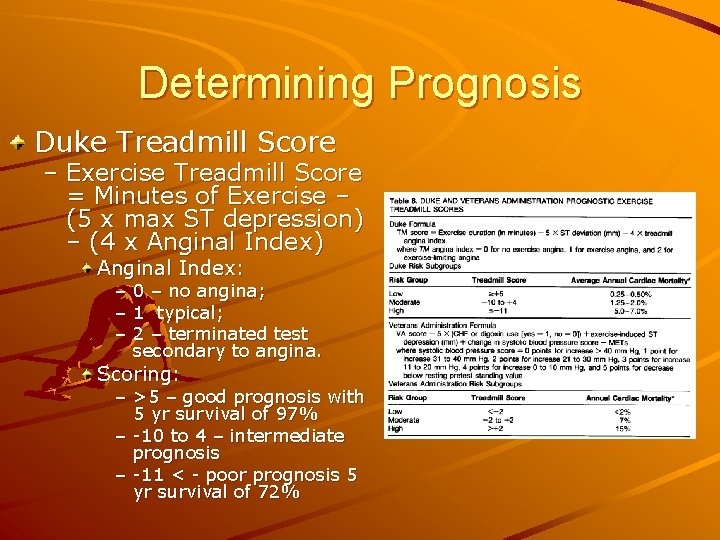
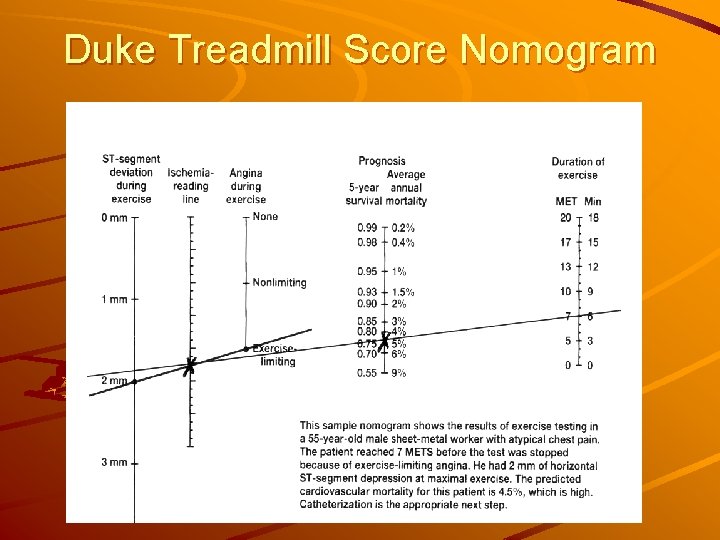
Determining Prognosis Duke Treadmill Score – Exercise Treadmill Score = Minutes of Exercise – (5 x max ST depression) – (4 x Anginal Index) Anginal Index: – 0 – no angina; – 1 typical; – 2 – terminated test secondary to angina. Scoring: – >5 – good prognosis with 5 yr survival of 97% – -10 to 4 – intermediate prognosis – -11 < - poor prognosis 5 yr survival of 72%
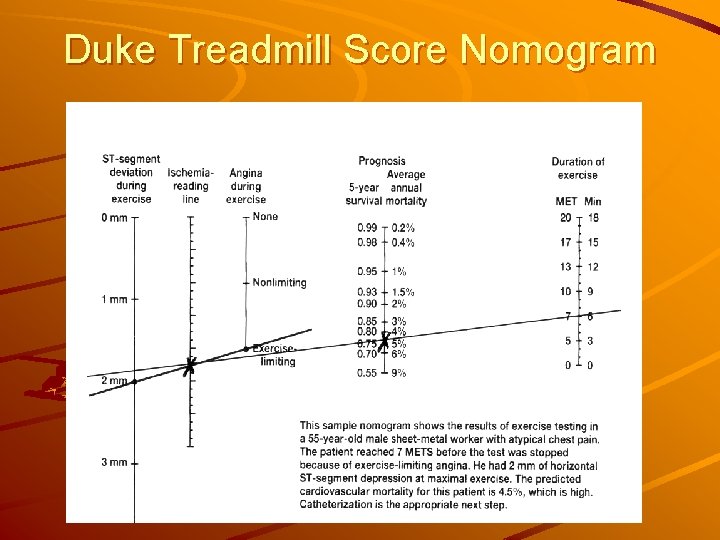
Duke Treadmill Score Nomogram
Function is Everything!
Summary