Traumatic Pneumothorax Chest Xray vs eFAST Abstract Number
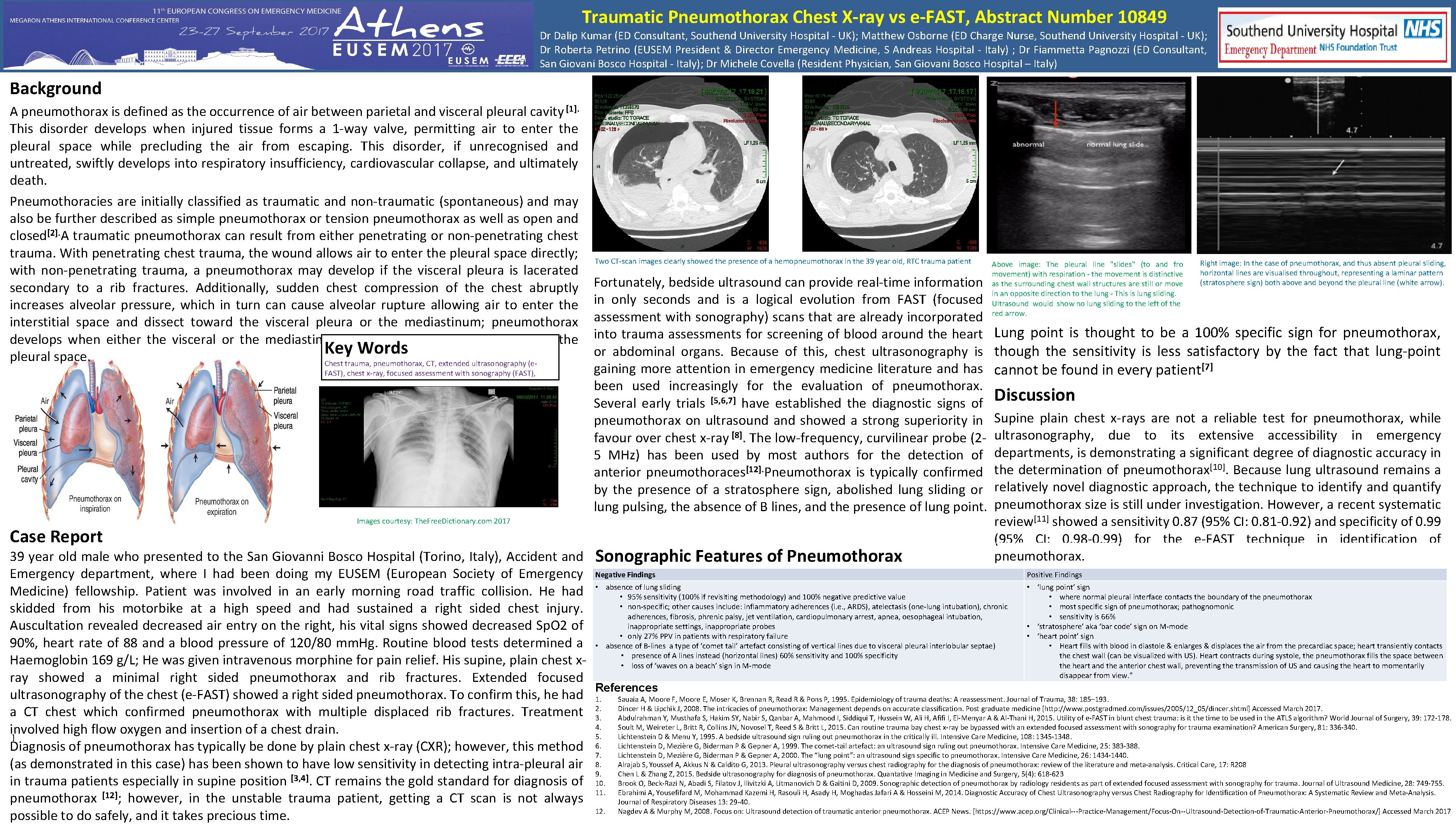
Traumatic Pneumothorax Chest X-ray vs e-FAST, Abstract Number 10849 Dr Dalip Kumar (ED Consultant, Southend University Hospital - UK); Matthew Osborne (ED Charge Nurse, Southend University Hospital - UK); Dr Roberta Petrino (EUSEM President & Director Emergency Medicine, S Andreas Hospital - Italy) ; Dr Fiammetta Pagnozzi (ED Consultant, San Giovani Bosco Hospital - Italy); Dr Michele Covella (Resident Physician, San Giovani Bosco Hospital – Italy) Background A pneumothorax is defined as the occurrence of air between parietal and visceral pleural cavity [1]. This disorder develops when injured tissue forms a 1 -way valve, permitting air to enter the pleural space while precluding the air from escaping. This disorder, if unrecognised and untreated, swiftly develops into respiratory insufficiency, cardiovascular collapse, and ultimately death. Pneumothoracies are initially classified as traumatic and non-traumatic (spontaneous) and may also be further described as simple pneumothorax or tension pneumothorax as well as open and closed[2]. A traumatic pneumothorax can result from either penetrating or non-penetrating chest trauma. With penetrating chest trauma, the wound allows air to enter the pleural space directly; with non-penetrating trauma, a pneumothorax may develop if the visceral pleura is lacerated secondary to a rib fractures. Additionally, sudden chest compression of the chest abruptly increases alveolar pressure, which in turn cause alveolar rupture allowing air to enter the interstitial space and dissect toward the visceral pleura or the mediastinum; pneumothorax develops when either the visceral or the mediastinal pleura ruptures, permitting air into the Key Words pleural space. Chest trauma, pneumothorax, CT, extended ultrasonography (e. FAST), chest x-ray, focused assessment with sonography (FAST), Case Report Two CT-scan images clearly showed the presence of a hemopneumothorax in the 39 year old, RTC trauma patient Fortunately, bedside ultrasound can provide real-time information in only seconds and is a logical evolution from FAST (focused assessment with sonography) scans that are already incorporated into trauma assessments for screening of blood around the heart or abdominal organs. Because of this, chest ultrasonography is gaining more attention in emergency medicine literature and has been used increasingly for the evaluation of pneumothorax. Several early trials [5, 6, 7] have established the diagnostic signs of pneumothorax on ultrasound and showed a strong superiority in favour over chest x-ray [8]. The low-frequency, curvilinear probe (25 MHz) has been used by most authors for the detection of anterior pneumothoraces[12]. Pneumothorax is typically confirmed by the presence of a stratosphere sign, abolished lung sliding or lung pulsing, the absence of B lines, and the presence of lung point. Images courtesy: The. Free. Dictionary. com 2017 Above image: The pleural line "slides" (to and fro movement) with respiration - the movement is distinctive as the surrounding chest wall structures are still or move in an opposite direction to the lung - This is lung sliding. Ultrasound would show no lung sliding to the left of the red arrow. Right image: In the case of pneumothorax, and thus absent pleural sliding, horizontal lines are visualised throughout, representing a laminar pattern (stratosphere sign) both above and beyond the pleural line (white arrow). Lung point is thought to be a 100% specific sign for pneumothorax, though the sensitivity is less satisfactory by the fact that lung-point cannot be found in every patient[7] Discussion Supine plain chest x-rays are not a reliable test for pneumothorax, while ultrasonography, due to its extensive accessibility in emergency departments, is demonstrating a significant degree of diagnostic accuracy in the determination of pneumothorax[10]. Because lung ultrasound remains a relatively novel diagnostic approach, the technique to identify and quantify pneumothorax size is still under investigation. However, a recent systematic review[11] showed a sensitivity 0. 87 (95% CI: 0. 81 -0. 92) and specificity of 0. 99 (95% CI: 0. 98 -0. 99) for the e-FAST technique in identification of pneumothorax. 39 year old male who presented to the San Giovanni Bosco Hospital (Torino, Italy), Accident and Sonographic Features of Pneumothorax Positive Findings Emergency department, where I had been doing my EUSEM (European Society of Emergency Negative Findings • ‘lung point’ sign Medicine) fellowship. Patient was involved in an early morning road traffic collision. He had • absence of lung sliding • 95% sensitivity (100% if revisiting methodology) and 100% negative predictive value • where normal pleural interface contacts the boundary of the pneumothorax • non-specific; other causes include: inflammatory adherences (i. e. , ARDS), atelectasis (one-lung intubation), chronic • most specific sign of pneumothorax; pathognomonic skidded from his motorbike at a high speed and had sustained a right sided chest injury. adherences, fibrosis, phrenic palsy, jet ventilation, cardiopulmonary arrest, apnea, oesophageal intubation, • sensitivity is 66% inappropriate settings, inappropriate probes • ‘stratosphere’ aka ‘bar code’ sign on M-mode Auscultation revealed decreased air entry on the right, his vital signs showed decreased Sp. O 2 of • only 27% PPV in patients with respiratory failure • ‘heart point’ sign 90%, heart rate of 88 and a blood pressure of 120/80 mm. Hg. Routine blood tests determined a • absence of B-lines a type of ‘comet tail’ artefact consisting of vertical lines due to visceral pleural interlobular septae) • Heart fills with blood in diastole & enlarges & displaces the air from the precardiac space; heart transiently contacts • presence of A lines instead (horizontal lines) 60% sensitivity and 100% specificity the chest wall (can be visualized with US). Heart contracts during systole, the pneumothorax fills the space between Haemoglobin 169 g/L; He was given intravenous morphine for pain relief. His supine, plain chest x • loss of ‘waves on a beach’ sign in M-mode the heart and the anterior chest wall, preventing the transmission of US and causing the heart to momentarily Authors disappear from view. ” Dr Dalip Kumar, MBBS (ED Consultant-Southend University Hospital) ray showed a minimal right sided pneumothorax and rib fractures. Extended focused Matthew Osborne, RN, Dip. He, BSc, PGCert, PGDip (ED Charge Nurse- Southend University Hospital) References ultrasonography of the chest (e-FAST) showed a right sided pneumothorax. To confirm this, he had 1. Sauaia A, Moore F, Moore E, Moser K, Brennan R, Read R & Pons P, 1995. Epidemiology of trauma deaths: A reassessment. Journal of Trauma, 38: 185– 193. Dr Mohammad Abu Watfa, Mu Dr (ED Consultant-Southend University Hospital) Dr Caroline Howard, MBBS, MRCP, FCEM ( Clinical Director and Consultant ED-Southend University Hospital) 2. Dincer H & Lipchik J, 2008. The intricacies of pneumothorax: Management depends on accurate classification. Post graduate medicine [http: //www. postgradmed. com/issues/2005/12_05/dincer. shtml] Accessed March 2017. a CT chest which confirmed pneumothorax with multiple displaced rib fractures. Treatment 3. Abdulrahman Y, Musthafa S, Hakim SY, Nabir S, Qanbar A, Mahmood I, Siddiqui T, Hussein W, Ali H, Afifi I, El-Menyar A & Al-Thani H, 2015. Utility of e-FAST in blunt chest trauma: is it the time to be used in the ATLS algorithm? World Journal of Surgery, 39: 172 -178. Dr Claire Willis, MBBS, MRCS {A&E Ed}, FCEM (ED Consultant-Southend University Hospital) Dr Dilshad Al-Sheikh, MBCHB, Dip. Med (U. K. ), MRCEM ( Locum ED Consultant-Southend University Hospital) 4. Soult M, Weireter L, Britt R, Collins JN, Novosel T, Reed S & Britt L, 2015. Can routine trauma bay chest x-ray be bypassed with an extended focused assessment with sonography for trauma examination? American Surgery, 81: 336 -340. involved high flow oxygen and insertion of a chest drain. 5. Lichtenstein D & Menu Y, 1995. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Intensive Care Medicine, 108: 1345 -1348. ]. Diagnosis of pneumothorax has typically be done by plain chest x-ray (CXR); however, this method 6. 7. Lichtenstein D, Mezière G, Biderman P & Gepner A, 1999. The comet-tail artefact: an ultrasound sign ruling out pneumothorax. Intensive Care Medicine, 25: 383 -388. Lichtenstein D, Mezière G, Biderman P & Gepner A, 2000. The “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Medicine, 26: 1434 -1440. (as demonstrated in this case) has been shown to have low sensitivity in detecting intra-pleural air 8. Alrajab S, Youssef A, Akkus N & Caldito G, 2013. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Critical Care, 17: R 208 9. Chen L & Zhang Z, 2015. Bedside ultrasonography for diagnosis of pneumothorax. Quantative Imaging in Medicine and Surgery, 5(4): 618 -623 in trauma patients especially in supine position [3, 4]. CT remains the gold standard for diagnosis of 10. Brook O, Beck-Razi N, Abadi S, Filatov J, Ilivitzki A, Litmanovich D & Gaitini D, 2009. Sonographic detection of pneumothorax by radiology residents as part of extended focused assessment with sonography for trauma. Journal of Ultrasound Medicine, 28: 749 -755. 11. Ebrahimi A, Yousefifard M, Mohammad Kazemi H, Rasouli H, Asady H, Moghadas Jafari A & Hosseini M, 2014. Diagnostic Accuracy of Chest Ultrasonography versus Chest Radiography for Identification of Pneumothorax: A Systematic Review and Meta-Analysis. [12] pneumothorax ; however, in the unstable trauma patient, getting a CT scan is not always Journal of Respiratory Diseases 13: 29 -40. 12. Nagdev A & Murphy M, 2008. Focus on: Ultrasound detection of traumatic anterior pneumothorax. ACEP News. [https: //www. acep. org/Clinical---Practice-Management/Focus-On--Ultrasound-Detection-of-Traumatic-Anterior-Pneumothorax/] Accessed March 2017 possible to do safely, and it takes precious time.
- Slides: 1