Traumatic childbirth and its effects on mental health
Traumatic childbirth and its effects on mental health: Navigating an “Uncertain Road Ahead”
Disclosure �I have no actual or potential conflict of interest in relation to this presentation.
Objectives � Describe the unique interplay of variables that result in traumatic birth � Identify risk factors for traumatic birth � Discuss outcomes of traumatic birth on breastfeeding and subsequent pregnancies � Describe postpartum post-traumatic stress disorder and potential avenues for provider intervention
“I left the hospital with my life and my daughter, so ostensibly I am a success story. However, as my nurse wheeled me through the hospital doors and out into the warm sun of early spring, I knew I was but a shell of my former self, with an uncertain road ahead. ” - Michelle Hall, Ed. D, LPCC-S
Hannah’s Story � The patient is a 35 yo married Caucasian G 2 P 1 woman with Celiac disease who was referred by her OB for worsening anxiety during pregnancy. Patient notes that she had a difficult and traumatic delivery 3 years ago, during which she had complications secondary to placenta accreta with extensive postpartum hemorrhage resulting from retained products of conception.
“My first birth was traumatic. ” � For the first 6 -8 weeks following delivery, Hannah had recurrent medical admissions for bleeding requiring multiple hysteroscopies. She notes repeatedly having to present to the ER to be taken seriously by staff who attempted to reassure her when she would call her OB office in distress: “It’s like they thought I was stupid. ” She ultimately transferred care during her postpartum with an OB she found to be a better fit.
“I want to be happy I’m pregnant, but I’m scared. ” � She now returns with mixed feelings about current pregnancy, which was planned and desired. She had been managed well with a combination of sertraline and individual therapy, but since discovering this pregnancy has become more symptomatic. � She expresses significant fears about her delivery and is hoping for an elective Caesarean. At her last OB appointment, concern was raised for recurrent accreta, and patient’s distress led her doctor to refer her for a psychiatric assessment.
“I would just think to myself, ‘Why me? ’” � She has flashbacks to her delivery frequently (triggers included seeing food trays in the hospital, smelling hospital soap, watching birth scenes on television). Regularly had nightmares of her delivery on the nights prior to medical appointments during postpartum, though this has improved with current pregnancy. She notes poor sleep, irritability, tearfulness and anxiety with panic symptoms though no discrete attacks. � Patient reports 1 prior episode of depression in her early teens which resolved spontaneously after several months.
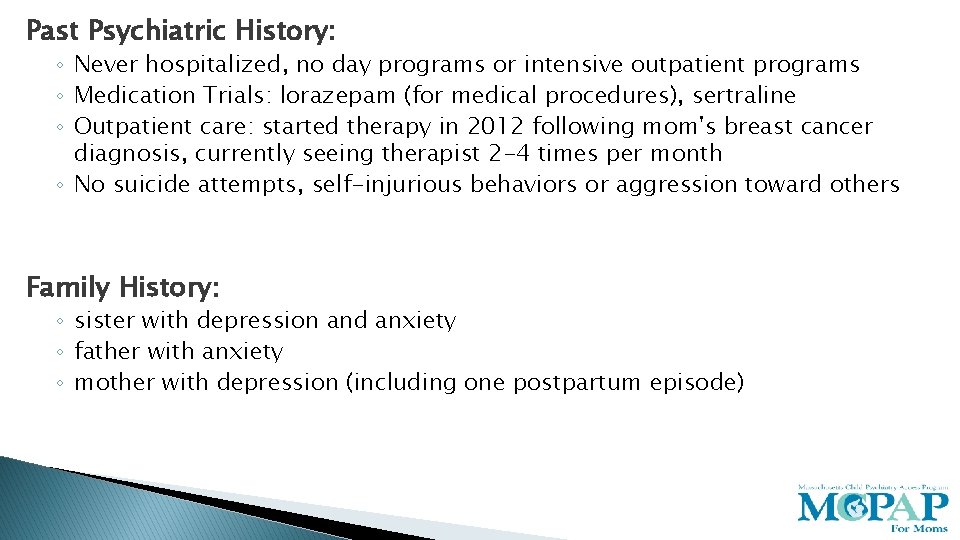
Past Psychiatric History: ◦ Never hospitalized, no day programs or intensive outpatient programs ◦ Medication Trials: lorazepam (for medical procedures), sertraline ◦ Outpatient care: started therapy in 2012 following mom's breast cancer diagnosis, currently seeing therapist 2 -4 times per month ◦ No suicide attempts, self-injurious behaviors or aggression toward others Family History: ◦ sister with depression and anxiety ◦ father with anxiety ◦ mother with depression (including one postpartum episode)
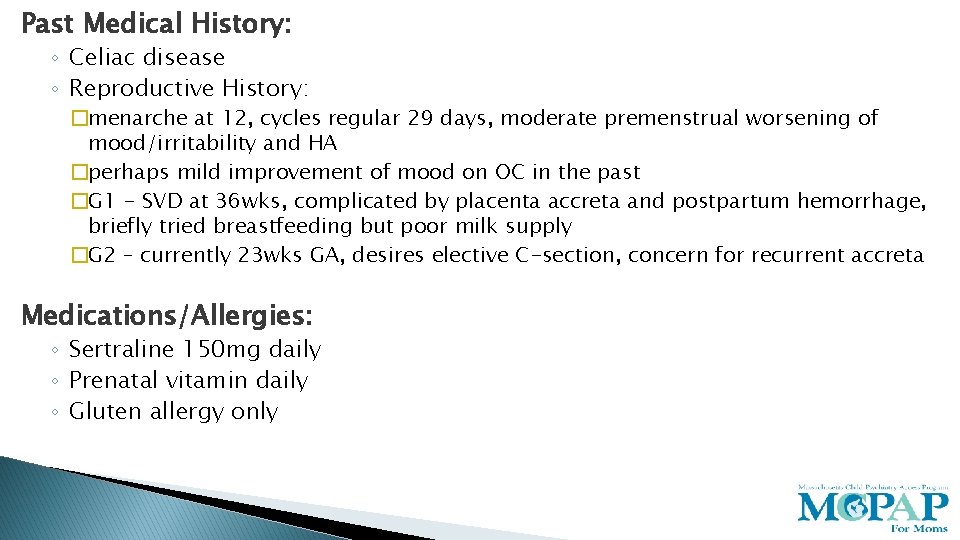
Past Medical History: ◦ Celiac disease ◦ Reproductive History: �menarche at 12, cycles regular 29 days, moderate premenstrual worsening of mood/irritability and HA �perhaps mild improvement of mood on OC in the past �G 1 - SVD at 36 wks, complicated by placenta accreta and postpartum hemorrhage, briefly tried breastfeeding but poor milk supply �G 2 – currently 23 wks GA, desires elective C-section, concern for recurrent accreta Medications/Allergies: ◦ Sertraline 150 mg daily ◦ Prenatal vitamin daily ◦ Gluten allergy only
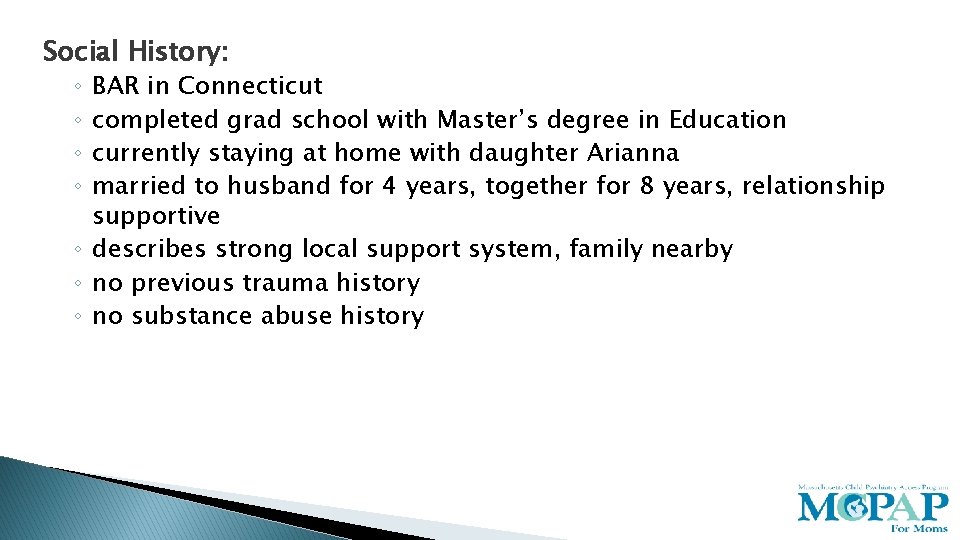
Social History: BAR in Connecticut completed grad school with Master’s degree in Education currently staying at home with daughter Arianna married to husband for 4 years, together for 8 years, relationship supportive ◦ describes strong local support system, family nearby ◦ no previous trauma history ◦ no substance abuse history ◦ ◦
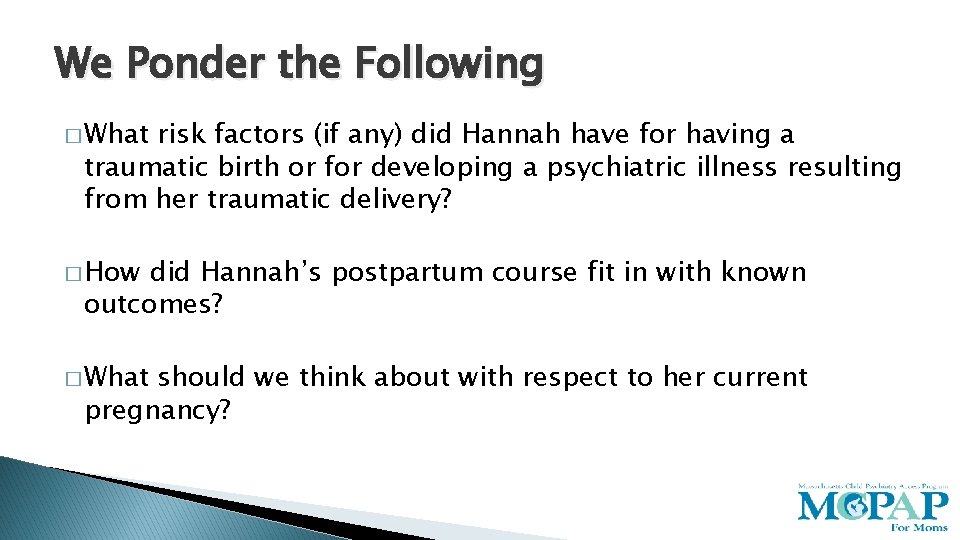
We Ponder the Following � What risk factors (if any) did Hannah have for having a traumatic birth or for developing a psychiatric illness resulting from her traumatic delivery? � How did Hannah’s postpartum course fit in with known outcomes? � What should we think about with respect to her current pregnancy?

Childbirth and Trauma – 2 Categories � Women who view the childbirth experience itself as traumatic � Women with prior trauma histories who become re-traumatized during childbirth (which becomes a trigger) Radosti 1999
Defining Traumatic Birth � No conventional definition of traumatic birth ◦ Beck (2004): “an event occurring during the labor and delivery process that involves actual or threatened serious injury or death to the mother or her infant. The birthing mother experiences intense fear, helplessness, loss of control, and horror. ” �Later expanded to include events during which “the [birthing mother] perceives she is stripped of her dignity” Beck 2004; Elmir 2010
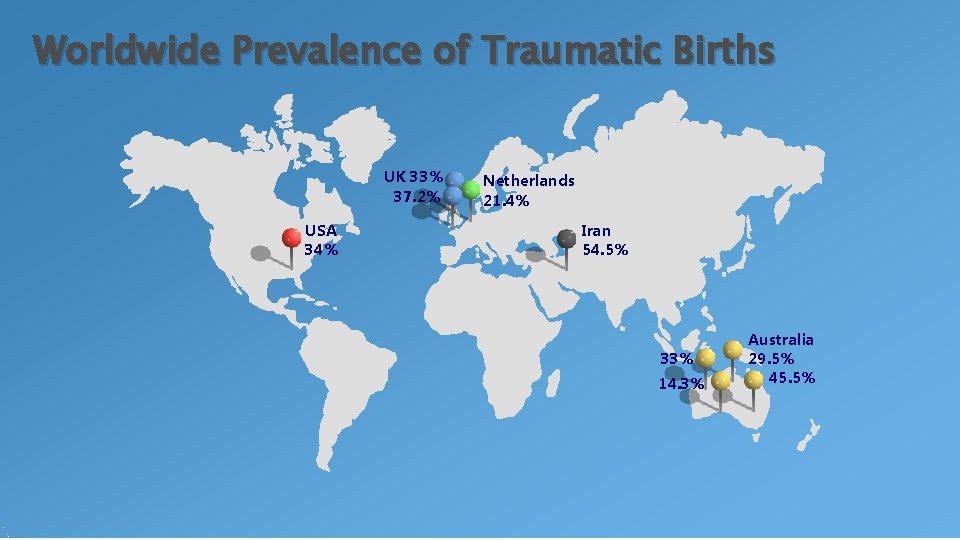
Worldwide Prevalence of Traumatic Births UK 33% 37. 2% USA 34% Netherlands 21. 4% Iran 54. 5% 33% 14. 3% Australia 29. 5% 45. 5%
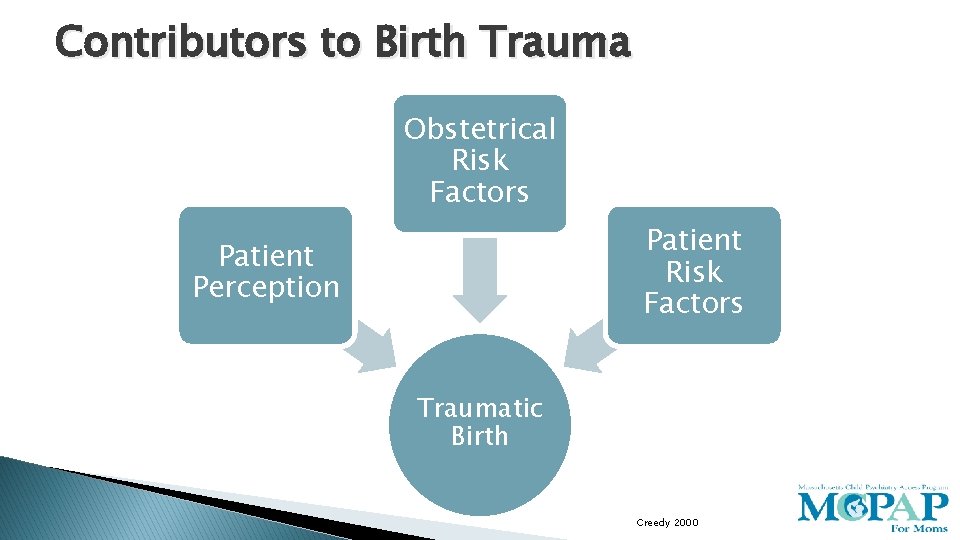
Contributors to Birth Trauma Obstetrical Risk Factors Patient Perception Traumatic Birth Creedy 2000
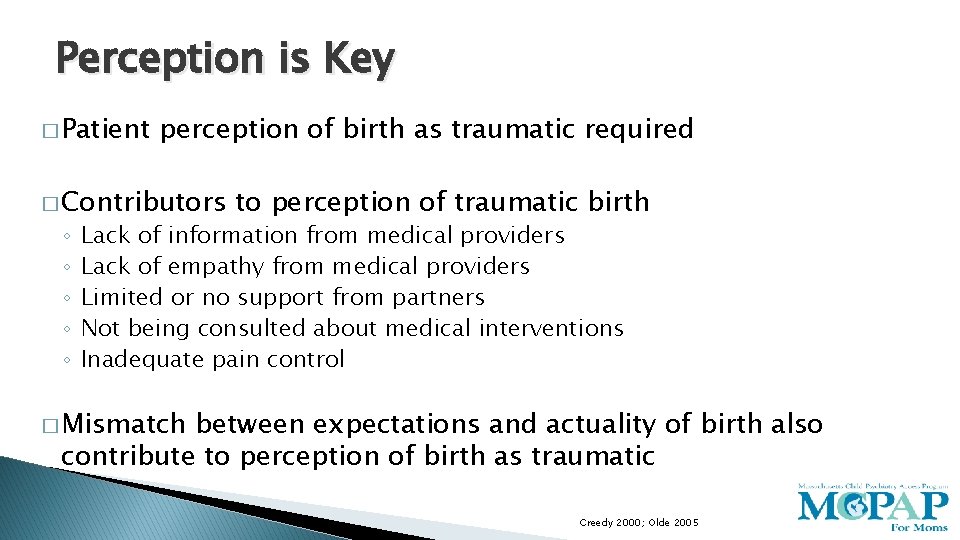
Perception is Key � Patient perception of birth as traumatic required � Contributors ◦ ◦ ◦ to perception of traumatic birth Lack of information from medical providers Lack of empathy from medical providers Limited or no support from partners Not being consulted about medical interventions Inadequate pain control � Mismatch between expectations and actuality of birth also contribute to perception of birth as traumatic Creedy 2000; Olde 2005
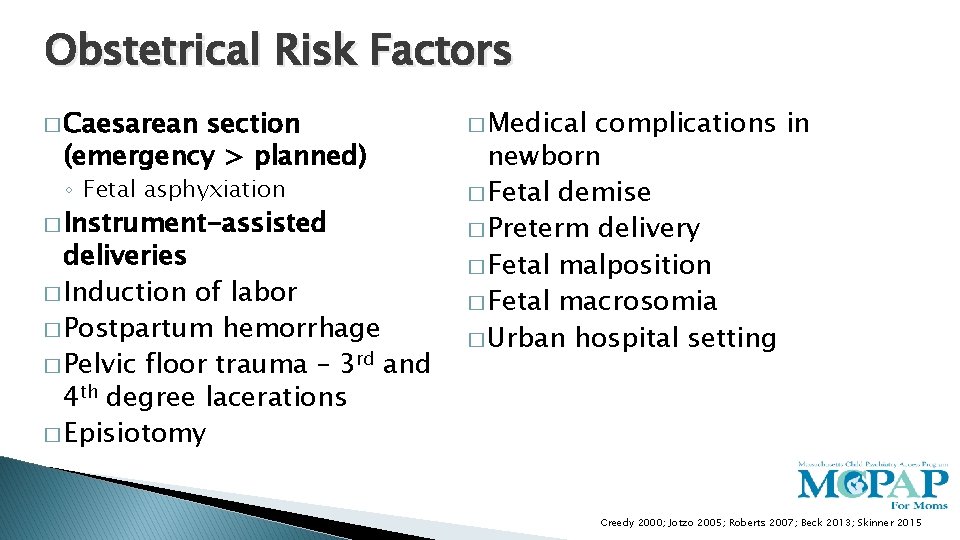
Obstetrical Risk Factors � Caesarean section (emergency > planned) ◦ Fetal asphyxiation � Instrument-assisted deliveries � Induction of labor � Postpartum hemorrhage � Pelvic floor trauma – 3 rd and 4 th degree lacerations � Episiotomy � Medical complications in newborn � Fetal demise � Preterm delivery � Fetal malposition � Fetal macrosomia � Urban hospital setting Creedy 2000; Jotzo 2005; Roberts 2007; Beck 2013; Skinner 2015
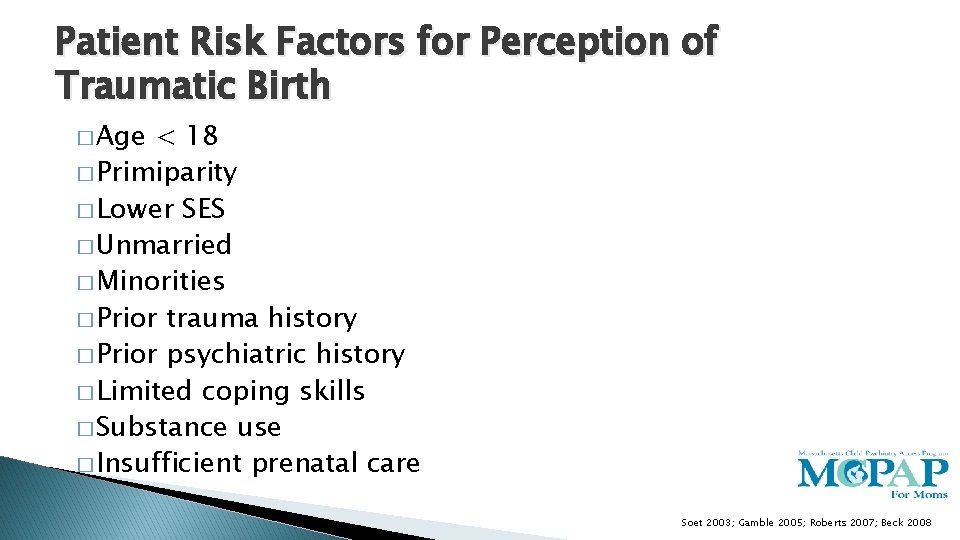
Patient Risk Factors for Perception of Traumatic Birth � Age < 18 � Primiparity � Lower SES � Unmarried � Minorities � Prior trauma history � Prior psychiatric history � Limited coping skills � Substance use � Insufficient prenatal care Soet 2003; Gamble 2005; Roberts 2007; Beck 2008
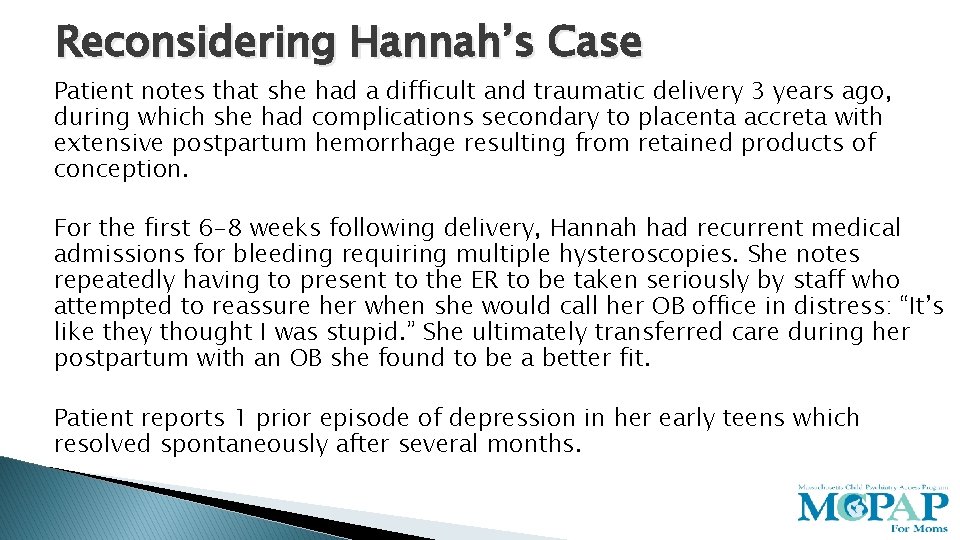
Reconsidering Hannah’s Case Patient notes that she had a difficult and traumatic delivery 3 years ago, during which she had complications secondary to placenta accreta with extensive postpartum hemorrhage resulting from retained products of conception. For the first 6 -8 weeks following delivery, Hannah had recurrent medical admissions for bleeding requiring multiple hysteroscopies. She notes repeatedly having to present to the ER to be taken seriously by staff who attempted to reassure her when she would call her OB office in distress: “It’s like they thought I was stupid. ” She ultimately transferred care during her postpartum with an OB she found to be a better fit. Patient reports 1 prior episode of depression in her early teens which resolved spontaneously after several months.
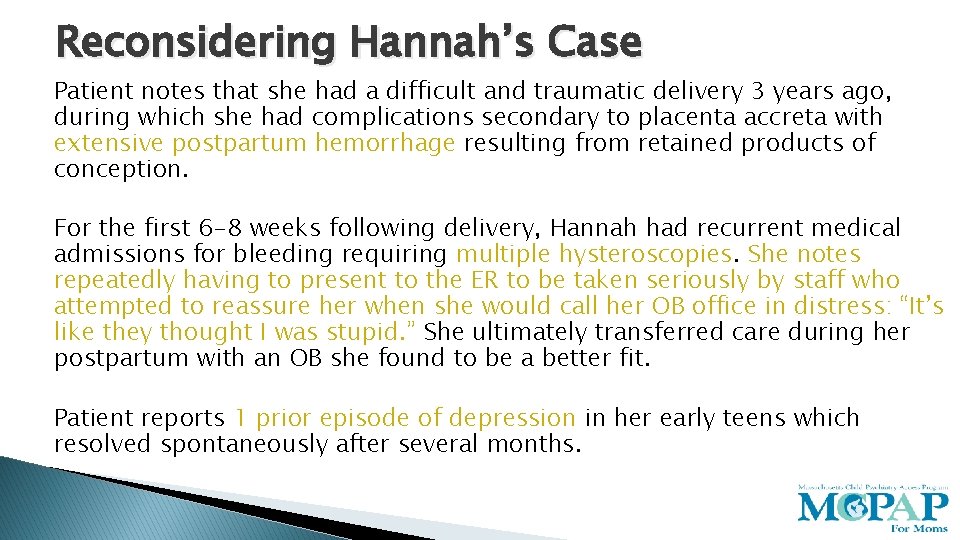
Reconsidering Hannah’s Case Patient notes that she had a difficult and traumatic delivery 3 years ago, during which she had complications secondary to placenta accreta with extensive postpartum hemorrhage resulting from retained products of conception. For the first 6 -8 weeks following delivery, Hannah had recurrent medical admissions for bleeding requiring multiple hysteroscopies. She notes repeatedly having to present to the ER to be taken seriously by staff who attempted to reassure her when she would call her OB office in distress: “It’s like they thought I was stupid. ” She ultimately transferred care during her postpartum with an OB she found to be a better fit. Patient reports 1 prior episode of depression in her early teens which resolved spontaneously after several months.
Outcomes � Impact on Breastfeeding � Impact on Relationships/Intimacy � Impact on Subsequent Pregnancies � Impact on Mental Health and Well-being

Impact on Breastfeeding - Lactogenesis � Associated with delayed lactogenesis ◦ Stress of traumatic delivery linked with decreased milk synthesis via 2 mechanisms � Lower rates of successful breastfeeding ◦ Long duration of labor and emergent Caesarean section powerful predictors for delayed lactogenesis Dewey 2008
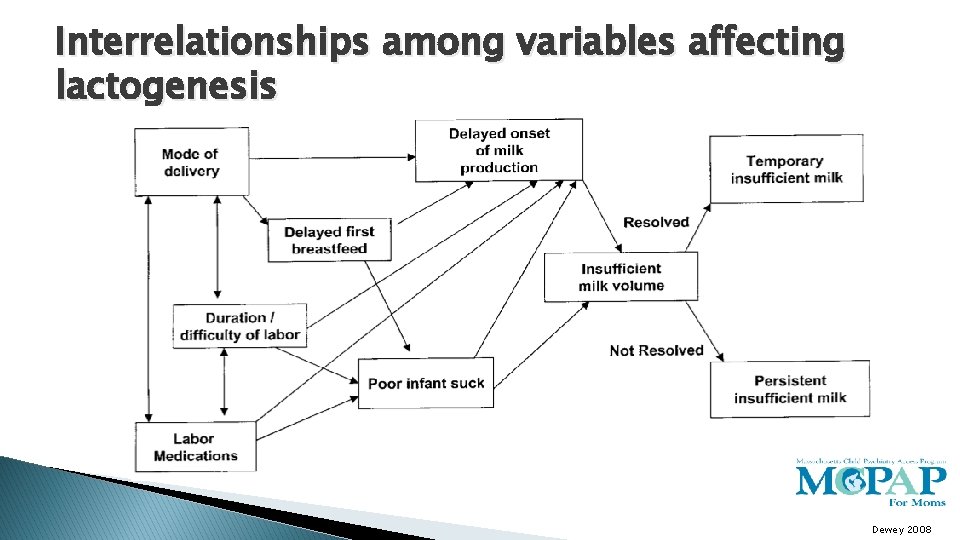
Interrelationships among variables affecting lactogenesis Dewey 2008
Impact on Breastfeeding - Emotional � Another trigger: “When I breastfed my baby, I felt like it was one more invasion upon my body and I couldn’t handle that after the labor I had suffered. Whenever I put her to breast, I wanted to scream and vomit at the same time. ” ◦ Flashbacks to delivery ◦ Dissociation during feeding ◦ Can lead some to stop breastfeeding altogether ◦ Staff efforts to assist with feeding can be re-traumatizing Beck 2011

Impact on Breastfeeding - Emotional �A corrective experience: “Breastfeeding was a timeout from the pain in my head. It was a ‘current reality’ – a way to cling onto some ‘real life, ’ whereas all the trauma that continued to live on in my head belonged to the past, even though I couldn’t keep it there. ” ◦ “Soothing” used frequently in narratives ◦ Themes of regaining control and mastery over body Beck 2011; Coates 2014
Impact on Intimacy � “It’s almost like trying to do it for the first time…and I’m almost in tears because I’m so scared. He’s so patient, but he does go, ‘Maybe tonight we can try, ’ and I’m like ‘Sure. ’ I was so anxious about it-I made myself really sick. ” � “Six weeks without sex – that’s the little magic number you hear, but to still be eighteen months down the track and it’s very rare that we can achieve intercourse…so it certainly has impacted on our relationship because you know he thought things would be back to normal by now. ” Priddis 2014

Traumatic Birth and Subsequent Pregnancies � Fear of subsequent pregnancies ◦ Tan et al, evaluating small sample of women with postpartum hemorrhage or preeclampsia � 85% reported fear of recurrent pregnancy �Women noted decreased desired family size (3. 75 → 1. 60) ◦ Primiparous more likely to avoid ◦ May translate into requests for sterilization or terminations of subsequent pregnancies � For women that have recurrent pregnancies ◦ Higher rate of requests for elective C-sections ◦ Longer pregnancy intervals Johnston 2004; Alder 2006; Callahan 2008; Tan 2013

Traumatic Birth and Subsequent Pregnancies Women’s future reproduction in relation to overall birth experience assessed two months after the first birth. Time to the second birth in relation to overall birth experience. Scores of birth experience 1 – 7 as above (1 ¼ very negative, 7 ¼ very positive) Gottvall 2002
Depressive and Anxiety Symptoms � 20 -30% of women experience significant depressive symptoms or anxiety following traumatic birth ◦ Fears of being an adequate mother or of not being able to adequately manage a medical emergency involving infant � Studies limited by ◦ Lack of adequate controlling for premorbid psychopathology ◦ Inconsistent measures to determine psychopathology Creedy 2005; Alcorn 2010; Goutaudier 2011
Narrative Themes in Traumatic Births � Being stripped of protective layers ◦ “After an hour trying to deliver the baby…the obstetrician said…the baby was truly stuck. By now the doctors are acting like I’m not there. The attending physician was saying, ‘We may have lost this bloody baby. ’ The hospital staff discussed my baby’s possible death in front of me, and argued in front of me just as if I weren’t there. ” � Invisible wounds “This is a hidden injury and I cannot share this with anyone. ” “I was congratulated for how ‘quickly and easily’ the baby came out and that he scored a perfect 10! The worst thing was that nobody acknowledged that I had a bad time…I felt as if I had been raped!” � Insidious repercussions ◦ “I could not attach to my baby for 6 months. I have to bite my hand to stop myself from telling [other women] how bad birth and delivery will be. ” Beck 2011; Kahl 2012; Beck 2013; Skinner 2015
Postpartum Post-Traumatic Stress Disorder � Best studied of mental illnesses postpartum resulting from traumatic birth � Majority of literature qualitative or epidemiological studies looking at retrospective data Creedy 2003; Soet 2003; Beck 2011
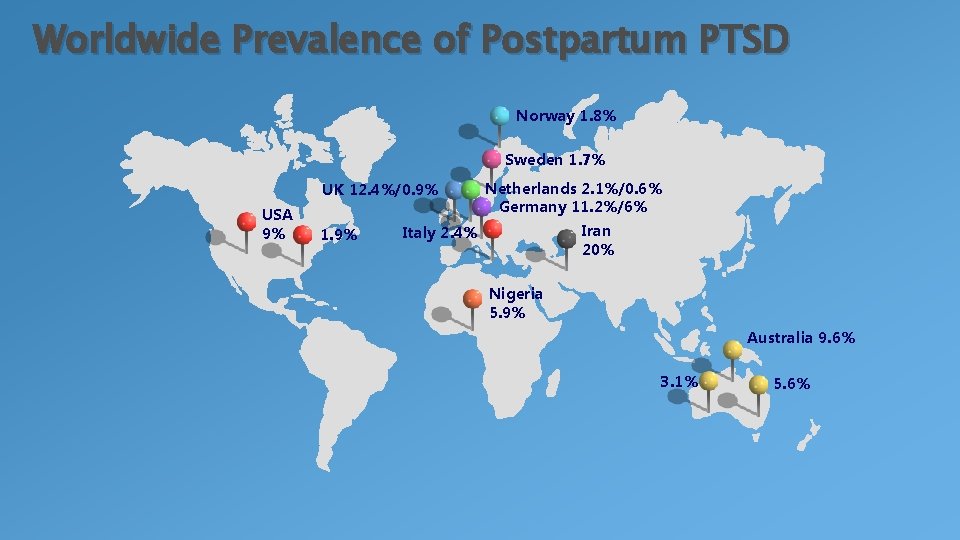
Worldwide Prevalence of Postpartum PTSD Norway 1. 8% Sweden 1. 7% Netherlands 2. 1%/0. 6% Germany 11. 2%/6% Iran Italy 2. 4% 20% UK 12. 4%/0. 9% USA 9% 1. 9% Nigeria 5. 9% Australia 9. 6% 3. 1% 5. 6%
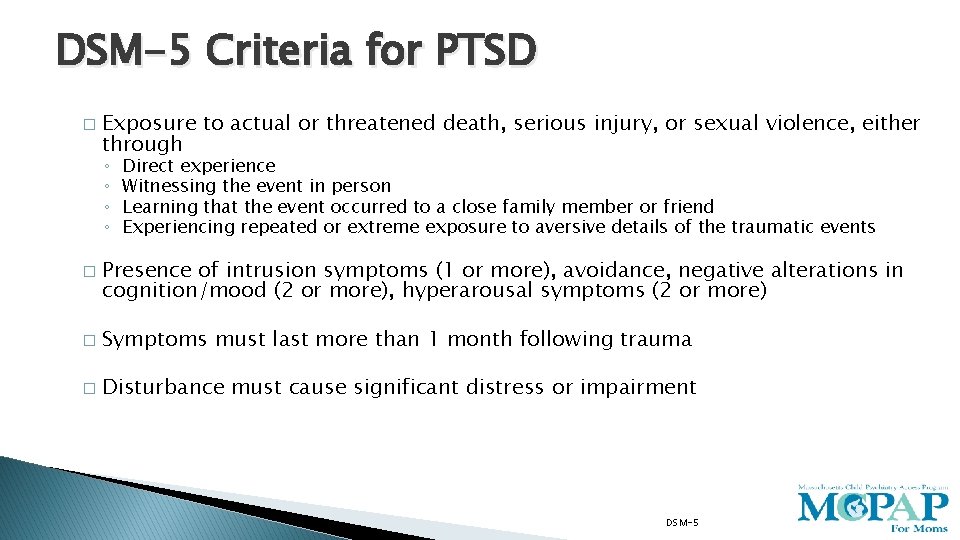
DSM-5 Criteria for PTSD � Exposure to actual or threatened death, serious injury, or sexual violence, either through ◦ ◦ � Direct experience Witnessing the event in person Learning that the event occurred to a close family member or friend Experiencing repeated or extreme exposure to aversive details of the traumatic events Presence of intrusion symptoms (1 or more), avoidance, negative alterations in cognition/mood (2 or more), hyperarousal symptoms (2 or more) � Symptoms must last more than 1 month following trauma � Disturbance must cause significant distress or impairment DSM-5
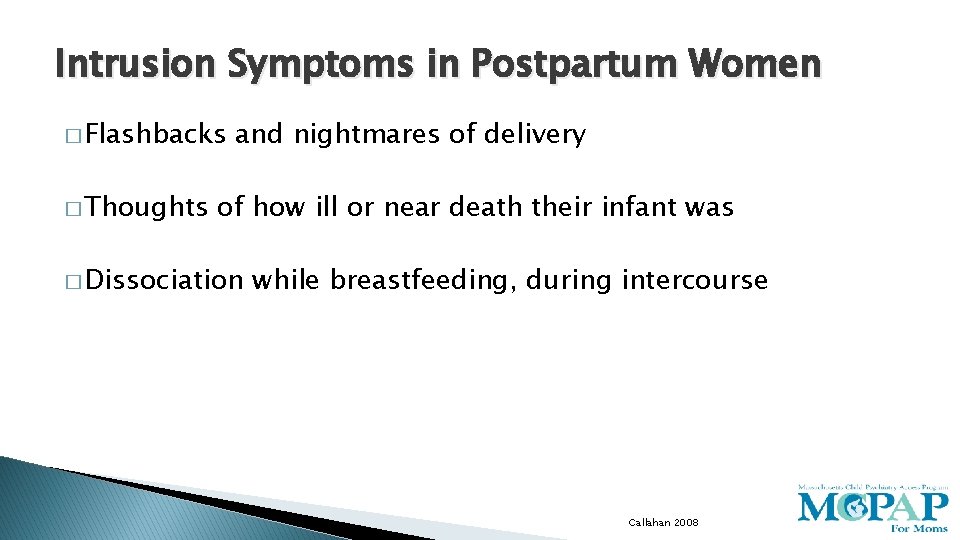
Intrusion Symptoms in Postpartum Women � Flashbacks � Thoughts and nightmares of delivery of how ill or near death their infant was � Dissociation while breastfeeding, during intercourse Callahan 2008
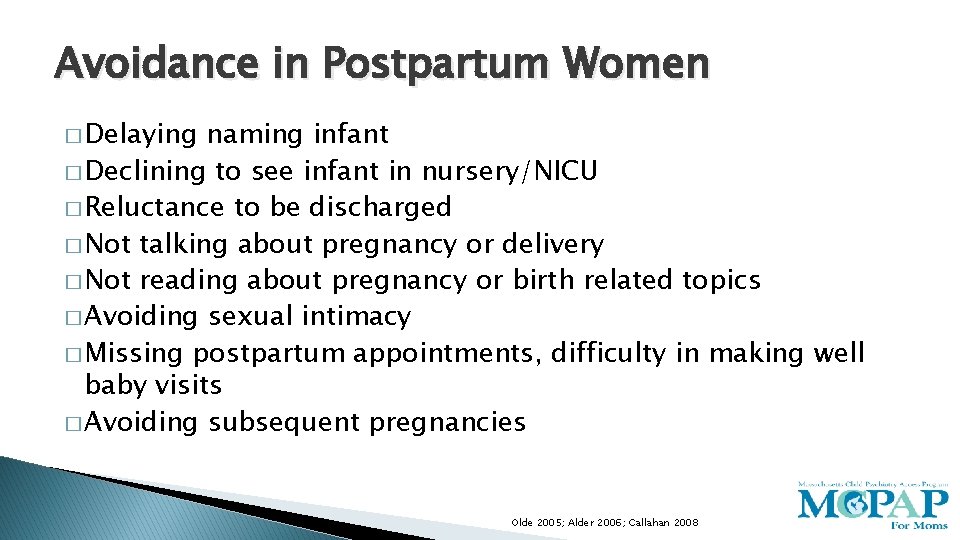
Avoidance in Postpartum Women � Delaying naming infant � Declining to see infant in nursery/NICU � Reluctance to be discharged � Not talking about pregnancy or delivery � Not reading about pregnancy or birth related topics � Avoiding sexual intimacy � Missing postpartum appointments, difficulty in making well baby visits � Avoiding subsequent pregnancies Olde 2005; Alder 2006; Callahan 2008
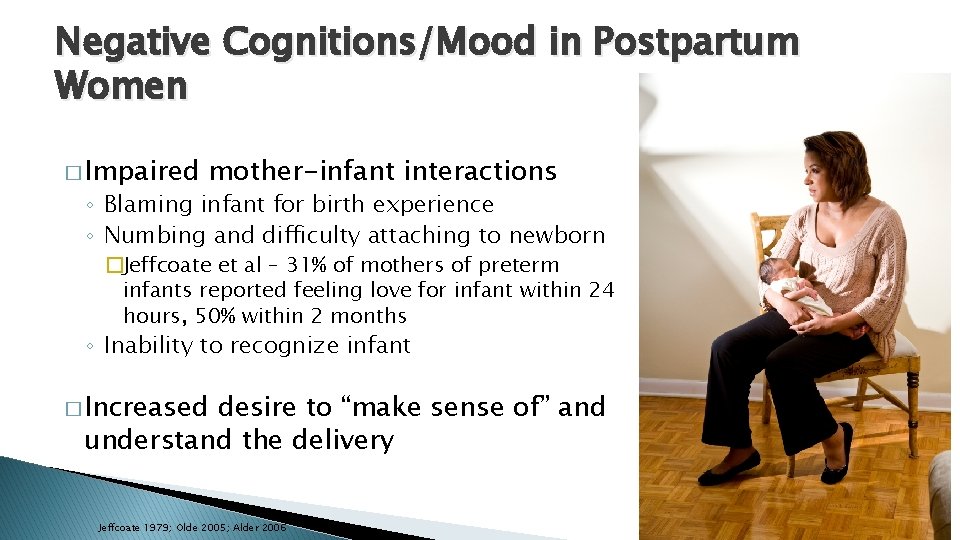
Negative Cognitions/Mood in Postpartum Women � Impaired mother-infant interactions ◦ Blaming infant for birth experience ◦ Numbing and difficulty attaching to newborn �Jeffcoate et al – 31% of mothers of preterm infants reported feeling love for infant within 24 hours, 50% within 2 months ◦ Inability to recognize infant � Increased desire to “make sense of” and understand the delivery Jeffcoate 1979; Olde 2005; Alder 2006
Hyperarousal Symptoms in Postpartum Women � Sweating � Trembling � Irritability and angry outbursts � Sleep disturbances � Exaggerated startle response Olde 2005; Callahan 2008
Predictors of developing postpartum PTSD � Emergent C-section or operative vaginal delivery � 2+ pre-delivery physical risk factors (hyperemesis, preeclampsia, preterm contractions, et cetera) � Manual removal of placenta � Dissociation during the delivery � Pain during delivery � Episiotomy � Primiparity � Ill or stillborn newborn � Preterm delivery and preterm labor � < 2 years pregnancy interval � Absent/uninformed partner � Negative appraisal of past deliveries � External locus of control � Poor self-efficacy � Poor coping skills � Low levels of social support Creedy 2003; Soet 2003; Gamble 2005; Alder 2006; Goutaudier 2011; Modarres 2012
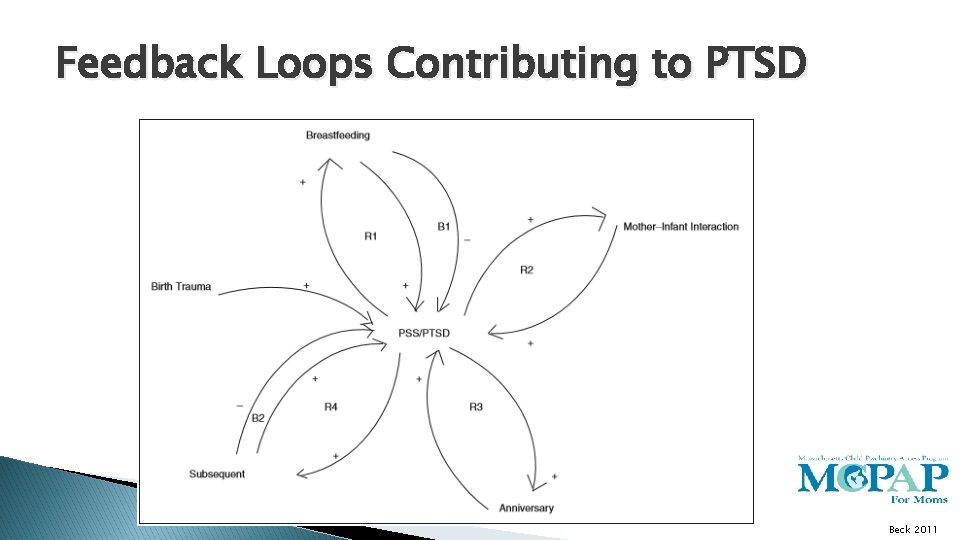
Feedback Loops Contributing to PTSD Beck 2011
Hannah Returns for her Follow-up � Recurrent placenta accreta has been confirmed now ◦ Caesarean section is now preferred method of delivery � She has noted her mood remains stable but continues to experience intrusive thoughts and hyperarousal. She notes her husband is supportive, although she struggles to share as “he was traumatized too. ” She worries delivering at the hospital again will be too much for her to bear. � Her OB asks if anything can be done in preparation for her delivery in the coming months.
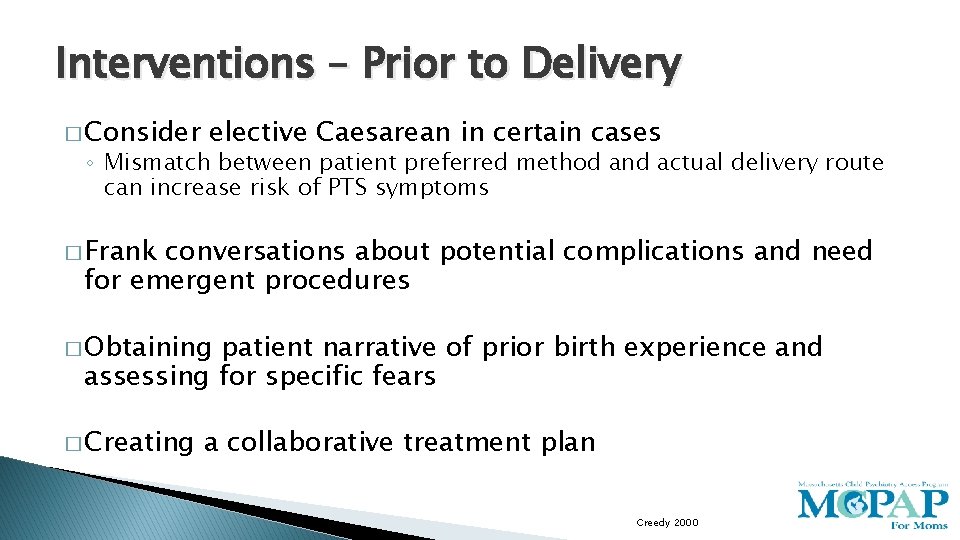
Interventions – Prior to Delivery � Consider elective Caesarean in certain cases ◦ Mismatch between patient preferred method and actual delivery route can increase risk of PTS symptoms � Frank conversations about potential complications and need for emergent procedures � Obtaining patient narrative of prior birth experience and assessing for specific fears � Creating a collaborative treatment plan Creedy 2000
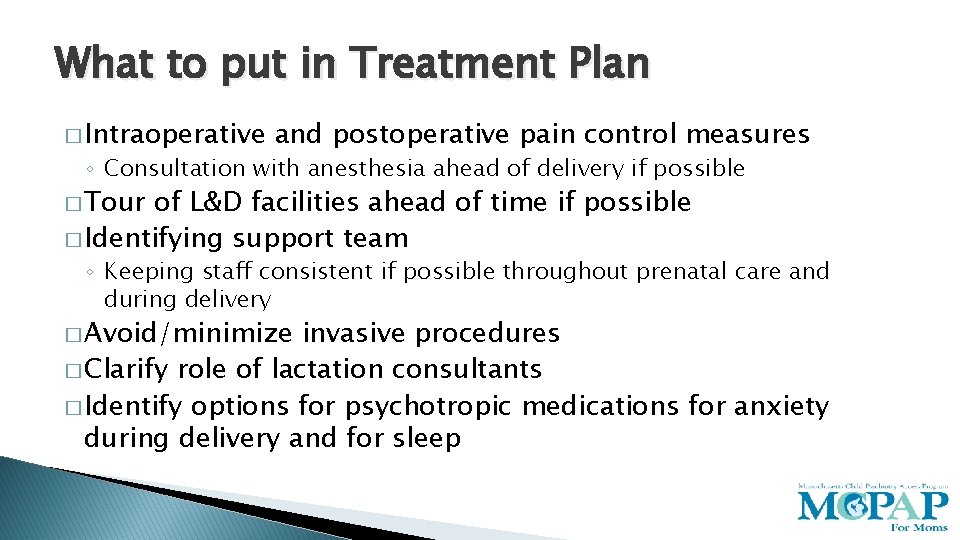
What to put in Treatment Plan � Intraoperative and postoperative pain control measures ◦ Consultation with anesthesia ahead of delivery if possible � Tour of L&D facilities ahead of time if possible � Identifying support team ◦ Keeping staff consistent if possible throughout prenatal care and during delivery � Avoid/minimize invasive procedures � Clarify role of lactation consultants � Identify options for psychotropic medications for anxiety during delivery and for sleep
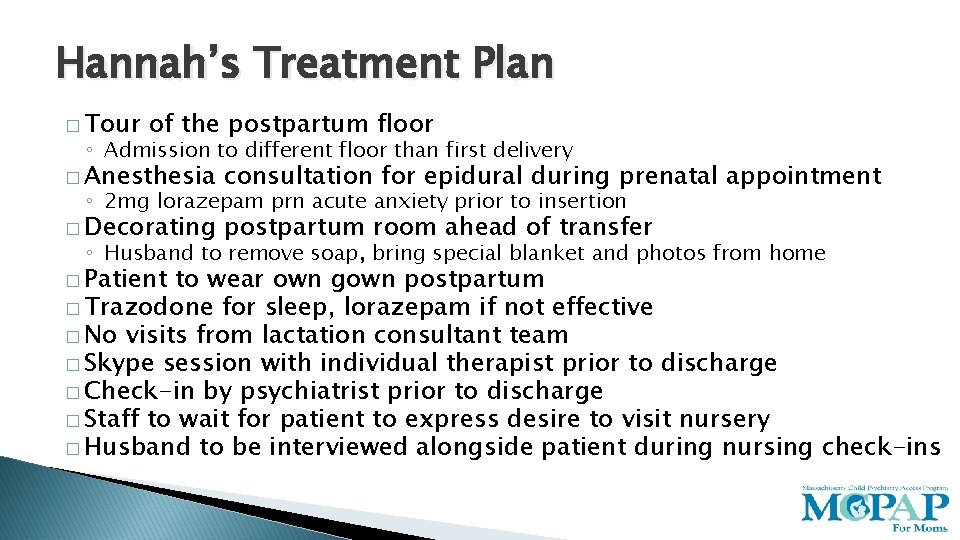
Hannah’s Treatment Plan � Tour of the postpartum floor ◦ Admission to different floor than first delivery � Anesthesia consultation for epidural during prenatal appointment � Decorating postpartum room ahead of transfer ◦ 2 mg lorazepam prn acute anxiety prior to insertion ◦ Husband to remove soap, bring special blanket and photos from home � Patient to wear own gown postpartum � Trazodone for sleep, lorazepam if not effective � No visits from lactation consultant team � Skype session with individual therapist prior to discharge � Check-in by psychiatrist prior to discharge � Staff to wait for patient to express desire to visit nursery � Husband to be interviewed alongside patient during nursing check-ins
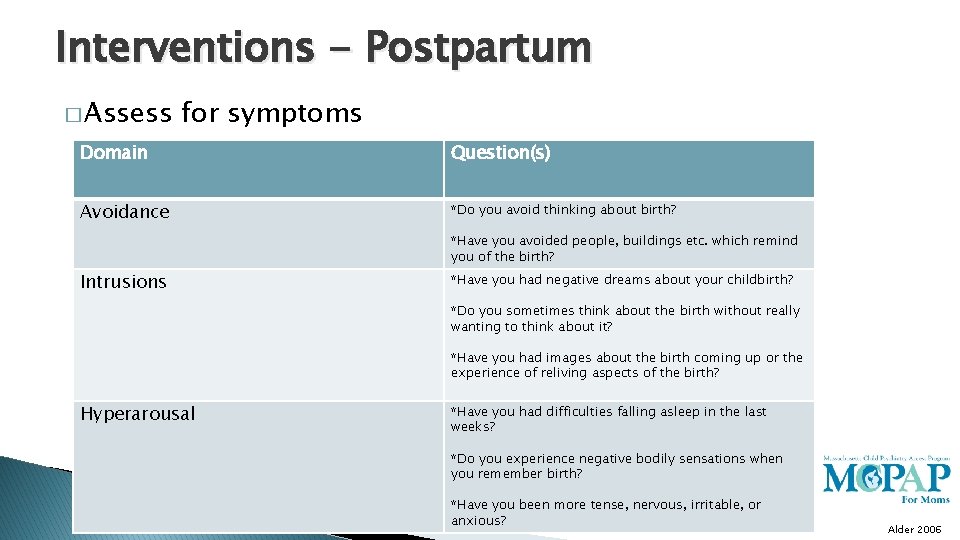
Interventions - Postpartum � Assess for symptoms Domain Question(s) Avoidance *Do you avoid thinking about birth? *Have you avoided people, buildings etc. which remind you of the birth? Intrusions *Have you had negative dreams about your childbirth? *Do you sometimes think about the birth without really wanting to think about it? *Have you had images about the birth coming up or the experience of reliving aspects of the birth? Hyperarousal *Have you had difficulties falling asleep in the last weeks? *Do you experience negative bodily sensations when you remember birth? *Have you been more tense, nervous, irritable, or anxious? Alder 2006
Interventions – Postpartum � Psychological debriefings ◦ Focus on attentive listening, validation, filling in gaps of patient narrative, connection emotions with events, finding support, reinforcing positive coping strategies ◦ High rates of patient satisfaction with ability to share narrative (up to 90%) ◦ Limited evidence showing effectiveness in reducing rates of postpartum psychiatric disorders ◦ No consistent treatment guidelines Gamble 2004; Gamble 2005; Peeler 2013
Interventions – Postpartum Counseling � Select techniques both shown to be efficacious though little data evaluating psychotherapy modalities themselves ◦ Exposures can include recounting birth story or writing birth narrative ◦ Bolstering partner support (including psychoeducation) ◦ Mindfulness techniques including progressive muscle relaxation and safe place guided imagery Alder 2006; Peeler 2013
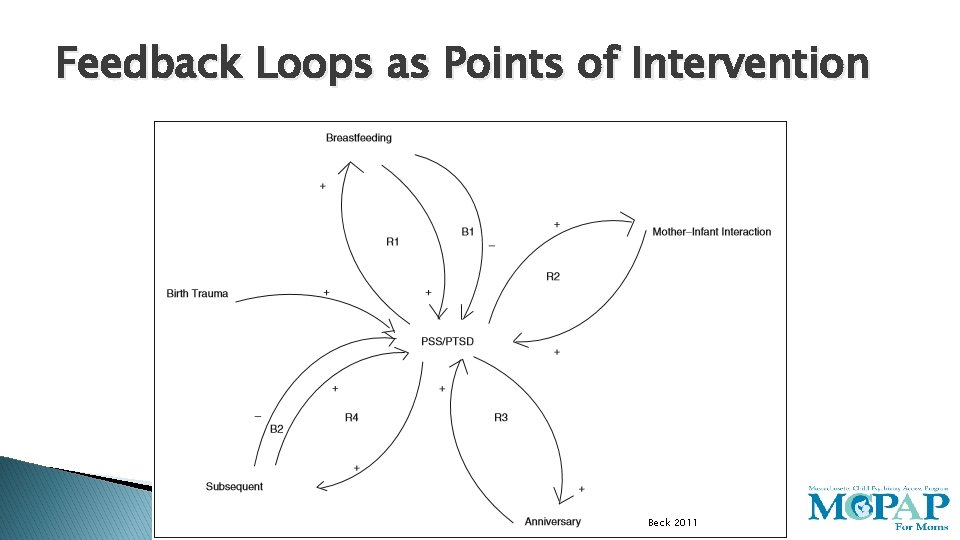
Feedback Loops as Points of Intervention Beck 2011
Psychopharmacology Options � Traditional ◦ ◦ SSRIs – first line medication choice Sedating TCAs, mirtazapine Atypical antipsychotics Prazosin, clonidine, propranolol � Subject to debate ◦ Benzos ◦ Trazodone ◦ Topiramate � Down the pipeline ◦ D-cycloserine ◦ Glucocorticoids ◦ Ketamine Berlin 2013
From Trauma to Triumph: Posttraumatic Growth (PTG) � Incremental � Domains ◦ ◦ ◦ psychological change impacted Greater sense of personal strength Improved relationships Greater appreciation for life Spiritual growth New possibilities Callahan 2008; Sawyer 2009; Sawyer 2012
Predictors of PTG � Approach coping strategies that seek guidance and support as well as problem solving � Avoidance coping strategy of seeking alternative rewards � Younger age � Caesarean section > vaginal delivery � Sense of internal control Sawyer 2009; Sawyer 2012

Summary � As many as 1 in 3 women experience childbirth as traumatic � Obstetrical factors, patient perception of care and patient vulnerabilities contribute to perception of birth as traumatic � Impaired lactogenesis, difficulty breastfeeding as well as reluctance with subsequent pregnancies may result from traumatic birth � Psychological consequences of traumatic birth include depression, anxiety and posttraumatic stress disorder � Posttraumatic growth has been described in the literature as a mode of interpersonal development following traumatic delivery

Questions?
www. mcpapformoms. org Call 855 -Mom-MCPAP 855 – (666 -6272) Kara Brown, MD Psychiatrist kbrown 32@bwh. Harvard. edu

Resources for Patients � Postpartum Support International � Postpartum Progress �www. postpartum. net �www. postpartumprogress. com � MGH’s Women’s Mental Health Blog �https: //womensmentalhealth. org/blog
- Slides: 56