Trauma Screenings Marisol Acosta MEd LPCSupervisor Project Director




- Slides: 51
Trauma Screenings Marisol Acosta, MEd, LPC-Supervisor , Project Director April 17, 2015 Texas Children Recovering From Trauma Initiative Department of State Health Services, Mental Health and Substance Abuse Division
Objectives Increase the understanding and importance of trauma screenings: “why” screen, “what” to screen, and “how” to screen Differentiate Trauma Screenings vs Trauma Assessment Overview of different types of trauma screening tools

The “WHY”
Facts • Trauma is widespread and pervasive • Trauma does not occur on a vacuum, but within the context of a community • SAMHSA, 2014
Facts 5 Physical traumas are the leading cause of death for individuals ages 1 -44 (University Health System of Bexar County, 2014) 70% of adults have experienced some type of traumatic event at least once in their lives. (National Council on Behavioral Health, 2014) In the U. S. a woman is beaten every 15 seconds; and a forcible rape occurs every 6 minutes. (National Council on Behavioral Health, 2014)
Facts about children 25% of all children have experienced at least one traumatic event (NCTSN, 2007) Before age of four, 26% of all children have witnessed or experienced a traumatic event (SAMHSA, 2011) Children with disabilities are at least 2 times more likely to be abused or neglected. (NCTSN, 2004) 83 -93% of children living in neighborhoods with high rates of violent crimes would have experienced trauma (National Center for Children in Poverty, 2007)
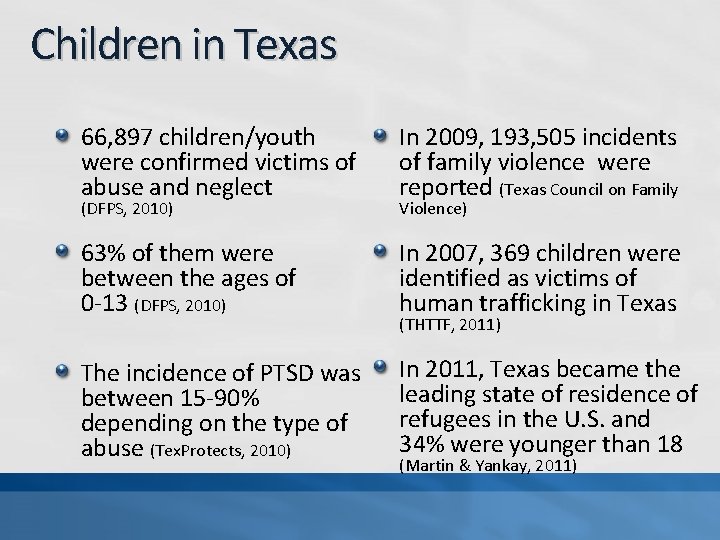
Children in Texas 66, 897 children/youth were confirmed victims of abuse and neglect In 2009, 193, 505 incidents of family violence were reported (Texas Council on Family 63% of them were between the ages of 0 -13 (DFPS, 2010) In 2007, 369 children were identified as victims of human trafficking in Texas The incidence of PTSD was between 15 -90% depending on the type of abuse (Tex. Protects, 2010) In 2011, Texas became the leading state of residence of refugees in the U. S. and 34% were younger than 18 (DFPS, 2010) Violence) (THTTF, 2011) (Martin & Yankay, 2011)
WHY Screen for Trauma? To Understand Support Develop a collaborative relationship Prevent Adverse Effects To Provide Appropriate Care and Services Treat Adverse Effect Address the impact of trauma and increase functioning and coping mechanisms Foster Resilience & Recovery
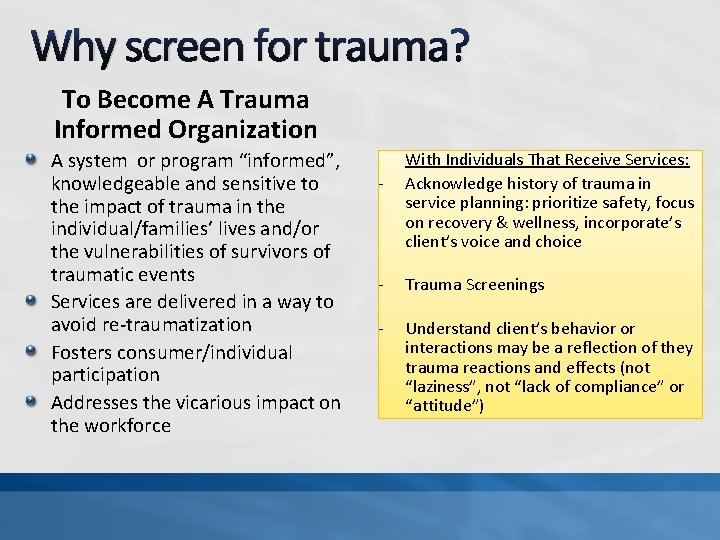
Why screen for trauma? To Become A Trauma Informed Organization A system or program “informed”, knowledgeable and sensitive to the impact of trauma in the individual/families’ lives and/or the vulnerabilities of survivors of traumatic events Services are delivered in a way to avoid re-traumatization Fosters consumer/individual participation Addresses the vicarious impact on the workforce - With Individuals That Receive Services: Acknowledge history of trauma in service planning: prioritize safety, focus on recovery & wellness, incorporate’s client’s voice and choice - Trauma Screenings - Understand client’s behavior or interactions may be a reflection of they trauma reactions and effects (not “laziness”, not “lack of compliance” or “attitude”)
It’s a Best Care Practice National Association of State Mental Health Program Directors (NASMHPD) Substance Abuse and Mental Health Administration National Center on Trauma Informed Care National Child Traumatic Stress Network National Council on Behavioral Health Professional Associations
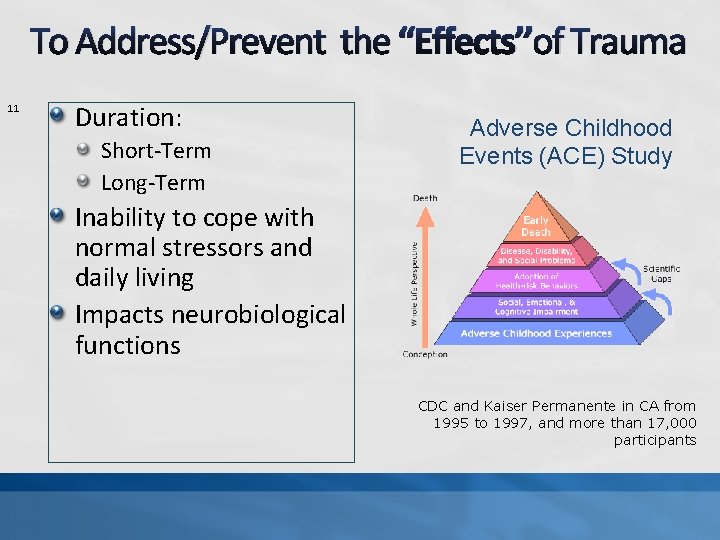
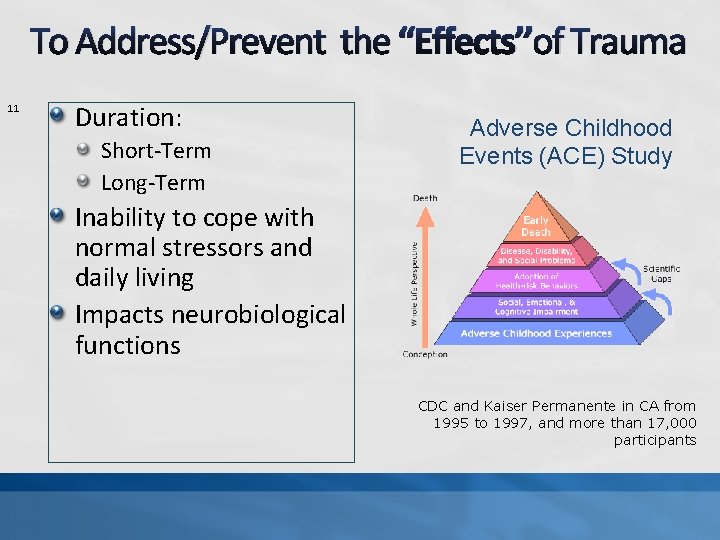
To Address/Prevent the “Effects’’of Trauma 11 Duration: Short-Term Long-Term Adverse Childhood Events (ACE) Study Inability to cope with normal stressors and daily living Impacts neurobiological functions CDC and Kaiser Permanente in CA from 1995 to 1997, and more than 17, 000 participants
The impact of lack of screenings Trauma history is overlooked by professionals in mental health settings. Even when 1 event is has been reported, clinicians overlook other forms of abuse or maltreatment (Briere, 2004) Studies have found that child abuse disclosure of psychotic patients are often dismissed, ignored, or marginalized under the belief that discussing the issues will make them worse. (Hammersley, 2004)
Trauma is rarely reflected in primary or secondary diagnosis Study Findings 46% of women in psychiatric hospitals with a psychotic disorder have history of incest (van der Kolk, 1987) 98 % of patients with serious mental illness (schizophrenia and bipolar disorder) reported at least 1 traumatic event, only 2% had a diagnosis of PTSD in their chart. (Mueser et al, 1998)
Trauma responses are often misdiagnosed under symptoms of: ADHD Bipolar Disorder Mood Disorder NOS Psychosis NOS Borderline Personality - Tucker, 2002

Risks of Failing to Screen Misdiagnosis Inappropriate treatment plan Increase vulnerability to substance use Increases the probability of developing other serious mental illness, physical illness and risk of early death Increase chances of re-traumatization Increase social isolation Increase risk of suicide (in some traumatic events) Creating cascading effect on the individuals life and inappropriate care.
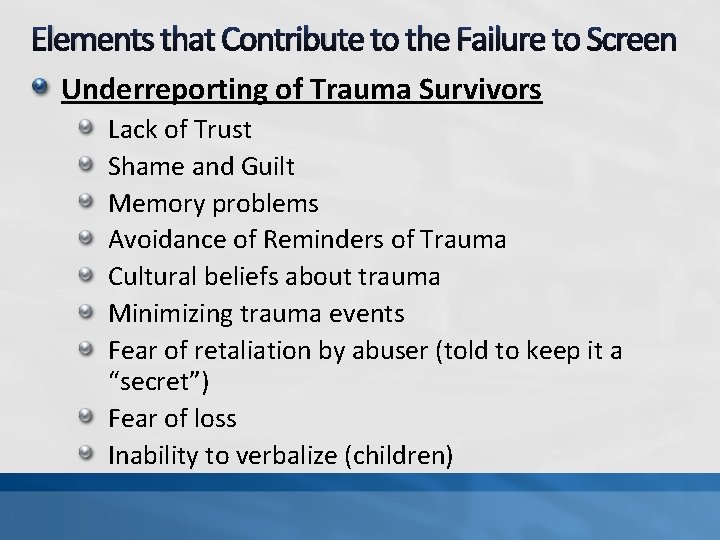
Elements that Contribute to the Failure to Screen Underreporting of Trauma Survivors Lack of Trust Shame and Guilt Memory problems Avoidance of Reminders of Trauma Cultural beliefs about trauma Minimizing trauma events Fear of retaliation by abuser (told to keep it a “secret”) Fear of loss Inability to verbalize (children)
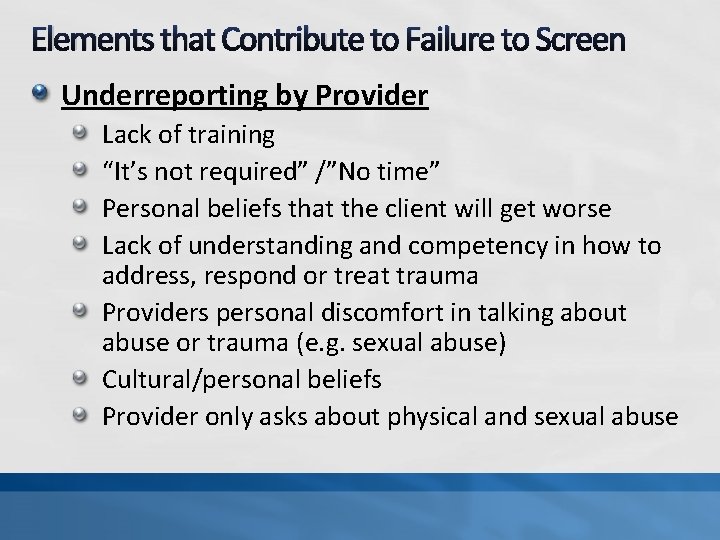
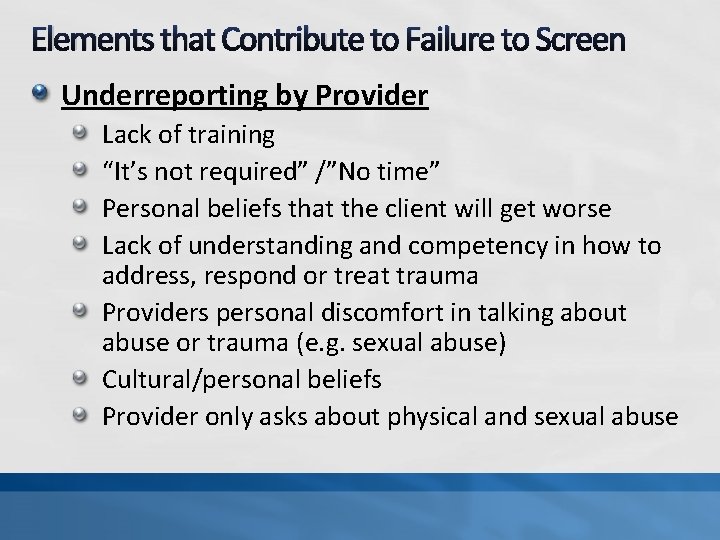
Elements that Contribute to Failure to Screen Underreporting by Provider Lack of training “It’s not required” /”No time” Personal beliefs that the client will get worse Lack of understanding and competency in how to address, respond or treat trauma Providers personal discomfort in talking about abuse or trauma (e. g. sexual abuse) Cultural/personal beliefs Provider only asks about physical and sexual abuse
“Universal trauma screenings and specific trauma assessment methods are necessary to developing relationships with trauma survivors and offering appropriate services” Harris & Fallot 2001
The “WHAT” What are we screening?
TRAUMA Shell Shock Aftermath Trauma Why so many words? Traumatic Event Childhood Traumatic Stress Adverse Childhood Events Toxic Stressors
What is considered a traumatic “Event”? Event or circumstances that created the experience that caused an actual or extreme threat of physical or emotional harm (SAMHSA, 2014) A common definition in the trauma field: – A traumatic event is an experience that causes physical, emotional, psychological distress, or harm. It is an event that is perceived and experienced as a threat to one's safety or to the stability of one's world.
An “Event” as a “Stressor” 22 The person was exposed to: death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence, as follows: (1 required) Direct exposure. Witnessing, in person , or Indirectly Repeated or extreme indirect exposure to aversive details of the event(s), usually in the course of professional duties Diagnostic Statistical Manual -5 of Mental Health Disorders (APA, 2013)
The “Experience” of the event 23 …helps determine whether the event or circumstances is a traumatic event The experience and perception of a particular event may be considered traumatic by one in individual and not for another How individuals labels, assigns meaning, and is disrupted physically and psychologically by an event will contribute to whether or not it is experienced as traumatic (SAMHSA, 2014)
VIOLENCE Buddhist Swastika Definitions of violence change through time and vary according to culture of a particular country or region (Online Encyclopedia of Mass Violence, 2012) Nazi Swastika
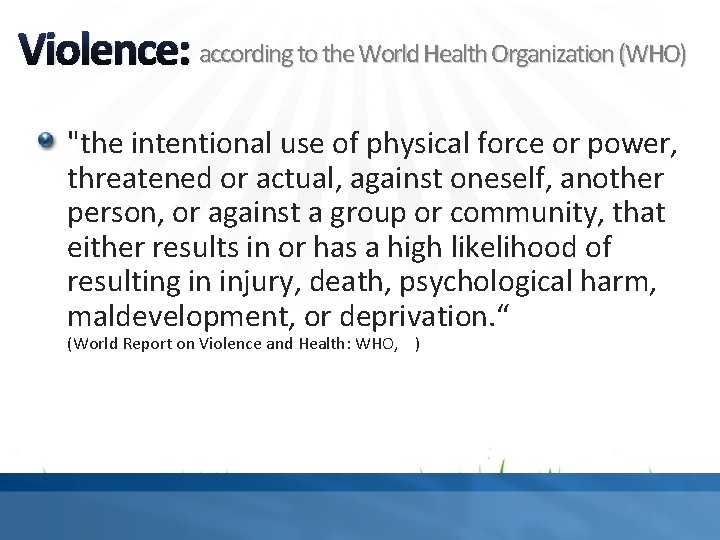
Violence: according to the World Health Organization (WHO) "the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community, that either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment, or deprivation. “ (World Report on Violence and Health: WHO, )
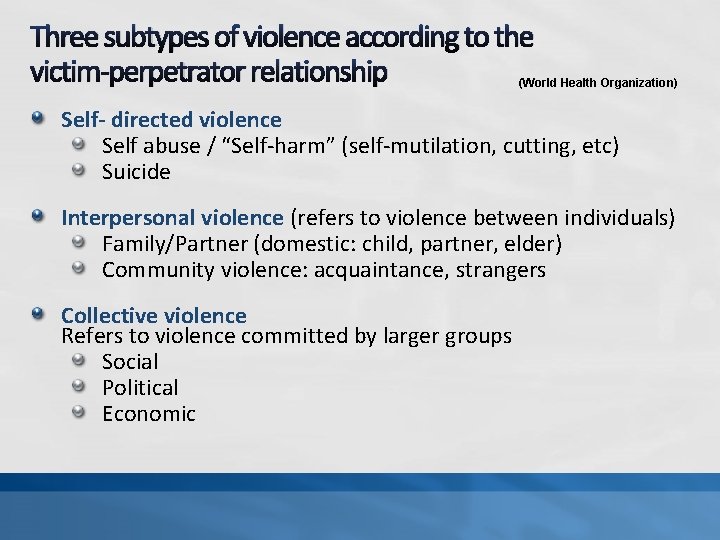
Three subtypes of violence according to the victim-perpetrator relationship (World Health Organization) Self- directed violence Self abuse / “Self-harm” (self-mutilation, cutting, etc) Suicide Interpersonal violence (refers to violence between individuals) Family/Partner (domestic: child, partner, elder) Community violence: acquaintance, strangers Collective violence Refers to violence committed by larger groups Social Political Economic
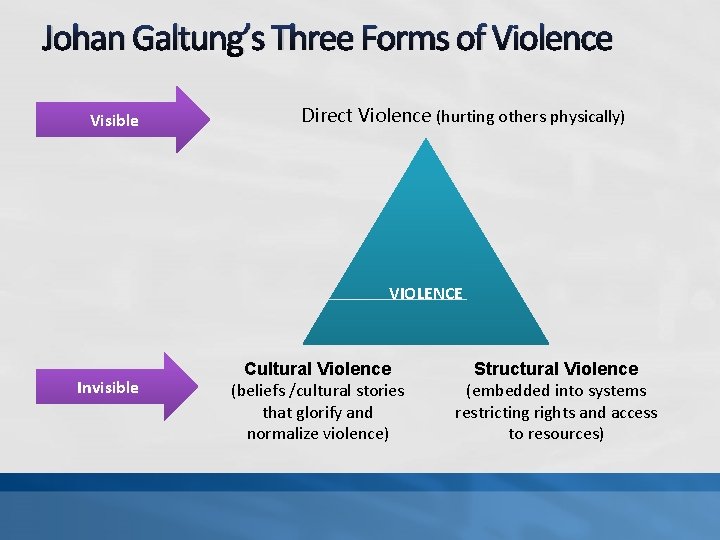
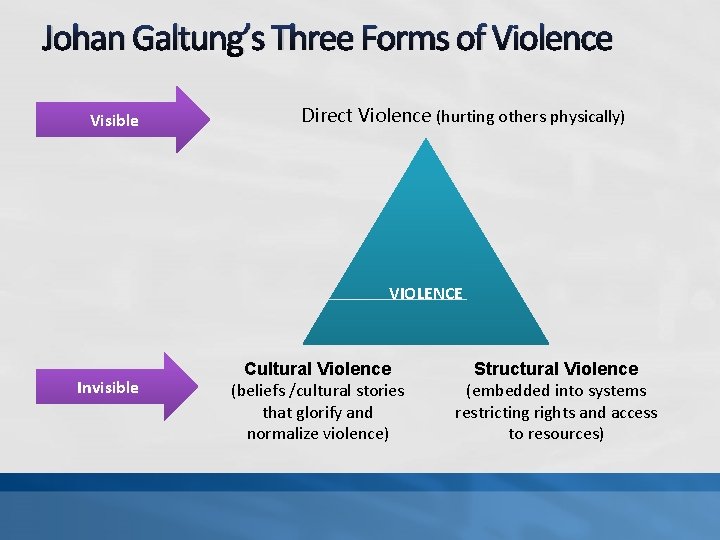
Johan Galtung’s Three Forms of Violence Visible Direct Violence (hurting others physically) VIOLENCE Invisible Cultural Violence (beliefs /cultural stories that glorify and normalize violence) Structural Violence (embedded into systems restricting rights and access to resources)
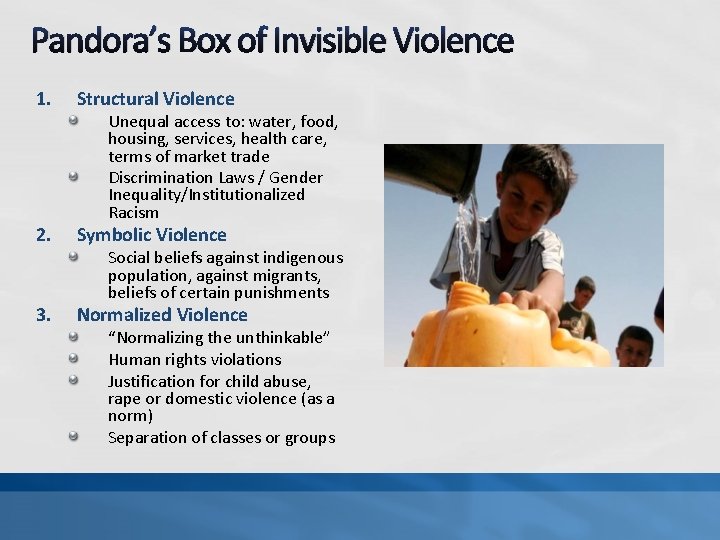
Pandora’s Box of Invisible Violence 1. Structural Violence 2. Symbolic Violence 3. Normalized Violence Unequal access to: water, food, housing, services, health care, terms of market trade Discrimination Laws / Gender Inequality/Institutionalized Racism Social beliefs against indigenous population, against migrants, beliefs of certain punishments “Normalizing the unthinkable” Human rights violations Justification for child abuse, rape or domestic violence (as a norm) Separation of classes or groups
Childhood Traumatic Stress 29 Child traumatic stress occurs when children and adolescents are exposed to traumatic events or traumatic situations that overwhelm their ability to cope. These reactions interfere with his or her daily life and ability to function and interact with others. -National Child Traumatic Stress Network
Events that can be considered traumatic 30 Neglect Accidents, Medical Procedures Natural /Man-Made Disasters Abuse: emotional, physical, sexual Bullying Exploitation/Human Trafficking Domestic Violence/Community Violence War/Torture Historical Trauma Military Life Transitions/Experiences Witnessing an “event”
In Young Children 31 Separation from parent or caregiver/attachment disruption Abuse Neglect Hunger Accidents/Physical Trauma Witnessing Violence (Family Violence) Impaired Caregiver Rapid developing brains increase vulnerability. Infants and Toddlers are impacted by problems affecting their parents. (e. g. Post-Partum Depression, substance abuse, disruptive bond or lack of understanding)
Common Responses to Traumatic Stress • • Physical Responses Mental Responses Behavioral Responses Social Responses
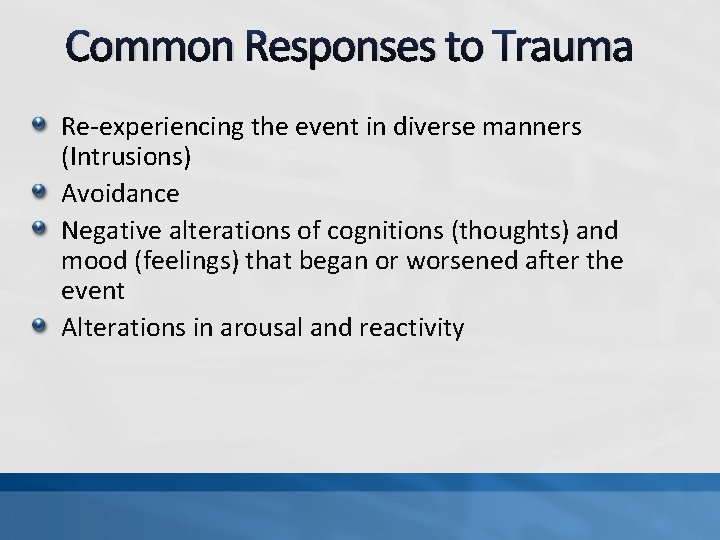
Common Responses to Trauma Re-experiencing the event in diverse manners (Intrusions) Avoidance Negative alterations of cognitions (thoughts) and mood (feelings) that began or worsened after the event Alterations in arousal and reactivity
Exposure to Trauma Exposure to traumatic events is related to the onset of behavior changes in children/youth. In some, it also increases the risk of onset of mental disorders: Depression* Anxiety Trauma-and-Stressor Related Disorders Other
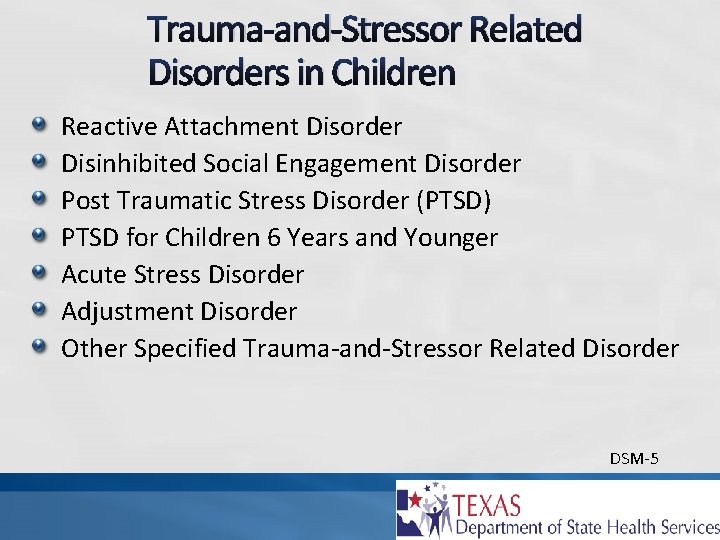
Trauma-and-Stressor Related Disorders in Children Reactive Attachment Disorder Disinhibited Social Engagement Disorder Post Traumatic Stress Disorder (PTSD) PTSD for Children 6 Years and Younger Acute Stress Disorder Adjustment Disorder Other Specified Trauma-and-Stressor Related Disorder DSM-5
The “HOW” How do you screen?
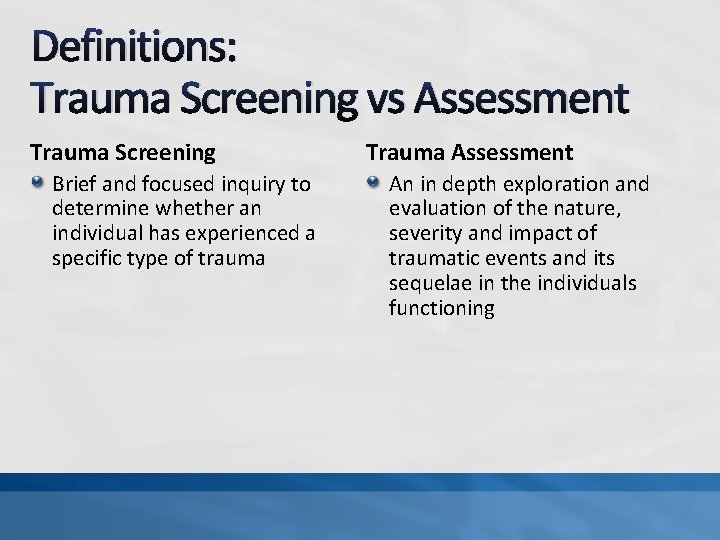
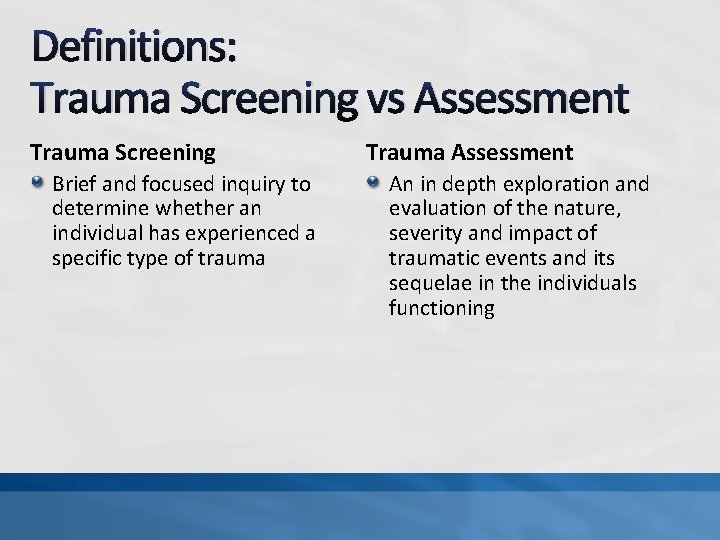
Definitions: Trauma Screening vs Assessment Trauma Screening Brief and focused inquiry to determine whether an individual has experienced a specific type of trauma Trauma Assessment An in depth exploration and evaluation of the nature, severity and impact of traumatic events and its sequelae in the individuals functioning

Types of Trauma Screenings History of traumatic event exposure (types of trauma exposure) Presence of Symptoms/responses to Trauma or Post Traumatic Stress Disorder Combines both history of exposure and presence of symptoms Multiple Symptoms of Trauma and Other related diagnosis or life domains (e. g. depression, anxiety, anger, trauma, PTSD, sexual concerns) (Strand, Sarmiento, and Pasquale, 2005)
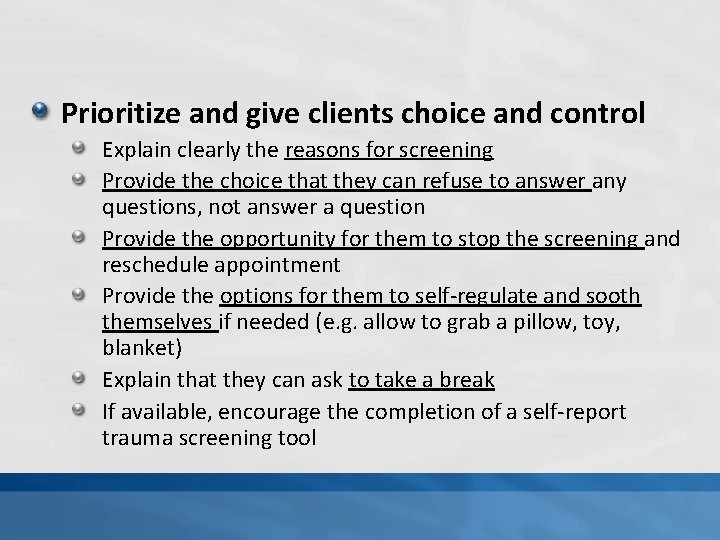
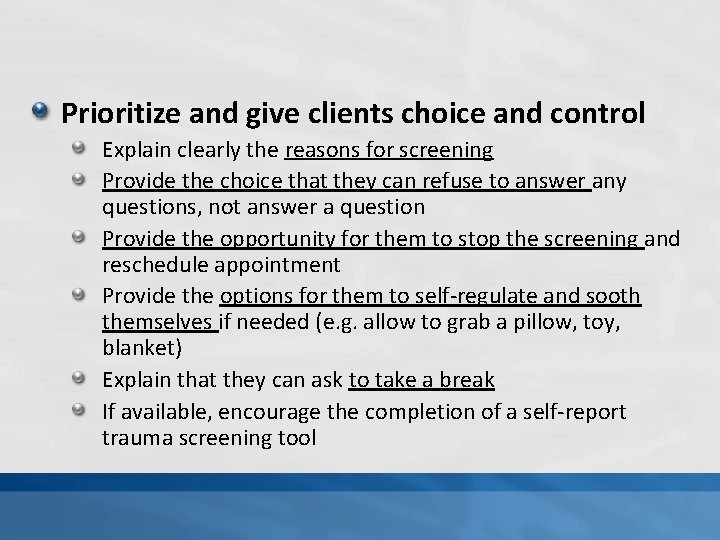
Prioritize and give clients choice and control Explain clearly the reasons for screening Provide the choice that they can refuse to answer any questions, not answer a question Provide the opportunity for them to stop the screening and reschedule appointment Provide the options for them to self-regulate and sooth themselves if needed (e. g. allow to grab a pillow, toy, blanket) Explain that they can ask to take a break If available, encourage the completion of a self-report trauma screening tool

How to Ask: Best Practice: Ask for exposure of all types of trauma (like a checklist) Other practice (not as effective) Ask general question: “Have you ever or has your child ever experience or have been exposed to an event or incident that was actual or threatening serious injury, violence or danger to you (child) or someone else? Or an event that someone can consider traumatic? ” How NOT to ask: “Have you ever experienced a traumatic event or witnessed trauma?
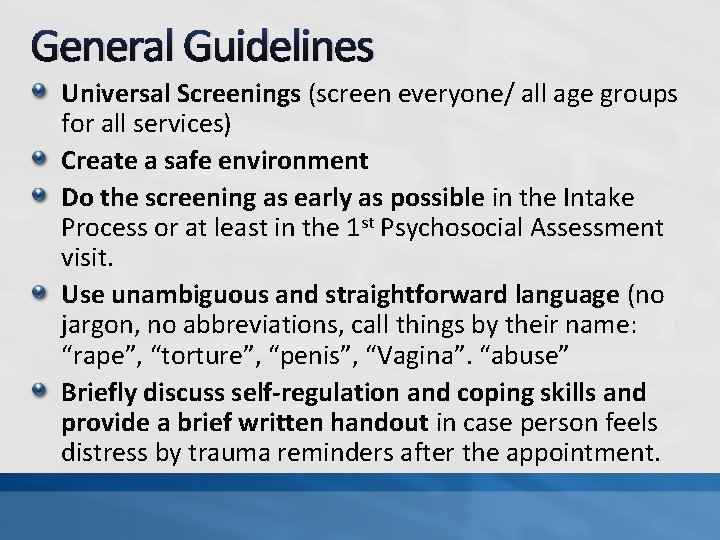
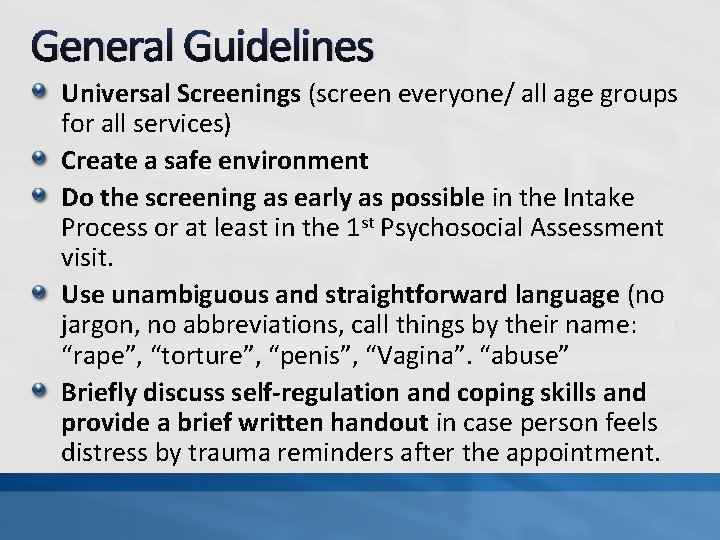
General Guidelines Universal Screenings (screen everyone/ all age groups for all services) Create a safe environment Do the screening as early as possible in the Intake Process or at least in the 1 st Psychosocial Assessment visit. Use unambiguous and straightforward language (no jargon, no abbreviations, call things by their name: “rape”, “torture”, “penis”, “Vagina”. “abuse” Briefly discuss self-regulation and coping skills and provide a brief written handout in case person feels distress by trauma reminders after the appointment.
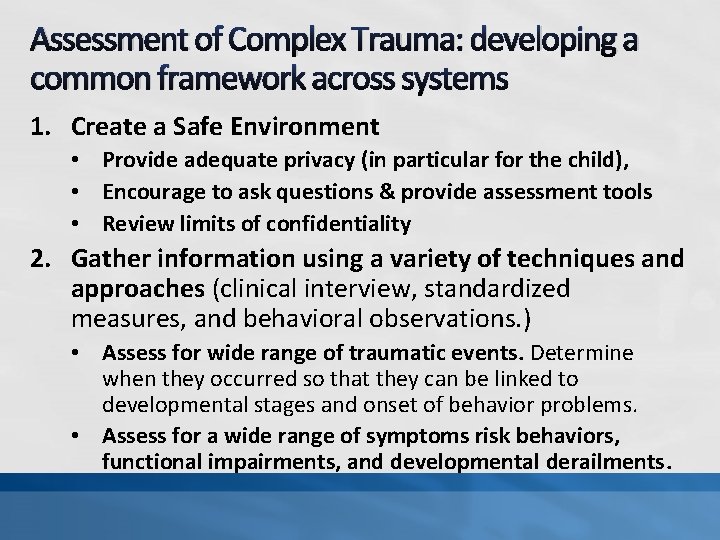
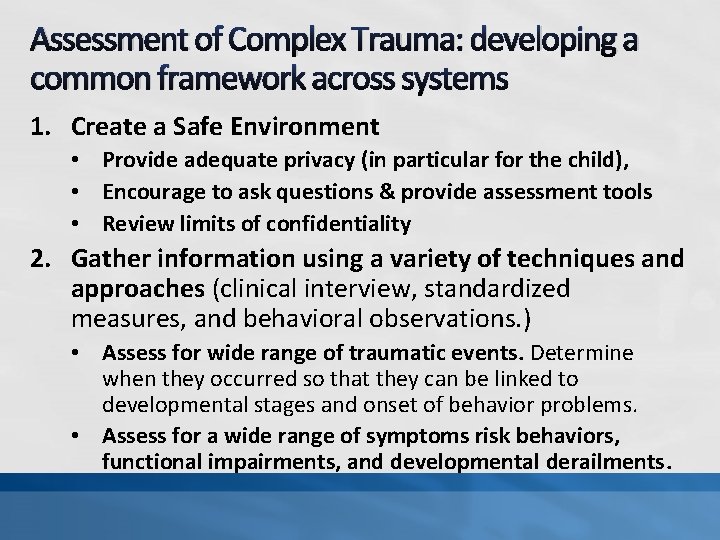
Assessment of Complex Trauma: developing a common framework across systems 1. Create a Safe Environment • Provide adequate privacy (in particular for the child), • Encourage to ask questions & provide assessment tools • Review limits of confidentiality 2. Gather information using a variety of techniques and approaches (clinical interview, standardized measures, and behavioral observations. ) • Assess for wide range of traumatic events. Determine when they occurred so that they can be linked to developmental stages and onset of behavior problems. • Assess for a wide range of symptoms risk behaviors, functional impairments, and developmental derailments.
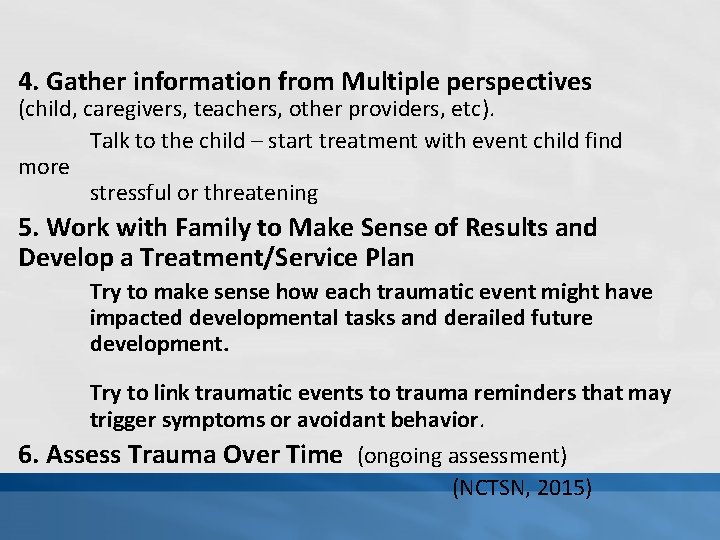
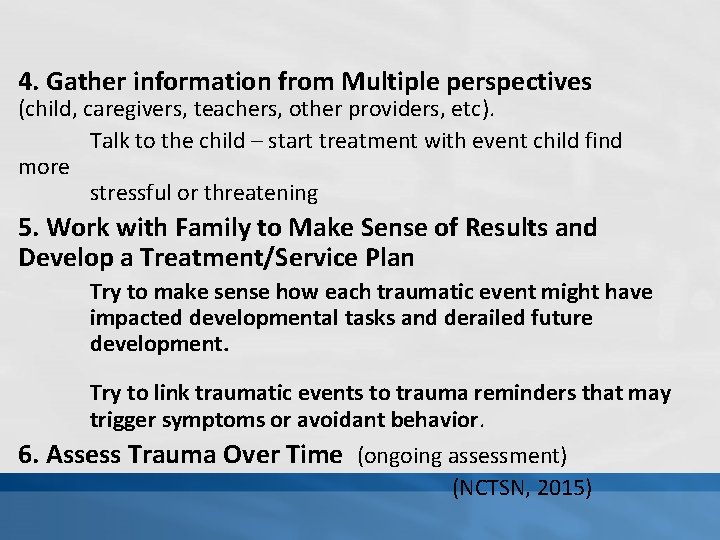
4. Gather information from Multiple perspectives (child, caregivers, teachers, other providers, etc). Talk to the child – start treatment with event child find more stressful or threatening 5. Work with Family to Make Sense of Results and Develop a Treatment/Service Plan Try to make sense how each traumatic event might have impacted developmental tasks and derailed future development. Try to link traumatic events to trauma reminders that may trigger symptoms or avoidant behavior. 6. Assess Trauma Over Time (ongoing assessment) (NCTSN, 2015)
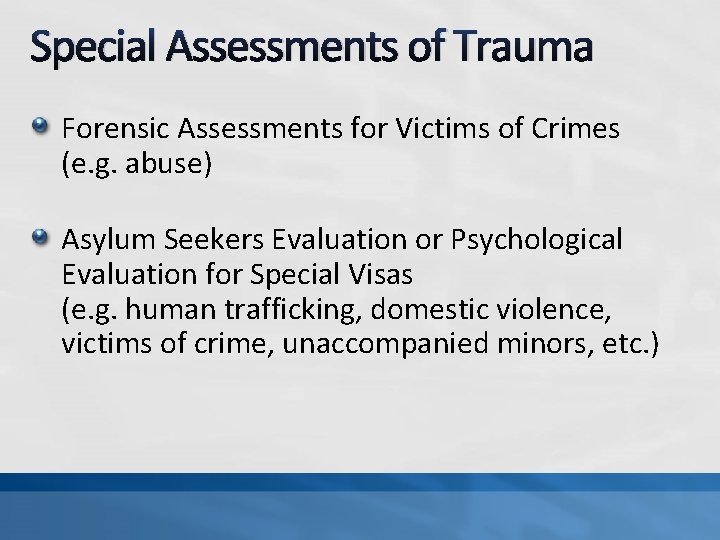
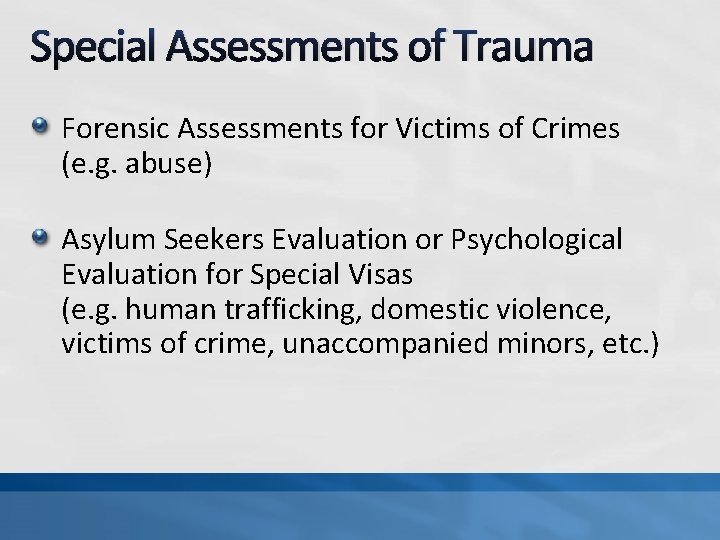
Special Assessments of Trauma Forensic Assessments for Victims of Crimes (e. g. abuse) Asylum Seekers Evaluation or Psychological Evaluation for Special Visas (e. g. human trafficking, domestic violence, victims of crime, unaccompanied minors, etc. )
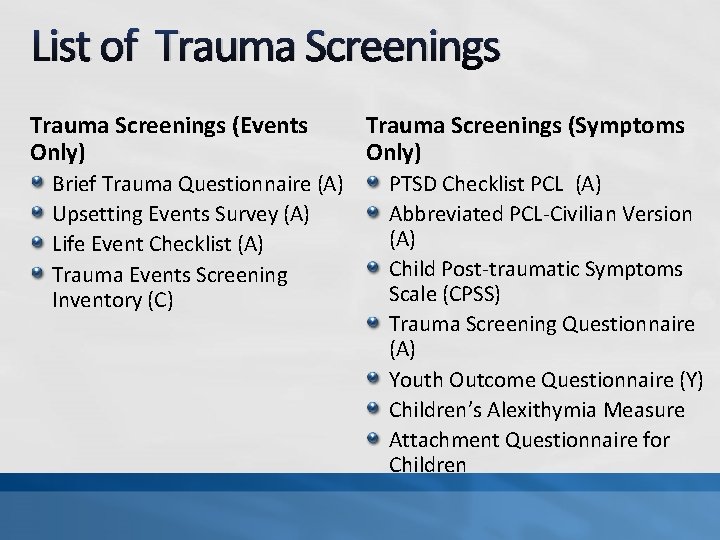
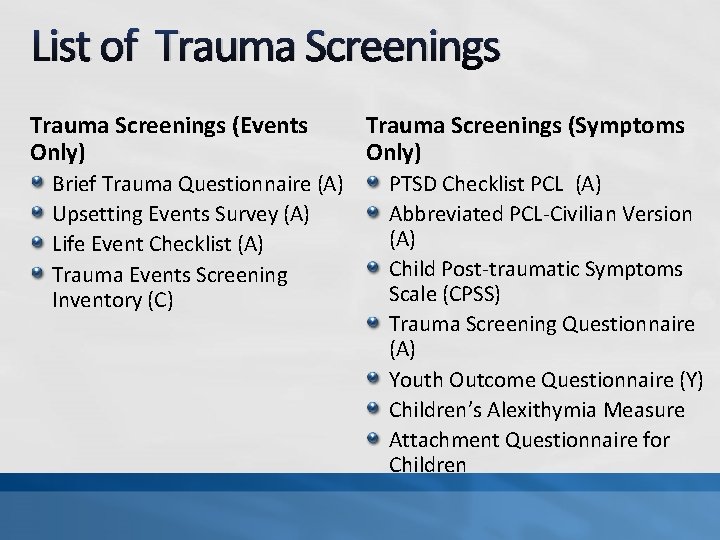
List of Trauma Screenings (Events Only) Brief Trauma Questionnaire (A) Upsetting Events Survey (A) Life Event Checklist (A) Trauma Events Screening Inventory (C) Trauma Screenings (Symptoms Only) PTSD Checklist PCL (A) Abbreviated PCL-Civilian Version (A) Child Post-traumatic Symptoms Scale (CPSS) Trauma Screening Questionnaire (A) Youth Outcome Questionnaire (Y) Children’s Alexithymia Measure Attachment Questionnaire for Children
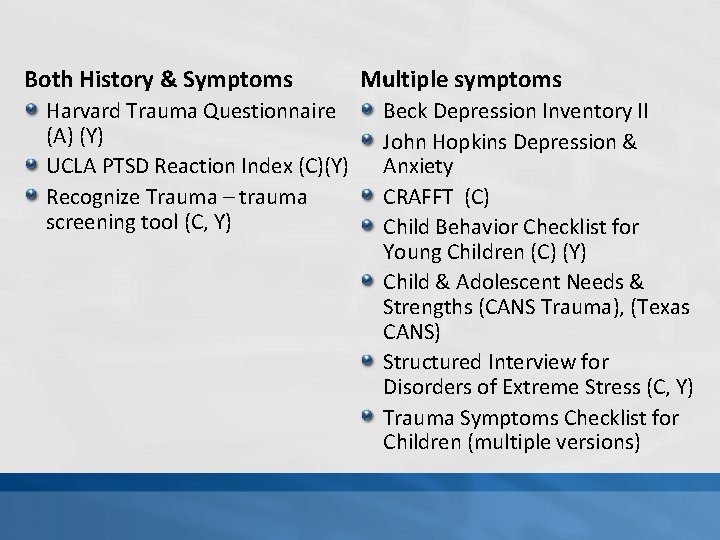
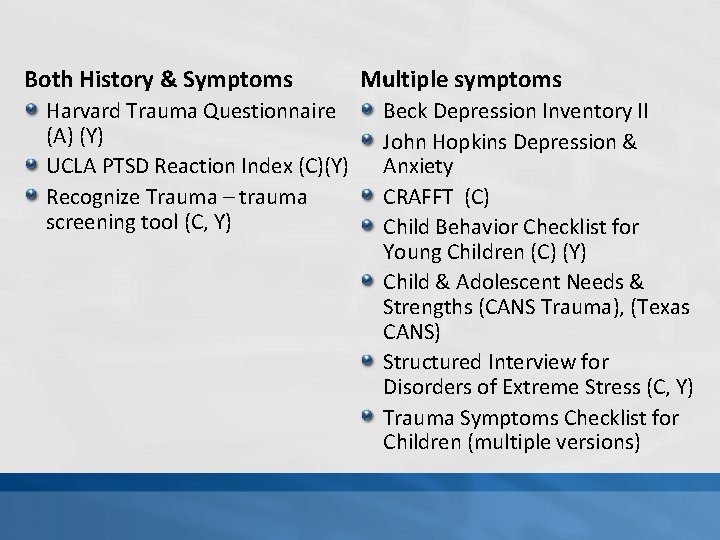
Both History & Symptoms Harvard Trauma Questionnaire (A) (Y) UCLA PTSD Reaction Index (C)(Y) Recognize Trauma – trauma screening tool (C, Y) Multiple symptoms Beck Depression Inventory II John Hopkins Depression & Anxiety CRAFFT (C) Child Behavior Checklist for Young Children (C) (Y) Child & Adolescent Needs & Strengths (CANS Trauma), (Texas CANS) Structured Interview for Disorders of Extreme Stress (C, Y) Trauma Symptoms Checklist for Children (multiple versions)
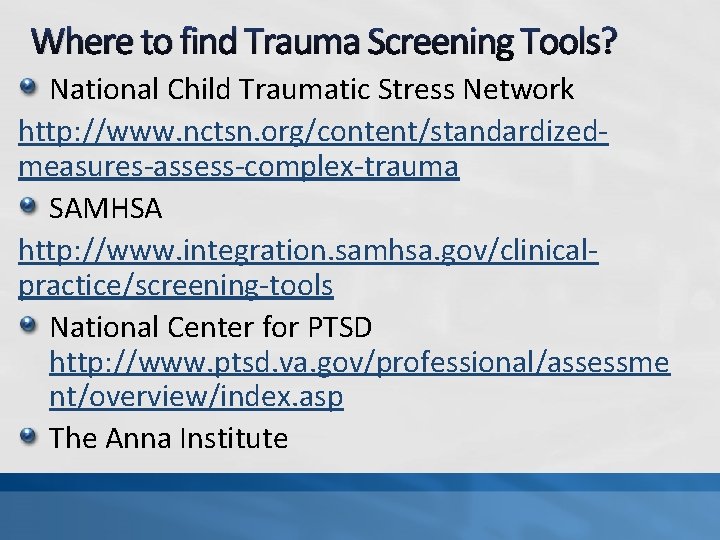
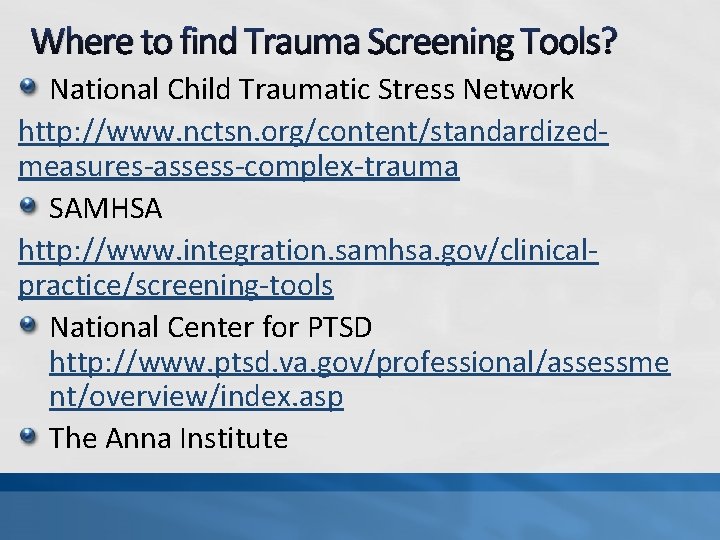
Where to find Trauma Screening Tools? National Child Traumatic Stress Network http: //www. nctsn. org/content/standardizedmeasures-assess-complex-trauma SAMHSA http: //www. integration. samhsa. gov/clinicalpractice/screening-tools National Center for PTSD http: //www. ptsd. va. gov/professional/assessme nt/overview/index. asp The Anna Institute
Children's Mental Health Awareness Walk nd Saturday, May 2 2015 Texas State Capitol
Texas Children Recovering From Trauma Aim: Transform children’s mental health services in Texas into a trauma-informed care system that fosters resilience and recovery. How? Creating a Category III Community Treatment Services Centers members of the National Child Traumatic Stress Network (NCTSN) and their learning community: Heart of Texas Region MHMR Center Serves the following counties: Bosque, Hill, Mc. Lennan, Falls, Limestone and Freestone. Target Population: Children ages 3 to 17 impacted by trauma or children of military families. Funded by: SAMHSA’s National Child Traumatic Stress Initiative Grant No: 1 U 79 SM 061177 -01 Funding Period Oct 2012 -Sept 2016
How? Through Training: Creating Community Partners Creating of a Statewide Transformation Strategic Plan Statewide Summit on Transformation to Trauma. Informed Care ANNOUNCEMENTS: TRAUMA INFORMED NETWORK OF TEXAS TRAUMA INFORMED CARE SUMMIT (Join Us!) (August 2016)
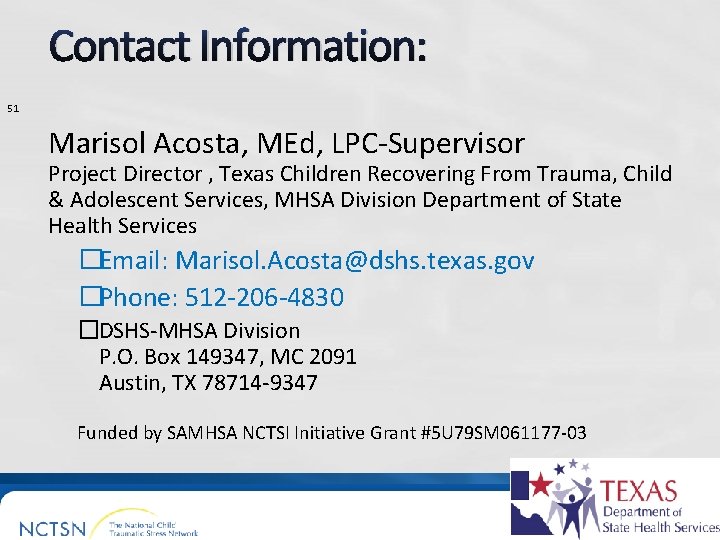
Contact Information: 51 Marisol Acosta, MEd, LPC-Supervisor Project Director , Texas Children Recovering From Trauma, Child & Adolescent Services, MHSA Division Department of State Health Services �Email: Marisol. Acosta@dshs. texas. gov �Phone: 512 -206 -4830 �DSHS-MHSA Division P. O. Box 149347, MC 2091 Austin, TX 78714 -9347 Funded by SAMHSA NCTSI Initiative Grant #5 U 79 SM 061177 -03
 Marisol acosta
Marisol acosta Universidad cecilio acosta enfermería
Universidad cecilio acosta enfermería Paula molina acosta
Paula molina acosta Test del bastón de galtón
Test del bastón de galtón Hospital federico lleras acosta ese - sede limonar
Hospital federico lleras acosta ese - sede limonar Darin acosta
Darin acosta Humberto ibarrola
Humberto ibarrola Colegio universitario cecilio acosta
Colegio universitario cecilio acosta Alvaro acosta de hart
Alvaro acosta de hart Ihfanın tanımı
Ihfanın tanımı Marisol es tan simpatica
Marisol es tan simpatica Marisol rubecindo
Marisol rubecindo Marisol vicens bello
Marisol vicens bello Marisol escobar biografia
Marisol escobar biografia Mucho gusto rosabel in english
Mucho gusto rosabel in english Marisol left and right
Marisol left and right En que coinciden víctor y marisol
En que coinciden víctor y marisol Marissol pedroza nua
Marissol pedroza nua Marisol henao
Marisol henao Como se cita una imagen
Como se cita una imagen Marisol giraud
Marisol giraud Marisol aguila
Marisol aguila Pronostico marisol
Pronostico marisol Kswan vc
Kswan vc The text-based director, also known as the
The text-based director, also known as the Responsabilidades de un director de escuela
Responsabilidades de un director de escuela Penitenciarul miercurea ciuc
Penitenciarul miercurea ciuc Tugas director syarikat
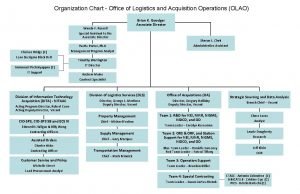
Tugas director syarikat Logistics organizational chart
Logistics organizational chart Director marketing turistico tenerife
Director marketing turistico tenerife Oliver stone
Oliver stone Salaam bombay! nominations
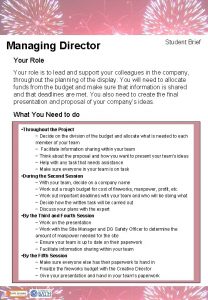
Salaam bombay! nominations Role brief
Role brief Types of span of control in organization
Types of span of control in organization Nuh management structure
Nuh management structure Emerald director usana salary
Emerald director usana salary Floor manager signals
Floor manager signals Fashion show staff positions
Fashion show staff positions Importance of audience in theatre
Importance of audience in theatre Electron donating groups examples
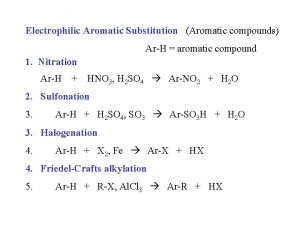
Electron donating groups examples Vestuario del teatro griego
Vestuario del teatro griego Director del pianista
Director del pianista Director regional de alajuela
Director regional de alajuela Director of technical education hp
Director of technical education hp Director message in company profile
Director message in company profile Director class
Director class Change management pictures
Change management pictures Bartholomew cubbins director
Bartholomew cubbins director Traffic director triage
Traffic director triage Qualification of a director
Qualification of a director Cisco threat intelligence director
Cisco threat intelligence director Organigrama ani
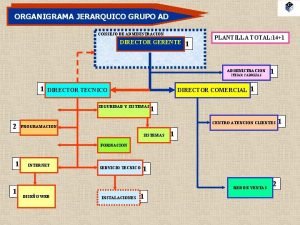
Organigrama ani