TRAUMA Informed Care Practice UNDERSTANDING TRAUMA FRAMEWORK FOR





- Slides: 63
TRAUMA Informed Care & Practice UNDERSTANDING TRAUMA: FRAMEWORK FOR SUPPORTS Trisha Wright and Gail Clarke RSA 1
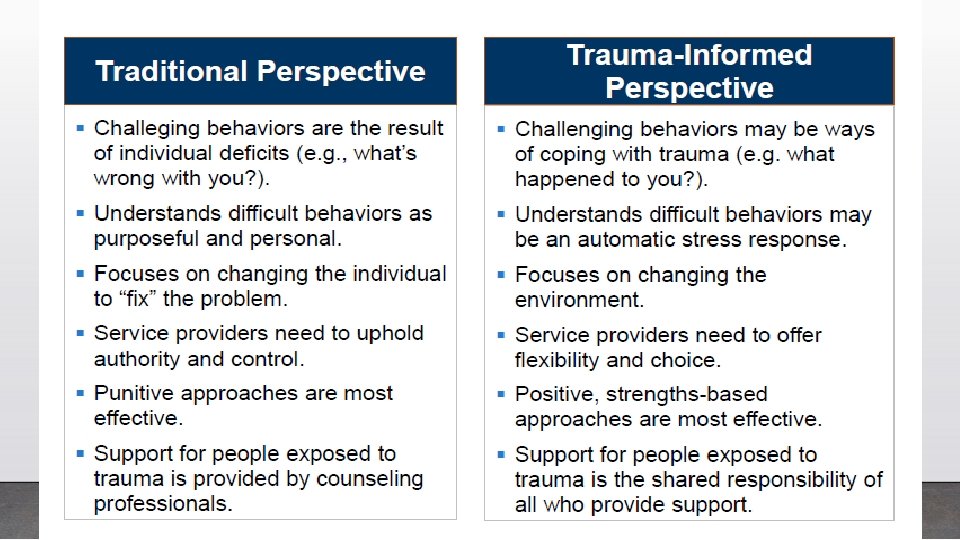
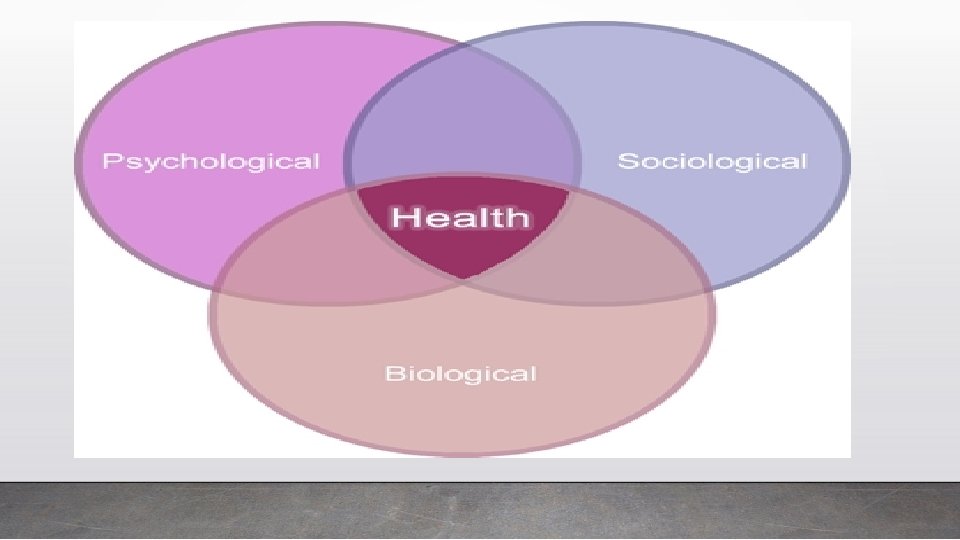
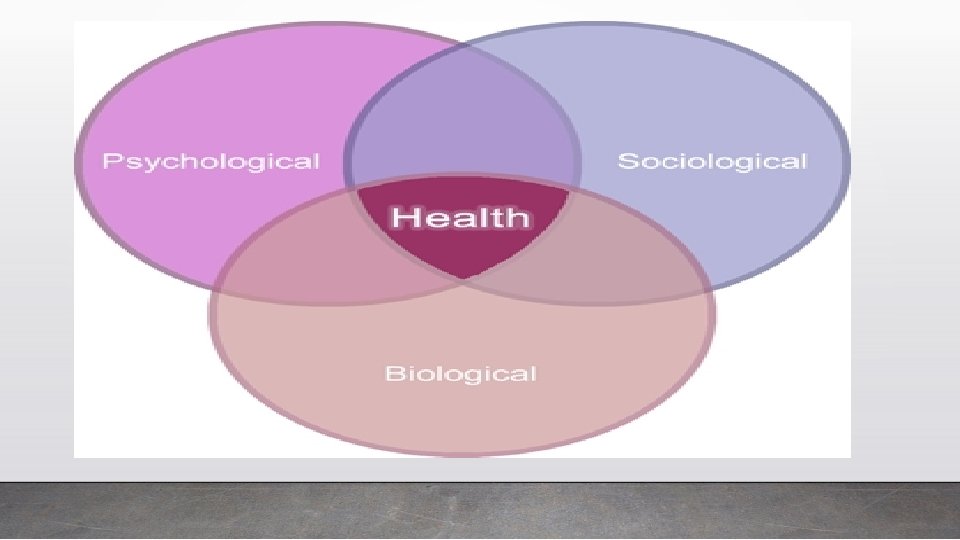
So what is trauma informed practice? v A strengths based framework grounded in an understanding of the impact of trauma with the people we serve v Promotes psychological, physical, and emotional safety for both providers and survivors v Provides opportunities for survivors to rebuild a sense control and empowerment in their life
THE CORE VALUES OF TRAUMA INFORMED CARE üSafety üTrustworthiness and Transparency üPeer Support üCollaboration üEmpowerment, Voice, and Choice üCultural, Historical and Gender Issues

Why Incorporate TIC within your agency? • Current literature indicates many people have experienced some form of trauma (SAMSHA, 2010) • Both clients and care providers may have a history of trauma • Experts believe up to 95% of people with intellectual disabilities have experienced some form of trauma • It makes sense from the start use this approach because we do not always know someone's history, and this approach will not harm someone if they have not experienced trauma.
Research • People with developmental disabilities are more likely than non-disabled people to experience physical, emotional and sexual abuse and neglect (anywhere from 1. 5 to 10 times greater) • Ruth Ryan (1994) found that of 310 people with developmental disabilities referred for treatment, almost all had experienced at least one severe traumatic event and 16. 5% (51 people) met the criteria for PTSD • None had been diagnosed with PTSD previously, instead many had been misdiagnosed with schizophrenia Ryan, R. (1994). Posttraumatic Stress Disorder in Persons with Developmental Disabilities Community Mental Health Journal, Vol. 30, No. 1. 45 -54. 6
Trauma Informed Systems ü Can Increase the and engagement and effectiveness of treatment with clients who have experienced trauma ü Decrease the likelihood that clients are re-traumatized ü Decrease the secondary trauma and compassion fatigue experienced by staff
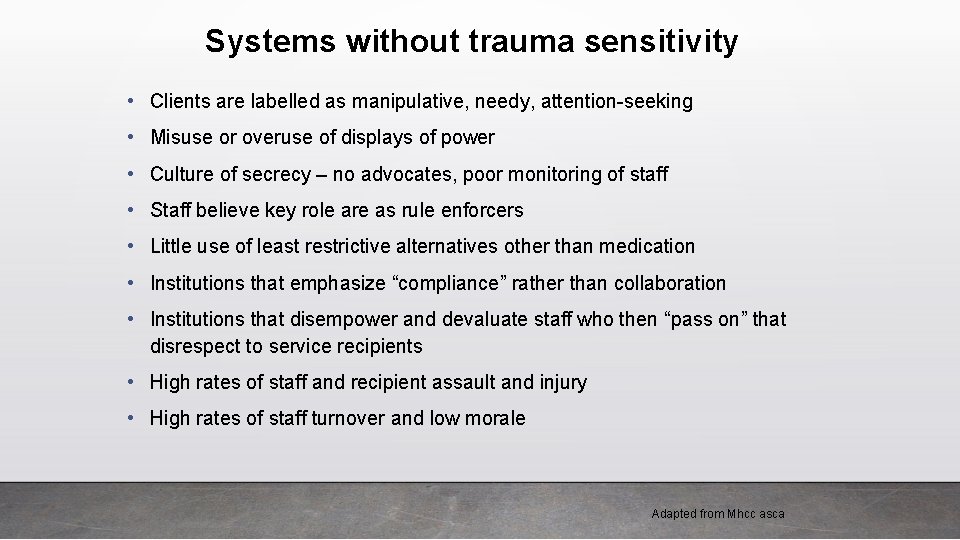
Systems without trauma sensitivity • Clients are labelled as manipulative, needy, attention-seeking • Misuse or overuse of displays of power • Culture of secrecy – no advocates, poor monitoring of staff • Staff believe key role are as rule enforcers • Little use of least restrictive alternatives other than medication • Institutions that emphasize “compliance” rather than collaboration • Institutions that disempower and devaluate staff who then “pass on” that disrespect to service recipients • High rates of staff and recipient assault and injury • High rates of staff turnover and low morale Adapted from Mhcc asca
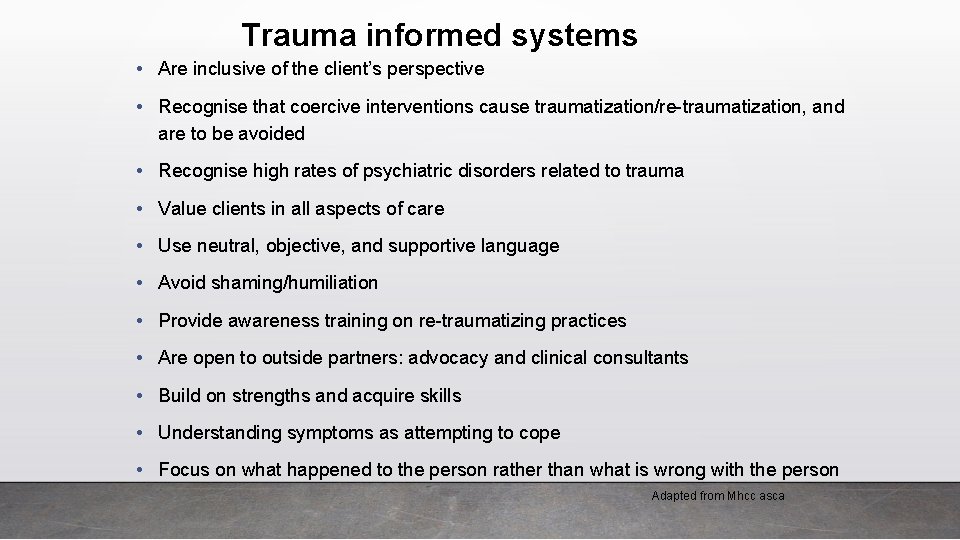
Trauma informed systems • Are inclusive of the client’s perspective • Recognise that coercive interventions cause traumatization/re-traumatization, and are to be avoided • Recognise high rates of psychiatric disorders related to trauma • Value clients in all aspects of care • Use neutral, objective, and supportive language • Avoid shaming/humiliation • Provide awareness training on re-traumatizing practices • Are open to outside partners: advocacy and clinical consultants • Build on strengths and acquire skills • Understanding symptoms as attempting to cope • Focus on what happened to the person rather than what is wrong with the person Adapted from Mhcc asca
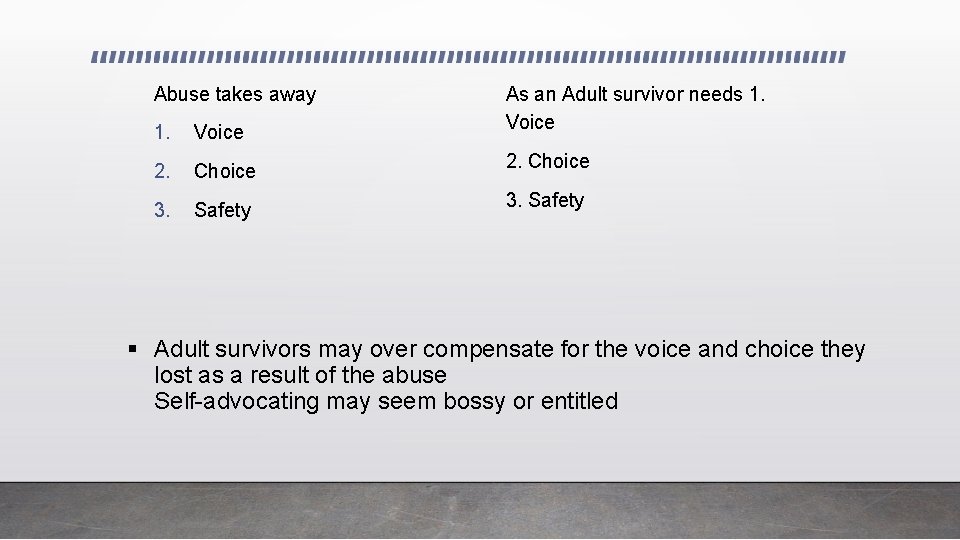
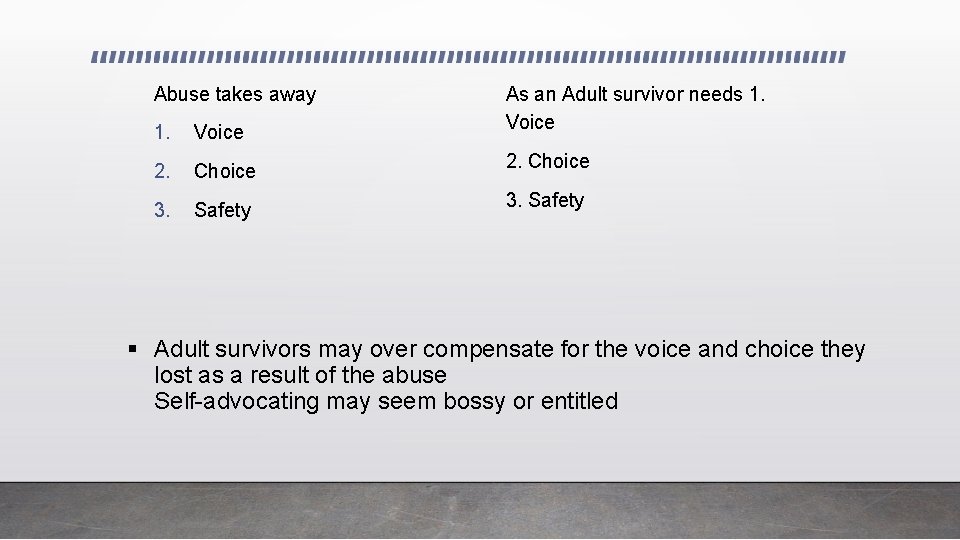
Abuse takes away 1. Voice As an Adult survivor needs 1. Voice 2. Choice 2. Choice 3. Safety 3. Safety § Adult survivors may over compensate for the voice and choice they lost as a result of the abuse Self-advocating may seem bossy or entitled
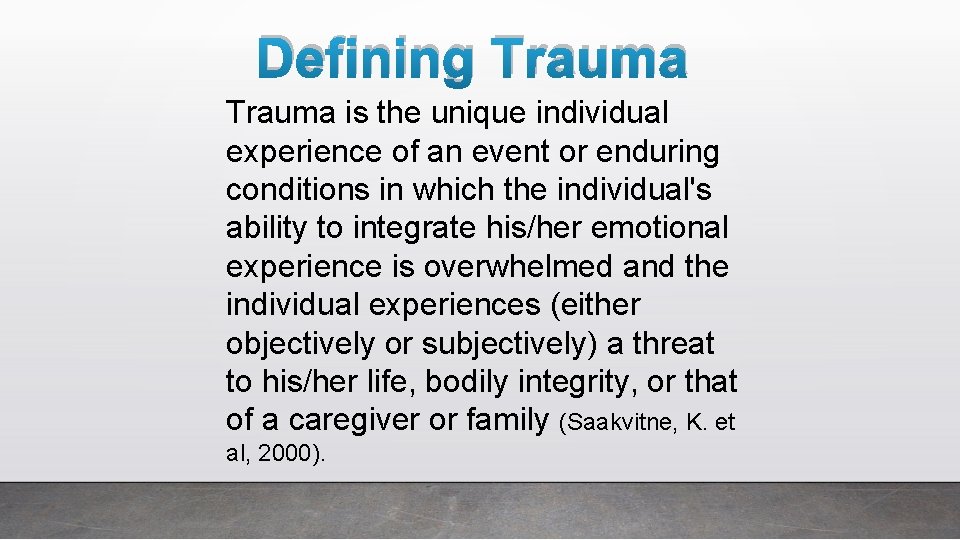
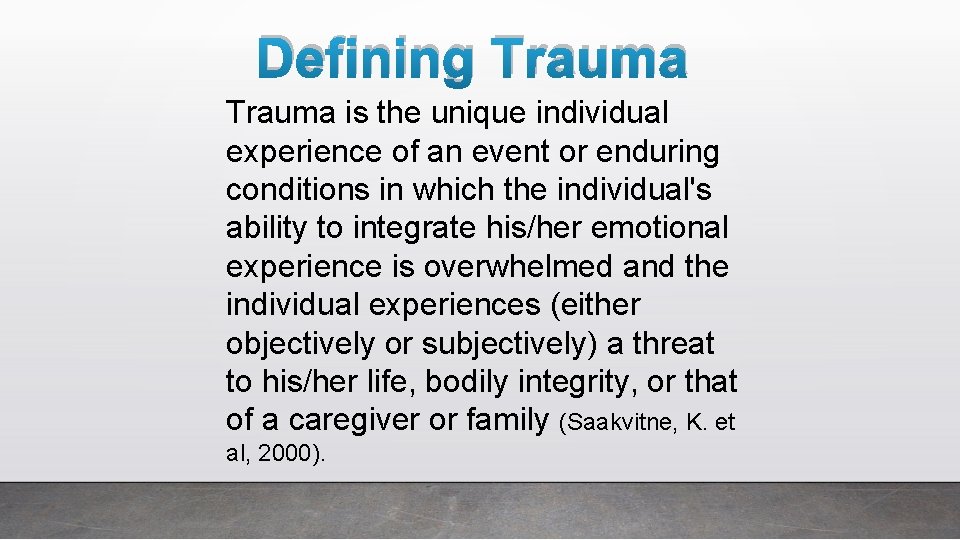
Defining Trauma is the unique individual experience of an event or enduring conditions in which the individual's ability to integrate his/her emotional experience is overwhelmed and the individual experiences (either objectively or subjectively) a threat to his/her life, bodily integrity, or that of a caregiver or family (Saakvitne, K. et al, 2000).
• Trauma is feeling unsafe and out of control • Everything someone does after a trauma is to try to maintain or regain a sense of safety and control • Often interpreted as being manipulative or selfish • Trauma is always waiting for something good to be destroyed
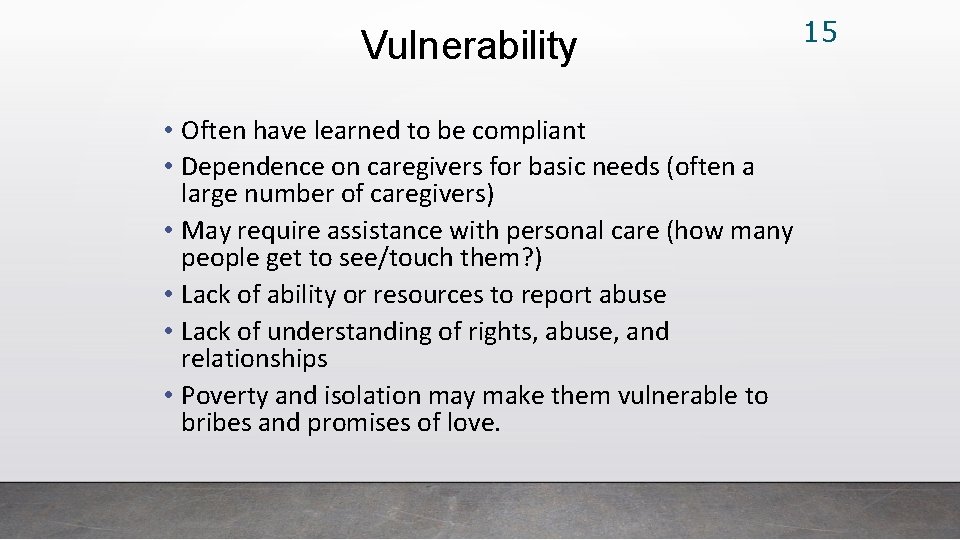
Vulnerability • Often have learned to be compliant • Dependence on caregivers for basic needs (often a large number of caregivers) • May require assistance with personal care (how many people get to see/touch them? ) • Lack of ability or resources to report abuse • Lack of understanding of rights, abuse, and relationships • Poverty and isolation may make them vulnerable to bribes and promises of love. 15
Challenges 16 • Some “treatments” for people with intellectual developmental disabilities (IDD) are traumatic or perpetuate trauma (e. g. aversive therapies, seclusion time out, restraints) • Assessment instruments are not ‘normed’ for people with intellectual developmental disabilities • Very difficult to assess those with limited verbal communication • Lack of professionals trained and comfortable to support this population in trauma processing work • Most trauma in this population is complex trauma, however the current understanding of trauma in Mental Health fields does not encompass the multiple and chronic abuse experiences of people with IDD • Untreated trauma will persist
17 Challenges…cont’d In people with IDD, the most consistent indicator of trauma is aggression
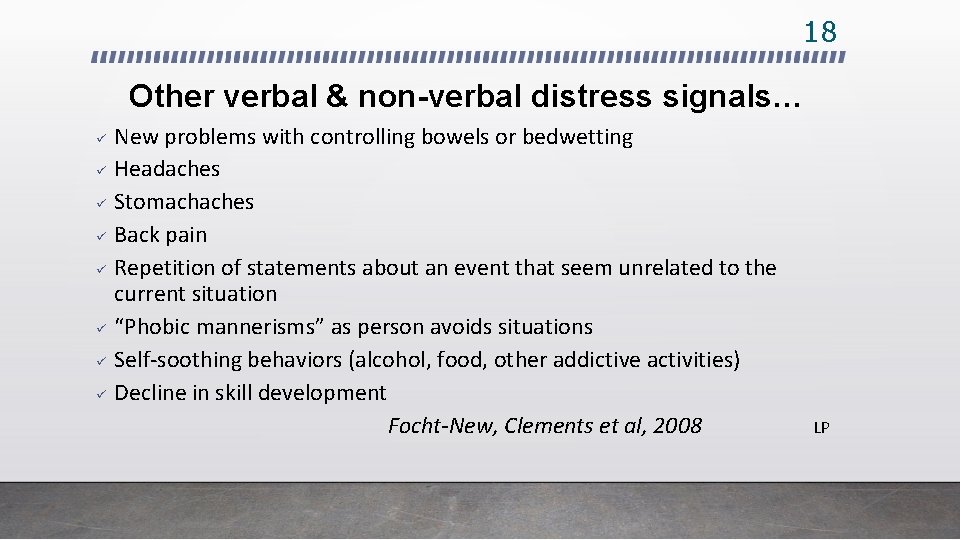
18 Other verbal & non-verbal distress signals… ü ü ü ü New problems with controlling bowels or bedwetting Headaches Stomachaches Back pain Repetition of statements about an event that seem unrelated to the current situation “Phobic mannerisms” as person avoids situations Self-soothing behaviors (alcohol, food, other addictive activities) Decline in skill development Focht-New, Clements et al, 2008 LP
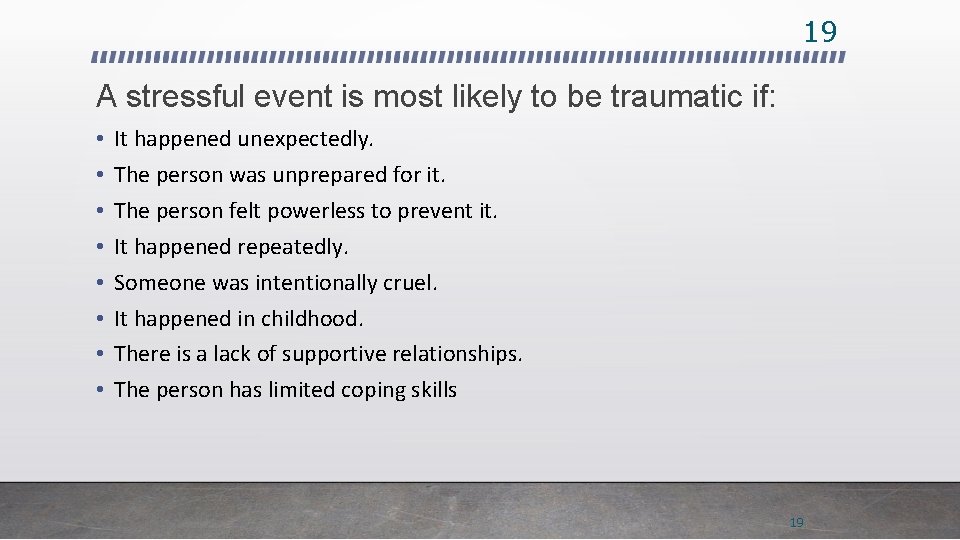
19 A stressful event is most likely to be traumatic if: • • It happened unexpectedly. The person was unprepared for it. The person felt powerless to prevent it. It happened repeatedly. Someone was intentionally cruel. It happened in childhood. There is a lack of supportive relationships. The person has limited coping skills 19
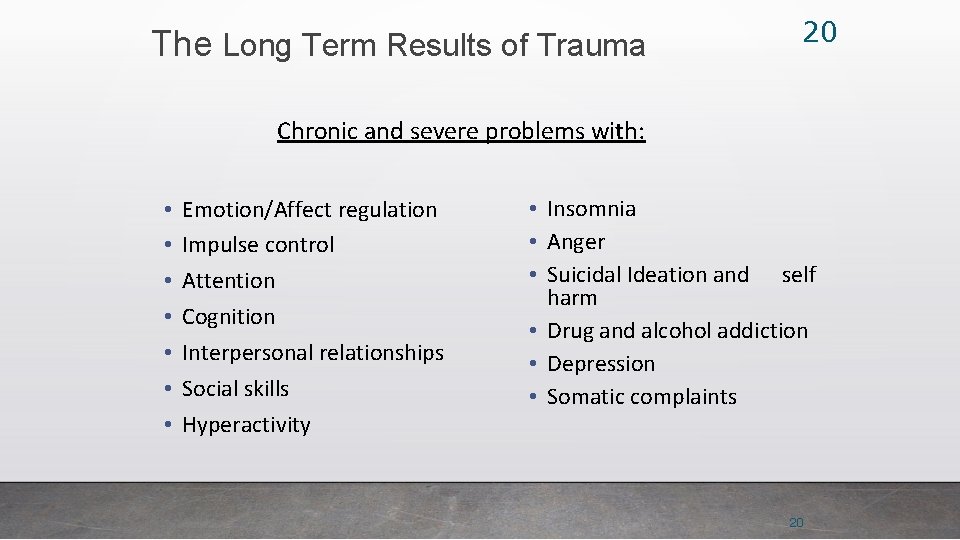
The Long Term Results of Trauma 20 Chronic and severe problems with: • • Emotion/Affect regulation Impulse control Attention Cognition Interpersonal relationships Social skills Hyperactivity • Insomnia • Anger • Suicidal Ideation and self harm • Drug and alcohol addiction • Depression • Somatic complaints 20
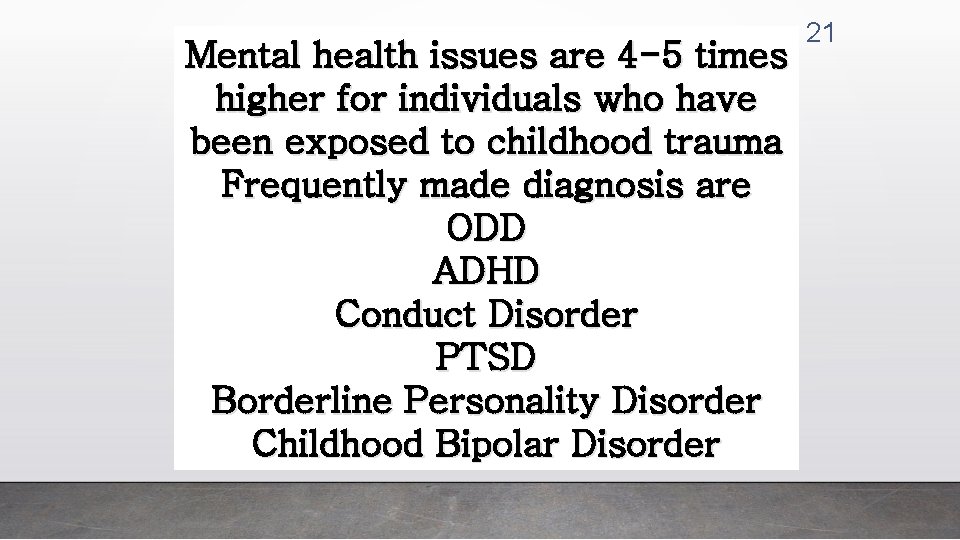
Mental health issues are 4 -5 times higher for individuals who have been exposed to childhood trauma Frequently made diagnosis are ODD ADHD Conduct Disorder PTSD Borderline Personality Disorder Childhood Bipolar Disorder 21
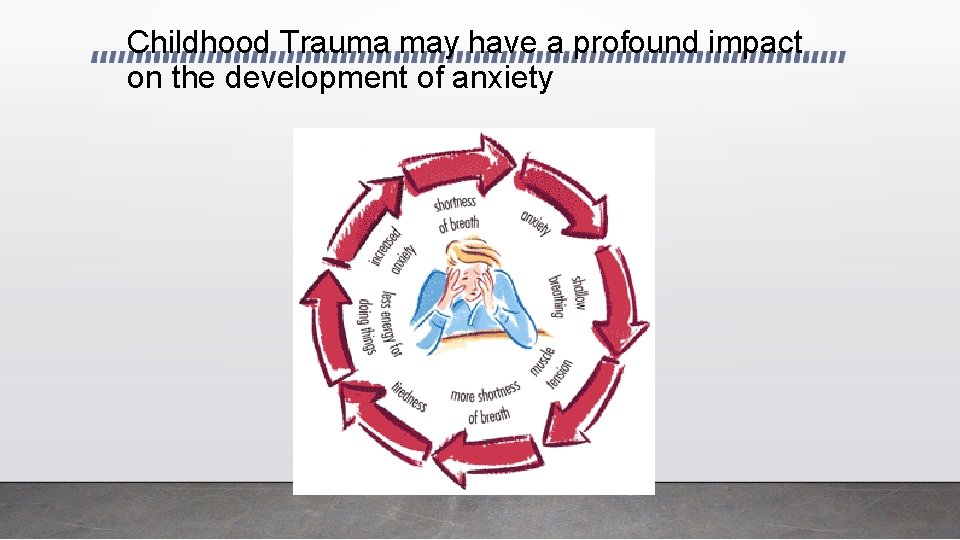
Childhood Trauma may have a profound impact on the development of anxiety
Anxiety
Anxiety • Studies 14% to 26. 85% adults with DD had comorbid anxiety disorder Why Is Anxiety Hard to See in Clients with ID? • Difficulty describing internalizing symptoms of anxiety • Deficits in communication, social skills and intellectual functioning • Challenging behaviors may mask anxiety https: //coc. unm. edu/common/training/Anxiety%20 Intellectual%20 Disability. pdf
Recognising anxiety disorders Cont’d 1. Emotions: Unrealistic or excessive fear, irritability, impatience, anger, confusion, feeling on edge, nervousness, depressed mood 2. Thoughts: Lots of worry about past or future events, mind racing or going blank, poorer concentration and memory and trouble making decisions 3. Behaviour: Avoiding situations or people, obsessive or compulsive behaviour, withdrawal or distress in social situations, increased use of alcohol or other drugs 4. Physical: Pounding heart, chest pain, rapid heartbeat, blushing, rapid shortness of breath, dizziness, headache, sweating, stomach pains, nausea, vomiting, and diarrhoea, muscle aches and pains (especially neck, shoulders and back), restlessness and tremors and difficulty sleeping https: //rampages. us/LENDfiles/intellectual-disability-and-anxiety-disorders. pdf
Individual Interventions • Analyze specific behaviors related to anxiety and trigger • Consistently reinforce positive, calming, relaxing behavior and use of skills • Use of proactive and instructive modeling strategies to encourage positive behaviors and problem solve with the client • Teach client with ID to self-monitor anxiety and cue when needed https: //coc. unm. edu/common/training/Anxiety%20 Intellectual%20 Disability. pdf
Individual Interventions Cont’d • Provide activities and opportunities to engage with others • Teaching techniques for improving communication • Setting boundaries • Positive reinforcement of desired behaviors, non-contingent reinforcement procedures • Activity schedules for predictability
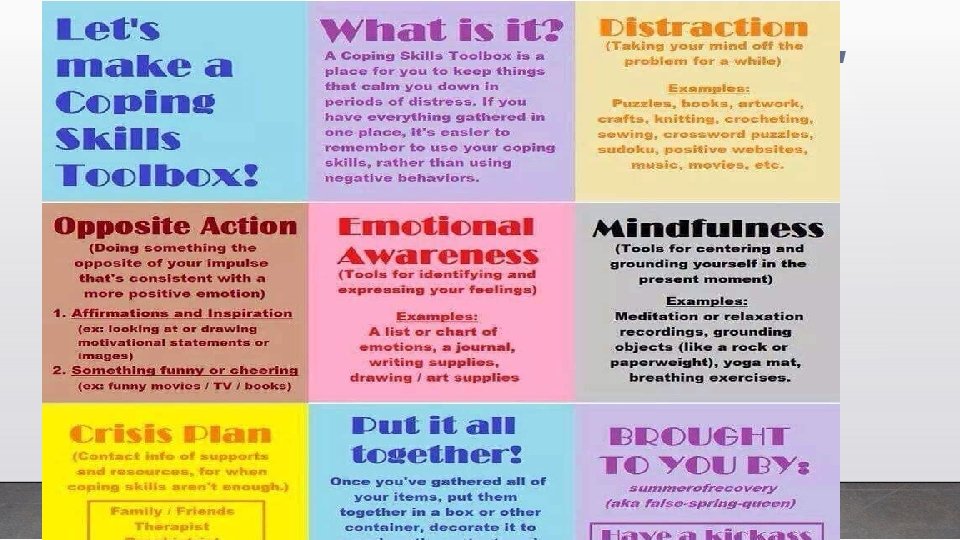
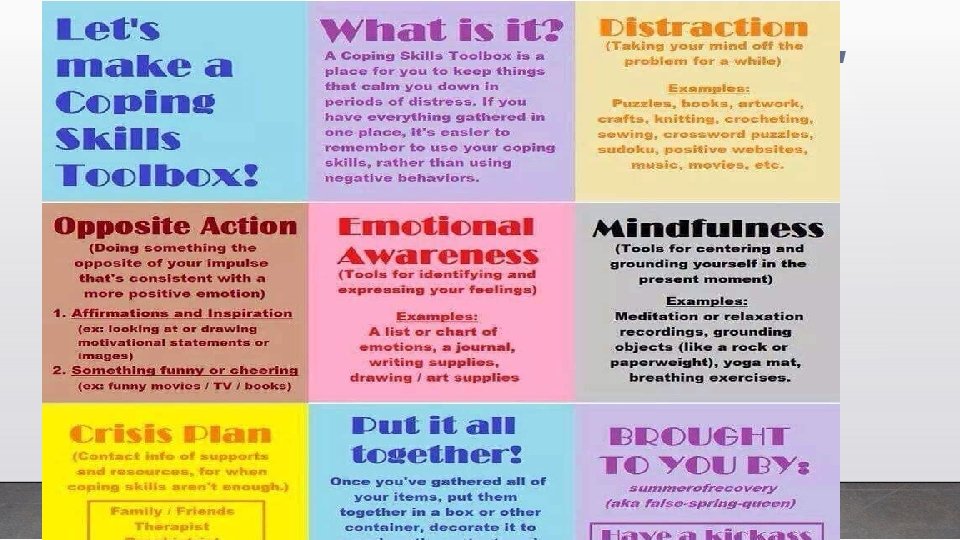
28 Symptom Management Skills Help people understand manage their responses • Teach coping skills • Management of symptoms (e. g. hyperarousal, intrusive thoughts, dissociation, flashbacks, body memories etc. ) • Socio-sexual education • Teach norms and boundaries within relationships • Teach emotion recognition • Teach affect regulation skills to modulate emotion 28
29 Key Messages in Psycho-Education • • • Normalize and validate the person’s experiences (It makes sense that you would feel/react that way – you felt overwhelmed/scared/frustrated) Trauma responses are a normal reaction to an abnormal situation or event Educate the person about the impact trauma can have on them Reframe symptoms as adaptations Identify and reinforce the person’s strengths Help the person to understand her/himself 29
30 Making Psycho-Education and Skill Building Accessible • • • Use visuals to support the learning of all concepts Present one concept at a time Go slow and review often Ensure the whole team is aware and supportive of strategies being learned Make use of a variety of teaching tools (modeling, written and pictorial information, role play, videos etc. ) 30
31 Making Psycho-Education and Skill Building Accessible…cont’d • • Adapt tools to person’s specific skills and developmental level Ensure that skills taught for self soothing or calming are never turned into punitive tasks Practice skills first in a calm and neutral state, then use them in the moment as needed Ongoing evaluation of tools and techniques (what’s working? What isn’t? ) 31
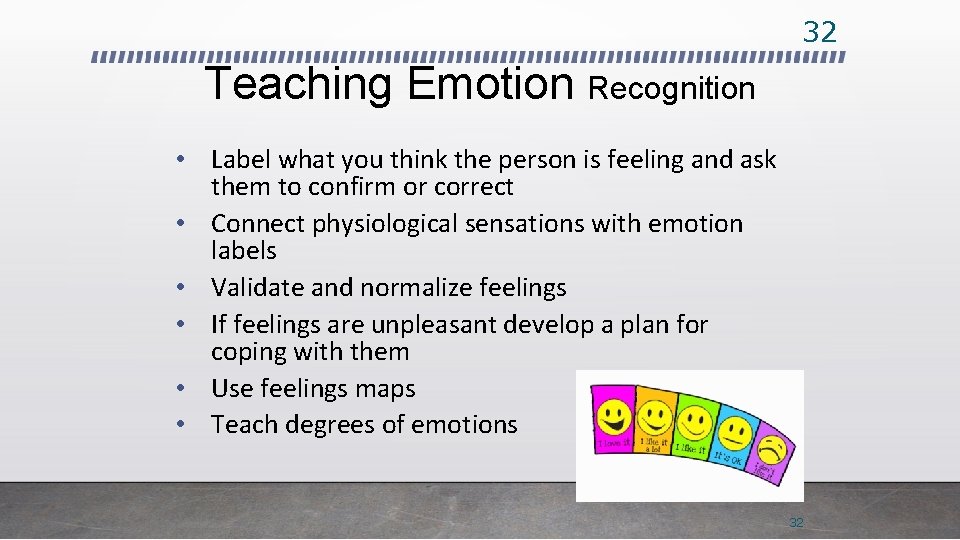
32 Teaching Emotion Recognition • Label what you think the person is feeling and ask them to confirm or correct • Connect physiological sensations with emotion labels • Validate and normalize feelings • If feelings are unpleasant develop a plan for coping with them • Use feelings maps • Teach degrees of emotions 32
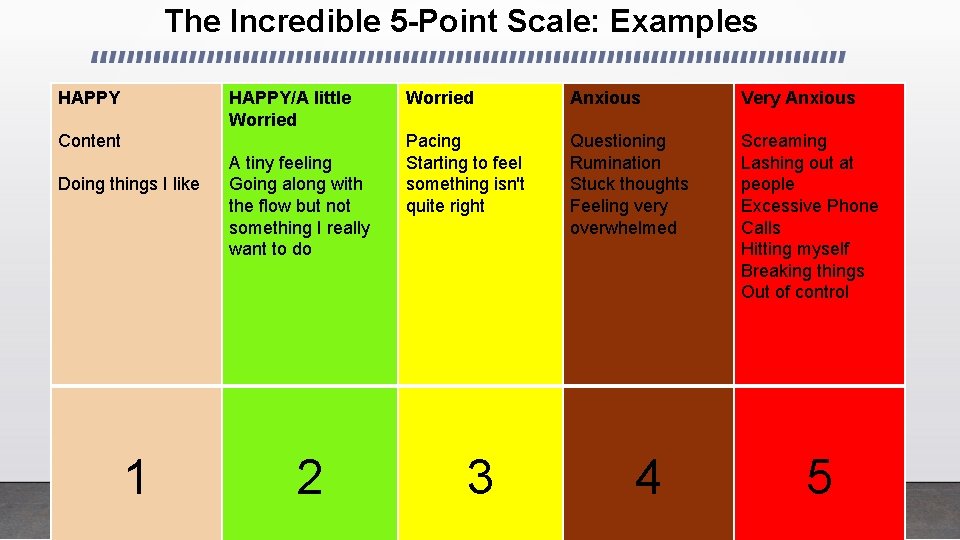
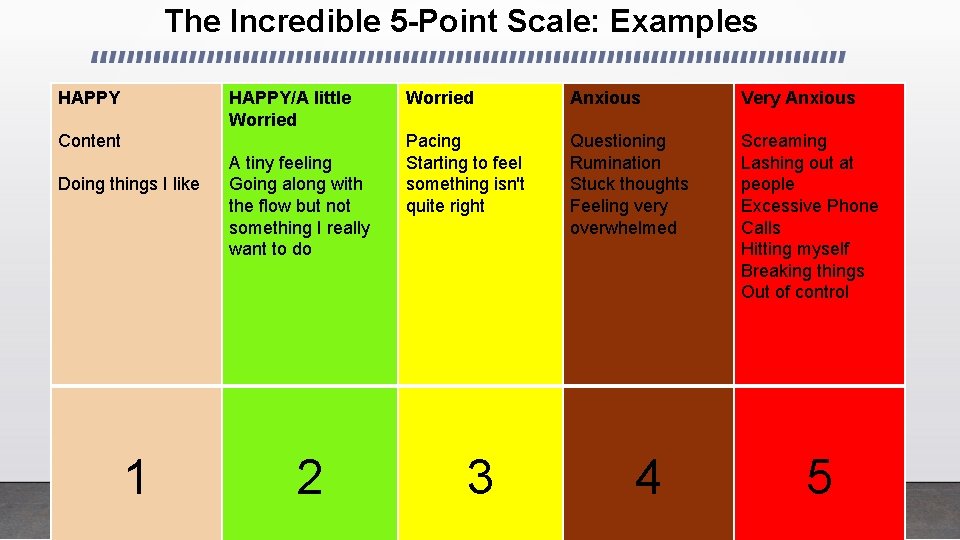
The Incredible 5 -Point Scale: Examples HAPPY/A little Worried Content Doing things I like 1 A tiny feeling Going along with the flow but not something I really want to do 2 Worried Anxious Very Anxious Pacing Starting to feel something isn't quite right Questioning Rumination Stuck thoughts Feeling very overwhelmed Screaming Lashing out at people Excessive Phone Calls Hitting myself Breaking things Out of control 3 4 5
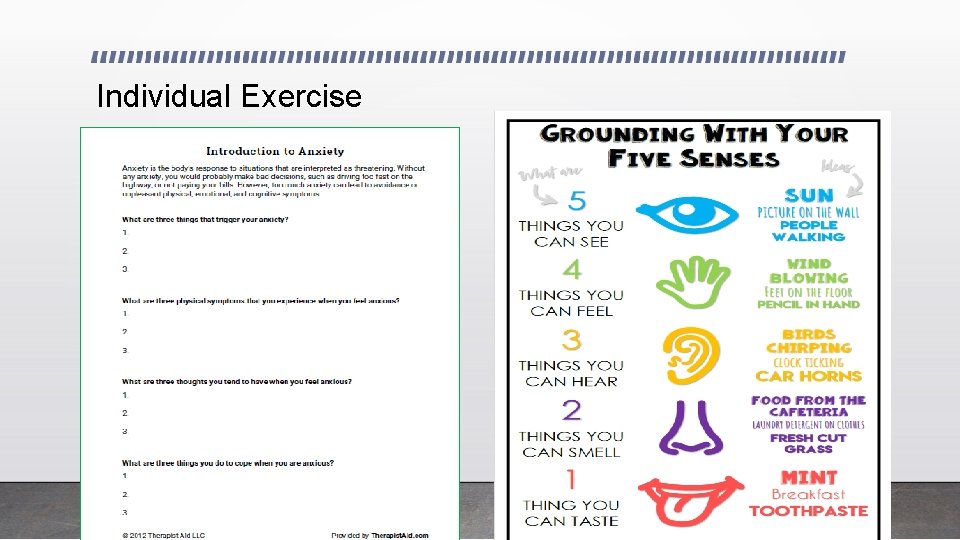
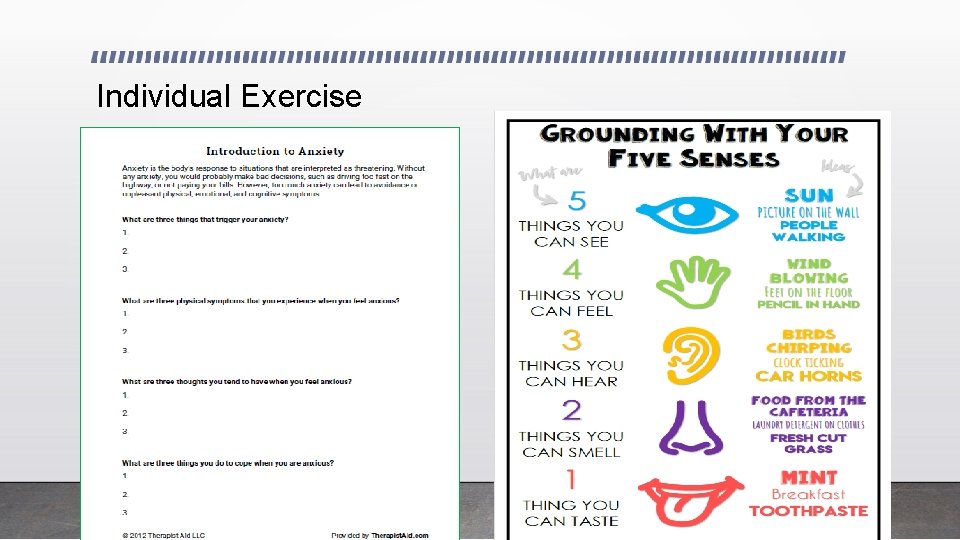
Individual Exercise
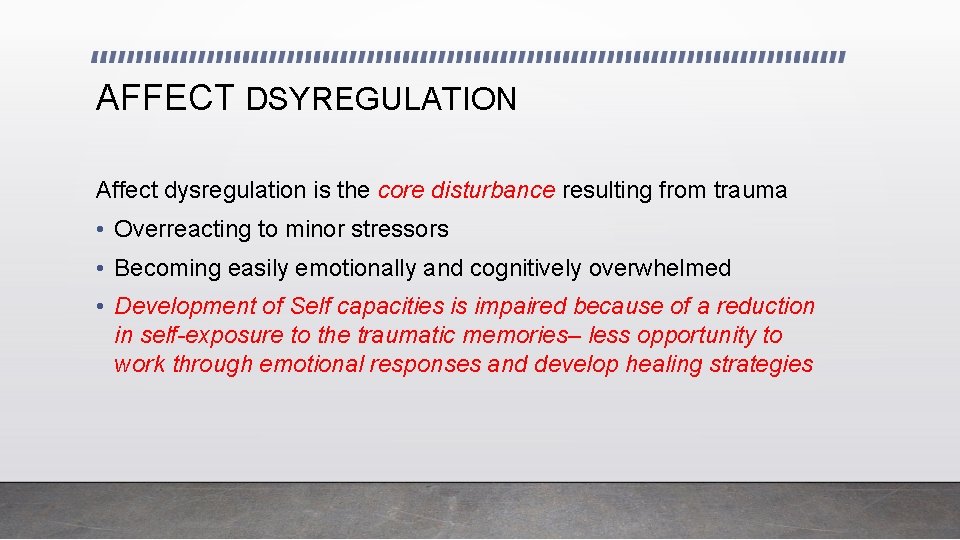
AFFECT DSYREGULATION Affect dysregulation is the core disturbance resulting from trauma • Overreacting to minor stressors • Becoming easily emotionally and cognitively overwhelmed • Development of Self capacities is impaired because of a reduction in self-exposure to the traumatic memories– less opportunity to work through emotional responses and develop healing strategies
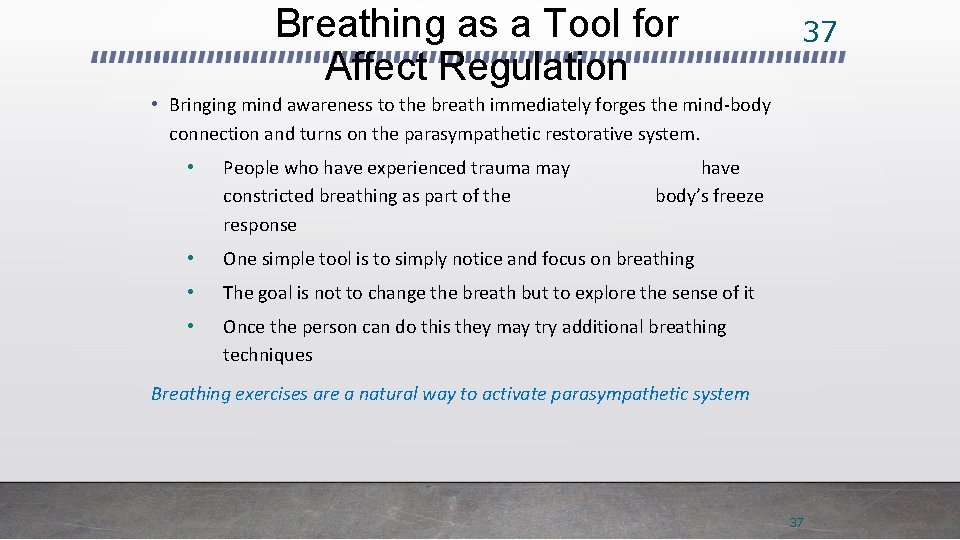
Breathing as a Tool for Affect Regulation 37 • Bringing mind awareness to the breath immediately forges the mind-body connection and turns on the parasympathetic restorative system. • People who have experienced trauma may constricted breathing as part of the response have body’s freeze • One simple tool is to simply notice and focus on breathing • The goal is not to change the breath but to explore the sense of it • Once the person can do this they may try additional breathing techniques Breathing exercises are a natural way to activate parasympathetic system 37
38 Imagery as a Tool for Affect Regulation • • • Have the person select an image that is associated with a safe place or that makes him/her feel calm. It can be real or imagined. Cue the person to think of this place and notice the feelings and sensations in their body. Stay in that safe place for a few minutes. Ask the person to think of a word that best fits the image of their safe place (relax, mountain, beach etc. ) Practice bringing up the word and image first during nonstressful times and then use during times of stress. Use visuals/cue cards to aid in the use of this tool. 38
Trigger Awareness and Intervention • anticipate that they will be triggered • recognize what their triggers are • develop strategies to ground themselves when they are triggered 39
40 Trigger Awareness and Intervention…cont’d • Identify triggers • Identify the person’s usual responses (e. g. freeze, dissociate, panic attack etc. ) • Figure out the “chain of events” • Validate and normalize • Plan intervention strategies ahead of time • Provide support in the moment to implement intervention strategies 40

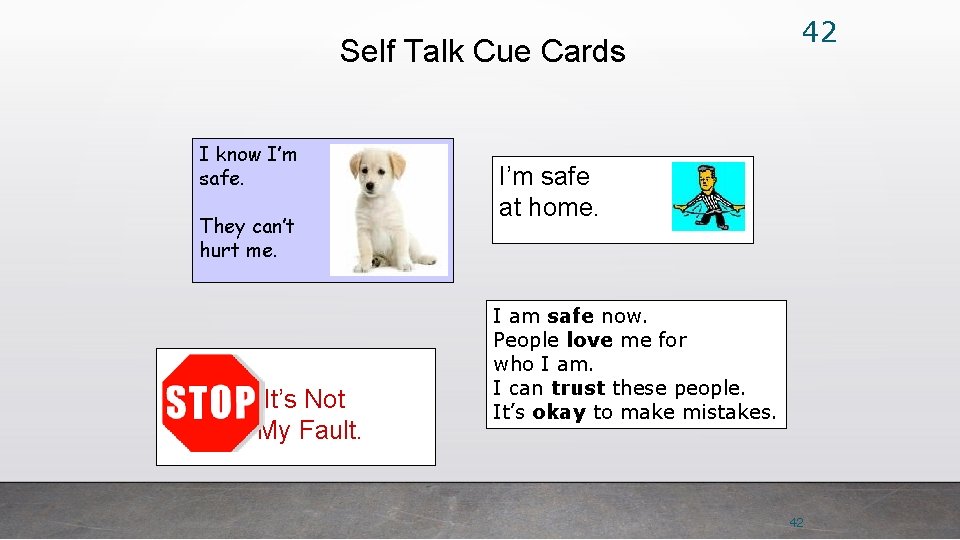
Interventions may include: • Positive self-talk • Moving away from the trigger (have an ‘escape strategy’ preplanned) • Breathing • Distraction • Grounding • Graduated exposure 41
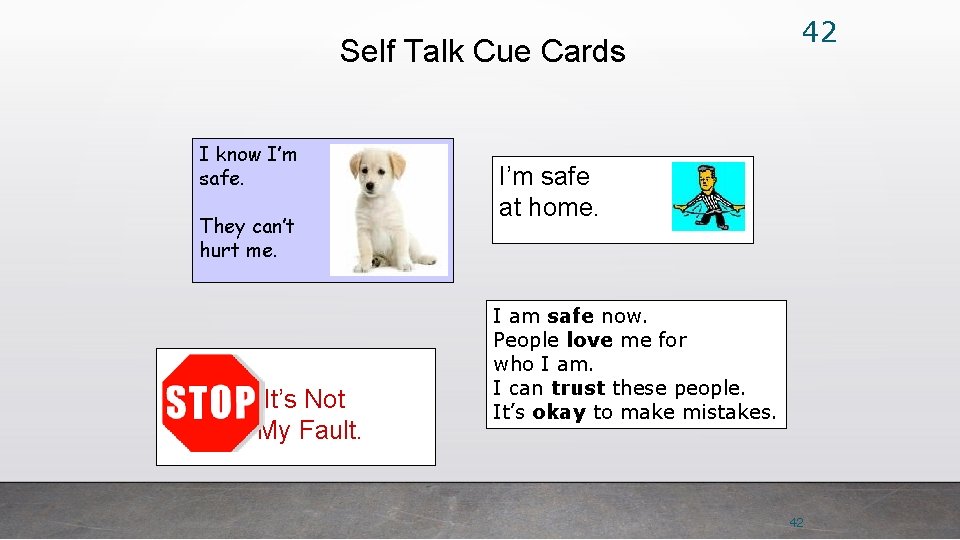
Self Talk Cue Cards I know I’m safe. They can’t hurt me. It’s Not My Fault. 42 I’m safe at home. I am safe now. People love me for who I am. I can trust these people. It’s okay to make mistakes. 42
Impact on Relationships Difficulty trusting others Trusting too easily Hypervigilance, hyper sensitivity to danger Inability to recognize abusive relationships Engage in relationships that continue to be abusive • Lack of a healthy template for interpersonal relationships • Relationships that create the “norm” of what the person is used to and continues to create external chaos and feeds into the maladaptive internalized beliefs that the person is inherently worthless • • • 43
Poor interpersonal relationships • Isolation • Re-victimization (“re-enactment”) • Victimizing others • Distrust • Deep fear of abandonment • A repeated search for a rescuer • Often don’t have appropriate peer groups • Often strained relationships in individuals with ID/DD

Poor interpersonal relationships • Trauma affects the way people approach potentially helpful relationships. • Not surprisingly, those individuals with histories of abuse are often reluctant to engage in, or quickly drop out of, many human services. • Being vigilant and suspicious are often important and thoroughly understandable self-protective mechanisms in coping with trauma exposure. • But these same ways of coping may make it more difficult for survivors to feel the safety and trust necessary to helpful relationships.
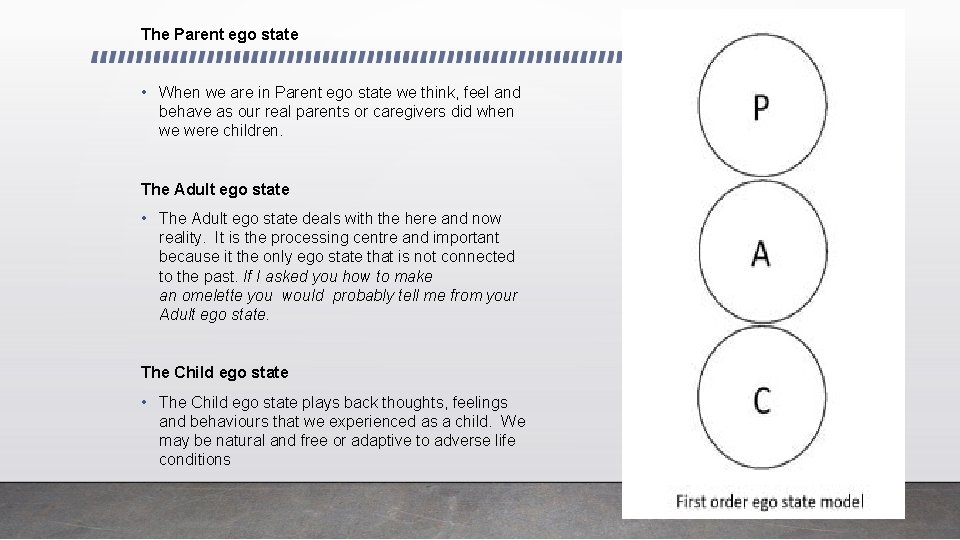
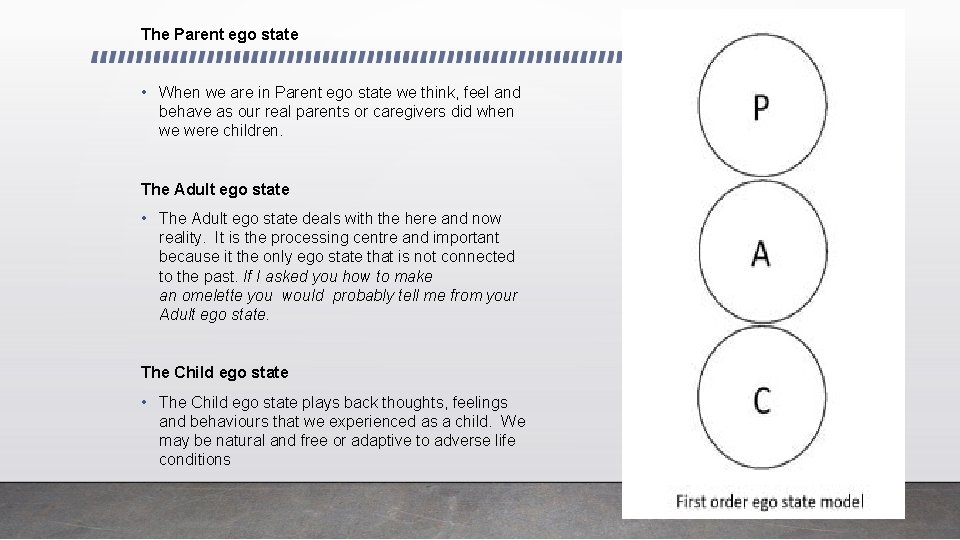
The Parent ego state • When we are in Parent ego state we think, feel and behave as our real parents or caregivers did when we were children. The Adult ego state • The Adult ego state deals with the here and now reality. It is the processing centre and important because it the only ego state that is not connected to the past. If I asked you how to make an omelette you would probably tell me from your Adult ego state. The Child ego state • The Child ego state plays back thoughts, feelings and behaviours that we experienced as a child. We may be natural and free or adaptive to adverse life conditions
How do you transact with clients? Look at the handout & Analysis different transactions and give examples of both positive and negative ones that may be experienced with a client
Positive Systems Approach is ………… "an amalgamation of systems theory, applied behaviour analysis, gentle teaching and other aspects of the major approaches that are currently in use" PSA
Values of Positive Behaviour Support • Respect for the rights of all citizens • The importance of the individual • Treating people with dignity • Individuals should be free from abuse and neglect
50 Workers Can Become Seen As A Primary Attachment & The Person Supported Needs To Feel Safe & Have Clear Boundaries
Evaluating Attitudes Necessary for PSA ASPECTS OF A HEALTHY RELATIONSHIP What are the aspects of a Healthy Relationship

If a healthy relationship exists, how does this impact on challenging behaviour?

Something to Think About… • The focus will be to teach, coach and model appropriate social behaviors rather then responding or identifying negative behaviors • Be inventive and use fun to reinforce good choices and behavior • Social stories are often a good way to teach appropriate behavior • Role playing situations is also a great way to model appropriate behavior
What is a supportive response? • We all know that to decrease anxiety people need boundaries and limits set. • Remember to set limits with people, not imposing limitations on people • People like to have clear expectations and structured, consistent routines • There needs to be a balance of activity and down time/ favored activity and required activity • Always remember when we respond to an anxious person we need to be “supportive”
Something to Think About… • Supportive responses take time to be effective • To be supportive needs your undivided and sincere attention • The person you are supporting needs to know that you are hearing them, listening and willing to help them through what they are feeling • Validate the person’s experience • Remain calm and do not take statements personally
56 Behaviour Through a Trauma Framework… • Symptoms are viewed as adaptations • Adaptations are attempts to solve a problem and to cope with an intolerable circumstance • There is a function and a purpose to adaptive responses • The most seemingly bizarre or strange presentations have meaning, given the right context or perspective they will make sense NORMAL reactions to ABNORMAL events 56
Collaborative Problem Solving • Work together to find solutions- don’t jump to solve the problem if you are both not sure what the problem really is • Invite solutions and ideas from the individual then contract around the solution • Make sure all of the person’s concerns are heard, clarified, understood, validated and addressed
Trauma response • Supporting the person is to make them feel safe, heard, and understood even when you may not fully understand what is making them feel unsafe • The individual may be looking to push buttons but may really just need us to be beside them and supportive CHANGE THE LENS FROM ATTENTION SEEKING TO ATTACHMENT SEEKING • Remember you are the professional and are likely not the true target to their outburst
Models to use with People with an ID • DBT has success • CBT • Expressive play and role plays • ACT • Mindfulness • The support staff can become your ally and support your work outside of sessions.
Skills System: Trauma-Informed Treatment for Individuals with ID • Emotion Regulation Skills • for Individuals with • Learning Challenges • Julie F. Brown, LICSW • (Doctoral Candidate) • juliebrown@theskillssystem. com
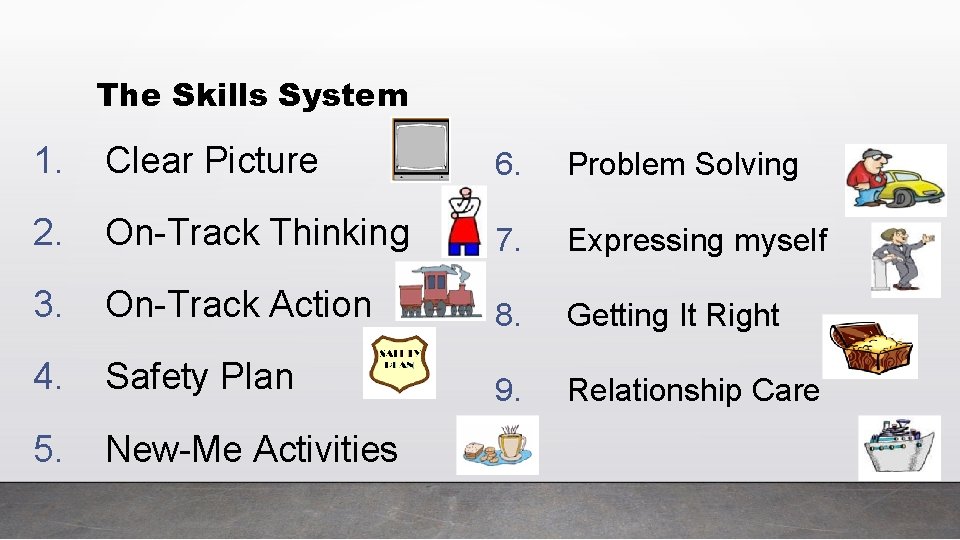
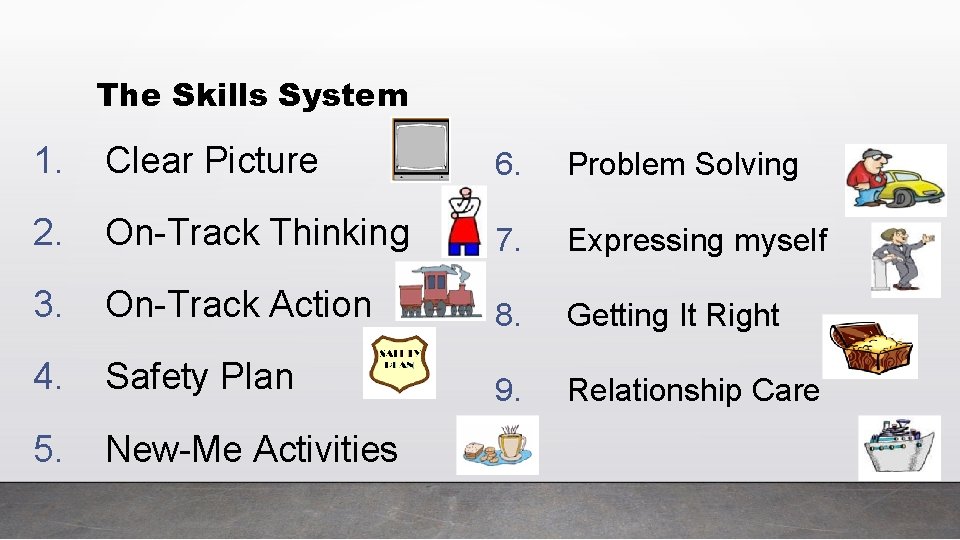
The Skills System 1. Clear Picture 6. Problem Solving 2. On-Track Thinking 7. Expressing myself 3. On-Track Action 8. Getting It Right 4. Safety Plan 9. Relationship Care 5. New-Me Activities
Contact information • Gail Clarke, RP, (Cert) OAMHP, CCTP • Regional Support Associates Clinical Manager • 519 -532 -1037 • gclarke@wgh. on. ca • GC Counselling Services • 226 -919 -5779 • gclarke 55@outlook. com