Trauma Documentation and Trauma Triage North Country EMS






- Slides: 82
Trauma Documentation and Trauma Triage North Country EMS Conference October 17, 2004
The planning of the TEMSIS Project and Trauma Documentation & Trauma Triage Educational Programs are funded in part by the United States Department of Health and Human Services, Health Resources and Services Administration – Trauma-EMS Grant Program. HRSA – H 81 MC 00025 -02 -04
Objectives At the conclusion of this course, the participant will be able to describe appropriate: ■ Trauma triage steps ■ Completion of the NH BEMS PCR ■ Trauma ■ General PCR communication / guidelines report format ■ SOAP format ■ Transport decision ■ 17 Key Data Fields making
Why is good documentation essential? ØIf it was not documented, it was not done! ØReflects adherance to the standard of care. Resource Guide & Power Point: Available for download at: http: //www. nh. gov/safety/ems/traumapresentations. html
Saf-C 5902. 07 Recordkeeping and Reporting “Recordkeeping and reporting shall be made by providing the information required by Saf-C 5902. 08 and Saf-C 5902. 09, as applicable…” using paper or electronic methods Saf-C 5902. 08 PCR Form – Left Side Describes how to complete items on the left side of the PCR. Saf-C 5902. 09 PCR Form – Right Side Describes how to complete items on the right side of the PCR.
Trauma System Goal To get the right patient to the right hospital at the right time.
Trauma Statistics – NH ■ Leading cause of death in people age 1 -34 ■ #1: MVCs ■ #2: Firearms ■ #3: Falls ■ 5 th leading cause of death overall ■ 1/3 intentional ■ 2/3 unintentional ■ Someone in NH dies of trauma every 20 hours
When Do Trauma Patients Die? Severe Head or CV Injury % of Deaths Major Torso or Head Injury Infection and MSOF
Organized Trauma Systems Death & Disability Through: ■ Injury Prevention ■ System Planning ■ Evaluation & Monitoring ■ Communication / Collaboration / Teamwork
NH Trauma System Development ■ 1980 s: Exclusive Regional Trauma System ■ Each of the 5 Regions was asked to make Trauma Center designations ■ Not successful ■ 1992 & 1994: Inclusive Statewide Trauma System Plan ■ Grants from HRSA
NH Trauma System Development ■ 1995: Statewide Trauma Plan Finalized ■ Senate Bill 122 ■ Trauma Coordinator position created ■ Trauma Medical Review Committee named as the Oversight Committee ■ Bureau of EMS named as the Lead Agency
NH Trauma System Development ■ 1999: “Trauma Triage, Communications, and Transport Decision Making Educational Program” offered ■ 2002: TEMSIS Grant – year 1 ■ 2004: “Trauma Documentation and Trauma Triage” Resource Guide & Train-the-Trainer Program
NH Trauma System Components ■ Prevention & Public Education ■ Hospitals & EMS Providers ■ Medical Direction: On-line & Standing Orders ■ Triage & Transport Guidelines ■ Rehabilitation ■ Evaluation
“Need to Know” Information ■ Hospital Assessment ■ Trauma Triage Guidelines ■ Communication Guidelines ■ Transport Guidelines ■ Resources available to you
Hospital Assessment ■ Performance Levels ■ Initial, Advanced, or Leadership ■ Roles ■ Area or Regional ■ Capability Levels ■ Adult & Pediatric; Level I, II, or III
Hospital Assessment: Process ■ Hospital Staff Self-Assessment ■ Site Visit by Members of TMRC ■ Confirmation ■ Consultative / Assistance
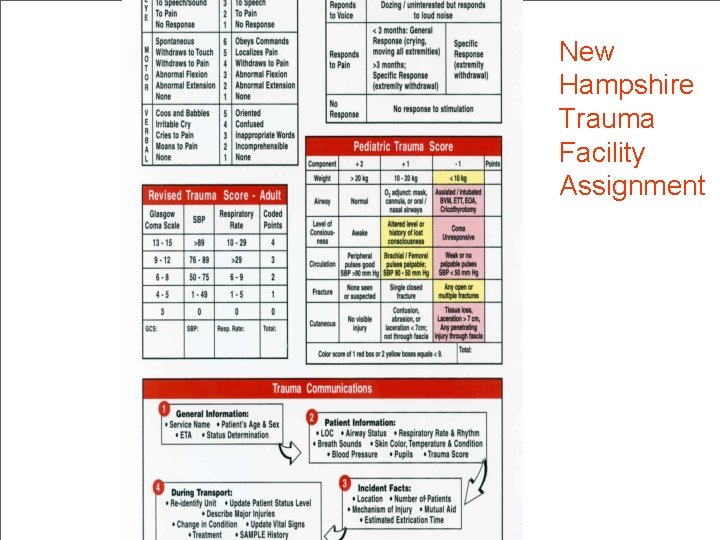
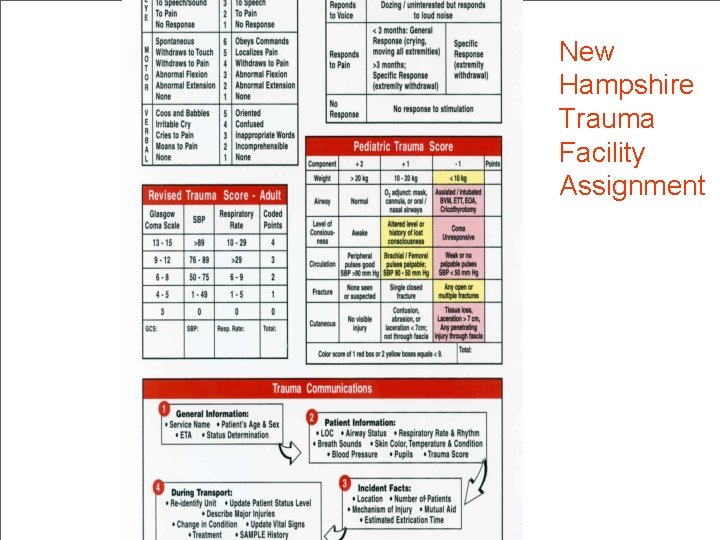
New Hampshire Trauma Facility Assignment
What is Trauma Triage? Patient Needs MATCH Hospital Resources Trauma patients are assessed and transported to the most appropriate hospital for that patient’s injuries.
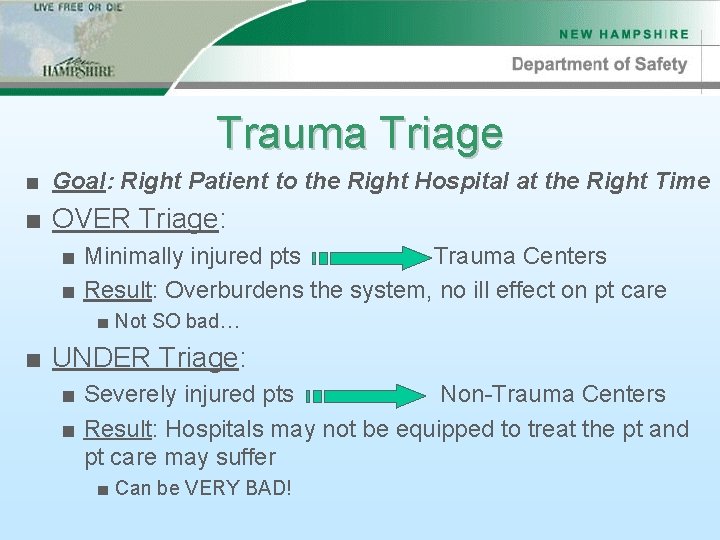
Trauma Triage ■ Goal: Right Patient to the Right Hospital at the Right Time ■ OVER Triage: ■ Minimally injured pts Trauma Centers ■ Result: Overburdens the system, no ill effect on pt care ■ Not SO bad… ■ UNDER Triage: ■ Severely injured pts Non-Trauma Centers ■ Result: Hospitals may not be equipped to treat the pt and pt care may suffer ■ Can be VERY BAD!
Steps to Trauma Triage Accuracy ■ Know the “Trauma Triage and Transport Pathways” Card ■ Available through NH Department of Safety & EMS-C program ■ Be familiar with severity indicators (GCS & RTS) ■ Listen to your “gut” (“sick v. not sick”) ■ Know your local resources ■ On Scene: Mutual Aid, ALS Intercept, Air Transport ■ Hospital: Local Hospital capabilities, distance to Regional Trauma Center
Front of Card Severity Indicators are based on: • Physiology • Anatomy • MOI & Comorbid Factors

Back of Card • Scales & Scores • Trauma Communication


Trauma Triage Steps: To Recap ■ Use Pathway Card to determine Pt Status ■ Trauma Triage Communication ■ Contact Medical Control ■ Relay enough info to aid in decision making ■ Transport Decision → Transport

Scenario 1
Scene Info u. Motorcycle v. Pickup Truck u. Truck traveling 40 mph, ? Cycle speed u 30 y/o male thrown 20 feet u. Truck has damage u. Rider’s helmet has few, minor scratches What does this information provide us? What additional information do you need?
Initial Assessment u Airway is open and clear u Opens eyes to loud verbal stimuli u Localizes painful stimuli u Confused verbal response to questions u RR=32, ≠ chest expansion, R. wall bruising u Strong radial pulses, no major bleeding u Skin pale, moist, cool Can you estimate GCS & RTS? What is the Patient Status?
Focused H&P u No obvious head injury, PERRLA u No JVD or tracheal tugging, C-spine non-tender u ≠ Chest expansion, crepitus, lung sounds R. u Abdomen soft, but guarding; pelvis stable u Open L. femur fracture u Abrasions and small laceration on R. arm u Pulse = 100, BP 110/68, RR = 32 u Medic alert tag for Coumadin use Confirm or dispute your initial severity determination.
Trauma Communications What pertinent information will you communicate to medical control? “MIVT”
Transport Decision u. Injury Severity u. Hospital capability, location, driving time u. Area Level III Trauma Hospital is 10 minutes u. Regional Level II Hospital is 20 minutes u. ALS intercept is unavailable u. Helicopter is available and ETA to scene is 20 minutes What decision will Medical Control make? Why?
Questions? Additional scenarios are available to download on the NH BEMS website.

General PCR Guidelines ■ Complete a PCR for every call and every pt ■ This includes when care or transport was: ■ Requested ■ Rendered ■ Refused ■ Cancelled This includes pts treated by one agency and transported by another. >1 PCR may be generated for the same pt/pt encounter.
General PCR Guidelines ■ A written PCR is: ■ ■ Complete Accurate Legible Professional ■ Be: ■ ■ Objective Brief Accurate Clear Legible Handwriting & Correct Grammar and Spelling are a must! “Poor documentation = Poor care”
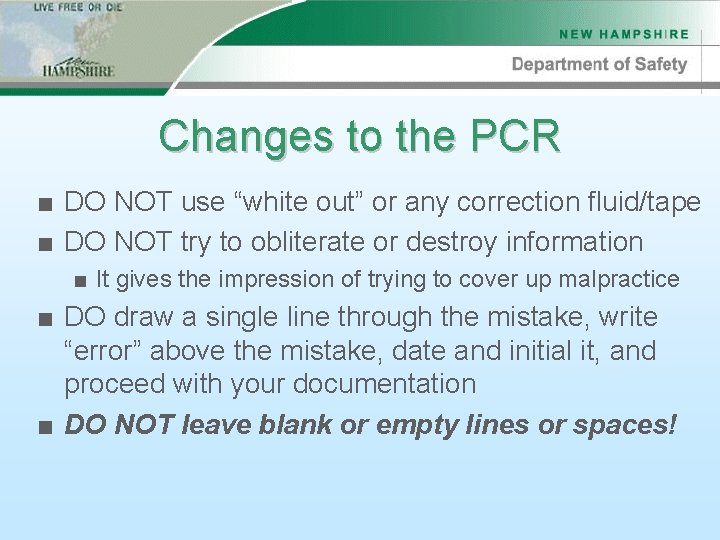
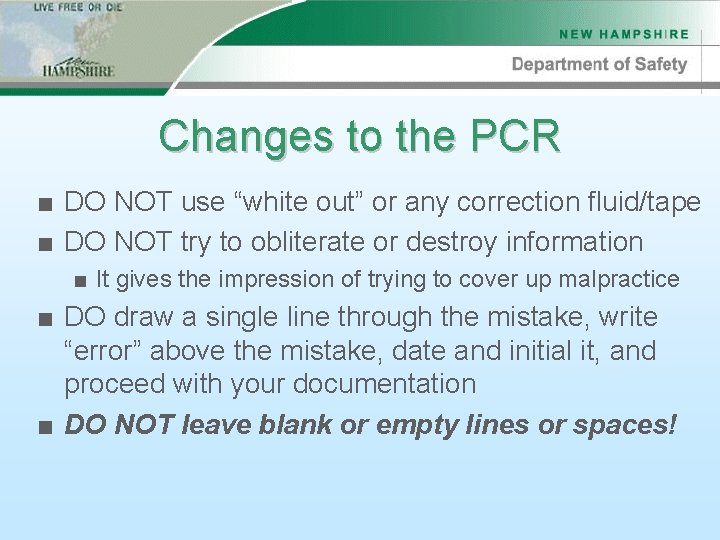
Changes to the PCR ■ DO NOT use “white out” or any correction fluid/tape ■ DO NOT try to obliterate or destroy information ■ It gives the impression of trying to cover up malpractice ■ DO draw a single line through the mistake, write “error” above the mistake, date and initial it, and proceed with your documentation ■ DO NOT leave blank or empty lines or spaces!
Addendums to the PCR ■ If applicable, a separate, carbonless lined sheet, attached as an “Addendum” may be included with the PCR. ■ The addendum shall be numbered by the provider to correspond with the preprinted serial number on the PCR shall be submitted. ■ The addendum shall be a two-copy form and shall be routed in the following manner: ■ Top (original) copy shall be retained by the EMS agency ■ Second copy shall be retained by the receiving hospital/facility
Addendums to the PCR ■ The addendum shall also contain: ■ The date of the call ■ The provider license number(s) ■ The signature of the reporting provider(s) ■ A sequential number for each page, as well as the total number of pages (e. g. “page 3 of 4”) ■ The addendum shall be used to record details from the narrative section of the PCR form in the event that the form does not provide sufficient space
What to Write in a PCR ■ Who started care before you arrived ■ How you found the patient ■ Anything you found during your assessment ■ Pertinent (+) and (-) findings ■ ■ Anything you did for the patient & their response Where you left the patient (& with whom) Report given (to whom) & questions answered Condition of the patient upon termination of care ■ PIVs patent? MAE=x 4? ETT position verified? If you did it, you should write it (& vice versa)
“Within Normal Limits” Or “We Never Looked” ? ? ? ?
What NOT to Write in a PCR ■ Any foul or objectionable language ■ Anything that could be considered as libel ■ Example: “He was drunk. ” ■ It is far better to write objective comments, such as: ■ “Patient had odor of intoxicating substance on breath. ” ■ “Patient admits to drinking two beers. ” ■ “Patient unable to stand on his own without staggering and visual hallucinations. ” ■ Do not write on anything you have lying on top of a PCR because it will copy through onto the PCR, obscuring your report
Refusal Documentation ■ Patients ABLE to refuse care include: ■ Competent individuals – defined as the ability to understand the nature and consequences of their actions AND ■ Adult – defined as 18 years of age or older, except: ■ An emancipated minor ■ A married minor ■ A minor in the military
Refusal Documentation ■ Patients NOT ABLE to refuse care include: ■ Patients in whom the severity of their condition prevents them from making an informed, rational decision regarding their medical care. ■ ■ ■ Altered level on consciousness (head injury, Et. OH, hypoxia) Suicide (attempts or verbalizes) Severely altered vital signs Mental retardation and/or deficiency Any patient who makes clearly irrational decisions in the presence of an obvious potentially life or limb threatening injury, including persons who are emotionally unstable ■ Any patient who is deemed a danger to self or others (under protective custody) ■ Not acting as a “reasonable and prudent” person would, given the same circumstances ■ Under age 18 (except as denoted above)
Refusal Procedure ■ Perform a complete exam with vitals ■ If refused, document this ■ Determine if the patient is competent to refuse ■ Ensure the pt or responsible party: ■ Has been told of his/her condition ■ Understands the risks or refusal ■ Assumes all risk & releases EMS from liability ■ Understands he/she can call you back anytime
Narrative Charting
Subjective ■ Any information you are able to elicit while taking the patient’s history: ■ Chief Complaint (CC) ■ History of Present Illness (HPI) ■ “OPQRST – AS/PN” ■ Past Medical & Surgical History ■ Meds and Allergies
Objective ■ General Impression ■ Primary Assessment ■ ABCDE ■ Secondary Assessment ■ Head to Toe Exam
Assessment ■ Field Diagnosis ■ What you believe the problem to be ■ Working diagnosis ■ Example: “Chest pain, R/O MI”; “closed head injury with altered LOC”; “pelvic fracture”
Plan / Management ■ Treatment ■ Patient Response ■ Example: ■ “Patient placed on O 2 at 4 lpm by NC and placed on the cardiac monitor. Medical control contacted, and the following orders received from Dr. Smith: Nitroglycerine sublingual x 3, 5 minutes apart for continued chest pain and BP >90/60. If no relief from nitroglycerine, administer morphine 2 mg SIVP, titrated to a maximum of 10 mg for continued chest pain and BP >90/60. ”
Narrative Charting
CHART ■ Chief Complaint ■ History ■ Assessment ■ Rx ■ Transport
Demographics 3 Key Trauma Fields
EMS Response Times Key Trauma Field
Vital Signs 4 Key Trauma Fields: Pulse, SBP, DBP, RR
Lung Sounds, Pupils, Skin, Temp Key Trauma Field
4 Key Trauma Fields: GCS & RTS 4 Key Trauma Fields: GCS Eye RTS GCS Verbal RTS BP GCS Motor RTS RR GCS Total RTS Total
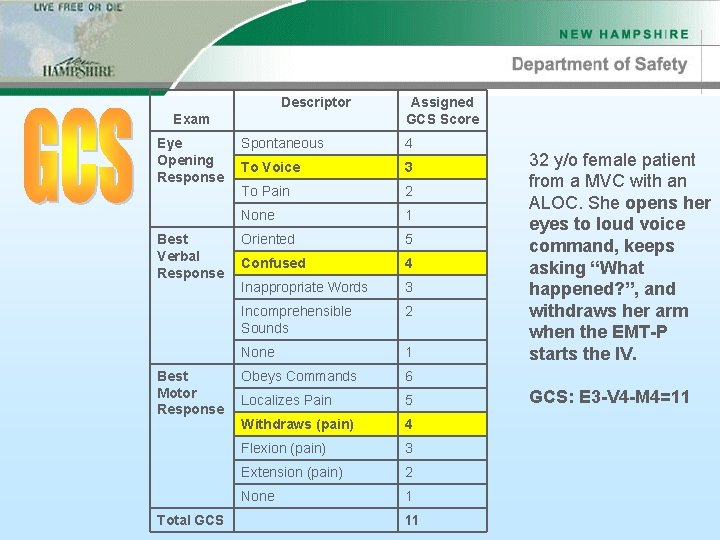
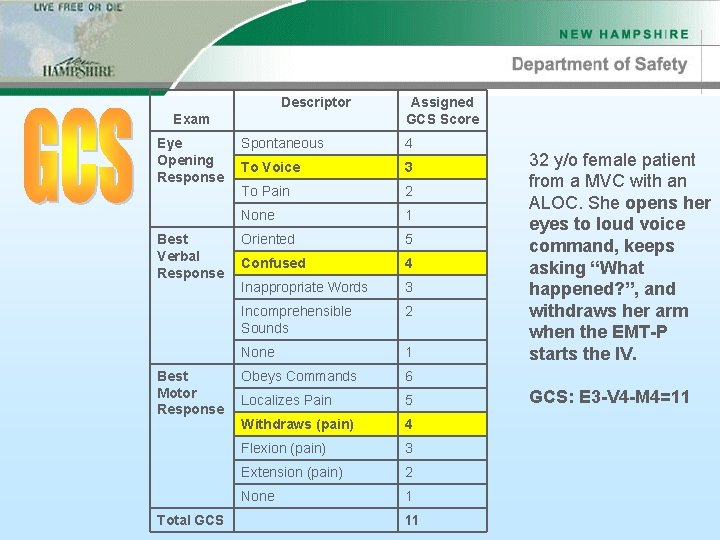
Descriptor Exam Eye Opening Response Best Verbal Response Best Motor Response Total GCS Assigned GCS Score Spontaneous 4 To Voice 3 To Pain 2 None 1 Oriented 5 Confused 4 Inappropriate Words 3 Incomprehensible Sounds 2 None 1 Obeys Commands 6 Localizes Pain 5 Withdraws (pain) 4 Flexion (pain) 3 Extension (pain) 2 None 1 11 32 y/o female patient from a MVC with an ALOC. She opens her eyes to loud voice command, keeps asking “What happened? ”, and withdraws her arm when the EMT-P starts the IV. GCS: E 3 -V 4 -M 4=11

Parameter Glascow Coma Scale (GCS) Total points Systolic Blood Pressure (SBP) Respiratory Rate (RR) Value Assigned RTS Score 13 -15 4 9 -12 3 6 -8 2 4 -5 1 3 0 >89 mm Hg 4 76 -89 mm Hg 3 50 -75 mm Hg 2 1 -49 mm Hg 1 No Pulse 0 10 -29/min 4 >29/min 3 6 -9/min 2 1 -5/min 1 None 0 Total RTS: ____11_____ Example: The 32 y/o female patient from the MVC with: GCS of E 3 -V 4 -M 4=11 SBP of 92 RR of 12
Why do we collect data? ■ ■ Benefit patient care Provide feedback to the EMS agency/provider Evaluate system performance Determine if the patient treatment protocols are working for the patient population served ■ Design injury prevention programs ■ Perform quality assurance ■ Outline opportunities for improvement in data collection and the reporting system
Examples of Reports ■ Response time ■ Performance, such as ETI success rates ■ Procedures, such as number of IVs per provider per year ■ Number of CPR calls
Difficulties… “Garbage in…garbage out. ” Information collected must be complete and accurate or it will not be useful.
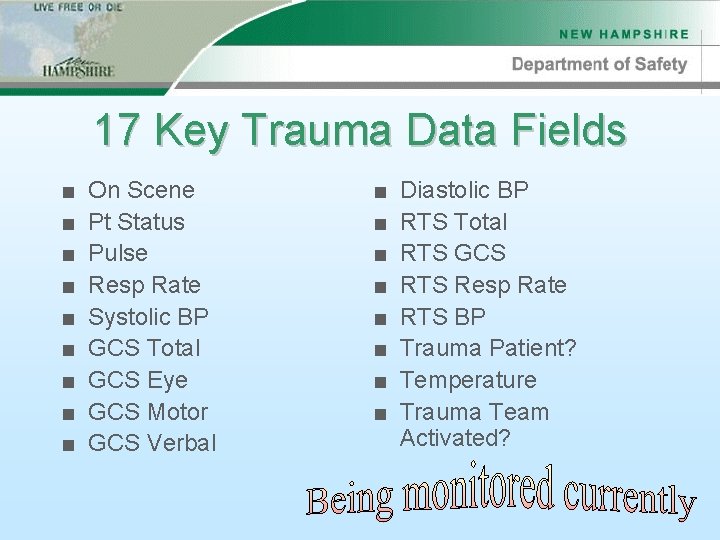
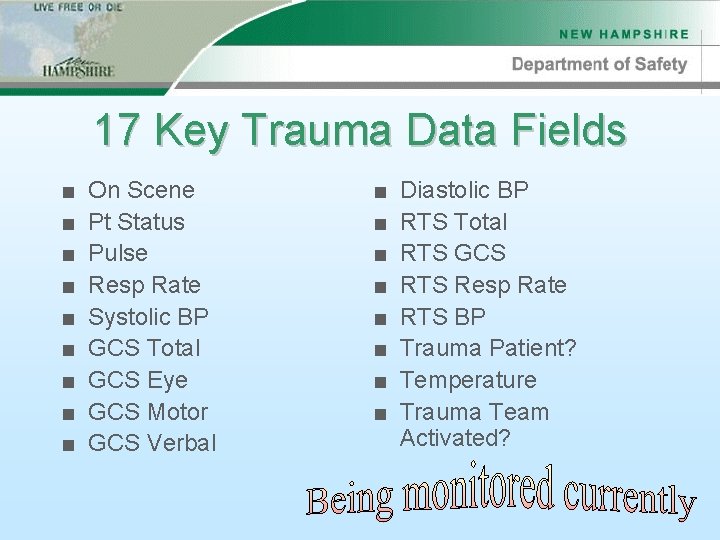
17 Key Trauma Data Fields ■ ■ ■ ■ ■ On Scene Pt Status Pulse Resp Rate Systolic BP GCS Total GCS Eye GCS Motor GCS Verbal ■ ■ ■ ■ Diastolic BP RTS Total RTS GCS RTS Resp Rate RTS BP Trauma Patient? Temperature Trauma Team Activated?
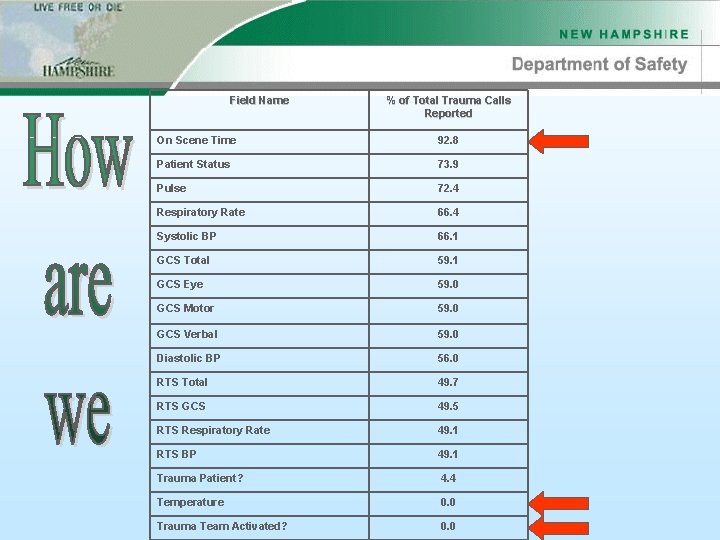
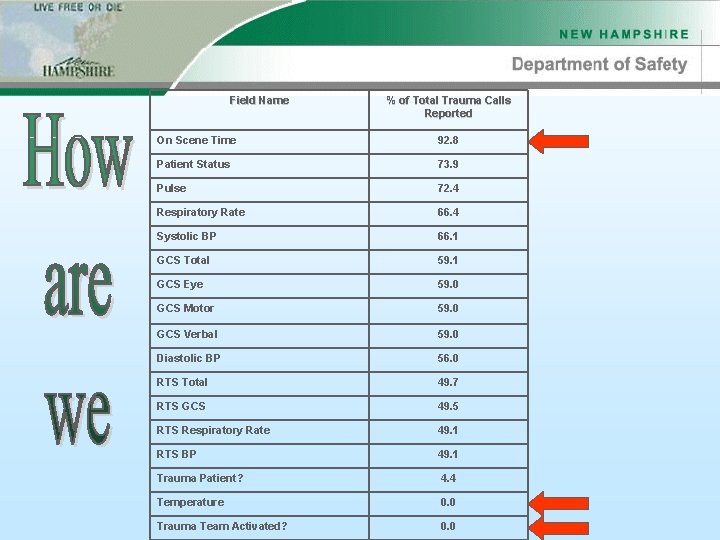
Field Name % of Total Trauma Calls Reported On Scene Time 92. 8 Patient Status 73. 9 Pulse 72. 4 Respiratory Rate 66. 4 Systolic BP 66. 1 GCS Total 59. 1 GCS Eye 59. 0 GCS Motor 59. 0 GCS Verbal 59. 0 Diastolic BP 56. 0 RTS Total 49. 7 RTS GCS 49. 5 RTS Respiratory Rate 49. 1 RTS BP 49. 1 Trauma Patient? 4. 4 Temperature 0. 0 Trauma Team Activated? 0. 0
Approved Abbreviations A complete list is available in the accompanying Resource Guide
Data Dictionary Clearly defines each data field and how to fill in the corresponding “box” on the PCR. Available through the State Office.
Summary Trauma Systems Save Lives! Trauma Triage is a crucial component of the NH Trauma System. The Bureau of EMS is committed to getting the Right Patient to the Right Facility in the Right Time.
Questions? Thank You.