Transplacental infections Dr Salwa Seif Eldin PNU College


- Slides: 33

Transplacental infections Dr. Salwa Seif Eldin PNU, College of Medicine ssseifeldin@pnu. edu. sa
OBJECTIVES; Identify types of infant infections. Identify major trans placental transmitted pathogens causing congenital infections (TORCH) syndrome. ( Toxoplasma, (Treponema pallidum , Hepatitis B, Parvovirus , Varicella Zoster Virus), Rubella virus , Cytomegalovirus, Herpes simplex. . Describe the major features & epidemiology, manifestations of congenital infection, diagnosis of congenital infection. Describe their management and prevention of each congenital infection.
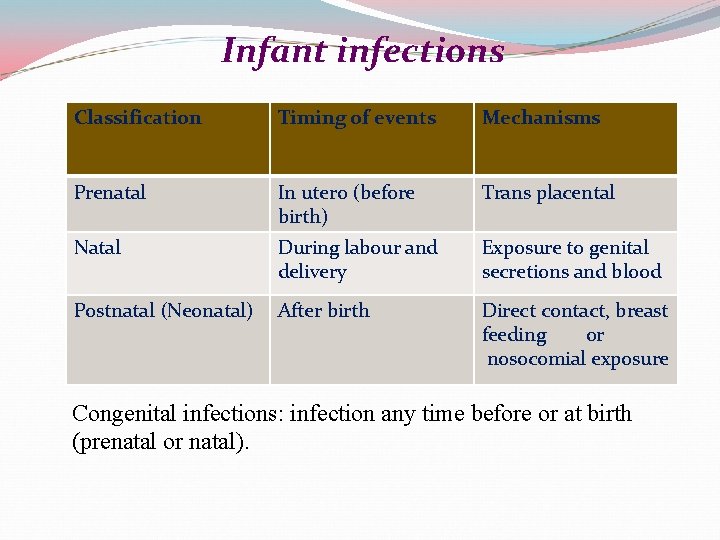
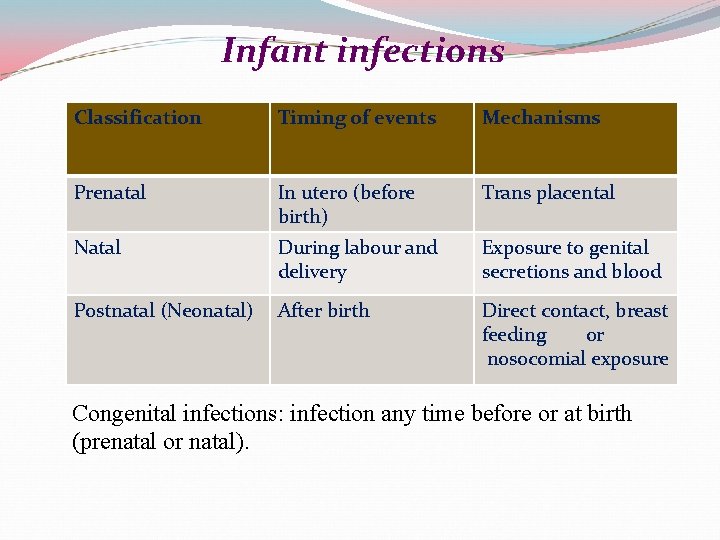
Infant infections Classification Timing of events Mechanisms Prenatal In utero (before birth) Trans placental Natal During labour and delivery Exposure to genital secretions and blood Postnatal (Neonatal) After birth Direct contact, breast feeding or nosocomial exposure Congenital infections: infection any time before or at birth (prenatal or natal).
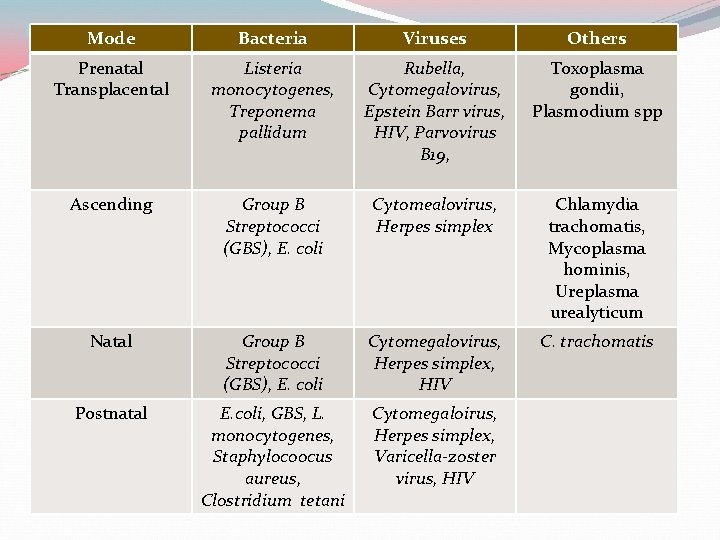
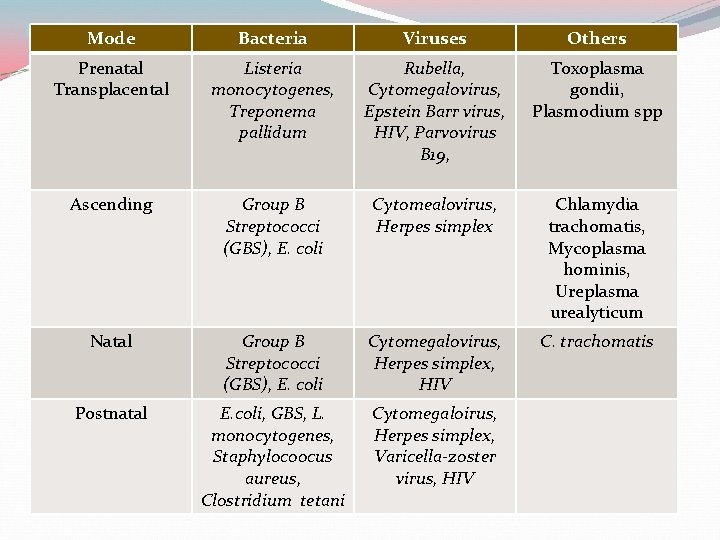
Modes. Mode of infection and major agents Bacteria Viruses Others Prenatal Transplacental Listeria monocytogenes, Treponema pallidum Rubella, Cytomegalovirus, Epstein Barr virus, HIV, Parvovirus B 19, Toxoplasma gondii, Plasmodium spp Ascending Group B Streptococci (GBS), E. coli Cytomealovirus, Herpes simplex Chlamydia trachomatis, Mycoplasma hominis, Ureplasma urealyticum Natal Group B Streptococci (GBS), E. coli Cytomegalovirus, Herpes simplex, HIV C. trachomatis Postnatal E. coli, GBS, L. monocytogenes, Staphylocoocus aureus, Clostridium tetani Cytomegaloirus, Herpes simplex, Varicella-zoster virus, HIV
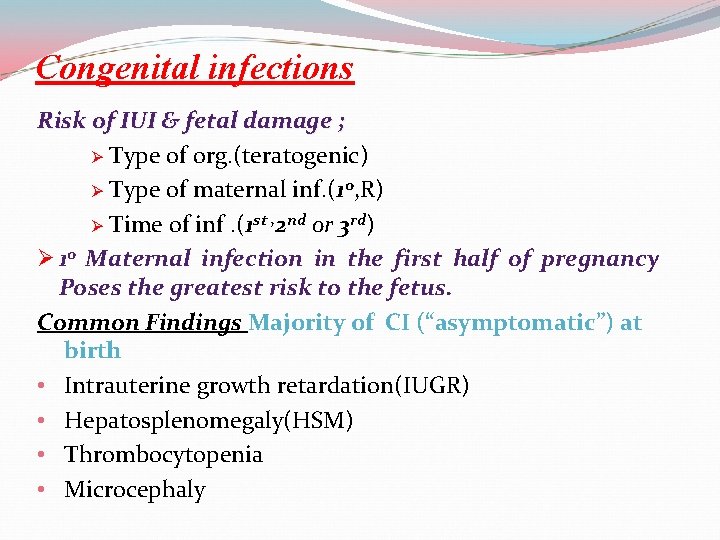
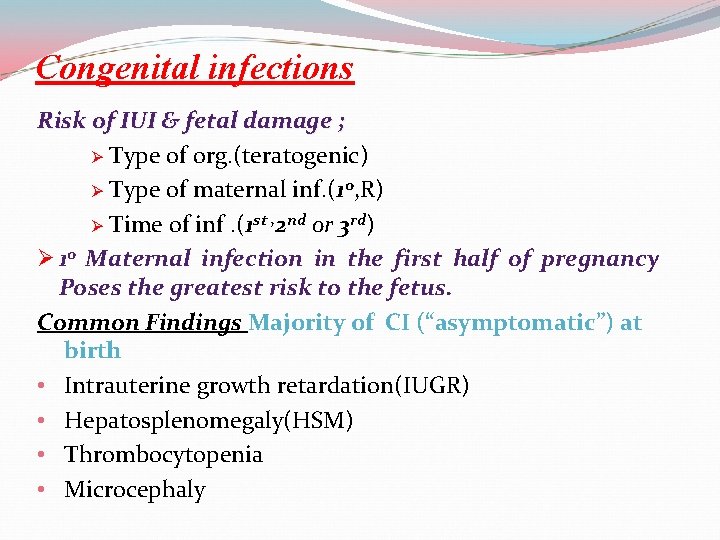
Congenital infections Risk of IUI & fetal damage ; Ø Type of org. (teratogenic) Ø Type of maternal inf. (1 o, R) Ø Time of inf. (1 st , 2 nd or 3 rd) Ø 1 o Maternal infection in the first half of pregnancy Poses the greatest risk to the fetus. Common Findings Majority of CI (“asymptomatic”) at birth • Intrauterine growth retardation(IUGR) • Hepatosplenomegaly(HSM) • Thrombocytopenia • Microcephaly
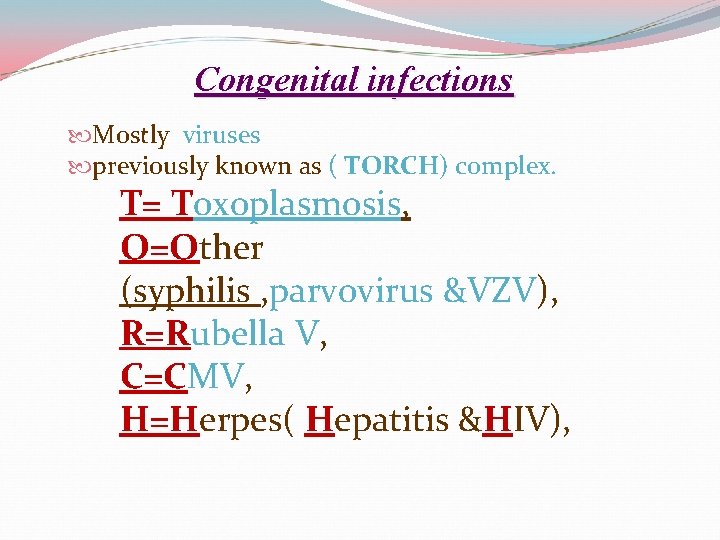
Congenital infections Mostly viruses previously known as ( TORCH) complex. T= Toxoplasmosis, O=Other (syphilis , parvovirus &VZV), R=Rubella V, C=CMV, H=Herpes( Hepatitis &HIV),
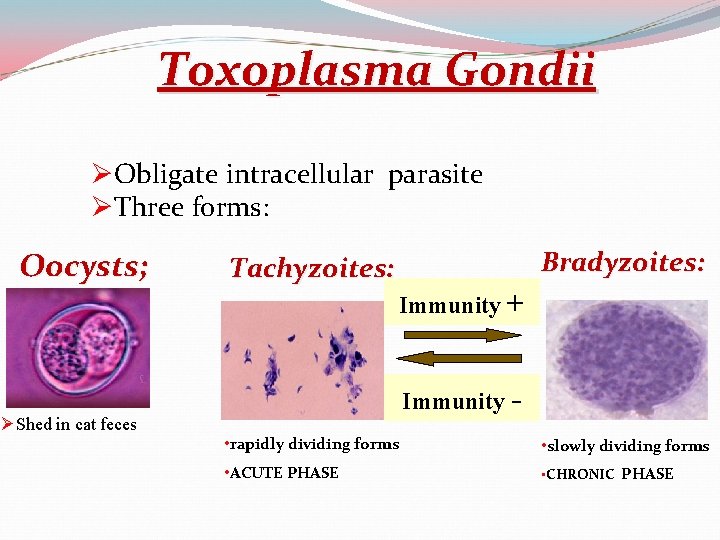
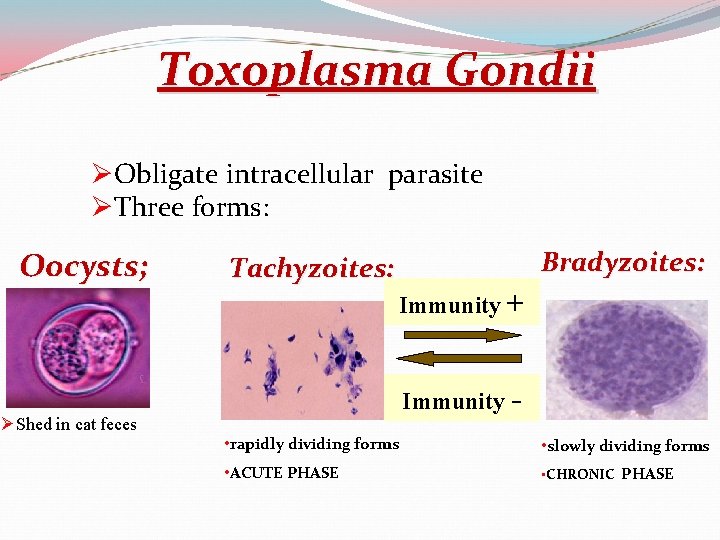
Toxoplasma Gondii ØObligate intracellular parasite ØThree forms: Oocysts; ØShed in cat feces Tachyzoites: Bradyzoites: Immunity + Immunity • rapidly dividing forms • slowly dividing forms • ACUTE PHASE • CHRONIC PHASE
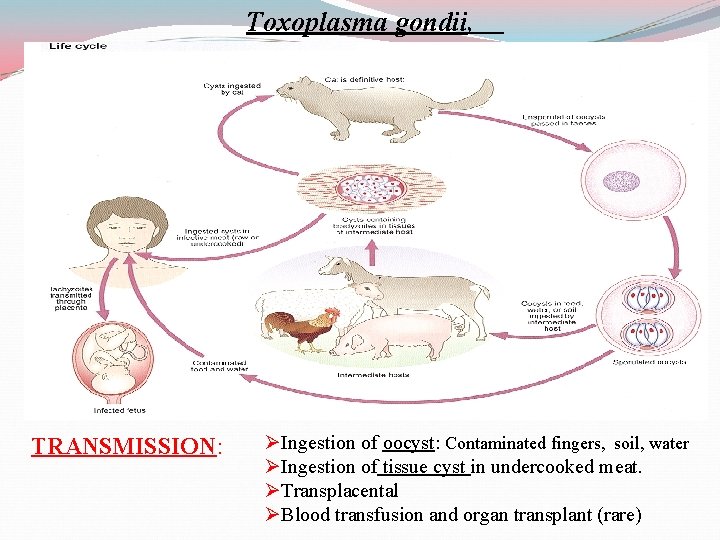
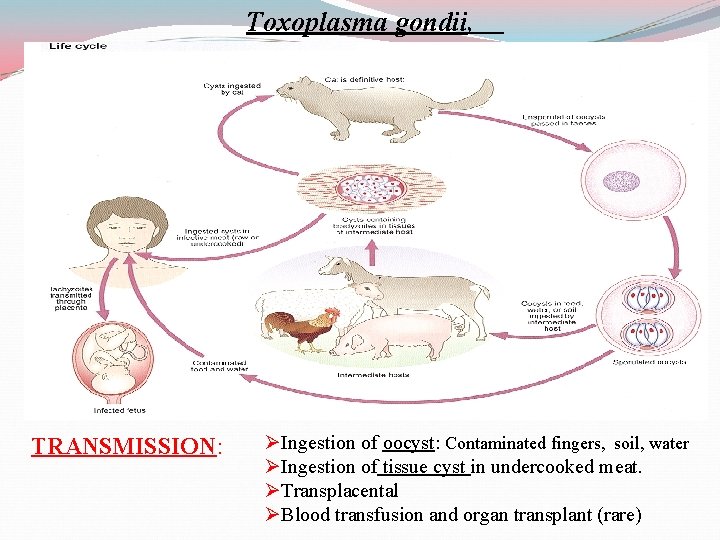
Toxoplasma gondii, TRANSMISSION: ØIngestion of oocyst: Contaminated fingers, soil, water ØIngestion of tissue cyst in undercooked meat. ØTransplacental ØBlood transfusion and organ transplant (rare)
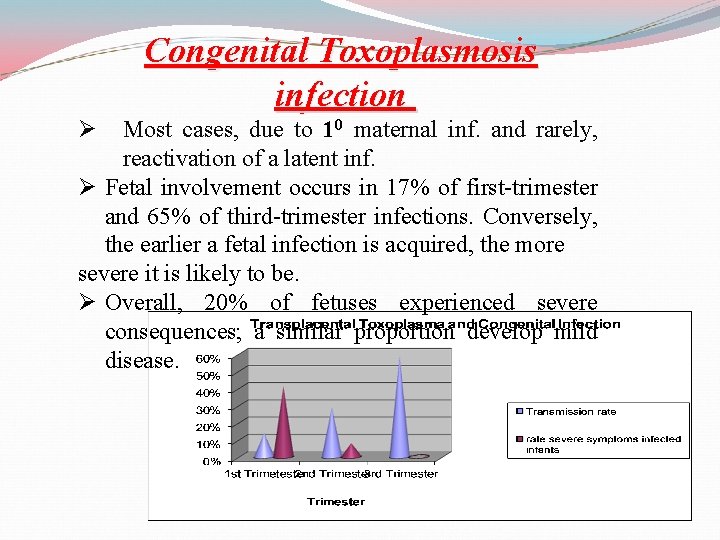
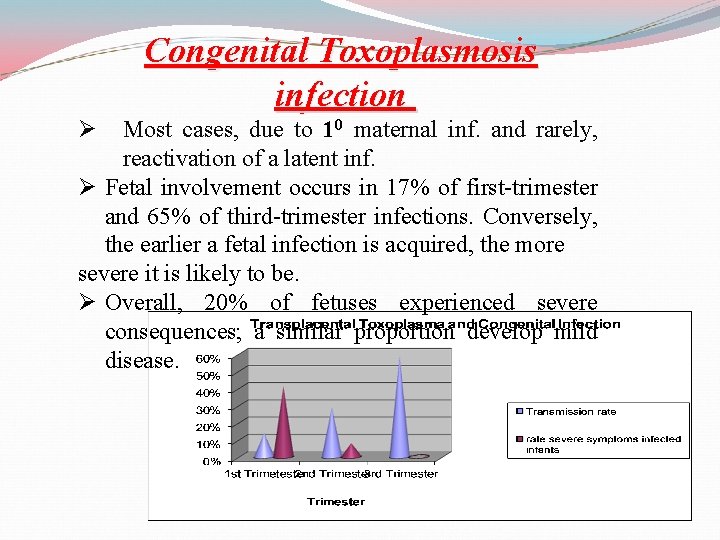
Congenital Toxoplasmosis infection Ø Most cases, due to 10 maternal inf. and rarely, reactivation of a latent inf. Ø Fetal involvement occurs in 17% of first-trimester and 65% of third-trimester infections. Conversely, the earlier a fetal infection is acquired, the more severe it is likely to be. Ø Overall, 20% of fetuses experienced severe consequences; a similar proportion develop mild disease.
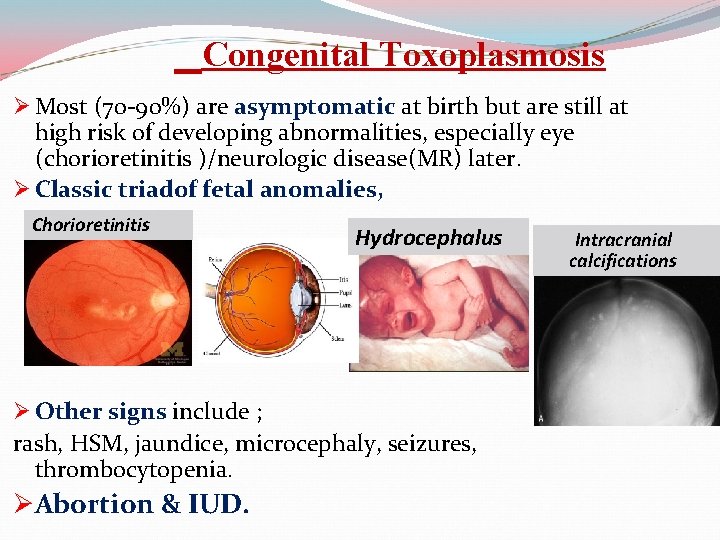
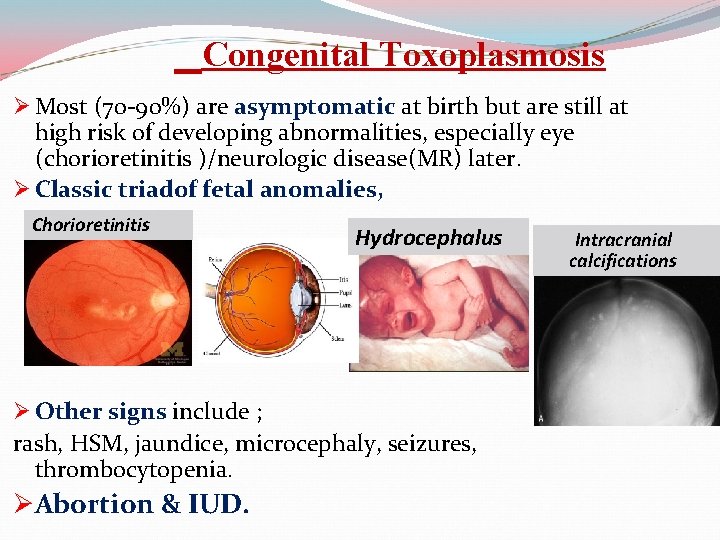
Congenital Toxoplasmosis Ø Most (70 -90%) are asymptomatic at birth but are still at high risk of developing abnormalities, especially eye (chorioretinitis )/neurologic disease(MR) later. Ø Classic triadof fetal anomalies, Chorioretinitis Hydrocephalus Ø Other signs include ; rash, HSM, jaundice, microcephaly, seizures, thrombocytopenia. ØAbortion & IUD. Intracranial calcifications
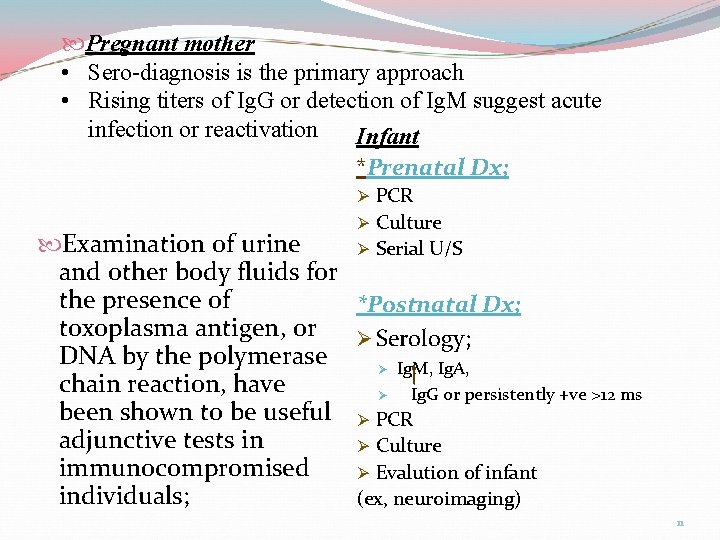
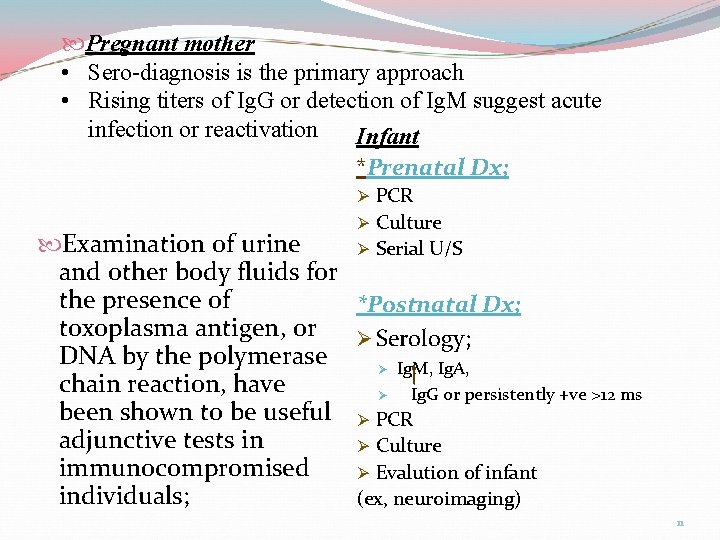
Pregnant mother • Sero-diagnosis is the primary approach • Rising titers of Ig. G or detection of Ig. M suggest acute infection or reactivation Infant *Prenatal Dx; Ø PCR Ø Culture Examination of urine Ø Serial U/S and other body fluids for the presence of *Postnatal Dx; toxoplasma antigen, or Ø Serology; DNA by the polymerase Ø Ig. M, Ig. A, chain reaction, have Ø Ig. G or persistently +ve >12 ms been shown to be useful Ø PCR adjunctive tests in Ø Culture immunocompromised Ø Evalution of infant individuals; (ex, neuroimaging) 11

Treatment Spiramycin. pyrimethamine& sulfadiazine. Prevention Avoid exposure to cat feces; Wash ; - hands with soap and water - fruits/vegetables, - surfaces that touched fruits/vegetables/raw meat. Cook all meats thoroughly
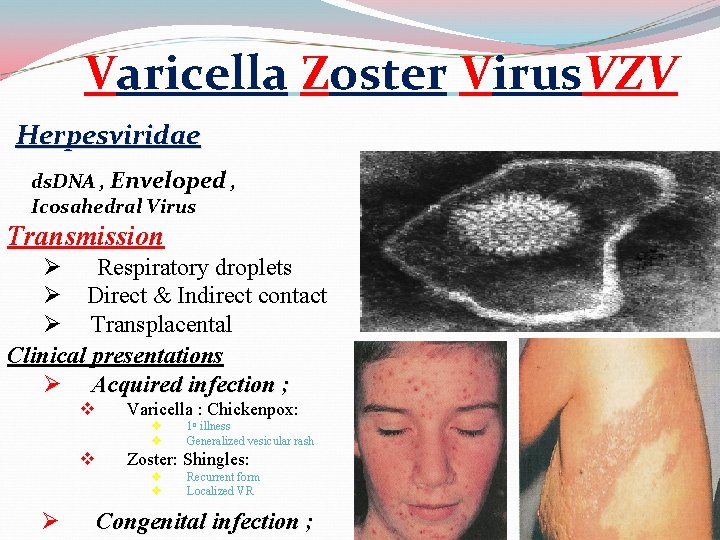
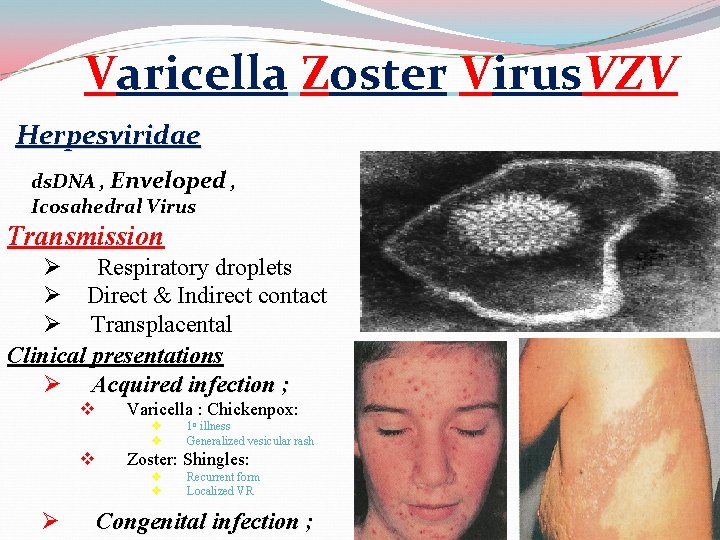
Varicella Zoster Virus. VZV Herpesviridae ds. DNA , Enveloped , Icosahedral Virus Transmission Ø Respiratory droplets Ø Direct & Indirect contact Ø Transplacental Clinical presentations Ø Acquired infection ; v Varicella : Chickenpox: v v v Zoster: Shingles: v v Ø 1 o illness Generalized vesicular rash Recurrent form Localized VR Congenital infection ;
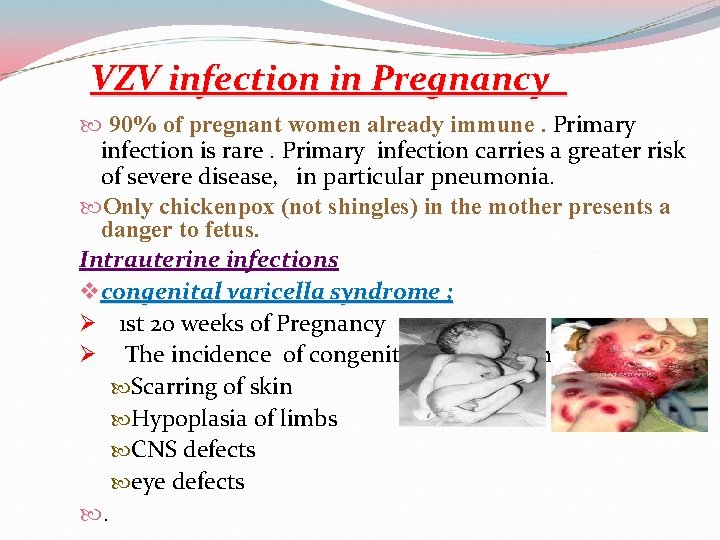
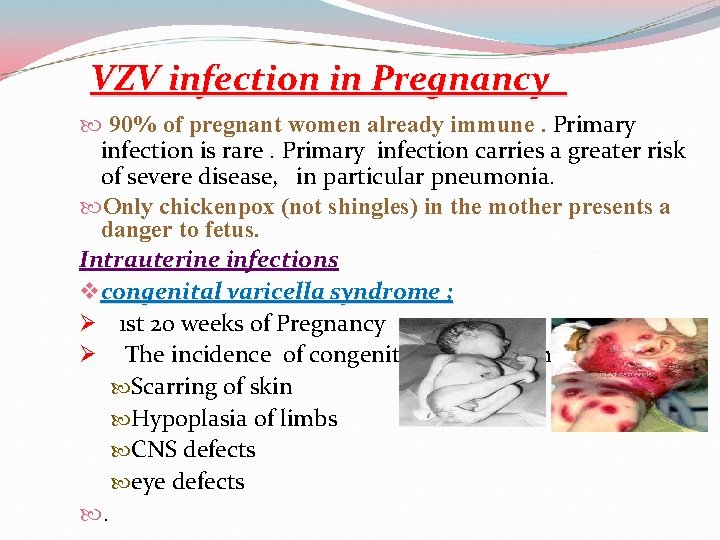
VZV infection in Pregnancy 90% of pregnant women already immune. Primary infection is rare. Primary infection carries a greater risk of severe disease, in particular pneumonia. Only chickenpox (not shingles) in the mother presents a danger to fetus. Intrauterine infections v congenital varicella syndrome ; Ø 1 st 20 weeks of Pregnancy Ø The incidence of congenital varicella syndrome is ~ 2% Scarring of skin Hypoplasia of limbs CNS defects eye defects .
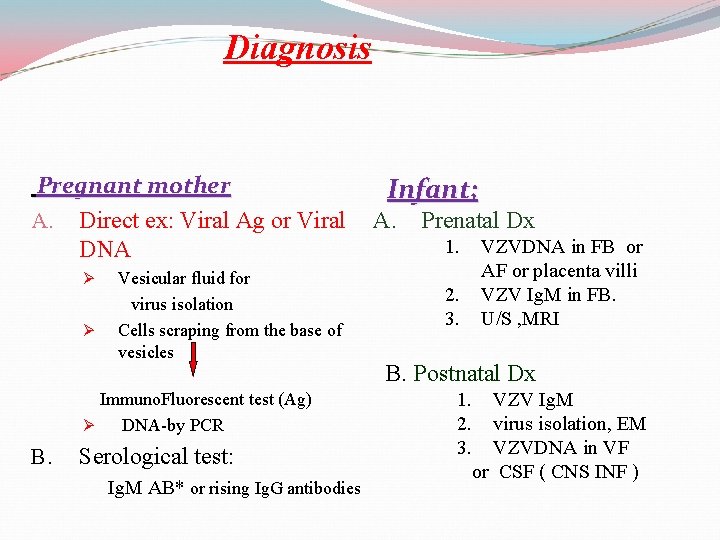
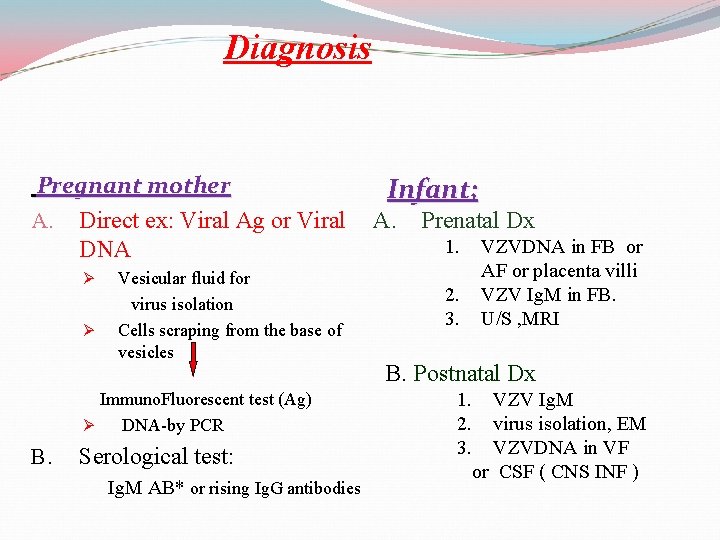
Diagnosis Pregnant mother A. Direct ex: Viral Ag or Viral DNA Ø Ø Vesicular fluid for virus isolation Cells scraping from the base of vesicles Immuno. Fluorescent test (Ag) Ø DNA-by PCR B. Serological test: Ig. M AB* or rising Ig. G antibodies Infant; A. Prenatal Dx 1. 2. 3. VZVDNA in FB or AF or placenta villi VZV Ig. M in FB. U/S , MRI B. Postnatal Dx 1. VZV Ig. M 2. virus isolation, EM 3. VZVDNA in VF or CSF ( CNS INF )
Rx Acyclovir, vidarabine Prevention; Pre exposure; live-attenuated vaccines. Varivax Post exposure; VZIG Øsusceptible pregnant women have been exposed to VZV. Øinfants whose mothers develop V < 5 days of delivery or the first 2 days after delivery.
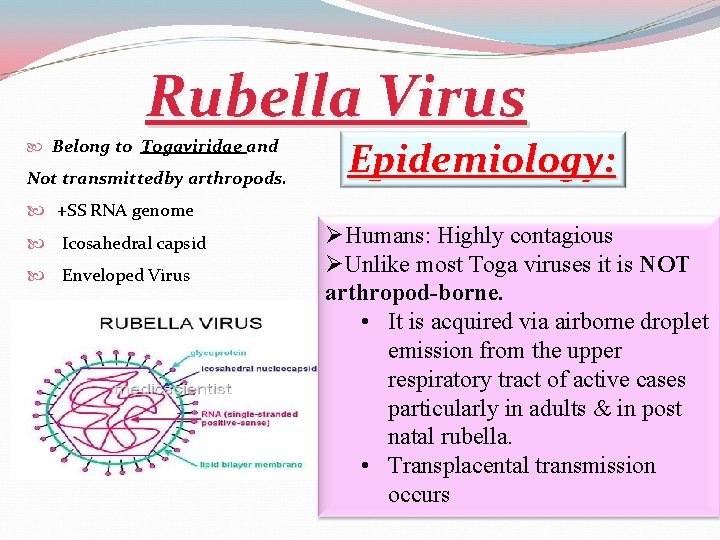
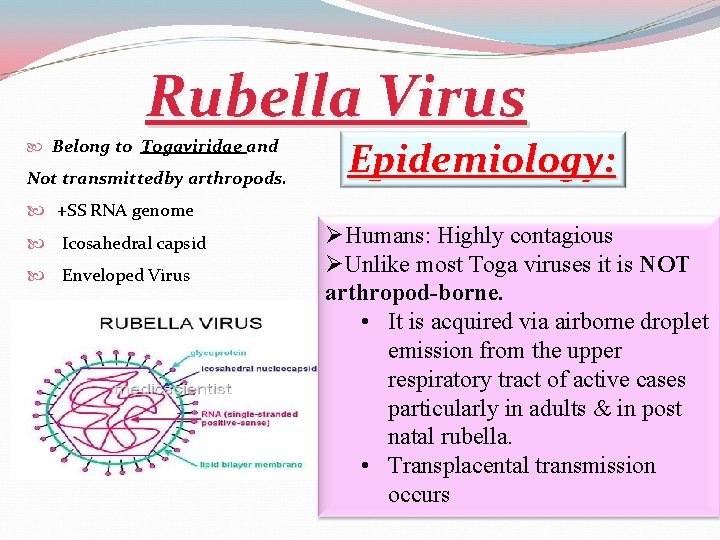
Rubella Virus Belong to Togaviridae and Not transmittedby arthropods. +SS RNA genome Icosahedral capsid Enveloped Virus Epidemiology: ØHumans: Highly contagious ØUnlike most Toga viruses it is NOT arthropod-borne. • It is acquired via airborne droplet emission from the upper respiratory tract of active cases particularly in adults & in post natal rubella. • Transplacental transmission occurs
The name "rubella" is derived from the Latin, meaning little red. Rubella is a contagious viral infection best known by its distinctive red rash. Aetiology: Rubella virus is the only member of the Rubivirus genus of the Togavirus family. It is an enveloped (toga=cloak), non-segmented, positive sense, RNA virus and replicates in the cytoplasm. Its nucleocapsid has icosahedral symmetry. The virus carries haemagglutinin. There is only one major antigenic type.
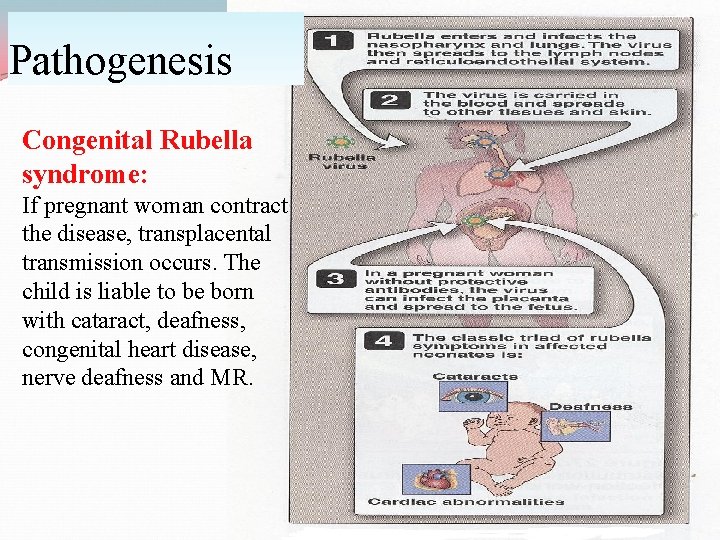
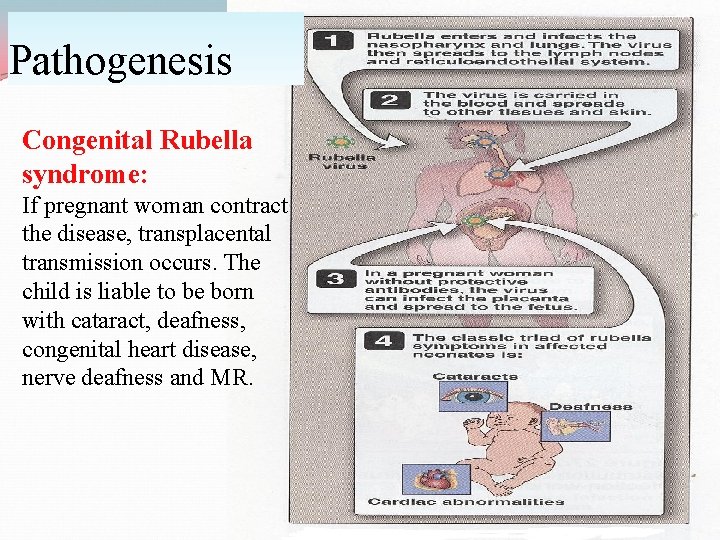
Pathogenesis Congenital Rubella syndrome: If pregnant woman contract the disease, transplacental transmission occurs. The child is liable to be born with cataract, deafness, congenital heart disease, nerve deafness and MR.
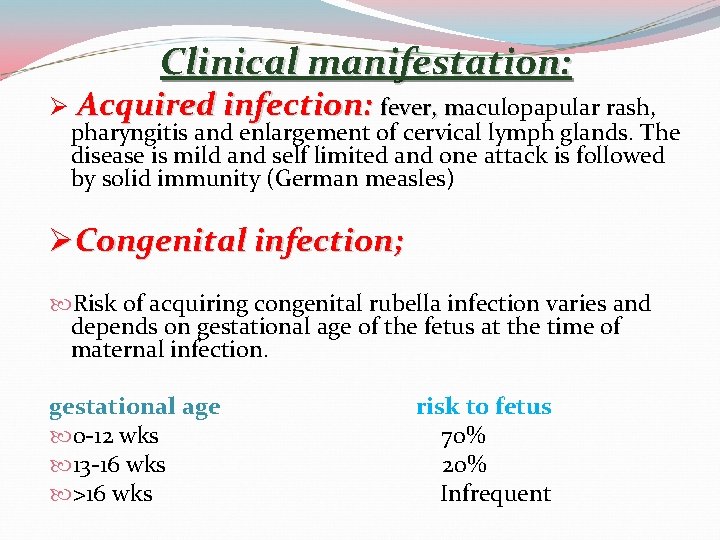
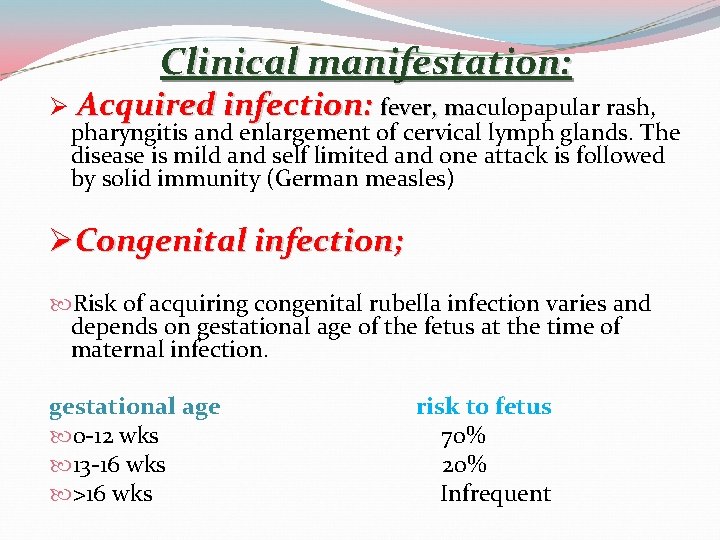
Clinical manifestation: Ø Acquired infection: fever, maculopapular rash, m pharyngitis and enlargement of cervical lymph glands. The disease is mild and self limited and one attack is followed by solid immunity (German measles) ØCongenital infection; Risk of acquiring congenital rubella infection varies and depends on gestational age of the fetus at the time of maternal infection. gestational age 0 -12 wks 13 -16 wks >16 wks risk to fetus 70% 20% Infrequent
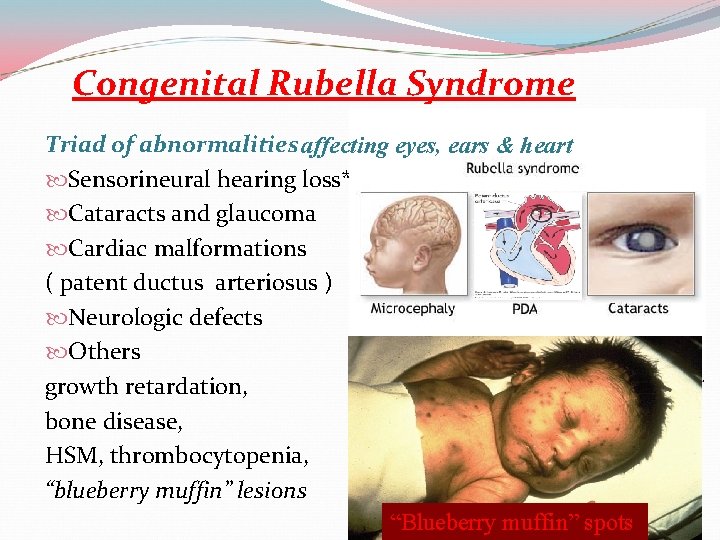
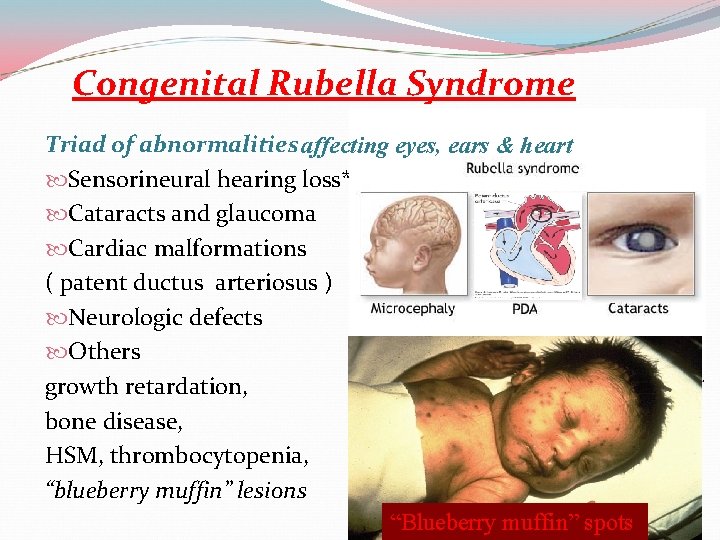
Congenital Rubella Syndrome Triad of abnormalities affecting eyes, ears & heart Sensorineural hearing loss* Cataracts and glaucoma Cardiac malformations ( patent ductus arteriosus ) Neurologic defects Others growth retardation, bone disease, HSM, thrombocytopenia, “blueberry muffin” lesions “Blueberry muffin” spots 21
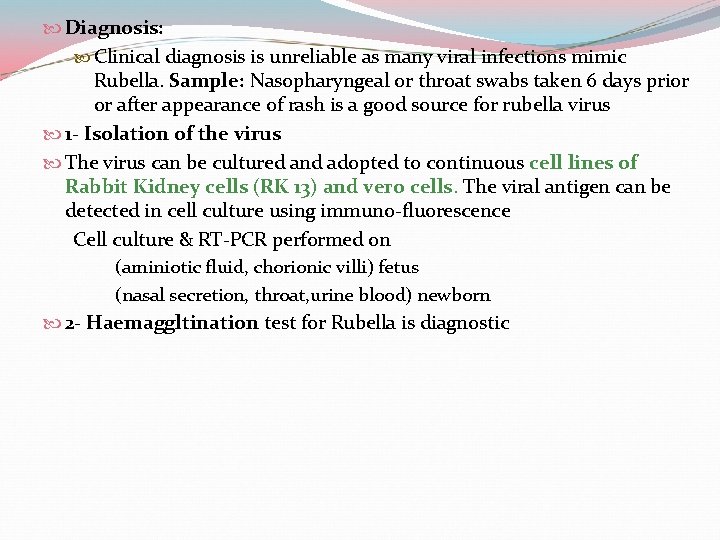
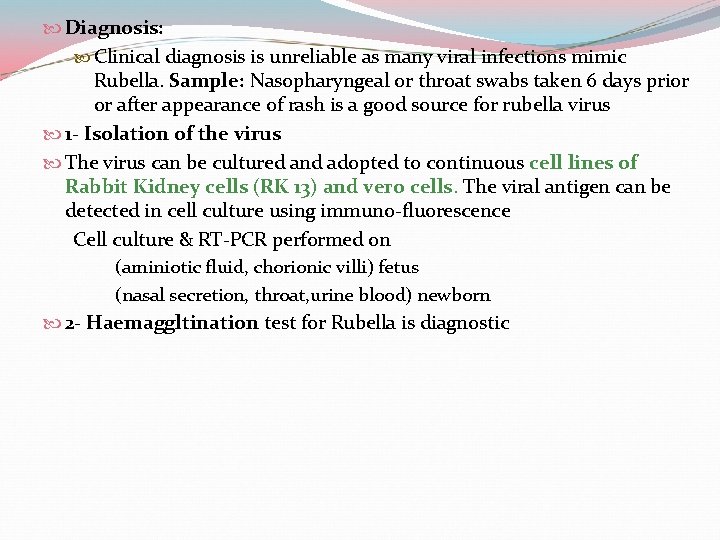
Diagnosis: Clinical diagnosis is unreliable as many viral infections mimic Rubella. Sample: Nasopharyngeal or throat swabs taken 6 days prior or after appearance of rash is a good source for rubella virus 1 - Isolation of the virus The virus can be cultured and adopted to continuous cell lines of Rabbit Kidney cells (RK 13) and vero cells. The viral antigen can be detected in cell culture using immuno-fluorescence Cell culture & RT-PCR performed on (aminiotic fluid, chorionic villi) fetus (nasal secretion, throat, urine blood) newborn 2 - Haemaggltination test for Rubella is diagnostic
3 - Evidence of seroconversion ELISA tests are of greater importance Detection of Rubella specific Ig. M in single serum specimen is diagnostic for recent infection A rise in antibody (Ig. G) titre must be demonstrated between 2 serum samples taken at least 10 days a part. For congenital Rubella syndrome the demonstration of Rubella Ig. M antibodies in a new born is diagnostic as Ig. M don’t cross the placenta and are produced in the infected fetus.
Treatment: Rubella is a mild self limited illness; no specific antiviral treatment is indicated Prevention and control: The MMR vaccine is a mixture of 3 live attenuated viruses administered via injection for immunization against measles, mumps and rubella It is generally administered to children around the age of one year with a second dose before starting school (ie: age 4 -5 years). Routine antenatal screening: Rubella specific Ig. G Non-immune women vaccination, ( avoid pregnancy for 3 months). vaccination : - before or after pregnancy but not during pregnancy.
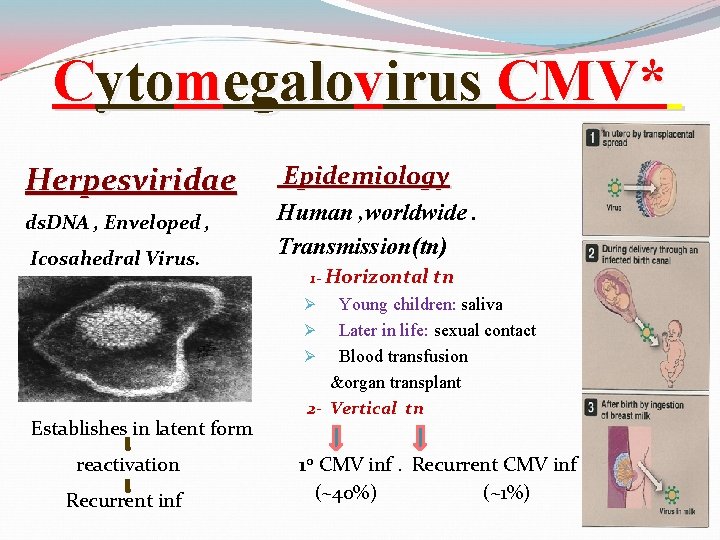
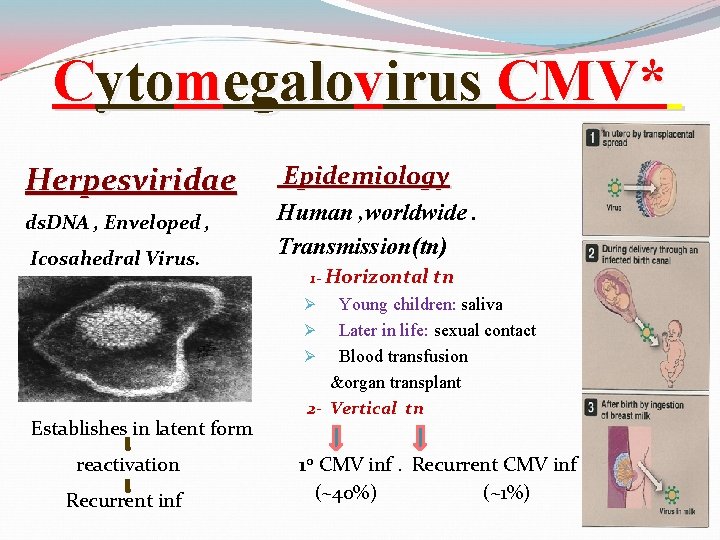
Cytomegalovirus CMV* Herpesviridae ds. DNA , Enveloped , Icosahedral Virus. Epidemiology Human , worldwide. Transmission(tn) 1 - Horizontal tn Young children: saliva Ø Later in life: sexual contact Ø Blood transfusion &organ transplant 2 - Vertical tn Ø Establishes in latent form reactivation Recurrent inf 10 CMV inf. Recurrent CMV inf (~40%) (~1%)
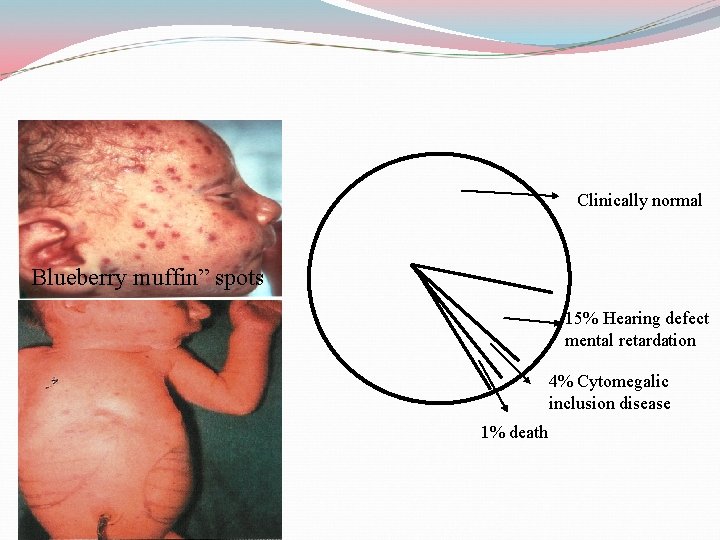
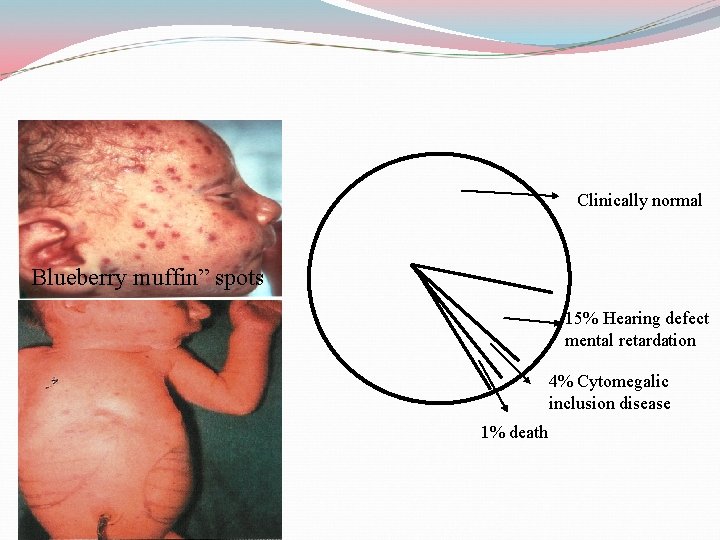
Clinically normal Blueberry muffin” spots 15% Hearing defect mental retardation 4% Cytomegalic inclusion disease 1% death
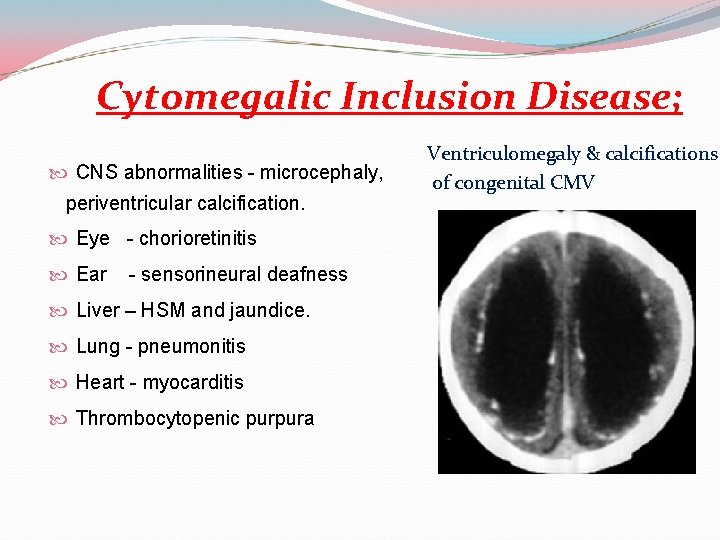
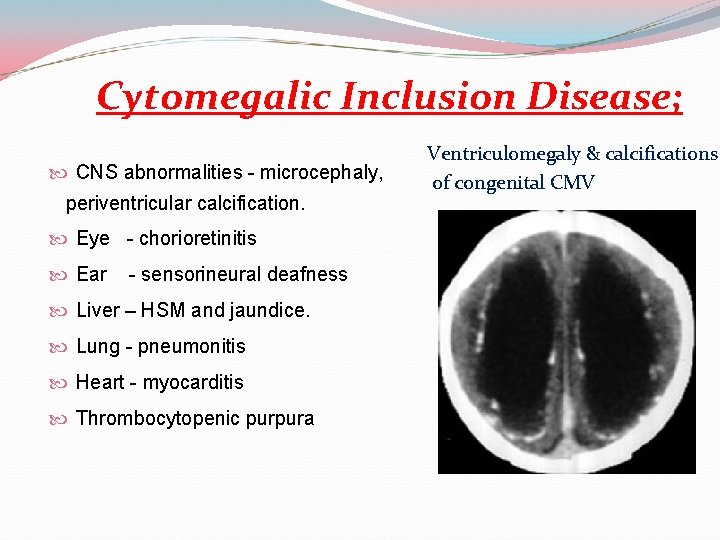
Cytomegalic Inclusion Disease; CNS abnormalities - microcephaly, periventricular calcification. Eye - chorioretinitis Ear - sensorineural deafness Liver – HSM and jaundice. Lung - pneumonitis Heart - myocarditis Thrombocytopenic purpura Ventriculomegaly & calcifications of congenital CMV
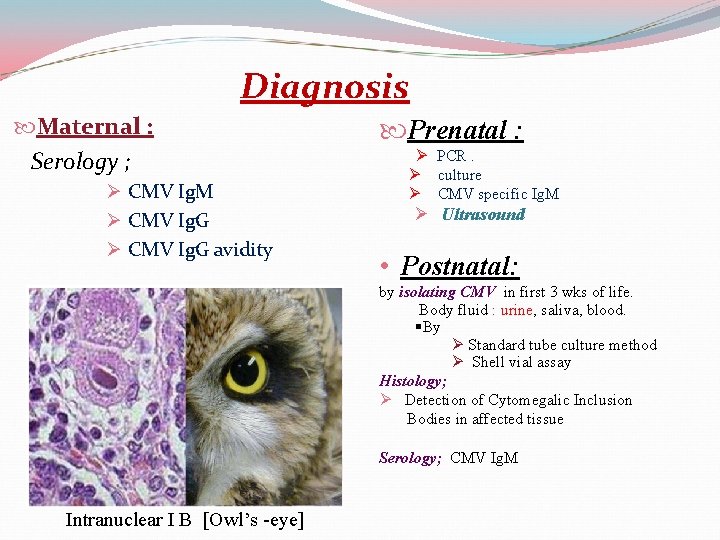
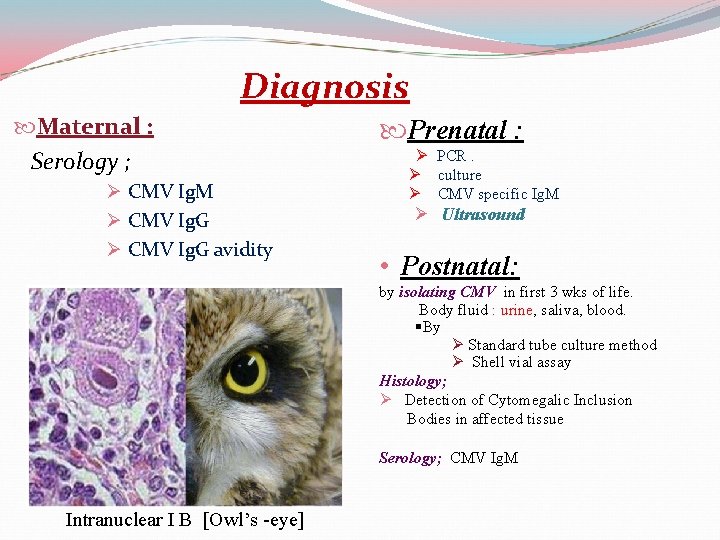
Diagnosis Maternal : Serology ; Ø CMV Ig. M Ø CMV Ig. G avidity Prenatal : Ø PCR. Ø culture Ø CMV specific Ig. M Ø Ultrasound • Postnatal: by isolating CMV in first 3 wks of life. Body fluid : urine, saliva, blood. §By Ø Standard tube culture method Ø Shell vial assay Histology; Ø Detection of Cytomegalic Inclusion Bodies in affected tissue Serology; CMV Ig. M Intranuclear I B [Owl’s -eye]
Treatment Symptomatic infants Asymptomatic infants Prevention !? Education about CMV & how to prevent it through hygiene; hand washing Vaccine is not available (TRIAL) Ganciclovir. not recommended.
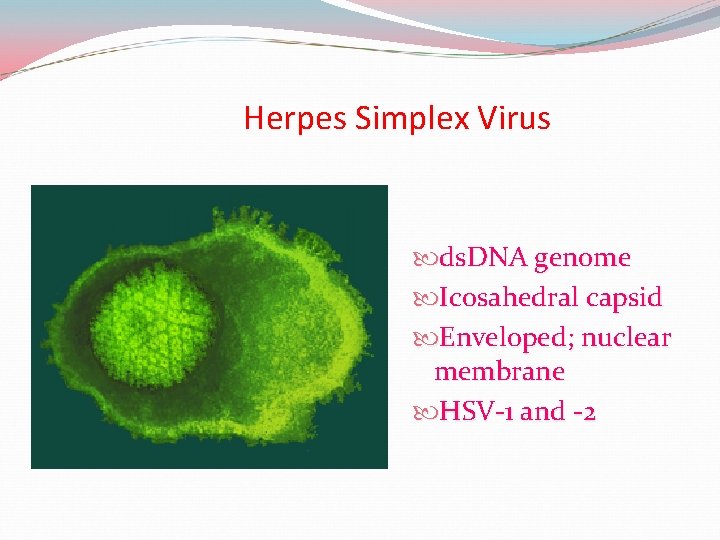
Herpes Simplex Virus ds. DNA genome Icosahedral capsid Enveloped; nuclear membrane HSV-1 and -2
Neonatal Herpes Simplex The baby is usually infected perinatally during passage through the birth canal. Premature rupturing of the membranes is a well recognized risk factor. The risk of perinatal transmission is greatest when there is a florid primary infection in the mother. There is an appreciably smaller risk from recurrent lesions in the mother, probably because of the lower viral load and the presence of specific antibody. The baby may also be infected from other sources such as oral lesions from the mother or a herpetic whitlow in a nurse.
Neonatal Herpes Simplex The spectrum of neonatal HSV infection varies from a mild disease localized to the skin to a fatal disseminated infection. Infection is particularly dangerous in premature infants Where dissemination occurs, the organs most commonly involved are the liver, adrenals and the brain. Where the brain is involved, the prognosis is particularly severe. The encephalitis is global and of such severity that the brain may be liquefied. Acyclovir should be promptly given in all suspected cases of neonatal HSV infection. The only means of prevention is to offer caesarean section to mothers with florid genital HSV lesions.
Reference books