Transitions of Care May 2018 Learning Session Background

Transitions of Care May 2018 Learning Session
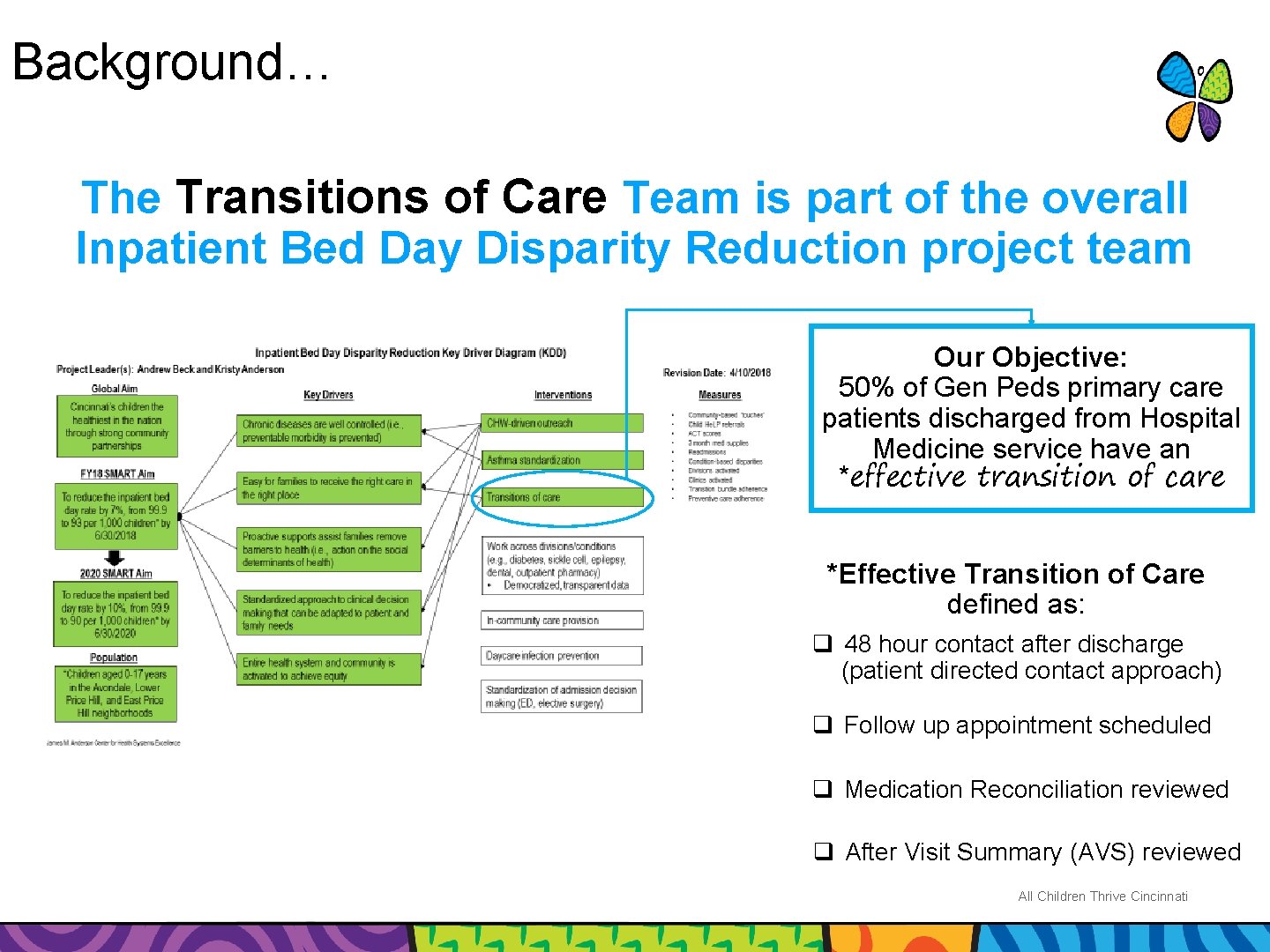
Background… The Transitions of Care Team is part of the overall Inpatient Bed Day Disparity Reduction project team Our Objective: 50% of Gen Peds primary care patients discharged from Hospital Medicine service have an *effective transition of care *Effective Transition of Care defined as: q 48 hour contact after discharge (patient directed contact approach) q Follow up appointment scheduled q Medication Reconciliation reviewed q After Visit Summary (AVS) reviewed All Children Thrive Cincinnati
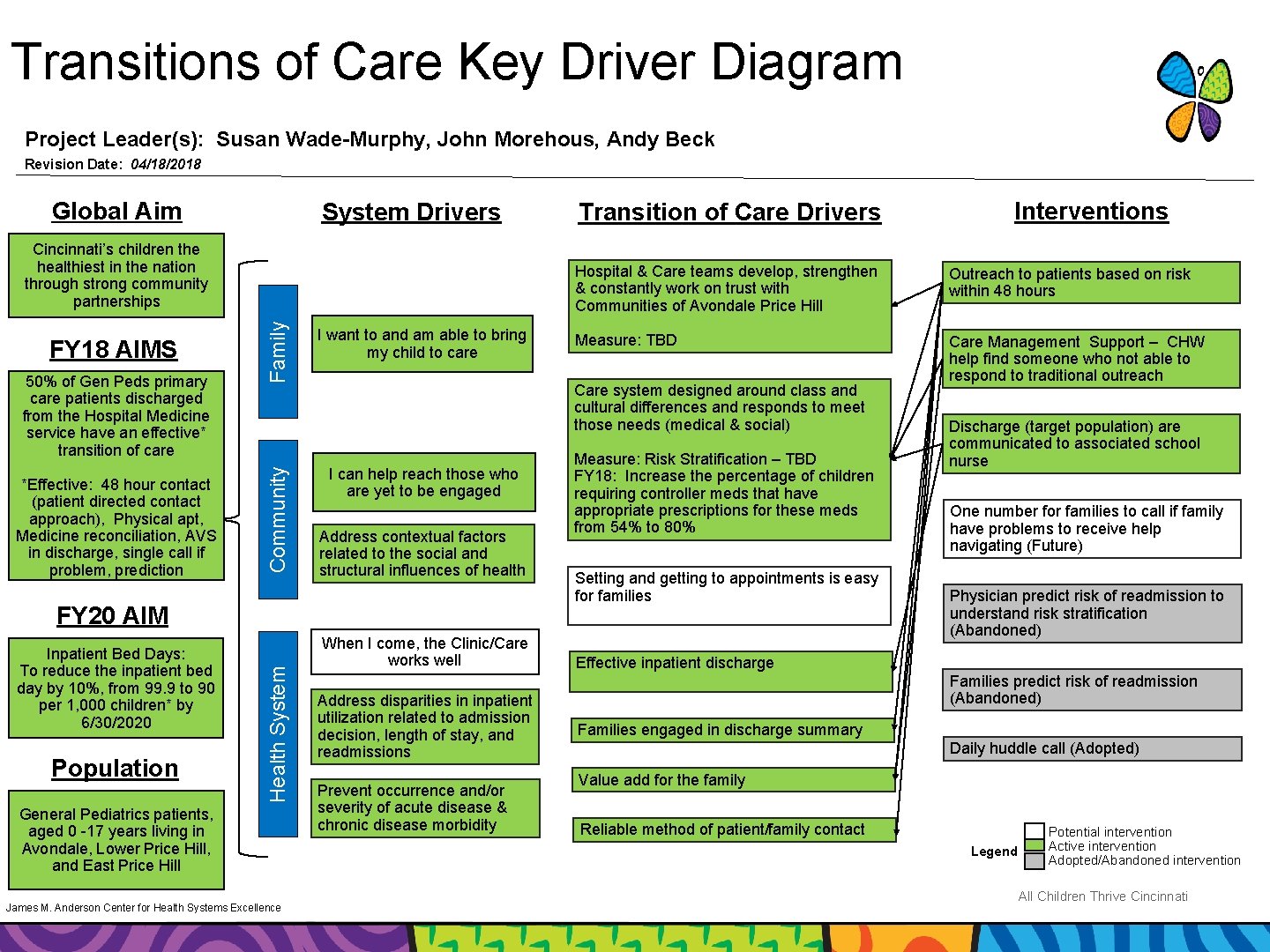
Transitions of Care Key Driver Diagram Project Leader(s): Susan Wade-Murphy, John Morehous, Andy Beck Revision Date: 04/18/2018 Global Aim System Drivers 50% of Gen Peds primary care patients discharged from the Hospital Medicine service have an effective* transition of care *Effective: 48 hour contact (patient directed contact approach), Physical apt, Medicine reconciliation, AVS in discharge, single call if problem, prediction Community FY 18 AIMS Family Cincinnati’s children the healthiest in the nation through strong community partnerships I want to and am able to bring my child to care I can help reach those who are yet to be engaged Address contextual factors related to the social and structural influences of health Health System Population General Pediatrics patients, aged 0 -17 years living in Avondale, Lower Price Hill, and East Price Hill James M. Anderson Center for Health Systems Excellence When I come, the Clinic/Care works well Address disparities in inpatient utilization related to admission decision, length of stay, and readmissions Prevent occurrence and/or severity of acute disease & chronic disease morbidity Interventions Hospital & Care teams develop, strengthen & constantly work on trust with Communities of Avondale Price Hill Outreach to patients based on risk within 48 hours Measure: TBD Care Management Support – CHW help find someone who not able to respond to traditional outreach Care system designed around class and cultural differences and responds to meet those needs (medical & social) FY 20 AIM Inpatient Bed Days: To reduce the inpatient bed day by 10%, from 99. 9 to 90 per 1, 000 children* by 6/30/2020 Transition of Care Drivers Measure: Risk Stratification – TBD FY 18: Increase the percentage of children requiring controller meds that have appropriate prescriptions for these meds from 54% to 80% Setting and getting to appointments is easy for families Discharge (target population) are communicated to associated school nurse One number for families to call if family have problems to receive help navigating (Future) Physician predict risk of readmission to understand risk stratification (Abandoned) Effective inpatient discharge Families predict risk of readmission (Abandoned) Families engaged in discharge summary Daily huddle call (Adopted) Value add for the family Reliable method of patient/family contact Legend Potential intervention Active intervention Adopted/Abandoned intervention All Children Thrive Cincinnati
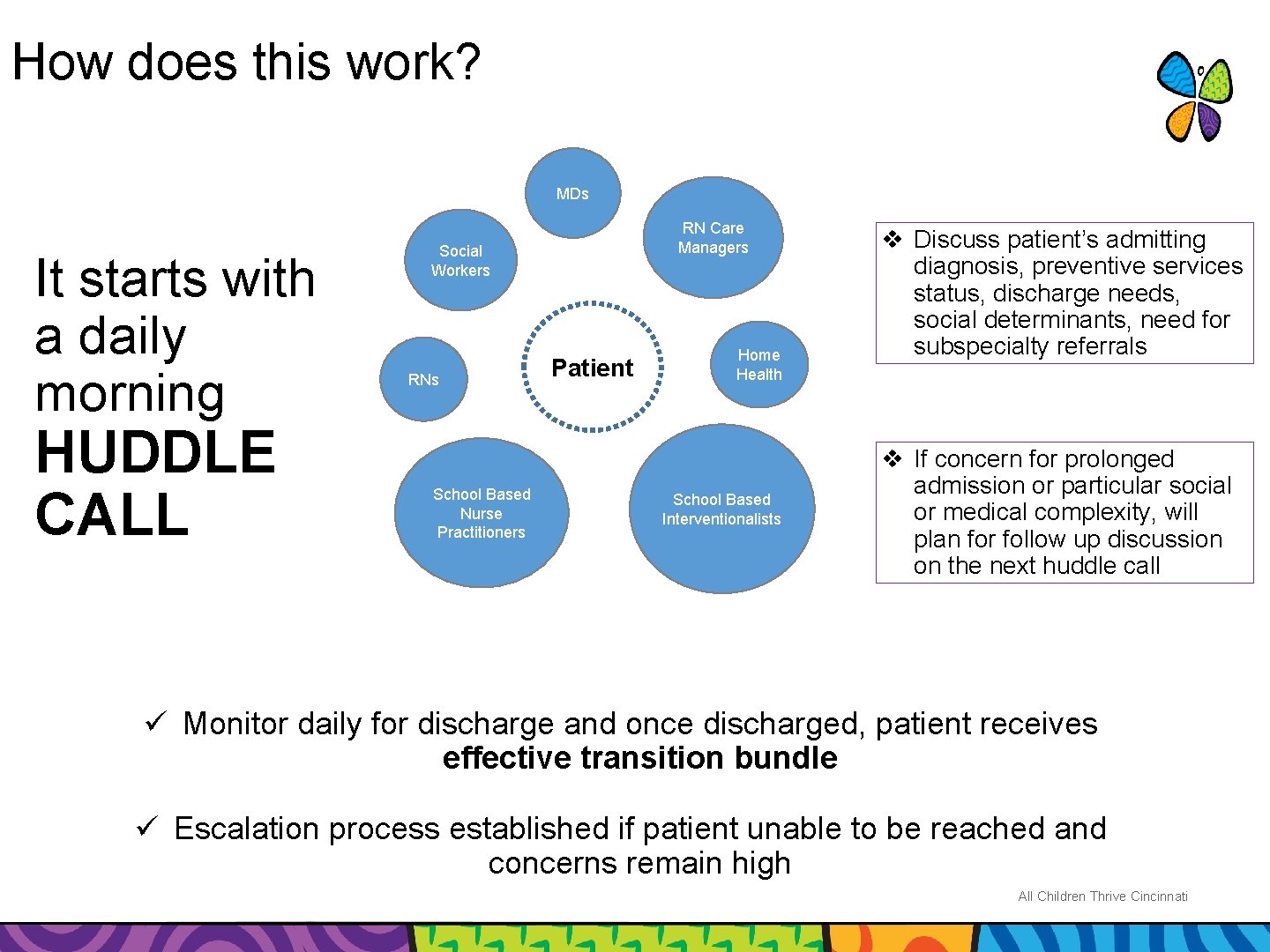
How does this work? MDs It starts with a daily morning HUDDLE CALL RN Care Managers Social Workers RNs School Based Nurse Practitioners Patient Home Health School Based Interventionalists v Discuss patient’s admitting diagnosis, preventive services status, discharge needs, social determinants, need for subspecialty referrals v If concern for prolonged admission or particular social or medical complexity, will plan for follow up discussion on the next huddle call ü Monitor daily for discharge and once discharged, patient receives effective transition bundle ü Escalation process established if patient unable to be reached and concerns remain high All Children Thrive Cincinnati
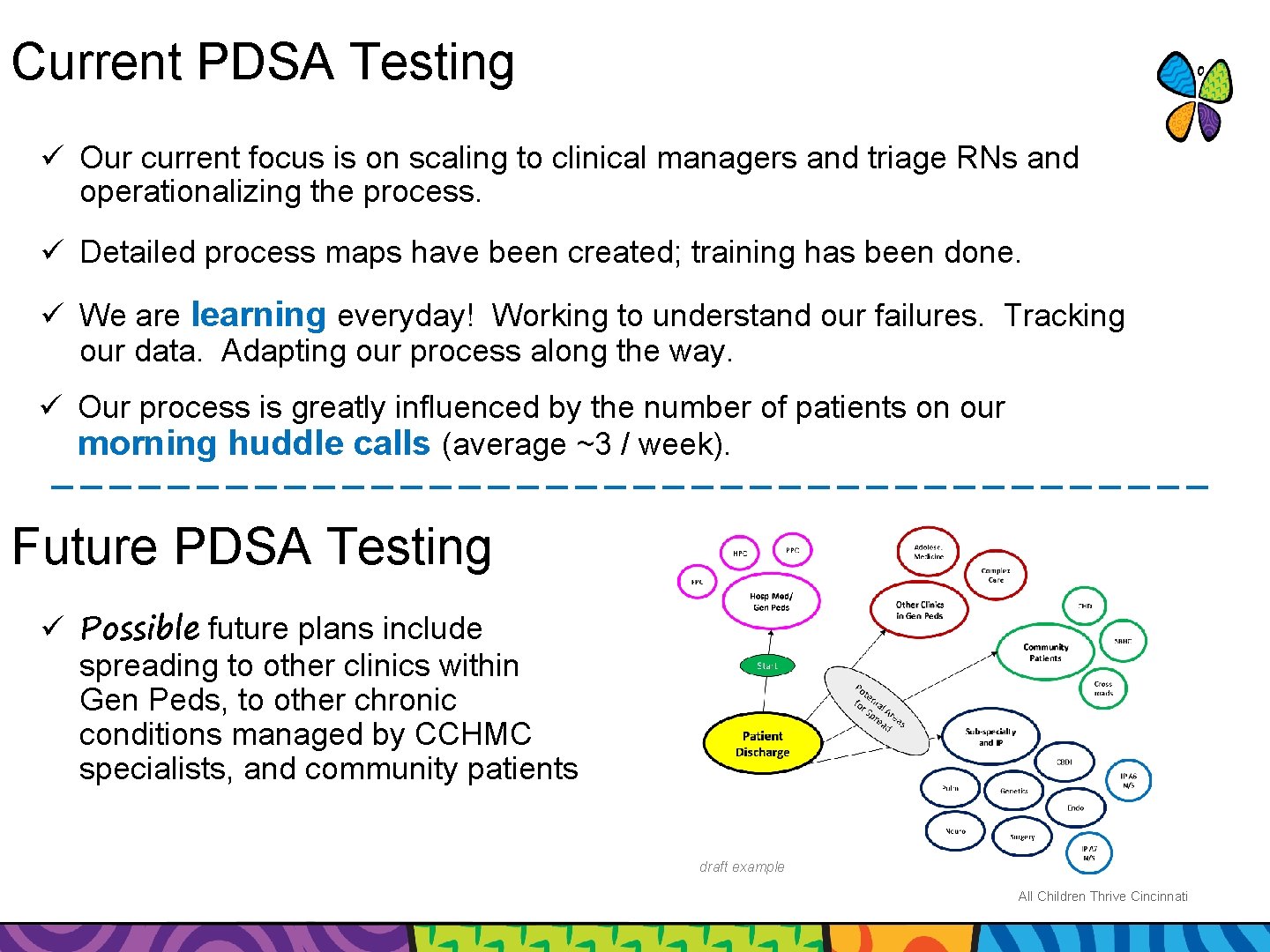
Current PDSA Testing ü Our current focus is on scaling to clinical managers and triage RNs and operationalizing the process. ü Detailed process maps have been created; training has been done. ü We are learning everyday! Working to understand our failures. Tracking our data. Adapting our process along the way. ü Our process is greatly influenced by the number of patients on our morning huddle calls (average ~3 / week). Future PDSA Testing ü Possible future plans include spreading to other clinics within Gen Peds, to other chronic conditions managed by CCHMC specialists, and community patients draft example All Children Thrive Cincinnati
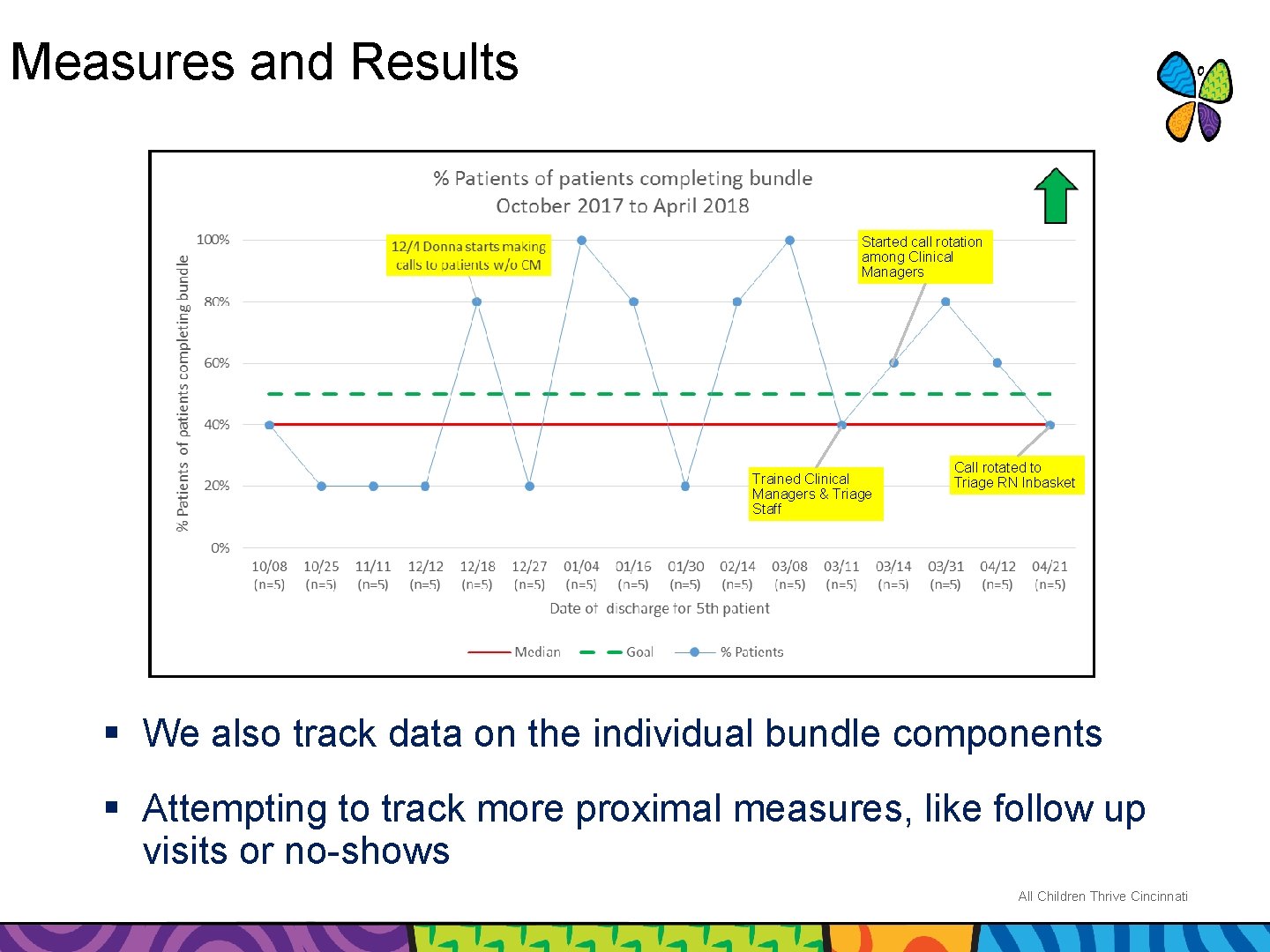
Measures and Results Started call rotation among Clinical Managers Trained Clinical Managers & Triage Staff Call rotated to Triage RN Inbasket § We also track data on the individual bundle components § Attempting to track more proximal measures, like follow up visits or no-shows All Children Thrive Cincinnati
Contacts Thank you! We welcome any questions or further discussion… Susan Wade-Murphy, RN John Morehous, MD Andy Beck, MD Donna White, RN Susan. Wade-Murphy@cchmc. org John. Morehous@cchmc. org Andrew. Beck 1@cchmc. org Donna. White@cchmc. org General Pediatrics Clinical Manager Asst VP - Patient Services General Pediatrics All Children Thrive Cincinnati
- Slides: 7