Transitions of Care Focused Use Case Scenario example



- Slides: 28
Transitions of Care Focused Use Case Scenario (example) PACIO PROJECT
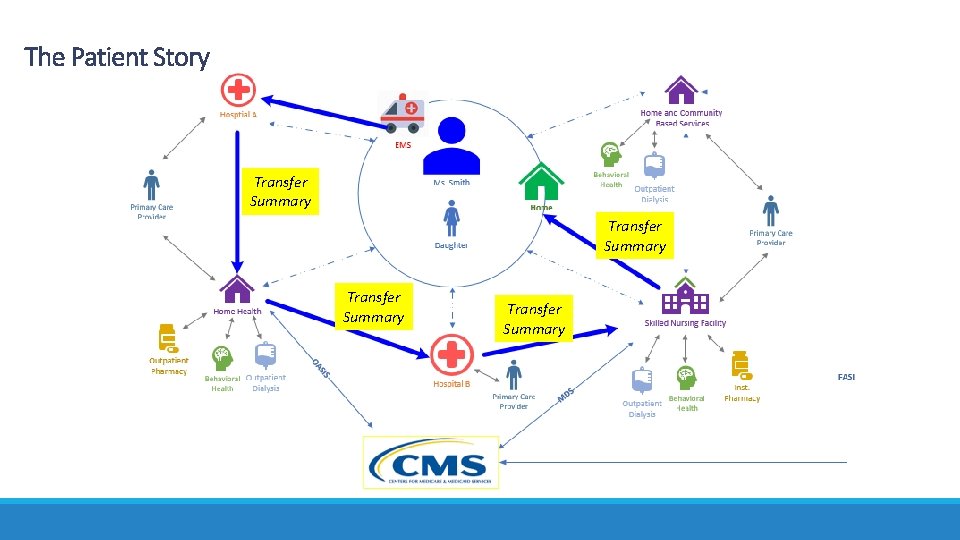
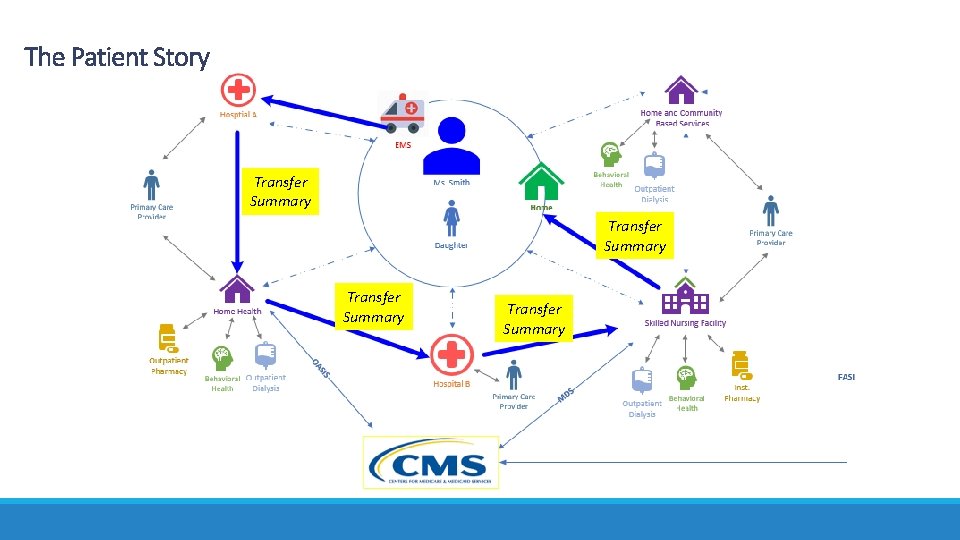
The Patient Story Transfer Summary
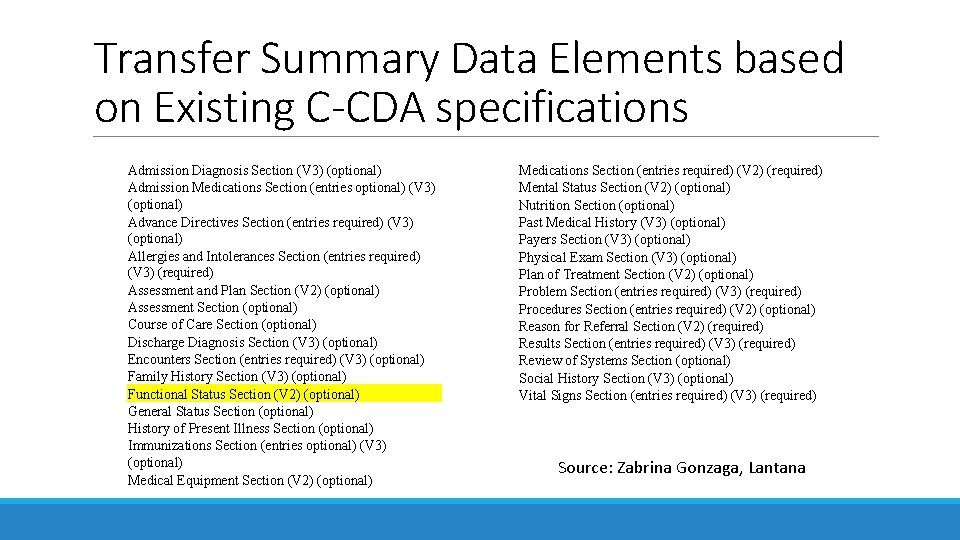
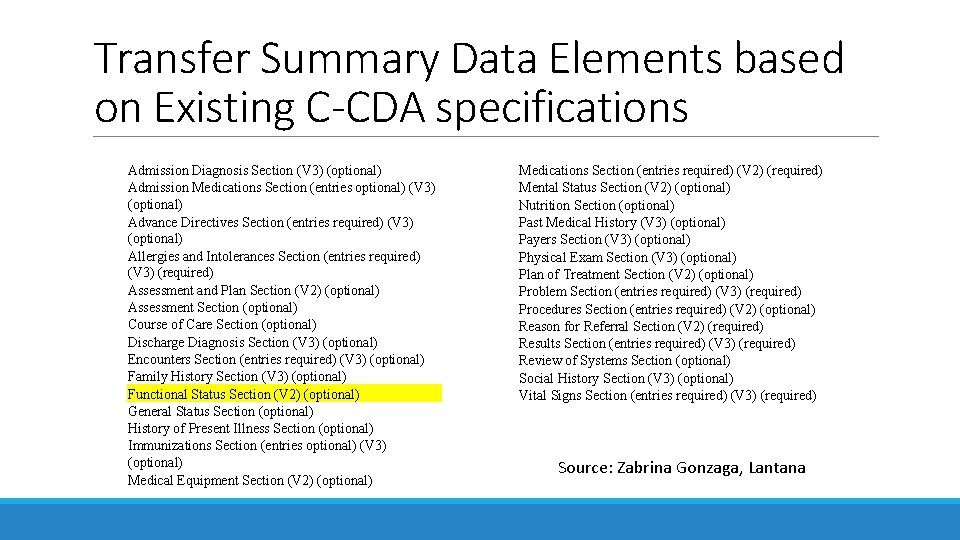
Transfer Summary Data Elements based on Existing C-CDA specifications Admission Diagnosis Section (V 3) (optional) Admission Medications Section (entries optional) (V 3) (optional) Advance Directives Section (entries required) (V 3) (optional) Allergies and Intolerances Section (entries required) (V 3) (required) Assessment and Plan Section (V 2) (optional) Assessment Section (optional) Course of Care Section (optional) Discharge Diagnosis Section (V 3) (optional) Encounters Section (entries required) (V 3) (optional) Family History Section (V 3) (optional) Functional Status Section (V 2) (optional) General Status Section (optional) History of Present Illness Section (optional) Immunizations Section (entries optional) (V 3) (optional) Medical Equipment Section (V 2) (optional) Medications Section (entries required) (V 2) (required) Mental Status Section (V 2) (optional) Nutrition Section (optional) Past Medical History (V 3) (optional) Payers Section (V 3) (optional) Physical Exam Section (V 3) (optional) Plan of Treatment Section (V 2) (optional) Problem Section (entries required) (V 3) (required) Procedures Section (entries required) (V 2) (optional) Reason for Referral Section (V 2) (required) Results Section (entries required) (V 3) (required) Review of Systems Section (optional) Social History Section (V 3) (optional) Vital Signs Section (entries required) (V 3) (required) Source: Zabrina Gonzaga, Lantana
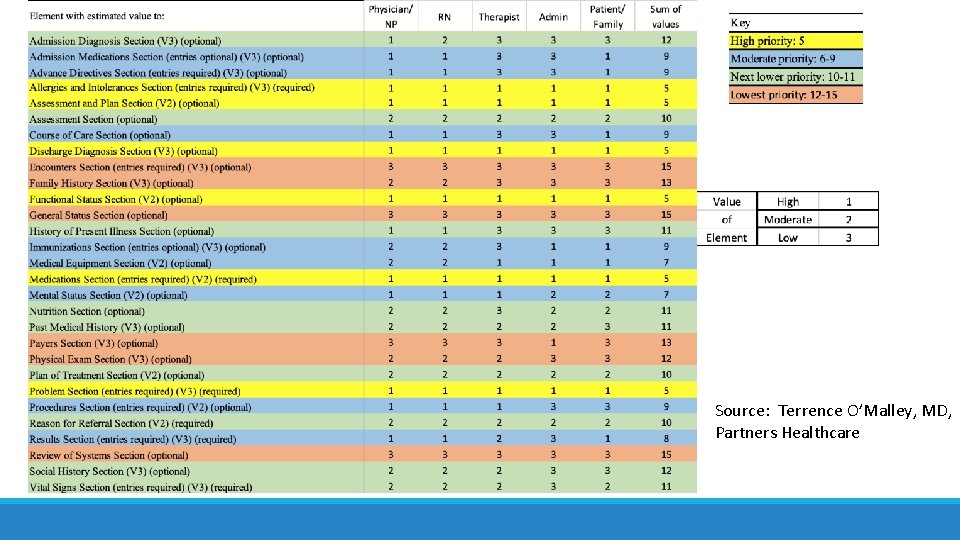
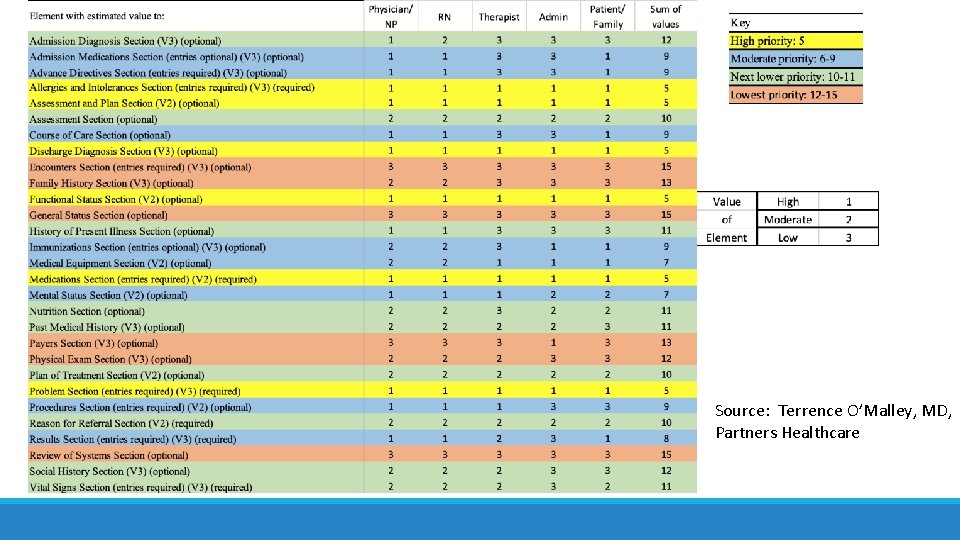
Source: Terrence O’Malley, MD, Partners Healthcare
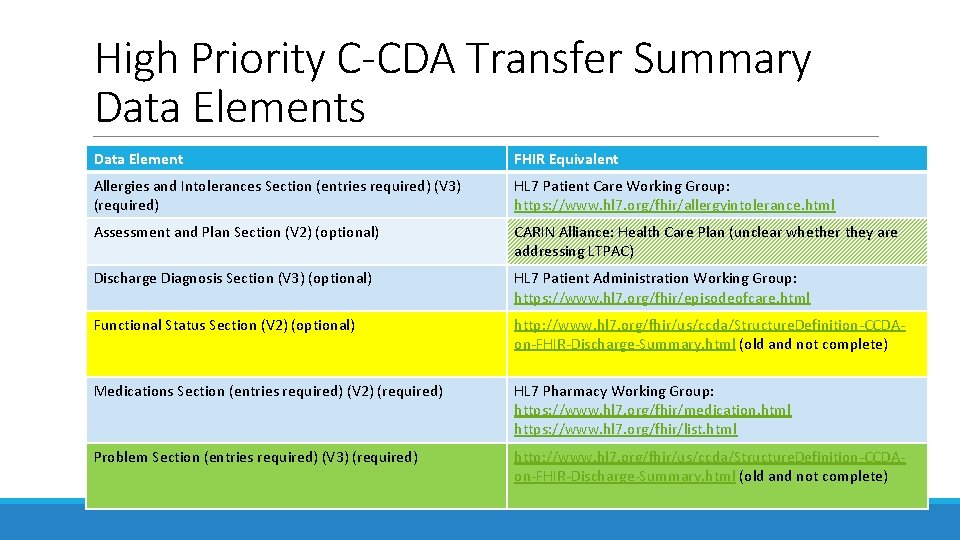
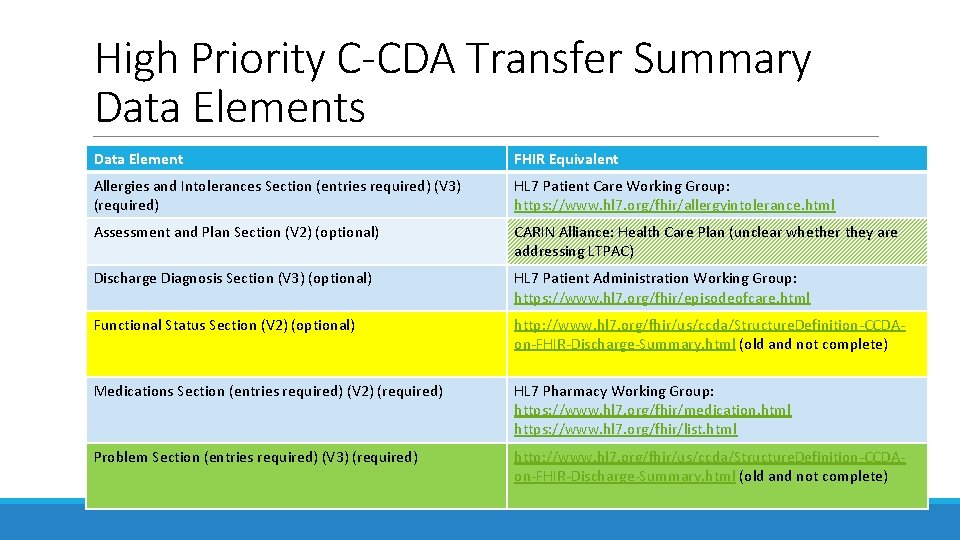
High Priority C-CDA Transfer Summary Data Elements Data Element FHIR Equivalent Allergies and Intolerances Section (entries required) (V 3) (required) HL 7 Patient Care Working Group: https: //www. hl 7. org/fhir/allergyintolerance. html Assessment and Plan Section (V 2) (optional) CARIN Alliance: Health Care Plan (unclear whether they are addressing LTPAC) Discharge Diagnosis Section (V 3) (optional) HL 7 Patient Administration Working Group: https: //www. hl 7. org/fhir/episodeofcare. html Functional Status Section (V 2) (optional) http: //www. hl 7. org/fhir/us/ccda/Structure. Definition-CCDAon-FHIR-Discharge-Summary. html (old and not complete) Medications Section (entries required) (V 2) (required) HL 7 Pharmacy Working Group: https: //www. hl 7. org/fhir/medication. html https: //www. hl 7. org/fhir/list. html Problem Section (entries required) (V 3) (required) http: //www. hl 7. org/fhir/us/ccda/Structure. Definition-CCDAon-FHIR-Discharge-Summary. html (old and not complete)

Patient MS. SMITH AND HER PERSPECTIVE
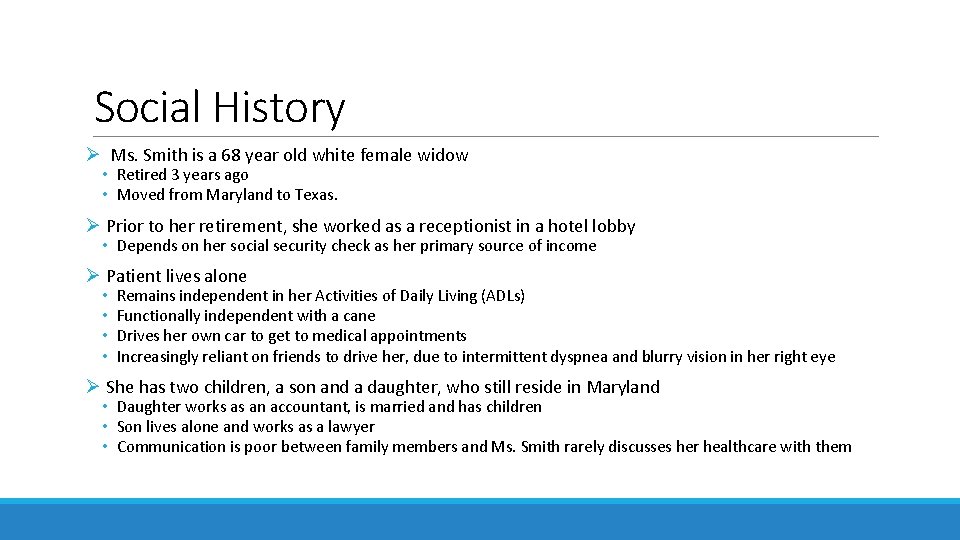
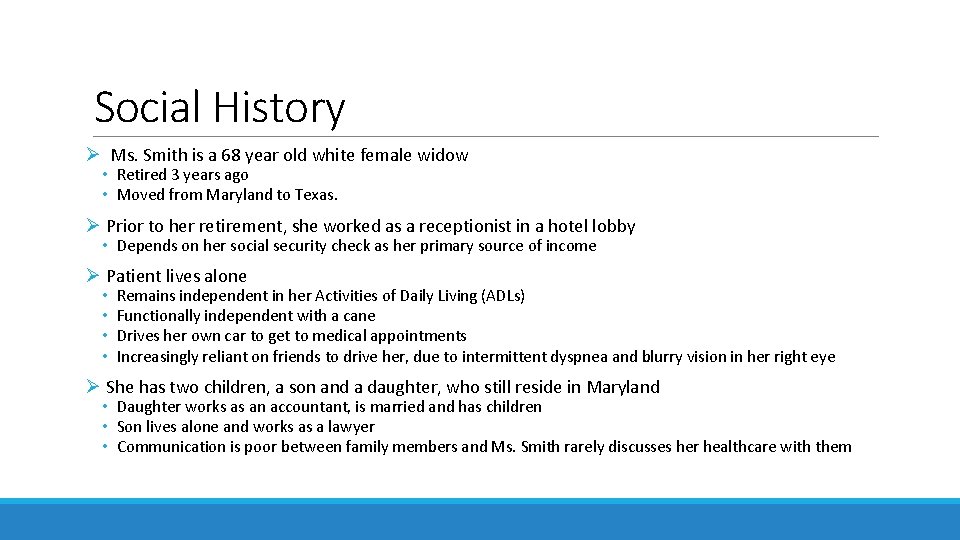
Social History Ø Ms. Smith is a 68 year old white female widow • Retired 3 years ago • Moved from Maryland to Texas. Ø Prior to her retirement, she worked as a receptionist in a hotel lobby • Depends on her social security check as her primary source of income Ø Patient lives alone • • Remains independent in her Activities of Daily Living (ADLs) Functionally independent with a cane Drives her own car to get to medical appointments Increasingly reliant on friends to drive her, due to intermittent dyspnea and blurry vision in her right eye Ø She has two children, a son and a daughter, who still reside in Maryland • Daughter works as an accountant, is married and has children • Son lives alone and works as a lawyer • Communication is poor between family members and Ms. Smith rarely discusses her healthcare with them
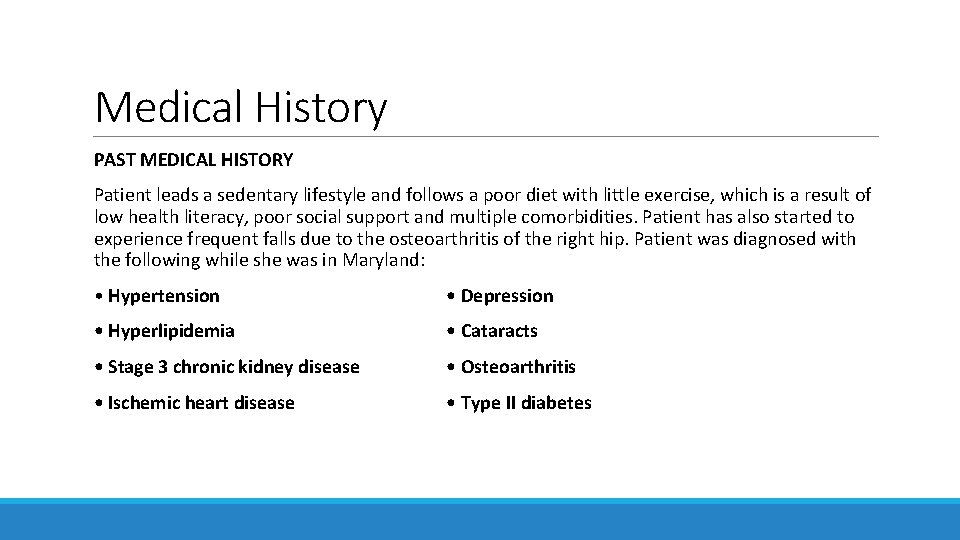
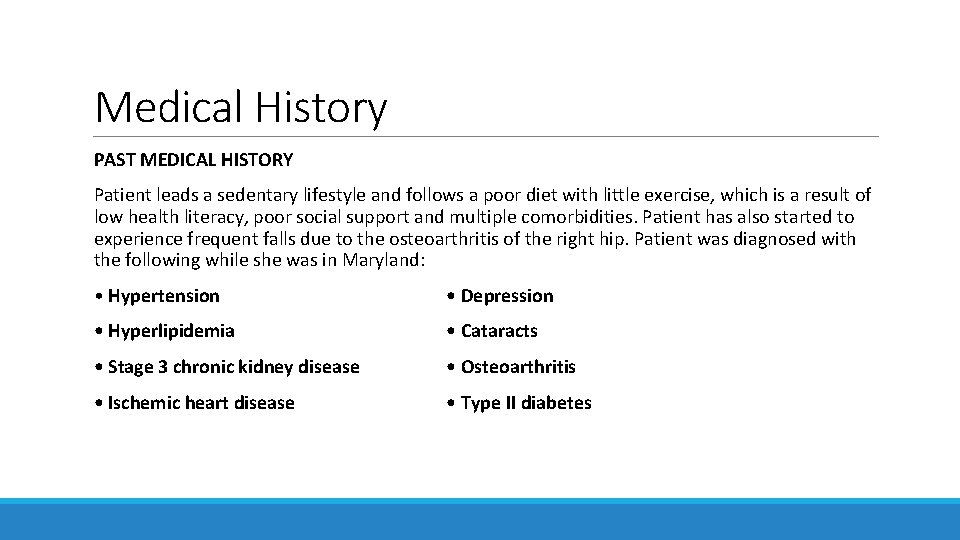
Medical History PAST MEDICAL HISTORY Patient leads a sedentary lifestyle and follows a poor diet with little exercise, which is a result of low health literacy, poor social support and multiple comorbidities. Patient has also started to experience frequent falls due to the osteoarthritis of the right hip. Patient was diagnosed with the following while she was in Maryland: • Hypertension • Depression • Hyperlipidemia • Cataracts • Stage 3 chronic kidney disease • Osteoarthritis • Ischemic heart disease • Type II diabetes
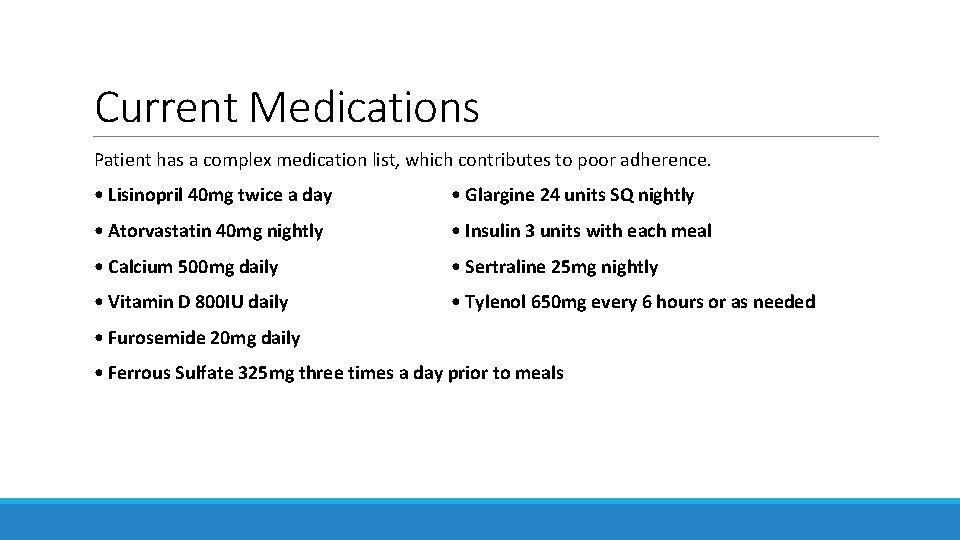
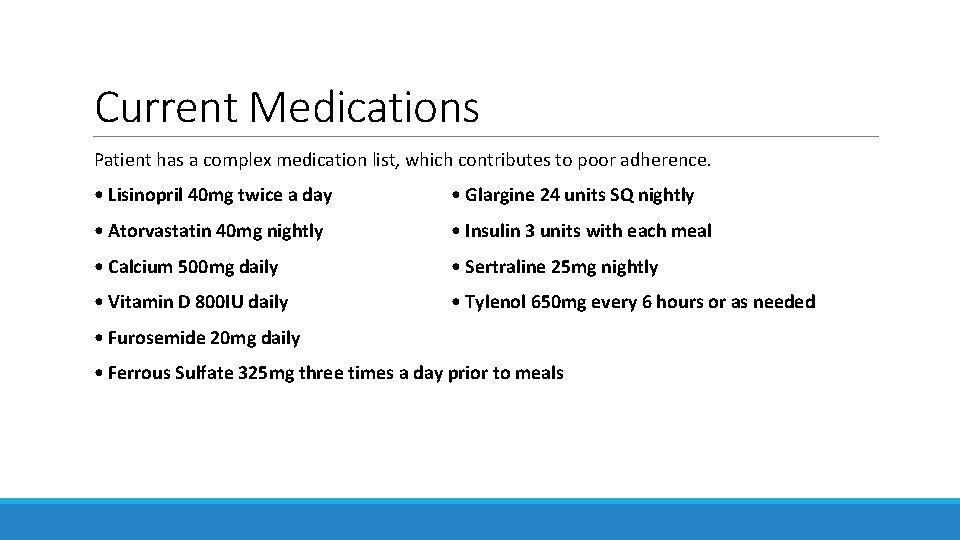
Current Medications Patient has a complex medication list, which contributes to poor adherence. • Lisinopril 40 mg twice a day • Glargine 24 units SQ nightly • Atorvastatin 40 mg nightly • Insulin 3 units with each meal • Calcium 500 mg daily • Sertraline 25 mg nightly • Vitamin D 800 IU daily • Tylenol 650 mg every 6 hours or as needed • Furosemide 20 mg daily • Ferrous Sulfate 325 mg three times a day prior to meals
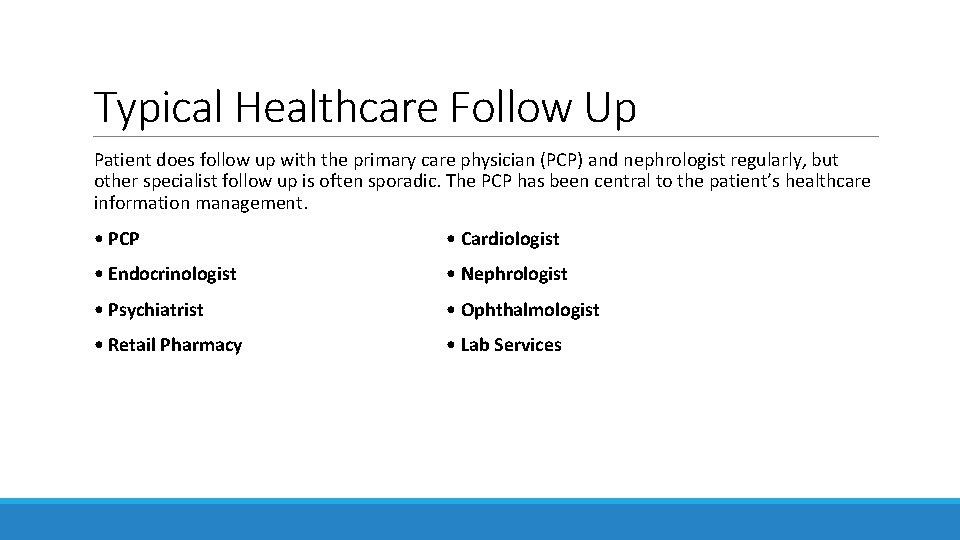
Typical Healthcare Follow Up Patient does follow up with the primary care physician (PCP) and nephrologist regularly, but other specialist follow up is often sporadic. The PCP has been central to the patient’s healthcare information management. • PCP • Cardiologist • Endocrinologist • Nephrologist • Psychiatrist • Ophthalmologist • Retail Pharmacy • Lab Services
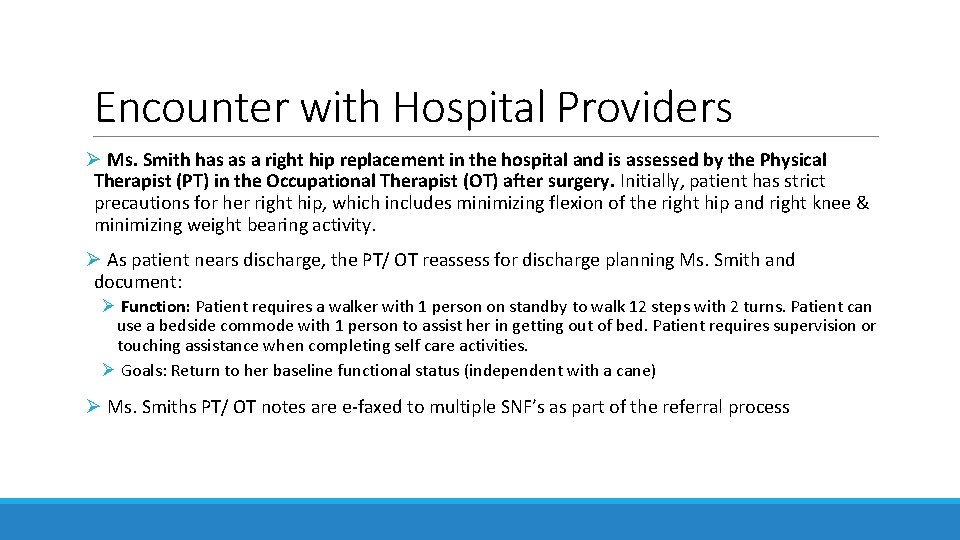
Encounter with Hospital Providers Ø Ms. Smith has as a right hip replacement in the hospital and is assessed by the Physical Therapist (PT) in the Occupational Therapist (OT) after surgery. Initially, patient has strict precautions for her right hip, which includes minimizing flexion of the right hip and right knee & minimizing weight bearing activity. Ø As patient nears discharge, the PT/ OT reassess for discharge planning Ms. Smith and document: Ø Function: Patient requires a walker with 1 person on standby to walk 12 steps with 2 turns. Patient can use a bedside commode with 1 person to assist her in getting out of bed. Patient requires supervision or touching assistance when completing self care activities. Ø Goals: Return to her baseline functional status (independent with a cane) Ø Ms. Smiths PT/ OT notes are e-faxed to multiple SNF’s as part of the referral process
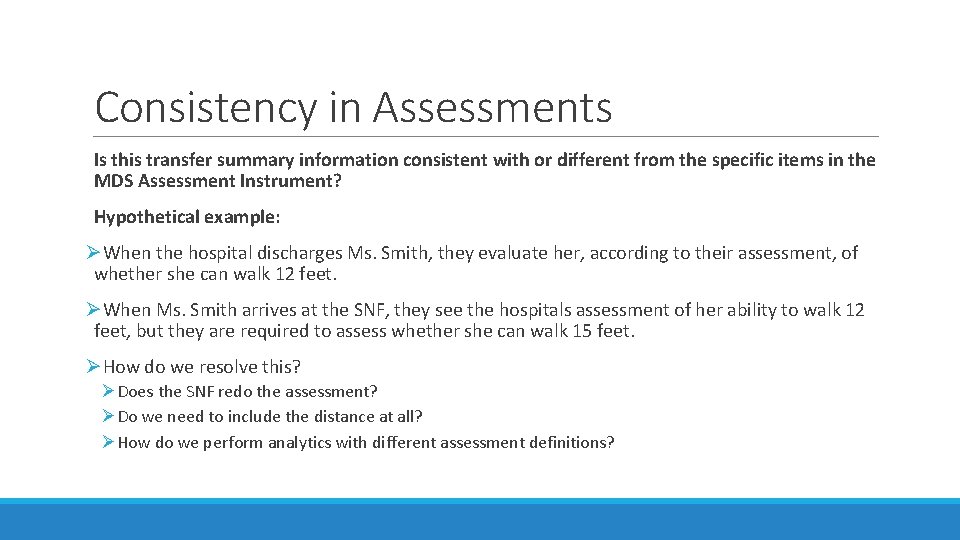
Consistency in Assessments Is this transfer summary information consistent with or different from the specific items in the MDS Assessment Instrument? Hypothetical example: ØWhen the hospital discharges Ms. Smith, they evaluate her, according to their assessment, of whether she can walk 12 feet. ØWhen Ms. Smith arrives at the SNF, they see the hospitals assessment of her ability to walk 12 feet, but they are required to assess whether she can walk 15 feet. ØHow do we resolve this? ØDoes the SNF redo the assessment? ØDo we need to include the distance at all? ØHow do we perform analytics with different assessment definitions?
Considerations 1. Outpatient/ ambulatory, acute and post acute care functional assessments are not captured and documented the same way 2. Post acute care utilizes a standardized functional assessment (IMPACT Act mandated Standardized Patient Assessment Data Element (SPADE)) 3. Previously utilized CARE Tool captured information related to weight bearing status and endurance, however there are no LOINC codes associated with them at this time 4. The Centers for Medicare & Medicaid Services (CMS), as part of the Testing Experience and Functional Tools (TEFT) demonstration, tested the use of the Functional Assessment Standardized Items (FASI) measures among individuals receiving home and communitybased services (HCBS), aligning with national efforts to create exchangeable data across Medicare and Medicaid programs
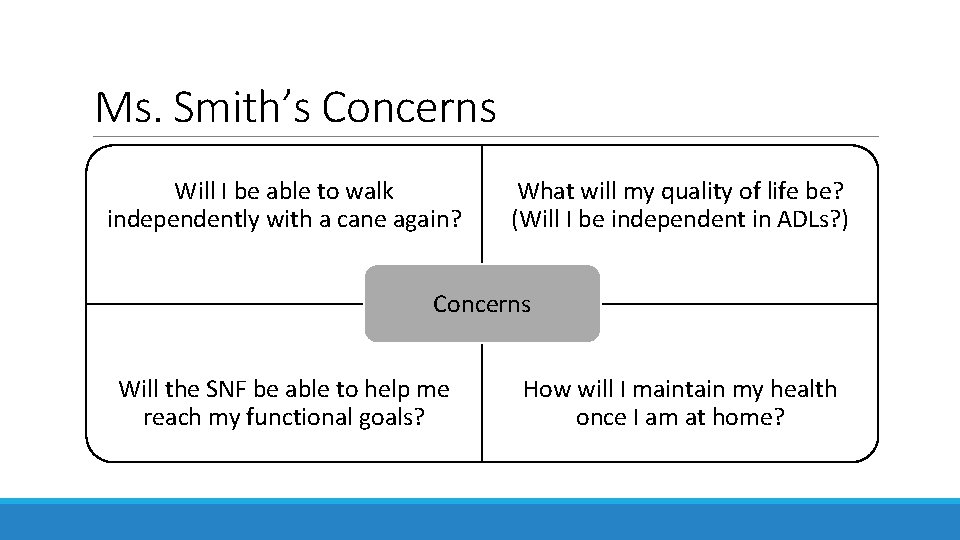
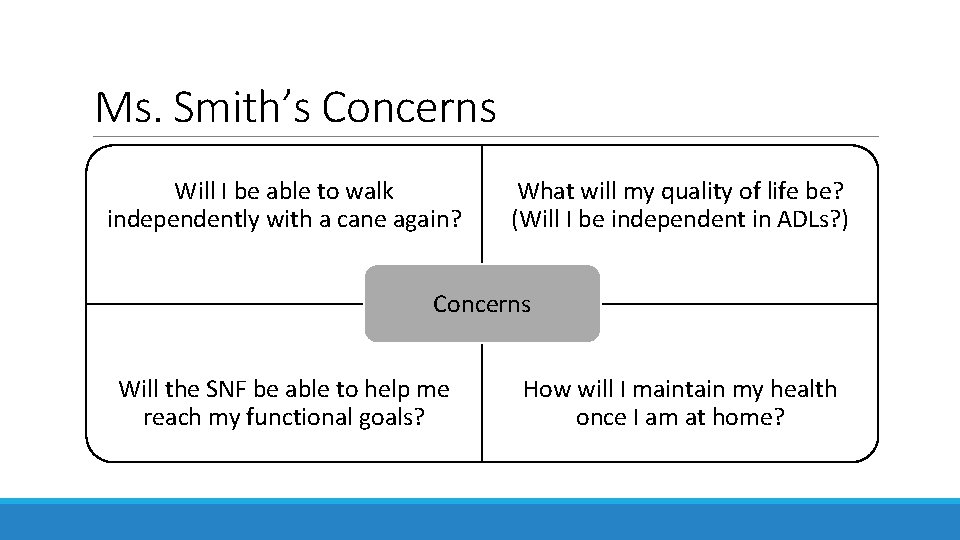
Ms. Smith’s Concerns Will I be able to walk independently with a cane again? What will my quality of life be? (Will I be independent in ADLs? ) Concerns Will the SNF be able to help me reach my functional goals? How will I maintain my health once I am at home?
Ms. Smith would like… Ø To be able to recall and communicate her functional goals to all her providers as well as track her progress Ø To provide access to her children regarding her functional status goals and Durable Medical Equipment (DME) needs Ø To have the ability to update my goals

Daughter THE PERSPECTIVE FROM THE PATIENT’S DAUGHTER
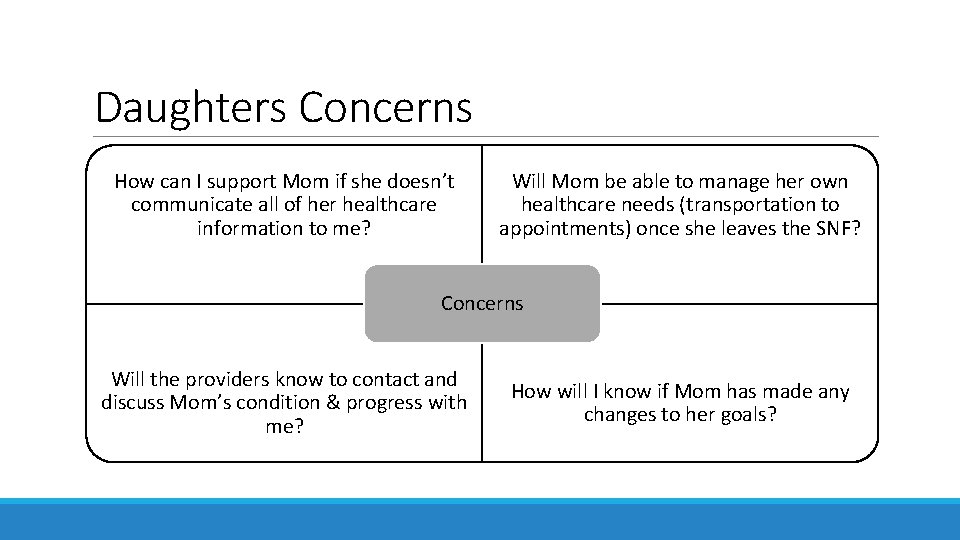
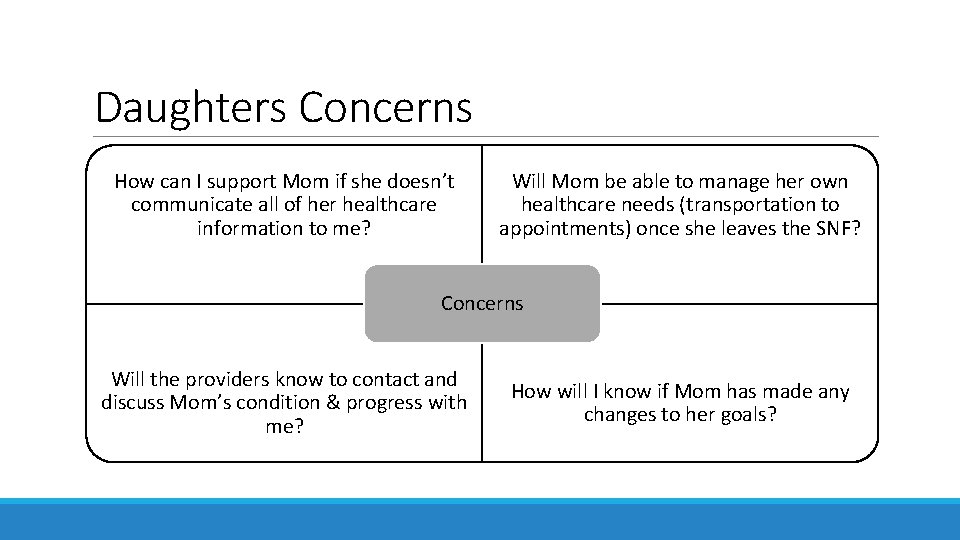
Daughters Concerns How can I support Mom if she doesn’t communicate all of her healthcare information to me? Will Mom be able to manage her own healthcare needs (transportation to appointments) once she leaves the SNF? Concerns Will the providers know to contact and discuss Mom’s condition & progress with me? How will I know if Mom has made any changes to her goals?
Daughter Would Like… Ø To have easy access to her Mother’s functional goals in the event her mother is incapacitated Ø To be notified if her Mother’s functional status changes
Case Manager/ Social Worker (CM/ SW) CARE COORDINATION PERSPECTIVE (HOSPITAL AND SNF)
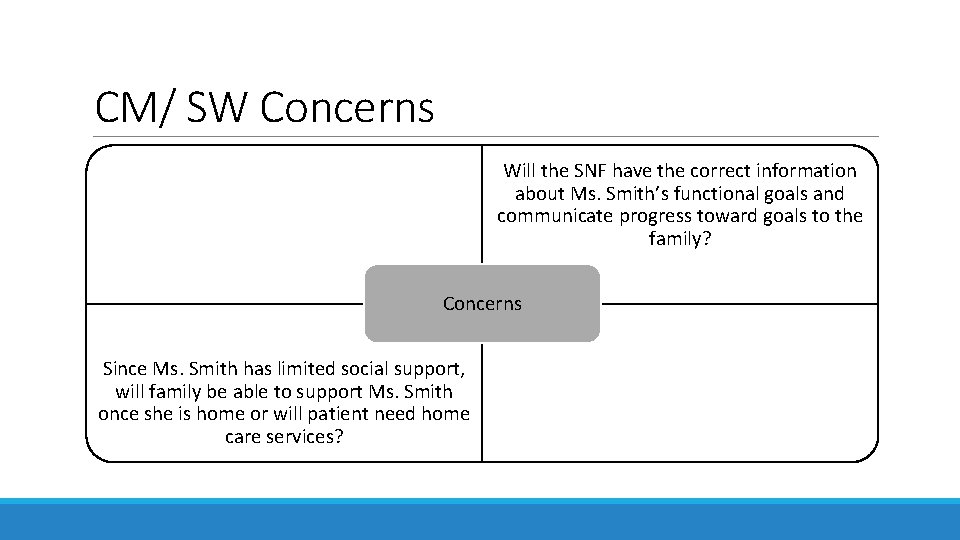
CM/ SW Concerns Will the SNF have the correct information about Ms. Smith’s functional goals and communicate progress toward goals to the family? Concerns Since Ms. Smith has limited social support, will family be able to support Ms. Smith once she is home or will patient need home care services?
CM/ SW would like… Ø To be able to identify whether the patient has functional goals in the EHR and, if so, to access the patient’s goals quickly and efficiently Ø To minimize clicks required to send functional status progress, goals and DME needs to other healthcare providers
Provider Persona HOSPITAL PROVIDER PERSPECTIVE
Provider Concerns Will Post Acute Care (PAC) have the correct information about the surgery, activity restrictions, and medication list? Concerns Since Ms. Smith has limited social support, will she be able to follow medical orders and take medications as prescribed?
Provider would like… Ø To be able to identify whether the patient has functional goals in the EHR from other healthcare settings, and if so to access the patient’s goals quickly and efficiently Ø To be able to send cognitive status, functional status progress, goals and DME needs to other healthcare providers with minimal clicks.

Payor THE PAYOR PERSPECTIVE
Payor Concerns Do members have the right PAC services established? Will PAC have the correct information about the surgery, activity restrictions, and medication lists to give the best, most efficient care? Concerns Do providers know what the members functional goals are? Does the treatment plan maximize cost efficiency?
Payor would like… Ø To engage members in their healthcare and goals
Next Steps 1. Finalize and vote on transfer summary data elements for use case 2. Examine what is currently available that addresses the data element (FHIR or a C-CDA data model) 3. Identify any gaps in the available data model 4. Fill in gaps and build a FHIR Implementation Guide (IG)