Transitional Care How to Move Elderly Patients through

- Slides: 36
Transitional Care: How to Move Elderly Patients through the Emergency Department Michael A. La. Mantia MD, MPH Kevin Biese MD, MAT Ellen Roberts Ph. D, MPH Jan Busby-Whitehead MD University of North Carolina at Chapel Hill Division of Geriatric Medicine Center for Aging and Health Department of Emergency Medicine With Support from John A. Hartford Foundation & American Geriatrics Society
Disclosures • Work supported by: » NIA Grant # 2 T 32 AG 000272 -06 A 2 » UNC John A. Hartford Foundation Center of Excellence in Geriatric Medicine and Training » John A. Hartford Foundation Geriatrics for Specialists Grant 10/7/2020 2
Outline • Aging: Global and American Perspectives • Elderly Patients and the Emergency Department • Case Study One --- Getting it Wrong • Transitional Care: Definitions and Quality Indicators • Case Study Two --- Getting it Right 10/7/2020 3
Learning Objectives 1. To identify ways in which the care of older patients in the emergency department differ from that of younger patients 2. To define key components of effective transitional care of elderly patients 3. To identify potential strategies to improve the coordination of care for elderly patients who are seen in the emergency department 10/7/2020 4
Aging: International and Domestic Scope • Baby Boom Generation » Born between 1946 and 1964 » Quickly approaching age of retirement 10/7/2020 5

Aging: Worldwide Issue • World Health Organization (WHO) report (2002): » Age cohort >60 fastest growing population segment worldwide » Decreases in fertility rates and increases in life expectancy will change age compositions of many nations • WHO and United Nations estimate: » 35% of Japan’s population >60 in 2025 » 34% of Italy’s population >60 in 2025 » China’s population >60 will increase from 134 million in 2002 to 287 million in 2025 • WHO calls for “healthy and active ageing” to be key world-wide policy concern 10/7/2020 6
Aging: Impact on Emergency Departments • Elderly patients: » » » » 10/7/2020 Are more ill at presentation Arrive by ambulance more frequently Receive more tests than younger patients Suffer from more chronic medical comorbidities Are admitted to the hospital at higher rates Experience longer ED stays Incur higher medical bills Return frequently to the ED 7
Case One – Mr. S • Mr. S: Friday, 7: 30 pm » 85 year old with a past medical history of moderate dementia arrives via ambulance from an assisted living facility » Arrives with no paperwork or medication administration list » Patient can’t give chief complaint » Person on call from the facility who knows patient has gone home » Grandson states patient has been coughing and that doctor at facility suspected pneumonia 10/7/2020 8
Case One – Mr. S • Past Medical History: » Coronary Artery Disease » Hypertension » Moderate Dementia • Allergies: No Known Drug Allergies • Medications: (grandson believes he remembers these) » » 10/7/2020 Metoprolol Donepezil Aspirin 81 mg Simvastatin 9
Case One – Mr. S » Physical Exam: BP 130/70, Pulse 76, Respirations 18, Oxygen Saturation 96% on room air, afebrile • Patient slightly confused (this is change from baseline according to grandson) • Pupils equal/round/reactive to light, moist mucous membranes • Regular S 1 S 2, no murmurs/rubs/gallops • Some very mild crackles at right base otherwise clear, normal work of breathing • Rest of exam: unremarkable 10/7/2020 10
Case One – Mr. S » Labs: White Blood Cells: 10. 0 (Differential: neutrophils 8. 7, lymphocytes 1. 0, eosinophils 0. 3) Hemoglobin: 12. 0 Hematocrit: 36. 0 Platelets: 350 » Blood chemistry: within normal limits » Chest X-ray: Possible developing right lower lobe infiltrate vs. atelactasis. Clinical correlation recommended. 10/7/2020 11
Case One – Mr. S • Pneumonia Severity Index score: 105 points --- Risk Class IV – approximately 9% mortality • You recommend hospitalization ---- but • Grandson states he is health care power of attorney and patient would not wish to be hospitalized. He wishes to take patient home and care for him there. Patient is confused but agreeable. • You prescribe course of Levofloxacin and ask that they see their provider on Monday 10/7/2020 12
Case One - Resolution • Patient goes home and does well for 3 days • He does so well, family does not follow-up with primary care provider on Monday • Tuesday evening: Patient returns with skin bruising and blood in his urine. » Platelets: within normal limit » INR: 7. 2 • When the patient’s pills are brought from home, it is discovered he is taking warfarin 10/7/2020 13
Case One – Breakdown • What went well? • What could have gone better? 10/7/2020 14
Transitional Care • Definition: “A set of actions designed to ensure the coordination and continuity of healthcare as patients transfer between different locations or different levels of care within the same institution. ” –American Geriatrics Society (2003) 10/7/2020 15
Transitional Care • During transitions, patients are at risk for: • • 10/7/2020 Medical errors Service duplication Inappropriate care Critical elements of care plan “falling though the cracks” -AGS (2003) 16
Transitional Care • Conceptual model of effective transitional care (Coleman 2003): • Communication between sending and receiving clinicians • Preparation of the caregiver and patient for transition • Reconciliation of medication lists • Arranging a plan for follow-up of outstanding tests • Arranging an appointment with receiving physician • Discussing warning signs that might necessitate more emergent evaluation 10/7/2020 17
How to Improve Transitional Care • Suggestions: » Changes to health care delivery systems (i. e. use of nurses to follow patients and/or expanding Program of All-Inclusive Care of the Elderly programs) » Adoption of information transfer technology » Changes to health care policy (i. e. pay for coordination of care or make providers responsible for coordinating transitional care) 10/7/2020 18
How to Improve Transitional Care • Society for Academic Emergency Medicine (SAEM) Geriatric Task Force: » Developed at recommendation of SAEM and American College of Emergency Medicine » Identified and adopted quality measures to allow assessment of care provided to elderly patients » Quality measures were vetted by/at: • SAEM Geriatric Task Force • SAEM annual meeting • American Geriatric Society annual meeting 10/7/2020 19
How to Improve Transitional Care • Quality Measures 1 -4: * » If nursing home patient goes to emergency department, then paperwork should state: • • Reason for Transfer Code Status Medication Allergies Contact Information for: » Nursing home » Primary care or on-call MD » Resident’s health care power of attorney or closest family member *Terrell et al. Quality Indicators for Geriatric Emergency Care. Academic Emergency Medicine 2009; 16: 441 -449. 10/7/2020 20
How to Improve Transitional Care • Quality Measures 5 -6: » If nursing home patient goes to emergency department, then paperwork should include: • Patient’s medication administration record » If nursing home patient goes to emergency room for requested studies, then: • Document the performance of requested tests or the reason why such tests were not performed 10/7/2020 21
How to Improve Transitional Care • Quality Measures 7 -9: » If nursing home patient goes to emergency department and then will be released from the emergency department, then: • Emergency department provider should speak with the nursing home provider, primary care or on-call MD for the nursing home prior to discharge from the emergency department » If nursing home patient goes to emergency department and then will be released from the emergency department, then written paperwork should state: • Emergency department diagnosis • Tests performed with results (and tests with pending results) 10/7/2020 22
How to Improve Transitional Care • Quality Measures 10 -11 » If nursing home patient goes to emergency department and then is released back to the nursing home, then: • The patient should receive the recommended follow-up • The recommended changes to the patient’s medications or plan of care should be followed (or the reason why not followed documented) 10/7/2020 23
Case 2 – Mrs. J • Mrs. J: Saturday morning, 4 am » 92 year old woman who presents from local nursing home for “evaluation of increasingly combative behavior” » Past Medical History: • Parkinsonism • Diabetes • Urinary incontinence • Chronic back pain secondary to osteoarthritis and degenerative joint disease » Little accompanying paperwork --- no medication administration record » Call to the facility --- the staff who are there don’t know the patient --- they give you son’s phone number 10/7/2020 24
Case 2 – Mrs. J • Vital Signs: Blood pressure 124/78, Pulse 84, Respirations 16, afebrile » Elderly woman lying on stretcher. Awake, but does not interact much with you or other staff » Remainder exam: within normal limits » Labs and urinalysis: unrevealing • Reach son – he is thankful and says he will be over in about 1 hour • Patient awakens and starts to pull at lines --- request is made for risperidone 1. 0 mg • Patient receives risperidone, calms down, and eventually goes to sleep 10/7/2020 25
Case 2 – Mrs. J • Son arrives --- you offer hospitalization – he says that this is not what his mother would want. • He asks she be transferred back to the nursing home and that you provide a prescription for risperidone. • What do you do? 10/7/2020 26
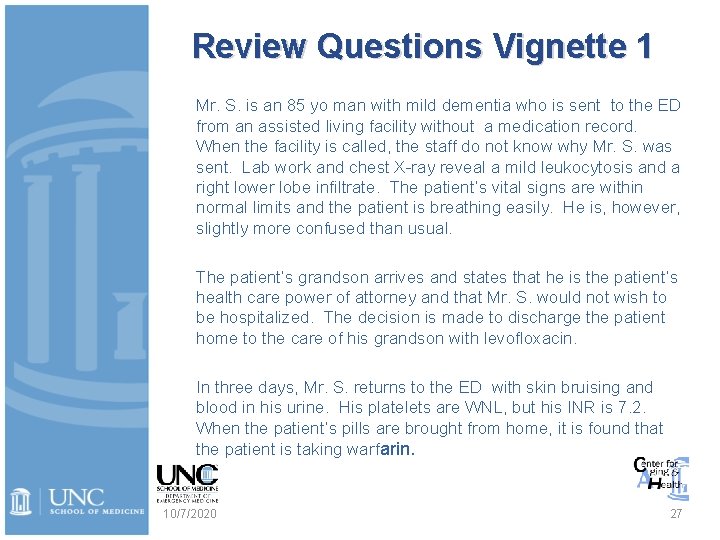
Review Questions Vignette 1 Mr. S. is an 85 yo man with mild dementia who is sent to the ED from an assisted living facility without a medication record. When the facility is called, the staff do not know why Mr. S. was sent. Lab work and chest X-ray reveal a mild leukocytosis and a right lower lobe infiltrate. The patient’s vital signs are within normal limits and the patient is breathing easily. He is, however, slightly more confused than usual. The patient’s grandson arrives and states that he is the patient’s health care power of attorney and that Mr. S. would not wish to be hospitalized. The decision is made to discharge the patient home to the care of his grandson with levofloxacin. In three days, Mr. S. returns to the ED with skin bruising and blood in his urine. His platelets are WNL, but his INR is 7. 2. When the patient’s pills are brought from home, it is found that the patient is taking warfarin. 10/7/2020 27
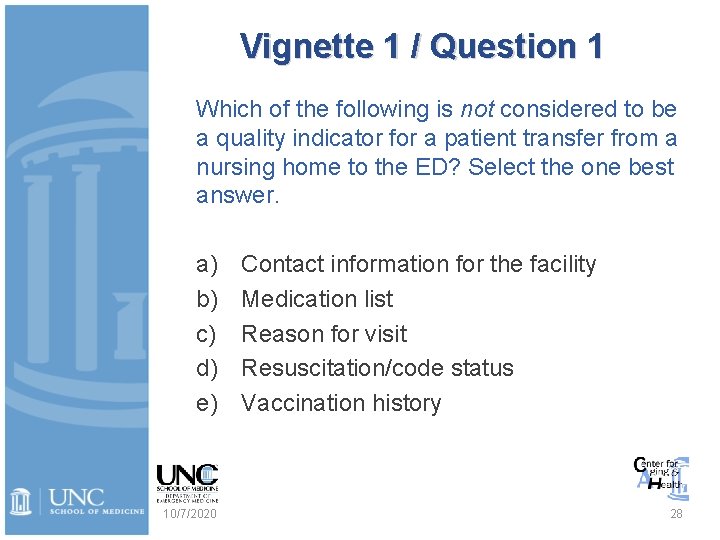
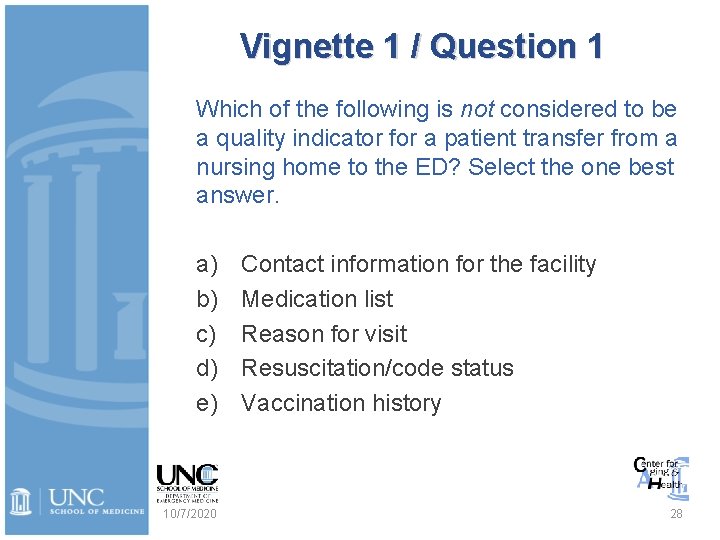
Vignette 1 / Question 1 Which of the following is not considered to be a quality indicator for a patient transfer from a nursing home to the ED? Select the one best answer. a) b) c) d) e) 10/7/2020 Contact information for the facility Medication list Reason for visit Resuscitation/code status Vaccination history 28
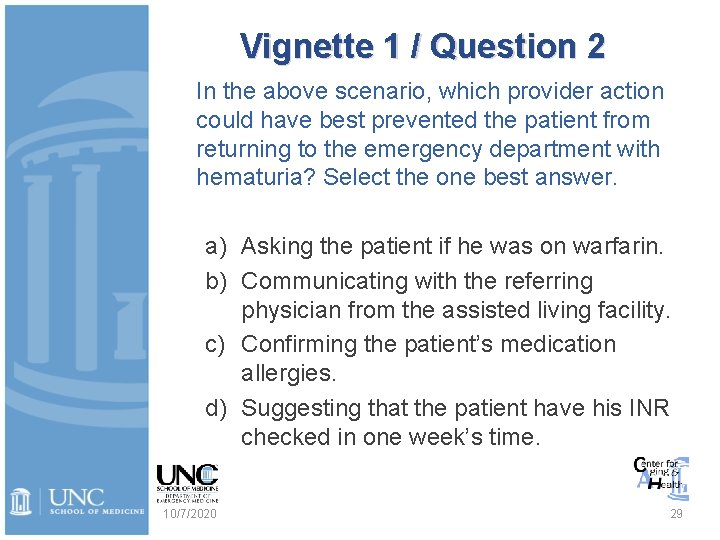
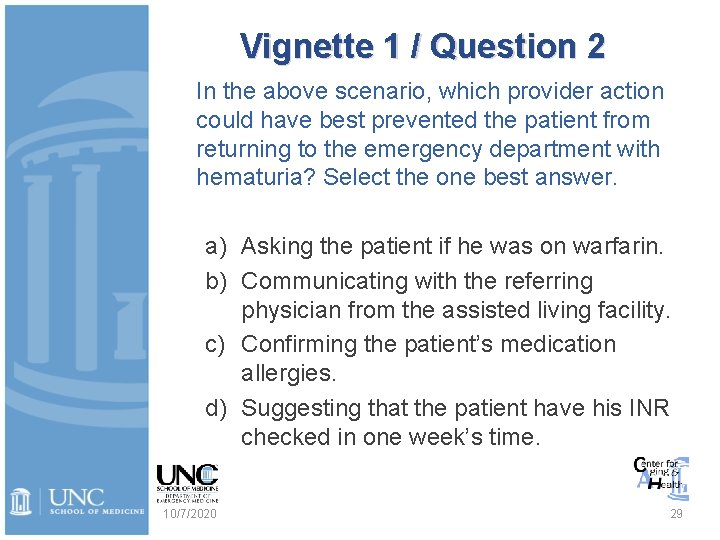
Vignette 1 / Question 2 In the above scenario, which provider action could have best prevented the patient from returning to the emergency department with hematuria? Select the one best answer. a) Asking the patient if he was on warfarin. b) Communicating with the referring physician from the assisted living facility. c) Confirming the patient’s medication allergies. d) Suggesting that the patient have his INR checked in one week’s time. 10/7/2020 29
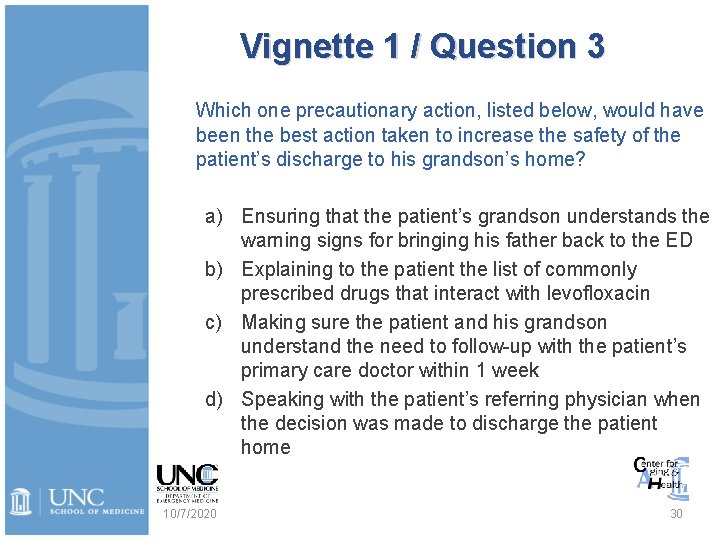
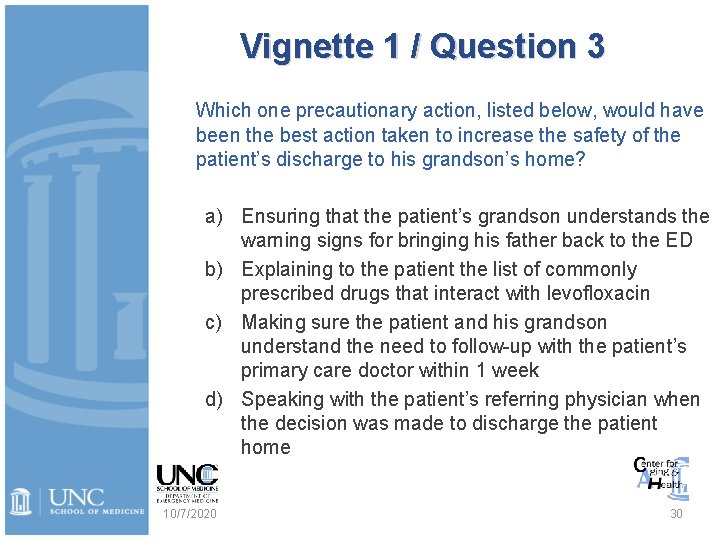
Vignette 1 / Question 3 Which one precautionary action, listed below, would have been the best action taken to increase the safety of the patient’s discharge to his grandson’s home? a) Ensuring that the patient’s grandson understands the warning signs for bringing his father back to the ED b) Explaining to the patient the list of commonly prescribed drugs that interact with levofloxacin c) Making sure the patient and his grandson understand the need to follow-up with the patient’s primary care doctor within 1 week d) Speaking with the patient’s referring physician when the decision was made to discharge the patient home 10/7/2020 30
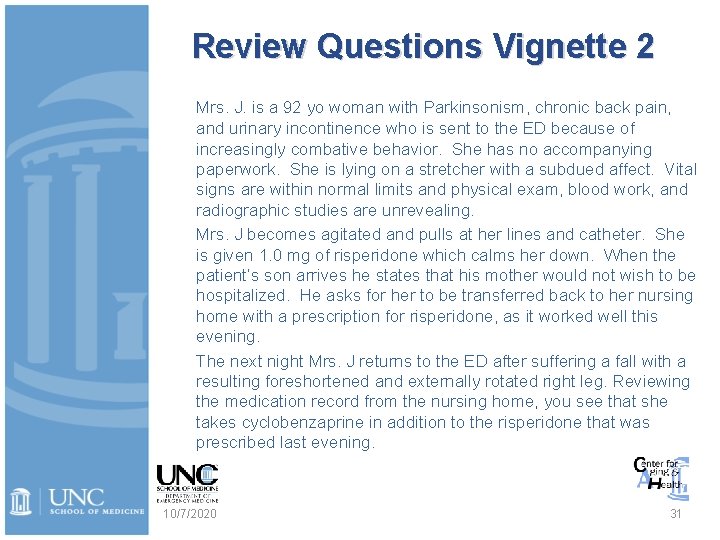
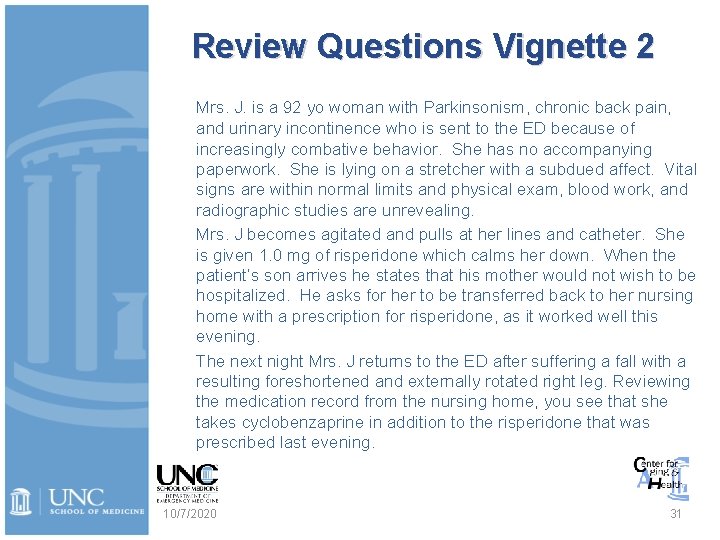
Review Questions Vignette 2 Mrs. J. is a 92 yo woman with Parkinsonism, chronic back pain, and urinary incontinence who is sent to the ED because of increasingly combative behavior. She has no accompanying paperwork. She is lying on a stretcher with a subdued affect. Vital signs are within normal limits and physical exam, blood work, and radiographic studies are unrevealing. Mrs. J becomes agitated and pulls at her lines and catheter. She is given 1. 0 mg of risperidone which calms her down. When the patient’s son arrives he states that his mother would not wish to be hospitalized. He asks for her to be transferred back to her nursing home with a prescription for risperidone, as it worked well this evening. The next night Mrs. J returns to the ED after suffering a fall with a resulting foreshortened and externally rotated right leg. Reviewing the medication record from the nursing home, you see that she takes cyclobenzaprine in addition to the risperidone that was prescribed last evening. 10/7/2020 31
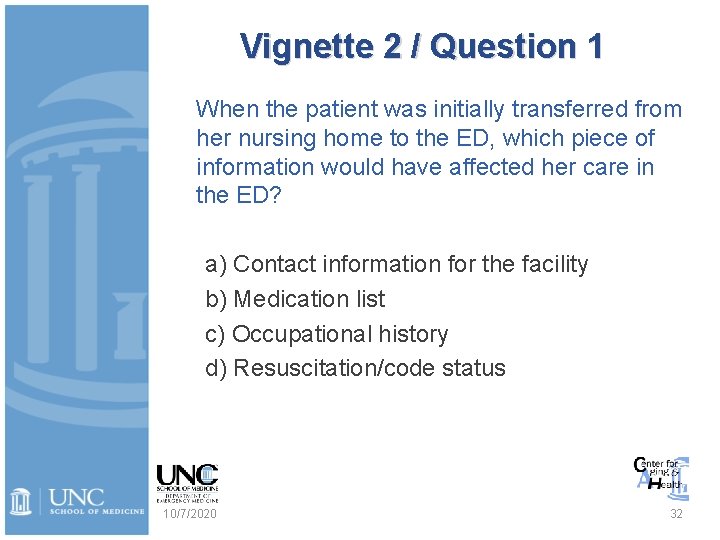
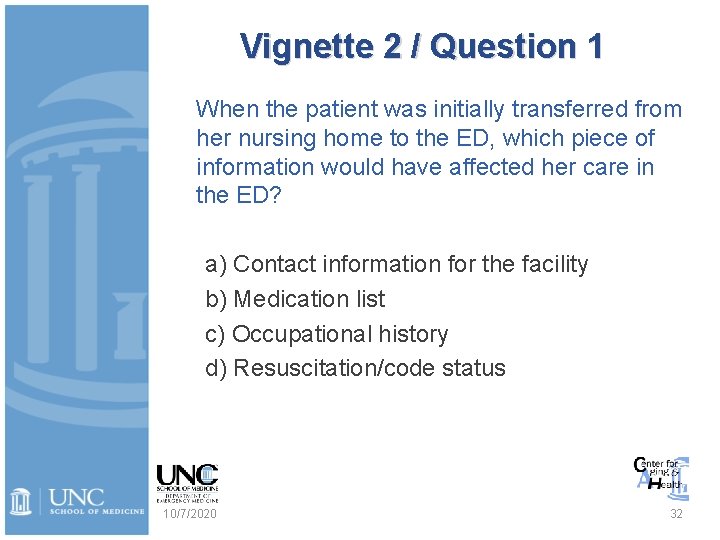
Vignette 2 / Question 1 When the patient was initially transferred from her nursing home to the ED, which piece of information would have affected her care in the ED? a) Contact information for the facility b) Medication list c) Occupational history d) Resuscitation/code status 10/7/2020 32
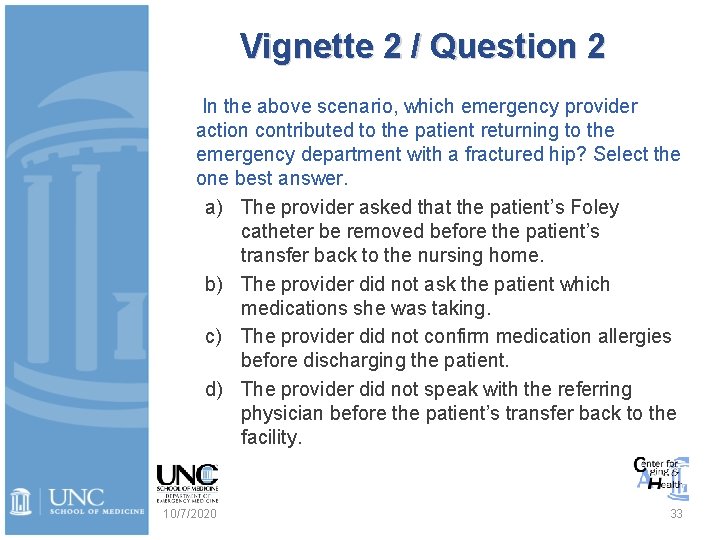
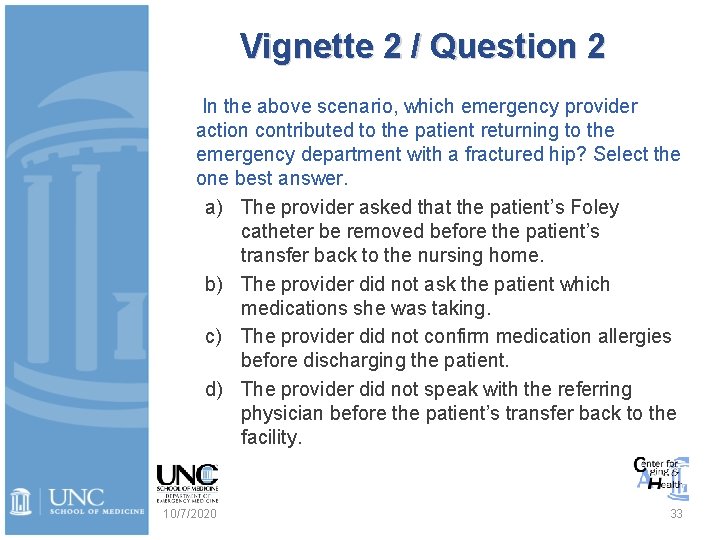
Vignette 2 / Question 2 In the above scenario, which emergency provider action contributed to the patient returning to the emergency department with a fractured hip? Select the one best answer. a) The provider asked that the patient’s Foley catheter be removed before the patient’s transfer back to the nursing home. b) The provider did not ask the patient which medications she was taking. c) The provider did not confirm medication allergies before discharging the patient. d) The provider did not speak with the referring physician before the patient’s transfer back to the facility. 10/7/2020 33
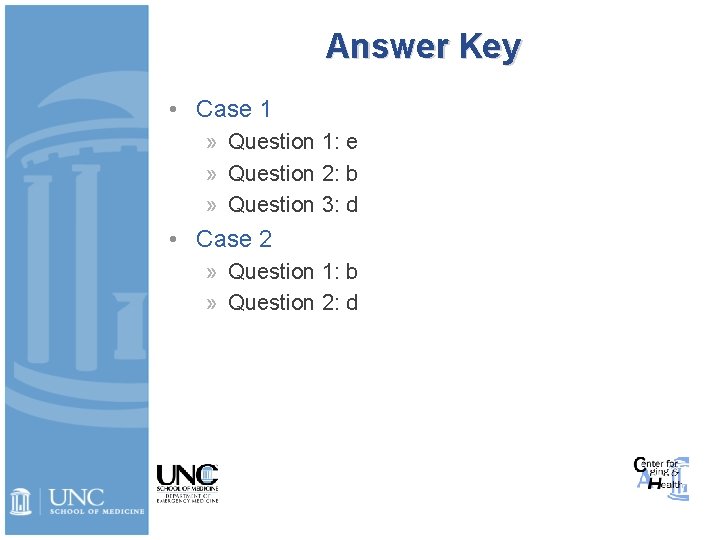
Answer Key • Case 1 » Question 1: e » Question 2: b » Question 3: d • Case 2 » Question 1: b » Question 2: d
Acknowledgements and Disclaimer This project was supported by funds from the American Geriatrics Society/John A. Hartford Geriatrics for Specialists Grant. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the American Geriatrics Society or John A. Hartford Foundation. The UNC Center for Aging and Health and UNC Department of Emergency Medicine also provided support for this activity. This work was compiled and edited through the efforts of Jennifer Link, BA.
• Copyright © 2011 The University of North Carolina School of Medicine at Chapel Hill 10/7/2020 36