Transition to 2021 EM Medical Coding Presented By
Transition to 2021 E/M Medical Coding Presented By: Brenda L. Whyte, RHIT, CPC UW Health Compliance Education Coordinator AAPC Local Chapter Meeting November 19, 2020
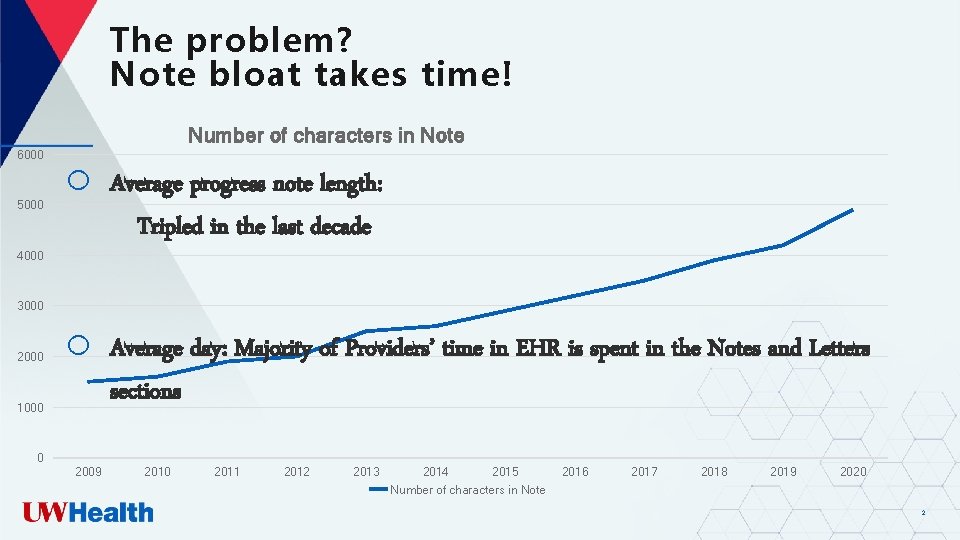
The problem? Note bloat takes time! Number of characters in Note 6000 5000 o Average progress note length: Tripled in the last decade o Average day: Majority of Providers’ time in EHR is spent in the Notes and Letters sections 4000 3000 2000 1000 0 2009 2010 2011 2012 2013 2014 2015 Number of characters in Note 2016 2017 2018 2019 2020 2
Overview of 2021 Changes o o o Implementation Date: January 1, 2021 Supported by both CMS and AMA The most significant change to E/M documentation requirements in 25 years Objectives for the new E/M documentation requirements: • Simplify code level selection • Reduce repetitive clinical documentation in medical record • Reduce clinician burnout ü Administrative burden due to “note bloat” and the time it takes to document in the medical record 3
What is changing? The new AMA CPT E/M changes are specific only to Office or Other Outpatient Services (99201 -99205 and 99211 -99215) codes o o o Deletion of 99201 New guidelines specific to 99202 -99215 Changes in component scoring for both new and established patient codes (99202 -99215) Changes to the medical decision-making table Changes to the typical times associated with each E/M code (99202 -99215) 4
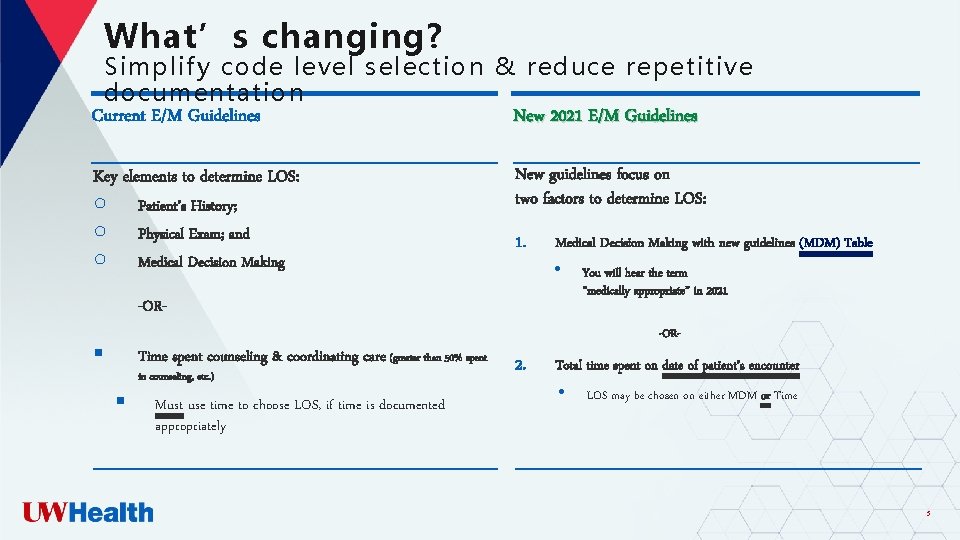
What’s changing? Simplify code level selection & reduce repetitive documentation Current E/M Guidelines New 2021 E/M Guidelines Key elements to determine LOS: ○ ○ ○ Patient’s History; Physical Exam; and Medical Decision Making New guidelines focus on two factors to determine LOS: 1. Medical Decision Making with new guidelines (MDM) Table • -OR- You will hear the term “medically appropriate” in 2021 -OR- § Time spent counseling & coordinating care (greater than 50% spent § in counseling, etc. ) Must use time to choose LOS, if time is documented appropriately 2. Total time spent on date of patient’s encounter • LOS may be chosen on either MDM or Time 5
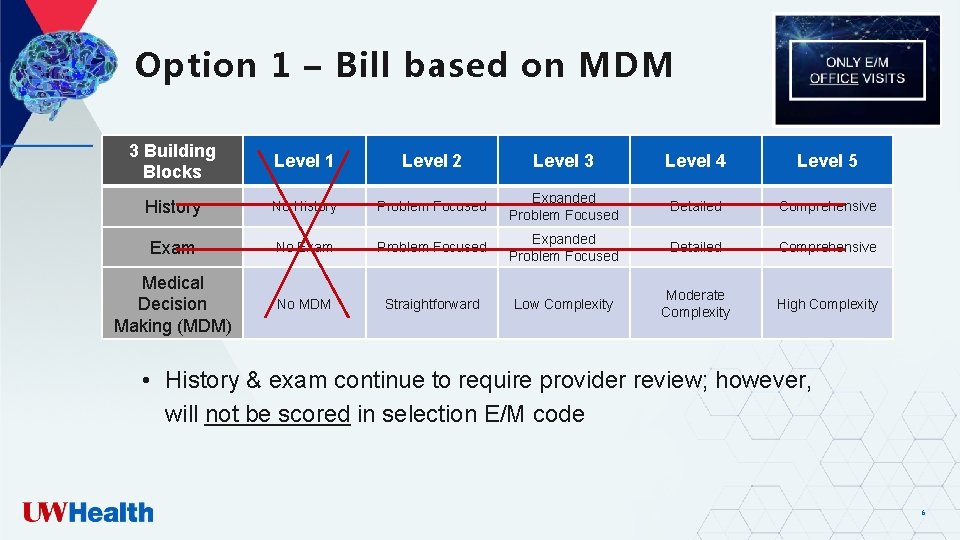
Option 1 – Bill based on MDM 3 Building Blocks Level 1 Level 2 Level 3 Level 4 Level 5 History No History Problem Focused Expanded Problem Focused Detailed Comprehensive Exam No Exam Problem Focused Expanded Problem Focused Detailed Comprehensive Medical Decision Making (MDM) No MDM Straightforward Low Complexity Moderate Complexity High Complexity • History & exam continue to require provider review; however, will not be scored in selection E/M code 6
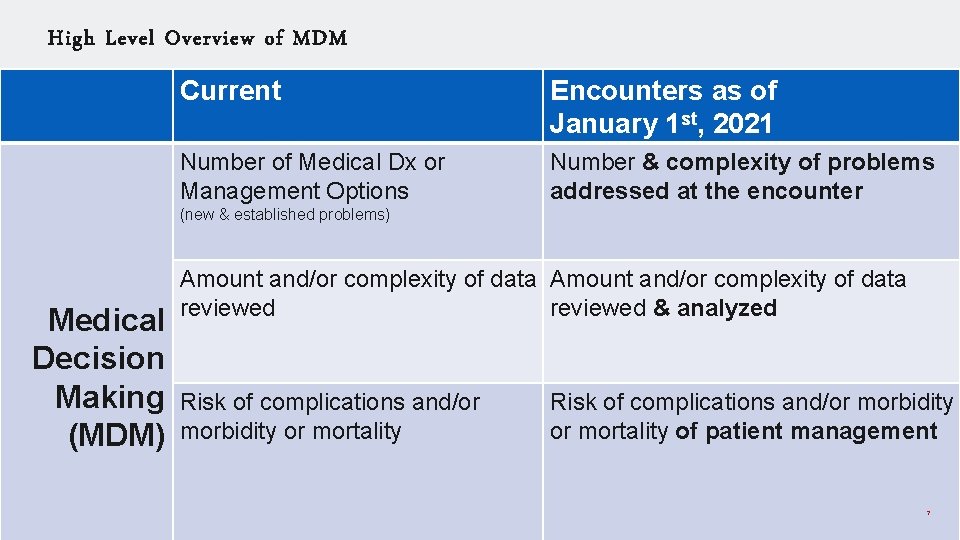
High Level Overview of MDM Current Encounters as of January 1 st, 2021 Number of Medical Dx or Management Options Number & complexity of problems addressed at the encounter (new & established problems) Medical Decision Making (MDM) Amount and/or complexity of data reviewed & analyzed Risk of complications and/or morbidity or mortality of patient management 7
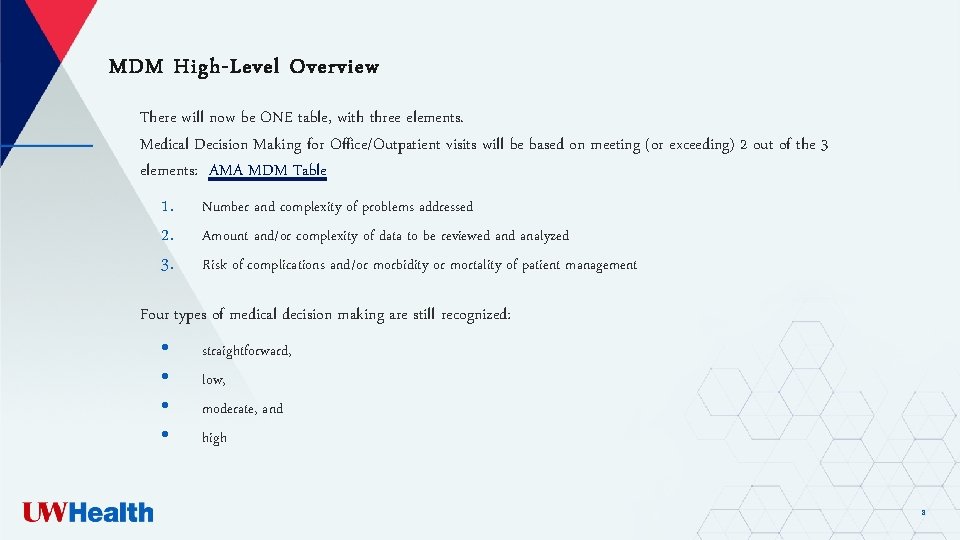
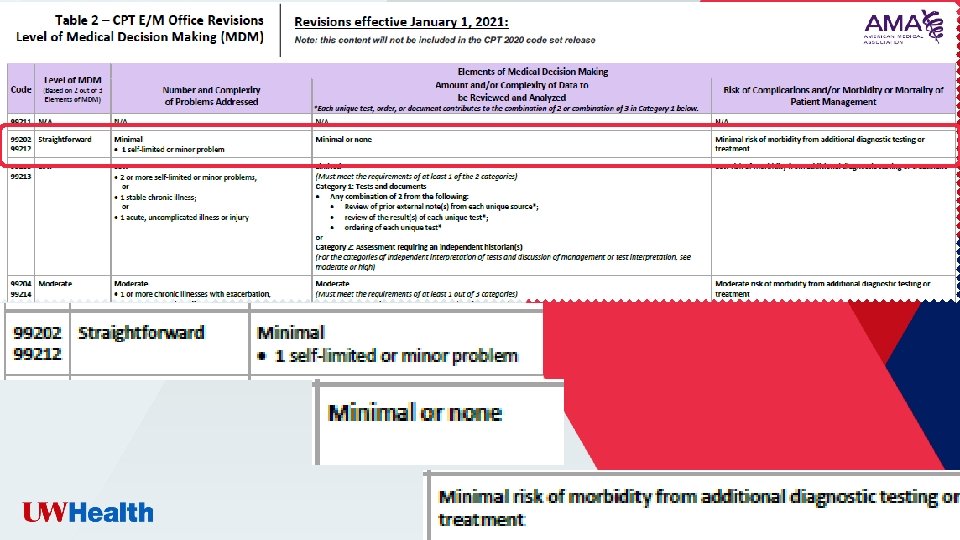
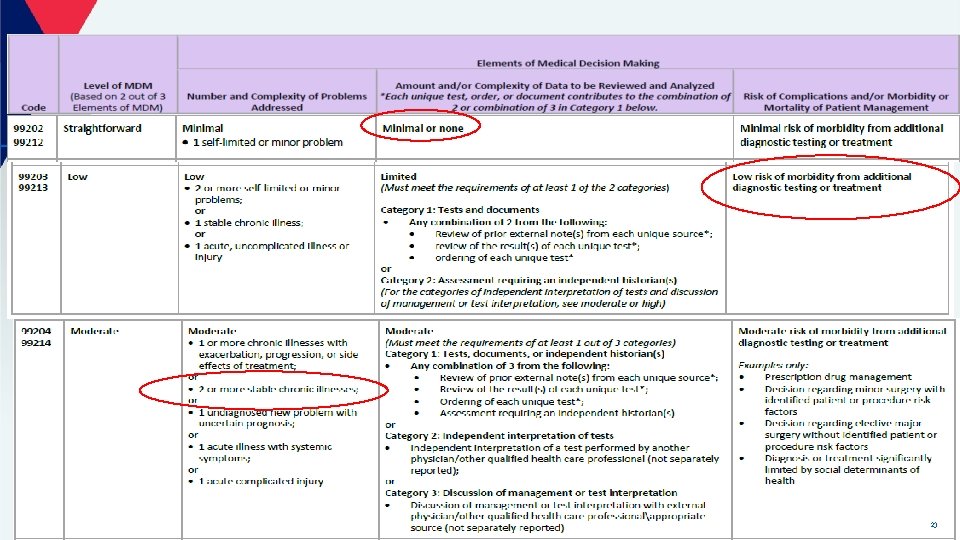
MDM High-Level Overview There will now be ONE table, with three elements. Medical Decision Making for Office/Outpatient visits will be based on meeting (or exceeding) 2 out of the 3 elements: AMA MDM Table 1. 2. 3. Number and complexity of problems addressed Amount and/or complexity of data to be reviewed analyzed Risk of complications and/or morbidity or mortality of patient management Four types of medical decision making are still recognized: • • straightforward, low, moderate, and high 8
9
Medical-Decision-Making (MDM) Component New Definitions 3 elements to MDM; must meet 2/3 1. Number & Complexity of Problems Addressed • Clearly document relevance to the encounter • Address the patient’s problems in Problem List “Blown in” problem lists not sufficient 10
Medical-Decision-Making (MDM) Component New Definitions 3 elements to MDM; must meet 2/3 2. Amount &/or Complexity of Data Reviewed & • Clearly document data analyzed & relevance to encounter Analyzed • Review of prior external note(s) from each unique source* • • • (documentation outside your specialty) Review of the result(s) of each unique test* (individual lab, radiology, etc. ) Ordering of each unique test* (individual lab, radiology, etc. ) Independent Interpretation of Tests (not separately reported) Assessment requiring independent historian (caregiver, parent) Discussion of Management or Test Interpretation with External Provider(s) (not separately reported) Not sufficient: Copy & Pasted reports without analysis 11
Medical-Decision-Making (MDM) Component New Definitions Risk of Complications &/or must meet 2/3 33. elements to MDM; Morbidity or Mortality of Patient Management • New: Includes possible management options selected and those • • considered, but not selected New: Addresses risks associated with social determinants of health Examples: (not an all-inclusive list) • Prescription drug management • Decision regarding minor surgery with identified patient or procedure risk factors • Diagnosis or treatment significantly limited by social determinants of health (need to order a prescription but patient has no insurance) • Drug therapy requiring intensive monitoring for toxicity • Decision regarding emergency major surgery • Decision regarding hospitalization 12
13
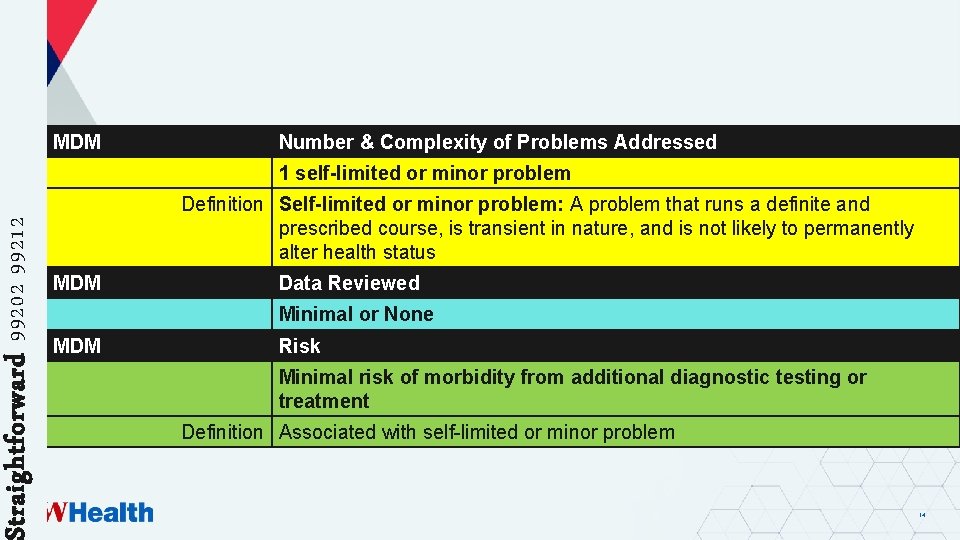
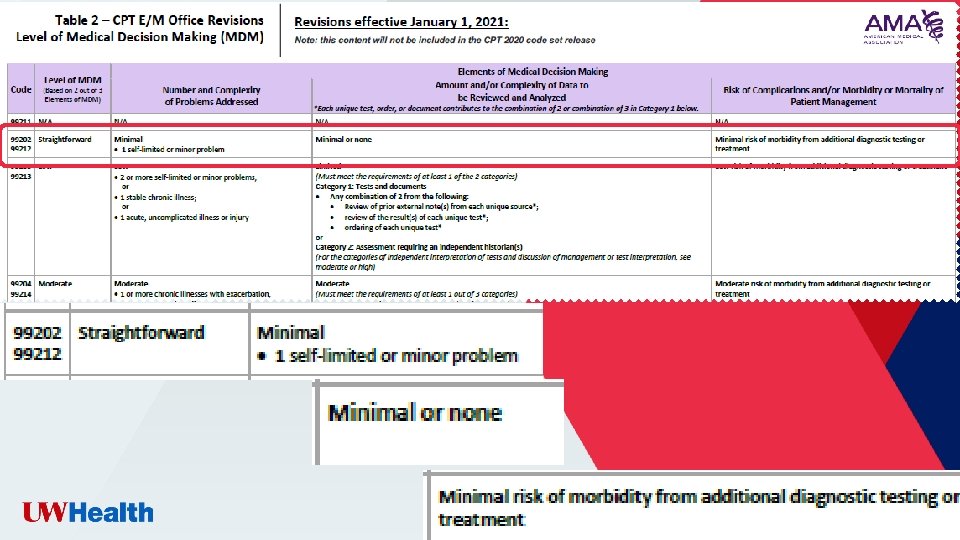
Straightforward 99202 99212 MDM Number & Complexity of Problems Addressed 1 self-limited or minor problem Definition Self-limited or minor problem: A problem that runs a definite and prescribed course, is transient in nature, and is not likely to permanently alter health status MDM Data Reviewed Minimal or None MDM Risk Minimal risk of morbidity from additional diagnostic testing or treatment Definition Associated with self-limited or minor problem 14
15
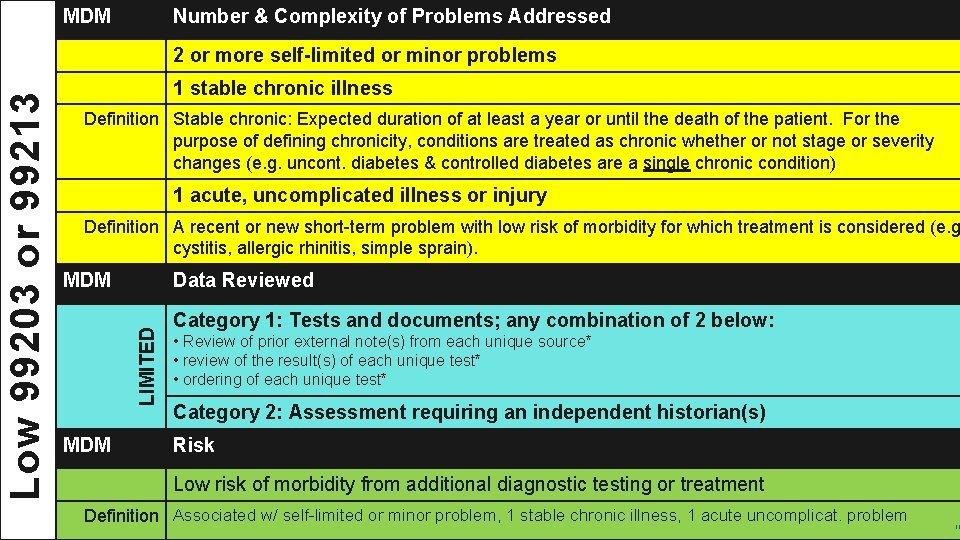
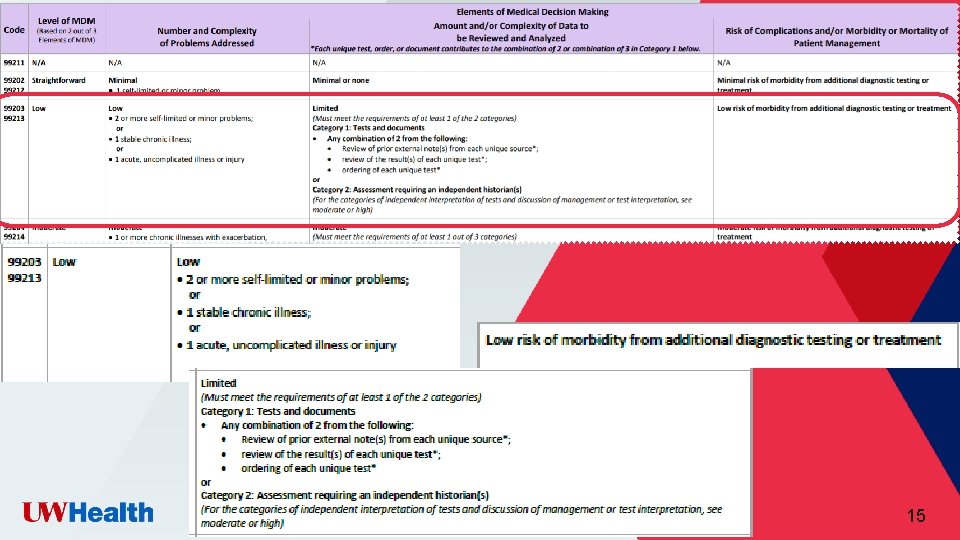
MDM Number & Complexity of Problems Addressed 1 stable chronic illness Definition Stable chronic: Expected duration of at least a year or until the death of the patient. For the purpose of defining chronicity, conditions are treated as chronic whether or not stage or severity changes (e. g. uncont. diabetes & controlled diabetes are a single chronic condition) 1 acute, uncomplicated illness or injury Definition A recent or new short-term problem with low risk of morbidity for which treatment is considered (e. g cystitis, allergic rhinitis, simple sprain). MDM Data Reviewed LIMITED Low 99203 or 99213 2 or more self-limited or minor problems MDM Category 1: Tests and documents; any combination of 2 below: • Review of prior external note(s) from each unique source* • review of the result(s) of each unique test* • ordering of each unique test* Category 2: Assessment requiring an independent historian(s) Risk Low risk of morbidity from additional diagnostic testing or treatment Definition Associated w/ self-limited or minor problem, 1 stable chronic illness, 1 acute uncomplicat. problem 16
17
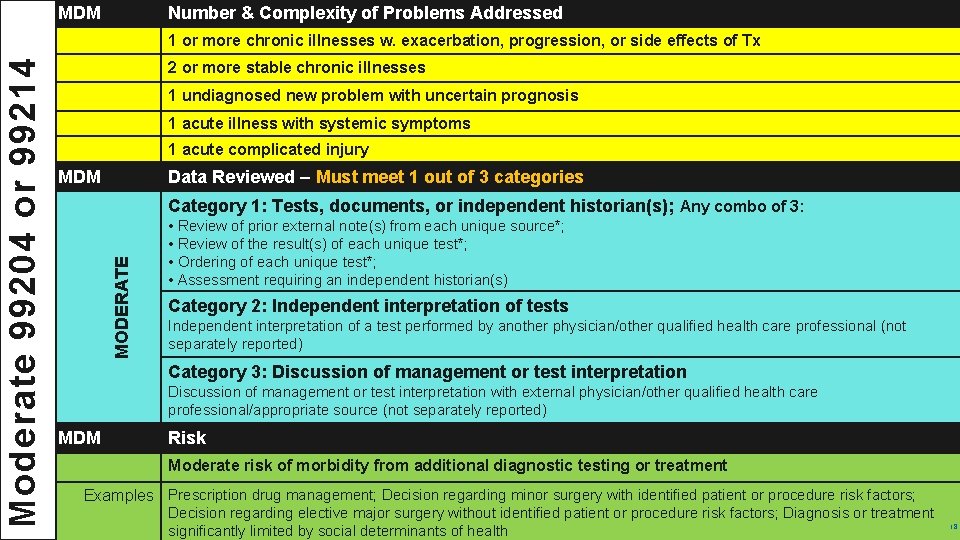
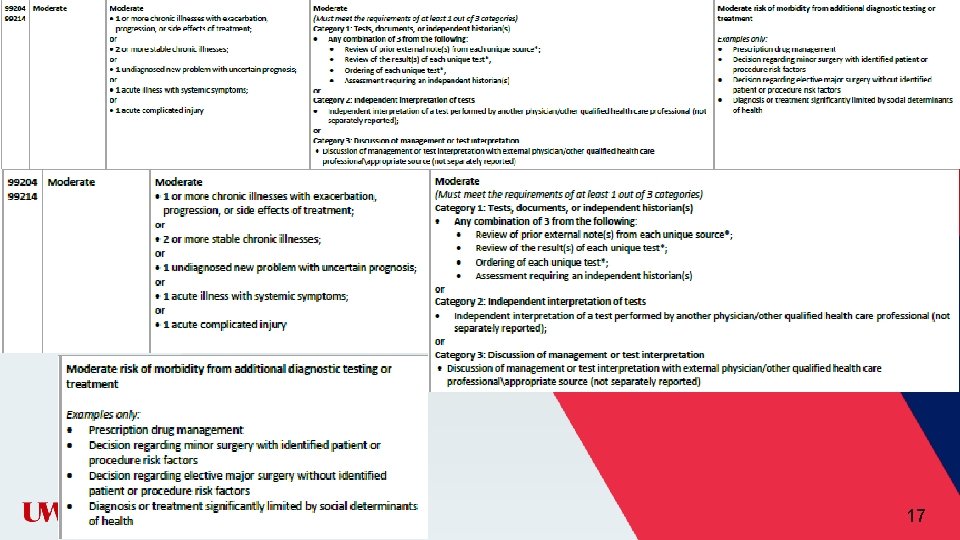
MDM Number & Complexity of Problems Addressed 2 or more stable chronic illnesses 1 undiagnosed new problem with uncertain prognosis 1 acute illness with systemic symptoms 1 acute complicated injury MDM Data Reviewed – Must meet 1 out of 3 categories Category 1: Tests, documents, or independent historian(s); Any combo of 3: MODERATE Moderate 99204 or 99214 1 or more chronic illnesses w. exacerbation, progression, or side effects of Tx • Review of prior external note(s) from each unique source*; • Review of the result(s) of each unique test*; • Ordering of each unique test*; • Assessment requiring an independent historian(s) Category 2: Independent interpretation of tests Independent interpretation of a test performed by another physician/other qualified health care professional (not separately reported) Category 3: Discussion of management or test interpretation with external physician/other qualified health care professional/appropriate source (not separately reported) MDM Risk Moderate risk of morbidity from additional diagnostic testing or treatment Examples Prescription drug management; Decision regarding minor surgery with identified patient or procedure risk factors; Decision regarding elective major surgery without identified patient or procedure risk factors; Diagnosis or treatment significantly limited by social determinants of health 18
19
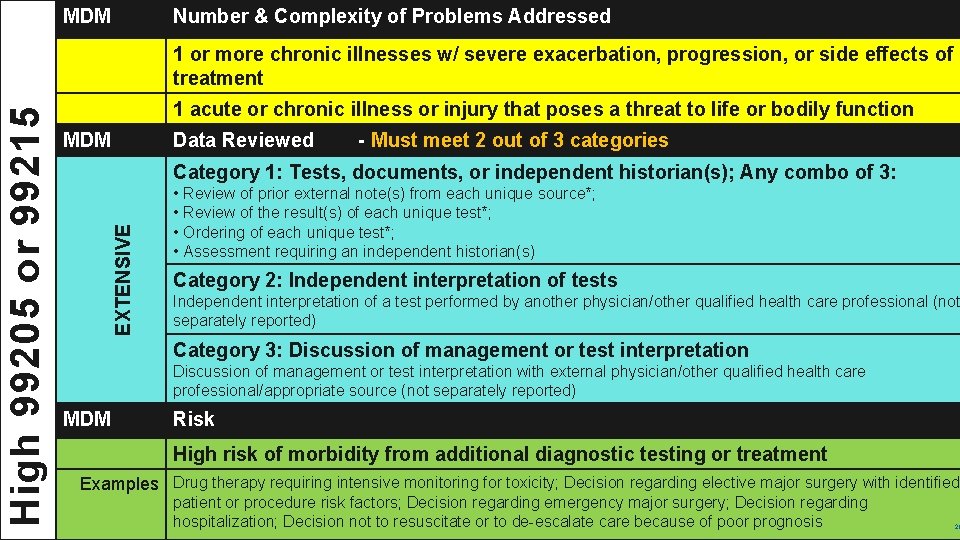
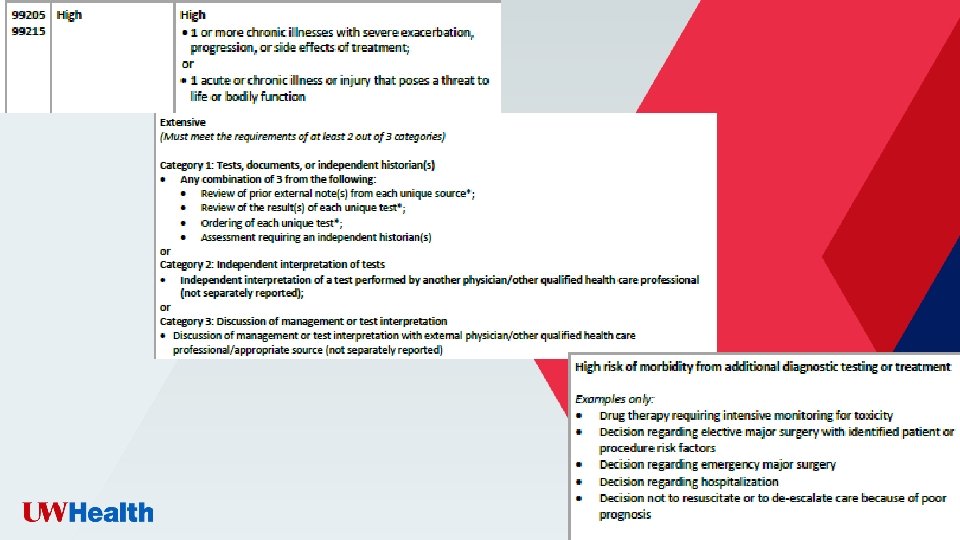
MDM Number & Complexity of Problems Addressed 1 acute or chronic illness or injury that poses a threat to life or bodily function MDM Data Reviewed - Must meet 2 out of 3 categories Category 1: Tests, documents, or independent historian(s); Any combo of 3: EXTENSIVE High 99205 or 99215 1 or more chronic illnesses w/ severe exacerbation, progression, or side effects of treatment • Review of prior external note(s) from each unique source*; • Review of the result(s) of each unique test*; • Ordering of each unique test*; • Assessment requiring an independent historian(s) Category 2: Independent interpretation of tests Independent interpretation of a test performed by another physician/other qualified health care professional (not separately reported) Category 3: Discussion of management or test interpretation with external physician/other qualified health care professional/appropriate source (not separately reported) MDM Risk High risk of morbidity from additional diagnostic testing or treatment Examples Drug therapy requiring intensive monitoring for toxicity; Decision regarding elective major surgery with identified patient or procedure risk factors; Decision regarding emergency major surgery; Decision regarding hospitalization; Decision not to resuscitate or to de-escalate care because of poor prognosis 20
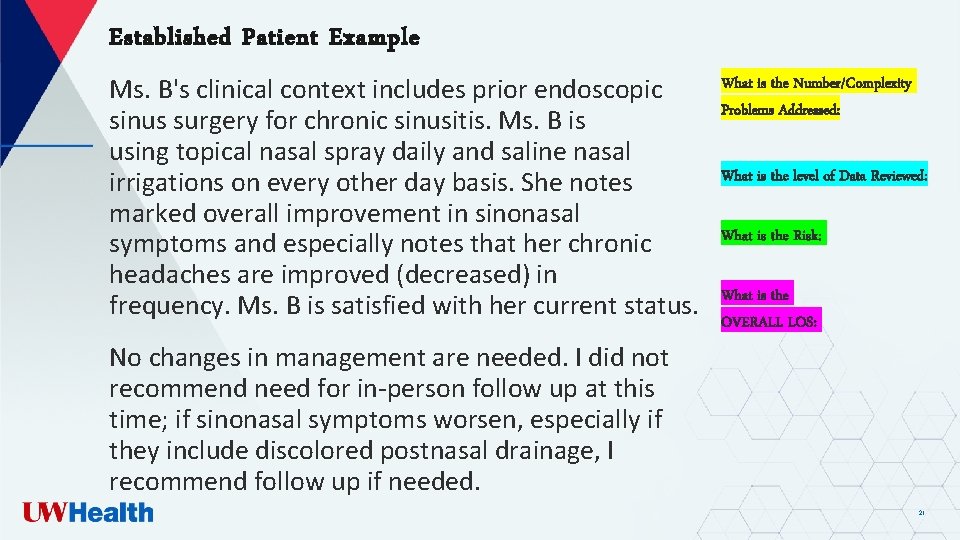
Established Patient Example Ms. B's clinical context includes prior endoscopic sinus surgery for chronic sinusitis. Ms. B is using topical nasal spray daily and saline nasal irrigations on every other day basis. She notes marked overall improvement in sinonasal symptoms and especially notes that her chronic headaches are improved (decreased) in frequency. Ms. B is satisfied with her current status. No changes in management are needed. I did not recommend need for in-person follow up at this time; if sinonasal symptoms worsen, especially if they include discolored postnasal drainage, I recommend follow up if needed. What is the Number/Complexity Problems Addressed: What is the level of Data Reviewed: What is the Risk: What is the OVERALL LOS: 21
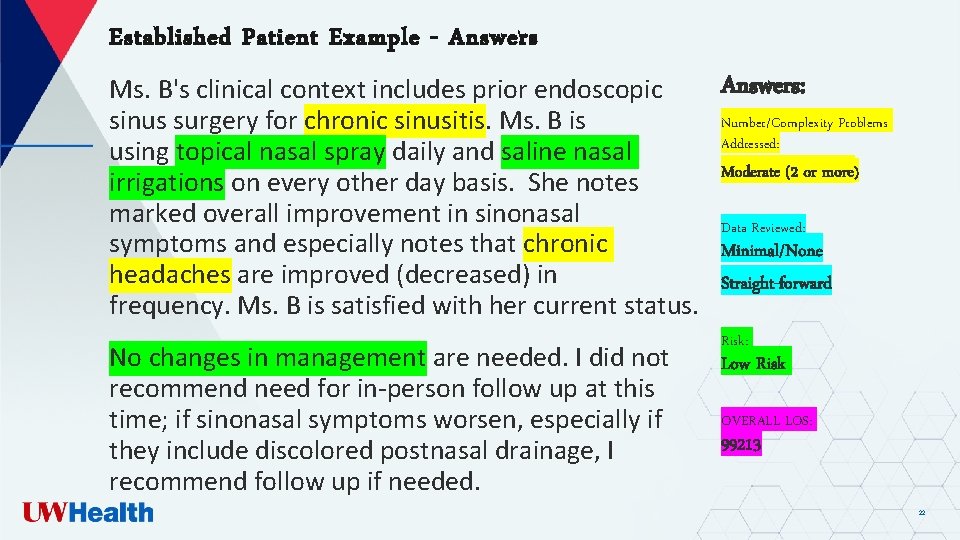
Established Patient Example - Answers: Ms. B's clinical context includes prior endoscopic Number/Complexity Problems sinus surgery for chronic sinusitis. Ms. B is Addressed: using topical nasal spray daily and saline nasal Moderate (2 or more) irrigations on every other day basis. She notes marked overall improvement in sinonasal Data Reviewed: symptoms and especially notes that chronic Minimal/None headaches are improved (decreased) in Straight-forward frequency. Ms. B is satisfied with her current status. No changes in management are needed. I did not recommend need for in-person follow up at this time; if sinonasal symptoms worsen, especially if they include discolored postnasal drainage, I recommend follow up if needed. Risk: Low Risk OVERALL LOS: 99213 22
23 23
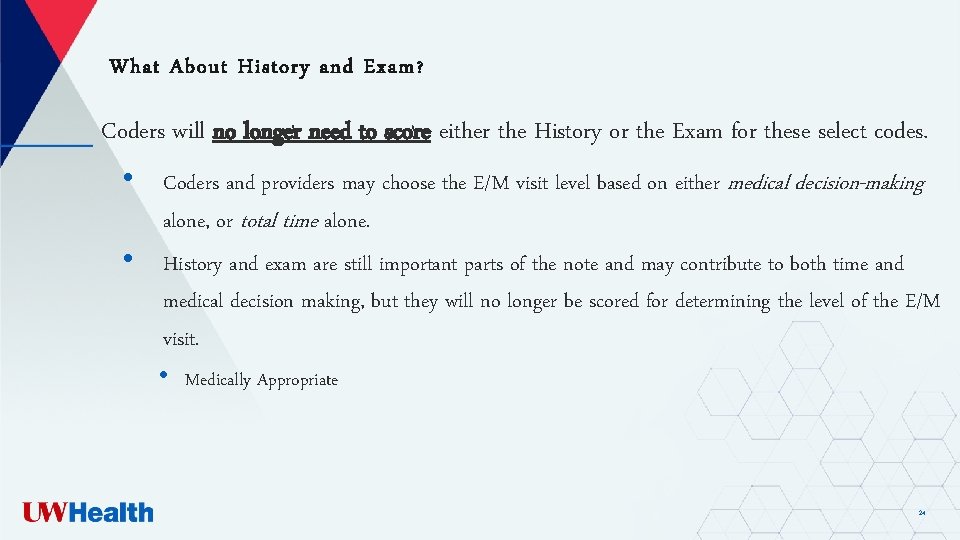
What About History and Exam ? Coders will no longer need to score either the History or the Exam for these select codes. • Coders and providers may choose the E/M visit level based on either medical decision-making alone, or total time alone. • History and exam are still important parts of the note and may contribute to both time and medical decision making, but they will no longer be scored for determining the level of the E/M visit. • Medically Appropriate 24

New Time Documentation Requirements 25
Option 2 – Bill based on Time Now includes total time spent on patient on the day of the encounter • Includes non-face-to face time associated with the visit on the same day prior to MIDNIGHT • BEFORE visit + DURING visit + AFTER visit = TOTAL TIME • Recommended time statement: Total time spent caring for the patient on the day of the encounter was *** minutes. • Counseling does not have to dominate the visit • There are no history and/or exam requirements 26
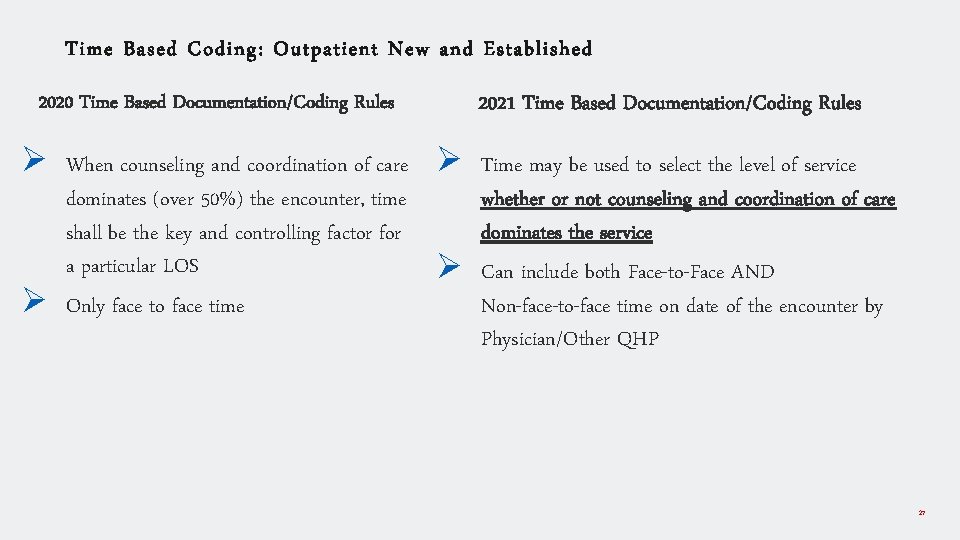
Time Based Coding: Outpatient New and Established 2021 Time Based Documentation/Coding Rules 2020 Time Based Documentation/Coding Rules Ø When counseling and coordination of care Ø Time may be used to select the level of service Ø dominates (over 50%) the encounter, time shall be the key and controlling factor for a particular LOS Only face to face time Ø whether or not counseling and coordination of care dominates the service Can include both Face-to-Face AND Non-face-to-face time on date of the encounter by Physician/Other QHP 27
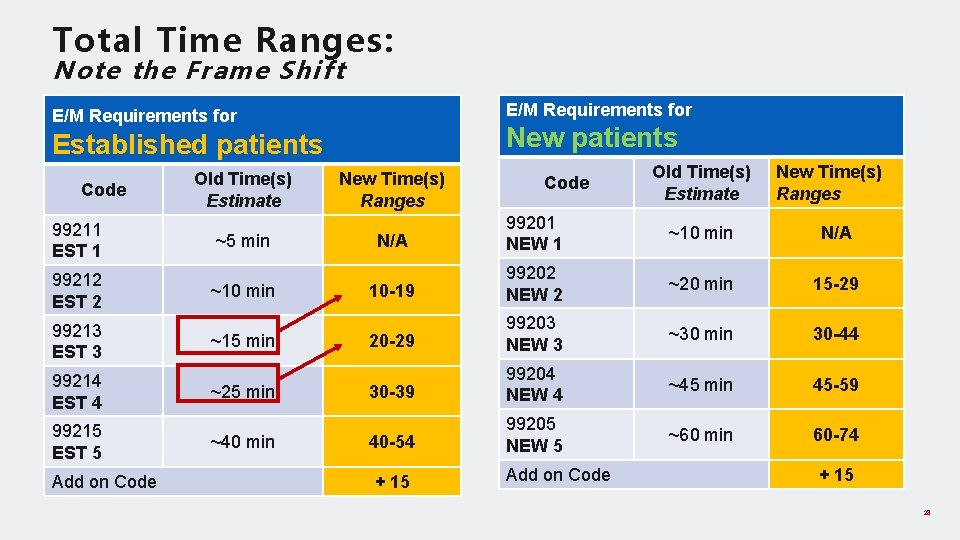
Total Time Ranges: Note the Frame Shift E/M Requirements for New patients Established patients Code 99211 EST 1 99212 EST 2 99213 EST 3 99214 EST 4 99215 EST 5 Add on Code Old Time(s) Estimate ~5 min ~10 min ~15 min ~25 min ~40 min New Time(s) Ranges Code Old Time(s) Estimate New Time(s) Ranges N/A 99201 NEW 1 ~10 min N/A 10 -19 99202 NEW 2 ~20 min 15 -29 20 -29 99203 NEW 3 ~30 min 30 -44 30 -39 99204 NEW 4 ~45 min 45 -59 40 -54 99205 NEW 5 ~60 min 60 -74 + 15 Add on Code + 15 28

Time counts for any of the following as long as they are performed on same date as encounter : ü Preparing to see the patient (e. g. , review of the chart/tests) ü Obtaining & reviewing separately obtained history (history taken by RN, previously or for current encounter) ü • If seen the week before, may not be relevant to complete another exam but may review pertinent components Document what is important & relevant Counseling & educating the patient/family/caregiver Ordering medications, tests or procedures Referring & communicating with other health care professionals (when not reported separately) ü Performing a medically necessary exam and/or evaluation • ü ü ü Documenting clinical information in the electronic or other medical record • ü ü ü Is now included due to feedback obtained by providers regarding “PJ” time Independently interpreting results (not reported separately) Care coordination (not reported separately) Anything reported separately, do not count towards time 29
Established Time Example Dos: 04/07/2020 Reason for Visit: Chronic back and pelvic pain. Also, she wants to lose weight. OBJECTIVE: BP 109/69 | Pulse 71 | Resp 16 GEN: Alert, NAD ASSESSMENT/PLAN: I spent 25 minutes counseling and coordinating care regarding the diagnosis of chronic pain. Discussion included: Prognosis. Instructions for mgmt. (treatment) and/or follow up. Reviewed history of chronic pain. At this point we discussed bid/daily regimen to improve weight and hopefully this will be generally helpful to her with pain. She will continue with EMG as previously planned and from there will continue with pelvic floor pt and pain providers as she has been doing. Discussed also she could trial increased dose or frequency of gabapentin. 30
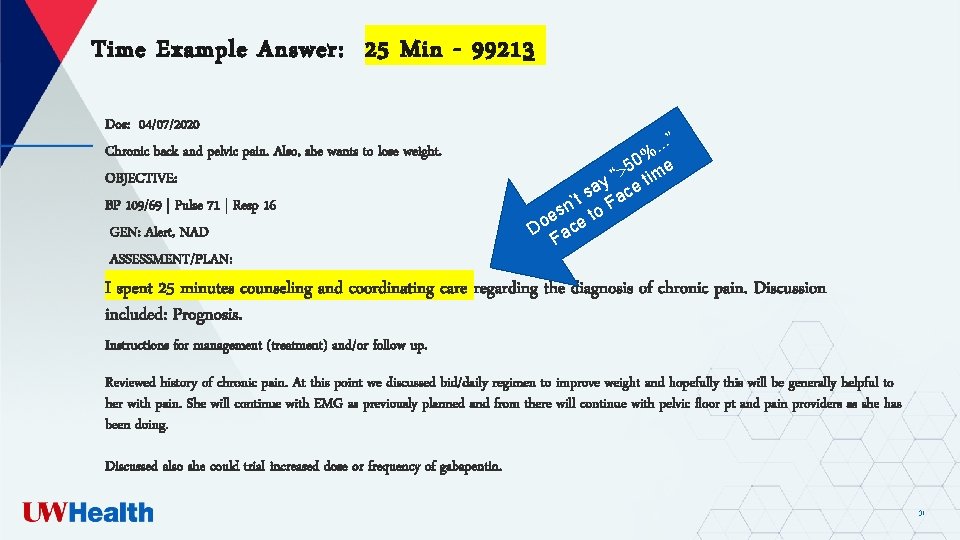
Time Example Answer: 25 Min - 99213 Dos: 04/07/2020 Chronic back and pelvic pain. Also, she wants to lose weight. OBJECTIVE: BP 109/69 | Pulse 71 | Resp 16 GEN: Alert, NAD ASSESSMENT/PLAN: . . ”. 0% e 5 “ tim y sa ace t ’ sn to F e Do ace F I spent 25 minutes counseling and coordinating care regarding the diagnosis of chronic pain. Discussion included: Prognosis. Instructions for management (treatment) and/or follow up. Reviewed history of chronic pain. At this point we discussed bid/daily regimen to improve weight and hopefully this will be generally helpful to her with pain. She will continue with EMG as previously planned and from there will continue with pelvic floor pt and pain providers as she has been doing. Discussed also she could trial increased dose or frequency of gabapentin. 31
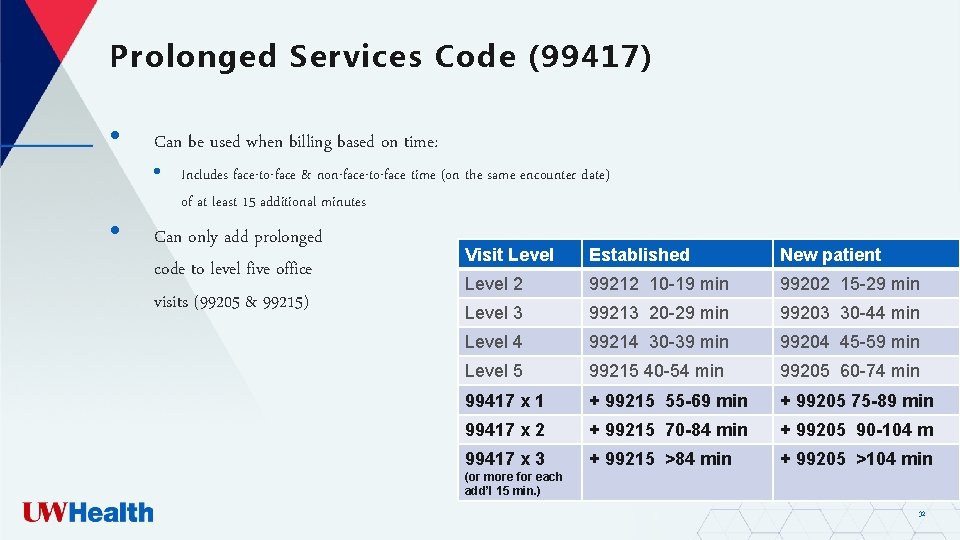
Prolonged Services Code (99417) • • Can be used when billing based on time: • Includes face-to-face & non-face-to-face time (on the same encounter date) of at least 15 additional minutes Can only add prolonged code to level five office visits (99205 & 99215) Visit Level Established New patient Level 2 99212 10 -19 min 99202 15 -29 min Level 3 99213 20 -29 min 99203 30 -44 min Level 4 99214 30 -39 min 99204 45 -59 min Level 5 99215 40 -54 min 99205 60 -74 min 99417 x 1 + 99215 55 -69 min + 99205 75 -89 min 99417 x 2 + 99215 70 -84 min + 99205 90 -104 m 99417 x 3 + 99215 >84 min + 99205 >104 min (or more for each add’l 15 min. ) 32
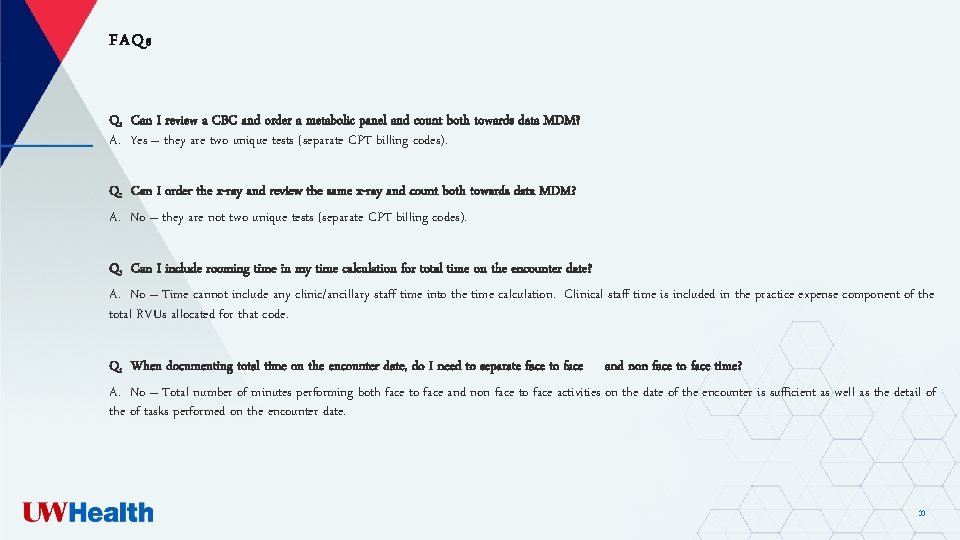
FAQs Q. Can I review a CBC and order a metabolic panel and count both towards data MDM? A. Yes – they are two unique tests (separate CPT billing codes). Q. Can I order the x-ray and review the same x-ray and count both towards data MDM? A. No – they are not two unique tests (separate CPT billing codes). Q. Can I include rooming time in my time calculation for total time on the encounter date? A. No – Time cannot include any clinic/ancillary staff time into the time calculation. Clinical staff time is included in the practice expense component of the total RVUs allocated for that code. Q. When documenting total time on the encounter date, do I need to separate face to face and non face to face time? A. No – Total number of minutes performing both face to face and non face to face activities on the date of the encounter is sufficient as well as the detail of the of tasks performed on the encounter date. 33
FAQs, cont. Q. If a provider spends time prepping the chart the night before they see a patient, does that count when using time? What if the visit is within 24 hours? A. No. Total time is defined as the day of the encounter (i. e. calendar date). Q. Does MDM apply to code 99211? A. No, the concept of MDM does no apply to 99211, that may not require the presence of a physician or other QHP. Usually the problem(s) are minimal. MDM includes establishing diagnoses, assessing the status of a condition and/or selecting a management option. 34

Check your Knowledge 35
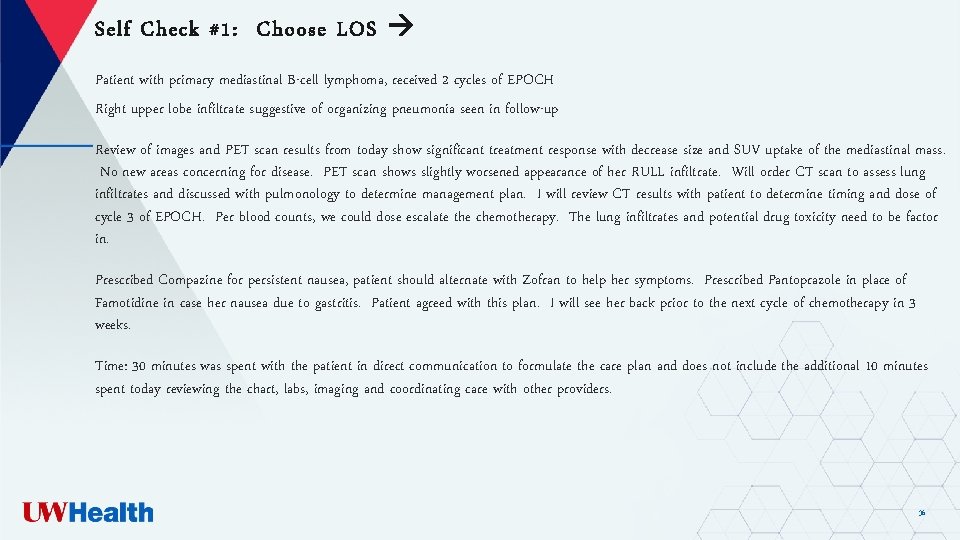
Self Check #1: Choose LOS Patient with primary mediastinal B-cell lymphoma, received 2 cycles of EPOCH Right upper lobe infiltrate suggestive of organizing pneumonia seen in follow-up Review of images and PET scan results from today show significant treatment response with decrease size and SUV uptake of the mediastinal mass. No new areas concerning for disease. PET scan shows slightly worsened appearance of her RULL infiltrate. Will order CT scan to assess lung infiltrates and discussed with pulmonology to determine management plan. I will review CT results with patient to determine timing and dose of cycle 3 of EPOCH. Per blood counts, we could dose escalate the chemotherapy. The lung infiltrates and potential drug toxicity need to be factor in. Prescribed Compazine for persistent nausea, patient should alternate with Zofran to help her symptoms. Prescribed Pantoprazole in place of Famotidine in case her nausea due to gastritis. Patient agreed with this plan. I will see her back prior to the next cycle of chemotherapy in 3 weeks. Time: 30 minutes was spent with the patient in direct communication to formulate the care plan and does not include the additional 10 minutes spent today reviewing the chart, labs, imaging and coordinating care with other providers. 36
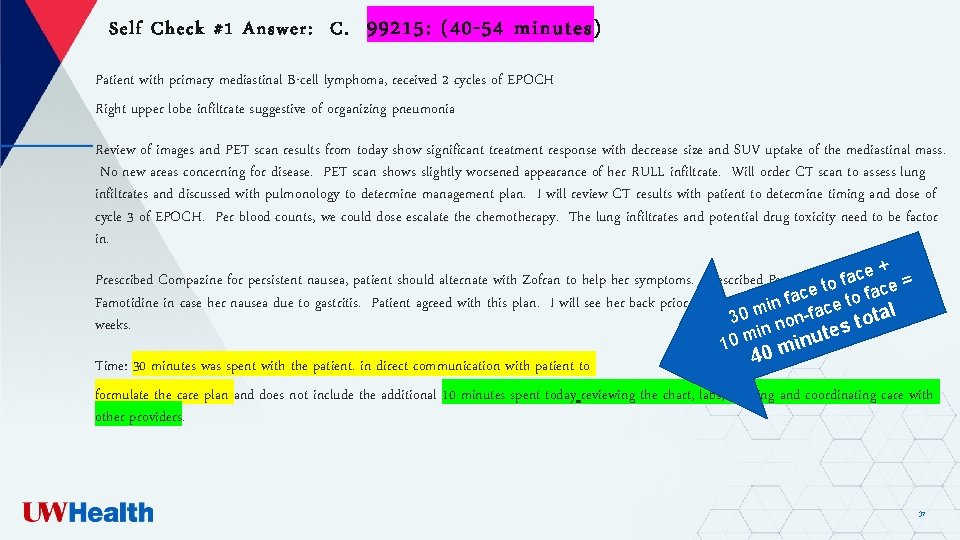
Self Check #1 Answer: C. 99215: (40 -54 minutes) Patient with primary mediastinal B-cell lymphoma, received 2 cycles of EPOCH Right upper lobe infiltrate suggestive of organizing pneumonia Review of images and PET scan results from today show significant treatment response with decrease size and SUV uptake of the mediastinal mass. No new areas concerning for disease. PET scan shows slightly worsened appearance of her RULL infiltrate. Will order CT scan to assess lung infiltrates and discussed with pulmonology to determine management plan. I will review CT results with patient to determine timing and dose of cycle 3 of EPOCH. Per blood counts, we could dose escalate the chemotherapy. The lung infiltrates and potential drug toxicity need to be factor in. + e of cplace a Prescribed Compazine for persistent nausea, patient should alternate with Zofran to help her symptoms. Prescribed Pantoprazole in f = o t e c e a c Famotidine in case her nausea due to gastritis. Patient agreed with this plan. I will see her back prior to the nextmcycle to f in 3 in faof chemotherapy e c tal 30 non-fa o t weeks. in es t m u 0 n i 1 m 0 4 Time: 30 minutes was spent with the patient. in direct communication with patient to formulate the care plan and does not include the additional 10 minutes spent today reviewing the chart, labs, imaging and coordinating care with other providers. 37
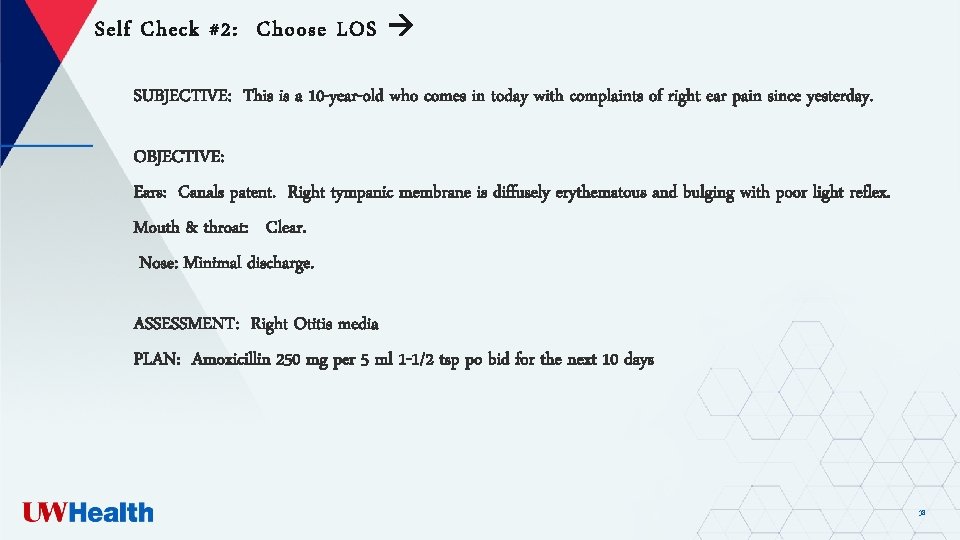
Self Check #2: Choose LOS SUBJECTIVE: This is a 10 -year-old who comes in today with complaints of right ear pain since yesterday. OBJECTIVE: Ears: Canals patent. Right tympanic membrane is diffusely erythematous and bulging with poor light reflex. Mouth & throat: Clear. Nose: Minimal discharge. ASSESSMENT: Right Otitis media PLAN: Amoxicillin 250 mg per 5 ml 1 -1/2 tsp po bid for the next 10 days 38
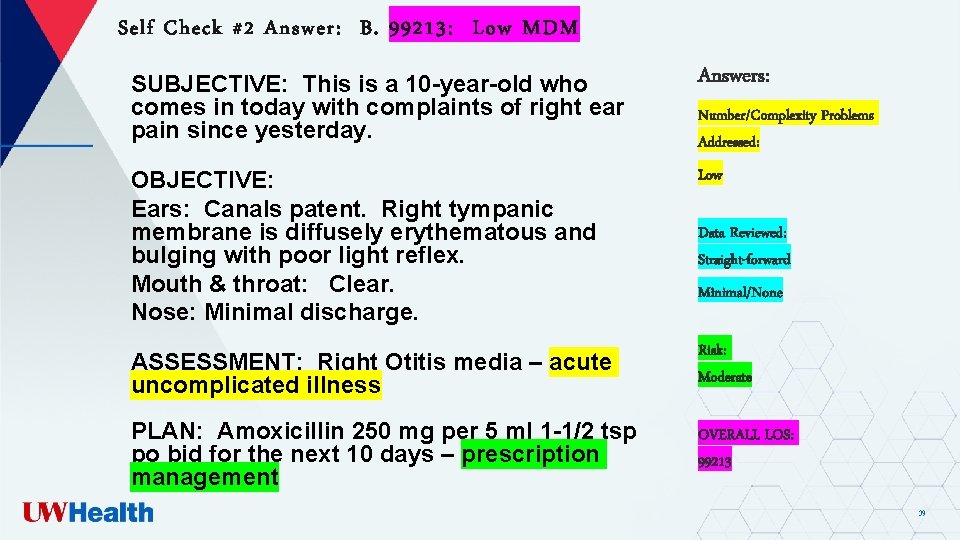
Self Check #2 Answer: B. 99213: Low MDM SUBJECTIVE: This is a 10 -year-old who comes in today with complaints of right ear pain since yesterday. Answers: OBJECTIVE: Ears: Canals patent. Right tympanic membrane is diffusely erythematous and bulging with poor light reflex. Mouth & throat: Clear. Nose: Minimal discharge. Low ASSESSMENT: Right Otitis media – acute uncomplicated illness Risk: Moderate PLAN: Amoxicillin 250 mg per 5 ml 1 -1/2 tsp po bid for the next 10 days – prescription management OVERALL LOS: 99213 Number/Complexity Problems Addressed: Data Reviewed: Straight-forward Minimal/None 39
Self Check #3: Choose LOS Patient is an 83 -year-old female, new patient, was examined in Otolaryngology for a patient requested 2 nd opinion regarding prior episodes of rotational vertigo. Prior workup was at Clinic X. PLAN: 1. We reviewed the option of clinical monitoring or ranging for physical exam to assess for evidence for vestibular hypofunction or proceeding with VNG and rotary chair testing to further clarify and then follow-up in-person. After detailed review of these tests, she is interested in proceeding with both VNG and rotary chair testing and this will be facilitated. 2. There is no interval history to suggest need for MRI without contrast given review of previous MRIs and no evidence for retro cochlear structural pathology on numerous previous MRIs. She agrees and prefers not to undergo this testing unless strongly recommended. 3. We reviewed that she is a candidate for bilateral hearing aids though she has low hearing handicap. Reviewed relevance of increased cognitive load associated with hearing loss as an independent risk factor for imbalance as well as independent factor contributing to postural difficulties. More detail counseling will be required with regard to options for therapy and will minimally monitor hearing in several months to ensure stability given the asymmetry. 4. Reviewed mechanisms that may trigger brief clicking tinnitus and advised monitoring for any escalating frequency or facial or diffuse myoclonic symptoms that would recommend updated conference of lab work and potentially additional neurology input. Reviewed the manner which polypharmacy alone may contribute to a variety of auditory and vestibular disturbances. 5. Advise close follow-up with her. At risk given the history for analgesic overuse contributing to chronic pain central sensitization as well as rebound phenomena which may interact negatively with postural control via autonomic dysfunction. At present, reviewed the polypharmacy may interact negatively with auditory vestibular symptoms although no specific recommendations for changing her regimen is noted at present. We additionally reviewed the need for follow-up to discuss more detail strategies and utility of as-needed medication for symptomatic management as well as medications that may be considered for your stabilization of symptoms pending findings. 6. May need additional sleep evaluation given chronicity sleep initiation and maintenance difficulties, and to exclude unrecognized apnea. Briefly reviewed rational use of sleep medications given negative impact on balance/cognition, although on the other hand reviewed extremely poor sleep may also compromise of balance increased fall risk. The interval history does not suggest a need for an expedited cardiology evaluation although given history of orthostasis and multiple risk factors, advise symptoms that would suggest need for falls and faints evaluation. Time today: (Start Time: 9: 00; Finish Time 10: 30) was spent reviewing the above diagnoses, treatment, plan, counseling, and coordination of care. 40
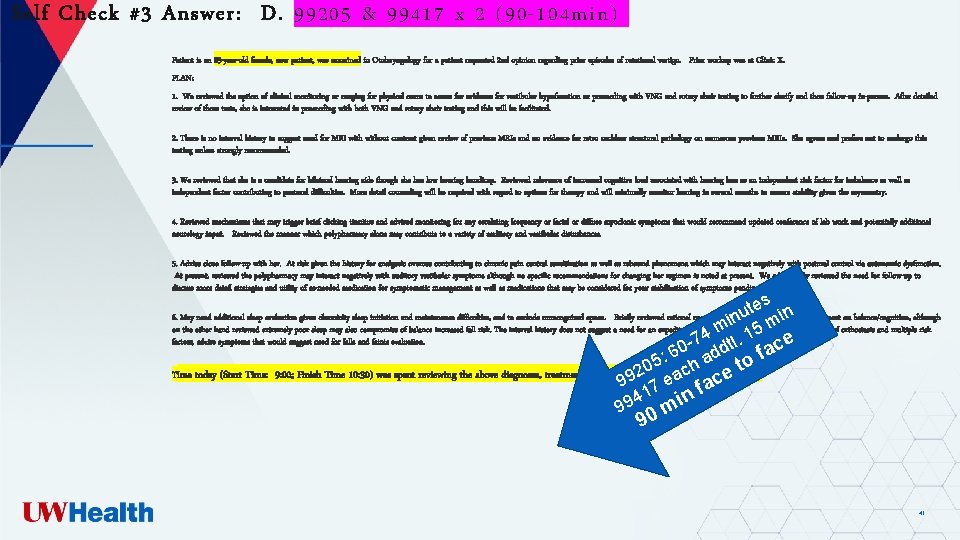
Self Check #3 Answer: D. 99205 & 99417 x 2 (90 -104 min) Patient is an 83 -year-old female, new patient, was examined in Otolaryngology for a patient requested 2 nd opinion regarding prior episodes of rotational vertigo. Prior workup was at Clinic X. PLAN: 1. We reviewed the option of clinical monitoring or ranging for physical exam to assess for evidence for vestibular hypofunction or proceeding with VNG and rotary chair testing to further clarify and then follow-up in-person. After detailed review of these tests, she is interested in proceeding with both VNG and rotary chair testing and this will be facilitated. 2. There is no interval history to suggest need for MRI without contrast given review of previous MRIs and no evidence for retro cochlear structural pathology on numerous previous MRIs. She agrees and prefers not to undergo this testing unless strongly recommended. 3. We reviewed that she is a candidate for bilateral hearing aids though she has low hearing handicap. Reviewed relevance of increased cognitive load associated with hearing loss as an independent risk factor for imbalance as well as independent factor contributing to postural difficulties. More detail counseling will be required with regard to options for therapy and will minimally monitor hearing in several months to ensure stability given the asymmetry. 4. Reviewed mechanisms that may trigger brief clicking tinnitus and advised monitoring for any escalating frequency or facial or diffuse myoclonic symptoms that would recommend updated conference of lab work and potentially additional neurology input. Reviewed the manner which polypharmacy alone may contribute to a variety of auditory and vestibular disturbances. 5. Advise close follow-up with her. At risk given the history for analgesic overuse contributing to chronic pain central sensitization as well as rebound phenomena which may interact negatively with postural control via autonomic dysfunction. At present, reviewed the polypharmacy may interact negatively with auditory vestibular symptoms although no specific recommendations for changing her regimen is noted at present. We additionally reviewed the need for follow-up to discuss more detail strategies and utility of as-needed medication for symptomatic management as well as medications that may be considered for your stabilization of symptoms pending findings. tes in u in m 5 m 4 1 0 -7 ddtl. face 6 5: ch a to 0 9: 00; Finish Time 10: 30) was spent reviewing the above diagnoses, treatment, plan, counseling, 2 and coordination of care. 99 7 ea face 41 in 9 9 m 6. May need additional sleep evaluation given chronicity sleep initiation and maintenance difficulties, and to exclude unrecognized apnea. Briefly reviewed rational use of sleep medications given negative impact on balance/cognition, although on the other hand reviewed extremely poor sleep may also compromise of balance increased fall risk. The interval history does not suggest a need for an expedited cardiology evaluation although given history of orthostasis and multiple risk factors, advise symptoms that would suggest need for falls and faints evaluation. Time today (Start Time: 90 41
Recap of Important Points The new AMA CPT E/M changes are specific only to Office or Other Outpatient Services (99201 -99205 and 99211 -99215) codes o o o Deletion of 99201 New guidelines specific to 99202 -99215 Changes in component scoring for both new and established patient codes (99202 -99215) Changes to the medical decision-making table Changes to the typical times associated with each E/M code (99202 -99215) 42
What is NOT changing These changes do not apply to the following code ranges: o Inpatient, o Emergency Department, o Consultation (outpatient or inpatient), o Nursing Home, o Home Health visits, or o Any other E/M services o Coders and providers will be working with 2 sets of guidelines for 2021 43

What questions do you have? This Photo by Unknown Author is licensed under CC BY
Homework & Resources is s i Th ur yo ork ew m ho Homework o Your new best friend - AMA’s document: CPT Evaluation and Management (E/M) Office or Other Outpatient (9920299215) and Prolonged Services (99354, 99355, 99356, 99 XXX) Code and Guideline Changes Resources o Implementing CPT Evaluation and Management (E/M) Revisions (video) 45

THANK YOU!!! Brenda L. Whyte, RHIT, CPC UW Health Compliance Education Coordinator brenda. whyte@uwmf. wisc. edu 46
- Slides: 46