Transcranial Doppler Sonography in Sickle Cell Anemia Dr
- Slides: 16
Transcranial Doppler Sonography in Sickle Cell Anemia Dr. O. Esmaeili Neurologist, M. D.
Introduction Transcranial Doppler Sonography (TCD) provides : rapid, non-invasive, real-time measure of cerebrovascular function. It measures the velocity of blood flow through the brain’s blood vessels by measuring the echoes of ultrasound waves moving through the cranium.
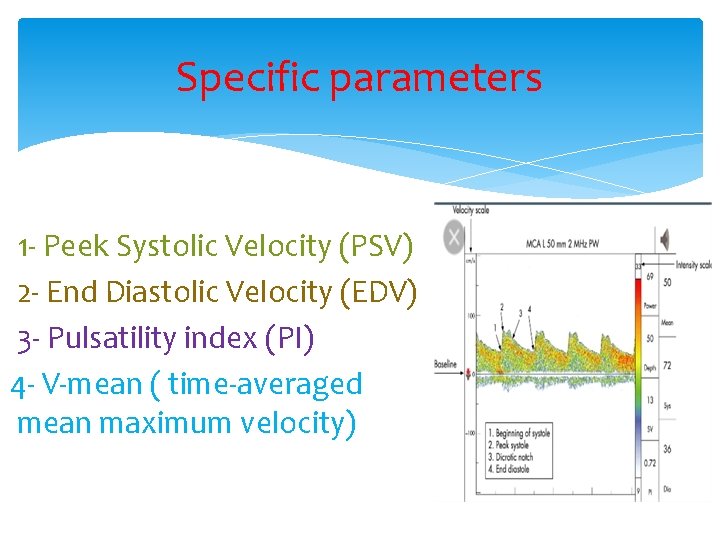
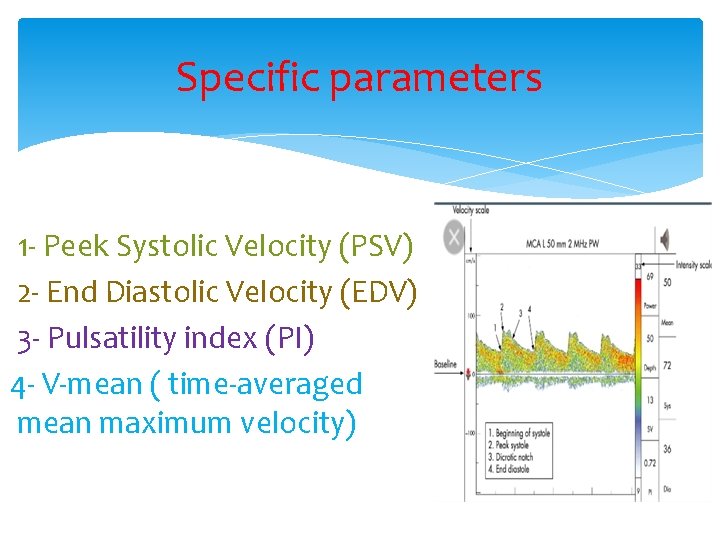
Specific parameters 1 - Peek Systolic Velocity (PSV) 2 - End Diastolic Velocity (EDV) 3 - Pulsatility index (PI) 4 - V-mean ( time-averaged mean maximum velocity)
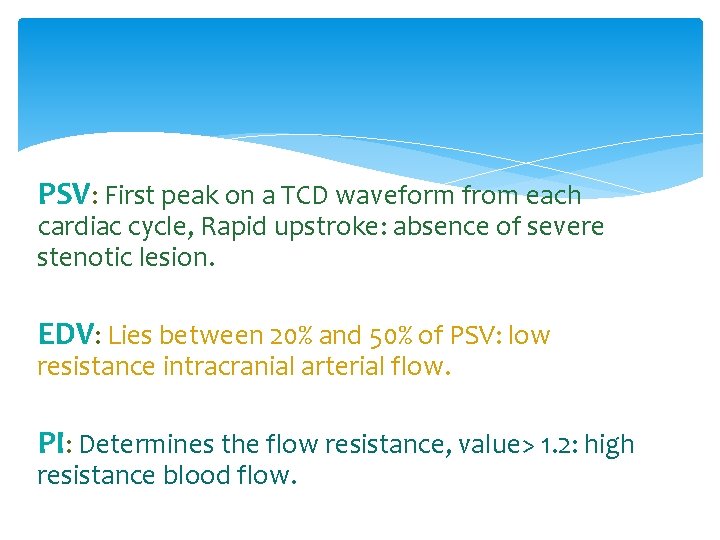
PSV: First peak on a TCD waveform from each cardiac cycle, Rapid upstroke: absence of severe stenotic lesion. EDV: Lies between 20% and 50% of PSV: low resistance intracranial arterial flow. PI: Determines the flow resistance, value> 1. 2: high resistance blood flow.
Physiologic variables that impact TCD 1 - Age 2 - Gender: F > M 3 - Hematocrit 4 - Viscosity 5 - Pco 2 6 - Temperature 7 - Blood Pressure 8 - Mental and Physical activity
Clinical applications of TCD 1 - Sub Arachnoid Hemorrhage & cerebral vasospasm 2 - Intracranial Steno-occlusive disease 3 - Acute Ischemic Stroke 4 - Collateral Flow 5 - Micro Emboli Detection 6 - Cerebral Circulatory Arrest 7 - Sickle Cell Disease
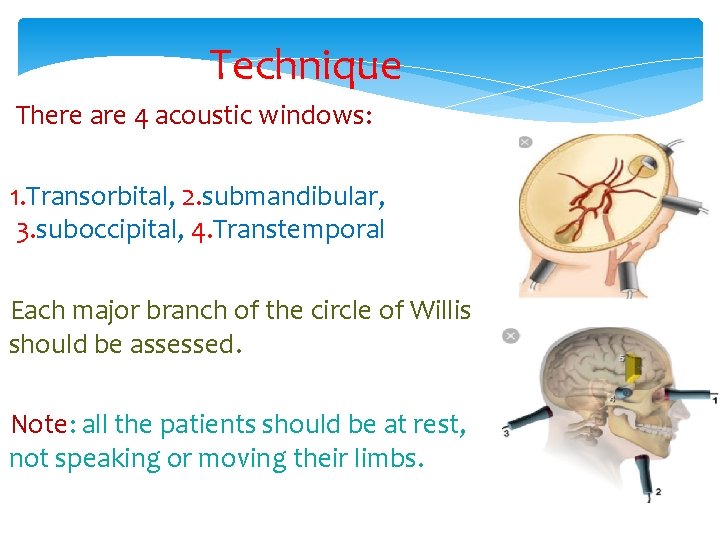
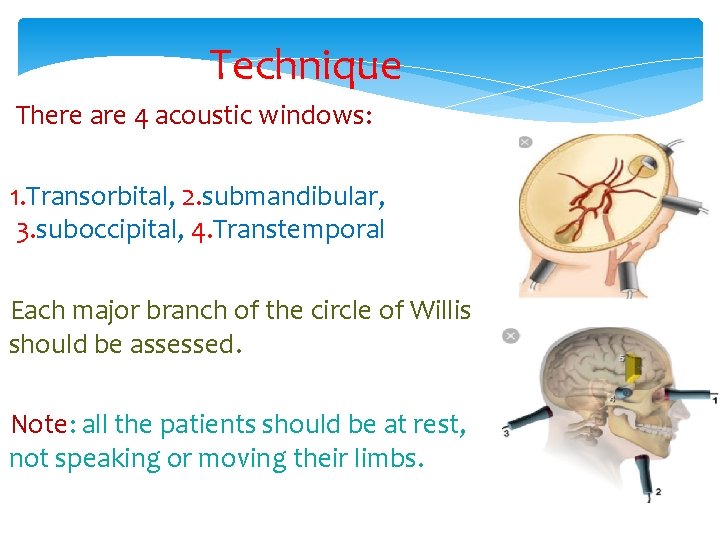
Technique There are 4 acoustic windows: 1. Transorbital, 2. submandibular, 3. suboccipital, 4. Transtemporal Each major branch of the circle of Willis should be assessed. Note: all the patients should be at rest, not speaking or moving their limbs.
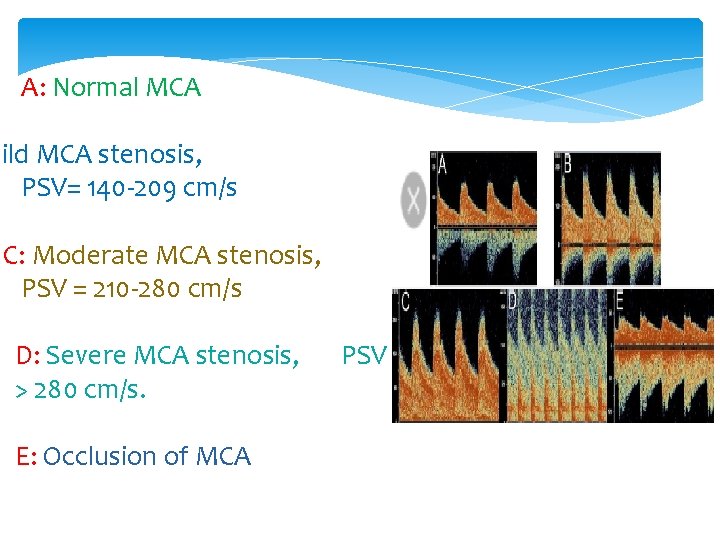
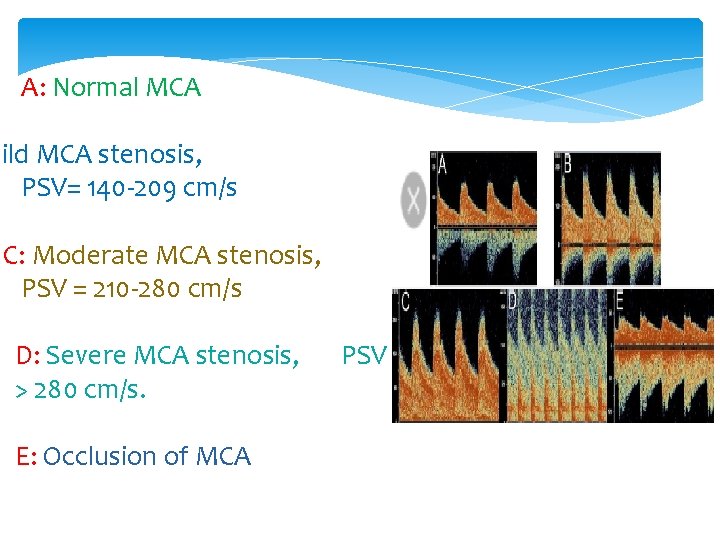
A: Normal MCA Mild MCA stenosis, PSV= 140 -209 cm/s C: Moderate MCA stenosis, PSV = 210 -280 cm/s D: Severe MCA stenosis, > 280 cm/s. E: Occlusion of MCA PSV
TCD in Sickle Cell Disease Pathophysiology: 1 - Chronic hemolysis resulting in low Hb content 2 - Chronic anemia and hypoxia triggers angiogenesis and neovascularization. 3 - Interaction of sickled red cells within the endothelium results inflammation and intracranial stenosis. * TCD should be avoided during acute illness, because factors such as hypoxia, fever, hypoglycemia.
Stroke is a complication of SCD, particularly during childhood, with an estimated 11% of patients with homozygous SCD having a stroke by the age of 20 years. The use of TCD identifies children with SCD who are at high risk for stroke. An increase in Vmean in the ICA or MCA detected by TCD has been shown to be associated with increased risk of ischemic stroke in these children.
In Stroke Prevention Trial in Sickle Cell Anemia (STOP) , (cohort of 130, 60 boys, 70 girls) children between 2 -16 years old (mean age 8. 3 y/o) with no history of stroke, an MCA Vmean > 200 cm/s were randomly allocated to standard care or to periodic blood transfusion therapy (63 patients) to lower the Hb. S concentration to < 30% of total Hb. Following STOP TCD criteria, a five fold decrease (92%) in the rate of first stroke was observed in children with sickle cell disease.
Stop II : Discontinuing Prophylactic Transfusions Used to Prevent Stroke in Sickle Cell Disease. This investigation reconsidered the safety of discontinuing long-term transfusion in normal MCA flow velocity, who had transfusion for 30 months or longer. They concluded that discontinuation of transfusion for the prevention of stroke in children with SCD results in a high rate of reversion to abnormal blood flow velocities on Doppler studies and stroke.
In another study¹: 10 fold decrease following TCD screening ( the pre-TCD period: 0. 67 per 100 patients -years, compared with post-TCD period: 0. 06 per 100 patients-year) and prophylactic blood transfusion over an 8 -year period. 1. Enniful-Eghan H, et al. J Pediatr. 2010.
Final Conclusion 1. Stroke in the children who affected with SCD is preventable with TCD. 2. TCD identifies high risk SCD patients and can guide use of Rx. 3. Stroke rate without transfusion = 10% / year. 4. Stroke risk remains in adults with SCD.
Questions will remain 1. Mechanism of high velocity ? (stenosis or hyperemia) 2. Mechanism of Rx effect ? 3. Correlation with MRA, CTA ? 4. How long to Rx ?
Thanks for your attention