TRANSCATHETER PDA CLOSURE USING THE AMPLATZER DUCT OCCLUDER

- Slides: 49
TRANSCATHETER PDA CLOSURE USING THE AMPLATZER DUCT OCCLUDER BY: JAMEEL AL-ATA, MD ASSISTANT PROFESSOR and CONSULTANT PEDIATRIC CARDIOLOGIST
INTRO: n Transcatheter closure of the small to moderate patent ductus arteriosus utilizing coils is an accepted treatment (…Hijazi, Galal Int card).
n Addressing the larger PDA using multiple coils was shown to be feasible, but not without problems (Hizji, > 4 mm PDA, Galal Zeitschrift kardiologie).
INTRO: n The large PDA remained the domain of surgery for a while. Only recently the Amplatzer duct occlude (ADO) has been introduced as an alternative (Masura) ( Saliba)
n Especially in the younger age and weight group there are still relatively few reports describing the experience with this device (Alwi JACC 2001)
The aim of this study: n To present our experience with the ADO to close large PDA in a relatively young patients population.
n Special attention was taken to focus on the selection of the optimum sized device as well as the problems and complications which can be encountered while using this device.
METHODS: n In a clinical study, all 43 patients (29/43 females, 14/43 males) who underwent attempt of transcatheter closure of their patent ductus arteriosus using an Amplatzer duct occlud between July 2001 and October 2003 were reviewed.
Inclusion criteria: n All patients who had a PDA, which was judged angiographically to be too large for a single coil implantation ( > 3 mm narrowest diameter) were included in this study.
Exclusion criteria: n Patients who underwent transcatheter closure in which coils were utilized. n Had other cardiac anomelies.
Clinical Examination and Echocardiographic Evaluation: n All patients underwent complete cardiac evaluation; including physical examination, twelve lead ECG, and a radiogram of the chest.
Cont. : n Detailed echocardiograms were performed at baseline using Hewlett Packard Sonos 5500.
CONT: n The narrowest diameter of the PDA was measured in the ductal view using color Doppler and electronic calipers.
Cont. : n Routine M-mode echo tracings were obtained in the parasternal long axis view as recommended by the American Association for ECHO.
Cont. : n Follow-up echocardiograms were performed in most before discharge, one month and then 6 months after closing the ductus arteriosus.
Cardiac Catheterization procedure: n In all patients signed consent was obtained from their parents. Patients were sedated with ketamine and midazolam during the procedure.
Cont. : n None of the patients received general anesthesia or intubation. n Heparin in a dose of 100 IU/kg was administered
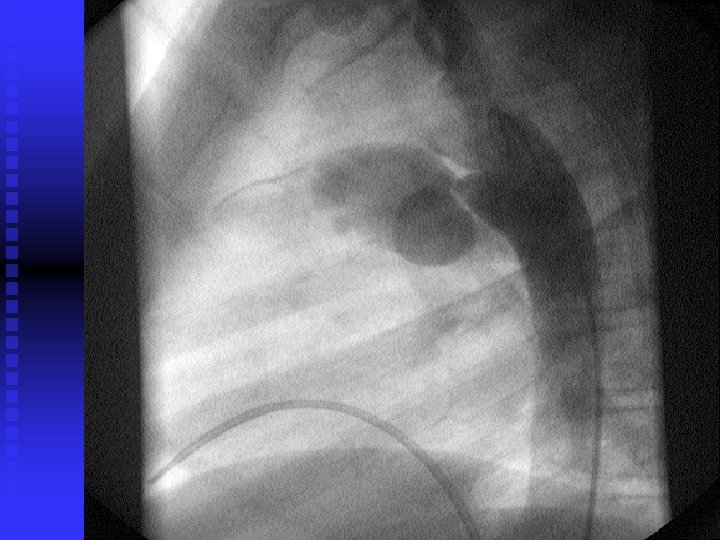
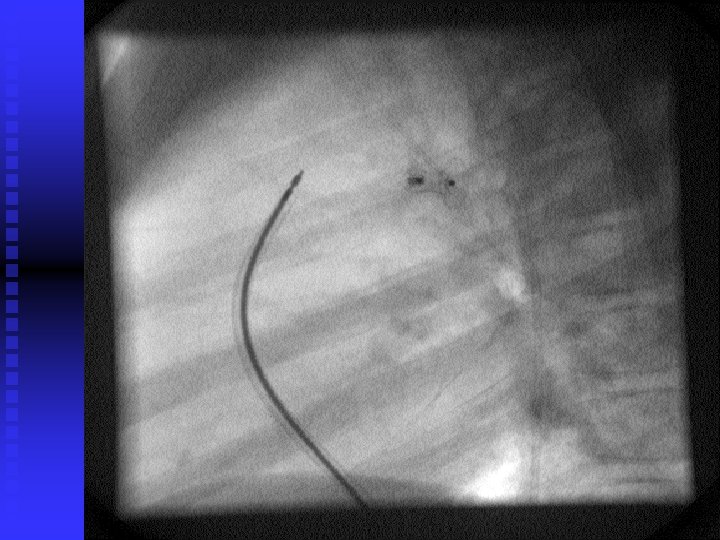
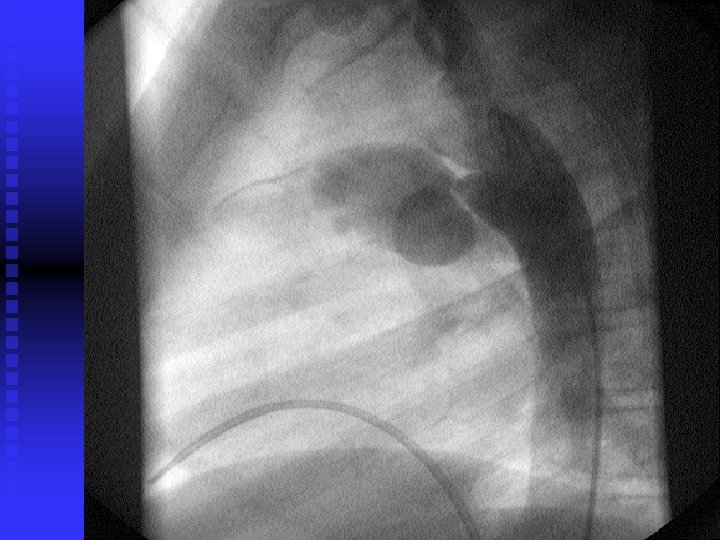
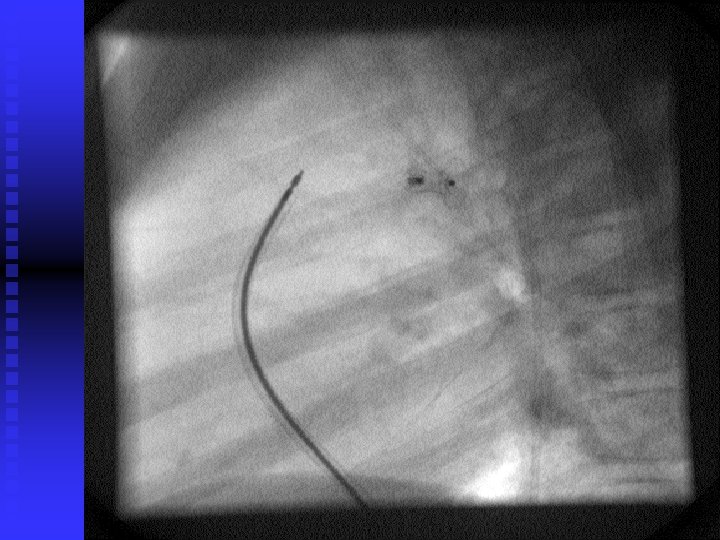
CONT: n Aortograms performed in straight lateral position were reviewed to determine the PDA diameter and the type of the ductus was described according to the classification of Krichenko.
Cont. : n The narrowest diameter of the PDA, the aortic diameter of the ampulla, the length of the ampulla and the mid diameter of the ampulla were measured.
CONT. : n Amplatzer duct occlud of the PDA was performed through anterograde approach
Study group: n The procedure proved successful in 42 patients (97. 5%). n We used a device of size 6/4 in 21 of the patients (50%), using the 8/6 device in 10 (24%), the 10/8 device in 7 (16. 5%), and the 12/10 device in 4 (9. 5%) of the patients.
Cont. : n In all patients who underwent implantation of devices, cefuroxime (30 mg/kg) was administered intravenously during the procedure. n Two more doses were given with the next 24 hours.
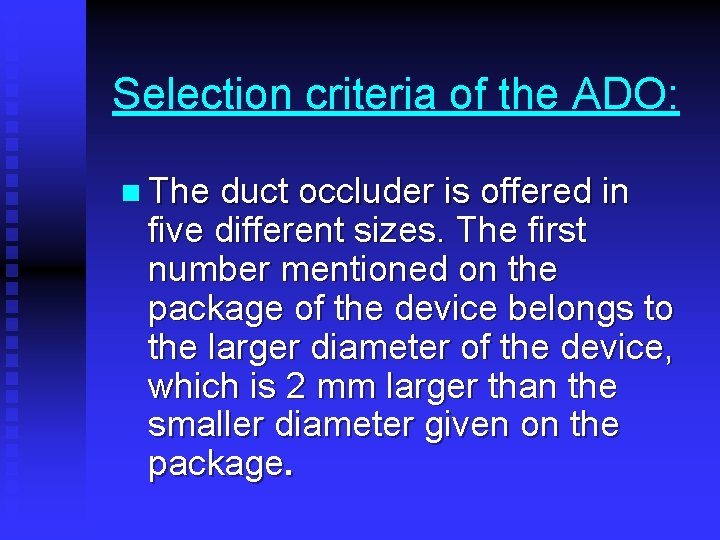
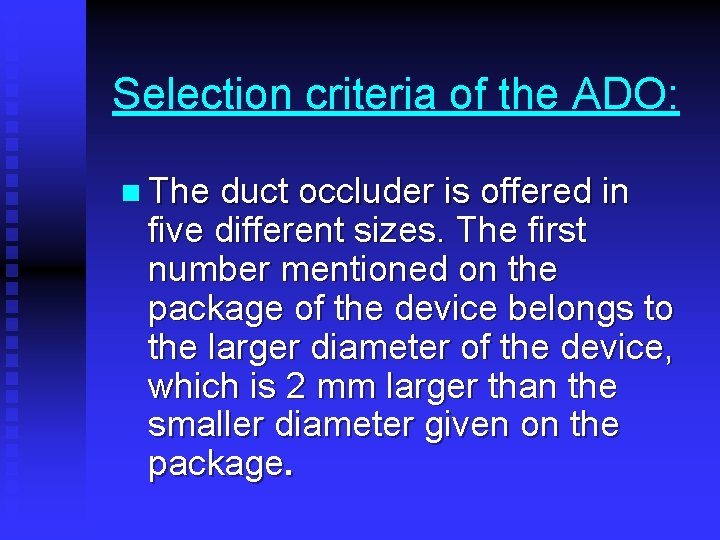
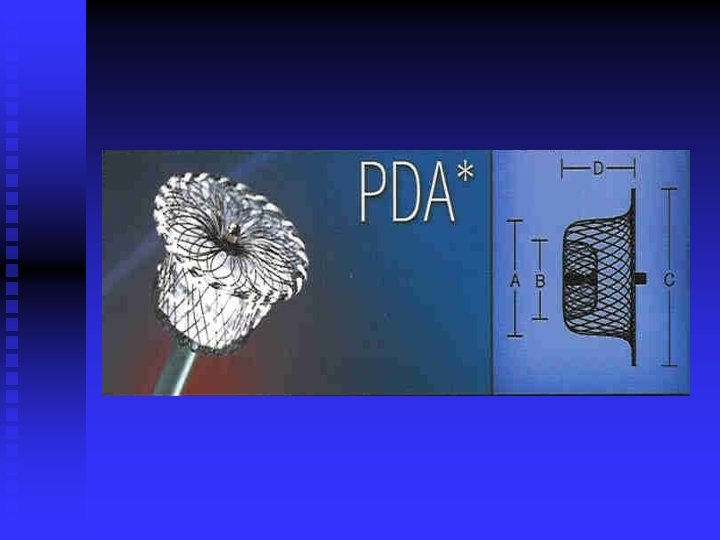
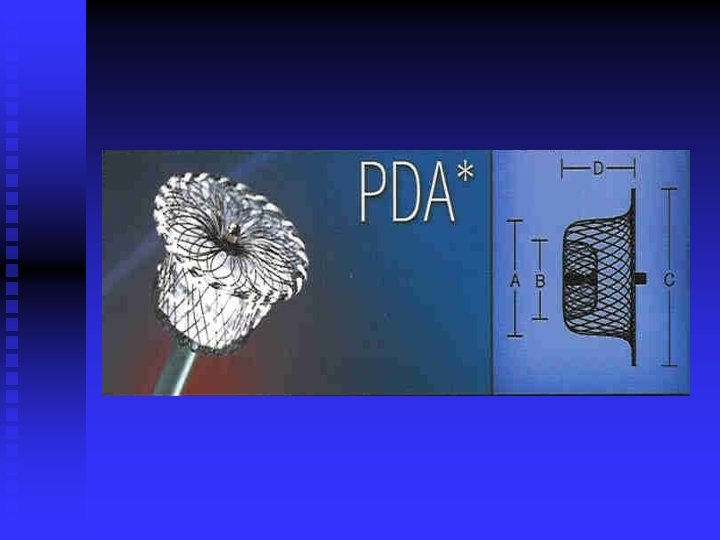
Selection criteria of the ADO: n The duct occluder is offered in five different sizes. The first number mentioned on the package of the device belongs to the larger diameter of the device, which is 2 mm larger than the smaller diameter given on the package.
Cont. : n The larger diameter is usually positioned in the aortic end of the ductul ampulla, while the smaller diameter is positioned at the pulmonary end.
Cont. : n In the first two patients, we followed the recommendation suggesting to use a duct occluder in which its smaller diameter (pulmonary end) is 12 mm larger than the narrowest diameter of the specific duct.
Cont. : n In view of the problems we encountered with positioning of the second device, we tried to put all the measurements of the PDA into consideration, while selecting adequate ADO.
Cont. : n In this specific case, though the Recommendation was followed, because of a mismatch between the skirt of the device and aortic end of the duct, the skirt of the device protruded into the descending aorta.
Cont. : n We therefore measured the narrowest diameter of the duct, its length, & the largest diameter for the aortic end,
Cont. : n Since it has to accommodate the skirt of the device, which is 4 mm larger than the number given for the larger (aortic) end of the ADO.
Cont. : n The mid ductul diameter was also measured, so to make sure in case the duct is too long, that the larger part of the ADO will fit.
Results:

Age (years) 3. 79 ± 3. 82 (0. 45 - 13) Sex 29 females, 14 males Weight (kilograms) 11. 9 ± 8. 91 (4. 5 – 44) Height (centimeters) 83. 6 ± 21. 1 (59 – 154)
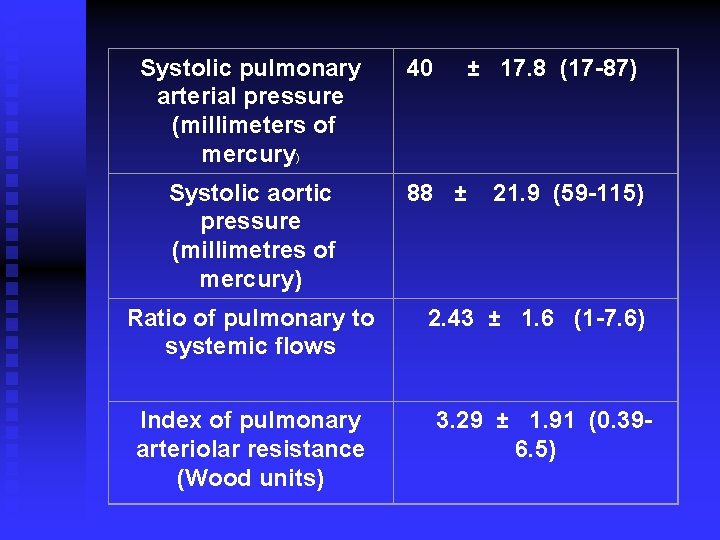
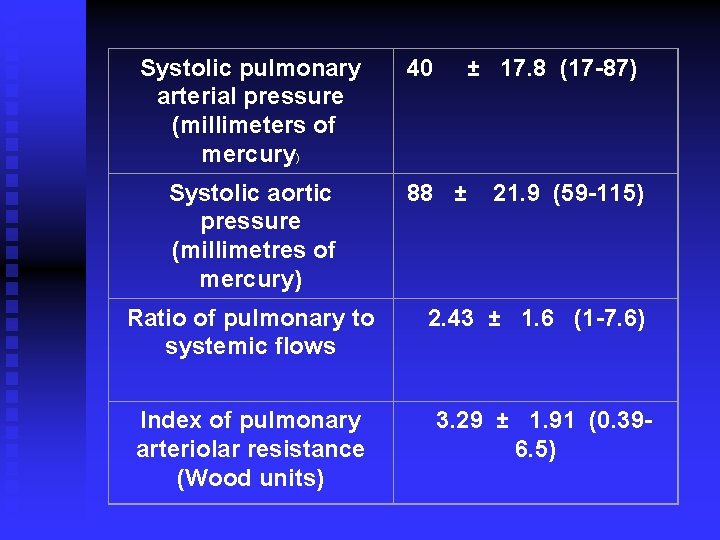
Systolic pulmonary arterial pressure (millimeters of mercury) 40 ± 17. 8 (17 -87) Systolic aortic pressure (millimetres of mercury) 88 ± 21. 9 (59 -115) Ratio of pulmonary to systemic flows Index of pulmonary arteriolar resistance (Wood units) 2. 43 ± 1. 6 (1 -7. 6) 3. 29 ± 1. 91 (0. 396. 5)
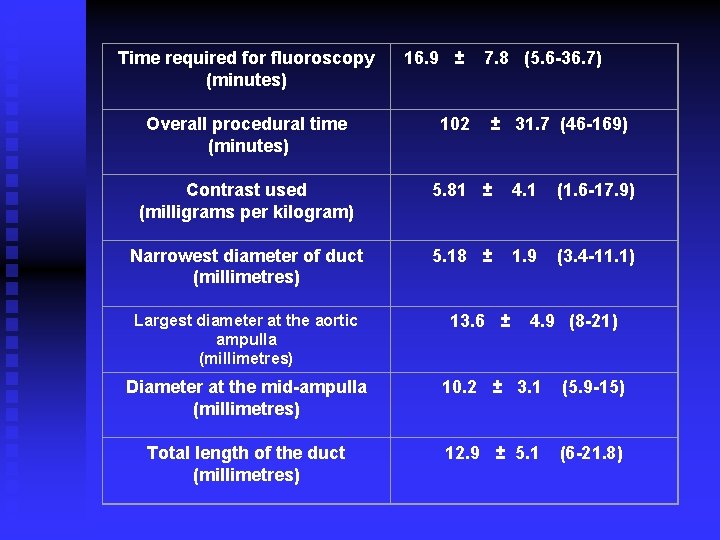
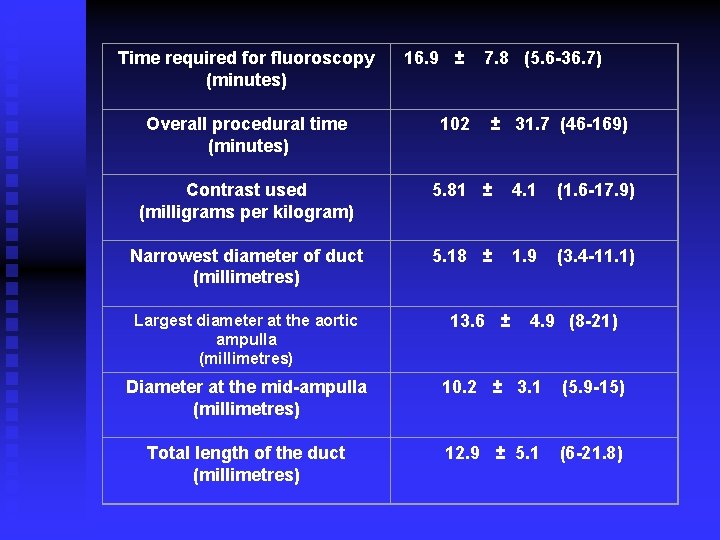
Time required for fluoroscopy (minutes) 16. 9 ± 7. 8 (5. 6 -36. 7) Overall procedural time (minutes) 102 ± 31. 7 (46 -169) Contrast used (milligrams per kilogram) 5. 81 ± 4. 1 (1. 6 -17. 9) Narrowest diameter of duct (millimetres) Largest diameter at the aortic ampulla (millimetres) 5. 18 ± 1. 9 (3. 4 -11. 1) 13. 6 ± 4. 9 (8 -21) Diameter at the mid-ampulla (millimetres) 10. 2 ± 3. 1 (5. 9 -15) Total length of the duct (millimetres) 12. 9 ± 5. 1 (6 -21. 8)
Cont. : n All patients were done as a day case. n None had to be admitted over night.
n n Rate of occlusion: Immediate occlusion, confirmed angiographically, was achieved in 25 (60%) patients. In another 8 (19%), complete occlusion occurred some hours after the procedure, as confirmed by echocardiography. In 33 (79%) of the patients, therefore, complete occlusion was achieved on the day of the procedure.
n At a further follow-up, of between one week and 6 months, complete occlusion had occurred in 6 more patients. n At that time, 2 patients had trivial residual shunting, while one had a significant residual leak.
Issues pertinent to Procedure: n Mean number of angiographies to visualize the PDA before implantation was 1. 8 injection (range 1 -7).
PROBLEMS & COMPLICATIONS n There was no device embolization. n There was no loss of pulse. n There was no mortality.
Cont. : n Waist of coils 3 coils in one patient n Waiste of Amplatzer in two patients n Pull through of device in three patients
Cont. : n Kinking of sheath and inability to retrieve a too large device. n Excessive bleeding needing transfusion in one. n Difficulty in visualizing the large PDA.
Conclusions: n Transcatheter occlusion of PDA by the ADO has a high complete occlusion rate and is effective in PDA up to a narrowest diameter of 10 mm and probably larger PDAs.
Cont. : Especially in the young age group, problems & complication rate of 30% can be encountered in the learning phase. n The ADO diameter should not exceed the largest ampulla diameter of the PDA in order to avoid descending aortic obstruction. n