TRANEXAMIC ACID IN PATIENTS UNDERGOING CORONARY ARTERY SURGERY
- Slides: 40
TRANEXAMIC ACID IN PATIENTS UNDERGOING CORONARY ARTERY SURGERY VAAIGA AUTAGAVAIA WAIKATO CARDIOTHORACIC UNIT JOURNAL CLUB
QUESTION 1. WHAT ARE THE RISKS AND BENEFITS OF USING TRANEXAMIC ACID (TXA) DURING CARDIAC ARTERY BYPASS SURGERY (CABG)? 1. BENEFIT: WILL IT REDUCE PERI-OPERATIVE BLEEDING? 2. RISKS: WILL IT INCREASE THE RISK OF POST-OPERATIVE SEIZURES? WILL IT INCREASE THROMBOTIC EVENTS?
INTRODUCTION
BACKGROUND • SIGNIFICANT TRANSFUSION REQUIREMENT IN CARDIAC SURGERY • ROBICH ET AL. , RATE OF TRANSFUSION OF BLOOD PRODUCTS, 2015 • RETROSPECTIVE • US, >4. 4 MIL PTS, 1999 -2010 (11 YRS) • CABG, 32% • VALVE SURGERY, 36% • COMBINED, 40%
BACKGROUND • POORER OUTCOMES WITH RE-EXPLORATION FOR BLEEDING AFTER CARDIAC SURGERY • BIANCARI, ET AL. , 2012 • SYSTEMATIC REVIEW AND META-ANALYSIS: • RISK OF COMPLICATIONS RELATED TO RE-EXPLORATION FOR BLEEDING IN CARDIAC SURGERY • 8 OBSERVATIONAL STUDIES, >550 K PTS. • INCREASED RISK OF IMMEDIATE POST-OPERATIVE MORTALITY AND MORBIDITY
BACKGROUND • TXA: REDUCTION IN TRANSFUSION REQUIREMENT • KER, ET AL. , 2012 • SYSTEMATIC REVIEW AND CUMULATIVE META-ANALYSIS: • EFFECT OF TXA ON SURGICAL BLEEDING • 129 RCTS, >10 KPTS , 1972 -2011 • 1/3 REDUCTION IN TRANSFUSION • UNCERTAIN THROMBOTIC EFFECT
BACKGROUND • TXA: POST-OPERATIVE SEIZURES, ‘ALL SUGERIES’ • MURKIN, ET AL. , 2010 • RETROSPECTIVE ANALYSIS • 669 PTS, CARDIAC SURGERY, HIGH RISK FOR BLEEDING • 24 CASES • 1. 3 -3. 8% INCREASE IN INCIDENCE OF POST-OPERATIVE SEIZURES • MAJORITY NON-ISCHAEMIC • LIKELY DOSE-RELATED
BACKGROUND • TXA: POST-OPERATIVE SEIZURES, CARDIAC SURGERY • SHARMA, ET AL. , 2013 • MULTIVARIATE ANALYSIS • 11, 529 PTS, CARDIOPULMONARY BYPASS • 100 CASES • TXA, STRONG PREDICTOR OF SEIZURES • HIGHER MORTALITY, LONGER HOSPITAL ANDICU I CU STAY • DOSE-RELATED
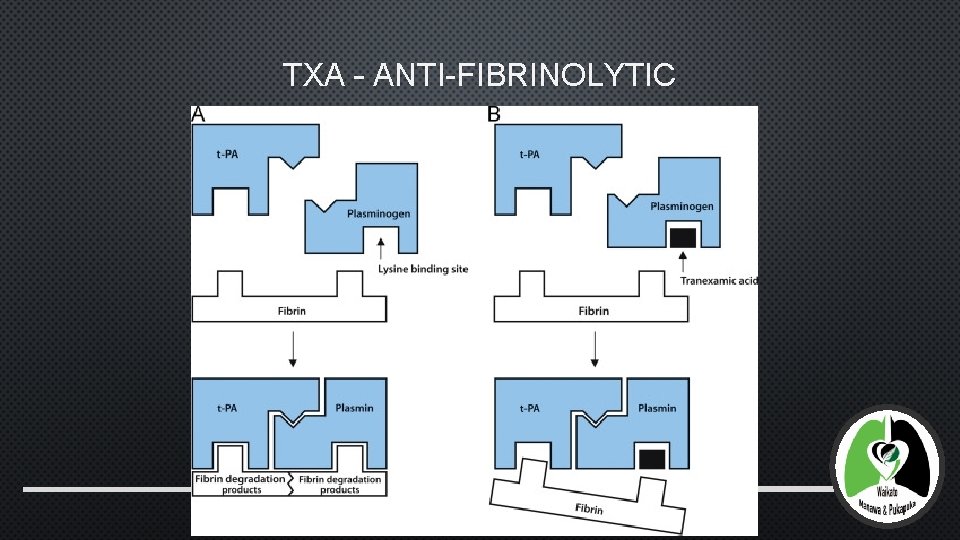
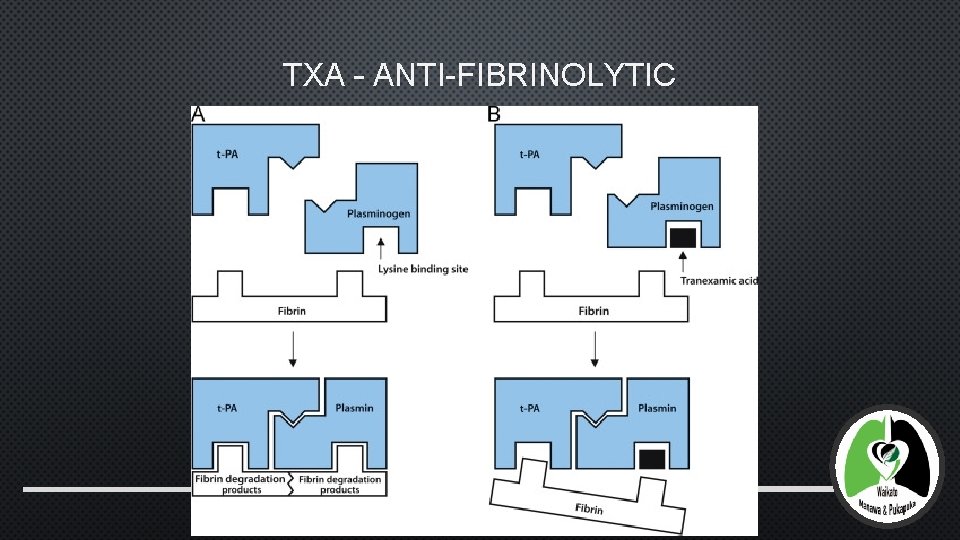
TXA – ANTI-FIBRINOLYTIC
BACKGROUND • COMMON CLINICAL QUESTION – AS PER WKT. CO. NZ, 857 INPATIENTS FOR WAIKATO CTS IN 2016 • ? ELECTIVE PROPORTION THAT ARE CABG/CARDIAC • ? INCIDENCE OF PERI-OPERATIVE BLEEDING AND SUBSEQUENT MORTALITY OR MORBIDITY • ? RISK OF POST-OPERATIVE SEIZURES GREATER THAN THE BENEFIT OF REDUCED BLEEDING AND RELATED COMPLICATIONS
OBJECTIVE • ‘… WHETHER TXA INCREASES THE RISK OF DEATH AND THROMBOTIC COMPLICATIONS AMONG AT-RISK PATIENTS UNDERGOING CORONARY-ARTERY SURGERY’ • (? IMPLICITY) TO RE-AFFIRM THE REDUCTION IN PERI-OPERATIVE BLEEDING PRIMARY OUTCOMES • COMPOSITE OF DEATH AND THROMBOTIC EVENTS, 30 DAYS POST-OP SECONDARY OUTCOMES • DEATH, NONFATAL MYOCARDIAL INFARCTION, MAJOR HAEMORRHAGE, CARDIAC TAMPONADE, AND A REQUIREMENT FOR TRANSFUSION, 30 DAYS POST-OP
METHODOLOGY
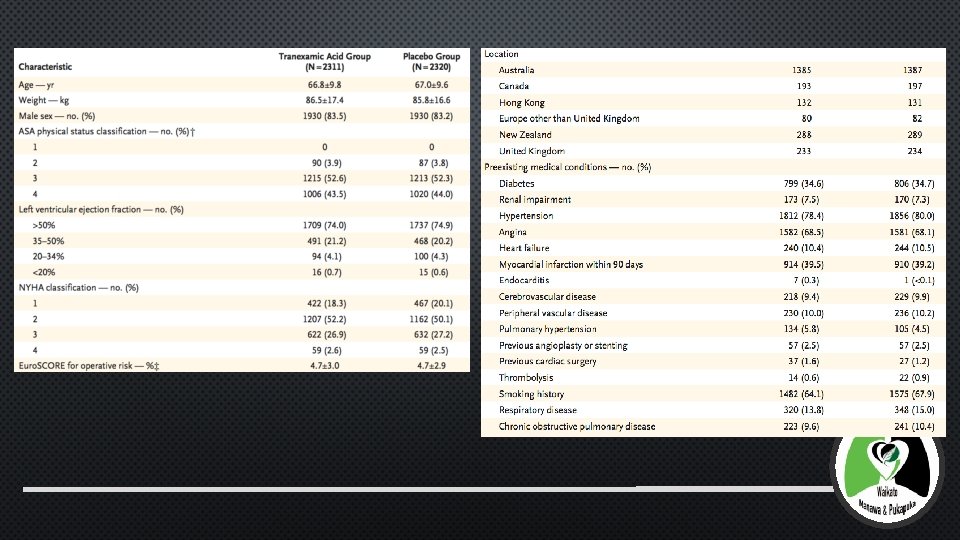
METHODS – ENTRY CRITERIA • ELECTIVE ON-PUMP OR OFF-PUMP CORONARY ARTERY SURGERYAT RISK FOR MAJOR COMPLICATIONS…
METHODS – INCLUSION CRITERIA • MEN AND WOMEN, AGED ≥ 18 Y • ANY OF THE FOLLOWING RISK FACTORS FOR MAJOR COMPLICATIONS: • AGE ≥ 70 Y • LV IMPAIRMENT • CONCOMITANT VALVULAR OR AORTIC SURGERY • LV ANEURYSMECTOMY • REPEATED CARDIAC SURGERY (“RE-DO”) • COPD • RENAL IMPAIRMENT • OBESITY • PULMONARY HTN • PVD
METHODS – EXCLUSION CRITERIA • • • • POOR (ENGLISH) LANGUAGE COMPREHENSION CLINICIAN PREFERENCE FOR ANTIFIBRINOLYTIC THERAPY URGENT SURGERY FOR UNSTABLE CORONARY SYNDROMES ACTIVE PEPTIC ULCERATION ALLERGY OR CONTRAINDICATION TO ASPIRIN ORT XA ASPIRIN THERAPY WITHIN 5 D OF SURGERY WARFARIN OR CLOPIDOGREL THERAPY WITHIN 7 D OF SURGERY GLYCOPROTEIN IIB/IIIA ANTAGONISTS WITHIN 24 H OF SURGERY THROMBOCYTOPENIA OR ANY OTHER KNOWN HISTORY OF BLEEDING DISORDER SEVERE RENAL IMPAIRMENT RECENT HEMATURIA THROMBOEMBOLIC DISEASE PREGNANCY
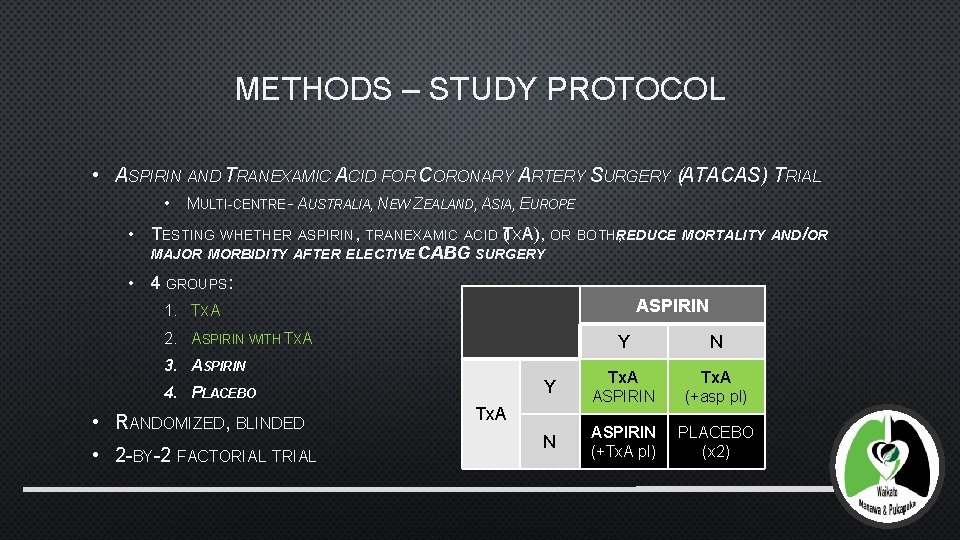
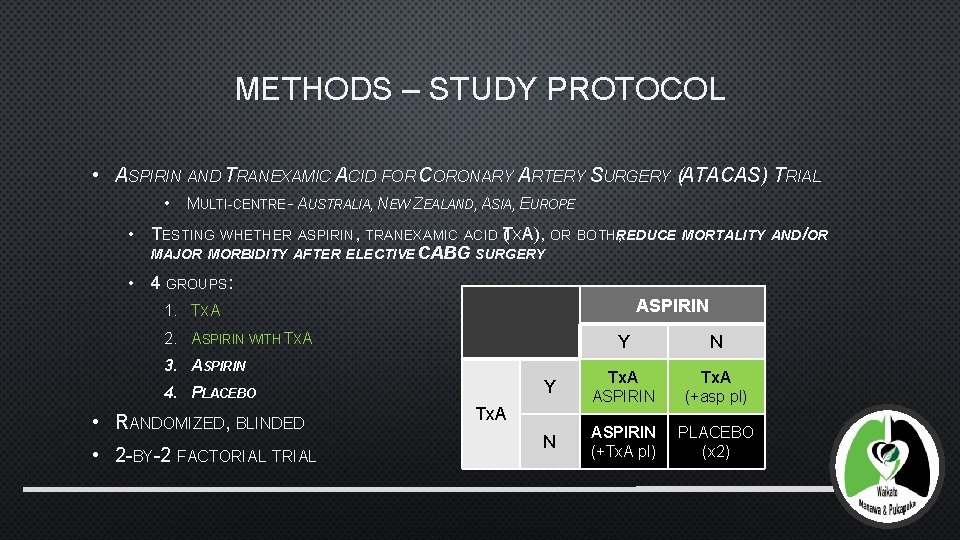
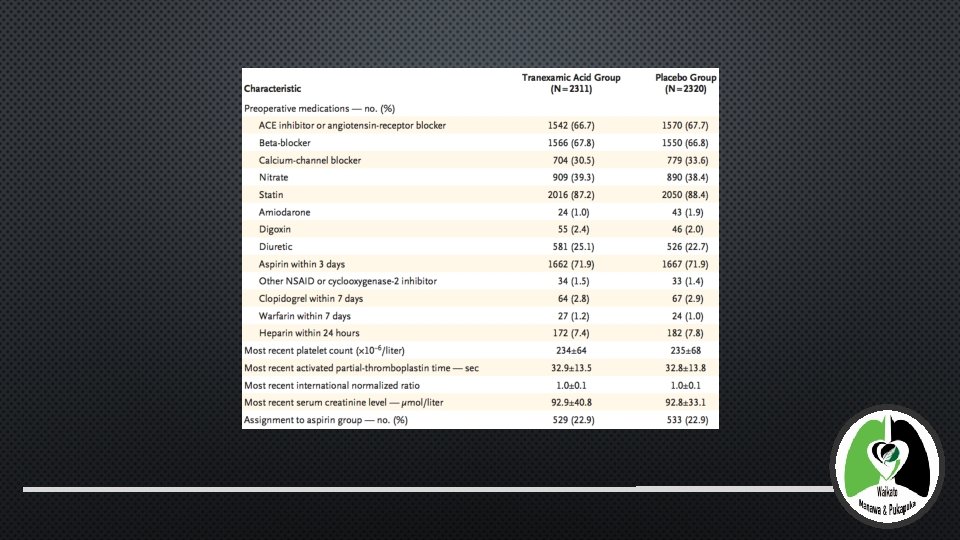
METHODS – STUDY PROTOCOL • ASPIRIN AND TRANEXAMIC ACID FOR CORONARY ARTERY SURGERY (ATACAS) TRIAL • MULTI-CENTRE – AUSTRALIA, NEW ZEALAND, ASIA, EUROPE • TESTING WHETHER ASPIRIN, TRANEXAMIC ACID (TXA), OR BOTHREDUCE , MORTALITY AND/OR MAJOR MORBIDITY AFTER ELECTIVE CABG SURGERY • 4 GROUPS: ASPIRIN 1. TXA 2. ASPIRIN WITH TXA Y N Y Tx. A ASPIRIN Tx. A (+asp pl) N ASPIRIN (+Tx. A pl) PLACEBO (x 2) 3. ASPIRIN 4. PLACEBO • RANDOMIZED, BLINDED • 2 -BY-2 FACTORIAL Tx. A
METHODS – SURGICAL DETAILS • ELECTIVE CABG, ON- OR OFF-PUMP • INCLUDING: • ANEURYSMECTOMY • CONCOMITANT VALVULAR OR AORTIC SURGERY • REDO • NB: EXCLUDING URGENT SURGERY FOR UNSTABLE CORONARY SYMPTOMS • STANDARD SURGICAL/PERIOPERATIVE CARE – INCL. SELECTION OF VEIN/ARTERY CONDUIT HARVESTING • HEPARIN
METHODS – TXA AND PLACEBO • TXA: 100 MG/KG BODY WEIGHT • PLACEBO: 0. 9% SALINE • >30 MINUTES AFTER THE INDUCTION OF ANAESTHESIA • SEIZURES OCCURRING DURING TRIAL, 1392 PTS ENROLLED • TXA DOSE HALVED
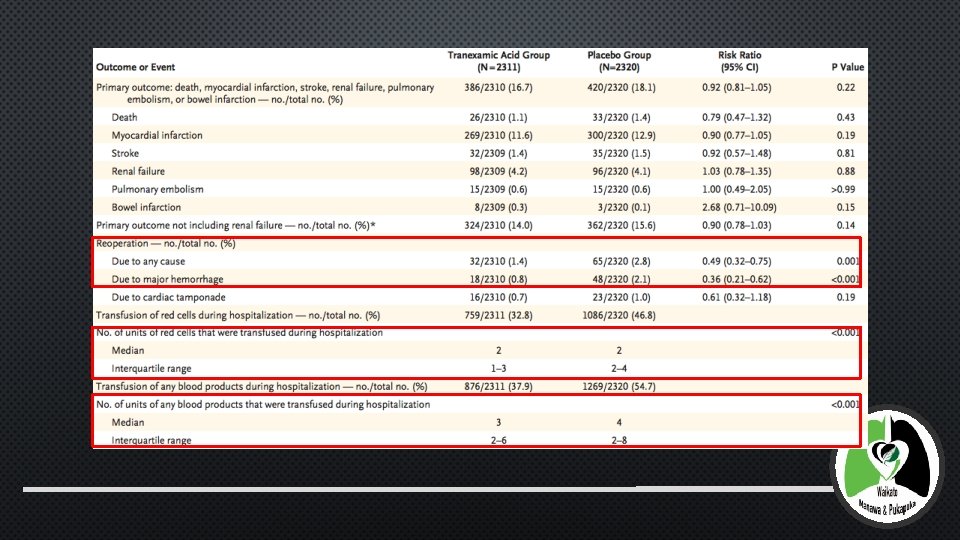
METHODS – PRIMARY ENDPOINTS • WITHIN 30 DAYS OF SURGERY • COMPOSITE: • DEATH • THROMBOTIC EVENTS: • NON-FATAL MI • STROKE • PE • ACUTE RENAL FAILURE • BOWEL INFARCTION
METHODS – SECONDARY ENDPOINTS • WITHIN 30 DAYS OF SURGERY • DEATH • NON-FATAL MI • MAJOR HAEMORRHAGE • CARDIAC TAMPONADE • BLOOD TRANSFUSION
METHODS – STATISTICAL ANALYSIS • PRIMARY OUTCOME: • ESTIMATED SAMPLE SIZE: 4484 PATIENTS • 90% POWER • 8. 5% (POOLED TRANEXAMIC) V 5. 95% (PLACEBO) DIFFERENCE • (ASPIRIN GROUP DISCONTINUED WHEN 2127 PTS ENROLLED) • NO INTENTION TO TREAT ANALYSIS • SUBGROUP SECONDARY ANALYSIS
RESULTS
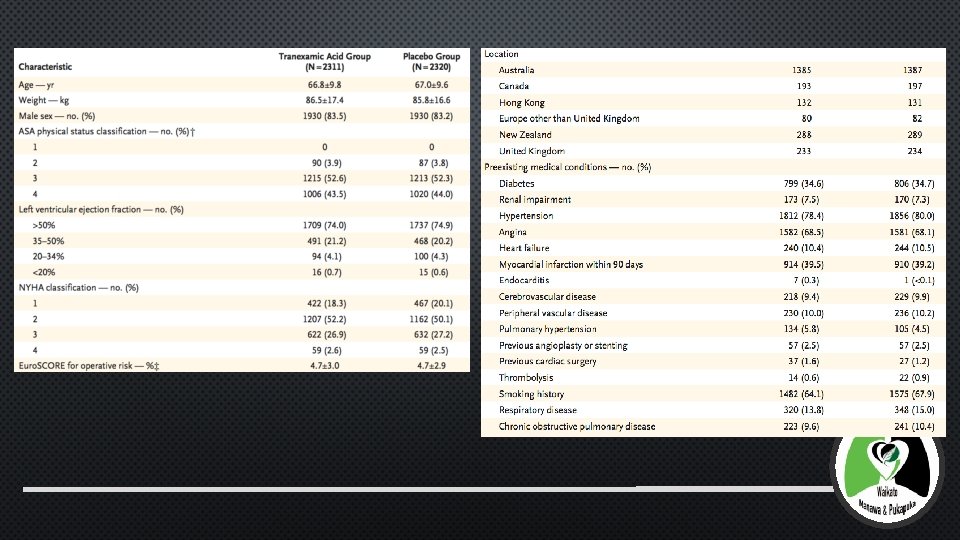
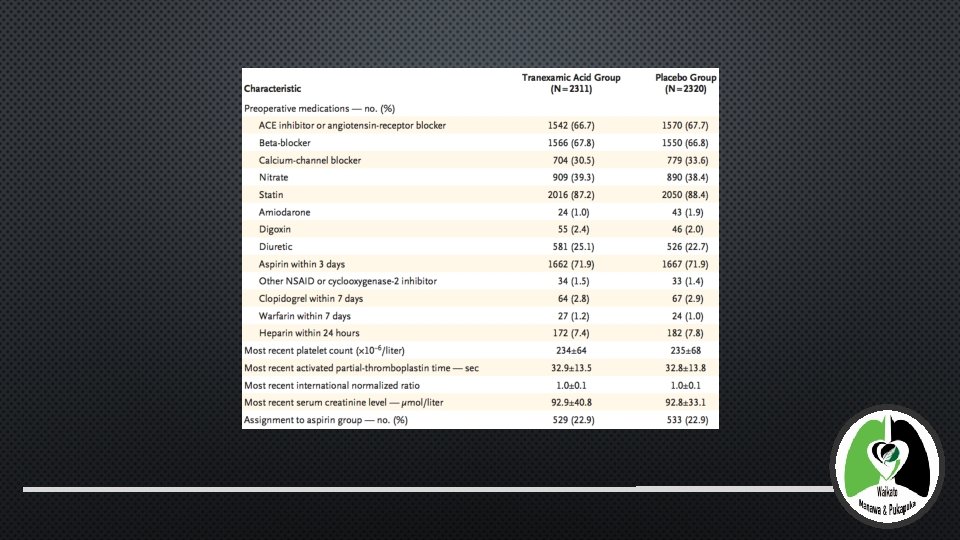
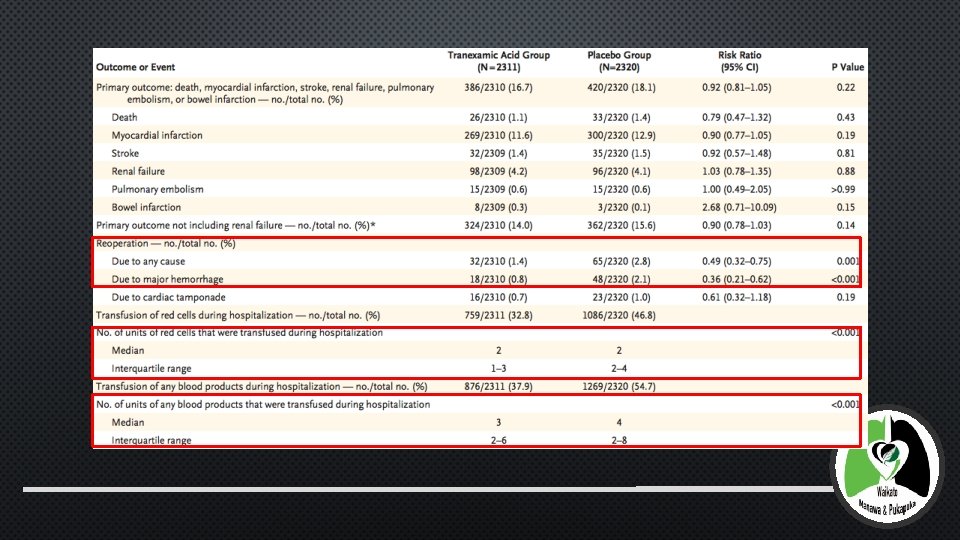
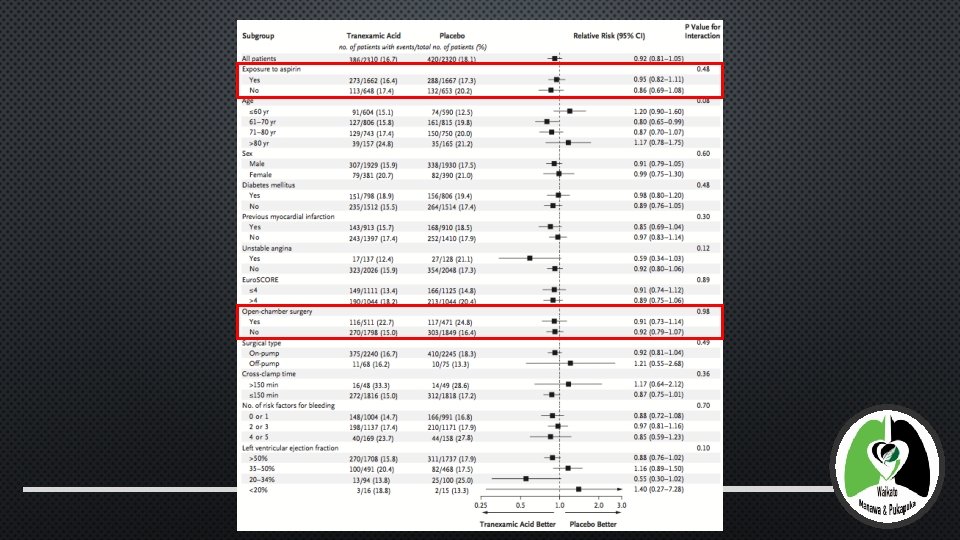
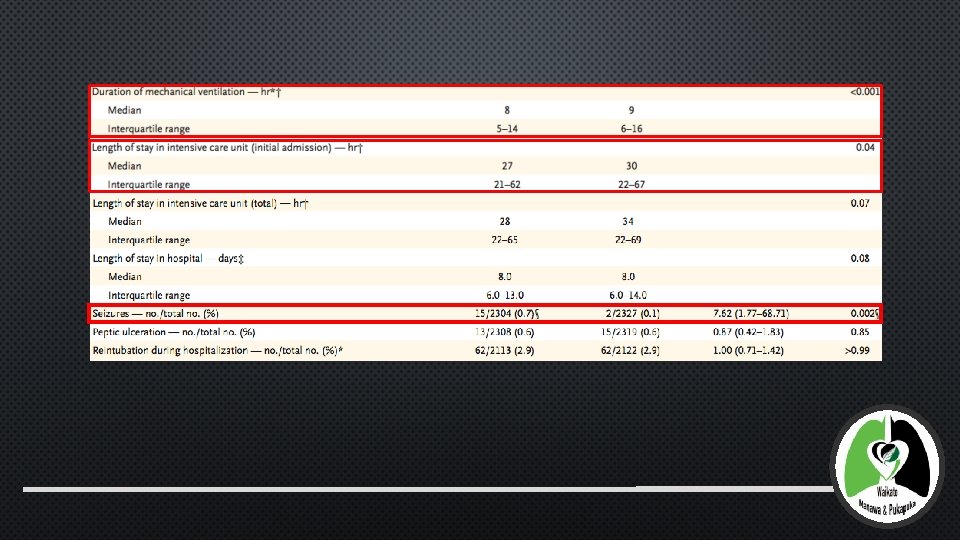
RESULTS (TABLES AND DIAGRAMS)
RESULTS • NUMBER NEEDED TO TREAT WITHTXA • TO PREVENT ONE RE-OPERATION • 30 DAYS POST-OP • 71 • RE-OPERATION ALSO HAD HIGHER MORTALITY AND THROMBOTIC COMPLICATIONS
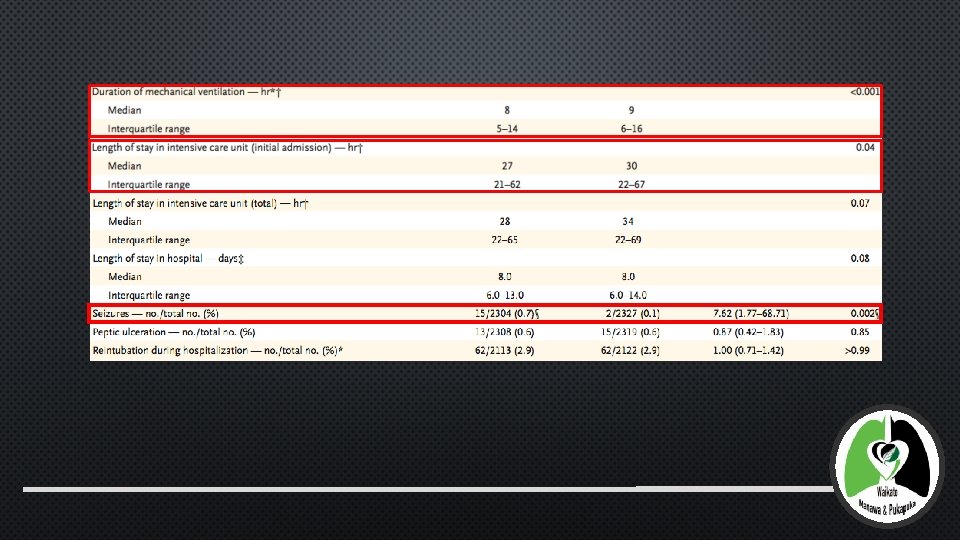
RESULTS • NUMBER NEEDED TO HARM WITHTXA • CAUSING 1 ADDITIONAL PATIENT TO HAVE 1 OR MORE SEIZURE • 30 DAYS POST-OP • 177 • PTS WHO HAD SEIZURES ALSO HAD HIGHER INCIDENCE OF STROKE
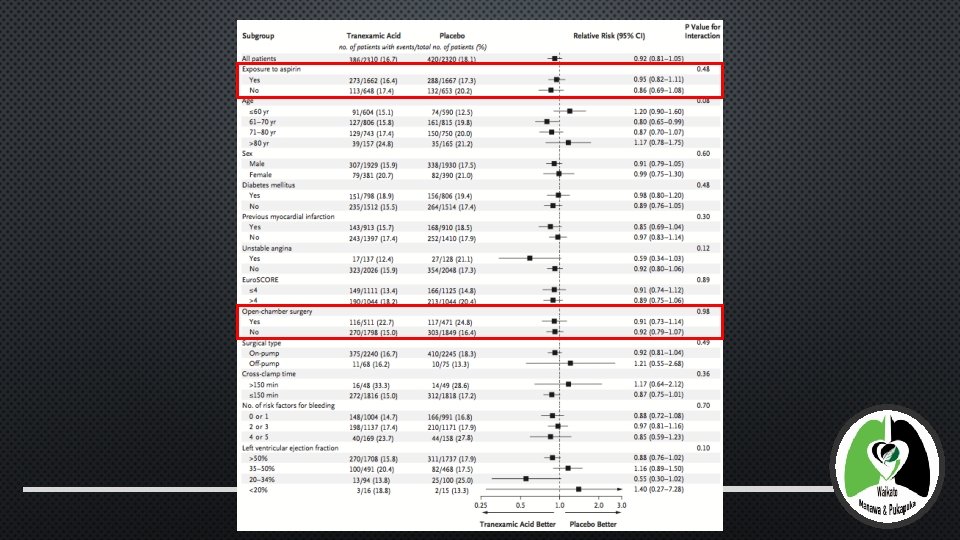
AUTHOR’S CONCLUSION • TXA DID NOT RESULT IN A HIGHER RISK OF MORTALITY OR THROMBOTIC COMPLICATIONS • TXA REDUCED THE RISK OF BLOOD LOSS, BLOOD TRANSFUSION AND REOPERATION • REDUCTION IN 57 U BLOOD PRODUCTS PER 100 PATIENTS • TXA INCREASED THE RISK OF POST-OP SEIZURES • CONVERSE: NO IMPROVED MORTALITY OR THROMBOTIC COMPLICATIONS WITHTXA • REDUCED ICU AND MECHANICAL VENTILATION – NOT TRANSLATED TO REDUCED HOSPITAL
DISCUSSION
STRENGTHS OF THE STUDY • LARGE SAMPLE SIZE • STATISTICALLY SIGNIFICANT RESULTS • RE-AFFIRMED BENEFIT OF TXA AND INCREASED RISK OF TXA TO REDUCE BLEEDING SEIZURES
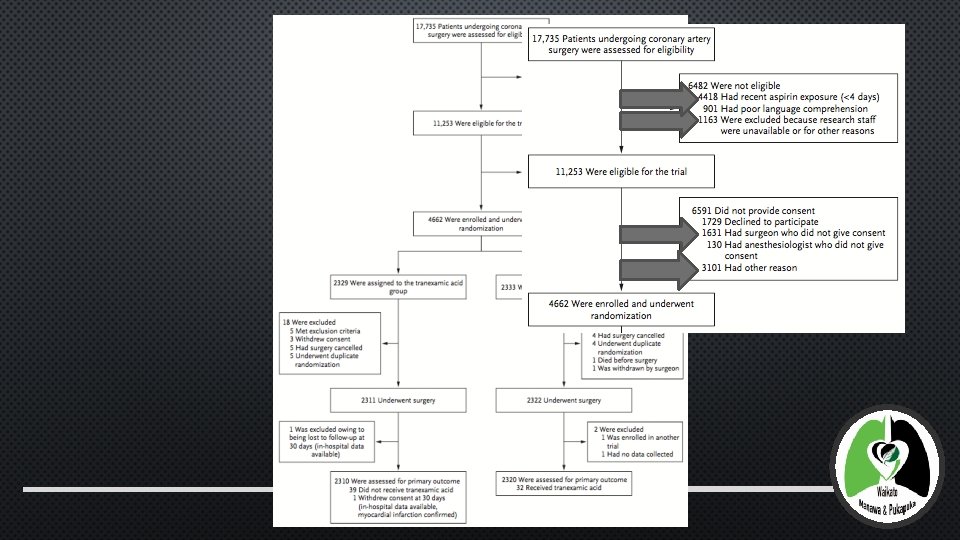
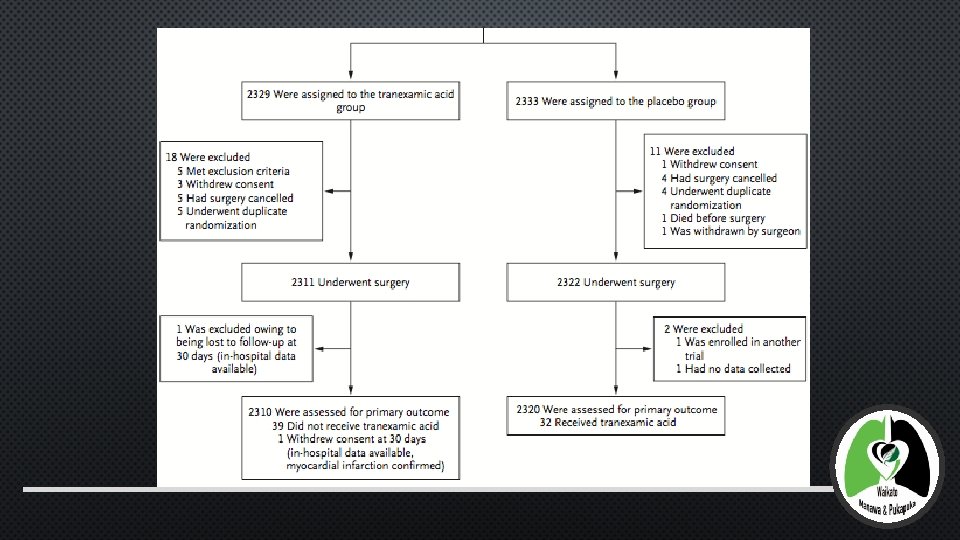
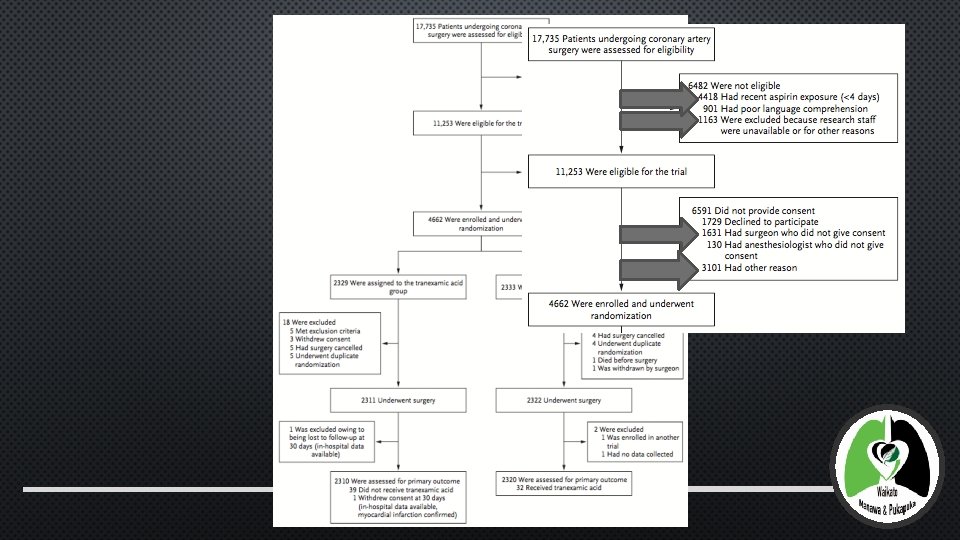
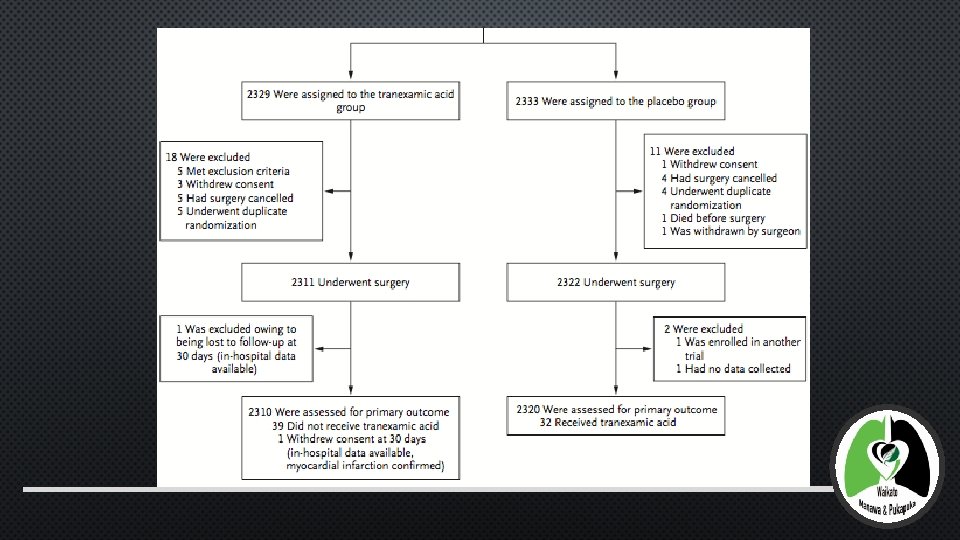
LIMITATIONS OF THE STUDY • LOSS OF PATIENTS DURING RECRUITMENT • ASPIRIN EXPOSURE • STAFFING RESOURCES • SURGEON/ANAESTHETIST PREFERENCE • OTHER REASON • ? ASPIRIN EFFECT ON RECRUITMENT
GENERAL DISCUSSION POINTS • RECRUITMENT AND STUDY STAGE - ? UNTIDY • DESPITE POWER AND SIGNIFICANT RESULTS, NO ADDITIONAL OR NEW EVIDENCE
IMPACT OF THE STUDY
HOW HAS THE STUDY IMPACTED ON PRACTICE • BALANCING THE RISK (? AND STIGMA) OF SEIZURES WITH THE BENEFITS OF REDUCTION IN BLEEDING • BLEEDING - ? IMPORTANT CLINICAL CONSEQUENCES… • MORTALITY, MORBIDITY • ECONOMIC/CLINICAL RESOURCES
ENDING QUESTION FOR AUDIENCE 1. BENEFIT: WILL IT REDUCE PERI-OPERATIVE BLEEDING? YES 2. RISKS: 1. WILL IT INCREASE THE RISK OF POST-OPERATIVE SEIZURES? YES 2. WILL IT INCREASE THROMBOTIC EVENTS? NO POSITIVE OR NEGATIVE EVIDENCE MULTIPLE LAYERS TO CONSIDER: • CLINICAL CONTEXT OF BENEFIT/RISK • PERCEIVED HARM
• MYLES PS, ET AL. STOPPING VS. CONTINUING ASPIRIN BEFORE CORONARY ARTERY SURGERY. N ENGL J MED 2016; 374: 728 -37. • ROBICH MP, KOCH CG, JOHNSTON DR, ET AL. TRENDS IN BLOOD UTILIZATION INU NITED STATES CARDIAC SURGICAL PATIENTS. TRANSFU- SION 2015; 55: 805 -14. • BIANCARI F, MIKKOLA R, HEIKKINEN J, LAHTINEN J, AIRAKSINEN KE, JUVONEN T. ESTIMATING THE RISK OF COMPLICATIONS RELATED TO RE-EXPLORATION FOR BLEEDING AFTER ADULT CARDIAC SURGERY: A SYSTEMATIC REVIEW AND META-ANALYSIS. EUR J CARDIOTHORAC SURG 2012; 41: 50 -5. • KER K, EDWARDS P, PEREL P, SHAKUR H, ROBERTS I. EFFECT OF TRANEXAMIC ACID ON SURGICAL BLEEDING: SYSTEMATIC REVIEW AND CUMULATIVE META-ANALYSIS. BMJ 2012; 344: E 3054. • MURKIN JM, FALTER F, GRANTON J, YOUNG B, BURT C, CHU M. HIGH-DOSE TRANEXAMIC ACID IS ASSOCIATED WITH NONISCHEMIC CLINI- CAL SEIZURES IN CARDIAC SURGICAL PATIENTSA. NESTH ANALG 2010; 110: 350 -3. • SHARMA V, KATZNELSON R, JERATH A, ET AL. THE ASSOCIATION BETWEEN TRANEXAMIC ACID AND CONVULSIVE SEIZURES AFTER CARDIAC SURGERY: A MULTIVARIATE ANALYSIS IN 11 529 PATIENTS. ANAESTHESIA 2014; 69: 124 -30. • WWW. WKT. CO. NZ/HOME • C. J. DUNN, ET AL. TRANEXAMIC ACID: A REVIEW OF ITS USE IN SURGERY AND OTHER INDICATIONS. DRUGS, 57 (1999), PP. 1005 -1032