Training and monitoring patients on home parenteral nutrition








- Slides: 25
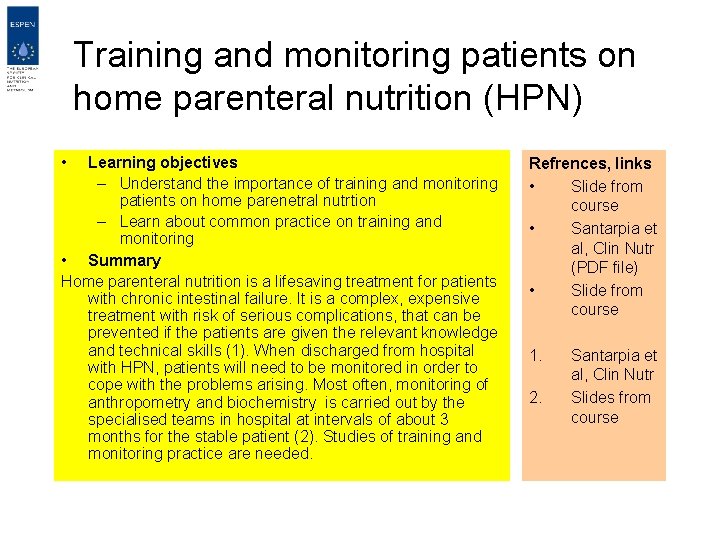
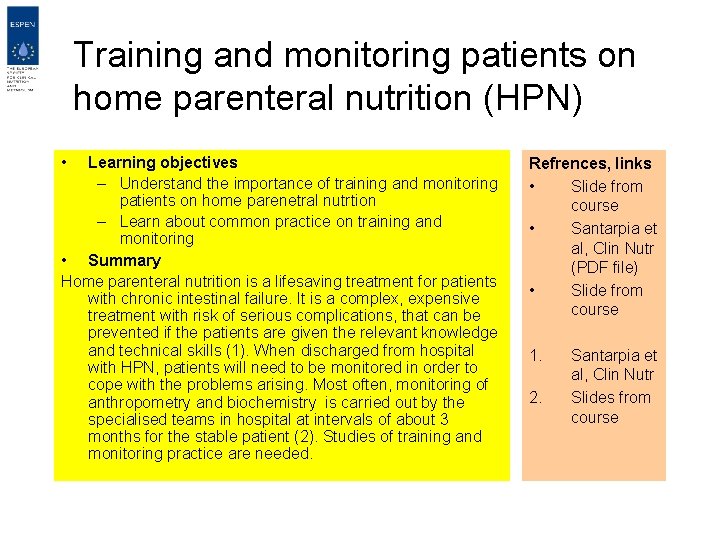
Training and monitoring patients on home parenteral nutrition (HPN) • Learning objectives – Understand the importance of training and monitoring patients on home parenetral nutrtion – Learn about common practice on training and monitoring • Summary Home parenteral nutrition is a lifesaving treatment for patients with chronic intestinal failure. It is a complex, expensive treatment with risk of serious complications, that can be prevented if the patients are given the relevant knowledge and technical skills (1). When discharged from hospital with HPN, patients will need to be monitored in order to cope with the problems arising. Most often, monitoring of anthropometry and biochemistry is carried out by the specialised teams in hospital at intervals of about 3 months for the stable patient (2). Studies of training and monitoring practice are needed. Refrences, links • Slide from course • Santarpia et al, Clin Nutr (PDF file) • Slide from course 1. 2. Santarpia et al, Clin Nutr Slides from course
Training patients for HPN • • • Training objectives The European practice Selection of patients for HPN The teaching program How to teach the patients ? Where are patients trained for HPN? Monitoring the skills Guidelines Conclusions
Training objectives • Patients or relatives able to manage procedures safely • Learn about complications and how to handle • Low rate of complications • To obtain the best quality of life
Teaching practice in Europe • Questionnaire based study • 51 centres in 7 countries • Range 0 -95 patients on HPN, 63 % of centres < 10 patients • Contraindication criteria • Teaching • Guidelines Home parenteral nutrition (HPN) teaching practice in Europe A. Micklewright. A. A. Prins, F. Bozzett!2, X. Hebuterne, J. M. Moreno Villares, M. Pertkiewicz, L. Pironi, M. Staun, P. Thul A. Van Gossum and the HAN-W group, Clin Nutr 2002; 21, 42, abstract.
Selection of patients for HPN • Criteria to exclude patients in 62 % of centres – Intellect (33%) – Physical disability (24 %) – Social situation, education (25%) – Underlying disease (18%) – Age (16%) Home parenteral nutrition (HPN) teaching practice in Europe A. Micklewright. A. A. Prins, F. Bozzett!2, X. Hebuterne, J. M. Moreno Villares, M. Pertkiewicz, L. Pironi, M. Staun, P. Thul A. Van Gossum and the HAN-W group, Clin Nutr 2002; 21, 42, abstract.

The teaching program The European survey reported the following: • Catheter care (100%) • Preventing and recognising complications (98%) • Most common mistakes (92%) • Pump care (92%) • Managing complications (90%) • Adding vitamins (55%) • Bag preparation (50%) • Intravenous medication (50%) Home parenteral nutrition (HPN) teaching practice in Europe A. Micklewright. A. A. Prins, F. Bozzett!2, X. Hebuterne, J. M. Moreno Villares, M. Pertkiewicz, L. Pironi, M. Staun, P. Thul A. Van Gossum and the HAN-W group, Clin Nutr 2002; 21, 42, abstract.
The impact of HPN training • Group A – Oral instruction, two sessions ’hands on’ – 91 port-a-cath, 26 tunnelled cath. • Group B – Detailed instruction theoretical and practical, written material etc – 68 port-a-cath, 45 tunnelled cath • Fewer infections in B (p<0. 001) Santarpia L, Pasanisi F, Alfonsi L, et al. Clin Nutr. 2002; 21: 207 -11.

How to teach the patients ? • Written manuals with photographic instructions • Videotapes • Interactive programs – ‘HPN-school’ with demonstrations, hands on and exercises by patients/relatives and community nurses – PC-based ?

Teaching the patient in the ward
Where are the patients trained for HPN? • At the ward of the discharging hospital – Involving the nutrition team – By far the most common procedure according to survey data • At home – By the team as an outgoing service – By a home care agency

Monitoring skills • Aim – Quality of life – Reduce rate of complications • Monitoring skills – When readmitted – Periodic surveys – Following the occurrence of complications

Guidelines training • The survey showed – 96% of centres had guidelines for training – 26 % had local guidelines – Guidelines based on national standards in some centres Home parenteral nutrition (HPN) teaching practice in Europe. A. Micklewright. A. A. Prins, F. Bozzett!2, X. Hebuterne, J. M. Moreno Villares, M. Pertkiewicz, L. Pironi, M. Staun, P. Thul A. Van Gossum and the HAN-W group, Clin Nutr 2002; 21, 42, abstract.
Training conclusions • Practice varies between centres – Training at hospital / home • Current practice based on local experience and guidelines • Prospective studies of different training regimens are warranted

Monitoring patients on HPN • Monitoring goals • Monitoring practice of HPN patients in Europe • Guidelines • Conclusions

Why monitoring HPN patients ? • Quality of life • Manage complications – Line infections – Mechanical problems – Thrombosis – Metabolic problems – Depression, social life
Monitoring practice in Europe • • Questionnaire based study in 2002 42 centres in 8 countries Experience 2 -30 years, 0 -125 patients 934 patients, 90% non-malignant disease, 54% on HPN > 1 year Wengler, A. Micklewright, X. Hebuterne, F. Bozzetti, M. Pertkiewicz, J. Moreno, L. Pironi, P. Thul, A. Van Gossum and M. Staun and The ESPEN HAN Working Group. Clin Nutr 2003; 22: s 87
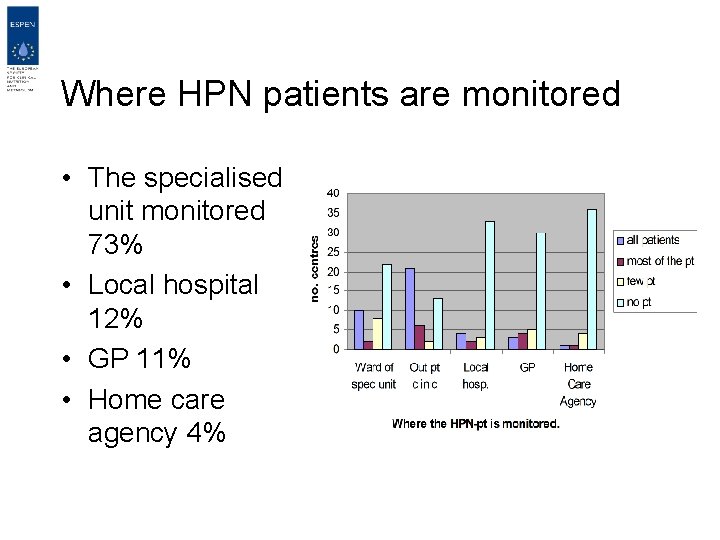
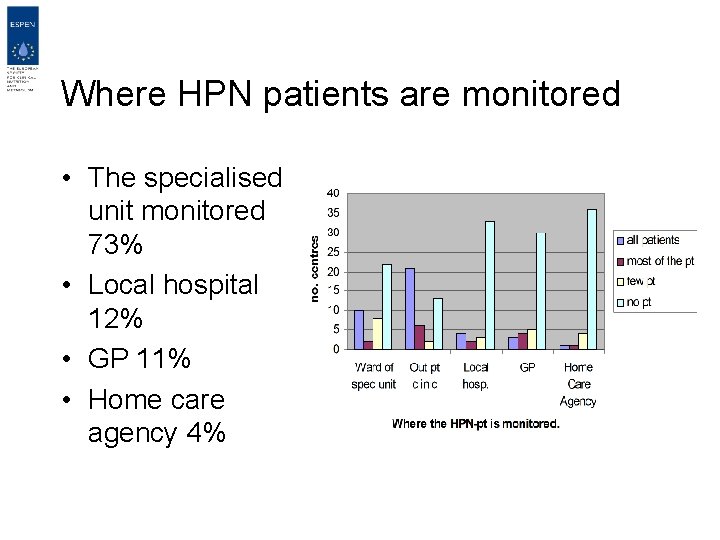
Where HPN patients are monitored • The specialised unit monitored 73% • Local hospital 12% • GP 11% • Home care agency 4%
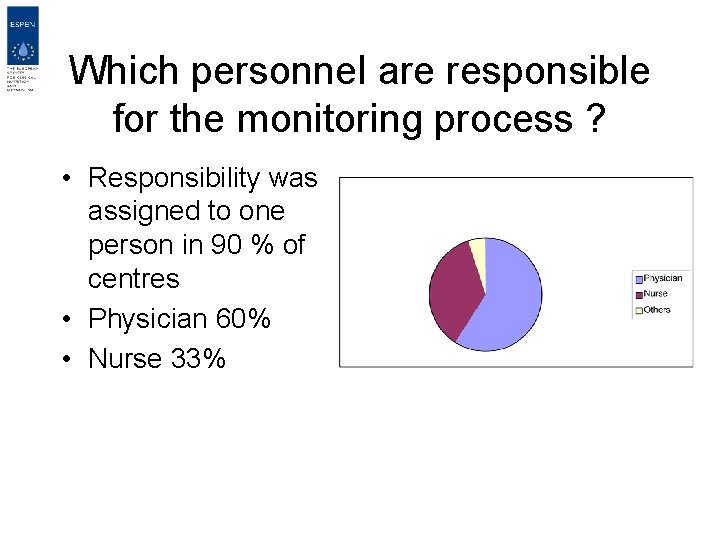
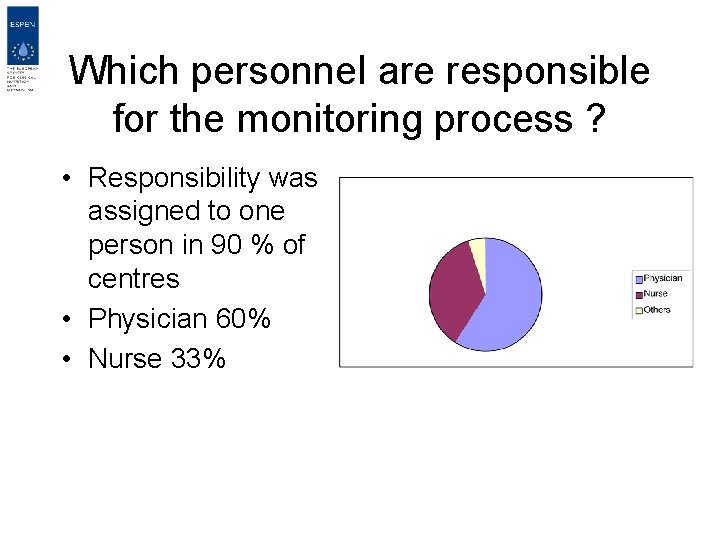
Which personnel are responsible for the monitoring process ? • Responsibility was assigned to one person in 90 % of centres • Physician 60% • Nurse 33%
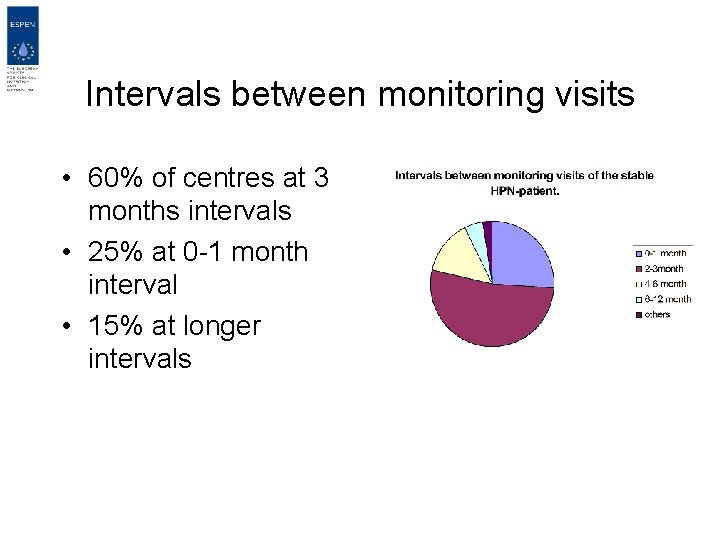
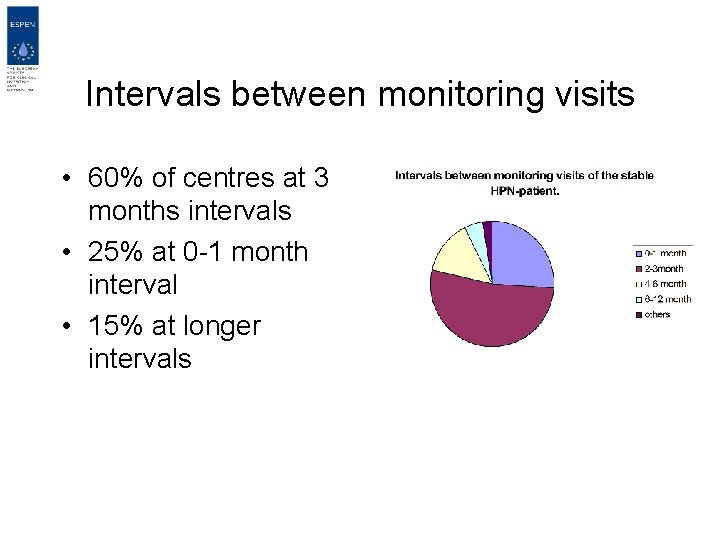
Intervals between monitoring visits • 60% of centres at 3 months intervals • 25% at 0 -1 month interval • 15% at longer intervals
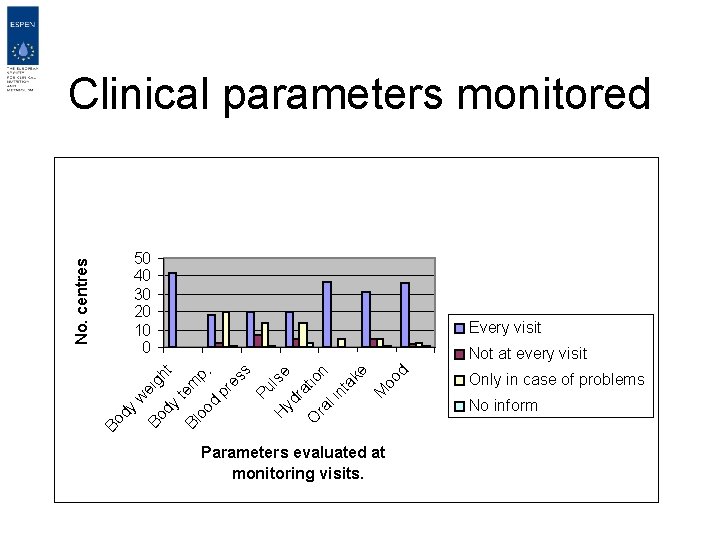
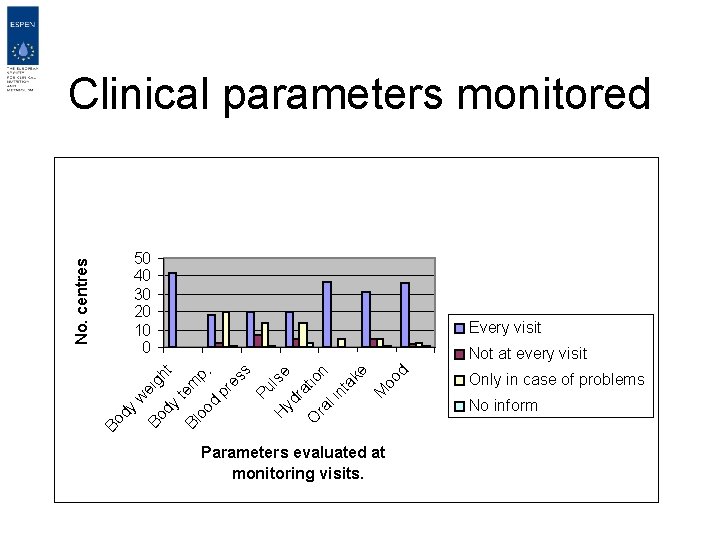
50 40 30 20 10 0 Every visit oo d M w Bo eig dy ht t Bl em oo p. d pr es s Pu ls H yd e ra ti O ra on li nt ak e Not at every visit Bo dy No. centres Clinical parameters monitored Parameters evaluated at monitoring visits. Only in case of problems No inform
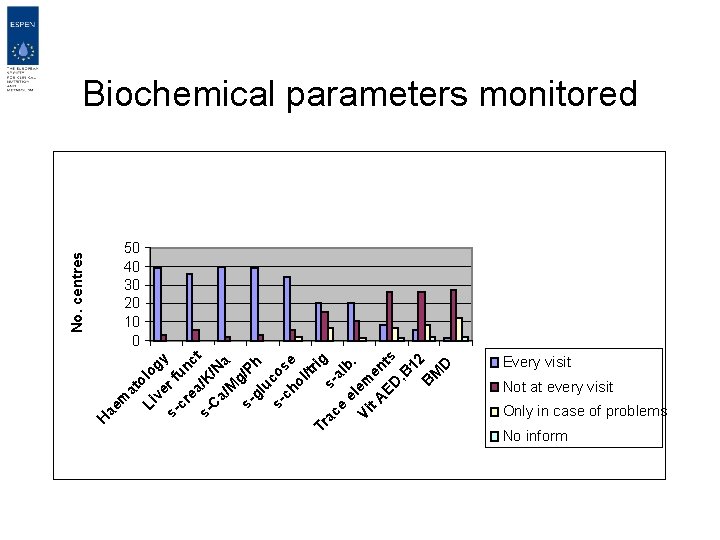
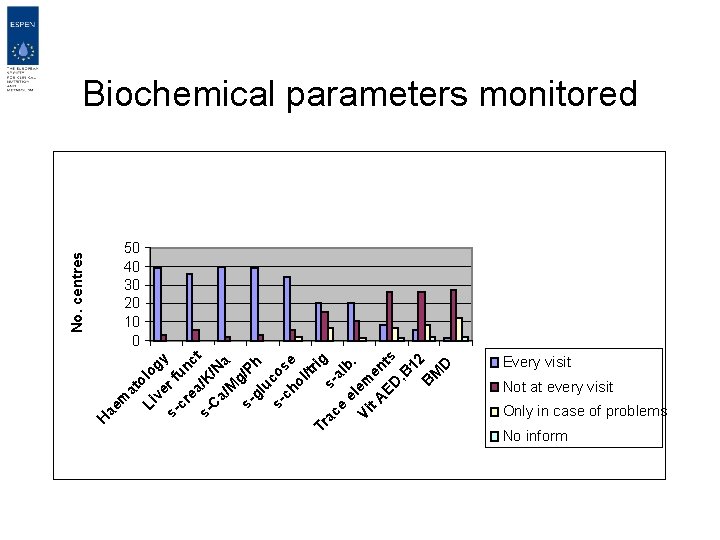
m at Li olo ve gy s- r f cr un ea ct s- /K / C a/ Na M g s- /P h gl uc s- os ch e ol /tr ig Tr ac sa e el lb. Vi em t A en ED ts , B 12 B M D ae H No. centres Biochemical parameters monitored 50 40 30 20 10 0 Every visit Not at every visit Only in case of problems No inform
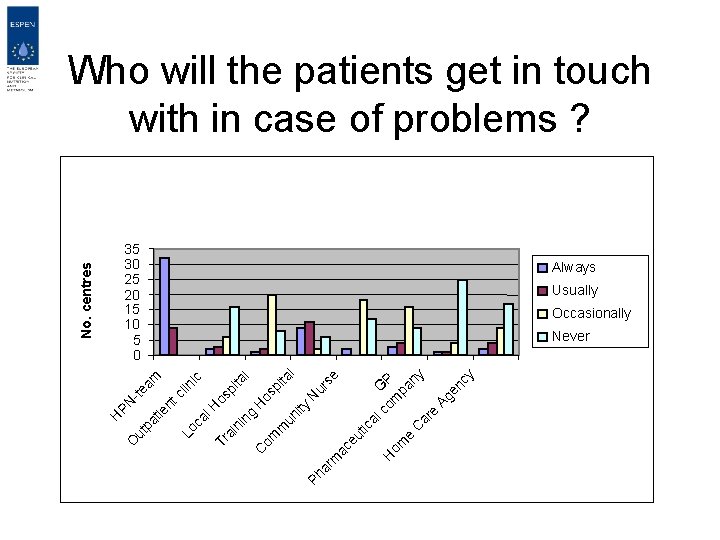
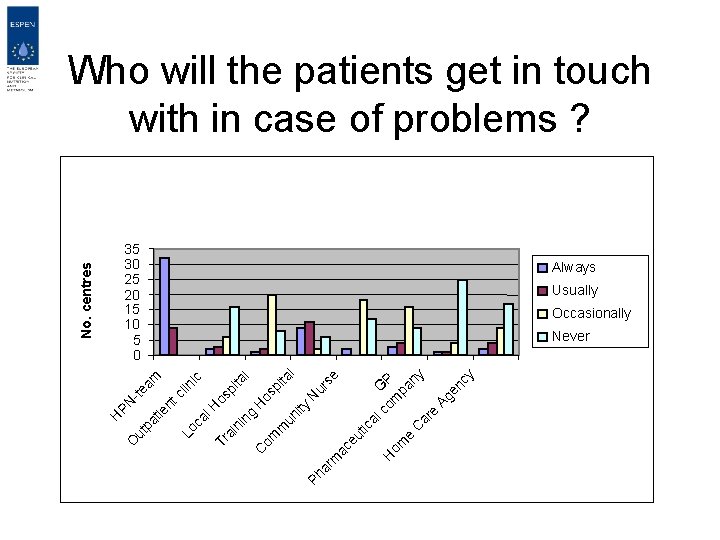
ty ur se N l pi ta l os H pi ta os ic ic al co GP H m om pa e ny C ar e Ag en cy ac eu t m Ph ar un i m om C ng Tr ai ni al H Lo c nt cl in am -te PN ie ut pa t O H No. centres Who will the patients get in touch with in case of problems ? 35 30 25 20 15 10 5 0 Always Usually Occasionally Never
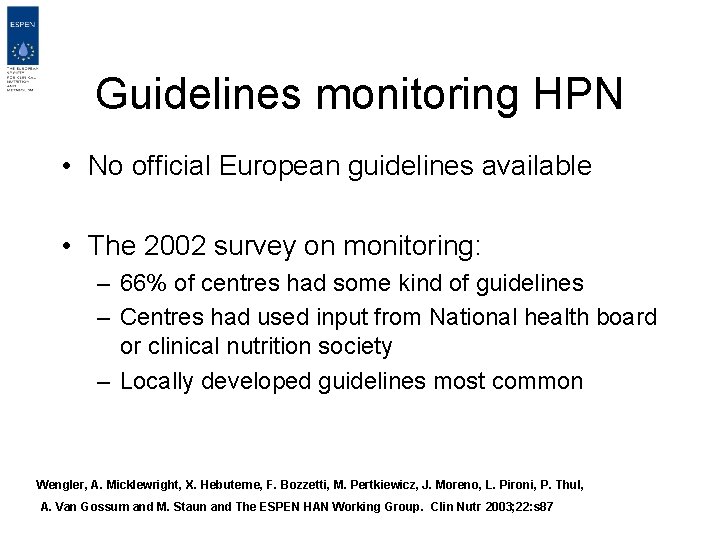
Guidelines monitoring HPN • No official European guidelines available • The 2002 survey on monitoring: – 66% of centres had some kind of guidelines – Centres had used input from National health board or clinical nutrition society – Locally developed guidelines most common Wengler, A. Micklewright, X. Hebuterne, F. Bozzetti, M. Pertkiewicz, J. Moreno, L. Pironi, P. Thul, A. Van Gossum and M. Staun and The ESPEN HAN Working Group. Clin Nutr 2003; 22: s 87

Summary and conclusion for monitoring HPN • Monitoring usually at discharging hospital – Access to specialised team • Intervals between visits vary, being on average 3 months – The unstable patient needs more attention • Biochemistry, anthropometry at all visits – Trace elements, vitamins and BMD occasionally • Official guidelines for monitoring not available – Prospective studies warranted
 How to calculate calories in dextrose solutions
How to calculate calories in dextrose solutions Continuous parenteral nutrition
Continuous parenteral nutrition Complication of parenteral nutrition
Complication of parenteral nutrition Ppn vs tpn
Ppn vs tpn Rxkinetics tpn
Rxkinetics tpn Tpn complication
Tpn complication Total parenteral nutrition cost
Total parenteral nutrition cost Small bowel obstruction
Small bowel obstruction Andreas leischker
Andreas leischker Nutrition monitoring definition
Nutrition monitoring definition Arti dari homecare
Arti dari homecare Perbedaan home care dan home visit
Perbedaan home care dan home visit Mobile home parks for sale in sc
Mobile home parks for sale in sc Plurals of flower
Plurals of flower Come home come home jesus is calling
Come home come home jesus is calling New mobile home sales oak springs mobile home community
New mobile home sales oak springs mobile home community Let's go to your house
Let's go to your house Arman home sweet home
Arman home sweet home She said that, home economics stands for the ideal home.
She said that, home economics stands for the ideal home. Home sweet home survival
Home sweet home survival Civil rights training certificate
Civil rights training certificate Nutrition focused physical examination
Nutrition focused physical examination Route of drug administration
Route of drug administration Mydriatics and miotics drugs
Mydriatics and miotics drugs Pharmacological and parenteral therapies
Pharmacological and parenteral therapies Moving lifting and transferring the patient
Moving lifting and transferring the patient