Tracheostomy Care Definition Tracheotomy n Surgical incision into




- Slides: 38
Tracheostomy Care
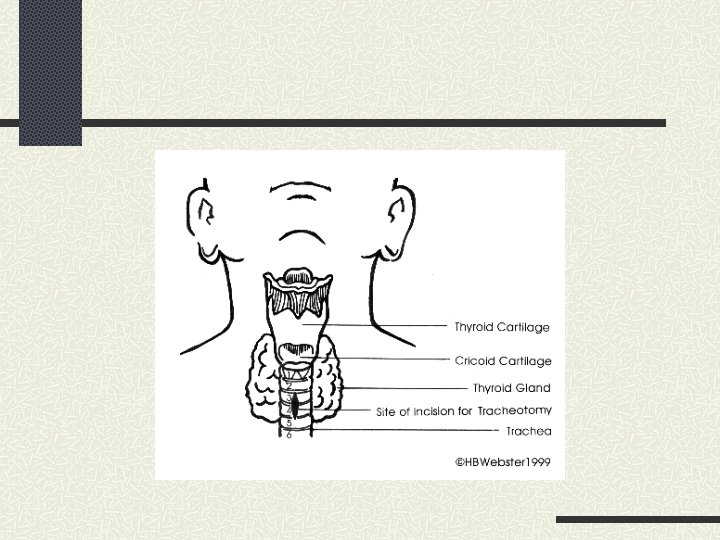
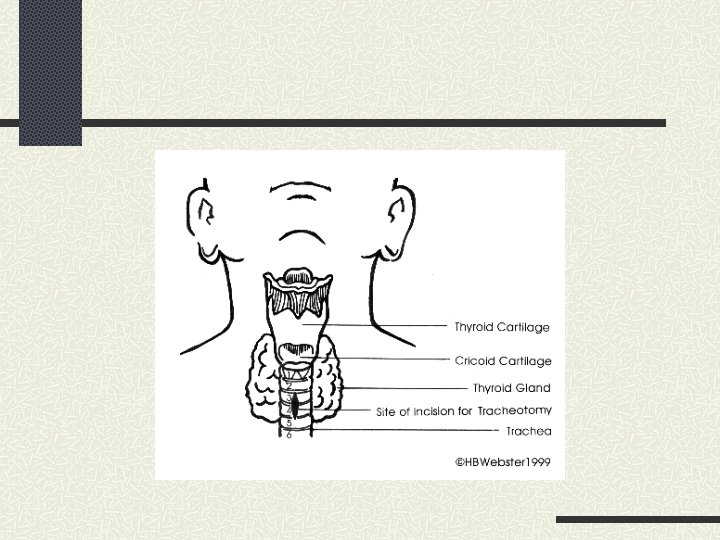
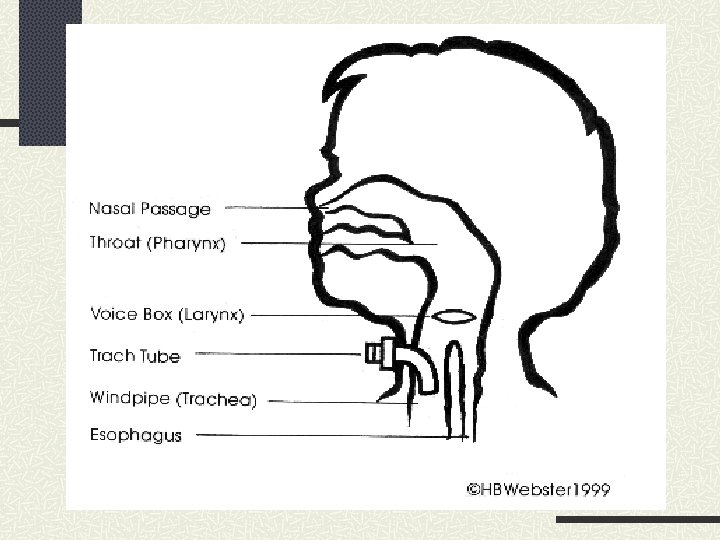
Definition Tracheotomy n Surgical incision into the trachea to establish an airway Tracheostomy n Stoma that results from tracheotomy
Indications for a Tracheostomy Tumor Stenosis: subglottic, tracheomalacia Congenital abnormalities of the airway: large tongue or small jaw Broncho Pulmonary Dysplasia Chronic pulmonary disease Chest wall injury Diaphragm dysfunction
Indications Bypass upper airway obstruction Facilitate removal of secretions Long-term mechanical ventilation Permit oral intake and speech in patient who requires long-term mechanical ventilation
Advantages Less risk of long-term damage to airway Increased comfort Patient can eat. Increased mobility because tube is more secure
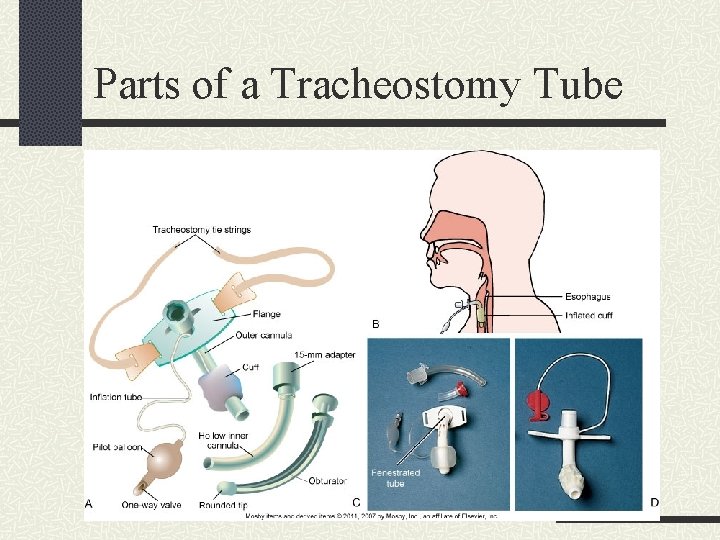
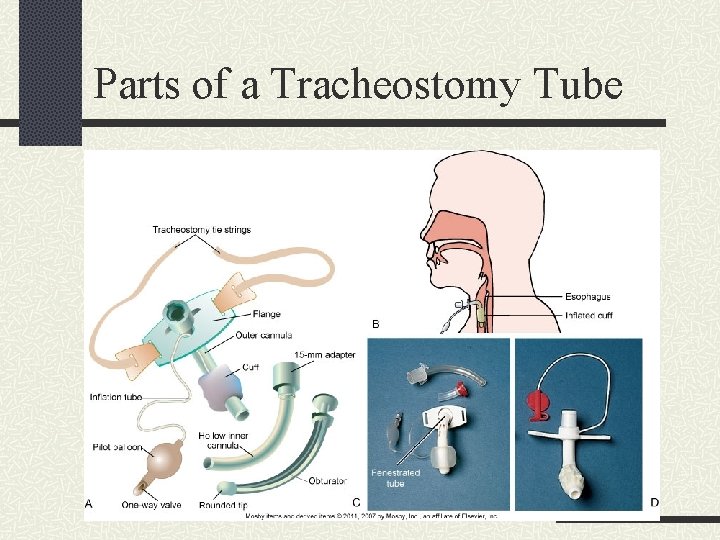
Parts of a Tracheostomy Tube
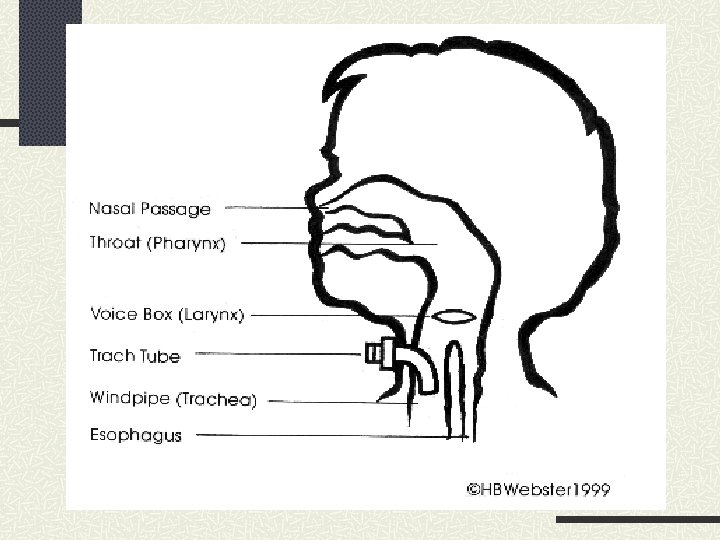
Tracheostomy Care Tubes contain a faceplate or flange. n Rest on neck between clavicles and outer cannula During insertion, obturator is placed inside outer cannula, with rounded tip protruding from end to ease insertion.
Tracheostomy Care After insertion, obturator must be immediately removed to allow airflow. Keep obturator near bedside in case of decannulation. Some tubes have a removable inner cannula for easier cleaning.
Tracheostomy Care involves Suctioning the airway to remove secretions n Cleaning around stoma n Changing ties n Providing inner cannula care n
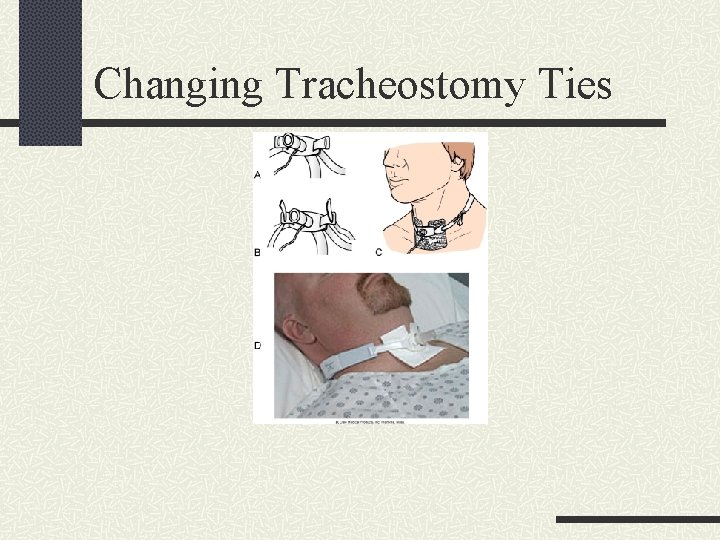
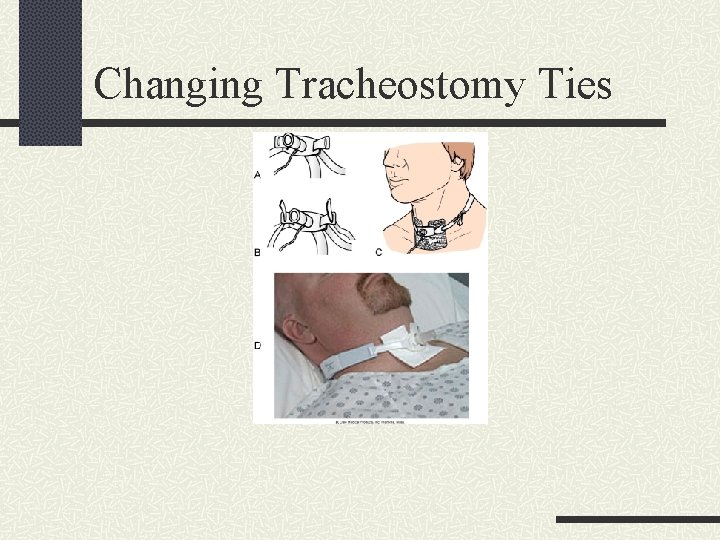
Changing Tracheostomy Ties

Tracheostomy Care Tube with inflated cuff is used for risk of aspiration or in mechanical ventilation. n Inflate cuff with minimum volume required to create an airway seal. n Should not exceed 20 mm Hg or 25 cm H 2 O
Tracheostomy Care Excessive cuff pressure can Compress tracheal capillaries n Limit blood flow n Predispose to tracheal necrosis n
Tracheostomy Care Minimal leak technique (MLT) Inflate cuff with minimum amount of air to form seal. n Then withdraw 0. 1 m. L of air. n Risk for aspiration n Not used if trach is bypassing upper airway construction n
Tracheostomy Care Deflation To remove secretions accumulating above the cuff n Patient should cough up secretions before deflation to avoid aspiration. n Suction mouth and tube. n During exhalation as gas helps propel secretions into mouth n Patient should cough and be suctioned again. n
Tracheostomy Care Deflation Assess patient’s ability to protect airway from aspiration. n Remain with patient when cuff is initially deflated, unless patient can protect against aspiration and breathe without respiratory distress. n When patient can protect against aspiration and does not require mechanical ventilation, a cuffless tube is used. n
Tracheostomy Care Reinflation During inspiration n Monitor inflation volume daily as it may ↑ with tracheal dilation from cuff pressure. n
Tracheostomy Care Retention sutures Placed in tracheal cartilage during tracheostomy n Free ends taped to skin and left accessible in case tube is dislodged n

Tracheostomy Care Precautions for tube replacement n n n Tube of equal or smaller size kept at bedside for emergency reinsertion Tapes not changed for at least 24 hours after insertion First change by physician no sooner than 7 days after tracheostomy
Tracheostomy Care Accidental dislodging Immediately replace tube. n Spread opening with retention sutures grasped or hemostat. n Insert obturator into replacement tube. n n Lubricated with saline poured over tip n Inserted at 45 degrees to neck
Tracheostomy Care Another method for reinsertion Insert suction catheter to allow for air passage and to serve as a guide for obturator. n Tube should be threaded over catheter and suction catheter removed. n
Tracheostomy Care If tube cannot be replaced Assess level of respiratory distress n Minor dyspnea may be alleviated with semi. Fowler’s position n Severe distress may progress to respiratory arrest n Cover stoma with sterile dressing and ventilate with bag-mask until help arrives n

Tracheostomy Care Initially should receive humidified air. Tube should be changed monthly. Patient can be taught to change tube using clean technique at home.
Swallowing Dysfunction Inflated cuff Interferes with normal function of muscles used to swallow n Evaluate risk of aspiration with cuff deflated, or substitute with a cuffless tube. n
Swallowing Dysfunction Evaluate aspiration Add blue coloring to clear liquid and evaluate coughing and secretions, or suction trachea for blue fluid. n Test tracheobronchial secretions for glucose (mucus is generally very low). n
Speech Techniques to promote speech Spontaneously breathing patient may deflate cuff, allowing exhaled air to flow over vocal cords. n Patient on mechanical ventilation can allow constant air leak around cuff. n
Speech Techniques to promote speech Tracheostomy tubes and valves have been designed to facilitate speech. n Promote use to provide psychologic benefit and self-care. n

Speaking Tracheostomy Tubes
Speech Fenestrated tube has opening on surface of outer cannula to permit airflow over vocal cords to allow Spontaneous breathing through larynx n Speech n Secretion expectoration with tube in place n
Speech Fenestrated tube Requires frequent suctioning n Ability to swallow is determined before use. n Frequently assess for signs of respiratory distress on first use. n Potential for development of tracheal polyps n
Speech Speaking tracheostomy has two pigtail tubings One connects to cuff for inflation. n Other connects to opening just above cuff. n When second tube is connected to low-flow air source, this permits speech. n
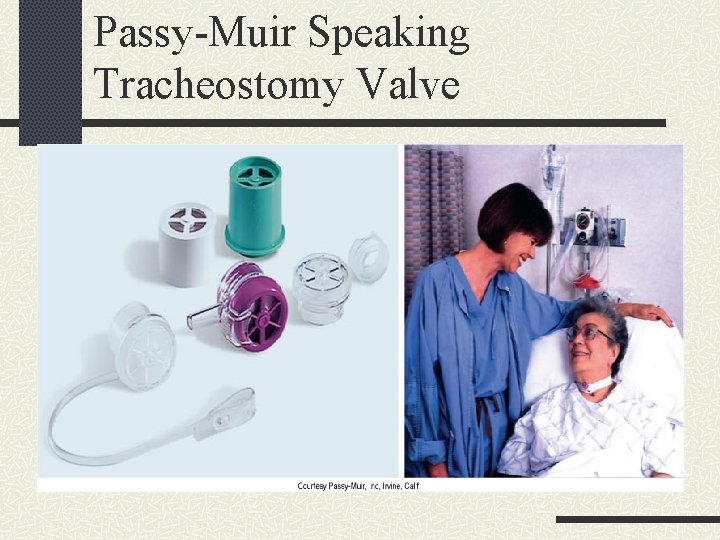
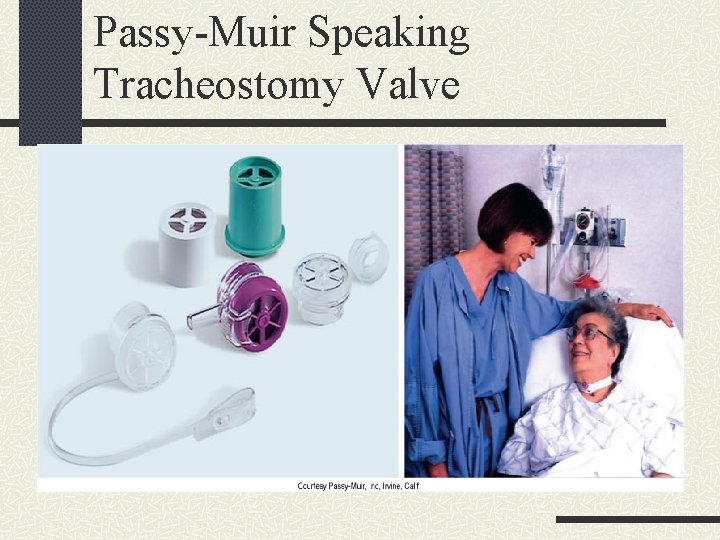
Passy-Muir Speaking Tracheostomy Valve
Speech Ability to tolerate cuff deflation without aspiration or respiratory distress must be evaluated. n If no aspiration, cuff is deflated and valve is placed over opening.
Speech Provide patient with writing tools if speaking devices are not used.
Decannulation When patient can adequately exchange air and expectorate Stoma closed with tape and covered with occlusive dressing n Instruct patient to splint stoma with fingers when coughing, swallowing, or speaking n
Decannulation Tissue forms in 24 to 48 hours. Opening will close in several days without surgical intervention.
After Decannulation The stoma begins closing as soon as the trach tube is removed. This may take months to achieve final closure. Until closed by nature or surgery, need to keep opening covered. Bandaids work nicely for this; change as needed.